Abstract
Purpose
To evaluate the rate of sterile endophthalmitis (SE) following intravitreal injection of three different formulations of triamcinolone acetonide (TA) in a single physician practice and also to assess the mean diameter and concentration of particles of the two TA formulations currently available commercially in the USA. It was hypothesized that TA formulations with smaller particles and/or greater concentrations would have a higher incidence of SE.
Methods
Single-site, interventional case series in which the medical records of 392 consecutive eyes receiving intravitreal TA as Triesence®, Kenalog®-40, or preservative-free TA between September 2008 and October 2013 were retrospectively reviewed for the incidence of SE. Particle sizing of TA formulations was conducted by an independent commercial laboratory.
Results
Five cases of SE were identified. The four cases of SE following Triesence® (4.6%) represented a rate significantly higher than the one case of SE following preservative-free TA (0.6%; P=0.049) and the 0% incidence rate of SE following Kenalog®-40 (P=0.0210). Triesence® had significantly smaller particles than Kenalog®-40 (P<0.0001).
Conclusion
The rate of SE was the highest with the formulation of TA that had the smallest particle size and highest particle load (number of particles injected). The lowest rate of SE was seen with Kenalog®-40, the only TA formulation that contained a benzyl alcohol preservative. The data do not support a principal causative role of benzyl alcohol in the development of TA-induced SE. Instead, the data support the particle theory of TA-induced SE; however, larger-scale, multicenter studies are needed to confirm and expand on these findings.
Keywords: sterile endophthalmitis, benzyl alcohol, Triesence®, Kenalog®-40, preservative-free triamcinolone acetonide, particle size, frustrated phagocytosis
Introduction
Since the early preclinical work of Tano et al1 and the subsequent initial report in 1995 of its use in humans to treat exudative macular degeneration,2 the administration of intravitreal triamcinolone acetonide (IVTA) has become a common and useful therapy for a variety of vitreoretinal diseases (for review, see the work by Tao and Jonas3). The most common adverse events associated with IVTA are elevated intraocular pressure4 and progression of cataracts.5 Less frequent events include postinjection infectious6 and noninfectious endophthalmitis,7–10 including pseudoendophthalmitis.11 Infectious endophthalmitis is a potential consequence following any intravitreal injection. Noninfectious endophthalmitis and pseudoendophthalmitis, however, are more prevalent following IVTA compared to any other intravitreally injected pharmaceutical agent.12
Noninfectious or sterile endophthalmitis (SE) is an acute, severe, usually painless postinjection inflammatory response. It typically develops within 1 day following intravitreal injection and often results in a significant decrease in visual acuity. SE can involve both the anterior chamber and the vitreous, and hypopyon is often present. Pseudoendophthalmitis is the migration of TA crystals into the anterior chamber after intravitreal TA injection without secondary inflammation in the vitreous or anterior chamber. Pseudoendophthalmitis crystals are easily differentiated from a hypopyon.
The rate of SE following IVTA is variable and may be underestimated because some cases may not be reported by the patient or detected by the physician if follow-up is extended and the inflammatory reaction spontaneously regresses. Estimates of the rates of SE following IVTA range from 0.1% of injections13 to 23.8%.14 In some reports, rates may be inflated by the inclusion of cases of pseudoendophthalmitis and, more rarely, cases of infectious endophthalmitis. Further complicating the accurate assessment of the rate of SE following IVTA is the apparent temporal clustering of cases. Jonisch et al15 reported a rate of SE of 1.9% in patients receiving IVTA from January 2005 through July 2006, which increased to a rate of 9.3% of eyes injected from May through July 2006. Stepien et al16 reported a similar clustering of cases in spring 2006 and suggested that a change in formulation or manufacturing may have been involved.
The pathogenesis of SE following IVTA remains unknown. The benzyl alcohol preservative found in Kenalog®-40 (Bristol-Myers Squibb, New York, NY, USA) has been suggested as a factor,17 and the Kenalog®-40 package insert states that intraocular injection “is not recommended because of potential toxicity from the benzyl alcohol”.18 Owing to concerns with benzyl alcohol, the American Academy of Ophthalmology requested that Bristol-Myers Squibb develop a preservative-free formulation of Kenalog®-40.19 Preservative-free formulations of TA (PFTA) subsequently became available from compounding pharmacies, but have mostly been replaced by an FDA (US Food and Drug Administration)-approved PFTA marketed for intraocular use (Triesence®, Alcon Laboratories, Inc., Fort Worth, TX, USA). A second PFTA has received FDA approval for intraocular use (Trivaris™, Allergan Inc., Irvine, CA, USA), but it has not been marketed. Despite the removal of benzyl alcohol, TA-induced SE has not been eliminated.20
Other factors have been suggested as possible etiological factors for the development of SE, including the presence of endotoxins21 and the potential of TA crystals to directly produce inflammation.22 Here, we report a single-center, retrospective, consecutive case series analysis of the rate of SE following intravitreal injections of Triesence®, Kenalog®-40, and PFTA. We also report the results of a particle size analysis comparing Triesence® and Kenalog®-40. The incidence of SE was significantly greater in Triesence®-treated eyes compared to the other two formulations. We hypothesize that the smaller particle size of Triesence® produces a greater particle load, which increases its tendency to produce SE.
Methods
This was a single-site, interventional case series in which the medical records of 392 consecutive eyes receiving intravitreal TA as Triesence®, Kenalog®-40, or PFTA (Leiter’s Compounding Pharmacy, San Jose, CA, USA) between September 2008 and October 2013 were retrospectively reviewed for the incidence of SE. SE was defined as the presence of inflammation in the anterior chamber and vitreous cavity associated with a painless decrease in visual acuity within 1 day of intravitreal injection. Eyes with pseudoendophthalmitis were excluded. A minimum of three different lots of each formulation of TA were used. Additionally, the mean particle sizes for the commercially available formulations of TA were assessed. The study was reviewed by the Springfield Committee for Research Involving Human Subjects and granted an exemption. Patients gave informed consent for treatment. In conducting the study, no patient identifiers were recorded or reported.
All injections followed a standard protocol. Eyes were anesthetized with 2% lidocaine hydrochloride jelly, USP, and a controlled aseptic technique was used. A drop of 5% povidone–iodine (PVI) solution was instilled in each treated eye, followed by a gentle wiping of the eyelids and lashes (both upper and lower) as well as surrounding skin with 10% PVI-soaked swabs. Gloves were worn by the treating physician, and a sterile lid speculum was placed between the lids. Triesence® was administered via a 30-gauge needle, and Kenalog®-40 and PFTA were administered via a 27-gauge needle through the pars plana. A drop of 5% PVI was placed in the eye after injection and the lid speculum removed. For injections prior to September 2011, antibiotic drops (moxifloxacin or gatifloxacin) were used for 2 days postinjection, as was common practice. Since that time, antibiotic drops have not been used postinjection. Patients with SE invariably returned within 24 h of treatment, reporting a severe, painless decrease in vision in the treated eye.
Particle sizing of Kenalog®-40 (lot numbers 3G75654 and 3G73804) and Triesence® (lot numbers 221360F and 214166F) was conducted by an independent commercial laboratory (Particle Technology Labs, Downers Grove, IL, USA) using a Model 770 Accusizer (Particle Sizing Systems, Port Richey, FL, USA), a single-particle optical-sensing instrument of high resolution (lower size limit: 0.50 μm). In order to measure nonaggregate, primary particle sizes, a carrier/dispersing solution of Triton X-100 (1 g/L, Integra Chemical Co, Kent, WA, USA) was utilized. The carrier solution was filtered (0.22 μm), and samples were diluted to achieve a concentration of 5,500–7,000 particles/mL. Samples were dispersed by ultrasonication for a timed 30 s, and data were collected from a volume of 60 mL across 60 s. Mean particle size was calculated for a minimum of 88,000 particles for each TA formulation/lot based on a volume distribution.
Photographs of Kenalog®-40 and Triesence® were taken both in Triton X-100 as well as in aggregating conditions in balanced salt solution using a Nikon Labophot-Pol with Clemex Vision Lite 4.0 software at a magnification of 400×.
Statistical analyses
Rates of SE were compared statistically using Fisher’s exact tests. A 2×2 analysis of variance (ANOVA) was conducted to assess if the TA formulation and/or lot contributed significantly to results of particle sizing. Student’s t-testing was done post hoc to compare different TA formulations and lots. Fisher’s exact test and Student’s unpaired, two-tailed t-tests were conducted using the GraphPad online software (http://www.graphpad.com/quickcalcs/). ANOVA was conducted using the statspages.org online software (http://statpages.org/#Comparisons).
Results
Table 1 summarizes the dates when specific TA formulations were used, the number of patients injected, the range of doses, the number of SE cases, and the rate of SE incidence for each formulation. Four cases of SE were identified following 87 injections of Triesence® (4.6%). One case of SE was identified following 166 injections of PFTA (0.6%), and zero cases of SE were identified following 139 injections of Kenalog®-40 (0%). The incidence rate of SE following intravitreal Triesence® was significantly higher than the rate of SE following either intravitreal Kenalog®-40 (P=0.0210) or PFTA (P=0.0490). There was no significant difference in the incidence rate of SE following intravitreal Kenalog®-40 and PFTA.
Table 1.
Summary of the use of three different formulations of triamcinolone acetonide (TA) and the rates of sterile endophthalmitis (SE) with each formulation
| TA formulation | Dates of use | Number of injections | Doses used (mg) | Cases of SE | Rate of SE (%) |
|---|---|---|---|---|---|
| Triesence® | September 2008 to April 2009 | 87 | 4–8 | 4 | 4.60a,b |
| Kenalog®-40 | April 2009 to February 2010 | 97 | 2–8 | 0 | 0.00 |
| PFTA | February 2010 to October 2012 | 166 | 2–8 | 1 | 0.60 |
| Kenalog®-40 | October 2012 to October 2013 | 42 | 1–2 | 0 | 0.00 |
Notes: Four cases of SE were seen following Triesence®, and one case was seen following preservative-free TA. No cases were seen following Kenalog®-40.
Triesence® > Kenalog®-40 (P=0.0210);
Triesence® > PFTA (P=0.0490).
Abbreviation: PFTA, Preservative-free formulations of TA.
In each of the patients who developed SE, a painless, profound decrease in visual acuity and a severe diffuse inflammatory response within the vitreous were noted within 24 h after injection. Pre- and postinjection data on these patients are presented in Table 2. Three Triesence®-treated patients had a hypopyon. All of the Triesence®-treated patients who developed SE had previous IVTA exposure and developed SE following their first injection with Triesence®. The patient treated with Triesence® in whom hypopyon was absent had the least number of intravitreal injections. The patient who developed SE following PFTA and did not have a hypopyon had the most rapid presentation of symptoms and received the earliest treatment for SE. All patients were treated with topical steroids (1% prednisolone acetate). Two patients received antibiotic drops (gatifloxacin or moxifloxacin), one patient received intravitreal vancomycin (1 mg), and one patient received intravitreal dexamethasone sodium phosphate (1.2 mg). All patients had resolution of symptoms and return of visual acuity within 7 weeks. The most rapid recovery (2 days) was seen in the PFTA patient, the patient who had the earliest presentation of symptoms and initiation of treatment for SE. The most rapid recovery among Triesence® patients occurred in the patient who received intravitreal dexamethasone for SE.
Table 2.
Pre- and postdiagnosis data on patients with sterile endophthalmitis following intravitreal triamcinolone acetonide
| Patient number – IVTA formulation (dose) | Diagnosis | Onset of symptoms (h) | Exam | Pretreatment visual acuity | Posttreatment visual acuity | Final visual acuity |
|---|---|---|---|---|---|---|
| 1 – Triescence® (4 mg) | CME, ERM | 24 | 4+ cell and flare, vitreous opacity | 20/30 | 20/60 | 20/30 |
| 2 – Triescence® (4 mg) | Ex AMD | 24 | Hypopyon, dense vitritis | 20/60 | HM | 20/60 |
| 3 – Triescence® (4 mg) | CRVO, CME, SIG | 24 | Hypopyon, vitreous opacity | 20/30 | 20/200 | 20/30 |
| 4 – Triescence® (4 mg) | CME, ERM | 24 | Hypopyon, dense vitritis | 20/200 | HM | 20/200 |
| 5 – PFTA (2 mg) | Ex AMD | 6 | 1+ cell and flare vitreous opacity | 20/20 | HM | 20/20 |
| Patient number – IVTA formulation | Time until recovery | Cultures | Therapy | Patient history | ||
| 1 – Triescence® | 4 wk | NA | Topical steroids | IVK, IVB ×2, PCIOL, PPV, Ahmed valve, valve removal, diode CYC | ||
| 2 – Triescence® | 7 wk | NA | Topical steroids | IVK, STK, IVB ×15, PCIOL | ||
| 3 – Triescence® | 5 wk | NA | Topical steroids and antibiotics; IV vancomycin | PFTA ×5, STK, IVA ×4 PCIOL, valve | ||
| 4 – Triescence® | 3.5 wk | Negative | Topical steroids and antibiotics; IV dexamethasone | IVTA ×2, STK ×2, PCIOL, valve, PPV | ||
| 5 – PFTA | 2 d | NA | Topical steroids | PDT ×1, IVR ×19, IVA ×19 |
Notes: All patients presented with a painless decrease of vision within 24 h of intravitreal injection. All patients responded to treatment in days to weeks.
Abbreviations: CME, cystoid macular edema; ERM, epiretinal membrane; Ex AMD, exudative age-related macular degeneration; CRVO, central retinal vein occlusion; SIG, steroid-induced glaucoma; HM, hand motion; IVK, intravitreal Kenalog®-40; IVB, intravitreal bevacizumab; IVR, intravitreal ranibizumab; IVA, intravitreal aflibercept; IVTA, intravitreal triamcinolone acetonide; PCIOL, posterior chamber intraocular lens; PPV, pars plana vitrectomy; diode CYC, diode laser transscleral cyclophotocoagulation; PFTA, preservative-free triamcinolone acetonide; NA, not available; STK, sub-tenon’s Kenalog(r); PDT, photodynamic therapy; IV, intravitreal.
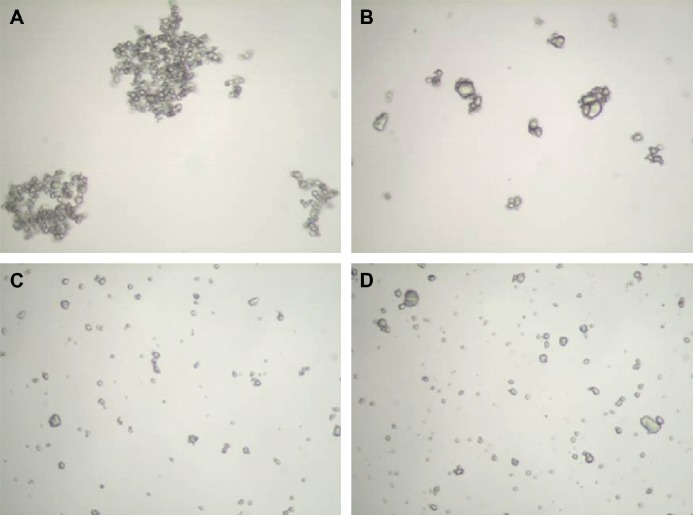
In Figure 1, representative photographs of Triesence® (A and C) and Kenalog®-40 (B and D) particles are shown in aggregate-promoting balanced salt solution (A and B) and in nonaggregating Triton X-100 solution (1 g/L, C and D). The volume-weighted distribution of particle sizes in the nonaggregating condition for two lots each of Triesence® and Kenalog®-40 are shown in Figure 2, and the results of particle sizing analyses are shown in Table 3. ANOVA revealed very large main effects of formulations (P<10−28) and a formulation by lot interaction (P<10−15). Post hoc t-testing revealed very large differences among each of the lots/formulations (P<10−19). The mean particle diameter of both the lots of Kenalog®-40 are larger than that of both the lots of Triesence®. The concentrations of particles in both the lots of Triesence® are higher than those of both the lots of Kenalog®-40.
Figure 1.
Representative images of particles of Triesence® (A, C) and Kenalog®-40 (B, D). In (A and B), samples were diluted in buffered salt solution. In (C and D), samples were diluted in a solution containing 1 g/L Triton X-100. Samples were photographed with a Nikon Labophot polarizing light microscope with Clemex Vision Lite 4.0 software. Images were taken at a magnification of 400×.
Figure 2.
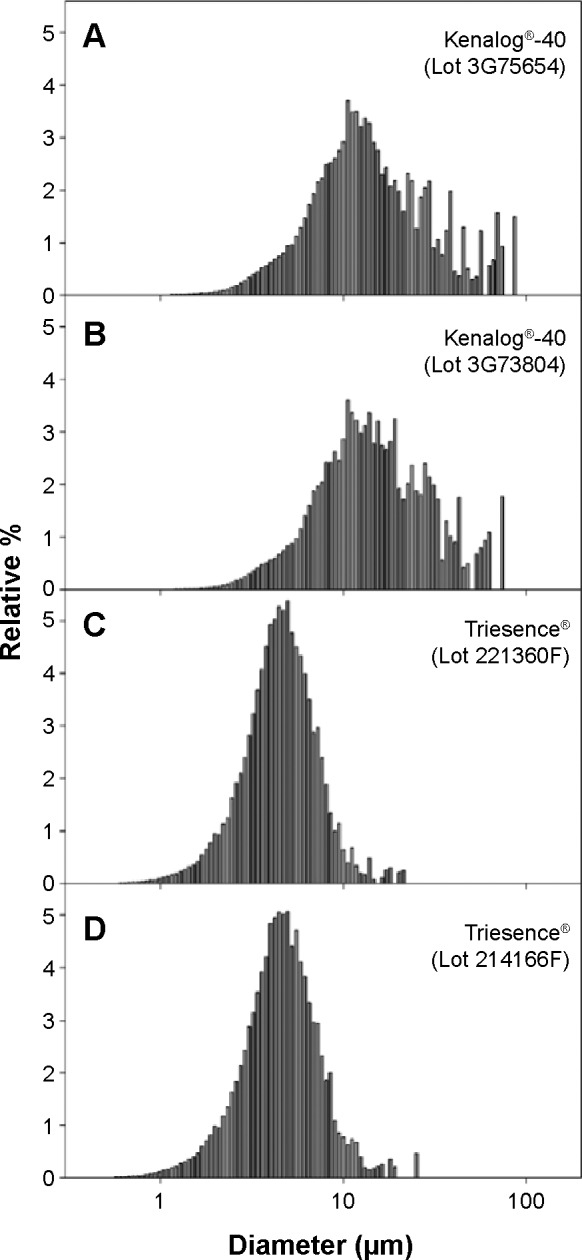
Distributions of particle sizes of Kenalog®-40 (A, B), Triesence® (C, D). Mean diameter of each formulation was determined using a Model 700 Accusizer on a volume-weighted basis. Each bar represents the percentage of all particles of the formulation which were of the corresponding diameter indicated on the x-axis.
Table 3.
Particle analyses of different formulations of triamcinolone acetonide
| Lot number | Kenalog®-40
|
Triesence®
|
||
|---|---|---|---|---|
| 3G75654 | 3G73804 | 221360F | 214166F | |
| Mean diameter (± SEM) (μm) | 19.20±0.040 | 18.60±0.049 | 5.01±0.007 | 5.11±0.008 |
| Median (μm) | 13.09 | 13.82 | 4.45 | 4.45 |
| Mode (μm) | 10.55 | 10.55 | 4.96 | 4.96 |
| Skewness | 2.06 | 1.82 | 2.26 | 2.66 |
| Number of particles/mL | 1.07×107 | 1.01×108 | 1.28×109 | 1.23×109 |
Notes: Particle diameters were calculated on a volume-weighted basis. A minimum of 88,000 particles from each formulation and lot were measured. The differences among the formulations/lots are highly significant (P<0.0001).
Abbreviation: SEM, standard error of the mean.
Discussion
Although it has been known for many years that TA can produce SE following intravitreal injection, its cause has not been elucidated, nor have there been reports of differences among formulations of TA. We report that Triesence® has the greatest propensity to produce SE of the three formulations examined. The mean particle size of Triesence® is significantly smaller than that of Kenalog®-40. These data support the hypothesis that the propensity of TA to produce SE is inversely proportional to the size of the particles within the formulation of the drug.
When particle size analysis was conducted for this study, compounded PFTA was no longer commercially available. In 2009, however, we presented data from a preliminary study of particle sizes of PFTA, Triesence®, and Kenalog®-40.23 Nonaggregating conditions were used, and the rank ordering of particle sizes was Triesence® < PFTA < Kenalog®-40, a rank ordering inversely identical to the ordering for the incidence of SE. For this report, particle analyses were repeated because of issues with the earlier study, including uncertainty in the concentration of Triton X-100 used and the lack of an estimation of particle concentrations. Nevertheless, the results of the preliminary study are in agreement with those of the present analysis.
At the same dosage, Triesence® has a greater particle load (number of particles) than the other two formulations, given its smaller mean particle size. Estimates of particle concentrations suggest a 12–120 times greater particle load for Triesence® compared to Kenalog®-40. Patients treated with Triesence® in the current study also had a greater particle load because of the higher doses used. In each instance of SE following Triesence®, a dose of 4 mg was used, whereas in the one PFTA-associated instance of SE, a dose of 2 mg was used. Dose alone is likely not sufficient to explain the higher rate of SE with Triesence® as some individuals were treated with doses as high as 8 mg for each of the formulations.
These data and other observations argue against benzyl alcohol being the principal factor in the development of SE. Only Kenalog®-40, the formulation with the lowest rate of SE, contained this preservative. Additionally, benzyl alcohol-containing dexamethasone phosphate was used to successfully treat one eye with Triesence®-induced SE, and it was used separately in ~150 eyes during the time course of this study without any cases of SE.
It is possible that no cases of SE following Kenalog®-40 were seen in the present analysis due to the small sample size examined and the fact that TA-induced SE is a rare event. It is also possible that the lower doses of 1–2 mg of Kenalog®-40, frequently used in this study, had a decreased likelihood of inciting an inflammatory response due to a lower particle load. The possibility that the lack of Kenalog®-40-related SE cases was a result of the timing of observation cannot be ruled out, as it is known that instances of Kenalog®-40-induced SE can cluster temporally.15,16
The SE incidence rate of 4.6% reported here for Triesence® could be considered a clustering of cases. Although there is a report of a single incidence of Triesence®-induced SE,24 there is no evidence to suggest that there was a widespread temporal clustering of cases of SE, as the present report is the only known report of Triesence®-induced SE outside of the early single case report. The present report is of significance, in that it further documents the incidence of SE with this formulation.
Clustering of cases within a single practice may be due to physician technique or to clinic-specific factors. It is doubtful that these contributed to the incidence of SE as these factors would be expected to result in an increase in SE with other agents. During the time period that Triesence® was used, over 1,000 intravitreal injections of bevacizumab were performed without a single case of SE.
Particles or crystals of TA in the vitreous have been proposed to be a factor in the development of SE by providing phagocytic targets that activate macrophages present in the vitreous.12 Activated macrophages are unable to digest TA particles, resulting in TA accumulation and eventual macrophage death in a phenomenon referred to as “frustrated phagocytosis”.25 The rupturing of the macrophages releases inflammatory cytokines and chemokines, leading to the signs and symptoms of SE.
A similar inflammatory response has been reported following intrasynovial injection of sodium urate26 and calcium phosphate27 crystals, which were targets for phagocytosis.28 Intra-articular injection of corticosteroid crystals has been shown to induce inflammation29 and postinjection flare following intra-articular use, as listed in the product insert for Kenalog-40® as an adverse reaction.
Several papers have examined the properties of Triesence®, Kenalog®-40, and/or compounded PFTA. Moshfeghi et al30 reported that PFTA (New England Compounding Center, Framingham, MA, USA) in Balance Salt Solution Plus® (Alcon Laboratories, Fort Worth, TX, USA) had smaller, but more numerous aggregates and Triesence® had larger aggregates. The effect of aggregate size on inflammatory response was not addressed. Although we did not analyze aggregate sizes, Figure 1A and B and clinical experience are in agreement and suggest that Triesence® has larger aggregates than does Kenalog-40®.
Crystalline Triesence® has been reported to reduce the viability of human retina pigment epithelial and rat neurosensory cells in culture.31 In contrast, Triesence® which was solubilized in dimethyl sulfoxide did not reduce cellular viability, suggesting that TA crystals are necessary for this toxic effect.
Zacharias et al32 conducted a particle size analysis for Triesence®, Kenalog®-40, and PFTA (Leiter’s). In contrast to our findings, PFTA had a smaller particle size than Triesence®. Potential explanations for this discrepancy include differences in instrumentation, use of water as a dispersant, and a high pump speed with ultrasonication.
Recently, Otsuka et al22 presented data supporting the role of TA particles in inflammation. Studies with lens and retinal pigment epithelial cells in culture demonstrated that IL-6 and IL-8 levels were increased if TA particles contacted cells, but not in conditions in which particles could not directly contact cells.
Two large, multicenter trials have utilized Trivaris™ in which PFTA is suspended in a hydrogel vehicle. No cases of SE were seen following 1,378 injections in the Diabetic Retinopathy Clinical Research Network (DRCRnet) Protocol B study or following 631 injections of Trivaris™ in the Standard Care vs COrticosteroid for REtinal Vein Occlusion (SCORE) study.33 The authors suggest that suspension of TA crystals in a viscous polymer shields free crystals, preventing phagocytosis by macrophages and a subsequent inflammatory response.
Triesence® and Kenalog®-40 are both suspensions of TA, and both contain carboxymethylcellulose (CMC) sodium (a suspending agent) and polysorbate 80 (a wetting agent). Triesence®, however, contains lower concentrations of these ingredients. Specifically, Triesence® contains 0.5% (w/v) CMC and 0.015% polysorbate 8034 compared with 0.75% CMC and 0.04% polysorbate 8018 in Kenalog®-40. The potential impact of the concentrations of these ingredients on the incidence of SE is unknown.
The principal weakness of this study is the nonoverlap of times when the different formulations of TA were in use and the different dose ranges used. A larger-scale, multicenter study examining these three formulations when given at similar doses may be needed to confirm or refute the findings reported here.
In summary, the rate of SE was highest for Triesence®, the formulation with the highest average particle size/load. These data do not support the hypothesis that benzyl alcohol plays a major causative role in SE following TA and instead provide support for the particle theory of TA-induced SE.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Tano Y, Chandler D, Machemer R. Treatment of intraocular proliferation with intravitreal injection of triamcinolone acetonide. Am J Ophthalmol. 1980;90(6):810–816. doi: 10.1016/s0002-9394(14)75196-7. [DOI] [PubMed] [Google Scholar]
- 2.Penfold PL, Gyory JF, Hunyor AB, Billson FA. Exudative macular degeneration and intravitreal triamcinolone. A pilot study. Aust N Z J Ophthalmol. 1995;23(4):293–298. doi: 10.1111/j.1442-9071.1995.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 3.Tao Y, Jonas JB. Intravitreal triamcinolone. Ophthalmologica. 2011;225(1):1–20. doi: 10.1159/000317909. [DOI] [PubMed] [Google Scholar]
- 4.Wingate RJ, Beaumont PE. Intravitreal triamcinolone and elevated intraocular pressure. Aust N Z J Ophthalmol. 1999;27(6):431–432. doi: 10.1046/j.1440-1606.1999.00238.x. [DOI] [PubMed] [Google Scholar]
- 5.Gillies MC, Kuzniarz M, Craig J, Ball M, Luo W, Simpson JM. Intravitreal triamcinolone-induced elevated intraocular pressure is associated with the development of posterior subcapsular cataract. Ophthalmology. 2005;112(1):139–143. doi: 10.1016/j.ophtha.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Jonas JB, Kreissig I, Degenring RF. Endophthalmitis after intravitreal injection of triamcinolone acetonide. Arch Ophthalmol. 2003;121(11):1663–1664. doi: 10.1001/archopht.121.11.1663-b. [DOI] [PubMed] [Google Scholar]
- 7.Roth DB, Chieh J, Spirn MJ, Green SN, Yarian DL, Chaudhry NA. Noninfectious endophthalmitis associated with intravitreal triamcinolone injection. Arch Ophthalmol. 2003;121(9):1279–1282. doi: 10.1001/archopht.121.9.1279. [DOI] [PubMed] [Google Scholar]
- 8.Roth DB, Flynn HW., Jr Distinguishing between infectious and noninfectious endophthalmitis after intravitreal triamcinolone injection. Am J Ophthalmol. 2008;146(3):346–347. doi: 10.1016/j.ajo.2008.04.037. [DOI] [PubMed] [Google Scholar]
- 9.Roth DB, Realini T, Feuer WJ, et al. Short-term complications of intravitreal injection of triamcinolone acetonide. Retina. 2008;28(1):66–70. doi: 10.1097/IAE.0b013e3181593e38. [DOI] [PubMed] [Google Scholar]
- 10.Nelson ML, Tennant MT, Sivalingam A, Regillo CD, Belmont JB, Martidis A. Infectious and presumed noninfectious endophthalmitis after intravitreal triamcinolone acetonide injection. Retina. 2003;23(5):686–691. doi: 10.1097/00006982-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Sutter FK, Gillies MC. Pseudo-endophthalmitis after intravitreal injection of triamcinolone. Br J Ophthalmol. 2003;87(8):972–974. doi: 10.1136/bjo.87.8.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roth D, Lee SS, Flynn HW, Jr, Moshfeghi DM. Inflammatory reactions after intravitreal triamcinolone acetonide: possible mechanisms and therapeutic options. Expert Rev Ophthalmol. 2010;5(3):273–276. [Google Scholar]
- 13.Westfall AC, Osborn A, Kuhl D, Benz MS, Mieler WF, Holz ER. Acute endophthalmitis incidence: intravitreal triamcinolone. Arch Ophthalmol. 2005;123(8):1075–1077. doi: 10.1001/archopht.123.8.1075. [DOI] [PubMed] [Google Scholar]
- 14.Wang LC, Yang CM. Sterile endophthalmitis following intravitreal injection of triamcinolone acetonide. Ocul Immunol Inflamm. 2005;13(4):295–300. doi: 10.1080/09273940590951007. [DOI] [PubMed] [Google Scholar]
- 15.Jonisch J, Lai JC, Deramo VA, Flug AJ, Fastenberg DM. Increased incidence of sterile endophthalmitis following intravitreal preserved triamcinolone acetonide. Br J Ophthalmol. 2008;92(8):1051–1054. doi: 10.1136/bjo.2007.136069. [DOI] [PubMed] [Google Scholar]
- 16.Stepien KE, Eaton AM, Jaffe GJ, Davis JL, Raja J, Feuer W. Increased incidence of sterile endophthalmitis after intravitreal triamcinolone acetonide in spring 2006. Retina. 2009;29(2):207–213. doi: 10.1097/IAE.0b013e31818eccb3. [DOI] [PubMed] [Google Scholar]
- 17.Jonas JB, Kreissig I, Spandau UH, Harder B. Infectious and noninfectious endophthalmitis after intravitreal high-dosage triamcinolone acetonide. Am J Ophthalmol. 2006;141(3):579–580. doi: 10.1016/j.ajo.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Kenalog®-40 (triamcinolone acetonide injectable suspension, USP) [package insert] Princeton, NJ: Bristol-Myers Squibb; 2014. [Google Scholar]
- 19.Dunbar H, Hoskins MD., Jr . Letter on behalf of American Academy of Ophthalmology regarding warning section of the prescribing Information for KENLOG to Freda Lewis-Hall MD. Bristol-Myers Squibb Company; Dec 8, 2006. [Google Scholar]
- 20.Maia M, Farah ME, Belfort RN, et al. Effects of intravitreal triamcinolone acetonide injection with and without preservative. Br J Ophthalmol. 2007;91(9):1122–1124. doi: 10.1136/bjo.2007.115386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lorenzo Carrero J, Perez Flores I, Gonzalez Barcia M. Infectious and noninfectious endophthalmitis after intravitreal high-dosage triamcinolone acetonide. Am J Ophthalmol. 2006;142(3):529. doi: 10.1016/j.ajo.2006.05.032. author reply 529–530. [DOI] [PubMed] [Google Scholar]
- 22.Otsuka H, Kawano H, Sonoda S, Nakamura M, Sakamoto T. Particle-induced endophthalmitis: possible mechanisms of sterile endophthalmitis after intravitreal triamcinolone. Invest Ophthalmol Vis Sci. 2013;54(3):1758–1766. doi: 10.1167/iovs.12-11247. [DOI] [PubMed] [Google Scholar]
- 23.Dodwell DG, Krimmel DA. Sterile endophthalmitis from Triesence™; Platform presentation at: Retina Congress; October 2, 2009; New York, NY, USA. [Google Scholar]
- 24.Bakri SJ, Edwards AO, Couch SM. Noninfectious endophthalmitis occurring after intravitreal Triesence injection. Retinal Cases Brief Rep. 2009;3:316–318. doi: 10.1097/ICB.0b013e318199b086. [DOI] [PubMed] [Google Scholar]
- 25.Takemura R, Stenberg PE, Bainton DF, Werb Z. Rapid redistribution of clathrin onto macrophage plasma membranes in response to Fc receptor-ligand interaction during frustrated phagocytosis. J Cell Biol. 1986;102(1):55–69. doi: 10.1083/jcb.102.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Faires JS, McCarty DJ., Jr Acute arthritis in man and dog after intrasynovial injection of sodium urate crystals. Lancet. 1962;280(7258):682–685. doi: 10.1016/s0140-6736(62)91050-4. [DOI] [PubMed] [Google Scholar]
- 27.Kohn NN, Hughes RE, Mc CD, Jr, Faires JS. The significance of calcium phosphate crystals in the synovial fluid of arthritic patients: the “pseudogout syndrome”. II. Identification of crystals. Ann Intern Med. 1962;56:738–745. doi: 10.7326/0003-4819-56-5-738. [DOI] [PubMed] [Google Scholar]
- 28.McCarty DJ, Jr, Hogan JM. Inflammatory reaction after intrasynovial injection of microcrystalline adrenocorticosteroid esters. Arthritis Rheum. 1964;7:359–367. doi: 10.1002/art.1780070402. [DOI] [PubMed] [Google Scholar]
- 29.Selvi E, De Stefano R, Lorenzini S, Marcolongo R. Arthritis induced by corticosteroid crystals. J Rheumatol. 2004;31(3):622. [PubMed] [Google Scholar]
- 30.Moshfeghi AA, Nugent AK, Nomoto H, Sanislo SR, Kitchens JW, Moshfeghi DM. Triamcinolone acetonide preparations: impact of crystal size on in vitro behavior. Retina. 2009;29(5):689–698. doi: 10.1097/IAE.0b013e31819e390a. [DOI] [PubMed] [Google Scholar]
- 31.Zacharias LC, Estrago-Franco MF, Ramirez C, et al. The effects of commercially available preservative-free FDA-approved triamcinolone (Triesence(R)) on retinal cells in culture. J Ocul Pharmacol Ther. 2011;27(2):143–150. doi: 10.1089/jop.2010.0143. [DOI] [PubMed] [Google Scholar]
- 32.Zacharias LC, Lin T, Migon R, et al. Assessment of the differences in pharmacokinetics and pharmacodynamics between four distinct formulations of triamcinolone acetonide. Retina. 2013;33(3):522–531. doi: 10.1097/IAE.0b013e3182647f69. [DOI] [PubMed] [Google Scholar]
- 33.Bhavsar AR, Ip MS, Glassman AR. The risk of endophthalmitis following intravitreal triamcinolone injection in the DRCRnet and SCORE clinical trials. Am J Ophthalmol. 2007;144(3):454–456. doi: 10.1016/j.ajo.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Triesence® (triamcinolone acetonide injectable suspension) [package insert] Fort Worth, TX: Alcon Laboratories; 2007. [Google Scholar]