Abstract
Background
Endovascular reperfusion techniques are a promising intervention for acute ischemic stroke (AIS). Prior studies have identified markers of initial injury (arrival NIH stroke scale (NIHSS) or infarct volume) as predictive of outcome after these procedures. We sought to define the role of collateral flow at the time of presentation in determining the extent of initial ischemic injury and its influence on final outcome.
Methods
Demographic, clinical, laboratory, and radiographic data were prospectively collected on a consecutive cohort of patients who received endovascular therapy for acute cerebral ischemia at a single tertiary referral center from September 2004 to August 2010.
Results
Higher collateral grade as assessed by the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) grading scheme on angiography at the time of presentation was associated with improved reperfusion rates after endovascular intervention, decreased post-procedural hemorrhage, smaller infarcts on presentation and discharge, as well as improved neurological function on arrival to the hospital, discharge, and 90 days later. Patients matched by vessel occlusion, age, and time of onset demonstrated smaller strokes on presentation and better functional and radiographic outcome if found to have superior collateral flow. In multivariate analysis, lower collateral grade independently predicted higher NIHSS on arrival.
Conclusions
Improved collateral flow in patients with AIS undergoing endovascular therapy was associated with improved radiographic and clinical outcomes. Independent of age, vessel occlusion and time, in patients with comparable ischemic burdens, changes in collateral grade alone led to significant differences in initial stroke severity as well as ultimate clinical outcome.
INTRODUCTION
Endovascular therapy (ET) is a promising intervention for acute ischemic stroke (AIS). After three recent studies failed to demonstrate any benefit for these procedures over medical therapy, however, there has been increased scrutiny on methods of identifying patients likely to benefit from ET.1–3 Two features that have been focused upon and shown to play a role in influencing ultimate clinical outcome include time from symptom onset to recanalization as well as initial stroke severity at presentation in the form of the NIH stroke scale (NIHSS) or infarct volume on imaging.4,5
What then determines the initial stroke severity? It is not uncommon to encounter patients of comparable age, intracranial occlusion, and time from symptom onset with dramatically different cerebral injuries upon arrival to the hospital. One physiologic feature that likely plays a role in the varied presentations of these patients is the status of collaterals at the time of the vessel occlusion. The presence of adequate collateral flow has been shown to have a powerful effect on patient outcomes, and has been associated with decreased ischemia on CT and MRI, reduced hemorrhagic conversion, improved recanalization rates, and improved clinical outcomes.6–13 Methods of collateral assessments in these studies included conventional angiography, MRI, and CT angiography (CTA) evaluated as source, maximal intensity projection, and multiplanar reconstructed images.6,12,14,15
While the association of robust collaterals and improved outcomes in AIS has been made clear, a direct relationship between the two has not been established. These prior studies have demonstrated that collateral flow is also associated with reduced initial infarct volume and NIHSS, markers that have been independently shown to lead to good clinical outcome. Thus it is possible that improved collaterals could merely serve as a marker of reduced initial injury, and have no causative role in determining outcome. To address this issue, we sought to provide a single comprehensive view on the influence of collaterals on multiple outcome measures after AIS in an endovascular treatment cohort using the gold standard methodology for their assessment, cerebral angiography, and a single grading metric. We hypothesize that collateral grade in fact determines the degree of initial injury at the time of presentation and, as such, plays a pivotal role in determining the outcome. In thinking of the physiology of ischemic injury to the brain, the extent of infarction as well as the severity of clinical deficit is a function of the degree of reduction in cerebral blood flow, the areas of the brain involved, and the duration of ischemia.16 By matching patients with large vessel AIS by age, vessel occlusion, and time, we paired individuals with comparable ischemic burdens and determined whether changes in collateral grade alone led to significant differences in initial stroke severity as well as ultimate clinical outcome. We tested whether changes in collateral grade could independently lead to changes in the degree of initial injury, and thus directly modulate outcome.
METHODS
Demographic, clinical, laboratory, and radiographic data were prospectively collected on a consecutive cohort of patients who received ET (intra-arterial thrombolytic therapy or mechanical thrombectomy) for acute cerebral ischemia at a single tertiary referral center between September 2004 and January 2012. Patients were included in this study if they presented with symptoms of acute cerebral ischemia within the anterior circulation and underwent conventional angiography for consideration of ET.
The decision to proceed with ET at our institution is based on patient demographics, clinical history and examination, as well as imaging demonstration of large vessel occlusion that would be amenable to ET. Patients with occlusions that were felt by the interventionalist to be inaccessible or would confer significant risk were not included in this cohort. Patients with large infarct volumes on initial imaging are generally not offered ET. Conversely, patients with substantive clinical improvement after intravenous tissue plasminogen activator (tPA) are observed closely but not treated with ET without recurrence of symptoms or worsening that is shown on imaging to be due to continued ischemia. All patients with visualized large vessel occlusions without large infarcts on imaging are evaluated for possible ET, regardless of eligibility for intravenous tPA. Patients evaluated during this time period may have been enrolled in clinical trials of ET or non-ET interventions. As a result of these selection criteria, the resultant dataset reflects routine clinical practice while capturing advanced imaging data.
All patients underwent comprehensive diagnostic cerebral angiography, including injection of both internal carotid arteries and the dominant vertebral artery, with image acquisition into the late venous phase to assess collateral circulation from all possible sources. All cases had injections demonstrating the ipsilateral anterior cerebral artery and posterior cerebral artery. Angiographic collateral grade was evaluated with the American Society of Interventional and Therapeutic Neuroradiology/ Society of Interventional Radiology (ASITN/SIR) Collateral Flow Grading System on baseline angiography.17 This angiographic scale assigns patients to grade 0 (no collaterals visible to the ischemic site), 1 (slow collaterals to the periphery of the ischemic site with persistence of some of the defect), 2 (rapid collaterals to the periphery of ischemic site with persistence of some of the defect and to only a portion of the ischemic territory), 3 (collaterals with slow but complete angiographic blood flow of the ischemic bed by the late venous phase), and 4 (complete and rapid collateral blood flow to the vascular bed in the entire ischemic territory by retrograde perfusion). Collateral rating was performed by one author (DSL) with extensive experience in angiographic interpretation in acute stroke, in a retrospective manner, blinded to the clinical presentation and outcomes. Dichotomization was then performed by dividing into groups of 0–2 vs 3–4. Assessment of vascular recanalization was based on the Thrombolysis in Cerebral Infarction (TICI) scale.17 Hemorrhagic transformation was categorized as hemorrhagic infarctions or parenchymal hematomas as previously described.18
Routine clinical care included MRI before angiography therapy if not contraindicated. Follow-up imaging was then performed 24 h after arrival and prior to discharge. Diffusion-weighted imaging (DWI) and perfusion-weighted imaging (PWI) lesion volume measurements were performed by one of the authors blinded to the clinical information using a computer-assisted volumetric analysis program (Olea Medical, La Ciotat, France). Diffusion was measured at three values of b (b=0, 500, 1000 s/mm2), and average ADC maps were generated. DWI volumes were quantified from analysis of isotropic b1000 images and ADC maps with threshold of ADC <600. Final infarct measurements were gathered from the final MRI performed prior to discharge. PWI volumes were determined with Tmax of ≥2, 6, 8, and 10 s.19
Univariate comparisons between categorical variables were made using the Fisher exact test and the χ2 test, and between continuous variables using the Mann–Whitney U test. Matching algorithms were written in Matlab (R2010a, The Mathworks, Natick, Massachusetts, USA) to pair patients based on age, vessel occlusion, and time of onset by finding the control patient (collateral grade 0–2) that most closely matched each case patient (collateral grade 3–4). Comparisons between age-and time-matched cohorts were made using the Wilcoxon matched pairs test. Spearman correlation coefficient was used to analyze the association of collateral grade with the TICI recanalization. Multivariate analyses were performed using binomial logistic regression. All statistical analyses were performed using commercially available software (Prism 5.0a, GraphPad Software, La Jolla, California, USA and Matlab R2010a, The Mathworks). p<0.05 was considered statistically significant.
RESULTS
A total of 117 patients treated with ET for AIS were enrolled. This cohort is comparable in size to or larger than other recent studies on collaterals in ET.20–22 Baseline characteristics for the cohort are shown in table 1. Significantly fewer patients of white ethnicity were found to have grade 3–4 collaterals at the time of angiography. Patients with higher collateral grades presented with lower NIHSS. There were no significant differences in age, gender, past medical history, baseline function, vessel occlusion, or timing of arrival at the hospital, evaluation, and treatment.
Table 1.
Patient demographics
| Collateral grades 0–2 | Collateral grades 3–4 | p Value | |
|---|---|---|---|
| Number | 66 | 51 | |
| Age (mean±SD) | 68±17 | 65±17 | 0.51 |
| Female (%) | 45 (68%) | 27 (53%) | 0.13 |
| Ethnicity (%) | |||
| White | 57 (86%) | 32 (63%) | <0.01 |
| Black | 4 (6%) | 9 (18%) | 0.07 |
| Asian | 1 (2%) | 4 (8%) | 0.17 |
| History of hypertension | 42 (64%) | 29 (57%) | 0.57 |
| History of diabetes | 16 (24%) | 9 (18%) | 0.5 |
| History of HLD | 21 (32%) | 13 (26%) | 0.54 |
| Prior stroke or TIA | 12 (18%) | 4 (8%) | 0.06 |
| History of atrial fibrillation | 26 (39%) | 15 (29%) | 0.33 |
| Active smoking | 8 (12%) | 8 (16%) | 0.6 |
| Statin use | 12 (18%) | 12 (24%) | 0.82 |
| Baseline mRS | |||
| 0 | 63 (96%) | 48 (94%) | 1 |
| 1 | 1 (2%) | 1 (2%) | 1 |
| 2 | 2 (3%) | 2 (4%) | 1 |
| NIHSS | 19 [14–21] | 13 [8–19] | <0.01 |
| Target vessel | |||
| ICA | 22 (33%) | 13 (26%) | 0.42 |
| M1 | 37 (56%) | 29 (57%) | 1 |
| M2 or beyond | 7 (11%) | 9 (18%) | 0.29 |
| Left hemisphere | 35 (53%) | 30 (59%) | 0.58 |
| Mechanism | |||
| Cardioembolism | 33 (50%) | 26 (51%) | 1 |
| Large artery disease | 16 (24%) | 16 (31%) | 0.41 |
| Small artery disease | 0 (0%) | 1 (2%) | 0.44 |
| LKWT to ED arrival (min) | 228±186 | 210±205 | 0.54 |
| LKWT to DWI/PWI (min) | 299±183 | 260±232 | 0.28 |
| LKWT to groin puncture (min) | 364±178 | 340±235 | 0.72 |
All values expressed as median±SD or n (%) otherwise indicated.
DWI, diffusion weighted imaging; ED, emergency department; HLD, hyperlipidemia; ICA, internal carotid artery; mRS, modified Rankin scores; LKWT, last known well time; NIHSS, NIH stroke scale; PWI, perfusion weighted imaging; TIA, transient ischemic attack.
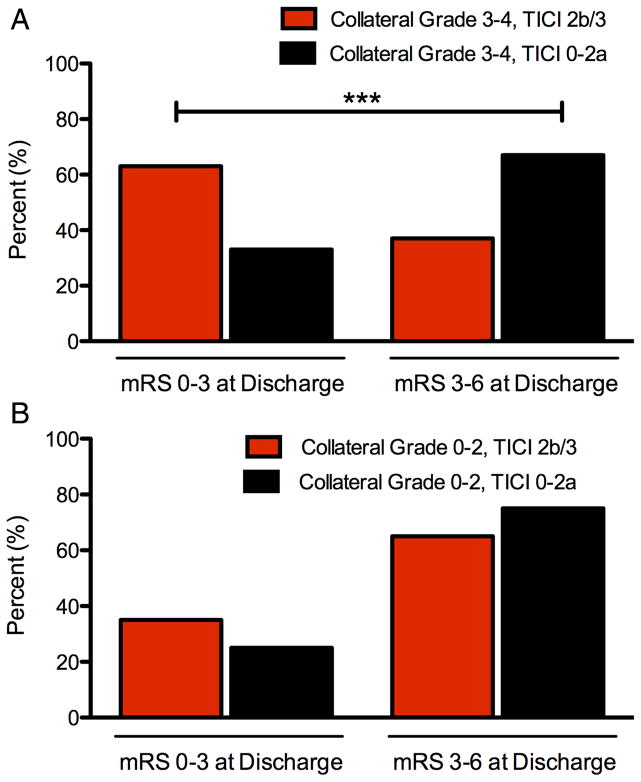
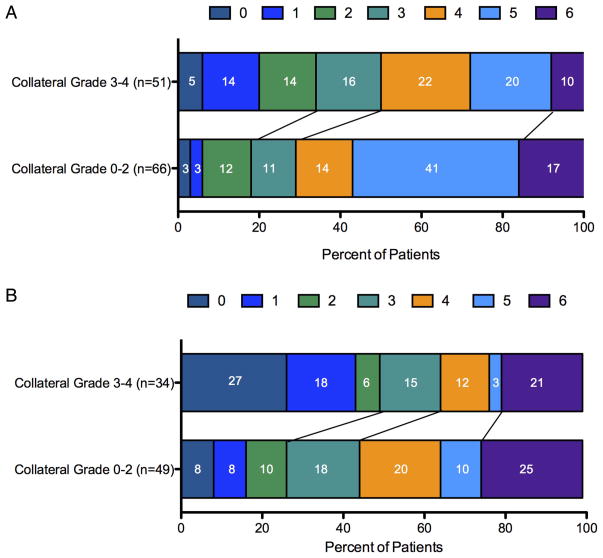
Treatment characteristics and outcomes are shown in table 2. Patients with more robust collaterals had smaller DWI lesions on arrival, with no significant difference in PWI volumes. Treatments modalities included intravenous tPA, intra-arterial tPA, and mechanical thrombectomy. The majority of patients had complete vessel occlusions (TICI 0) on arrival, and 41% and 53% achieved TICI 2b or 3 flow after the procedure in the groups with the lower 0–2 grade and higher 3–4 grade collateral groups, respectively. Improved collateral grade correlated positively with TICI reperfusion (r=0.23, p=0.01, Spearman correlation). Patients with higher grade 3–4 collaterals were more likely to have a good outcome of modified Rankin scores (mRS) 0–3 at discharge in the setting of successful reperfusion (TICI 2b/3) compared with poor reperfusion (TICI 0–2a) (63% vs 33%, TICI 2b/3 vs TICI 0–2a, p<0.001, Fisher exact test), as shown in figure 1. For patients with lower grade 0–2 collaterals, successful reperfusion (TICI 2b/3) compared with poor reperfusion (TICI 0–2a) did not result in a statistically significant difference in mRS at discharge. Rates of post-procedural hemorrhage were lower in the group with better collateral flow, with no significant differences between the timing of follow-up imaging. Final infarct DWI volumes were smaller and lengths of hospitalization were shorter for the group with higher collateral grade. Discharge and 90-day mRS were less in the group with higher collateral grade (figure 2).
Table 2.
Treatment characteristics and outcomes
| Collateral grades 0–2 | Collateral grades 3–4 | p Value | |
|---|---|---|---|
| Number | 66 | 51 | |
| Initial DWI volume (mL) | 30±40 | 10±13 | <0.01 |
| PWI volume (mL), s | |||
| 2 | 127±73 | 130±80 | 0.73 |
| 6 | 76±58 | 65±66 | 0.54 |
| 8 | 56±47 | 38±56 | 0.08 |
| 10 | 31±38 | 39±41 | 0.8 |
| PWI (8 s)/DWI ratio | 2.1±47 | 3.8±20 | 0.01 |
| Treatment modalities | 0.8 | ||
| Intravenous tPA | 22 (33%) | 21 (41%) | |
| Intra-arterial tPA | 9 (14%) | 7 (14%) | |
| Thrombectomy | 55 (83%) | 41 (80%) | |
| Pre-treatment TICI | 1 | ||
| 0 | 61 (92%) | 47 (92%) | |
| 1 | 5 (8%) | 4 (8%) | |
| Post-treatment TICI | 0.12 | ||
| 0 | 14 (21%) | 9 (18%) | |
| 1 | 2 (3%) | 1 (2%) | |
| 2a | 23 (35%) | 14 (27%) | |
| 2b | 27 (41%) | 22 (43%) | |
| 3 | 0 | 5 (10%) | |
| Any hemorrhage | 41 (62%) | 20 (39%) | 0.02 |
| Hemorrhage types | 0.02 | ||
| HI-1 | 5 (8%) | 4 (8%) | |
| HI-2 | 21 (32%) | 7 (14%) | |
| PH-1 | 8 (12%) | 1 (2%) | |
| PH-2 | 7 (11%) | 8 (16%) | |
| None | 25 (38%) | 31 (61%) | |
| PH-2 hemorrhage | 7 (11%) | 8 (16%) | 0.58 |
| Time to final follow-up imaging (days) | 4.5±2.0 | 4.3±2.2 | 0.44 |
| Infarct growth (mL) | 73±87 | 13±20 | <0.01 |
| Final infarct (mL) | 128±101 | 22±23 | <0.01 |
| mRS at discharge | 5±1.6 | 4±1.7 | <0.01 |
| Length of hospitalization (days) | 9±9.6 | 6±4.1 | <0.01 |
| mRS at 90 days | 4±1.9 | 2.5±2.3 | 0.03 |
| Missing to follow-up | 17 (28%) | 17 (33%) | 0.42 |
All continuous variables expressed as median±SD or n (%).
DWI, diffusion weighted imaging; HI, hemorrhagic infarction; mRS, modified Rankin scores; PH, parenchymal hematomas; PWI, perfusion weighted imaging; TICI, Thrombolysis in Cerebral Infarction; tPA, tissue plasminogen activator.
Figure 1.
Influence of dichotomized Thrombolysis in Cerebral Infarction (TICI) recanalization and collateral scores on outcome. (A) Effect of adequate (TICI 2b/3) versus poor (TICI 0–2a) reperfusion in patients with collateral grades 3–4 on outcomes as determined by modified Rankin scores (mRS) at discharge. (B) Effect of adequate (TICI 2b/3) versus poor (TICI 0–2a) reperfusion in patients with collateral grades 0–2 on outcomes as determined by mRS at discharge.
***p<0.001, Fisher exact test.
Figure 2.
Distribution of modified Rankin scores (mRS) by dichotomized collateral scores on presentation. (A) mRS at discharge for the cohorts of patients presenting with collateral grades 3–4 vs 0–2 (4±1.7 vs 5±1.6, p<0.01, Mann–Whitney U test). (B) mRS at 90 days for the cohorts of patients presenting with collateral grades 3–4 vs 0–2 (2.5±2.3 vs 4±1.9, p=0.03, Mann–Whitney U test). Values were available for a subset of the cohort, as indicated in parentheses. For both figures, numbers in white indicate the percentage of patients within each category.
We then sought to address whether collateral status predicted severity of stroke independent of age and last known well time. We selected a subset of patients from our cohort with proximal vessel occlusions (internal carotid artery (ICA) or proximal middle cerebral artery (M1)) and matched them pairwise for these two variables. As shown in table 3, in the setting of comparable vessel occlusions, age- and time-matched patients with higher collateral grade presented with lower NIHSS, had smaller stroke volumes on initial and final DWI, better mRS at time of discharge, and shorter length of stay in hospital.
Table 3.
Pairwise matched comparisons
| ICA or M1 occlusion, matched for age and LKWT | Pairs | p Value |
|---|---|---|
| Number of pairs | 34 | |
| Age difference (years) | 0±3.2 | |
| LKWT to ED arrival difference (min) | ±15.5 | |
| NIHSS (median±SD) | <0.001 | |
| Collateral grade 0–2 | 20±5.5 | |
| Collateral grade 3–4 | 13±6.8 | |
| DWI volume on presentation (mL) | <0.001 | |
| Collateral grade 0–2 | 37±49 | |
| Collateral grade 3–4 | 10±14 | |
| LKWT to groin puncture (min) | <0.05 | |
| Collateral grade 0–2 | 325±81 | |
| Collateral grade 3–4 | 364±178 | |
| Final DWI volume (mL) | <0.001 | |
| Collateral grade 0–2 | 112±114 | |
| Collateral grade 3–4 | 19±25 | |
| mRS on discharge | <0.01 | |
| Collateral grade 0–2 | 5±1.0 | |
| Collateral grade 3–4 | 4±1.7 | |
| Length of hospitalization (days) | <0.05 | |
| Collateral grade 0–2 | 8±11.5 | |
| Collateral grade 3–4 | 6±4.2 |
All values expressed as median±SD.
DWI, diffusion weighted imaging; ED, emergency department; ICA, internal carotid artery; mRS, modified Rankin scores; LKWT, last known well time; NIHSS, NIH stroke scale.
We then explored the relationship of collateral status with initial stroke severity in a multivariate analysis, as shown in table 4. Of note, we chose NIHSS 17 as our dichotomization point in our binomial logistic regression as this was the median value of our cohort. Collateral grade 0–2 and age >80 were significantly associated with worse initial stroke severity. There was a trend a towards higher likelihood of NIHSS ≥18 with ICA occlusions versus all others.
Table 4.
Multivariate analysis of variables leading to presentation NIH stroke scale (NIHSS) ≥18
| OR (CI) | p Value | |
|---|---|---|
| Age >80 | 5.48 (2.01 to 14.96) | <0.001 |
| Male gender | 1.32 (0.54 to 3.24) | 0.54 |
| ICA occlusion | 2.91 (0.91 to 9.31) | 0.07 |
| Time (LKWT to ED in min) | 0.97 (0.57 to 1.64) | 0.91 |
| Collateral grade 0–2 | 4.37 (1.75 to 10.95) | 0.002 |
ED, emergency department; ICA, internal carotid artery; LKWT, last known well time.
DISCUSSION
In this cohort of patients with AIS treated with ET, higher collateral grade as assessed by the ASITN/SIR grading scheme on angiography at the time of presentation was associated with improved reperfusion rates after endovascular intervention, decreased post-procedural hemorrhage, smaller infarcts on presentation and discharge, as well as improved neurological function on arrival to the hospital, discharge, and 90 days later. Hospital stays were also significantly briefer. In order to address the issue of the direct influence of collateralization on initial stroke severity and outcome, we matched patients based on vessel occlusion, time from last known well to presentation, and age. These factors are those used most consistently in models of predicting clinical outcome in AIS.5,23–26 It is worth noting that, while these models also include measures of initial stroke severity (NIHSS or initial DWI volume), we did not include these features in the matching algorithm as, in this paradigm, we used these factors as outcome measures, as measures of the extent of the patient’s injury on arrival. We found that, among these matched patients, superior collaterals were associated with smaller strokes at presentation and improved outcomes. This finding was corroborated in our multivariate analysis as well. Thus, for a given arterial occlusion over time, improved collaterals at the time of imaging led to smaller infarcts. In a multivariate analysis, lower collateral grade increased the likelihood of increased stroke severity independent of age, time of onset, and vessel occlusion. By driving a reduction in initial stroke severity at presentation, improved collateral flow has a direct role in the final clinical outcome.
Adequacy of reperfusion is another key factor in determining outcome after ET. Our findings continue to support the need for complete recanalization as we found that, even in the setting of robust collateral flow, higher grade TICI reperfusion is associated with improved rates of good outcome. On the other hand, we also found that patients with poor collaterals could have a good outcome in the setting of adequate reperfusion. Besides adequacy of reperfusion, the other variable that can be addressed by the physician rendering treatment is time. Time to reperfusion has emerged as a key variable in both intravenous lytic therapy and ET, but it is worth noting that not all patients who are treated rapidly do well.5,26 Conversely, not all patients who are treated at later time points do poorly. Perhaps the key variable that determines an individual’s vulnerability to time is the quality of collateral flow to the territories at risk. We found that patients matched by age, vessel occlusion, and time of symptom onset had improved outcomes with improved collateral grades in spite of longer times from last known well to groin puncture. Strict cutoffs for ET based on time alone are unlikely to capture the varied physiology that is a function of each individual’s collateral status.
The relationship between PWI volume, PWI/DWI mismatch, and collateral grade is not clear. In our study we did not note an association in total volume of PWI abnormality and collateral status consistent with other studies, and the elevations in PWI/ DWI mismatch ratios in our patients with robust collaterals is probably due to their significantly reduced DWI volumes.10 On the other hand, in a smaller cohort also using MRI perfusion and angiographic collateral grading, a linear relationship between collateral grade and PWI volume was seen, with lower collateral scores associated with larger PWI volumes.22 Other smaller cohorts have shown non-statistically significant trends towards a relationship between the two.27 In our data there was a trend towards larger PWI volumes defined by Tmax ≥8 and collateral status, and so it is possible that larger cohorts will be able to define this relationship more accurately.
Limitations to this study include its retrospective nature and, because of the reliance on angiography, a selection bias in only choosing patients considered for ET. Patients without large vessel occlusions, with significant brain injury on imaging, or with delayed presentations from symptom onset would likely have been excluded. Further, our finding that higher collateral grades were associated with improved TICI reperfusion scores may have been confounded by more aggressive recanalization attempts in the setting of well-visualized collateral flow. In addition, angiography is an invasive technique that may not be indicated in many presentations of AIS. In fact, an assessment of collateral flow prior to angiography may be helpful in determining whether angiography and ET are indicated. Non-invasive measurements of collateral flow using CTA have been shown to correlate with outcome in AIS and also to correlate with initial DWI lesion.7,28 However, because CTA provides a structural assessment and does not measure blood flow, collateral grades can often be elevated when compared with angiography. In addition, as the field of ET for AIS advances, time from symptom onset to reperfusion is emerging as a key target. One study has noted a 12% lower probability of good outcome for every 30 minute delay in reperfusion.5 As a result, there may be less justification for obtaining contralateral injections prior to the initiation of the recanalization portion of the procedure.
To date, reperfusion interventions comprise the only acute treatment modalities for patients presenting with ischemic stroke. In spite of almost 20 years of experience, use of intravenous tPA remains low nationwide, with estimates of 1–5% of stroke patients receiving this therapy.29,30 Substantial effort has been placed into identifying additional patients who may benefit from thrombolytic or mechanical revascularization techniques. In this paper we show that patients with adequate collateral flow can present with decreased stroke severity and, in this population, adequate reperfusion with ET increases the likelihood of a good outcome. Assessments of collateral status at the time of presentation may expand the population of patients in whom reperfusion is safe, effective, and ultimately leads to an improvement in functional outcomes.
Acknowledgments
Funding Funding for this manuscript includes grant support from NIH/NINDS K24NS072272, R13NS082049.
Footnotes
Contributors SAS was responsible for substantial contributions to the conception and design of the work, drafting and critically revising it, and its final approval. He agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. DSL was responsible for the conception of the work, revising the article, and for its final approval. He agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SS, LKA, DK, NRG, RJ, ST, GRD, JLS and FV were responsible for revising the article and for its final approval. They agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval This study was approved by the Institutional Review Board of the institution and was conducted in compliance with the Health Information Portability and Accountability Act.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The data discussed in this article are taken from our institutional cohort and are available to collaborators with IRB and HIPAA approval.
Competing interests DSL receives consulting fees from Stryker, Covidien, and Zoll (modest). ST receives consulting fees from Penumbra, Covidien, Stryker, and Reverse Medical. RJ receives consulting fees from Covidien and Stryker. GRD has consulting agreements with Asahi Medical and Sequent Medical. He is also a Proctor for the Pipeline device (Covidien). The University of California, Regents receive funding for JLS’s services as a scientific consultant regarding trial design and conduct to Covidien, CoAxia, Stryker, BrainsGate, Genervon, and Grifols. JLS has served as an unpaid site investigator in multicenter trials run by Lundbeck and Covidien for which the UC Regents received payments on the basis of clinical trial contracts for the number of subjects enrolled. The University of California has patent rights in retrieval devices for stroke.
References
- 1.Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368:914–23. doi: 10.1056/NEJMoa1212793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368:893–903. doi: 10.1056/NEJMoa1214300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ciccone A, Valvassori L, Nichelatti M, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368:904–13. doi: 10.1056/NEJMoa1213701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoo AJ, Verduzco LA, Schaefer PW, et al. MRI-based selection for intra-arterial stroke therapy: value of pretreatment diffusion-weighted imaging lesion volume in selecting patients with acute stroke who will benefit from early recanalization. Stroke. 2009;40:2046–54. doi: 10.1161/STROKEAHA.108.541656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khatri P, Abruzzo T, Yeatts SD, et al. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009;73:1066–72. doi: 10.1212/WNL.0b013e3181b9c847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Menon BK, Smith EE, Modi J, et al. Regional leptomeningeal score on CT angiography predicts clinical and imaging outcomes in patients with acute anterior circulation occlusions. AJNR Am J Neuroradiol. 2011;32:1640–5. doi: 10.3174/ajnr.A2564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lima FO, Furie KL, Silva GS, et al. The pattern of leptomeningeal collaterals on CT angiography is a strong predictor of long-term functional outcome in stroke patients with large vessel intracranial occlusion. Stroke. 2010;41:2316–22. doi: 10.1161/STROKEAHA.110.592303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kucinski T, Koch C, Eckert B, et al. Collateral circulation is an independent radiological predictor of outcome after thrombolysis in acute ischaemic stroke. Neuroradiology. 2003;45:11–18. doi: 10.1007/s00234-002-0881-0. [DOI] [PubMed] [Google Scholar]
- 9.Mohammad YM, Christoforidis GA, Bourekas EC, et al. Qureshi grading scheme predicts subsequent volume of brain infarction following intra-arterial thrombolysis in patients with acute anterior circulation ischemic stroke. J Neuroimaging. 2008;18:262–7. doi: 10.1111/j.1552-6569.2007.00233.x. [DOI] [PubMed] [Google Scholar]
- 10.Bang OY, Saver JL, Buck BH, et al. Impact of collateral flow on tissue fate in acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2008;79:625–9. doi: 10.1136/jnnp.2007.132100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Souza LCS, Yoo AJ, Chaudhry ZA, et al. Malignant CTA collateral profile is highly specific for large admission DWI infarct core and poor outcome in acute stroke. AJNR Am J Neuroradiol. 2012;33:1331–6. doi: 10.3174/ajnr.A2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bang OY, Saver JL, Kim SJ, et al. Collateral flow averts hemorrhagic transformation after endovascular therapy for acute ischemic stroke. Stroke. 2011;42:2235–9. doi: 10.1161/STROKEAHA.110.604603. [DOI] [PubMed] [Google Scholar]
- 13.Bang OY, Saver JL, Kim SJ, et al. Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke. 2011;42:693–9. doi: 10.1161/STROKEAHA.110.595256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Camargo ECS, Furie KL, Singhal AB, et al. Acute brain infarct: detection and delineation with CT angiographic source images versus nonenhanced CT scans. Radiology. 2007;244:541–8. doi: 10.1148/radiol.2442061028. [DOI] [PubMed] [Google Scholar]
- 15.Lee KY, Latour LL, Luby M, et al. Distal hyperintense vessels on FLAIR: an MRI marker for collateral circulation in acute stroke? Neurology. 2009;72:1134–9. doi: 10.1212/01.wnl.0000345360.80382.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donnan GA, Davis SM, Parsons MW, et al. How to make better use of thrombolytic therapy in acute ischemic stroke. Nat Rev Neurol. 2011;7:400–9. doi: 10.1038/nrneurol.2011.89. [DOI] [PubMed] [Google Scholar]
- 17.Higashida RT, Furlan AJ, Roberts H, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003;34:e109–37. doi: 10.1161/01.STR.0000082721.62796.09. [DOI] [PubMed] [Google Scholar]
- 18.Wolpert SM, Bruckmann H, Greenlee R, et al. Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. The rt-PA Acute Stroke Study Group. AJNR Am J Neuroradiol. 1993;14:3–13. [PMC free article] [PubMed] [Google Scholar]
- 19.Olivot J-M, Mlynash M, Thijs VN, et al. Optimal Tmax threshold for predicting penumbral tissue in acute stroke. Stroke. 2009;40:469–75. doi: 10.1161/STROKEAHA.108.526954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liebeskind DS, Jahan R, Nogueira RG, et al. Impact of collaterals on successful revascularization in Solitaire FR with the intention for thrombectomy. Stroke. 2014;45:2036–40. doi: 10.1161/STROKEAHA.114.004781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seeta Ramaiah S, Churilov L, Mitchell P, et al. The impact of arterial collateralization on outcome after intra-arterial therapy for acute ischemic stroke. AJNR Am J Neuroradiol. 2014;35:667–72. doi: 10.3174/ajnr.A3862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marks MP, Lansberg MG, Mlynash M, et al. Effect of collateral blood flow on patients undergoing endovascular therapy for acute ischemic stroke. Stroke. 2014;45:1035–9. doi: 10.1161/STROKEAHA.113.004085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flint AC, Faigeles BS, Cullen SP, et al. THRIVE score predicts ischemic stroke outcomes and thrombolytic hemorrhage risk in VISTA. Stroke. 2013;44:3365–9. doi: 10.1161/STROKEAHA.113.002794. [DOI] [PubMed] [Google Scholar]
- 24.Saposnik G, Guzik AK, Reeves M, et al. Stroke prognostication using age and NIH stroke scale: SPAN-100. Neurology. 2012;80:21–8. doi: 10.1212/WNL.0b013e31827b1ace. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osaki M, Miyashita F, Koga M, et al. Simple clinical predictors of stroke outcome based on National Institutes of Health Stroke Scale score during 1-h recombinant tissue-type plasminogen activator infusion. Eur J Neurol. 2014;21:411–18. doi: 10.1111/ene.12294. [DOI] [PubMed] [Google Scholar]
- 26.Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. 2013;309:2480–8. doi: 10.1001/jama.2013.6959. [DOI] [PubMed] [Google Scholar]
- 27.Jung S, Gilgen M, Slotboom J, et al. Factors that determine penumbral tissue loss in acute ischaemic stroke. Brain. 2013;136(Pt 12):3554–60. doi: 10.1093/brain/awt246. [DOI] [PubMed] [Google Scholar]
- 28.Schramm P, Schellinger PD, Fiebach JB, et al. Comparison of CT and CT angiography source images with diffusion-weighted imaging in patients with acute stroke within 6 hours after onset. Stroke. 2002;33:2426–32. doi: 10.1161/01.str.0000032244.03134.37. [DOI] [PubMed] [Google Scholar]
- 29.Prabhakaran S, O’Neill K, Stein-Spencer L, et al. Prehospital triage to primary stroke centers and rate of stroke thrombolysis. JAMA Neurol. 2013;70:1126–32. doi: 10.1001/jamaneurol.2013.293. [DOI] [PubMed] [Google Scholar]
- 30.Kleindorfer D, Lindsell CJ, Brass L, et al. National US estimates of recombinant tissue plasminogen activator use: ICD-9 codes substantially underestimate. Stroke. 2008;39:924–8. doi: 10.1161/STROKEAHA.107.490375. [DOI] [PubMed] [Google Scholar]