Abstract
Background:
Rhabdomyolysis is a clinical and biochemical syndrome, which is observed in some patients with acute chemical and/or pharmaceutical poisonings. We aimed to investigate rhabdomyolysis in patients with acute poisonings due to different chemicals, natural toxins or drug overdose.
Materials and Methods:
Following approval of the University medical research committee and obtaining informed consents from the patients or their relatives, all patients with acute poisonings who were treated between March 2009 and February 2010 in the Toxicologic Ward of Imam Reza Hospital and had serum creatine phosphokinase (CPK) above 975 IU/L (as a definition for rhabdomyolysis) were studied.
Results:
Of 3555 hospitalized poisoned patients, 114 patients had rhabdomyolysis with CPK of 5996 ± 892 IU/L (mean ± standard error). The most common intoxication to induce the rhabdomyolysis was opioid overdose (28%). Acute renal failure (ARF) was diagnosed in 11 (8.7%) patients. There was a linear correlation between CPK and creatinine (P < 0.001), which in turn had a significant correlation with death (P < 0.05).
Conclusion:
Patients with acute poisoning were at risk of rhabdomyolysis. Acute opioid poisoning was the most common cause of toxic rhabdomyolysis in the intoxicated patients, and ARF was the main complication.
Keywords: Acute poisoning, acute renal failure, creatine kinase, creatinine, intoxication, rhabdomyolysis
INTRODUCTION
Rhabdomyolysis was first described in the victims of crush injury during bombing raids of World War II (1940-1941) in London, England.[1]
Rhabdomyolysis is a syndrome caused by injury to skeletal muscles and with leakage of potentially toxic cellular contents into the systemic circulation. Myoglobinuria is the most significant consequence of the muscle breakdown and is reported to cause acute renal failure (ARF) in 15-33% of cases.[2] Rhabdomyolysis is the cause of 5-25% of all cases of ARF.[3,4] The overall mortality rate for patients with rhabdomyolysis is approximately 10%. It is higher in males than in females.[5,6] The triad of muscle weakness, myalgia, and dark urine indicate rhabdomyolysis. However, all 3 symptoms are rarely observed simultaneously.
Detection of myoglobinuria is the gold standard test for diagnosis of rhabdomyolysis. However, because of rapid clearance of myoglobin, it does not have high sensitivity.[5,7] Serum creatine kinase (CK) is the most practical diagnostic test for rhabdomyolysis. A level more than five-fold or greater increase in CK (above 975 U/L) in the absence of stroke or myocardial infarction should be considered as rhabdomyolysis.[2,3,8,9]
Complications of rhabdomyolysis include hypovolemia, hyperkalemia, metabolic acidosis, disseminated intravascular coagulation and ARF.[4] Electrolyte abnormalities are prominent features of rhabdomyolysis. The hyperkalemia may be due to both muscle injury and renal failure. This abnormality may cause life-threatening cardiac arrhythmias, which must be treated immediately.[10]
The etiologies of rhabdomyolysis may be divided into traumatic, toxicologic, environmental, metabolic, infectious, immunologic, and inherited disorders. More recently, as noted in one published series, drugs and alcohol have become frequent causative agents in up to 81% of cases with rhabdomyolysis.[11] Drug-induced rhabdomyolysis can be divided into primary or secondary myotoxic effects.[12] Primary toxic-induced rhabdomyolysis is caused by a direct insult on the skeletal myocyte function and integrity. Secondary effects of toxins are due to predisposing risk factors such as local muscle compression in coma, prolonged seizures, trauma, and metabolic abnormalities.[11]
In the present study, we aimed to investigate rhabdomyolysis in a large population of hospitalized patients with acute poisonings.
MATERIALS AND METHODS
The investigation was a prospective cross-sectional study carried out in the Medical Toxicology Center of Mashhad University of Medical Sciences, located in Imam-Reza Hospital of Mashhad which is one of the largest specialized referral Poisons Treatment Centers in the world covering more than 6 million populations. The center consists of a toxicologic emergency clinic with 8 beds, a ward for adults with 30 beds, a ward for poisoned children with 10 beds, a toxicologic Intensive Care Unit (ICU) for adults with 6 beds, a shared ICU for poisoned children with 18 beds and a 24 h toxicology laboratory.
Serum creatine phosphokinase (CPK) was first measured on hospital admission and afterwards on a daily basis. The diagnosis of rhabdomyolysis was defined as serum CPK values >5 times the upper limit of normal (195 IU/L), which is 975.[13,14] The patients included in the study during the hospitalization. For all patients, complications of rhabdomyolysis including ARF and death during hospitalization were recorded. ARF was defined as an increase in serum creatinine above 2 mg/dL that had no response to initial hydration.[15] Patients with recent evidence of myocardial infarction, stroke or cardiopulmonary resuscitation were excluded.
In addition to specific and intensive care therapy, 6 L of half-saline solution containing 50 mEq sodium bicarbonate per liter were infused for hydration and treatment of rhabdomyolysis.
Diagnosis of poisonings was made based on the history of poisons and drug taken as well as clinical findings. Poisons were confirmed by the relevant toxicological analyses in most cases. Opioids (morphine, tramadol, and methadone), benzodiazepines, tricyclic antidepressants, and amphetamines were identified by Immunochromatography (First Sign, EL Monte, USA). Phenotiazines were qualitatively assessed by a color test (FPN reagent, USA). Methanol levels were analyzed by Gas Chromatograph (Varian CP-3800, USA). Carbon monoxide and red blood cell cholinesterase were detected by UV-vis Spectrophtometry (550 standard error [SE] Perkin-Elmer, USA). Percents of pseudocholinesterase enzyme were determined by titrometry and acetyle cholinesterase activity by modified Ellman method. Gabapentin and beta-blockers were measured by high-performance liquid chromatography (KNAUER, Platin Blue, Germany) in the toxicology laboratory of the center.
Data are expressed as mean values ± standard deviation. Chi-square and Pearson correlation tests were undertaken for statistical analysis using Statistical Package for Social Sciences (SPSS Inc. Chicago, Illinois, USA) at a significant level of P < 0.05.
RESULTS
During 12 months (March 21, 2009- to March 21, 2010), around 12,000 patients were referred to this center, of which 3555 were admitted to the poisoning ward, of which 114 cases revealed rhabdomyolysis.
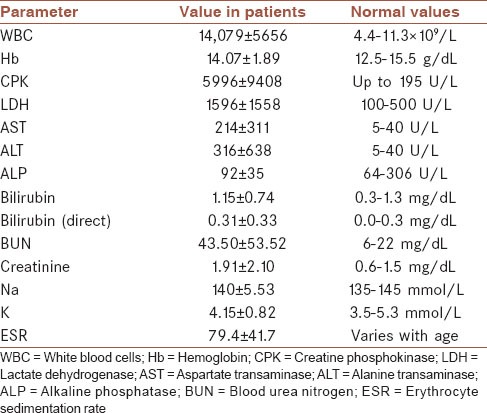
Of 114 studied patients, 82 and 32 were men and women, respectively. Their ages ranged from 15 to 85 (32 ± 14) years. Most patients were in the age group of 20-30 years old (48%). Thirteen patients (11%) had an underlying disease at the time of hospitalization. The most common underlying disease was a psychological disorder (5.5%). Only two patients (1.8%) had a history of trauma, and 11 patients (9.6%) had a seizure. Hematological and biochemical tests results are summarized in Table 1. The levels of CK (mean ± SE) had a wide range from 980 to 66,500 IU/L (5996 ± 892 IU/L).
Table 1.
Hematological and biochemical tests results of 114 poisoned patients with rhabdomyolysis
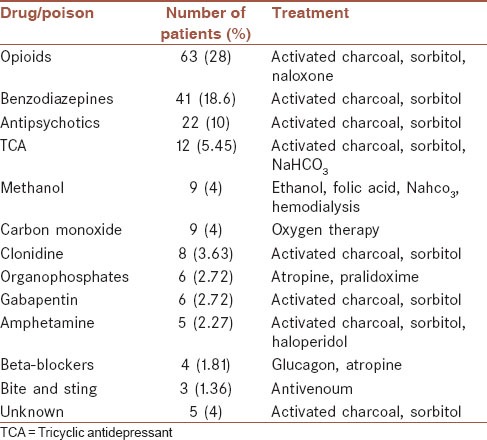
The most common acute poisonings associated with rhabdomyolysis included: Opioids (31%), benzodiazepines (18.6%), and antipsychotics (10%). In five patients (4.6%), the cause of acute poisonings was not diagnosed. ARF was present in 11 (8.7%) patients. Five patients with methanol poisoning went under hemodialysis, and nine patients succumbed to poisoning.
The most common drugs that induced ARF in the patients were opioids. There was a significant positive linear correlation between CPK and creatinine (P < 0.001, r = 0.313) as shown in Figure 1. The average serum level of CK in patients with ARF was 17099.82 (± 22743) that showed a significant difference compared with patients without ARF (P < 0.05). Moreover, ARF had a significant positive correlation with death (P < 0.05).
Figure 1.
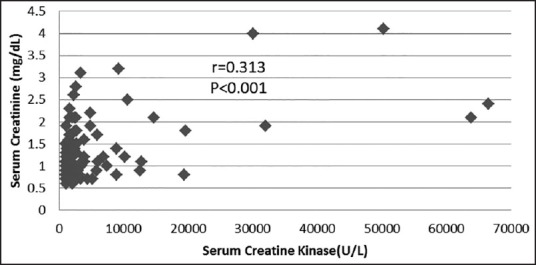
Correlation between peak serum creatine kinase (IU/L) and serum creatinine (mg/dL)
The causes of acute poisonings associated with rhabdomyolysis are listed in Table 2. In all acute poisonings, men were affected more frequently than women.
Table 2.
Causes of acute poisonings associated with rhabdomyolysis and the principle treatment in 114 patients
DISCUSSION
The most common causes of rhabdomyolysis in this study were overdoses of opioid, benzodiazepines, and antipsychotics. All patients received sodium bicarbonate for management of rhabdomyolysis with or without metabolic acidosis. Due to controversies on the effects of mannitol,[13] we did not use it for the treatment of rhabdomyolysis.
We found 12 types of acute poisonings associated with rhabdomyolysis. Few large population studies on rhabdomyolysis have been reported thus far.[2,5,16,17] Comparison between the present study and previous reports in terms of case numbers, sex, age, ranges of CK and illicit drugs involvement are summarized in Table 3. In the majority of the studies, ARF and the biochemical changes were the main concern. The different types in our study can explain the larger number of toxic etiologies that have been considered. Similar to our investigation, three previous studies have shown illegal drugs abuse as the most frequent causes of rhabdomyolysis.[5,18,19] This result is also confirmed by a recent publication on the annual incidence of ARF due to rhabdomyolysis associated with drug abuse, which showed a 3-fold increase in the period 1987-1997 in an urban area of Scotland.[20]
Table 3.
Comparison of data between the present study and previous reports of rhabdomyolysis
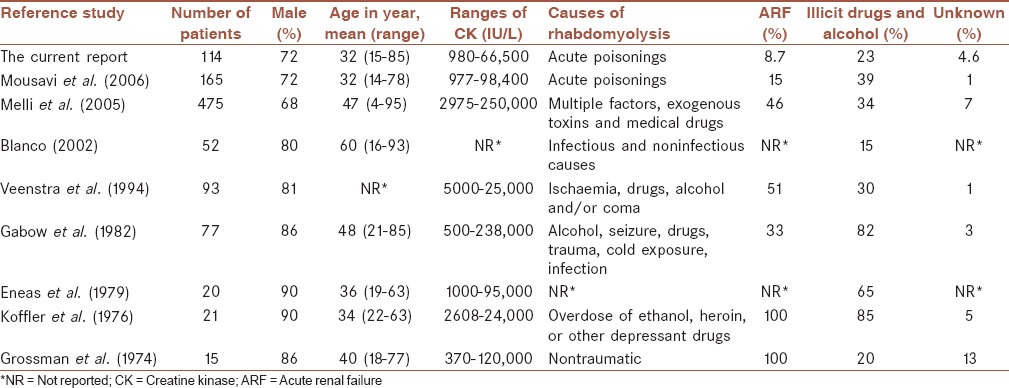
The demographic distribution in our study is generally similar to those previously reported. Men are predominantly affected, and the mean age of patients is also similar [Table 3]. Differences in the reported studies may be due to dissimilarities in the inclusion and exclusion criteria. The current study differs from previous studies in term of the association of rhabdomyolysis with ARF. This study includes patients who developed rhabdomyolysis with and without ARF, while previous series were usually collections of patients with rhabdomyolysis-induced ARF.[17,19,21] Another novel finding in our study was antipsychotics as the commonest nonillicit drug-induced rhabdomyolysis.
Acute renal failure, the most serious complication of rhabdomyolysis, was developed in 15% of patients, which is similar to what have been previously reported (15-33%) in general reviews.[5,9] The exact mechanism(s) of ARF in rhabdomyolysis are not completely obvious. Some of the proposed mechanisms include mechanical injury to the tubules caused by myoglobin precipitation, direct toxic effect of free chelatable iron on tubules, and hypovulemia.[13,22] It has been shown that the amount of myoglobin released in the blood correlates with serum CK and consequently to ARF.[23] Therefore, higher levels of CK should be present in the setting of ARF.[24] Indeed, our findings of the highly significant positive correlation between serum creatinine values (as a marker of renal function) and CK values are compatible with this explanation. However, further studies are required to find out the clear mechanism of rhabdomyolysis.
LIMITATIONS
Since some of our patients were unconscious on admission, obtaining a reliable history of symptoms and assessment of signs was very difficult and thus the causes of acute poisonings remained unknown in 5 of the patients.
Nine patients needed dialysis due to the severity of intoxications and not because of the ARF being induced by rhabdomyolysis. They received hemodialysis before or during ARF. However, differentiation between the two conditions was sometimes difficult. For instance, in five patients with severe acute methanol poisoning and raised creatinine levels, hemodialysis was performed due to the clinical severity of the poisoning and high levels of blood methanol, but all of them expired. In this patients, the discrimination between methanol intoxication and renal failure complications as the etiology of death was unknown.
CONCLUSIONS
Rhabdomyolysis was found as a common complication in severe acute poisonings. The most common poisons were opioids, benzodiazepines, and antipsychotics. ARF was a frequent complication of rhabdomyolysis, which was developed in a similar frequency as reported previously.
AUTHOR'S CONTRIBUTION
SM contributed in the conception of the work and conducting the study, prepared the first draft, approved of the final version of the manuscript, and agreed for all aspects of the work. MV contributed in the conception of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. AM collected the data, approval of the final version of the manuscript, and agreed for all aspects of the work. MV looked after the patients, cooperated for data collection, approval of the final version of the manuscript, and agreed for all aspects of the work. MS cooperated for data collection, approval of the final version of the manuscript, and agreed for all aspects of the work. RA performed patients’ clinical management, analyzing the data, and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MM confirmed the conception of the work and supervised the study, approved of the final version of the manuscript, and agreed for all aspects of the work.
ACKNOWLEDGEMENTS
The authors would like to thank the Vise-Presidency for Research of Mashhad University of Medical Sciences for financial support of the project.
Footnotes
Source of Support: Vise-Presidency for Research of Mashhad University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Bywaters EG, Beall D. Crush injuries with impairment of renal function. Br Med J. 1941;1:427–32. doi: 10.1136/bmj.1.4185.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melli G, Chaudhry V, Cornblath DR. Rhabdomyolysis: An evaluation of 475 hospitalized patients. Medicine (Baltimore) 2005;84:377–85. doi: 10.1097/01.md.0000188565.48918.41. [DOI] [PubMed] [Google Scholar]
- 3.Scharman EJ, Troutman WG. Prevention of kidney injury following rhabdomyolysis: A systematic review. Ann Pharmacother. 2013;47:90–105. doi: 10.1345/aph.1R215. [DOI] [PubMed] [Google Scholar]
- 4.Warren JD, Blumbergs PC, Thompson PD. Rhabdomyolysis: A review. Muscle Nerve. 2002;25:332–47. doi: 10.1002/mus.10053. [DOI] [PubMed] [Google Scholar]
- 5.Gabow PA, Kaehny WD, Kelleher SP. The spectrum of rhabdomyolysis. Medicine (Baltimore) 1982;61:141–52. doi: 10.1097/00005792-198205000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009;361:62–72. doi: 10.1056/NEJMra0801327. [DOI] [PubMed] [Google Scholar]
- 7.Curry SC, Chang D, Connor D. Drug- and toxin-induced rhabdomyolysis. Ann Emerg Med. 1989;18:1068–84. doi: 10.1016/s0196-0644(89)80933-3. [DOI] [PubMed] [Google Scholar]
- 8.Rupert SA. Pathogenesis and treatment of rhabdomyolysis. J Am Acad Nurse Pract. 2002;14:82–7. doi: 10.1111/j.1745-7599.2002.tb00095.x. [DOI] [PubMed] [Google Scholar]
- 9.Ward MM. Factors predictive of acute renal failure in rhabdomyolysis. Arch Intern Med. 1988;148:1553–7. [PubMed] [Google Scholar]
- 10.Abassi ZA, Hoffman A, Better OS. Acute renal failure complicating muscle crush injury. Semin Nephrol. 1998;18:558–65. [PubMed] [Google Scholar]
- 11.Prendergast BD, George CF. Drug-induced rhabdomyolysis – mechanisms and management. Postgrad Med J. 1993;69:333–6. doi: 10.1136/pgmj.69.811.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellenhorn MJ, editor, editors. Medical toxicology: Diagnosis and Treatment of Human Poisoning. 2nd ed. Baltimore, MD: Williams & Wilkins; 1977. The clinical approach. [Google Scholar]
- 13.Sauret JM, Marinides G, Wang GK. Rhabdomyolysis. Am Fam Physician. 2002;65:907–12. [PubMed] [Google Scholar]
- 14.Lane R, Phillips M. Rhabdomyolysis. BMJ. 2003;19;327:115–6. doi: 10.1136/bmj.327.7407.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schrier RW, Wang W, Poole B, Mitra A. Acute renal failure: Definitions, diagnosis, pathogenesis, and therapy. J Clin Invest. 2004;114:5–14. doi: 10.1172/JCI22353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blanco J. Rhabdomyolysis of infectious and noninfectious causes. South Med J. 2002;95:1227–8. [PubMed] [Google Scholar]
- 17.Veenstra J, Smit WM, Krediet RT, Arisz L. Relationship between elevated creatine phosphokinase and the clinical spectrum of rhabdomyolysis. Nephrol Dial Transplant. 1994;9:637–41. doi: 10.1093/ndt/9.6.637. [DOI] [PubMed] [Google Scholar]
- 18.Eneas JF, Schoenfeld PY, Humphreys MH. The effect of infusion of mannitol-sodium bicarbonate on the clinical course of myoglobinuria. Arch Intern Med. 1979;139:801–5. [PubMed] [Google Scholar]
- 19.Koffler A, Friedler RM, Massry SG. Acute renal failure due to nontraumatic rhabdomyolysis. Ann Intern Med. 1976;85:23–8. doi: 10.7326/0003-4819-85-1-23. [DOI] [PubMed] [Google Scholar]
- 20.Kokko J. Goldman L, Ausiello D, editors. Rhabdomyolysis. Cecil Text Book of Medicine. (22nd ed) 2004:649–51. Saunders. [Google Scholar]
- 21.Grossman RA, Hamilton RW, Morse BM, Penn AS, Goldberg M. Nontraumatic rhabdomyolysis and acute renal failure. N Engl J Med. 1974;291:807–11. doi: 10.1056/NEJM197410172911601. [DOI] [PubMed] [Google Scholar]
- 22.Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis — An overview for clinicians. Crit Care. 2005;9:158–69. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beetham R. Biochemical investigation of suspected rhabdomyolysis. Ann Clin Biochem. 2000;37 (Pt 5):581–7. doi: 10.1258/0004563001899870. [DOI] [PubMed] [Google Scholar]
- 24.Mousavi S, Taghaddosinejad F, Talaee H, Zare GA, Sadeghi M, Rajaee P, et al. Clinical and laboratory evaluation of rhabdomyolysis in 165 patients with severe acute poisonings. J Birjand Univ Med Sci. 2010;17:136–42. [Google Scholar]


