Abstract
Introduction
Family planning contributes significantly to the prevention of maternal and child mortality. However, many women still do not use modern contraception and the numbers of unintended pregnancies, abortions and subsequent deaths are high. In this paper, we estimate the service delivery costs of scaling up modern contraception, and the potential impact on maternal, newborn and child survival in South Africa.
Methods
The Family Planning model in Spectrum was used to project the impact of modern contraception on pregnancies, abortions and births in South Africa (2015-2030). The contraceptive prevalence rate (CPR) was increased annually by 0.68 percentage points. The Lives Saved Tool was used to estimate maternal and child deaths, with coverage of essential maternal and child health interventions increasing by 5% annually. A scenario analysis was done to test impacts when: the change in CPR was 0.1% annually; and intervention coverage increased linearly to 99% in 2030.
Results
If CPR increased by 0.68% annually, the number of pregnancies would reduce from 1.3 million in 2014 to one million in 2030. Unintended pregnancies, abortions and births decrease by approximately 20%. Family planning can avert approximately 7,000 newborn and child and 600 maternal deaths. The total annual costs of providing modern contraception in 2030 are estimated to be US$33 million and the cost per user of modern contraception is US$7 per year. The incremental cost per life year gained is US$40 for children and US$1,000 for mothers.
Conclusion
Maternal and child mortality remain high in South Africa, and scaling up family planning together with optimal maternal, newborn and child care is crucial. A huge impact can be made on maternal and child mortality, with a minimal investment per user of modern contraception.
Introduction
Every year, nearly 3,000 mothers and 40,000 children under five years die in South Africa mainly from preventable causes [1–3]. Although substantial progress has been made in reducing maternal and child mortality in the last few years, this will not be sufficient to reach the millennium development goals (MDGs) 4 and 5 [4]. There is now, more than ever, an urgent need to scale up high impact interventions to save the lives of mothers, newborns and children [5–7]. With just a few months left to the millennium development goals (MDG) deadline in 2015, the focus of the international community is shifting to the post-2015 development agenda, with calls for family planning to be at the core of the post-2015 goals because of its potential to contribute to sustainable development [8, 9]. Family planning offers good value for investment because it is cross-cutting and impacts nearly all the MDGs, including reduction of poverty and hunger, increasing universal education, promotion of gender equality, reduction in maternal and child mortality, reduction in HIV/AIDS and environmental sustainability [10].
The contribution of family planning to maternal and child health cannot be overemphasised. Globally, birth spacing through increased use of modern family planning methods can save the lives of more than 2 million newborns and children every year [11]. Scaling up family planning could prevent one third of maternal deaths by allowing women to delay motherhood, avoid unintended pregnancies and subsequent abortions [12]. In South Africa, there are over 80,000 registered abortions annually, some of which can be potentially avoided with increased family planning [13]. In addition, teenage pregnancy is high with more than 20% of girls between 15 and 19 reporting ‘ever having been pregnant’ [14, 15]. These pregnancies can be avoided by improved family planning. Further, because HIV is the underlying cause in over 40% of maternal deaths, family planning could have a significant impact on maternal mortality. Mother-to-child transmission of HIV can also be reduced, leading to a decline in child mortality.
Despite the benefits, many women in South Africa still do not use modern contraceptive methods. Their use among women 15–49 increased modestly from 62% in 1998 to 64% in 2003, and in that year the unmet need for family planning was measured at 13% [15]. It is thus critical to ramp up efforts to provide universal access to modern contraception, especially if family planning is to be at the core of the post-2015 agenda.
The South African government has demonstrated commitment to expanding its family planning programme. It is party to Family Planning 2020, a global partnership between governments, civil society, donors and other stakeholders, aiming to expand contraceptive use to 120 million more women and girls by 2020 [16]. In line with this commitment, in 2012, South Africa developed a new family planning policy, with emphasis on dual protection (using condoms together with other contraception) [17]. The policy revision sought to update family planning provision to include newer contraceptive methods and in early 2014, new sub-dermal contraception implants were introduced, adding to the available options.
Effective implementation of South Africa’s new family planning programme requires information on the necessary resources needed to expand modern contraceptive use. Such data is, however scant. In 2012, it was estimated that the cost of contraceptive care in the developing world was US$4 billion, and scaling up family planning to meet the need for modern contraception would cost an additional US$8 billion annually [18]. In South Africa, it is estimated that the total cost of family planning for all HIV positive women in 2009 was approximately US$3.3 million [19]. However, a complete picture is required to show the costs and benefits of expanding family planning to all women who need it.
This paper shows the potential costs and benefits of scaling up modern contraception in South Africa. We model the effects of increasing the contraceptive prevalence rate (CPR) on population size, growth rate, pregnancies, births, abortions and maternal and child mortality. This data can inform the implementation of South Africa’s new family planning policy.
Methods
We used the Spectrum program to model the impact of family planning on maternal and child mortality. Spectrum consists of a suite of modules that are used to assess the impact of interventions on population health. The modules in Spectrum include the Lives Saved Tool (LiST), AIDS Impact Module (AIM), Family Planning (FamPlan) and Demographic Projections (DemProj) [20]. DemProj is the main Spectrum model, which projects country specific populations by age and sex. The other modules interact with DemProj, to address various issues including fertility, HIV/AIDS and maternal and child survival. In this analysis, we use FamPlan and LiST to examine the impact of family planning on fertility rates, pregnancies, births, abortions and maternal and child survival.
FamPlan helps to inform policy on family planning by projecting the requirements needed to address unmet need for modern contraception in a country. The model can be used to set family planning goals, estimate the service expansion needed to meet the goals, and evaluate alternative methods to achieve the goals. FamPlan uses the proximate determinants model of fertility to relate contraception to the total fertility rate. The proximate determinants model of fertility explains the fertility inhibiting factors including contraception, abortion, marriage, postpartum insusceptibility and primary infertility [21, 22]. The model postulates that fertility would be at its highest if these inhibiting factors were non-existent or at a minimum. FamPlan projects the population fertility by considering the effect of each proximate determinant. Thus, inputs of each proximate determinant of fertility are required in the model: the percent of women aged 15–49 years in a sexual union (in our analysis, we consider sexually active women, given that many births in South Africa occur outside informal and formal unions), the proportion using modern contraception by method, the degree of primary infertility, the use of abortion, and the duration of postpartum insusceptibility to conception. Assumptions include the proximate determinants of fertility and the characteristics of the family planning program (method mix, source mix, discontinuation rates) to calculate the cost and the number of users and acceptors of different contraceptive methods by source. FamPlan calculates indicators showing the number of family planning users, commodities required, unplanned pregnancies and births, and numbers of abortions—all based on the data entered into the model, the assumptions made, and the desired outcomes.
In this analysis, the impact of family planning is estimated by increasing the contraceptive prevalence rate (CPR). The CPR, the percentage of sexually active women of reproductive age (15–49 years) using contraceptive methods [15], is used because it is generally easy to measure and a straight forward indicator of the number of contraceptive users. We used a CPR for South Africa of 64.6% at baseline (2014). The CPR was then increased by 0.68% per year in a 15 year period from 2015 to 2030. This was made on the basis of a previously observed change in CPR of approximately 0.68% per year between 1998 and 2003 [15].
FamPlan inputs and assumptions
Proximate determinants
The proximate determinants of fertility for South Africa included in this analysis are obtained mainly from the 2003 Demographic and Health Survey [15] and 2013 World Fertility Report [23], and include: a) proportion of women in sexual union aged 15–49 years (46%); b) postpartum insusceptibility—the period after a birth during which a woman is not exposed to the risk of pregnancy, was 13 months [15]; c) contraception—the level of contraception use by method is given in Table 1. The use of the sub-dermal implant was negligible before 2014, when the National Department of Health began scaling it up. We assumed the use of the implant would increase to 0.5% by the end of 2014, 1% in 2015 and 2016, and to 2% thereafter (with the remaining methods of contraception maintaining the same proportions relative to each other); d) the level of unintended pregnancy terminated or induced abortion was 19%, based on Southern African regional estimates [24]; and e) the prevalence of sterility was 5% [15].
Table 1. Percentage use of contraception by method.
| Methods | Percent |
|---|---|
| Male condom | 12 |
| Female sterilization | 16 |
| Male sterilization | 1 |
| Injectable contraceptive | 51 |
| Implant (3 years) | 0 |
| IUD | 1 |
| Oral contraceptive | 19 |
Source: South Africa Demographic and Health Survey, 2003; World Fertility Report, 2013; Spectrum defaults
Other assumptions
The unmet need for family planning used was 13% [15], this reflects the difference between women’s contraceptive behaviour and their reproductive intentions. Based on Spectrum, the total fertility rate, the number of children that would be born to a woman if she were to live to the end of her childbearing years, was estimated to be 2.43 in 2014.
Contraception costs
Costs of scaling up family planning were modelled in FamPlan, using cost data from the United Nations Population Fund (UNFPA). Details of the costing methodology are provided elsewhere [18]. Costing took an ingredients approach and was undertaken from a health service provider perspective. Both direct and indirect costs are included. Direct costs were estimated for contraceptive commodities, supplies and labour needed for counselling, method provision and supply, follow-up and method removal (where needed). Unit costs are obtained from the Management for Sciences Health International Drug Price Indicator, United Nations Children’s Fund Supply Catalogue and the WHO-CHOICE database. Indirect costs included programme management, supervision, personnel training, health education, monitoring and evaluation, advocacy, systems strengthening and maintenance and expansion of physical capacity for health facilities. All prices were adjusted to 2012 US dollars. The annual unit costs of each contraceptive method are provided in Table 2.
Table 2. Unit costs (2012 US dollars) of contraceptive methods per year.
| Method | Cost (US$) |
|---|---|
| Male condom | 3.9 |
| Female sterilization | 2.79 |
| Male sterilization | 1.59 |
| Injectable contraceptive | 9.14 |
| Implanon (3 years) | 7.74 |
| Oral contraceptive | 8.72 |
| IUD | 1.01 |
Source: UNFPA
Estimating the impact of Family Planning on maternal and child survival
After making adjustments to the FamPlan model in Spectrum, the impact of scaling up family planning on maternal, newborn and child survival can be assessed in LiST [25], which has been extensively used to model the impact of intervention scale up on maternal and child mortality [5, 6, 26]. National baseline information on mortality rates and causes of death, background variables (e.g. fertility, economic status), current coverage of more than 60 interventions and their associated effectiveness values relative to specific causes of death and risk factors are used to estimate the deaths averted, overall and by specific interventions.
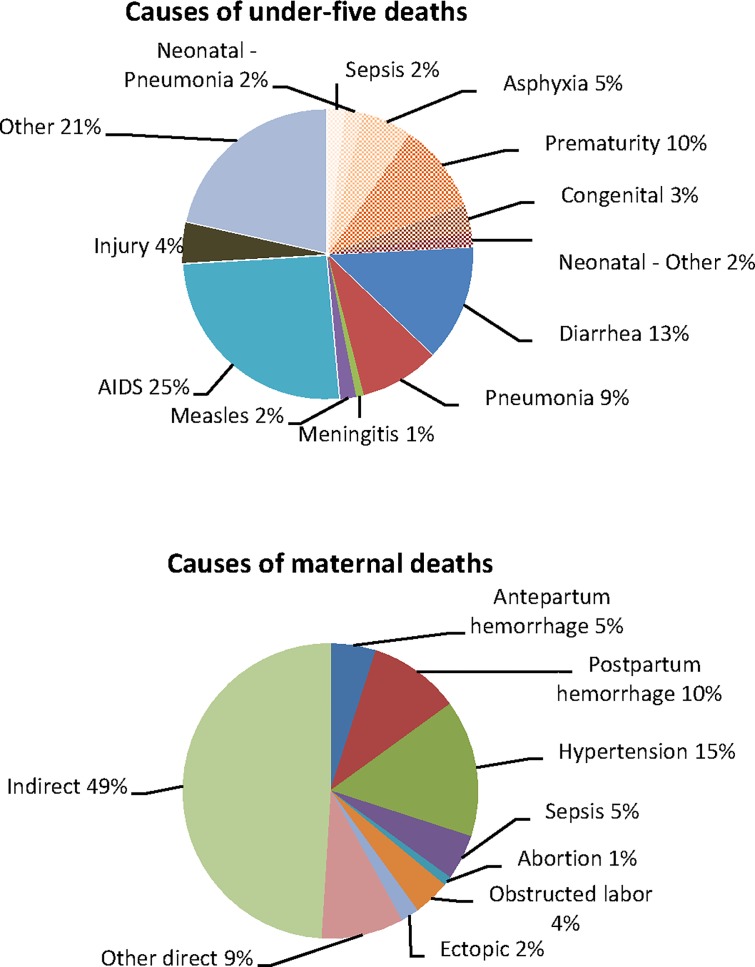
We used a maternal mortality ratio of 269 deaths per 100,000 live births [4], under-five mortality rate of 41/1,000 and neonatal mortality rate of 13/1,000 [3]. The causes of maternal [27], newborn and child [28] mortality used are given in Fig 1.
Fig 1. Causes of child, new born and maternal deaths in SA used in the LiST model.
The baseline coverage of interventions included in LiST was reviewed and where possible compiled using national population based data (Table 3). LiST does not provide default coverage values for all interventions included in the model. Some of these interventions include ectopic pregnancy, management of abortions, pre-eclampsia and clean birth practices. Data on the coverage of these interventions in South Africa are also not available. The coverage levels used in our analysis are based on consensus obtained from local experts across maternal and child health on reasonable coverage levels obtaining in South Africa, taking into consideration recent policy changes, financial and resource inputs, and observed localised coverage change. The consultation with the experts took place at a one day meeting to discuss the trends in maternal and child interventions in South Africa. We invited 23 participants who work in the health sector in various positions at national and district level, clinical practice and academia. The participants deliberated on the coverage levels of each intervention, drawing on their own experiences.
Table 3. Baseline (2014) intervention coverage of interventions included in the LiST model.
| Interventions | Baseline coverage |
|---|---|
| Safe abortion services | 35 |
| Post abortion case management | 60 |
| Ectopic pregnancy case management | 40 |
| Antenatal care (4 visits) | 50 |
| Tetanus toxoid vaccination | 77 |
| Calcium supplementation | 5 |
| Hypertensive disease case management | 40 |
| Diabetes case management | 10 |
| MgSO4—Management of pre-eclampsia | 75 |
| Fetal growth restriction detection and management | 10 |
| Skilled birth attendance (SBA) | 93 |
| Facility delivery (clinic and hospital) | 87 |
| Unassisted deliveries | 5 |
| Basic emergency obstetric care (BEMOC) | 5 |
| Comprehensive emergency obstetric care (CEMOC) | 50 |
| Clean birth practices | 70 |
| Immediate assessment and stimulation | 70 |
| Labour and delivery management | 93 |
| Neonatal resuscitation | 40 |
| Antenatal corticosteroids for preterm labour | 20 |
| Antibiotics for rapture of membrane | 25 |
| MgSO4 management of eclampsia | 80 |
| Active management of the third stage of labour | 80 |
| Induction of labour for pregnancies lasting 41+ weeks | 10 |
| Promotion of breastfeeding | 25 |
| Preventive postnatal care | 10 |
| Clean postnatal practices | 10 |
| Complementary feeding—education only | 10 |
| Complementary feeding—supplementation and education | 5 |
| Vitamin A supplementation | 50 |
| Improved water source | 91 |
| Water connection in the home | 69 |
| Improved sanitation—Utilization of latrines or toilets | 74 |
| Hand washing with soap | 17 |
| Hygienic disposal of children's stools | 41 |
| BCG | 74 |
| Polio | 74 |
| DPT | 66 |
| Hib | 66 |
| HepB | 74 |
| Pneumococcal | 64 |
| Rotavirus | 66 |
| Measles | 74 |
| Maternal Sepsis case management | 75 |
| Kangaroo mother care | 25 |
| Case management of severe neonatal infection | 44 |
| Injectable antibiotics | 70 |
| Full supportive care | 44 |
| ORS—oral rehydration solution | 50 |
| Antibiotics—for treatment of dysentery | 80 |
| Zinc—for treatment of diarrhoea | 10 |
| Oral antibiotics: case management of pneumonia in children | 73 |
| Vitamin A—for treatment of measles | 75 |
| Therapeutic feeding—for severe wasting | 45 |
| Treatment for moderate acute malnutrition | 10 |
| PMTCT | 90 |
| Early treatment of HIV in pregnant women | 40 |
| Treatment of TB in pregnant women | 50 |
| Treatment of injuries in children 1–5 years | 50 |
| Treatment of TB in children 1–5 years | 50 |
In the base case analysis, maternal, newborn and child deaths were then estimated, holding this baseline coverage constant, and compared to a scenario where coverage of all interventions was increased linearly by 0.5% per year. Taking 2014 as the base year, intervention scale up was started in 2015.
The impact of family planning on maternal and child mortality was measured in terms of deaths averted. First, we calculated the expected number of deaths at the current (baseline) level of intervention coverage. Second, the numbers of deaths were recalculated with increased coverage for all interventions in the year 2030 (5% annually). Deaths averted (or additional lives saved) were then estimated by subtracting the numbers of deaths at baseline from the deaths at scale. The deaths averted attributed to family planning were measured by subtracting the number of deaths with and without changes in the level of family planning. We also estimated the potential life years gained, which were calculated as deaths averted multiplied by life expectancy, using a life expectancy at birth of 60 years for newborns and children [29], and a reproductive-aged life expectancy of 27 years for mothers [30].
Scenario analysis
A scenario analysis was undertaken to test the impact of changes in the base case assumptions, where CPR was increased minimally by 0.1%. Due to data unavailability, this choice was made to represent a lower uptake of family planning. In the scenario analysis, all essential maternal, newborn and child interventions were linearly scaled up until coverage reached 99% in 2030.
Results
Base case analysis
The results of this analysis show the impact of increasing the contraceptive prevalence rate (CPR) on the total fertility rate (TFR), births, abortions and maternal and child deaths. Also presented are the total annual costs of scaling up family planning methods by 0.68% per year. The baseline CPR was 64.6% (Table 4), which was projected to increase to 75.5% in 2030 (with CPR increasing by 0.68% per year).
Table 4. Base case results for projected demographic events and impact of family planning on maternal, newborn and child mortality.
| Projected demographic events | 2014 baseline | Changes in 2030 |
| Contraceptive prevalence rate (%) | 64.6 | 75.5 |
| Total fertility rate (number) | 2.43 | 1.65 |
| Total number of pregnancies | 1 336 800 | 1 006 000 |
| Unintended pregnancies (number) | 535 400 | 383 500 |
| Abortions (number) | 103 400 | 74 071 |
| Live births (number) | 1 059 600 | 939 500 |
| Projected impact on mortality | 2014 baseline | Changes in 2030 |
| Number of maternal deaths | 2 800 | 1 700 |
| Number of child deaths (0–69) | 38 100 | 28 300 |
| Number of neonatal deaths | 12 800 | 10 800 |
| Maternal mortality ratio (deaths per 100,000 live births) | 269 | 210 |
| Maternal mortality rate (deaths per 10,000 women aged 15–49) | 21 | 11 |
| Under-5 mortality rate (deaths per 1,000 live births) | 41 | 34 |
| Neonatal mortality rate (deaths per 1,000 live births) | 12 | 12 |
| Deaths averted by family planning (2030) | Deaths averted | Potential life years gained |
| Maternal deaths | 600 | 16 200 |
| Child deaths (0–69 months) | 5 900 | 354 000 |
| Neonatal deaths | 1 500 | 90 000 |
All essential maternal and child health interventions linearly scaled up by 0.5% per year. Potential life years gained = total deaths multiplied by life expectancy (27 years for mothers and 60 years for neonates and children). CPR = Contraceptive prevalence rate. Figures rounded to the nearest 100.
Impact on demographic events and maternal, newborn and child mortality
The TFR was estimated to be 2.43 in 2014, and by 2030, would decline to 1.65; the total number of pregnancies reduce to one million (Table 4), and unintended pregnancies, abortions and births reduce by approximately 23%.
At baseline, before scale up of family planning or other interventions, the total annual number of maternal deaths was estimated to be 2,800 (Table 4). In 2030, this would reduce to approximately 1700 (with scale up of maternal and child interventions by 0.5% per year).
The annual numbers of child deaths reduce from approximately 38,000 in 2014 to 28,000; and the deaths of newborns reduce from 12,800 to 10,800 in 2030.
The maternal mortality ratio (estimated at 269 in 2014) would reduce to 210 maternal deaths per 100,000 live births. The maternal mortality rate (deaths per 10,000 women 15–49 years) reduces from 21/10,000 in 2014, to 12/10,000.
Increasing family planning by 0.68 percentage points per year averted an additional 600 maternal deaths in 2030. The number of child and neonatal deaths averted by family planning were 5,900 and 1,500, respectively (Table 4). The potential life years gained were 16,200 for mothers, 354,000 for children and 90,000 for neonates.
Commodity requirements and costs of family planning
Table 5 shows the annual number of units of each contraceptive method required to meet the need when family planning is scaled up. If family planning increases by 0.68 percentage points per year, the contraceptive requirements between 2014 and 2030 increase as follows: required units of male condoms increases from 54 million to 72 million; injectable contraception increases from 7 million to 10 million; the implant increases from 19,200 to 41,800; the oral contraceptive increases from 10 million to 12 million; and IUD from 23,500 to 27,800.
Table 5. Base case results for total commodity (number of units) requirements for each contraceptive method per year.
| Commodity | 2014 baseline | Changes in 2030 |
|---|---|---|
| Male condom | 54 636 800 | 72 260 200 |
| Injectable contraceptive | 7 740 200 | 10 238 000 |
| Implant | 19 270 | 41 800 |
| Oral contraceptive | 10 813 500 | 12 044 700 |
| IUD | 23 500 | 27 800 |
CPR = Contraceptive prevalence rate. IUD = Intrauterine device. Figures rounded to the nearest 100.
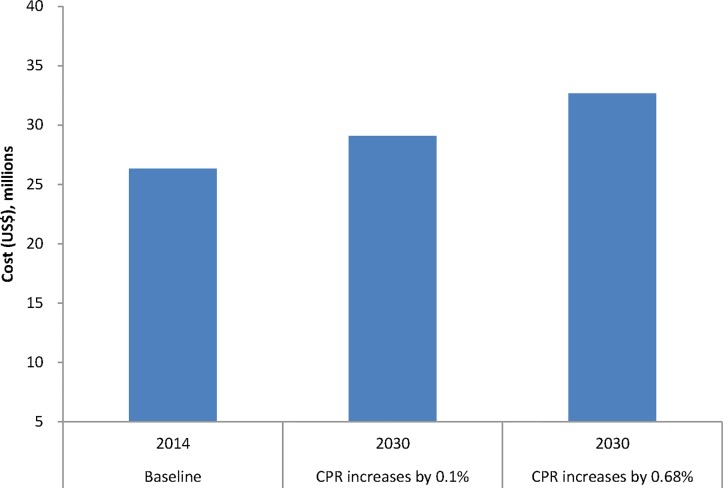
The total annual costs of providing contraception in 2014 (before scale up) are estimated to be approximately US$26 million. In 2030, the annual costs would be US$33 million (if CPR increases by 0.68% per year).
The annual number of users of modern methods of contraception is projected to be 4 million in 2014, and by 2030 will rise to 5.5 million. The average cost per user per year of modern contraception is about US$7 and the annual cost per capita (total cost/total South African population) is US$0.6. The annual cost of family planning per potential life year gained is US$ 2,000 for mothers, US$79 for children and US$320 for newborns. The incremental cost (2030 costs minus 2014 costs) per death averted is US$2400 for child and US$30,000 for maternal deaths. The incremental cost per life year gained is US$40 for children and US$1,000 for mothers.
Scenario analysis
Table 6 shows the results of the scenario analysis for the projected demographic events and impact of family planning on maternal, newborn and child mortality (in 2030). The projected TFR is 2.3, the total number of pregnancies are 1.3 million, and maternal deaths are 1,100. The maternal mortality rate (21/10,000 at baseline) is expected to be 8/10,000. Increasing family planning in the scenario analysis would avert 300 maternal, 4,500 child and 1,300 neonatal deaths in 2030 (Table 7).
Table 6. Results of scenario analysis for projected demographic events and impact of family planning on maternal, newborn and child mortality (shown are changes in 2030).
| Projected demographic events | CPR increases by 0.1% |
| Contraceptive prevalence rate (%) | 66.2 |
| Total fertility rate (number) | 2.30 |
| Total number of pregnancies | 1 341 100 |
| Unintended pregnancies (number) | 533 200 |
| Abortions (number) | 103 000 |
| Live births (number) | 1 064 000 |
| Projected impact on mortality | CPR increases by 0.1% |
| Number of maternal deaths | 1 100 |
| Number of child deaths (0–69) | 18 100 |
| Number of neonatal deaths | 4 700 |
| Maternal mortality ratio (deaths per 100,000 live births) | 108 |
| Maternal mortality rate (deaths per 100,000 women aged 15–49) | 8 |
| Under-5 mortality rate (deaths per 1,000 live births) | 17 |
| Neonatal mortality rate (deaths per 1,000 live births) | 4 |
All essential maternal and child health interventions are scaled up to 99% coverage. Potential life years gained = total deaths multiplied by life expectancy (27 years for mothers and 60 years for neonates and children). CPR = Contraceptive prevalence rate. *Results only for CPR increase by 5%. Figures rounded to the nearest 100.
Table 7. Results of the scenario analysis for projected deaths averted and potential life years gained by family planning.
| Deaths averted | CPR increases by 0.1% | |
|---|---|---|
| Deaths averted | Potential life years gained | |
| Maternal deaths | 300 | 8 100 |
| Child deaths (0–69 months) | 4 500 | 270 000 |
| Neonatal deaths | 1 300 | 78 000 |
All essential maternal and child health interventions are scaled up to 99% coverage. Potential life years gained = total deaths multiplied by life expectancy (27 years for mothers and 60 years for neonates and children). CPR = Contraceptive prevalence rate. Figures rounded to the nearest 100.
Fig 2 compares the total annual costs of providing contraception in all scenarios. Compared to an estimated cost of US$26 million in 2014, the annual costs of providing contraception would be US$29 million in the scenario analysis (Fig 2).
Fig 2. Total annual costs (2012 US$) of family planning projected by the model.
Discussion
This paper demonstrates the potential impact of increasing the use of modern contraception on fertility, and maternal, newborn and child survival in South Africa. Using a model for family planning, we scaled up the contraceptive prevalence rate, over a period of 15 years (2015 to 2030), by 0.68 percentage points annually. In a scenario analysis, we tested the impact of increasing CPR by 0.1% annually. In addition, we assumed that maternal, newborn and child interventions to reduce mortality (including emergency obstetric care, antenatal care, kangaroo mother care and breastfeeding promotion) were scaled up by 0.5% annually (and 99% by 2030 in the scenario analysis). The results show that in 2030, unintended pregnancies, abortions and births could reduce by approximately 23% if CPR increases by 0.68% per year. This could avert 7,000 child and newborn deaths and avert 600 maternal deaths per year. Scaling up family planning will have a huge impact on the total fertility rate, which would fall to 1.65. This is far below the population replacement rate, and would make South Africa comparable to countries such as Brazil (1.8) and Singapore (1.3) [31]. The fertility rate at this level would see an eventual decline in population growth in South Africa.
The results on maternal and child survival are made on the basis of aspirational goals (0.5% per year and 99% intervention coverage by 2030), which may not be easy for South Africa to attain in the short-term, and does not take into account the quality of these interventions. However, the rates of scale up were selected in order to show what might be possible if concerted efforts were made to optimise intervention coverage. The rapid increase in coverage of interventions such as skilled attendance at birth, immunisations and PMTCT in the last decade, indicate that attainment of full intervention coverage may be feasible. Similarly, achieving the suggested contraceptive prevalence rates may seem daunting, but it is possible as shown by countries such as Brazil and Thailand, where contraceptive prevalence is above 80% [31].
In this analysis, we have provided an estimate of the commodity requirements and costs should the contraceptive prevalence rate increase. The total annual costs of providing modern contraception are estimated to be US$33 million in the base case analysis and US$29 million (US$0.5 per capita) in the scenario analysis. The cost of scaling up family planning would amount to less than 0.5% of the 2014 national health budget, and about 1% of the current primary healthcare expenditure per capita of US$74 [32]. We, however, cannot state on the basis of this evidence that scaling up family planning is affordable to the South African government. In our results, we provide estimates of cost-effectiveness ratios measured as costs per potential life years gained. These show that scaling up family planning is highly cost-effective, when judged against the gross domestic product per capita threshold [33]. Such information could be used in future analyses to compare the cost-effectiveness of family planning to other maternal and child health interventions.
The results provided in this paper should be taken with caution, as they do not imply that expanding family planning will necessarily lead to an increased use in contraception. There are many barriers to contraceptive use from both the demand and supply side [34, 35]. In South Africa, the leading reasons for not using contraceptives include concerns regarding side effects and opposition by partners [36, 37]. Among adolescents, parental consent is often an issue, and in a country such as South Africa where ‘traditional’ values are entrenched, and sex is in many cases still a taboo topic, sexually active adolescents may not easily access contraception even if it were made freely available [38]. On the supply side, efforts should be made to address inadequate logistics and protocols [39] and strengthen the training of front-line health workers in the provision of family planning [36]. Contraceptives should also be made readily available and the demand for the variety of methods should be met, as this is essential to meeting women’s desire to space births. It is also important to deal with the problem of health worker biases and judgmental attitudes, particularly with regard to adolescents who wish to access family planning services [37].
Addressing these issues could require substantially more resources than the current model is capable of generating, and could significantly lead to higher societal costs. More needs to be done to understand these costs. Furthermore, the costs estimated in this paper are dependent on the contraceptive method mix, and a change in this distribution could impact the associated costs. However, should this be the case in future, the unit costs provided here [18] could be used to make the necessary adjustments. In addition, the costs of scaling up key interventions to reduce maternal, newborn and child mortality have not been included in this analysis, but they should be included in future, since funding for family planning cannot be considered in isolation, but as part of a package of essential interventions.
The full benefits of family planning on the health system could not be entirely addressed in this analysis, yet the consequences may be greater than the impact on mortality. We estimated approximately 1.3 million pregnancies and deliveries in South Africa, which can be reduced by ramping up family planning. With fewer pregnancies and births, more resources could be freed up, potentially leading to an improvement in service delivery for antenatal care and childbirth.
Further, in order to fully realise the benefits of family planning, choices must be made on the appropriate indicators to measure progress and impact. The choice of maternal mortality ratio, instead of maternal mortality rate as the key MDG 5 indicator does not adequately portray the positive role of family planning. As shown in our sensitivity analysis results, the impact of family planning on the maternal mortality ratio remained static even after scaling up family planning in both scenarios. This may be because the absolute number of maternal lives saved is not incorporated in the maternal mortality ratio, since increasing contraceptive prevalence reduces the number of births, the denominator in the ratio. Perhaps a more informative measure would be the maternal mortality rate, whose denominator is the number of women in the reproductive age group.
One of the impediments to effective investment in family planning is insufficient data on the use of modern contraception. Available data on contraceptive prevalence and the unmet need for family planning in South Africa are either outdated or inadequate. The last measurement of national level unmet need was made in the 2003 South Africa Demographic and Health Survey. Several developments have occurred since then, and the need to update these statistics cannot be overemphasized. National data on the method mix of contraceptive use is available in some surveys, and the District Health Information System (DHIS). On the face of it, the DHIS could provide a proxy for contraceptive use, but its reliability is of concern, since it is only collected in health facilities, and contains many inconsistencies. Furthermore, most of the data available, particularly institutional data, are not age-disaggregated or sub-group stratified. Therefore, in this analysis, we used a broad age-group of 15–49 years. A more insightful analysis could have been performed if data in five year age-groups had been available. It is important to take into account the age-distribution of users, as this has an impact on the usage of contraception and the benefits that can be realised from family planning. Another limitation of the Spectrum model is that it does not take into account the impact of birth spacing on child mortality, hence it underestimates the benefits of family planning. The importance of birth spacing to child survival is well documented and studies have shown that higher birth intervals are associated with lower risks of child mortality [11, 40]. Spectrum does not include this relationship, since intervention impact is estimated through the reduction of causes of child death. These are considerations that should be made in future analyses when changes to the model are made to account for such effects.
As we approach the post-2015 era, emphasis should be placed on renewed efforts to reduce maternal and child mortality. The expansion of family planning services in many low and middle income countries, including South Africa has been hampered by shifts in international health and development priorities, and the focus of attention on HIV/AIDS, infectious diseases and poverty alleviation [41]. This has resulted in a disproportionate allocation of resources to vertical programmes such as HIV/AIDS. Greater emphasis should be placed on more comprehensive packages.
Conclusions
Scaling up family planning can help avert nearly 7,000 newborn and child deaths and 300 maternal deaths annually; with investments of approximately US$7 per user per year. This is probably a minimal estimate because other requirements such as logistics and infrastructure, which impact on costs, have not been considered. As we approach the end line of the millennium development goals, there is great need for an appraisal of the impact of the family planning policy in the last decade, and to find solutions to the many challenges facing its adequate implementation. Significant strides could be made in the post-2015 agenda by focusing on increasing essential maternal and child interventions, and bringing family planning to the fore. We estimate that with concerted efforts and appropriate investment, South Africa can reach its MDG 4 target of 20 child deaths per 1,000 live births by 2030; and also get closer to meeting its MDG 5 target of reducing maternal mortality.
Acknowledgments
We would like to acknowledge Ingrid Friberg and Bill Winfrey at the John Hopkins Bloomberg School of Public Health for their support with respect to the LiST analyses.
Data Availability
All relevant data are available within the paper.
Funding Statement
The authors received no specific funding for this work.
References
- 1. WHO. Trends in Maternal Mortality: 1990 to 2010. Geneva, Switzerland: WHO, 2012. [Google Scholar]
- 2. Stats SA. Mortality and causes of death in South Africa, 2011: Findings from death notification. Pretoria, South Africa: Stats SA, 2014. [Google Scholar]
- 3. Dorrington RE, Bradshaw D, Laubscher R. Rapid mortality surveillance report 2012. Cape Town, South Africa: South African Medical Research Council, 2014. [Google Scholar]
- 4. Stats SA. Millennium Development Goals Country Report. Pretoria, South Africa: Stats SA, 2013. [Google Scholar]
- 5. Chopra M, Daviaud E, Pattinson R, Fonn S, Lawn JE. Saving the lives of South Africa's mothers, babies, and children: can the health system deliver? Lancet. 2009;374(9692):835–46. 10.1016/S0140-6736(09)61123-5 [DOI] [PubMed] [Google Scholar]
- 6. Pattinson R, Kerber K, Buchmann E, Friberg IK, Belizan M, Lansky S, et al. Stillbirths: how can health systems deliver for mothers and babies? Lancet. 2011;377(9777):1610–23. 10.1016/S0140-6736(10)62306-9 . [DOI] [PubMed] [Google Scholar]
- 7. South Africa Every Death Counts Writing Group, Bradshaw D, Chopra M, Kerber K, Lawn JE, Bamford L, et al. Every death counts: use of mortality audit data for decision making to save the lives of mothers, babies, and children in South Africa. Lancet. 2008;371(9620):1294–304. 10.1016/S0140-6736(08)60564-4 . [DOI] [PubMed] [Google Scholar]
- 8. Fabic MS, Choi Y, Bongaarts J, Darroch JE, Ross JA, Stover J, et al. Meeting demand for family planning within a generation: the post-2015 agenda. Lancet. 2014. 10.1016/S0140-6736(14)61055-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Petruney T, Wilson LC, Stanback J, Cates W. Family planning and the post-2015 development agenda. Bulletin of the World Health Organization. 2014;92:548–A. 10.2471/BLT.14.142893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cates W Jr. Family planning: the essential link to achieving all eight Millennium Development Goals. Contraception. 2010;81(6):460–1. 10.1016/j.contraception.2010.01.002 . [DOI] [PubMed] [Google Scholar]
- 11. Rutstein SO. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2005;89 Suppl 1:S7–24. 10.1016/j.ijgo.2004.11.012 . [DOI] [PubMed] [Google Scholar]
- 12. Collumbien M, Gerressu M, Cleland J. Non-use and use of ineffective methods of contraception In: Ezzati M, Lopez AD, Rogers A, Murray CJL, editors. Comparative quantification of health risks: Global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organisation; 2004. p. 1255–320. [Google Scholar]
- 13.Health Systems Trust. Termination of Pregnancy Durban, South Africa2013 [cited 2014 August 26]. Available: http://indicators.hst.org.za/healthstats/47/data.
- 14. Willan W. A review of teenage pregnancy in South Africa—Experiences of schooling, and knowledge and access to sexual and reproductive health services. South Africa: Partners in Sexual Health, 2013. [Google Scholar]
- 15. National Department of Health, Medical Research Council, OrcMacro. South Africa Demographic and Health Survey 2003. Pretoria: NDOH, 2007. [Google Scholar]
- 16. FP2020. Progress Report 2012–2013: Partnership in Action. Washington DC: FP2020, 2013. [Google Scholar]
- 17. National Department of Health. National contraception and fertility planning policy and service delivery guidelines, 2012—A companion to the national contraception and clinical guidelines. Pretoria: NDOH, 2012. [Google Scholar]
- 18. Singh S, Darroch JE. Adding It Up: Costs and Benefits of Contraceptive Services—Estimates for 2012. New York, USA: Guttmacher Institute and United Nations Population Fund (UNFPA), 2012. [Google Scholar]
- 19. Halperin DT, Stover J, Reynolds HW. Benefits and costs of expanding access to family planning programs to women living with HIV. Aids. 2009;23 Suppl 1:S123–30. 10.1097/01.aids.0000363785.73450.5a . [DOI] [PubMed] [Google Scholar]
- 20. Stover J, McKinnon R, Winfrey B. Spectrum: a model platform for linking maternal and child survival interventions with AIDS, family planning and demographic projections. International journal of epidemiology. 2010;39 Suppl 1:i7–10. 10.1093/ije/dyq016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stover J. Revising the proximate determinants of fertility framework: what have we learned in the past 20 years? Studies in family planning. 1998;29(3):255–67. . [PubMed] [Google Scholar]
- 22. Bongaarts J. A Framework for Analyzing the Proximate Determinants of Fertility. Population and Development Review. 1978;4(1):105–32. 10.2307/1972149 [DOI] [Google Scholar]
- 23. United Nations Department of Economic and Social Affairs. Population Division. World Fertility Report 2012. New York, USA: UN, 2013. [Google Scholar]
- 24. Singh S, Wulf D, Hussain R, Bankole A, Sedgh G. Abortion Worldwide: A Decade of Uneven Progress. New York: Guttmacher Institute, 2009. [Google Scholar]
- 25. Walker N, Tam Y, Friberg IK. Overview of the Lives Saved Tool (LiST). BMC public health. 2013;13 Suppl 3:S1 10.1186/1471-2458-13-S3-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014. 10.1016/S0140-6736(14)60792-3 . [DOI] [PubMed] [Google Scholar]
- 27. NCCEMD. Saving Mothers 2008–2010—Fifth report on the Confidential Enquiries into Maternal Deaths in South Africa. Pretoria, South Africa: NDOH, 2012. [Google Scholar]
- 28. Pillay-van Wyk V, Msemburi W, Laubscher R, Dorrington RE, Groenewald P, Matzopoulos R, et al. Second National Burden of Disease Study South Africa: national and subnational mortality trends, 1997?2009. The Lancet. 2013;381:S113. [Google Scholar]
- 29. Stats SA. Mid-year population estimates. Pretoria, South Africa: Stats SA, 2013. [Google Scholar]
- 30. Canudas-Romo V, Liu L, Zimmerman L, Ahmed S, Tsui A. Potential gains in reproductive-aged life expectancy by eliminating maternal mortality: a demographic bonus of achieving MDG 5. PloS one. 2014;9(2):e86694 10.1371/journal.pone.0086694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. UNICEF. State of the world's children—children with disabilities. New York: UNICEF, 2013. [Google Scholar]
- 32. Tathiah N. Financial indicators In: Massyn N, Day C, Dombo M, Barron P, English R, Padarath A, editors. District health barometer. Durban, South Africa: HST; 2013. [Google Scholar]
- 33. WHO. Guide to cost effectiveness analysis. Geneva: WHO, 2003. [Google Scholar]
- 34. Prata N. Making family planning accessible in resource-poor settings. Philosophical transactions of the Royal Society of London Series B, Biological sciences. 2009;364(1532):3093–9. 10.1098/rstb.2009.0172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Culwell KR, Vekemans M, de Silva U, Hurwitz M, Crane BB. Critical gaps in universal access to reproductive health: contraception and prevention of unsafe abortion. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2010;110 Suppl:S13–6. 10.1016/j.ijgo.2010.04.003 . [DOI] [PubMed] [Google Scholar]
- 36. Richter MS, Mlambo GT. Perceptions of rural teenagers on teenage pregnancy. Health SA Gesondheid. 2005;10(2):61–9. [Google Scholar]
- 37. Wood K, Jewkes R. Blood Blockages and Scolding Nurses: Barriers to Adolescent Contraceptive Use in South Africa. Reproductive health matters. 2006;14(27):109–18. [DOI] [PubMed] [Google Scholar]
- 38. Lebese RT, Maputle SM, Ramathuba DU, Khoza LB. Factors influencing the uptake of contraception services by Vatsonga adolescents in rural communities of Vhembe District in Limpopo Province, South Africa. Health SA Gesondheid. 2013;18(1). 10.4102/hsag.v18i1.654 [DOI] [Google Scholar]
- 39. Baumgartner JN, Morroni C, Mlobeli RD, Otterness C, Myer L, Janowitz B, et al. Timeliness of contraceptive reinjections in South Africa and its relation to unintentional discontinuation. International family planning perspectives. 2007;33(2):66–74. 10.1363/ifpp.33.066.07 . [DOI] [PubMed] [Google Scholar]
- 40. DaVanzo J, Hale L, Razzaque A, Rahman M. The effects of pregnancy spacing on infant and child mortality in Matlab, Bangladesh: how they vary by the type of pregnancy outcome that began the interval. Population studies. 2008;62(2):131–54. 10.1080/00324720802022089 . [DOI] [PubMed] [Google Scholar]
- 41. Singh S, Darroch JE, Ashford L, Vlassoff M. Adding it up: the costs and benefits of investing in family planning and maternal and newborn health. New York: Guttmacher Institute and UNFPA, 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are available within the paper.