Abstract
Mercury (Hg) is a toxic agent that evaporates in room temperature and its inhalation may cause poisoning. Due to the nonspecific symptoms, diagnosis is difficult in special circumstances with no initial history of Hg exposure. We report two such cases of Hg poisoning. The patients were two sisters, presenting with pain in extremities, itchy rashes, sweating, salivation, weakness, and mood changes. They have used a compound that contains mercury, for treatment of pedicullosis three months before admission. This compound was purchased from a herbal shop and was applied locally on the scalps for 2 days. Their urinary mercury concentrations were 50 and 70 mg/L. They were successfully treated by D-penicillamine and gabapentin. In a patient with any kind of bone and joint pain, skin rash erythema and peripheral neuropathy, mercury poisoning should be considered as a differential diagnosis.
Keywords: Acrodynia, mercury poisoning, pediculosis, twins
INTRODUCTION
It is known that mercury or hydrargyrom (Hg) or quicksilver is a toxic agent that is liquid at room temperature and evaporates gradually in the air.[1] Mercury has three forms in nature: organic, inorganic, and elementary.[2,3] The cases of metallic mercury vapor intoxication may occur in school science laboratories, from mercury dust and powders, from latex paint containing a mercury-based fungicide, and from installation of dental amalgam fillings. Another source of mercury exposure can be broken thermometers that may occur in the home.[4] American association of poison control center ranked mercury poisoning as the second among acute heavy metal poisoning cases.[2] Mercury poisoning may occur by inhalation of metal mercury vapor, particularly in children. The clinical presentations of mercury poisoning depend on its form and the route of exposure.[5,6] Due to the nonspecific symptoms and wide spectrum of the clinical presentations, diagnosis particularly in the case of chronic poisoning is difficult. Symptoms and signs such as joint and muscle pain, weakness, fatigue, peripheral neuropathy, hypertension, tachycardia, excessive salivation, sweating, insomnia, depression, exanthema, and even nephritic syndrome can be observed in mercury poisoning.[5,6,7] In this study, we report two cases of chronic Hg poisoning, which occurred due to mercury been used to treat pediculosis. We have obtained the research ethics committee approval and informed consents from the parents of patients for the treatment and publishing this case study.
CASE REPORT
Two 13-year-old twin sisters were admitted in the pediatric department of Imam Reza Hospital (Mashhad) with general body pain, especially in extremities, and back, headache, chilling and sweating in April 2010. They had a history of pain in their thighs and legs for two months. Their pain had gradually increased due to which they refused walking and missed school for more than a month. They had also anorexia, weakness, lethargy, excessive sweating, and salivation. Their parents described their weight loss and mood changes. Itchy rashes on the body especially the extremities were developed 2 weeks prior to admission [Figures 1-4]. Second degree relatives had a history of brucellosis. At the time of admission in our hospital, the sisters were irritable and depressed, their blood pressure and body temperature were normal but they had tachycardia [Table 1]. Their skins were dry with popular excoriated rashes in extremities and they had resting tremor in the upper extremities. On admission, serologic tests for brucellosis (Wright, 2-Mercaptoethanol and combs Wright) and typhoid (Widal test) were negative. Serum electrolytes, erythrocyte sedimentation rate (ESR), c-reactive protein (CRP) urinalysis, chest X-ray, magnetic resonance imaging (MRI) of brain and thigh, nerve conduction velocity (NCV), and electromyography (EMG) were normal in both patients.
Figure 1.

The pictures taken from the patients were not very impressive and unfortunately did not meet the journal criteria. We thus thought not include even one of them. However, four pictures were enclosed and leave it to the editor to decide
Figure 4.

The pictures taken from the patients were not very impressive and unfortunately did not meet the journal criteria. We thus thought not include even one of them
Table 1.
On admission clinical, laboratory, and radiographic findings in two 13-year-old twin sisters with mercury poisoning
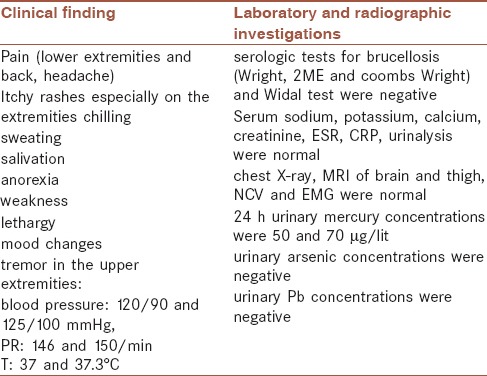
Figure 2.

The pictures taken from the patients were not very impressive and unfortunately did not meet the journal criteria. We thus thought not include even one of them
Figure 3.

The pictures taken from the patients were not very impressive and unfortunately did not meet the journal criteria. We thus thought not include even one of them
Because of the similarity and concurrence of presentations of the two sisters, after these assessments, what came to mind was an environmental poison exposure but they denied it, until their urinary Hg concentrations revealed toxic levels; post which their mother remembered that they had used a compound that contained mercury for the treatment of pediculosis 3 months ago. This compound was purchased from a herbal shop in Gorgan, Iran, and was applied locally on the scalps for 2 days.
Their 24 h urine mercury concentrations were measured in the laboratory of Medical Toxicology Center by an Atomic Absorption spectrometer (Perkin Elmer, Model 3030, Chicago, USA) using the Mercuric Hydride System The results were 50 and 70 µg/L in the twins which were higher than normal value (Normal < 25 μg/L). Clinical, laboratory, and radiographic investigations of the two sisters with mercury poisoning were described in Table 1.
Because of unavailability of dimercaptosuccinic acid (DMSA), the patients were treated with D-penicillamine (DPCN) 20 μg/kg/d orally in four divided doses. They were also treated with gabapentin (300 μg) orally in three divided doses to relieve the pain. Fortunately, no serious side effects were observed during their treatment course in the hospital.
Two weeks after starting the chelating therapy, the girls were less irritable and their pain had improved markedly, when their 24 h urine mercury concentrations declined to 9 and 15 μg/L and the patients discharged. They were followed up in an out-patient clinic for a year. They were symptomless at the end and their urinary mercury concentrations were below the detection limit of <2.5 μg/L.
DISCUSSION
The clinical presentation of our patients was compatible with acrodynia. Acrodynia or pink disease is a hypersensitivity syndrome of elemental mercury that sometimes occurs in children.[8] It is characterized by dark pink discoloration and scaling of the hands and feet, weakness, pain, irritability, hypertension, tachycardia, peripheral neuropathy, excessive salivation, and sweating.[9]
Due to the concurrence of manifestations in two members of the same family and history of brucellosis in their second degree relatives, the first investigations were focused on ruling out of infectious diseases. Since all laboratory investigations for infectious diseases including brucellosis were negative their urinary mercury concentrations were determined. Toxic urinary Hg levels confirmed our diagnosis for acrodynia and their mother reported of an herbal powder that she had used on the scalp. Since no powder left for toxicological analysis, we contacted the vendor in Gorgan who confirmed that the powder contained elemental mercury, but he had stopped making it and could not provide us with the powder.
Pheochromocytoma is the most common initial misdiagnosis for acrodynia, as levels of catecholamines may be elevated.[10] Hypertension, excessive sweating, and tachycardia are common in both acrodynia and pheochromocytoma.[11] However, pheochromocytoma is a part of syndrome like multiple endocrine neoplasia, Von Hippel–Lindau disease and neurofibromatosis that can have familial background.[12] In our patients, due to body pain, skin itchy rashes, and concomitant involvement of the two sisters, mercury poisoning was suspected. Kawasaki was not considered in our cases, as there was no history of fever and all of the inflammatory markers were normal.[13]
Other differential diagnosis of acrodynia in children is brucellosis, hyperthyroidism, Guillain Barré syndrome, sepsis, Lesch–Nyhan, and Fabry disease.[12]
In a study by Sasan et al., two boys with final diagnosis of acrodynia who were treated successfully by D-penicillamine and gabapentin in Mashhad Imam Reza hospital were similarly treated for brucellosis as outpatients in the initial phase, due to high prevalence of brucellosis in Iran.[12]
Tezer et al. describe a 14-year-old boy with fever, respiratory symptoms, and body rash. Diagnosis of mercury poisoning was made only after his mother presented with the similar symptoms a few days later.[14]
Exposure to other kind of heavy metals can produce similar complications. These include lead poisoning (arthralgia, hypertension and neuropathy, irritability), cadmium poisoning (weight loss, arthralgia, and loss of appetite), arsenic poisoning (weakness, nausea and vomiting, diarrhea, and irritability) and thallium poisoning (tachycardia, neuropathy, hypertension, and loss of appetite). But these poisonings did not match with our clinical findings and also the prevalence of these poisoning are rare.
Dimercaptosuccinic acid (DMSA) is the only chelator that was approved by the US Food and Drug Administration for treating mercury poisoning in children.[13] However, due to its unavailability, the patients were treated with D-penicillamine. Adverse reactions of D-penicillamine were reported in details on different organs such as the skin, gastrointestinal, cardiovascular, and nervous systems that may vary in different patients. We closely monitor the patients for the side effects, but fortunately we did not observe in our patient. Chelating therapy delayed bone pain and thus symptomatic pain therapy is important in the treatment of acrodynia. Celebi et al. reported that gabapentin and tramadol are effective in the treatment of neuropathic pain, mood disorders and sleep disturbances of mercury poisoning.[15] We used gabapentin that is safer than tramadol.
CONCLUSION
In a patient with any kind of bone and joint pain, skin rash erythema and peripheral neuropathy, mercury poisoning should be considered as a differential diagnosis. Where DMSA is not available, D-penicillamine may be effective for chelating therapy in children.
AUTHOR'S CONTRIBUTION
All authors have contributed in designing and conducting the study. All authors have assisted in preparation of the first draft of the manuscript or revising it critically for important intellectual content. All authors have read and approved the content of the manuscript and confirmed the accuracy or integrity of any part of the work.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Clarkson TW. The toxicology of mercury. Crit Rev Clin Lab Sci. 1997;34:369–403. doi: 10.3109/10408369708998098. [DOI] [PubMed] [Google Scholar]
- 2.Yilmaz C, Okur M, Geylani H, Çaksen H, Tuncer O, Ataş B. Chronic mercury poisoning: Report of two siblings. Indian J Occup Environ Med. 2010;14:17–9. doi: 10.4103/0019-5278.64610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarikaya S, Karcioglu O, Ay D, Cetin A, Aktas C, Serinken M. Acute mercury poisoning: A case report. BMC Emerg Med. 2010;10:7. doi: 10.1186/1471-227X-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tezer H, Erkoçoğlu M, Kara A, Bayrakcı B, Düzova A, Tekşam O, et al. Household poisoning cases from mercury brought from school. Eur J Pediatr. 2011;170:397–400. doi: 10.1007/s00431-010-1317-1. [DOI] [PubMed] [Google Scholar]
- 5.Patrick L. Mercury toxicity and antioxidants: Part 1: Role of glutathione and alpha-lipoic acid in the treatment of mercury toxicity. Altern Med Rev. 2002;7:456–71. [PubMed] [Google Scholar]
- 6.Gochfeld M. Cases of mercury exposure, bioavailability and absorption. Ecotoxicol Environ Saf. 2003;56:174–9. doi: 10.1016/s0147-6513(03)00060-5. [DOI] [PubMed] [Google Scholar]
- 7.Lebel J, Mergier D, Branches F, Lucotte M, Amorim M, Larribe F, et al. Neurotoxic effects of low level methyl mercury contamination in the Amazonian Basin. Environ Res. 1998;79:20–32. doi: 10.1006/enrs.1998.3846. [DOI] [PubMed] [Google Scholar]
- 8.Mercer JJ, Bercovitch L, Muglia JJ. Acrodynia and hypertension in a young girl secondary to elemental mercury toxicity acquired in the home. Pediatr Dermatol. 2012;29:199–201. doi: 10.1111/j.1525-1470.2012.01737.x. [DOI] [PubMed] [Google Scholar]
- 9.Van der Linde AA, Lewiszong-Rutjens CA, Verrips A, Gerrits GP. A previously healthy 11-year-old girl with behavioral disturbances, desquamation of the skin and loss of teeth. Eur J Pediatr. 2009;168:509–11. doi: 10.1007/s00431-008-0851-6. [DOI] [PubMed] [Google Scholar]
- 10.Brannan EH, Su S, Alverson BK. Elemental mercury poisoning presenting as hypertension in a young child. Pediatr Emerg Care. 2012;28:812–4. doi: 10.1097/PEC.0b013e3182628a05. [DOI] [PubMed] [Google Scholar]
- 11.Beck C, Krafchik B, Traubici J, Jacobson S. Mercury intoxication: It still exists. Pediatr Dermatol. 2004;21:254–9. doi: 10.1111/j.0736-8046.2004.21314.x. [DOI] [PubMed] [Google Scholar]
- 12.Sasan MS, Hadavi N, Afshari R, Mousavi SR, Alizadeh A, Balali-Mood M. Metal mercury poisoning in two boys initially treated for brucellosis in Mashhad, Iran. Hum Exp Toxicol. 2012;31:193–6. doi: 10.1177/0960327111417265. [DOI] [PubMed] [Google Scholar]
- 13.Mutter J, Yeter D. Kawasaki's disease, acrodynia, and mercury. Curr Med Chem. 2008;15:3000–10. doi: 10.2174/092986708786848712. [DOI] [PubMed] [Google Scholar]
- 14.Tezer H, Kaya A, Kalkan G, Erkocoglu M, Ozturk K, Buyuktasli M. Mercury poisoning: A diagnostic challenge. Pediatr Emerg Care. 2012;28:1236–7. doi: 10.1097/PEC.0b013e31827208b0. [DOI] [PubMed] [Google Scholar]
- 15.Celebi N, Canbay O, Aycan IO, Sahin A, Aypar U. Mercury intoxication and neuropathic pain. Paediatr Anaesth. 2008;18:440–2. doi: 10.1111/j.1460-9592.2008.02452.x. [DOI] [PubMed] [Google Scholar]


