Abstract
We evaluated whether phospholemman (PLM) regulates L-type Ca2+ current (ICa) in mouse ventricular myocytes. Expression of α1-subunit of L-type Ca2+ channels between wild-type (WT) and PLM knockout (KO) hearts was similar. Compared to WT myocytes, peak ICa (at −10 mV) from KO myocytes was ~41% larger, the inactivation time constant (τinact) of ICa was ~39% longer, but deactivation time constant (τdeact) was similar. In the presence of isoproterenol (1 µM), peak ICa was ~48% larger and τinact was ~144% higher in KO myocytes. With Ba2+ as the permeant ion, PLM enhanced voltage-dependent inactivation but had no effect on τdeact. To dissect the molecular determinants by which PLM regulated ICa, we expressed PLM mutants by adenovirus- mediated gene transfer in cultured KO myocytes. After 24 h in culture, KO myocytes expressing green fluorescent protein (GFP) had significantly larger peak ICa and longer τinact than KO myocytes expressing WT PLM; thereby independently confirming the observations in freshly isolated myocytes. Compared to KO myocytes expressing GFP, KO myocytes expressing the cytoplasmic domain truncation mutant (TM43), the non-phosphorylable S68A mutant, the phosphomimetic S68E mutant, and the signature PFXYD to alanine (ALL5) mutant all resulted in lower peak ICa. Expressing PLM mutants did not alter expression of α1-subunit of L-type Ca2+ channels in cultured KO myocytes. Our results suggested that both the extracellular PFXYD motif and the transmembrane domain of PLM but not the cytoplasmic tail were necessary for regulation of peak ICa amplitude. We conclude that PLM limits Ca2+ influx in cardiac myocytes by reducing maximal ICa and accelerating voltage-dependent inactivation.
Keywords: FXYD1, Ca2+ channels, phospholemman, arrhythmia
1. Introduction
Phospholemman (PLM), a 72-amino acid phosphoprotein with a single transmembrane (TM) domain [1], is highly expressed in cardiac muscle [2]. PLM co-immunoprecipitates with Na+-K+-ATPase [3–5], Na+/Ca2+ exchanger [6–8] and L-type Ca2+ channels [8] in the heart. PLM regulates the activities of Na+-K+-ATPase [5, 9–11] and Na+/Ca2+ exchanger [6, 12, 13] in cardiac myocytes. In HEK293 cells transfected with α1-subunit of cardiac L-type Ca2+ channel (Cav1.2) with the auxiliary subunits α2δ and β1b, PLM modulates the gating of L-type Ca2+ channels [8]. Specifically, in heterologous expression model systems, PLM slows deactivation and enhances the rate and magnitude of voltage-dependent inactivation (VDI). Ca2+-dependent inactivation (CDI) is not affected by PLM in heterologous expression model systems.
By virtue of its regulatory effects on Na+-K+-ATPase and Na+/Ca2+ exchanger, PLM is intimately involved in regulation of intracellular Ca2+ ([Ca2+]i) and Na+ concentrations ([Na+]i) and thus exerts major influences on cardiac excitation-contraction (EC) coupling, both in vitro [10] and in vivo [11, 14]. If PLM also regulates L-type Ca2+ channels in cardiac myocytes, the complexity of the relationship between PLM expression and cardiac contractility will escalate greatly. The successful engineering of PLM knockout (KO) mouse [15, 16] permits the hypothesis that PLM regulates L-type Ca2+ channels in cardiac myocytes to be rigorously tested. The present study was undertaken to examine whether PLM modulates L-type Ca2+ channels in adult cardiac myocytes, whether PLM limits Ca2+ influx via L-type Ca2+ channels under β-adrenergic stimulation; and to determine the molecular domain of PLM that is involved in regulation of L-type Ca2+ channels.
2. Materials and methods
2.1. Generation of PLM-deficient mice and animal care
PLM-KO mice backcrossed to a pure congenic C57BL/6 background were generated as described previously [15, 16]. Homozygous adult littermates ~3 mo old were used. Mice were housed and fed on a 12h:12h light-dark cycle at Temple University Animal Facility and were supervised by veterinary staff members. Standard care was provided to all mice used for experiments. All protocols applied to the mice in this study were approved and supervised by the Institutional Animal Care and Use Committee at Temple University.
2.2. Isolation and culture of adult murine cardiac myocytes
Cardiac myocytes were isolated from the septum and left ventricular (LV) free wall of WT and KO mice according to the protocol of Zhou et al. [17] and as modified by us [15, 18]. Isolated myocytes were plated on laminin-coated coverslips and either used on the same day, or placed in short-term culture [18] for 24h before calcium current measurements.
2.3. L-type Ca2+ current (ICa) measurements
Whole cell patch-clamp recordings were performed at 30°C as previously described [14, 15, 18]. The pipette diameter was 4–6 µm and the pipette resistance was 0.8–1.4 MΩ when filled with standard pipette solution containing (in mM): CsCl 110, TEA.Cl 20, HEPES 10, MgATP 5, and EGTA 10; pH 7.2. Extracellular bathing solution contained (in mM): N-methyl-D-glucamine 137, CsCl 5.4, CaCl2 2, MgSO4 1.3, HEPES 20, 4-aminopyridine 4, and glucose 15; pH 7.4. Our solutions were designed to be Na+- and K+-free. To ensure steady-state Ca2+ loading in the sarcoplasmic reticulum, 6 conditioning pulses (from −70 to 0 mV, 100 ms, 2 Hz) were delivered to the myocyte before the arrival of each test pulse (from −90 to +50 mV, 10 mV increments, 60 ms). In a subset of myocytes, after 6 conditioning pulses, holding potential was changed from −70 to −40 mV before each test pulse (from −40 to + 60 mV, 10 mV increments, 60 ms). Leak-subtracted inward currents were used in analysis for ICa amplitudes and inactivation and deactivation kinetics. Inward currents obtained under these conditions were blocked by 1 µM verapamil (data not shown). ICa was normalized to membrane capacitance (Cm) before comparison between WT and KO myocytes. All ICa amplitudes and τinact values, when given in Results, were measured at −10 mV. All experiments with Ca2+ as ion carrier used these solutions and voltage protocol. To evaluate the effects of holding potential on inhibition of ICa by PLM, in some experiments holding potential was varied between −90 and −40 mV and peak ICa was measured at −10 and 0 mV. To eliminate the possibility that at more hyperpolarizing holding potentials, ICa measured may potentially be contaminated by Ca2+ entry via fast Na+ channels, tetrodotoxin (TTX; 50 µM) was added to the bathing solution before current measurements. TTX at this concentration is known to totally block fast Na+ current in both rat [19] and mouse [20] cardiac ventricular cells. In another series of experiments, the effects of PLM on VDI were evaluated in freshly isolated WT and KO myocytes by replacing extracellular Ca2+ with Ba2+, and lengthening the test pulse to 300 ms.
2.4. Adenoviral infection of adult cardiac myocytes
Recombinant, replication-deficient adenovirus (Adv) expressing either green fluorescent protein (GFP) alone, GFP and WT dog PLM, or GFP and dog PLM mutants (non-phosphorylable S68A, phosphomimetic S68E, and cytoplasmic domain truncation TM43 mutants) were constructed as previously described [21, 22]. A new PLM mutant in which the signature extracellular PFXYD motif was mutated to alanine (ALL5) was generated using Altered Sites II in vitro mutagenesis system (Promega). Two hours after isolation from KO hearts, myocytes were infected with Adv-GFP (5.5 × 108 particles/ml), Adv-GFP-PLM (8.4 × 108 particles/ml) or Adv-GFP-PLM mutants (S68A 5.8 × 108; S68E 1.6 × 109; ALL5 7.5 × 108; TM43 6.4 × 108 particles/ml) in 5 ml of fetal bovine serum-free Eagle minimal essential medium (MEM) containing 0.2 % bovine serum albumin, creatine (5 mM), carnitine (2 mM), taurine (5 mM), NaHCO3 (4.2 mM), penicillin (30 mg/L), gentamicin (4 mg/L), insulin-transferrin-selenium supplement and 2,3-butanedione monoxime (10 mM) for 3h. An additional 5 ml of MEM (with same supplements) was then added, and myocytes were studied after 24h. Under our culture conditions, adult mouse LV myocytes maintain t-tubule organization and myocyte contractility for up to 48h [18]. For the sake of brevity, KO myocytes infected with Adv-GFP, Adv-GFP-PLM and Adv-GFP-PLM mutants are referred to as KO-GFP, KO-PLM, and the respective designation for the PLM mutant (e.g., KO-ALL5) myocytes, respectively.
2.5. Immunoblotting
Mouse LV homogenates [15, 23, 24] and cardiac myocyte lysates [18, 21] were prepared as previously described. For detection of WT PLM or its mutants (12% SDS-PAGE, reducing conditions with 5% β-mercaptoethanol), either monoclonal B8 which detects the NH2-terminus of dog but not rodent PLM [22] or polyclonal C2 antibody which detects the COOH-terminus of both rodent and dog PLM [21] was used. For detection of α1-subunit of L-type Ca2+ channel (Cav1.2)(5% SDS-PAGE, reducing conditions)[25] and calsequestrin (used as loading control)[15, 21], commercially available antibodies were used as previously described.
2.6. Statistics
All results are expressed as means ± SE. For analysis of ICa and IBa amplitudes, τinact, τdeact and protein abundance, 1-way ANOVA was used. A commercially available software package (JMP version 7, SAS Institute, Cary, NC) was used. In all analyses, p<0.05 was taken to be statistically significant.
3. Results
3.1. ICa in WT and KO myocytes
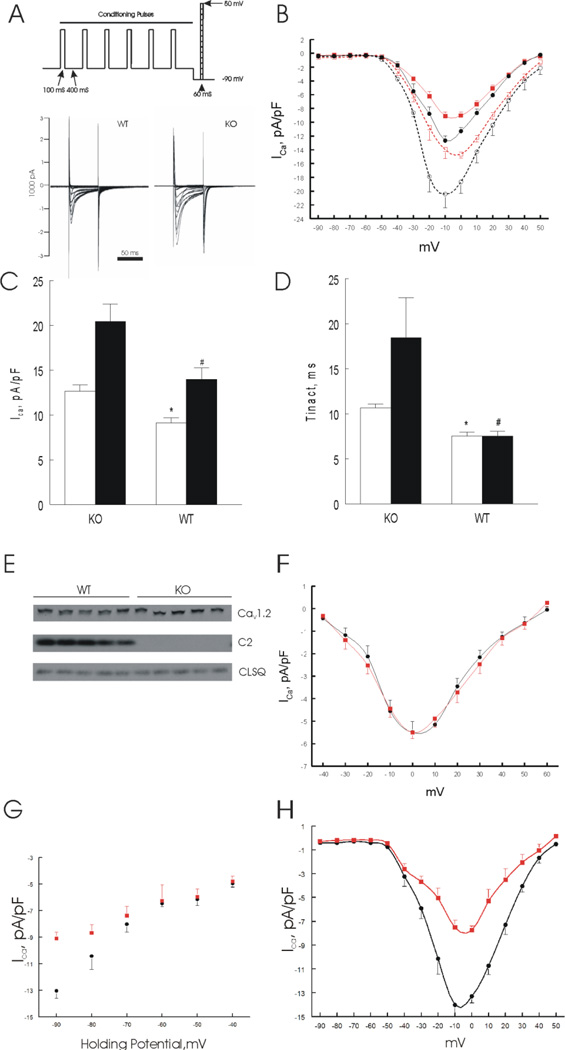
With Ca2+ as ion carrier and holding potential of −90 mV before test pulses, ICa amplitudes were larger in KO compared to WT myocytes (Fig. 1A). Peak ICa occurred at −10 mV for both WT and KO myocytes (Fig. 1B). At −10 mV, ICa amplitudes were 8.99 ± 0.49 and 12.67 ± 0.68 pA/pF, respectively, for WT (n=14) and KO (n=12) myocytes with holding potential at −90 mV (p<0.0002; Fig. 1C). Time constant of inactivation (τinact) in KO myocytes (10.65 ± 0.44 ms) was significantly (p<0.0001) longer than that in WT myocytes (7.67 ± 0.38 ms)(Fig. 1D). Time constant of deactivation (τdeact) was not different between WT (1.12 ± 0.10 ms) and KO myocytes (1.22 ± 0.18 ms)(p<0.65). Smaller ICa amplitude was not due to decreased Cav1.2 expression in WT (0.92 ± 0.02) compared to KO myocytes (0.94 ± 0.04 arbitrary units)(p<0.8; Fig.1E). However, when holding potential was stepped to −40 mV (a common practice to inactivate the fast inward Na+ current) before the arrival of test pulses, ICa differences between WT and KO myocytes were no longer apparent (Fig. 1F), in agreement with our previous report [15]. In addition, the voltage at which peak ICa occurred right-shifted from −10 to 0 mV. At 0 mV, ICa amplitudes were 5.51 ± 0.27 and 5.76 ± 0.50 pA/pF, respectively, for WT (n=6) and KO (n=4) myocytes (p<0.65) with holding potential at −40 mV (Fig. 1F). The differences in ICa amplitudes between WT and KO myocytes progressively decreased at more depolarizing holding potentials (Fig. 1G). Using TTX (50 µM) to block potential Ca2+ entry via activated fast Na+ channels, significant (p<0.0001) differences in ICa amplitudes persisted (Fig. 1H). Collectively, these observations suggest that in adult mouse ventricular myocytes held at more physiological membrane potential (−90 vs. −40 mV), PLM decreased ICa amplitude and enhanced inactivation but had no effect on deactivation.
Figure 1.
Phospholemman (PLM) regulates L-type Ca2+ current (ICa) in adult mouse left ventricular (LV) myocytes. Myocytes were isolated from LV of wild-type (WT) and phospholemman knockout (KO) mice and ICa was measured on the same day. A. Voltage-clamp protocol and representative ICa traces from WT and KO myocytes. B. Current-voltage (I-V) relationship of ICa from WT (■; n=14) and KO (●; n=12) myocytes at baseline; and after stimulation with 1 µM isoproterenol (□ WT, n=7; and ○ KO, n=5). Holding potential was −70 mV and stepped to −90 mV before arrival of test pulses. Error bars are not shown if they fall within the boundaries of the symbols. C & D. Peak ICa amplitudes and time constants of inactivation (τinact) (at −10 mV) of KO and WT myocytes, both in the absence (open bars) and presence (solid bars) of 1 µM isoproterenol.*p<0.0002, WT vs. KO; #p<0.008, WT-Iso vs. KO-Iso. E. LV homogenates were prepared from WT and KO mice and probed for α1-subunit of L-type Ca2+ channel (Cav1.2) and phospholemman (C2); calsequestrin (CLSQ) was used as loading control. There were no differences (p<0.8) in Cav1.2 expression between WT (0.92 ± 0.02) and KO myocytes (0.94 ± 0.04 arbitrary units)(n=5 each). F. I-V relationship of ICa from WT (■; n=6) and KO (●; n=4) myocytes at baseline. Holding potential (−70 mV) was stepped to −40 mV before arrival of test pulses. Error bars are not shown if they fall within the boundaries of symbols. Note the difference in ordinate scales between B and F. G. ICa amplitudes at −10 mV elicited at holding potentials from −90 to −40 mV for WT (■; n=3 to 15) and KO (●; n=3 to 15) myocytes at baseline. Two-way ANOVA indicates significant group (WT vs. KO; p<0.0001), holding potential (p<0.0001) and group × holding potential interaction (p<0.0001) effects, indicating that varying the holding potential significantly affected the inherent differences in ICa between WT and KO myocytes. H. Baseline current-voltage (I-V) relationship of ICa ilicited at holding potential of −90 mV from WT (■; n=4) and KO (●; n=4) myocytes in the presence of 50 µM TTX.
3.2 Effects of isoproterenol on ICa in WT and KO myocytes
Addition of isoproterenol (Iso, 1 µM) increased ICa in both WT and KO myocytes (Fig. 1B). At −10 mV, ICa amplitude was 20.42 ± 1.98 pA/pF in KO myocytes treated with Iso and was significantly (p<0.007) higher than the 13.80 ± 0.91 pA/pF measured in WT myocytes (Fig. 1C). In KO myocytes stimulated with Iso, τinact (18.43 ± 4.49 ms) was significantly (p<0.008) longer than that in WT myocytes exposed to Iso (7.54 ± 0.36 ms)(Fig. 1D).
3.3 PLM enhanced voltage-dependent inactivation
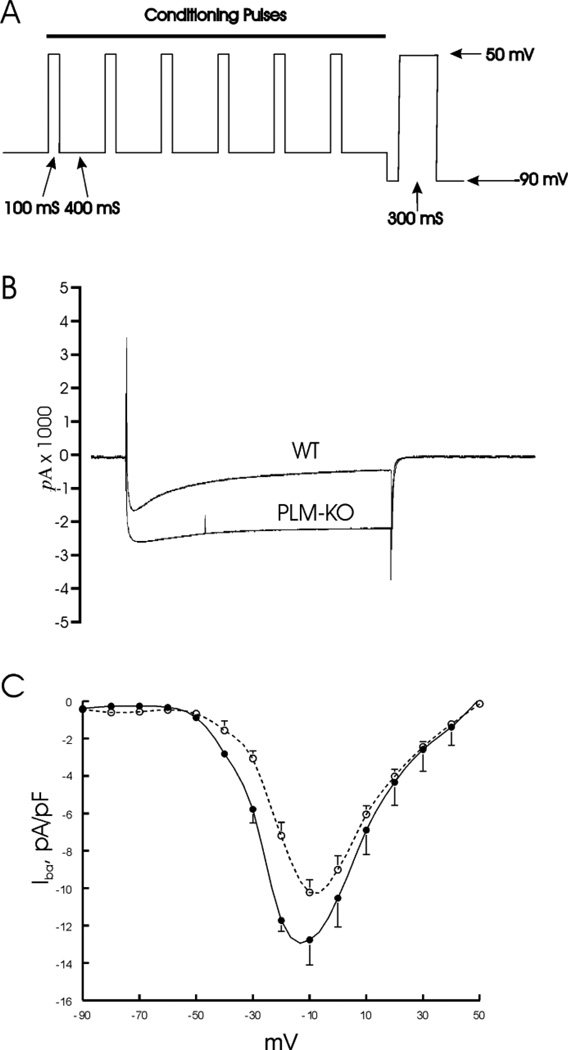
ICa inactivation is classically separated into Ca2+-dependent inactivation (CDI) and voltage-dependent inactivation (VDI). In a second series of experiments, Ba2+ was used to examine VDI (Fig. 2). Similar to ICa, peak IBa occurred at −10 mV (Fig. 2C) and was significantly (p<0.02) lower in WT (10.22 ± 0.67 pA/pF; n=5) when compared to KO myocytes (12.76 ± 1.35 pA/pF; n=5). With Ba2+ as the permeant ion, τinact was significantly slower (p<0.05) in KO (117.4 ± 15.9 ms) than WT (64.4 ± 15.2 ms) myocytes (Fig. 2B). At −10 mV, compared to WT myocytes, PLM accelerated VDI by 45%, similar to the 28% decrease in τinact when Ca2+ was used as the permeant ion. These observations suggest that the major PLM effect on ICa inactivation was VDI.
Figure 2.
PLM enhances voltage-dependent inactivation of ICa. ICa was measured in freshly isolated myocytes from WT and KO hearts, using Ba2+ (2 mM) as permeant ion. A. Voltage-clamp protocol: test pulses from −90 to +50 mV (in 10 mV increments) were extended from 60 to 300 ms duration (for simplicity, only one test pulse is shown). B. Representative IBa traces at −10 mV from WT and KO myocytes are shown. Note prolonged time course of IBa in KO compared to WT myocyte. C. I-V curves from WT (○; n=5) and KO myocytes (●; n=5).
In agreement with observations when Ca2+ was the permeant ion, τdeact of IBa was not different between WT (1.73 ± 0.02 ms) and KO myocytes (1.66 ± 0.11 ms)(p<0.55).
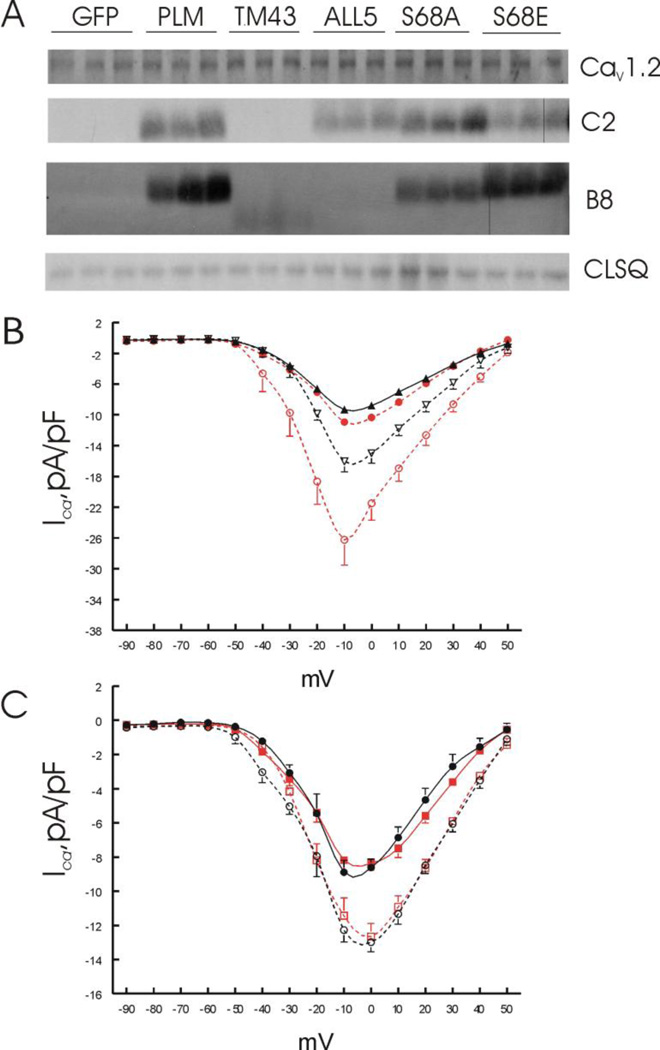
3.4 Adenovirus-mediated PLM expression decreased ICa in KO myocytes
In KO myocytes infected with Adv expressing WT PLM, expression of Cav1.2 was similar to KO myocytes infected with Adv expressing GFP (Fig. 3A). At baseline, peak ICa amplitudes were significantly (p<0.03) lower in KO-PLM (9.34 ± 0.50 pA/pF; n=6) compared to KO-GFP myocytes (10.93 ± 0.41 pA/pF; n=8)(Fig. 3B). At −10 mV, τinact was significantly (p<0.04) longer in KO-GFP (14.04 ± 2.20 ms) compared to KO-PLM myocytes (9.10 ± 0.72 ms)(Fig. 4C). Iso significantly (p<0.05) increased ICa in both KO-GFP (25.32 ± 2.92 pA/pF) and KO-PLM myocytes (16.05 ± 1.35 pA/pF)(Fig. 3B). These results corroborated the observations on ICa in freshly isolated WT and KO myocytes and indicated that short-term culture and adenovirus infection did not affect the ability of PLM to modulate ICa amplitudes in adult cardiac myocytes.
Figure 3.
Effects of PLM mutants on Cav1.2 expression and ICa. LV myocytes isolated from KO hearts were infected with adenovirus (Adv) expressing either green fluorescent protein (GFP), WT PLM, the cytoplasmic domain truncation mutant TM43, the signature PFXYD motif changed to Ala mutant (ALL5), the non-phosphorylable Ser68 mutant (S68A), or the phosphomimetic Ser68 mutant (S68E); and placed in culture for 24 hours prior to ICa measurements and Western blotting. A. Myocyte lysates were prepared and probed for Cav1.2, C-terminus (C2) or N-terminus (B8) of PLM and its mutants, with calsequestrin (CLSQ) serving as the loading control. There were no differences (p<0.98) in Cav1.2 expression among KO myocytes expressing GFP (1.44 ± 0.01), WT PLM (1.42 ±0.01), TM43 (1.45 ± 0.08), ALL5 (1.46 ± 0.07), S68A (1.42 ± 0.00) and S68E (1.46 ± 0.05) mutants (n=3 each; values in arbitrary units). As expected, C2 which detects the cytoplasmic tail of PLM fail to detect any signal in KO-GFP and KO-TM43 myocytes. Likewise, there were no B8 (detects the extracellular NH2-terminus of dog PLM) signals in KO-GFP and KO-ALL5 myocytes. B8 signals in KO-TM43 myocytes were weak, downward shifted but present. B. I-V curves of ICa in KO-GFP (●; n=8) and KO-PLM myocytes (▲; n=6) at baseline; and after exposure to 1 µM isoproterenol in KO-GFP (○; n=6) and KO-PLM (∇; n=4) myocytes. C. I-V curves of ICa in KO-S68A (●; n=6) and KO-S68E (■; n=6) myocytes at baseline, and after addition of 1 µM isoproterenol to KO-S68A (○; n=5) and KO-S68E (□; n=5) myocytes. Note the difference in ordinate scales between B and C.
Figure 4.
Effects of PLM and its mutants on peak ICa in cultured KO myocytes. A. Schematic representation of WT PLM (both dog and rat) and dog PLM mutants. The structure of dog PLM (PLM) is shown to consist of an extracellular NH2-terminal domain (black), a single-span transmembrane domain (blue), and cytoplasmic COOH-terminal domain (purple). The signature PFXYD sequence is shown in gold at the NH2-terminus, and the 4 potential phosphorylation sites (Ser62, Ser63, Ser68 and Thr69) are represented by pink boxes at the COOH-terminus. The 6 amino acid differences between dog PLM and rat PLM (ALIGN) are shown. Mouse PLM is identical to rat PLM except that Thr69 is replaced by Ser69 (not shown). All PLM mutants were constructed on the dog PLM backbone. Shown are representations of COOH-terminal deletion mutant (TM43), Ser68 substitution mutants (S68A and S68E), and ALL5 mutant in which the signature PFXYD motif is changed to Ala (shown as gold to red). Ser to Ala mutation is shown as pink to black, whereas Ser to Glu mutation is shown as pink to yellow. B. Summary of peak ICa (at −10 mV) measured in adenovirus-infected KO myocytes followed by culture for 24 hours, both in the absence (open bars) and presence (filled bars) of 1 µM isoproterenol. *p<0.03, KO-GFP vs. KO-PLM or KO-PLM mutants at baseline; #p<0.05, KO-GFP vs. KO-PLM or KO-PLM mutants in the presence of 1 µM isoproterenol; $p<0.04, KO-PLM vs. KO-ALL5 at baseline, and KO-PLM vs. KO-ALL5 or KO-S68E or KO-S68A in the presence of 1 µM isoproterenol. C. Summary of τinact (at −10 mV) measured in adenovirus-infected KO myocytes followed by culture for 24 hours, both in the absence (open bars) and presence (filled bars) of 1 µM isoproterenol. *p<0.035, KO-GFP vs. KO-PLM or KO-PLM mutants at baseline; #p<0.0045, KO-GFP vs. KO-PLM or KO-PLM mutants in the presence of 1 µM isoproterenol.
3.5 Effects of Ser68 phosphorylation on ICa
Phosphorylation of Ser68 of PLM is critical in its regulation of both Na+-K+-ATPase [9] and Na+/Ca2+ exchanger [13]. To examine the role of Ser68 phosphorylation in regulation of ICa, we expressed WT PLM or its Ser68 mutants (Fig. 4A) in KO myocytes by adenovirus-mediated gene transfer. After 24 h in culture, KO myocytes expressed WT PLM, S68A and S68E mutants as detected by B8 or C2 antibodies (Fig. 3A). Expression of Cav1.2 was similar among KO-GFP, KO-PLM, KO-S68A and KO-S68E myocytes (Fig. 3A). At baseline, compared to KO-GFP myocytes (10.93 ± 0.41pA/pF; n=9), both S68A (8.89 ± 0.70 pA/pF, n=6; p<0.02) and S68E mutants (8.19 ± 0.65 pA/pF, n=6; p<0.003) suppressed peak ICa equally (Fig. 3C). There were no statistically significant differences in ICa amplitudes between KO-PLM and KO-S68A (p<0.6) and between KO-PLM and KO-S68E (p<0.2) myocytes (Fig. 4B). These results suggest that at baseline, Ser68 phosphorylation did not play a major role in regulation of ICa by PLM.
In the presence of Iso, ICa amplitudes increased in both KO-S68A (12.27 ± 0.71 pA/pF) and KO-S68E (11.43 ± 1.04 pA/pF) myocytes (Fig. 3C). However, ICa amplitudes were significantly lower in both KO-S68A (p<0.04) and KO-S68E (p<0.03) when compared to KO-PLM myocytes (16.05 ± 1.35 pA/pF) and less than half (p<0.005) when compared to KO-GFP myocytes (25.32 ± 2.92 pA/pF)(Fig. 4B). These observations suggest that mutating Ser68 in PLM may alter the physical interaction between PLM and L-type Ca2+ channels in the presence of isoproterenol, resulting in enhanced inhibition of ICa by the Ser68 mutants.
3.6 Role of extracellular PFXYD motif in regulation of ICa
In heterologous expression systems, the signature PFXYD motif of PLM was found to be important in modulating ICa [26]. Mutation of the extracellular PFXYD motif did not affect detection by C2 antibody (raised against the C-terminus of PLM) but abolished the B8 (detects the N-terminus of dog PLM) signal as expected (Fig. 3A). Expression of ALL5 mutant in cultured KO myocytes did not affect Cav1.2 expression when compared to KO-GFP myocytes (Fig. 3A). ICa amplitudes in KO-ALL5 myocytes (7.21 ± 0.62 pA/pF, n=8; p<0.0006) were lower when compared to KO-GFP myocytes (10.93 ± 0.41 pA/pF; n=9)(Fig. 4B). Compared to KO-PLM myocytes (9.34 ± 0.50 pA/pF), ICa amplitudes were significantly (p<0.03) lower in KO-ALL5 myocytes (Fig. 4B). These results suggest that mutating the extracellular PFXYD motif to alanine resulted in further suppression of ICa amplitudes in adult cardiac myocytes.
In the presence of Iso, peak ICa amplitudes were significantly (p<0.0004) lower in KO-ALL5 (11.82 ± 0.70 pA/pF) when compared to KO-GFP (25.32 ± 2.92 pA/pF) myocytes (Fig. 4B) and τinact was significantly (p<0.005) shorter (Fig. 4C). Compared to KO-PLM myocytes (16.05 ± 1.35 pA/pF), peak ICa was significantly (p<0.01) lower in KO-ALL5 myocytes (Fig. 4B).
3.7 Role of cytoplasmic domain in regulation of ICa
We next expressed the truncation TM43 mutant (Fig. 4A) in KO myocytes to assess the role of cytoplasmic domain of PLM in regulating ICa. As expected, C2 antibody did not detect any signal while the B8 signal was present but weak in KO-TM43 myocytes (Fig. 3A). TM43 did not affect Cav1.2 expression in cultured KO myocytes (Fig. 3A). At baseline, ICa amplitudes in KO-TM43 myocytes (8.79 ± 0.51 pA/pF, n=9; p<0.005) were lower (Fig. 4B) and τinact was longer when compared to KO-GFP myocytes (Fig. 4C). ICa amplitudes (Fig. 4B) and τinact (Fig. 4C) in KO-PLM myocytes were similar to KO-TM43 myocytes. Collectively, these results suggest that at baseline, the cytoplasmic domain of PLM was not necessary in modulation of ICa.
In the presence of Iso, peak ICa amplitudes were significantly (p<0.0004) lower in KO-TM43 (13.63 ± 0.56 pA/pF)(Fig. 4B) and τinact (7.74 ± 1.20 ms)(Fig. 4C) was significantly (p<0.04) shorter when compared to KO-GFP myocytes. When compared to KO-PLM myocytes, neither peak ICa (Fig. 4B) nor τinact (Fig. 4C) was different in KO-TM43 myocytes.
To summarize, in the presence of Iso, when compared to KO-PLM myocytes, peak ICa amplitudes were similar in KO-TM43 myocytes (p<0.08) but significantly (p<0.015) lower in KO-ALL5, KO-S68A and KO-S68E myocytes (Fig. 4B). Our data suggest that it is the transmembrane domain of PLM that was largely responsible for the regulation of ICa amplitudes and that the extracellular PFXYD motif and cytoplasmic serine68 provide additional fine tuning of this regulation.
4 Discussion
It is well established that phospholemman regulates Na+-K+-ATPase and Na+/Ca2+ exchanger in the heart [27]. Recent studies utilizing heterologous expression systems suggest that PLM also regulates cardiac L-type Ca2+ channels [8, 26]. Enthusiasm for yet another novel regulatory function of PLM, however, must be tempered by the numerous unsuccessful attempts to reconstitute the complete β-adrenergic receptor induced regulation of ICa using heterologous expression systems [28, 29]. Thus the first major finding is that in freshly isolated adult cardiac myocytes held at the more physiological membrane potential of −90 mV, PLM decreased ICa amplitude by ~41% (Fig. 1C). It is important to note that both our pipette and bathing solutions were Na+- and K+-free, thereby eliminating any effect of PLM on Na+/Ca2+ exchanger and Na+-K+-ATPase that might secondarily affect ICa measurements. In addition, the differences in ICa amplitudes between WT and KO myocytes were maintained in the presence of TTX used to block potential Ca2+ entry via activated Na+ channels, indicating PLM’s effect was exerted on L-type Ca2+ rather than on fast Na+ channels. To evaluate the contribution by different PLM residues and domains on ICa inhibition, we expressed PLM mutants in KO myocytes cultured for 24 h. Peak ICa amplitudes in freshly isolated WT myocytes (Fig. 1C) were similar to those in cultured KO myocytes expressing WT PLM (Fig. 4B), consistent with previous report by Zhou et al. (31) that short term culture had no effect on ICa amplitudes in adult mouse myocytes. In addition, in cultured KO myocytes expressing WT PLM, ICa amplitudes were lower compared to those measured in KO myocytes expressing GFP (Fig. 4B). The results of the reconstitution experiment independently confirmed the inhibitory effects of PLM on ICa in freshly isolated myocytes (Fig. 1C).
We have previously reported that peak ICa amplitudes and inactivation time constants elicited at holding potential of −40 mV were not different between WT and PLM KO myocytes [15]. There were three major differences in experimental conditions that likely account for the differences. The first is that neither pipette nor extracellular solutions were Na+-free in our previous study, necessitating switching to a less physiological holding potential of −40 mV to inactivate the fast Na+ current. The second is that the range of test pulses (from −30 to +60 mV; previous study, vs. from −80 to +50 mV; present study) was different. It is known that pulsing from more positive holding potentials would result in inhibition, as opposed to facilitation, of ICa [30]. The third is that holding potential was −90 in the present study compared to −40 in the previous study. It is known that in rodent myocytes, ICa amplitudes elicited at holding potential of −90 mV are larger than those elicited at −40 mV [31]. Indeed, maximal ICa amplitudes in both WT and KO myocytes were lower when holding potential was at −40 mV (Fig. 1F) when compared to those measured when holding potential was at −90 mV (Fig. 1B). More importantly, differences in ICa amplitudes between WT and KO myocytes disappeared as holding potential became more positive (Fig. 1G). It is known that inhibition of L-type Ca2+ channel by dihydropyridines [32] and the indolizinsulphone SR33557 [33] is voltage-dependent. For example, 10−7 M SR33557 induced tonic block of ICa at holding potential of −50 mV but did not reduce ICa elicited at holding potential of −80 mV. The proposed mechanism is that both nitrendipine and SR33557 bind with high affinity to the L-type Ca2+ channel in the inactivated state (channel closed but not available to be opened). Since we have previously shown that PLM co-immunoprecipitates with Cav1.2 [8], and our current results with PLM mutants suggest interaction between the TM domains of Cav1.2 and PLM (Fig. 4), we speculate that PLM interacts with higher affinity to the rested state (channel closed but available to be opened by depolarization) compared to the inactivated state of the Ca2+ channel. This will explain the voltage-dependence of PLM inhibition of L-type Ca2+ channels. We also add that −90 mV is closer to the resting membrane potential than −40 mV. Thus under physiological conditions, PLM will likely exert its modulatory effect on ICa.
In the present study, we focused on residues of PLM that have previously been shown to be important in regulation of Na+-K+-ATPase and Na+/Ca2+ exchanger in the heart. Ser68 is phosphorylated by both protein kinase A and protein kinase C [34]. When phosphorylated at Ser68, inhibition of Na+-K+-ATPase is relieved but Na+/Ca2+ exchanger is simultaneously inhibited [27]. Thus a second major finding is that Ser68 phosphorylation and indeed the cytoplasmic tail (residues 44 to 72) were not crucial in regulation of ICa in adult cardiac myocytes under basal conditions (Fig. 4B). Based on the results of the four PLM mutants, the TM domain of PLM appears critical in its regulation of ICa. The signature PFXYD motif stabilizes interactions between α- and β-subunits of Na+-K+-ATPase [35] and modulates L-type Ca2+ channel gating in heterologous expression systems [26]. Our data indicate that in addition to the TM domain, the extracellular PFXYD motif contributes to inhibition of ICa.
In agreement with the observations in heterologous expression systems [8], PLM enhanced voltage-dependent inactivation in adult LV myocytes by ~39% (Fig. 2B). In addition, peak ICa in cardiac myocytes was lower in the presence of PLM (Fig. 1C), consistent with the observations in heterologous expression systems that Ca2+ influx was reduced during the depolarization step in the presence of PLM [8]. By contrast, we did not detect any effect of PLM on deactivation, regardless of whether Ca2+ or Ba2+ was the permeant ion. The major physiological effect of PLM on ICa in adult cardiac myocytes was modulation of Ca2+ influx during the depolarization phase of the action potential, due to both smaller peak ICa amplitude and speeding of voltage-dependent inactivation. Consistent with this interpretation is the observation that action potential duration (both at 50 and 90% repolarization) was significantly shorter in WT when compared to KO myocytes [15]. In KO myocytes, prolongation of APD90 is likely due to enhanced NCX1 activity [15, 36, 37] whereas prolongation of APD50 is consistent with increased ICa amplitude and slowed inactivation kinetics.
Under resting conditions, ~46% of Ser68 of PLM is estimated to be phosphorylated in adult rat myocytes based on inhibition of Na+/Ca2+ exchanger current by S68E mutant [22]. Using phospho-specific anti-PLM antibodies [38, 39], ~30–40% of PLM in adult rat myocytes [38, 40] and ~25% of PLM in guinea pig myocytes [41] are phosphorylated under basal conditions. Since myocyte contractility, [Ca2+]i transient amplitudes (1.8 mM [Ca2+]o, 1 Hz, 37°C), systolic and diastolic [Ca2+]i [15] and resting [Na+]i [9, 11] are similar between WT and KO myocytes under basal conditions, the regulatory effects of PLM on myocyte [Ca2+]i dynamics (Na+-K+-ATPase, Na+/Ca2+ exchanger and L-type Ca2+ channel) are not readily discernible and PLM is functionally quiescent [27, 42]. This conclusion is supported by the observation that in vivo cardiac function under basal conditions is similar between WT and KO mice [11]. Perhaps a subtle hint indicating the presence of PLM in resting myocytes is the shortening of both APD50 (accelerated ICa inactivation) and APD90 (partial inhibition of Na+/Ca2+ exchanger) in WT as compared to KO myocytes [15]. Although APD prolongation is associated with increased risks of arrhythmias, the physiological significance of APD prolongation in KO mice is not clear as these mice have normal life-spans compared to WT mice. However, the pathophysiological significance of APD prolongation in KO mice may be unmasked after myocardial infarction (MI), when despite significantly (p<0.01) higher ejection fraction (42.4 ± 4.6 vs. 20.8 ± 1.7%), KO-MI mice had reduced survival (50%) compared to WT-MI mice (70%) at 3 weeks post-MI [43], likely as a result of sudden death from increased arrhythmogenesis.
Under stressful conditions when catecholamine levels are high, PLM is phosphorylated at Ser68 [34]. Phosphorylated PLM minimizes Na+ overload (by relieving inhibition of Na+-K+-ATPase), thereby increasing the driving force for forward Na+/Ca2+ exchange and promotes Ca2+ efflux from cardiac cells under stress. Our present observation that in the presence of isoproterenol, the differences in ICa (~6.8 pA/pF) and τinact (~10.9 ms) between KO and WT myocytes was almost 2- and 4-times of those measured under baseline conditions (~3.7 pA/pF and ~3.0 ms, respectively), suggested that another function of PLM is to limit Ca2+ entry into cardiac myocytes under stress.
In summary, phospholemman modulated Ca2+ entry through L-type Ca2+ channels in adult LV myocytes. Phospholemman reduced peak L-type Ca2+ current amplitude and enhanced voltage-independent inactivation, but had no effect on deactivation of L-type Ca2+ channels. Only the transmembrane and the extracellular (signature PFXYD motif) domains but not the cytoplasmic tail of phospholemman were necessary for regulation of L-type Ca2+ channels. We conclude that in concert with its effects on Na+-K+-ATPase, Na+/Ca2+ exchanger and L-type Ca2+ channel, phospholemman reduces Na+ and Ca2+ overload in cardiac myocytes under high catecholamine stimulation, thereby minimizes risks of arrhythmogenesis and serves as a cardiac “stress” protein.
Highlights.
Phospholemman regulates cardiac L-type calcium channels.
Inhibition of L-type calcium channels is dependent on holding potential.
Phospholemman decreases peak calcium current.
Phospholemman enhances voltage-dependent inactivation.
Transmembrane domain of phospholemman is critical for inhibition.
Acknowledgments
This work was supported in part by National Institutes of Health Grants RO1-HL58672 and RO1-HL74854 (JYC); RO1-HL56205, RO1-HL61690, RO1-HL85503, PO1-HL-75443 and PO1-HL-91799 (WJK); and PO1-HL91799 (Project 2; AMF).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
None.
References
- 1.Palmer CJ, Scott BT, Jones LR. Purification and complete sequence determination of the major plasma membrane substrate for cAMP-dependent protein kinase and protein kinase C in myocardium. J Biol Chem. 1991;266:11126–11130. [PubMed] [Google Scholar]
- 2.Presti CF, Jones LR, Lindemann JP. Isoproterenol-induced phosphorylation of a 15-kilodalton sarcolemmal protein in intact myocardium. J Biol Chem. 1985;260:3860–3867. [PubMed] [Google Scholar]
- 3.Crambert G, Fuzesi M, Garty H, Karlish S, Geering K. Phospholemman (FXYD1) associates with Na,K-ATPase and regulates its transport properties. Proc Natl Acad Sci USA. 2002;99:11476–11481. doi: 10.1073/pnas.182267299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bossuyt J, Ai X, Moorman JR, Pogwizd SM, Bers DM. Expression and phosphorylation of the Na-pump regulatory subunit phospholemman in heart failure. Circ Res. 2005;97:558–565. doi: 10.1161/01.RES.0000181172.27931.c3. [DOI] [PubMed] [Google Scholar]
- 5.Fuller W, Eaton P, Bell JR, Shattock MJ. Ischemia-induced phosphorylation of phospholemman directly activates rat cardiac Na/K-ATPase. Faseb J. 2004;18:197–199. doi: 10.1096/fj.03-0213fje. [DOI] [PubMed] [Google Scholar]
- 6.Ahlers BA, Zhang XQ, Moorman JR, Rothblum LI, Carl LL, Song J, et al. Identification of an endogenous inhibitor of the cardiac Na+/Ca2+ exchanger, phospholemman. J Biol Chem. 2005;280:19875–19882. doi: 10.1074/jbc.M414703200. [DOI] [PubMed] [Google Scholar]
- 7.Mirza MA, Zhang XQ, Ahlers BA, Qureshi A, Carl LL, Song J, et al. Effects of phospholemman downregulation on contractility and [Ca2+]i transients in adult rat cardiac myocytes. Am J Physiol Heart Circ Physiol. 2004;286:H1322–H1330. doi: 10.1152/ajpheart.00997.2003. [DOI] [PubMed] [Google Scholar]
- 8.Wang X, Gao G, Guo K, Yarotskyy V, Huang C, Elmslie KS, et al. Phospholemman modulates the gating of cardiac L-type calcium channels. Biophys J. 2010;98:1149–1159. doi: 10.1016/j.bpj.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Despa S, Bossuyt J, Han F, Ginsburg KS, Jia LG, Kutchai H, et al. Phospholemman-phosphorylation mediates the β-adrenergic effects on Na/K pump function in cardiac myocytes. Circ Res. 2005;97:252–259. doi: 10.1161/01.RES.0000176532.97731.e5. [DOI] [PubMed] [Google Scholar]
- 10.Despa S, Tucker A, Bers D. PLM-mediated activation of Na/K-ATPase limits [Na]i and inotropic state during β-adrenergic stimulation in mouse ventricular myocytes. Circulation. 2008;117:1849–1855. doi: 10.1161/CIRCULATIONAHA.107.754051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang J, Gao E, Song J, Zhang XQ, Li J, Koch WJ, et al. Phospholemman and β-adrenergic stimulation in the heart. Am J Physiol Heart Circ Physiol. 2010;298:H807–H815. doi: 10.1152/ajpheart.00877.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang XQ, Qureshi A, Song J, Carl LL, Tian Q, Stahl RC, et al. Phospholemman modulates Na+/Ca2+ exchange in adult rat cardiac myocytes. Am J Physiol Heart Circ Physiol. 2003;284:H225–H233. doi: 10.1152/ajpheart.00698.2002. [DOI] [PubMed] [Google Scholar]
- 13.Zhang XQ, Ahlers BA, Tucker AL, Song J, Wang J, Moorman JR, et al. Phospholemman inhibition of the cardiac Na+/Ca2+ exchanger. Role of phosphorylation. J Biol Chem. 2006;281:7784–7792. doi: 10.1074/jbc.M512092200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Gao E, Rabinowitz J, Song J, Zhang XQ, Koch WJ, et al. Regulation of in vivo cardiac contractility by phospholemman: role of Na+/Ca2+ exchange. Am J Physiol Heart Circ Physiol. 2011;300:H859–H868. doi: 10.1152/ajpheart.00894.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tucker AL, Song J, Zhang XQ, Wang J, Ahlers BA, Carl LL, et al. Altered contractility and [Ca2+]i homeostasis in phospholemman-deficient murine myocytes: Role of Na+/Ca2+ exchange. Am J Physiol Heart Circ Physiol. 2006;291:H2199–H2209. doi: 10.1152/ajpheart.01181.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jia LG, Donnet C, Bogaev RC, Blatt RJ, McKinney CE, Day KH, et al. Hypertrophy, increased ejection fraction, and reduced Na-K-ATPase activity in phospholemman-deficient mice. Am J Physiol Heart Circ Physiol. 2005;288:H1982–H1988. doi: 10.1152/ajpheart.00142.2004. [DOI] [PubMed] [Google Scholar]
- 17.Zhou YY, Wang SQ, Zhu WZ, Chruscinski A, Kobilka BK, Ziman B, et al. Culture and adenoviral infection of adult mouse cardiac myocytes: methods for cellular genetic physiology. Am J Physiol Heart Circ Physiol. 2000;279:H429–H436. doi: 10.1152/ajpheart.2000.279.1.H429. [DOI] [PubMed] [Google Scholar]
- 18.Song J, Zhang XQ, Wang J, Cheskis E, Chan TO, Feldman AM, et al. Regulation of cardiac myocyte contractility by phospholemman:Na+/Ca2+ exchange vs. Na+-K+-ATPase. Am J Physiol Heart Circ Physiol. 2008;295:H1615–H1625. doi: 10.1152/ajpheart.00287.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown AM, Lee KS, Powell T. Sodium current in single rat heart muscle cells. J Physiol. 1981;318:479–500. doi: 10.1113/jphysiol.1981.sp013879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benndorf K, Boldt W, Nilius B. Sodium current in single myocardial mouse cells. Pflugers Arch. 1985;404:190–196. doi: 10.1007/BF00585418. [DOI] [PubMed] [Google Scholar]
- 21.Song J, Zhang XQ, Carl LL, Qureshi A, Rothblum LI, Cheung JY. Overexpression of phospholemman alter contractility and [Ca2+]i transients in adult rat myocytes. Am Journal of Physiol Heart Circ Physiol. 2002;283:H576–H583. doi: 10.1152/ajpheart.00197.2002. [DOI] [PubMed] [Google Scholar]
- 22.Song J, Zhang XQ, Ahlers BA, Carl LL, Wang J, Rothblum LI, et al. Serine68 of phospholemman is critical in modulation of contractility, [Ca2+]i transients, and Na+/Ca2+ exchange in adult rat cardiac myocytes. Am J Physiol Heart Circ Physiol. 2005;288:H2342–H2354. doi: 10.1152/ajpheart.01133.2004. [DOI] [PubMed] [Google Scholar]
- 23.Wang J, Chan TO, Zhang XQ, Gao E, Song J, Koch WJ, et al. Induced overexpression of Na+/Ca2+ exchanger transgene: Altered myocyte contractility, [Ca2+]i transients, SR Ca2+ contents and action potential duration. Am J Physiol Heart Circ Physiol. 2009;297:H590–H601. doi: 10.1152/ajpheart.00190.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J, Gao E, Chan TO, Zhang XQ, Song J, Shang X, et al. Induced overexpression of Na+/Ca2+ exchanger does not aggravate myocardial dysfunction induced by transverse aortic constriction. J Card Failure. 2013;19:60–70. doi: 10.1016/j.cardfail.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song J, Gao E, Wang J, Zhang XQ, Chan TO, Koch WJ, et al. Constitutive overexpression of phospholemman S68E mutant results in arrhythmias, early mortality and heart failure: Potenial involvement of Na+/Ca2+ exchanger. Am J Physiol Heart Circ Physiol. 2012;302:H770–H781. doi: 10.1152/ajpheart.00733.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guo K, Wang X, Gao G, Huang C, Elmslie KS, Peterson BZ. Amino acid substitutions in the FXYD motif enhance phospholemman-induced modulation of cardiac L-type calcium channels. Am J Physiol Cell Physiol. 2010;299:C1203–C1211. doi: 10.1152/ajpcell.00149.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheung JY, Zhang XQ, Song J, Gao E, Chan TO, Rabinowitz JE, et al. Coordinated regulation of cardiac Na+/Ca2+ exchanger and Na+-K+-ATPase by phospholemman (FXYD1) Adv Expt'l Med & Biol. 2013;961:175–190. doi: 10.1007/978-1-4614-4756-6_15. [DOI] [PubMed] [Google Scholar]
- 28.Weiss S, Oz S, Benmocha A, Dascal N. Regulation of cardiac L-type Ca2+ channel CaV1.2 via the β-adrenergic-cAMP-protein kinase A pathway: old dogmas, advances, and new uncertainties. Circ Res. 2013;113:617–631. doi: 10.1161/CIRCRESAHA.113.301781. [DOI] [PubMed] [Google Scholar]
- 29.Hofmann F, Flockerzi V, Kahl S, Wegener JW. L-type CaV1.2 calcium channels: from in vitro findings to in vivo function. Physiol Rev. 2014;94:303–326. doi: 10.1152/physrev.00016.2013. [DOI] [PubMed] [Google Scholar]
- 30.McDonald TF, Pelzer S, Trautwein W, Pelzer DJ. Regulation and modulation of calcium channels in cardiac, skeletal, and smooth muscle cells. Physiol Rev. 1994;74:365–507. doi: 10.1152/physrev.1994.74.2.365. [DOI] [PubMed] [Google Scholar]
- 31.Richard S, Tiaho F, Charnet P, Nargeot J, Nerbonne JM. Two pathways for Ca2+ channel gating differentially modulated by physiological stimuli. Am J Physiol. 1990;258:H1872–H1881. doi: 10.1152/ajpheart.1990.258.6.H1872. [DOI] [PubMed] [Google Scholar]
- 32.Bean BP. Nitrendipine block of cardiac calcium channels: high-affinity binding to the inactivated state. Proc Natl Acad Sci U S A. 1984;81:6388–6392. doi: 10.1073/pnas.81.20.6388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yasui K, Palade P. Inhibitory action of SR33557 on L-type calcium current in single ventricular myocytes of rat. Br J Pharmacol. 1995;114:468–474. doi: 10.1111/j.1476-5381.1995.tb13250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waalas SI, Czernik AJ, Olstad OK, Sletten K, Walaas O. Protein kinase C and cyclic AMP-dependent protein kinase phosphorylate phospholemman, an insulin and adrenaline-regulated membrane phosphoprotein, at specific sites in the carboxy terminal domain. Biochem J. 1994;304(Pt 2):635–640. doi: 10.1042/bj3040635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shinoda T, Ogawa H, Cornelius F, Toyoshima C. Crystal structure of the sodium-potassium pump at 2.4 A resolution. Nature. 2009;459:446–450. doi: 10.1038/nature07939. [DOI] [PubMed] [Google Scholar]
- 36.Armoundas AA, Hobai IA, Tomaselli GF, Winslow RL, O'Rourke B. Role of sodium-calcium exchanger in modulating the action potential of ventricular myocytes from normal and failing hearts. Circ Res. 2003;93:46–53. doi: 10.1161/01.RES.0000080932.98903.D8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shattock MJ, Bers DM. Rat vs. rabbit ventricle: Ca flux and intracellular Na assessed by ion-selective microelectrodes. Am J Physiol Cell Physiol. 1989;256:C813–C822. doi: 10.1152/ajpcell.1989.256.4.C813. [DOI] [PubMed] [Google Scholar]
- 38.Fuller W, Howie J, McLatchie L, Weber R, Hastie CJ, Burness K, et al. Fxyd1 phosphorylation in vitro and in adult rat cardiac myocytes: Threonine 69 is a novel substrate for protein kinase C. Am J Physiol Cell Physiol. 2009;296:C1346–C1355. doi: 10.1152/ajpcell.00523.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rembold CM, Ripley ML, Meeks MK, Geddis LM, Kutchai HC, Marassi FM, et al. Serine68 phospholemman phosphorylation during forskolin-induced wwine carotid artery relaxation. J Vasc Res. 2005;42:483–491. doi: 10.1159/000088102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang XQ, Moorman JR, Ahlers BA, Carl LL, Lake DE, Song J, et al. Phospholemman overexpression inhibits Na+-K+-ATPase in adult rat cardiac myocytes: Relevance to decreased Na+ pump activity in postinfarction myocytes. J Appl Physiol. 2006;100:212–220. doi: 10.1152/japplphysiol.00757.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Silverman BD, Fuller W, Eaton P, Deng J, Moorman JR, Cheung JY, et al. Serine68 phosphorylation of phospholemman: acute isoform-specific activation of cardiac Na/K ATPase. Cardiovasc Res. 2005;65:93–103. doi: 10.1016/j.cardiores.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 42.Cheung JY, Zhang XQ, Song J, Gao E, Rabinowitz J, Chan TO, et al. Phospholemman: A novel cardiac stress protein. Clinical Translational Science. 2010;3:189–196. doi: 10.1111/j.1752-8062.2010.00213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mirza MA, Lane S, Yang Z, Karaoli T, Akosah K, Hossack J, et al. Phospholemman deficiency in postinfarct hearts: enhanced contractility but increased mortality. Clinical and translational science. 2012;5:235–242. doi: 10.1111/j.1752-8062.2012.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]