Abstract
Background:
The preschool years are a crucial time to study the determinants of childhood obesity, as it is when eating and physical activity habits are becoming established. The purpose of this study was to compare the prevalence of overweight and obesity among preschoolers living in the capital of Iran and to determine relationships between overweight and obesity and selected motor- and health-related fitness parameters.
Materials and Methods:
This exploratory cross-sectional study was conducted with 190 boys and 191 girls aged 5−6 years. Study children were selected from the kindergartens in Tehran, the capital of Iran. All children underwent anthropometric, motor- and health-related fitness tests. Height, body mass, body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR) and percentage of body fat (PBF) were measured for anthropometric assessments. Sit-and-reach, modified sit-ups, modified pull-ups, the 4 m × 9 m shuttle run, the 20 m sprint test and the 20 m multistage shuttle run test were measured for motor- and health-related fitness tests. Overweight and obesity prevalence was determined by the International Obesity Task Force, Centers for Disease Control and Prevention and World Health Organization standard criteria.
Results:
International Obesity Task Force criteria indicate almost 12% (23/190) of boys and 22.5% (43/191) of girls were overweight or obese with 4.73% (9/190) of boys and 10.99% (21/191) of girls in the obese category. Significant correlations were found between modified pull-ups test and body mass, BMI, WC, WHR, WHtR, PBF in boys and modified pull-ups and modified sit-ups tests were significantly correlated with body mass, BMI, WC, WHR, WHtR, and PBF in girls. Compared to their counterparts, overweight and obese boys demonstrated inferior performance in modified pull-ups and predicted VO2max and overweight and obese girls demonstrated inferior performance in modified pull-ups, modified sit-ups, 4 m × 9 m agility shuttle run and predicted VO2max
Conclusion:
This study highlighted the relatively high prevalence of overweight and obesity in both genders of preschoolers and found that overweight and obesity were associated with poor fitness performances. The findings provided evidence to support the establishment of tailored physical fitness intervention programs to manage and prevent obesity in preschoolers.
Keywords: Anthropometric measures, body mass index, childhood obesity, physical fitness, preschool children
INTRODUCTION
The prevalence of childhood obesity has increased substantially in developed and developing countries during the last few decades, and it is probable that this trend will continue.[1] As with adults, obesity in childhood causes hypertension, dyslipidemia, chronic inflammation, increased blood clotting tendency, endothelial dysfunction, and hyperinsulinemia.[2,3] The preschool years have been identified as a crucial time to study the determinants of childhood obesity.[4] Not only is it a time when eating and physical activity habits are becoming established,[5] it is also a time period immediately preceding the upswing in body mass index (BMI) known as adiposity rebound.[6] Thus, this has become a major concern among health professionals because child obesity tracks into adulthood[7] and is a strong precursor of an increased all-cause morbidity and mortality in adult life.[8] The International Obesity Task Force (IOTF) has accepted BMI as a consistent, pragmatic (i.e., reasonable although imperfect) index of adiposity in children[9] and has published cut-off points to define overweight and obesity in children and adolescents based on adult BMI ranges.[10] On the other hand, improving physical fitness is a public health priority in developed and developing countries to curb the substantial and growing prevalence of lifestyle-related diseases. Since physical activity is an important factor related to weight control, there is renewed interest in the relationship between physical activity and the body composition of children and adolescents, as well as in the importance of physical activity in maintaining good health and well-being.[4,11,12] While the increasing prevalence of obesity has been reported in all regions of the world, there is a scarce data among Iranian preschoolers. Gaeini et al. studied the prevalence of overweight and obesity in 5-6 years old preschool children using Centers for Disease Control and Prevention (CDC) criteria. They reported that 9.09% of boys, and 9.72% of girls were overweight; 5.26% of boys, and 4.32% of girls were obese.[13]
Iran is an urbanized city-state country in the Middle East Region and is considered to be a country in the nutrition transition. Like most countries that have undergone rapid economic and the demographical transition, noncommunicable diseases, especially cardiovascular disease, are the major causes of mortality and morbidity in Iran with high prevalence reported.[14] Therefore, the present study was designed to:
Provide baseline data on the prevalence of overweight and obesity, using anthropometric measurements in the capital of Iran;
Compare the prevalence of overweight and obesity among preschool-age children using the World Health Organization (WHO), IOTF and CDC standard criteria and to explore the differences in estimates using the three standard criteria;
And determine the relationships between selected motor- and health-related fitness parameters and anthropometric indicators in the study population.
MATERIALS AND METHODS
Participants
This exploratory cross-sectional study was conducted in 2011 on 381 children aged 5-6 years (190 boys, and 191 girls). The sample size was calculated by Cochran formula  based on the study population. n = sample size, N = volume of the statistical population which was equal to 1 million children aged 5-6 years, d = acceptable margin of error which was equal to 0.06, z = value of z for 95% confidence interval, which was = 1.96, (p) (q) are the estimate of variance. Using a multistage cluster random sampling method, 20 kindergartens, as clusters were selected systematically from five geographic regions of Tehran (east, west, north, south, and center). In each cluster (kindergartens), 18-20 children (boys and girls) were selected. The subjects were invited to the appointed health screen center (Tarbiat Modars University) to undergo anthropometric assessments and physical fitness tests. All the parents gave informed consent for their children's participation in the study, whose protocol was approved by the Ethics Committee of the School of Medical Sciences of Tarbiat Modares University and was in accordance with the declaration of Helsinki.
based on the study population. n = sample size, N = volume of the statistical population which was equal to 1 million children aged 5-6 years, d = acceptable margin of error which was equal to 0.06, z = value of z for 95% confidence interval, which was = 1.96, (p) (q) are the estimate of variance. Using a multistage cluster random sampling method, 20 kindergartens, as clusters were selected systematically from five geographic regions of Tehran (east, west, north, south, and center). In each cluster (kindergartens), 18-20 children (boys and girls) were selected. The subjects were invited to the appointed health screen center (Tarbiat Modars University) to undergo anthropometric assessments and physical fitness tests. All the parents gave informed consent for their children's participation in the study, whose protocol was approved by the Ethics Committee of the School of Medical Sciences of Tarbiat Modares University and was in accordance with the declaration of Helsinki.
Anthropometric measures
Data collectors attended a ½-day training session, which provided information on the project and procedures to ensure consistency in measurements. The following anthropometric variables were evaluated in all children: Body mass, height, BMI, waist circumference (WC), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR), sum of two-point skinfolds and percentage of body fat (PBF). Body mass was measured to the nearest 100 g using a calibrated balance beam scale and with the subject standing and wearing only underwear in a private location with same gendered data collectors. For height, children were instructed to stand as straight as possible with his/her back against a wall mounted vertical ruler. Feet were flat on the floor with shoes removed. BMI was calculated as body mass/height squared (kg/m2).[15] Waist and hip circumferences were measured to the nearest mm using a flexible tape. WC was taken at the end of a normal expiration, with the measuring tape positioned at the midway between the lower rib and the iliac crest. The hip circumference was measured at the level of maximal protrusion of the gluteal muscles. WHR was calculated as WC (cm) divided by hip circumference (cm) and WHtR was calculated as WC (cm) divided by height (cm). Skinfold thickness (triceps and calf) was measured in triplicate to the nearest mm, on the right side of the body by Holtain Skinfold Caliper (Holtain Ltd., Crymmych, Dyfed, UK). The mean of three measurements represented the value for each skinfold site. PBF was calculated using the two-site equation.[16]
Definition of overweight and obesity
The prevalence of overweight and obesity was determined using the following methodology and analyzed by gender and age group:
CDC curves:[17] overweight was defined by a BMI >85th percentile but ≤95th percentile, related to gender and age, whereas obesity was defined by a BMI >95th percentile.
IOTF curves:[10] Based on the charts developed by Cole et al. BMI equal to or greater than the value plotted on the gender-related centiles, which crossed a BMI of 25 and 30 kg/m2 at the age of 18, defined overweight and obesity, respectively.
WHO reference charts:[18] Used the devised criteria developed by the WHO to define overweight and obesity. All children whose (body masses were >85th percentiles (body mass or BMI) for age and gender were considered as overweight and >95th percentiles (weight or BMI) for age and gender were considered obese.
Measurement of motor- and health-related fitness abilities
All subjects underwent six motor- and health-related fitness tests. These included sit-and-reach (flexibility), modified sit-ups for 60 s (abdominal muscular endurance), modified pull-ups (upper body strength and endurance), the 4 m × 9 m shuttle run (agility), the 20 m sprint test (maximum running speed) and the 20 m multistage shuttle run test (cardiorespiratory fitness).
Statistical analysis
Means and standard deviations or percentages were calculated for each variable. The Kolmogorov−Smirnov test was used to test the normality of the distribution for each variable before subsequent analyses were performed. The Chi-square test was used to compare the prevalence of overweight and obesity between the different criteria. Independent t-tests and one-way analysis of variances were used to compare variables between two groups (for instance, boys and girls) and for more than two groups, respectively. When a significant difference was revealed, the Tukey's post-hoc test was used to specify where the difference occurred. Cohen's kappa statistic was calculated to determine the level of agreement between the standard criteria. A κ > 0.80 signified very good agreement, between 0.60 and 0.80 signified a good level of agreement and <0.50 signified little to moderate agreement. Bivariate correlation coefficients were calculated to investigate associations between anthropometric variables and motor- and health-related fitness tests. All tests for statistical significance were two-tailed and performed assuming a type I error probability of ≤0.05. Data were analyzed using SPSS software package (SPSS for Windows; SPSS Inc., Chicago, IL, USA; Version 16.00).
RESULTS
Anthropometric data for boys and girls are provided in Table 1. Boys were slightly taller than girls (P < 0.01). Irrespective of BMI criteria, girls had a higher prevalence of overweight and obesity than boys [Table 2]. Based on IOTF reference, almost 12% (23/190) of boys and 22.5% (43/191) of girls were either overweight or obese with 4.73% (9/190) of boys and 10.99% (43/191) of girls in the obese category; whereas based on the CDC criterion, 5.78% (11/190) of boys and 12.04% (23/191) of girls were overweight and 7.36% (14/190) of boys and 9.42% (18/191) of girls were obese. Moreover, there was a significant gender difference in the prevalence of obesity based on the IOTF criteria (χ2 = 7.72; P = 0.021) that was absent in the other criteria.
Table 1.
Anthropometric variables in 5-6 years old preschool children in the capital of Iran
![]()
Table 2.
Prevalence of overweight and obesity in 5-6 years old preschool children in the capital of Iran using the IOTF, WHO, and CDC BMI criteria
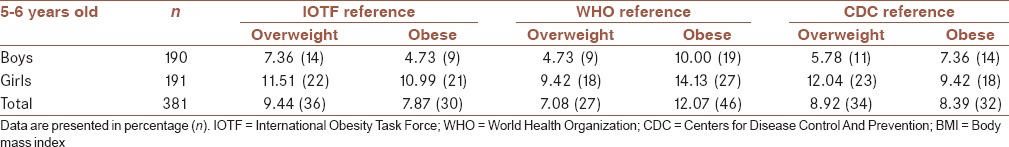
In this study, the CDC and the IOTF demonstrated the highest level of agreement, very well (kappa = 0.896). In addition, the level of agreements between the IOTF and the WHO (κ = 0.792) and the WHO and the CDC (κ = 0.808) were found to be good.
Body mass, WC, BMI, WHtR, and PBF were strongly correlated to each other in both sexes (boys: r = 0.539−886, P < 0.001; girls: r = 0.599−898, P < 0.001; data not shown in Tables), suggesting that measures of obesity based on these parameters will provide comparable information. However, WHR showed the weakest correlation with the other anthropometric measurements in both sexes.
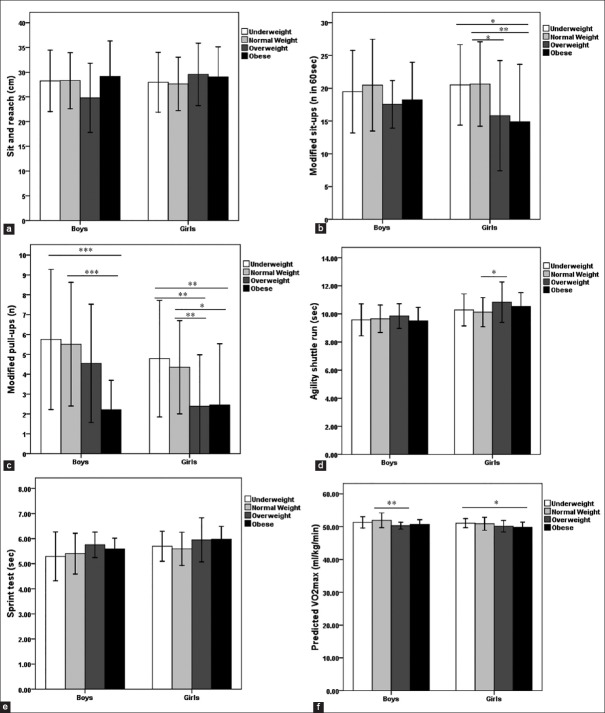
Values of motor- and health-related fitness tests are presented in Table 3 and Figure 1. Boys were better performers than girls in modified pull-ups, agility, and sprint test. In addition, they had higher predicted VO2max than girls (P < 0.001). Overweight and obese children, compared to their underweight and normal-weight counterparts, demonstrated inferior performance in modified pull-ups and predicted VO2max. Moreover, normal-weight girls had better performance than overweight and obese counterparts in modified sit-ups and agility shuttle run [Figure 1].
Table 3.
Values of motor- and health-related fitness tests in 5–6 years old preschool children in the capital of Iran
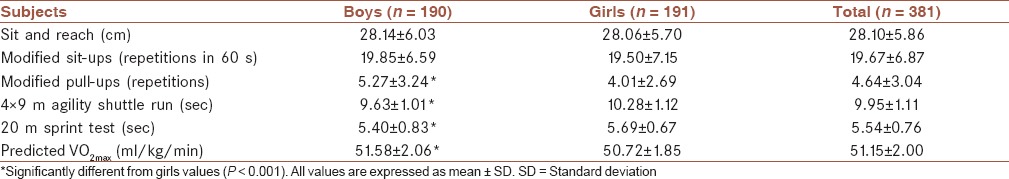
Figure 1.
Differences in motor- and health-related fitness tests among body mass index categories by gender. (a) Sit-and-reach. (b) Modified sit-ups. (c) Modified pull-ups. (d) Agility shuttle run. (e) Sprint test. (f) Predicted VO2max. Values significantly different at P < 0.05 (*), P < 0.01 (**) and P < 0.001 (***)
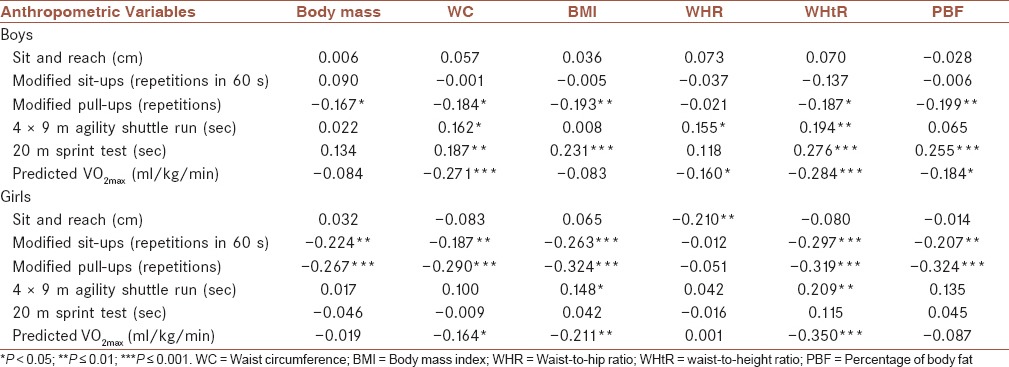
In boys, significant correlations were found between WC, BMI, WHtR and PBF on the one hand and modified pull-ups, sprint test, and predicted VO2max on the other hand [P ≤ 0.01; Table 4]. There were stronger correlations between anthropometric measurements and fitness parameters in girls: BMI, WHtR, and PBF had significant correlations with modified sit-ups, modified pull-ups and predicted VO2max [P ≤ 0.01; Table 4].
Table 4.
Correlation coefficients among anthropometric measures and motor- and health-related fitness abilities in boys and girls
DISCUSSION
Alarming trends in childhood obesity even among preschoolers have drawn attention to the health of this age group.[19] Unhealthy diets and physical inactivity are the main contributors to overweight and obesity, which are among the leading risk factors for major noncommunicable diseases.[14] Obesity in childhood often continues into adulthood,[20] and causes a wide range of serious complications such as increases in the risk of premature illness and death later in life.[3] Evidence indicates that many Iranian children are at risk for these complications. For instance, a high prevalence of metabolic syndrome among Iranian adolescents has been reported (boys: 10.3%; girls: 9.9%).[21] Because of their public health importance, the trends in child obesity should be closely monitored.
In the present study, the IOTF and the CDC demonstrated a very good level of agreement (κ = 0.896) in Iranian preschoolers. Among the BMI reference criteria, the WHO reference provided higher estimates of obesity [Table 2] which is consistent with a previous study.[22] The prevalence of overweight, as defined by the IOTF, was 7.36% and 11.51%, and the prevalence of obesity was 4.73% and 10.99% in boys and girls, respectively [Table 2]. In general, obesity was higher among girls; this is mostly the case in developing countries as well as in developed ones.[1] A survey was carried out on children aged 4-5 years old in two largely rural provinces of Iran using the IOTF criteria and reported a higher prevalence of overweight (boys: 17.6% and girls: 19.0%), but lower prevalence of obesity (boys: 7.1% and girls: 7.8%) compared with our results for overweight (boys: 7.36% and girls: 11.51%) and obesity (boys: 4.73% and girls: 10.99%).[23] In another study on children aged 6-year-old in three regions of Iran using CDC criteria, 12.8%, 13.5%, and 10.9% were overweight and 3.4%, 3.5%, and 3.4% were obese in 2007, 2008 and 2009, respectively.[24] In Northern Quebec, in children aged 5 years, the prevalence of overweight using IOTF was 31.6% (28.2% for boys and 35.0% for girls) and the corresponding prevalence based on CDC was 27.5% (23.8% for boys and 31.2% for girls)[25] which was much higher than our results [Table 2].
The increased prevalence of obesity internationally is associated with improved affluence and the intense process of urbanization, often characterized by less active lifestyles. Iran is an urbanized city-state country in the Middle East Region and is considered to be a country in the nutrition transition. Like most countries that have undergone rapid economic and demographic transition, noncommunicable diseases are the major cause of mortality and morbidity in Iran with a high prevalence reported.[14] However, the prevalence of obesity in Iranian preschoolers is not as serious as in some western countries. In a study conducted in six cities of northeast China, according to the IOTF reference, 10.29% of the 5-year-old children were overweight, and 3.85% were obese. The CDC reference classified 11.22% as overweight and 8.39% as obese.[22] Indeed, overweight and obesity rates in our sample are similar to those observed by Ma et al. A study carried out on children aged 2-5 years old in urban regions of India using the IOTF criteria reported a lower prevalence of overweight (boys: 6.8%; girls: 7.0%) and obesity (boys: 3.9%; girls: 2.4%) compared with our findings.[20] However, compared to Western countries that applied the same methods to define overweight and obesity, the prevalence rates in our study sample are lower.[25,26]
Regular physical activity is necessary for normal growth and the development of functional qualities such as aerobic capacity, muscle strength, flexibility and motor skills.[11] Studies indicated that the positive energy balance causing overweight was due possibly to low energy expenditure (i.e., low physical activity levels).[27,28] Regarding the influence of childhood obesity on fitness profile, the results of the present study revealed that overweight and obesity were associated with poorer cardiorespiratory and motor fitness, especially in girls. More specifically, overweight and obese children, compared to their underweight and normal-weight counterparts, demonstrated inferior performance in most studied parameters [Figure 1].
In this study, we compared the correlations between six obesity parameters (body mass, WC, BMI, WHR, WHtR, and PBF) and selected physical fitness parameters [Table 4]. Of all physical fitness parameters in this study, when adjustments were made for weight, there were significant correlations between the 20 m sprint test, predicted VO2max and most of the anthropometric indices in boys and there were significant correlations between modified sit-ups, predicted VO2max and most of the anthropometric indices in girls; however, the correlations were more pronounced in girls (data not shown in Table 4). Our findings are consistent with studies conducted among schoolchildren, showing that overweight and obesity was inversely related to several components of motor- and health-related fitness parameters.[29,30] Enhanced fitness performance mostly reflects the level of habitual physical activity. Indeed, studies in children have indicated that high physical fitness scores, especially high levels of cardiorespiratory fitness, are associated with increased levels of physical activity.[27,31] Trost et al. showed overweight 3–5-year-old boys to be significantly less active than nonoverweight peers during the preschool day. They suggested that a significant proportion of overweight children might be at increased risk for further gains in adiposity because of low levels of physical activity during the preschool day.[4] Children become overweight or obese because of the inactivity or vice versa. Obesity impairs the child's physical activity successes in agility, endurance, etc., that is discouraging to most children and may be embarrassing or a source of ridicule by others. Consequently, the significant differences in fitness performance observed between under/normal-weight and overweight/obese children could be partially attributed to differences in physical activity levels.[29] It has been shown that lower aerobic fitness results in greater adiposity gain in growing prepubertal children. This finding emphasizes the importance of increasing or maintaining aerobic fitness as an intervention for preventing the development of obesity in children. In addition to being protective against fat gain, aerobic fitness may also reduce the risk for CVD and diabetes.[32]
CONCLUSION
The study highlighted the relatively high prevalence of overweight and obesity in both genders of preschoolers as defined by the IOTF, CDC and WHO criteria and provided evidence to support the establishment of physical activity intervention programs to prevent weight problems in preschoolers, thus potentially reducing obesity-related disorder like metabolic syndrome. Overweight and obesity were indicative of poor physical fitness in both genders though genders were found to have different types of deficits. Regular physical activity is necessary for normal growth and the development of functional qualities such as aerobic capacity and motor skills. These findings emphasize the importance of increasing or maintaining aerobic fitness as an intervention for preventing the development of obesity in preschoolers.
Child obesity rates have increased in Iran and poor cardiovascular fitness of urban children is likely associated with low physical activity levels in this population. There is a direct relationship between physical activity and weight status, as well as between physical fitness and cardiovascular health among school-age children.[33] Data from many studies suggested decreases in physical activity among children over the past decade.[34] Therefore, it is critical to design effective interventions for increasing physical activity and improving physical fitness in order to prevent/reduce obesity among urban children. Boys and girls differ in their attitudes and beliefs regarding physical activity[35] as well as their motivation for[36] and barriers to.[37] Thus, classroom teachers and other professionals working with children should focus on incorporating a variety of fun and creative activities, in addition to structured and/or organized sports, into classroom activities, physical education classes and after school programs.[33] Therefore, providing expanded and enhanced health curricula regarding nutrition and physical activity in kindergartens may help children consider, adopt, and maintain healthier diets and more physically active habits throughout their lifetimes.
AUTHOR'S CONTRIBUTIONS
HAA carried out the design, coordinated the study, and revised the manuscript. BA has made substantial contributions to the acquisition of data and analysis and drafted the manuscript. MS coordinated and carried out all the experiments. SK coordinated and carried out all the experiments. BLH has been involved in critically revising the manuscript. MP provided assistance in the design of the study.
ACKNOWLEDGMENTS
This study was supported by I.R. Iran association of sports, aerobics, and fitness. We would like to acknowledge the study participants and field workers for their participation in the hard work of this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. (1-253).World Health Organ Tech Rep Ser. 2000;894:i–xii. [PubMed] [Google Scholar]
- 2.Reilly JJ. Descriptive epidemiology and health consequences of childhood obesity. Best Pract Res Clin Endocrinol Metab. 2005;19:327–41. doi: 10.1016/j.beem.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: Public-health crisis, common sense cure. Lancet. 2002;360:473–82. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 4.Trost SG, Sirard JR, Dowda M, Pfeiffer KA, Pate RR. Physical activity in overweight and nonoverweight preschool children. Int J Obes Relat Metab Disord. 2003;27:834–9. doi: 10.1038/sj.ijo.0802311. [DOI] [PubMed] [Google Scholar]
- 5.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–49. [PubMed] [Google Scholar]
- 6.Whitaker RC, Pepe MS, Wright JA, Seidel KD, Dietz WH. Early adiposity rebound and the risk of adult obesity. Pediatrics. 1998;101:E5. doi: 10.1542/peds.101.3.e5. [DOI] [PubMed] [Google Scholar]
- 7.Togashi K, Masuda H, Rankinen T, Tanaka S, Bouchard C, Kamiya H. A 12-year follow-up study of treated obese children in Japan. Int J Obes Relat Metab Disord. 2002;26:770–7. doi: 10.1038/sj.ijo.0801992. [DOI] [PubMed] [Google Scholar]
- 8.Crawford PB, Story M, Wang MC, Ritchie LD, Sabry ZI. Ethnic issues in the epidemiology of childhood obesity. Pediatr Clin North Am. 2001;48:855–78. doi: 10.1016/s0031-3955(05)70345-x. [DOI] [PubMed] [Google Scholar]
- 9.Bellizzi MC, Dietz WH. Workshop on childhood obesity: Summary of the discussion. Am J Clin Nutr. 1999;70:173S–5. doi: 10.1093/ajcn/70.1.173s. [DOI] [PubMed] [Google Scholar]
- 10.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raustorp A, Pangrazi RP, Ståhle A. Physical activity level and body mass index among schoolchildren in south-eastern Sweden. Acta Paediatr. 2004;93:400–4. [PubMed] [Google Scholar]
- 12.Fulton JE, Burgeson CR, Perry GR, Sherry B, Galuska DA, Alexander MP, et al. Assessment of physical activity and sedentary behavior in preschool-age children: Priorities for research. Pediatr Exerc Sci. 2001;13:113–26. [Google Scholar]
- 13.Gaeini A, Kashef M, Samadi A, Fallahi A. Prevalence of underweight, overweight and obesity in preschool children of Tehran, Iran. J Res Med Sci. 2011;16:821–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:5. doi: 10.1186/1745-6215-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gharakhanlou R, Farzad B, Agha-Alinejad H, Steffen LM, Bayati M. Anthropometric measures as predictors of cardiovascular disease risk factors in the urban population of Iran. Arq Bras Cardiol. 2012;98:126–35. doi: 10.1590/s0066-782x2012005000007. [DOI] [PubMed] [Google Scholar]
- 16.Slaughter MH, Lohman TG, Boileau RA, Horswill CA, Stillman RJ, Van Loan MD, et al. Skinfold equations for estimation of body fatness in children and youth. Hum Biol. 1988;60:709–23. [PubMed] [Google Scholar]
- 17.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 18.WHO Multicentre Growth Reference Study Group. Geneva: World Health Organization; 2006. WHO child growth standards: Length/height-for-age, weight-for-age, weight-for length, weight-for-height and body mass index-for-age: Methods and development. [Google Scholar]
- 19.Timmons BW, Naylor PJ, Pfeiffer KA. Physical activity for preschool children — How much and how? Can J Public Health. 2007;98(Suppl 2):S122–34. [PubMed] [Google Scholar]
- 20.Khadilkar VV, Khadilkar AV, Cole TJ, Chiplonkar SA, Pandit D. Overweight and obesity prevalence and body mass index trends in Indian children. Int J Pediatr Obes. 2011;6:e216–24. doi: 10.3109/17477166.2010.541463. [DOI] [PubMed] [Google Scholar]
- 21.Esmaillzadeh A, Mirmiran P, Azadbakht L, Etemadi A, Azizi F. High prevalence of the metabolic syndrome in Iranian adolescents. Obesity (Silver Spring) 2006;14:377–82. doi: 10.1038/oby.2006.50. [DOI] [PubMed] [Google Scholar]
- 22.Ma YN, Chen T, Wang D, Liu MM, He QC, Dong GH. Prevalence of overweight and obesity among preschool children from six cities of northeast China. Arch Med Res. 2011;42:633–40. doi: 10.1016/j.arcmed.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 23.Dorosty AR, Siassi F, Reilly JJ. Obesity in Iranian children. Arch Dis Child. 2002;87:388–91. doi: 10.1136/adc.87.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Motlagh ME, Kelishadi R, Ziaoddini H, Mirmoghtadaee P, Poursafa P, Ardalan G, et al. Secular trends in the national prevalence of overweight and obesity during 2007-2009 in 6-year-old Iranian children. J Res Med Sci. 2011;16:979–84. [PMC free article] [PubMed] [Google Scholar]
- 25.Willows ND, Johnson MS, Ball GD. Prevalence estimates of overweight and obesity in Cree preschool children in northern Quebec according to international and US reference criteria. Am J Public Health. 2007;97:311–6. doi: 10.2105/AJPH.2005.073940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edwards J, Evans J, Brown AD. Using routine growth data to determine overweight and obesity prevalence estimates in preschool children in the Capital Health Region of Alberta. Can J Public Health. 2008;99:91–4. doi: 10.1007/BF03405451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koutedakis Y, Bouziotas C, Flouris AD, Nelson PN. Longitudinal modeling of adiposity in periadolescent Greek schoolchildren. Med Sci Sports Exerc. 2005;37:2070–4. doi: 10.1249/01.mss.0000178099.80388.15. [DOI] [PubMed] [Google Scholar]
- 28.Rocandio AM, Ansotegui L, Arroyo M. Comparison of dietary intake among overweight and non-overweight schoolchildren. Int J Obes Relat Metab Disord. 2001;25:1651–5. doi: 10.1038/sj.ijo.0801793. [DOI] [PubMed] [Google Scholar]
- 29.Tokmakidis SP, Kasambalis A, Christodoulos AD. Fitness levels of Greek primary schoolchildren in relationship to overweight and obesity. Eur J Pediatr. 2006;165:867–74. doi: 10.1007/s00431-006-0176-2. [DOI] [PubMed] [Google Scholar]
- 30.Deforche B, Lefevre J, De Bourdeaudhuij I, Hills AP, Duquet W, Bouckaert J. Physical fitness and physical activity in obese and nonobese Flemish youth. Obes Res. 2003;11:434–41. doi: 10.1038/oby.2003.59. [DOI] [PubMed] [Google Scholar]
- 31.Huang YC, Malina RM. Physical activity and health-related physical fitness in Taiwanese adolescents. J Physiol Anthropol Appl Human Sci. 2002;21:11–9. doi: 10.2114/jpa.21.11. [DOI] [PubMed] [Google Scholar]
- 32.Johnson MS, Figueroa-Colon R, Herd SL, Fields DA, Sun M, Hunter GR, et al. Aerobic fitness, not energy expenditure, influences subsequent increase in adiposity in black and white children. Pediatrics. 2000;106:E50. doi: 10.1542/peds.106.4.e50. [DOI] [PubMed] [Google Scholar]
- 33.Shriver LH, Harrist AW, Hubbs-Tait L, Topham G, Page M, Barrett A. Weight status, physical activity, and fitness among third-grade rural children. J Sch Health. 2011;81:536–44. doi: 10.1111/j.1746-1561.2011.00624.x. [DOI] [PubMed] [Google Scholar]
- 34.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl 4):S229–53. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 35.Vilhjalmsson R, Kristjansdottir G. Gender differences in physical activity in older children and adolescents: The central role of organized sport. Soc Sci Med. 2003;56:363–74. doi: 10.1016/s0277-9536(02)00042-4. [DOI] [PubMed] [Google Scholar]
- 36.Wilson DK, Williams J, Evans A, Mixon G, Rheaume C. Brief report: A qualitative study of gender preferences and motivational factors for physical activity in underserved adolescents. J Pediatr Psychol. 2005;30:293–7. doi: 10.1093/jpepsy/jsi039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tergerson JL, King KA. Do perceived cues, benefits, and barriers to physical activity differ between male and female adolescents? J Sch Health. 2002;72:374–80. doi: 10.1111/j.1746-1561.2002.tb03562.x. [DOI] [PubMed] [Google Scholar]