Abstract
Objective
To examine neonatal morbidity associated with different maneuvers used among term patients who experience a shoulder dystocia.
Study Design
A retrospective cohort study of all women who experienced a clinically diagnosed shoulder dystocia at term requiring obstetric maneuvers at a single tertiary care hospital from 2005-2008. We excluded women with major fetal anomaly, intrauterine death, multiple gestation, and preterm. Women exposed to Rubin maneuver, Wood's screw maneuver, or delivery of the posterior arm were compared to women delivered by McRoberts/suprapubic pressure only, which served as the reference group. The primary outcome was a composite morbidity of neonatal injury (defined as clavicular or humeral fracture or brachial plexus injury) and neonatal depression (defined as Apgar <7 at 5 minutes, arterial cord pH <7.1, CPAP use, intubation, or respiratory distress). Logistic regression was used to adjust for nulliparity and duration of shoulder dystocia, defined as time from delivery of fetal head to delivery of shoulders.
Results
Among the 231 women who met inclusion criteria, 135 were delivered by McRoberts/suprapubic pressure alone (57.9%), 83 women were exposed to Rubin maneuver, 53 women were exposed to Wood's screw, and 36 women were exposed to delivery of posterior arm. Individual maneuvers were not associated with composite morbidity, neonatal injury, or neonatal depression after adjusting for nulliparity and duration of shoulder dystocia.
Conclusion
We found no association between shoulder dystocia maneuvers and neonatal morbidity after adjusting for duration, a surrogate for severity. Our results demonstrate that clinicians should utilize the maneuver most likely to result in successful delivery.
Keywords: neonatal morbidity, shoulder dystocia, shoulder dystocia maneuvers
Introduction
Shoulder dystocia is an obstetric emergency that complicates 0.6 to 1.4% of vaginal deliveries.1 Shoulder dystocia is defined as a delivery that requires additional obstetric maneuvers following failure of gentle downward traction on the fetal head to effect delivery of the shoulders.1 Several neonatal morbidities are associated with shoulder dystocia, including brachial plexus injury, humeral and clavicular fractures, hypoxic-ischemic encephalopathy, and even neonatal death.1,2
Many obstetrical maneuvers have been described to relieve shoulder dystocia; the most commonly used maneuvers include McRoberts, suprapubic pressure, rotational maneuvers and delivery of the posterior arm.3 Several previous studies have suggested that McRoberts and suprapubic pressure result in the lowest rate of neonatal morbidity and resolve 40-60% of shoulder dystocia events.4-6 Based on this evidence, ACOG recommends that McRoberts and suprapubic pressure be the initial maneuvers attempted in a shoulder dystocia.1 While prior studies have shown increased risks of adverse neonatal outcomes with use of additional maneuvers when compared with McRoberts and suprapubic pressure, none accounted for duration of shoulder dystocia.4-6 Further, there is little data on individual advanced maneuvers beyond McRoberts and suprapubic pressure and neonatal outcomes.
The objective of this study was to examine the independent effects of advanced maneuvers used in the management of shoulder dystocia as compared to McRoberts and suprapubic pressure alone on the risk of neonatal morbidity, accounting for duration, a surrogate for severity of dystocia.
Materials and Methods
We conducted a retrospective cohort study of all women who experienced a clinically diagnosed shoulder dystocia requiring obstetric maneuvers at term (≥ 37 weeks) at a single tertiary care hospital from 2005-2008. We excluded women with a known major fetal anomaly, intrauterine death, multiple gestation and preterm gestational age. This study was approved by the Washington University Human Research Protection Office.
The comparison groups were defined by exposure to a particular maneuver including McRoberts/suprapubic pressure only, Rubin maneuver, Wood's screw maneuver, or delivery of the posterior arm. Based on the ACOG recommendation that McRoberts and suprapubic pressure be the initial maneuvers attempted in a shoulder dystocia, we chose our reference group in this study to include all of those patients whose dystocia was resolved by McRoberts/suprapubic pressure alone. With the exception of the reference group, some women were exposed to more than one additional maneuver.
The primary outcome was a composite morbidity of neonatal injury and neonatal depression. We defined neonatal injury as the occurrence of clavicular or humeral fracture, or brachial plexus injury. Neonatal depression included any of the following: Apgar <7 at 5 minutes, arterial cord pH <7.1, continuous positive airway pressure (CPAP) use, intubation, or respiratory distress. Respiratory distress was defined as the requirement of oxygen support after 6 hours of life or any need for mechanical ventilation. Beyond those neonates delivered by McRoberts/suprapubic pressure only, neonatal morbidity was included under each maneuver to which the neonate was exposed.
Extensive data were extracted from the maternal and neonatal medical records to obtain sociodemographic information, medical and antenatal history, and neonatal outcomes. Data on the shoulder dystocia including duration of the shoulder dystocia defined as time from delivery of the fetal head to delivery of the fetal shoulders in seconds, and obstetric maneuvers performed were collected from a standardized delivery record. Baseline characteristics were compared between the reference group of McRoberts/suprapubic pressure only and women who required the use of an additional maneuver. Categorical variables were compared using the X2 or Fisher's exact test, as appropriate. Continuous variables were assessed for normality using Kolmogorov-Smirnov test. Variables that were not normally distributed were compared with the Mann-Whitney U test and normally distributed variables were compared using the Student's t test. The relationship between number of advanced maneuvers utilized and duration of shoulder dystocia was secondarily explored.
Odds ratios were calculated for the composite outcome comparing each of the exposure groups (delivery of posterior arm, Rubin maneuver, or Wood's screw maneuver) to the reference group (McRoberts/suprapubic pressure only). Logistic regression was used to control for confounding factors. A backward step-wise approach utilizing the likelihood ratio test to assess the impact of each covariate on the model was used. Duration of shoulder dystocia was included as a continuous variable in the model because there was a linear relationship between duration and morbidity as demonstrated by plotting the predicted probability of the composite outcome against time. The final model adjusted for nulliparity and duration of shoulder dystocia.
The relationship between duration of shoulder dystocia and risk of the composite morbidity was further assessed and presented visually by Kaplan-Meier curve. Differences in the duration of shoulder dystocia in pregnancies with and without the composite morbidity were compared using the log-rank test.
All analyses were performed using Stata Special Edition 12.1 (StataCorp, College Station, TX).
Results
Of 8,390 deliveries in the study period, 231 met the inclusion criteria. Of those, 135 were delivered by McRoberts/suprapubic pressure alone (57.9%). Eighty-three women were exposed to Rubin maneuver, 53 were exposed to Wood's screw maneuver, and 36 were exposed to delivery of the posterior arm.
Women who were delivered by McRoberts/suprapubic pressure alone did not differ by parity, gestational age, prevalence of diabetes (either pregestational or gestational), rate of operative vaginal delivery, or infant weight over 4000 grams as compared to women delivered using additional maneuvers (Table 1). However, women delivered by McRoberts/suprapubic pressure alone did have a significantly shorter duration of shoulder dystocia than women delivered by one of the other maneuvers with a median duration of 29 seconds (interquartile range 29-30 seconds) as compared to 60 seconds (interquartile range 40-90 seconds) (Table 1).
Table 1.
Baseline characteristics of those women exposed to McRoberts/suprapubic pressure only compared to those women exposed to advanced maneuvers.
| McRoberts and/or Suprapubic Only n=135 | Advanced Maneuvers n=96 | p value | |
|---|---|---|---|
|
| |||
| Median gestational age (weeks) | 40 (39-40) | 39 (38-40) | 0.11 |
|
| |||
| Nulliparity | 42 (31.1) | 28 (29.2) | 0.75 |
|
| |||
| Advanced maternal age | 11 (8.1) | 9 (9.4) | 0.74 |
|
| |||
| Race | |||
| Black | 89 (65.9) | 62 (64.6) | 0.63 |
| White | 33 (24.4) | 21 (21.9) | |
| Other | 13 (9.6) | 13 (13.5) | |
|
| |||
| Body mass index ≥30 kg/m2 | 91 (69.5) | 64 (69.6) | 0.99 |
|
| |||
| Diabetes | 12 (8.9) | 10 (10.4) | 0.70 |
|
| |||
| Regional anesthesia | 115 (85.1) | 83 (86.5) | 0.79 |
|
| |||
| Operative vaginal delivery | 24 (17.8) | 18 (18.9) | 0.82 |
|
| |||
| Infant weight >4000g | 37 (27.4) | 26 (27.1) | 0.96 |
|
| |||
| Median duration of shoulder dystocia (seconds) | 29 (29-30) | 60 (40-90) | <0.01 |
Data presented as n (%), unless specified as median (interquartile range)
Secondarily, we explored the relationship between number of advanced maneuvers utilized and duration of dystocia. We found that the median duration of dystocia increased with the utilization of an increasing number of maneuvers (p <0.01) (Table 2).
Table 2.
Duration of shoulder dystocia by number of maneuvers utilized.
| N (%) | Median duration (seconds) | Interquartile range (seconds) | |
|---|---|---|---|
| McRoberts and/or Suprapubic only | 135 (58.4) | 29 | 29-30 |
| +1 additional maneuver | 43 (18.6) | 60 | 29-60 |
| +2 additional maneuvers | 30 (13.0) | 60 | 42.5-80 |
| +3 additional maneuvers | 23 (10.0) | 90 | 60-157.5 |
p <0.01
The neonatal morbidity composite occurred in 65 of the 231 patients (28.1%). The rate of neonatal morbidity was higher with additional maneuvers compared with McRoberts/suprapubic pressure alone (22.2% versus 50.0% for delivery of the posterior arm, 36.1% for Rubin maneuver, and 39.6% for Wood's screw maneuver). In unadjusted analysis, each type of additional maneuver appeared to be associated with an increased risk of the composite outcome relative to the reference group delivered by McRoberts/suprapubic pressure alone (RR 2.25 [95% CI, 1.42 – 3.54] for delivery of the posterior arm, RR 1.63 [95% CI, 1.06 – 2.49] for Rubin maneuver, and RR 1.78 [95% CI, 1.13 – 3.03] for Wood's screw maneuver). However, after controlling for nulliparity and duration of shoulder dystocia, these differences were no longer statistically significant; aOR 1.77 (95% CI, 0.54 – 5.79) for delivery of the posterior arm, aOR 1.36 (95% CI, 0.63 – 2.93) for Rubin maneuver, and aOR 1.17 (95% CI, 0.45 – 3.03) for Wood's screw maneuver (Table 3).
Table 3.
Neonatal outcomes of each shoulder dystocia maneuver.
| McRoberts and/or suprapubic only N=135 | Delivery of posterior arm N=36 | Rubin maneuver N=83 | Wood's screw maneuver N=53 | |
|---|---|---|---|---|
| Composite neonatal morbidity n(%) | 30 (22.2) | 18 (50.0) | 30 (36.1) | 21 (39.6) |
| RR (95% CI) | ref | 2.25 (1.42-3.54) | 1.63 (1.06-2.49) | 1.78 (1.13-2.82) |
| aOR* (95% CI) | ref | 1.77 (0.54-5.79) | 1.36 (0.63-2.93) | 1.17 (0.45-3.03) |
| Neonatal injury n(%) | 8 (5.8) | 6 (16.7) | 9 (10.8) | 5 (9.4) |
| RR (95% CI) | ref | 2.83 (1.05-7.65) | 1.84 (0.74-4.59) | 1.60 (0.55-4.68) |
| aOR* (95% CI) | ref | 2.54 (0.44-14.77) | 2.33 (0.70-7.77) | 1.5 (0.33-7.21) |
| Neonatal depression n(%) | 24 (17.8) | 14 (38.9) | 24 (28.9) | 18 (34.0) |
| RR (95% CI) | ref | 2.19 (1.27-3.78) | 1.62 (0.99-2.67) | 1.91 (1.13-3.22) |
| aOR* (95% CI) | ref | 1.39 (0.40-4.91) | 1.01 (0.44-2.36) | 1.00 (0.36-2.81) |
Adjusted for nulliparity and duration of dystocia
Similarly, when we evaluated the components of the composite outcome separately as neonatal injury and neonatal depression, apparent positive associations between the adverse outcomes and exposure to additional maneuvers were not demonstrated after adjusting for parity and duration. Overall, neonatal injury occurred in 20 of the 231 patients (8.7%). Neonatal injury occurred in 5.8% of infants delivered by McRoberts/suprapubic pressure alone, 16.7% of infants exposed to delivery of the posterior arm (aOR 2.54 [95% CI, 0.44 – 14.77]), 10.8% of infants exposed to Rubin maneuver (aOR 2.33 [95% CI, 0.70 – 7.77]), and 9.4% of infants exposed to Wood's screw maneuver (aOR 1.50 [95% CI, 0.33 – 7.21]). Neonatal depression occurred in 50 of the 231 patients (21.6%) overall. Neonatal depression occurred in 17.8% of those delivered by McRoberts/suprapubic pressure alone, 38.9% of those exposed to delivery of the posterior arm (aOR 1.39 [95% CI, 0.40 – 4.91]), 28.9% of those exposed to Rubin maneuver (aOR 1.01 [95% CI, 0.44 – 2.36]), and 34.0% of those exposed to Wood's screw maneuver (aOR 1.00 [95% CI, 0.36 – 2.81]) (Table 3). The absolute number of each individual component of the morbidity composite that occurred with each maneuver is presented in Table 4.
Table 4.
Individual components of the composite neonatal morbidity that occurred with each shoulder dystocia maneuver.
| McRoberts and/or suprapubic only N=135 | Delivery of posterior arm N=36 | Rubin maneuver N=83 | Wood's screw maneuver N=53 | |
|---|---|---|---|---|
| Clavicular fracture | 2 (1.5) | 0 | 2 (2.4) | 1 (1.9) |
| Humeral fracture | 0 | 1 (2.8) | 0 | 0 |
| Brachial plexus injury | 7 (5.1) | 5 (13.9) | 8 (9.5) | 5 (9.4) |
| Apgar <7 at 5 minutes | 2 (1.5) | 1 (2.8) | 2 (2.4) | 2 (3.8) |
| Arterial cord pH <7.1 | 0 | 1 (2.8) | 1 (1.2) | 1 (1.9) |
| Respiratory distress | 8 (5.8) | 5 (13.9) | 9 (10.7) | 6 (11.3) |
| CPAP use | 21 (15.3) | 13 (36.1) | 21 (25.0) | 16 (30.2) |
| Intubation | 1 (0.7) | 0 | 2 (2.4) | 2 (3.8) |
Data presented as n (%)
The relationship between duration of shoulder dystocia and neonatal morbidity was also assessed using time-to-event analysis. Longer length of time elapsed between delivery of the fetal head and shoulders in the pregnancies complicated by the composite morbidity than in those without neonatal complications (p <0.01) (Figure 1).
Figure 1.
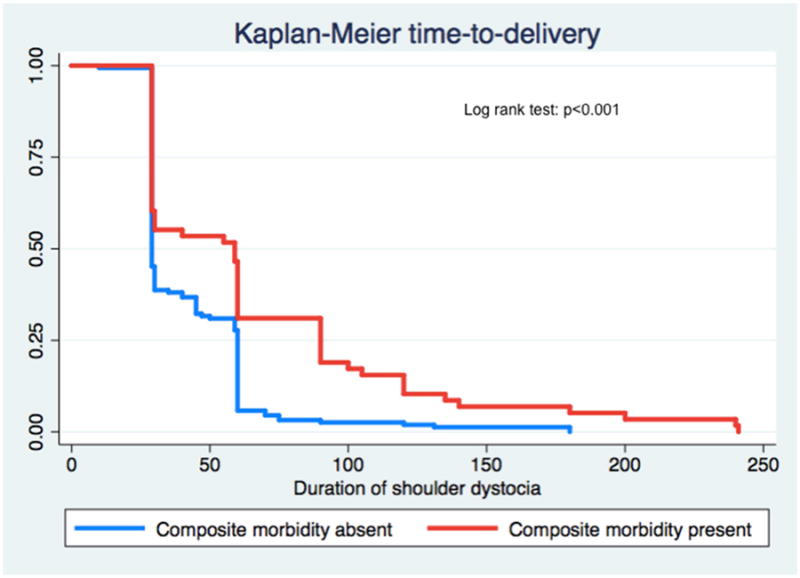
Comparison of presence or absence of composite neonatal morbidity and duration of shoulder dystocia (seconds).
Comment
We found higher rates of neonatal morbidity among infants requiring additional maneuvers beyond McRoberts or suprapubic pressure to resolve a shoulder dystocia. However, individual shoulder dystocia maneuvers were not independently associated with increased risk of neonatal morbidity, neonatal injury, or neonatal depression after adjusting for duration of dystocia, a surrogate for severity. Our results suggest it is not the individual maneuvers that are associated with neonatal morbidity, but rather the severity of the dystocia and difficulty of delivery.
There is currently conflicting evidence regarding the morbidity associated with various maneuvers used to relieve a shoulder dystocia. Both McFarland, et al. and Leung et al. have suggested that rotational maneuvers and delivery of the posterior arm should not be routinely used due to concern for increased maternal and neonatal morbidity.4,7 However, Gherman, et al. found no increase in the rate of bone fracture or brachial plexus injury with direct fetal manipulative techniques as compared to McRoberts, suprapubic pressure or proctoepisiotomy.2 Hoffman, et al. also found similar rates of neonatal morbidity among the individual maneuvers and only identified a higher rate of neonatal injury with an increasing number of maneuvers utilized.8
Recent data has suggested that delivery of the posterior arm is often the maneuver utilized that results in successful delivery.8-10 However, traditional teaching of shoulder dystocia maneuvers has been to attempt rotational maneuvers prior to delivery of the posterior arm. Our data demonstrate that each of these individual maneuvers are associated with similar rates of neonatal morbidity. Thus, clinicians should not delay the utilization of the maneuver that is most likely to resolve the dystocia in the given clinical scenario.
Our study is unique in that we controlled for the duration of dystocia, a surrogate for the severity of dystocia, in our analysis. Lerner, et al. found that neonates born with persistent brachial plexus injury and neonatal depression after shoulder dystocia had longer head-to-body delivery intervals than those with no complications after shoulder dystocia or persistent brachial plexus injury without neonatal depression.11 Previous studies of neonatal outcomes associated with shoulder dystocia maneuvers did not control for this important confounder.2,4,7,8,12 The increased risk of neonatal morbidity previously reported with the use of various maneuvers is likely confounded by the indication for use; meaning that the maneuvers previously associated with morbidity are employed in more severe cases. An additional strength of this study is that we analyzed neonatal outcomes as an overall morbidity composite as well as separate neonatal injuries associated with shoulder dystocia and neonatal depression.
While each of the morbidities included in our composite may occur in uncomplicated deliveries, shoulder dystocia is a known risk factor for these morbidities.1,2,4 An inherent limitation of data on shoulder dystocia is that it is usually not possible to know at exactly which point in the dystocia an injury occurred. In our study, those neonates with morbidity were included under each maneuver to which the neonate was exposed. In this study, we do not have data on the long-term outcomes of those neonates with morbidity, limiting the conclusions that can be reached. Future studies will require a very large sample size to assess a difference between maneuvers on the most serious, but rare outcomes including permanent brachial plexus injury, severe hypoxic-ischemic encephalopathy and neonatal death.
Our study has the inherent limitations of all observational studies. While we controlled for confounders there is the possibility of residual confounding by unmeasured factors. Additionally, because of the retrospective nature of the data collection, we were able to determine the maneuvers that were used, but not the order in which the maneuvers were used, or the specific maneuver that resulted in successful delivery. We cannot evaluate morbidity associated with the use of the advanced maneuvers completely independently, as they were performed in addition to McRoberts and suprapubic pressure as recommended by ACOG, and often multiple advanced maneuvers were required. However, this adds to the generalizability of our results, as this is consistent with typical clinical management of shoulder dystocia.
Our study demonstrates that once adjusting for duration of dystocia, a surrogate for severity, the individual maneuvers are associated with similar rates of neonatal injury and neonatal depression. Our results suggest that it is the severity of shoulder dystocia that is associated with increasing neonatal morbidity, not the maneuvers themselves. Thus, delivery utilizing the maneuver most likely to be successful in the clinical situation should be the primary focus of the obstetrician in the setting of shoulder dystocia.
Acknowledgments
Funding: Dr. Cahill is a Robert Wood Johnson Foundation Physician Faculty Scholar, which partially supports this work. Dr. Frey is supported by a training grant from the NICHD T32 grant (5 T32 HD055172-05) and this publication was supported by the Washington University CTSA grant (UL1 TR000448).
Footnotes
Disclosure: The authors report no conflicts of interest.
Presented in poster format at the 34th annual meeting of the Society for Maternal-Fetal Medicine, New Orleans, LA, February 3-8, 2014.
Reprints will not be available.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shoulder dystocia. ACOG Practice Bulletin No. 40, November 2002. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2002;100:1045–50. doi: 10.1016/s0029-7844(02)02513-9. [DOI] [PubMed] [Google Scholar]
- 2.Gherman RB, Ouzounian JG, Goodwin TM. Obstetric maneuvers for shoulder dystocia and associated fetal morbidity. Am J Obstet Gynecol. 1998;178:1126–30. doi: 10.1016/s0002-9378(98)70312-6. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham FG, Williams JW. Williams obstetrics. 22nd. New York (NY): McGraw-Hill Professional; 2005. [Google Scholar]
- 4.McFarland MB, Langer O, Piper JM, Berkus MD. Perinatal outcome and the type and number of maneuvers in shoulder dystocia. Int J Gynecol Obstet. 1996;55:219–24. doi: 10.1016/s0020-7292(96)02766-x. [DOI] [PubMed] [Google Scholar]
- 5.Gherman RB, Goodwin TM, Souter I, Neumann K, Ouzounian JG, Paul RH. The McRoberts' maneuver for the alleviation of shoulder dystocia: How successful is it? Am J Obstet Gynecol. 1997;176:656–61. doi: 10.1016/s0002-9378(97)70565-9. [DOI] [PubMed] [Google Scholar]
- 6.Chauhan SP, Laye MR, Lutgendorf M, McBurney JW, Keiser SD, Magann EF, Morrison JC. A multicenter assessment of 1,177 cases of shoulder dystocia: lessons learned. Am J Perinatol. 2013 Jul 24; doi: 10.1055/s-0033-1350056. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Leung TY, Stuart O, Suen SSH, Sahota DS, Lau TK, Lao TT. Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG. 2011;118:985–90. doi: 10.1111/j.1471-0528.2011.02968.x. [DOI] [PubMed] [Google Scholar]
- 8.Hoffman MK, Bailit JL, Branch DW, et al. A comparison of obstetric maneuvers for the acute management of shoulder dystocia. Obstet Gynecol. 2011;117:1272–8. doi: 10.1097/AOG.0b013e31821a12c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol. 2003;101:1068–72. doi: 10.1016/s0029-7844(02)02332-3. [DOI] [PubMed] [Google Scholar]
- 10.Kung J, Swan AV, Arulkumaran S. Delivery of the posterior arm reduces shoulder dimensions in shoulder dystocia. Int J Obstet Gynecol. 2006;93:233–7. doi: 10.1016/j.ijgo.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 11.Lerner H, Durlacher K, Smith S, Hamilton E. Relationship between head-to-body delivery interval in shoulder dystocia and neonatal depression. Obstet Gynecol. 2011;118:318–22. doi: 10.1097/AOG.0b013e31822467e9. [DOI] [PubMed] [Google Scholar]
- 12.Gherman RB, Chauhan S, Ouzounian JG, Lerner H, Gonik B, Goodwin TM. Shoulder dystocia: The unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol. 2006;195:657–72. doi: 10.1016/j.ajog.2005.09.007. [DOI] [PubMed] [Google Scholar]


