Abstract
Background:
Fractures of the distal third of the tibia are mostly associated with a fibular fracture that often requires fixation. The preferred treatment of distal tibial fracture is the minimally invasive percutaneous plate osteosynthesis (MIPPO) procedure. However, there are no clear cut guidelines on fixation of the fibular fracture and currently most orthopedic surgeons use a plate osteosynthesis for the fibula as well. A common complication associated with dual plating is an increased chance of soft tissue necrosis, infection, and in some cases resulting in an exposed implant. We conducted a prospective study to analyze the results of fractures of the distal in both leg bones managed by the MIPPO procedure for tibial fractures and a rush nail for fibular fractures.
Methods:
The study was conducted in a tertiary care hospital from November 2012 to May 2014, a total of 30 fractures in 30 patients (18 males, 12 females) with a mean age of 42.4 years (26-60 years) were treated in our institution in the aforesaid time period with MIPPO for tibia and rush nail for fibular fractures. All the cases were operated on by a single surgeon in emergency within 24 hours. The patients with skin blistering and compound fractures were excluded from this study. Rehabilitative measures were proceeded as per patient’s pain profile, isometric and isotonic exercises were started on the first post-operative day, with full weight bearing at 10-12 weeks after assessing clinical and radiological union. Regular follow up of patients was done, radiographs were taken at the immediate post-operative period and at 3, 6, 12 and 24 weeks.
Results:
All the patients were available for regular follow up. Radiological and clinical union proceeded normally in all the patients, no patients had signs of any deep infection, delayed union or nonunion, three patients had a superficial infection of the tibial incision that healed with a change in antibiotic.
Conclusions:
The use of dual plating for fixation of the lower tibia and fibula fractures is often associated with soft tissue complications, exposed implant, and increased risk of infection. We conclude that in fractures of the distal tibia and fibula it is better to use a rush nail for the fibula with a concurrent MIPPO for the tibia for the reasons cited above. Moreover, with the use of rush nail the cost of implant is also reduced, which is a very important factor in developing countries.
Key words: Distal fibula, Dual plating, Rush nail
Introduction
Fracture of the distal tibia accounts for 7 to 9% of lower extremity fractures, with the fibula fractured in about 85% of these cases (1-4). The fracture of the distal tibia occurs by either a low energy mechanism like rotational strain or a high energy mechanism like road traffic accidents or a fall from heights (4). The management of the distal tibia and fibula fracture is decided based on amount of swelling, blisters, and open wounds. The closed distal tibia and fibula fracture without excessive swelling, blistering, and compound injures are treated with dual plating with a locking plate through MIPPO in the tibia fracture and plating for the fibula fracture through the posterolateral approach. There is a high rate of superficial wound infection, wound dehiscence, implant exposure, and delayed or nonunion in patients treated with dual plating in these fractures (5-7). Rush nail is a better alternative for fibular fixation because it requires a smaller incision and less soft tissue dissection (8-9). It also affords better mechanical stability in osteoporotic bone and has the potential to reduce the incidence of complications (10). Favorable short term outcomes of rush nailing have been reported in small numbers of patients (8,11-12). We hypothesized that by using AO plating in the distal tibia through MIPPO and rush nail in the fibula fracture, ankle stability can be achieved and complications of dual plating can be avoided in these fractures.
Methods
A prospective study on 30 patients with a fracture of both distal leg bones was conducted in GMC Jammu from November 2012 to May 2014. The inclusion criteria included a fracture of both distal leg bones, patients of any sex who were more than 20 years old, and fractures associated with moderate swelling and no blisters. The fractures with blisters - especially over medial aspect, open wounds, associated talar and calcaneal fractured - were excluded from the study. Patients’ history with mode and mechanism of injury were noted. In the examination the following were noted: swelling of the ankle, blister, open wounds, and neurovascular status. Radiographs of the leg and ankle were taken in AP, lateral and Mortise view. The fractures of the tibial plafond are classified by Reudi-Allgower and AO/OTA classifications. We used the AO classification to classify the tibial plafond fractures. The fractures are classified into extra-articular, partial articular, and articular fractures. Further classifications are type A that includes extra-articular distal tibial fractures; type B that includes partial articular fractures in which a portion of the articular surface remains in continuity with the shaft, and type C with a complete metaphyseal fracture with articular involvement. The patients’ general conditions like obesity or history of smoking or alcohol intake and comorbidities like diabetes or neuropathy status were also noted and informed written consent was obtained from all the patients. The treatment plan, cost of operation, hospital stay, and possible complications of the surgery were explained to the patients and attendants in detail. Complications include superficial wound infection, wound dehiscence, implant exposure/failure, delayed or nonunion, ankle instability, and permanent ankle stiffness. Patients were assessed at 3, 6, 12, and 24 weeks for clinical and radiological evidence of bone healing.
Surgical technique
The patients were operated on under spinal/epidural anesthesia. The pre-op antibiotics were given 30 minutes before surgery. The patient was placed supine on a radiolucent table. A bump was placed under the ipsilateral hip to internally rotate the affected limb and to provide easier access to the lateral side of the ankle. A pneumatic tourniquet was applied and inflated after the entire limb was prepared and draped. For fixation of the fibular fracture a small incision starting ~2 cm proximal and extending to the tip of the lateral malleolus was given, after careful dissection of the soft tissue, the tip of the lateral malleolus was exposed and using a 2.7 mm drill bit, a portal was made into the medullary cavity of the distal fragment of the fibula. A rush nail of appropriate size was put initially into the distal fragment only, by doing so we were able to control the distal segment and it was reduced to proximal fragment under C-arm control. Once the fracture was reduced the nail was advanced into the proximal fragment. The fracture was reduced in a closed manner under C-arm control in all the patients and we did not perform a mini open technique for reduction in any case. The size of the rush nail varied upon the medullary cavity and location of the fracture. In the next step, the distal tibial fracture was then approached through the anteromedial incision of 5 cm at the distal part by the MIPPO technique. The fracture was reduced and stabilized with a locking compression plate. Postoperatively, the patient was put on IV antibiotics for three days and then on oral antibiotics for another five days. Stitch removal was done on the twelfth postop day. Isometric and isotonic exercises were started on the first post-operative day. Patients were assessed clinically for wound infection, wound dehiscence, and ankle instability. They were also assessed radiographically for delayed or nonunion and implant failure. Radiographs were taken immediately on postop day and then at 3, 6, 12 and 24 weeks [Figure 1] a and b [Figure 2] a, b and c. Partial weight bearing was started at 6-8 weeks and full weight bearing at 12-14 weeks. The weight bearing status was decided on the basis of clinical and radiological signs of healing.
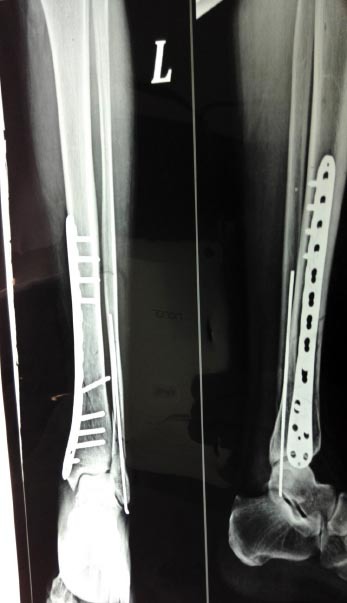
Figure 1.

(a). PreOp Radiograph of patient showing comminuted extraarticular fracture tibia with fractured fibula.
(b). immediate Post op radiograph showing an intramedullary nail for fibula and plate for tibia.
Figure 2.

(a). Preop radigraph of another patient.
(b). 4 week Post op radiograph of the same patient.
(c). 12 months post op radiograph of same patient.
Results
All the 30 patients (mean age: 42.4; 18 males and 12 females) were available for regular follow up until 6 months. Demographics and data on laterality is given in Table 1 & 2. The most number of patients were in the age group of 35-50 years. The fractures were classified according to OTA classification, there were 14 patients belonging to type A (46.67%), 11 cases of type B (36.67%) and 5 cases were classified as type C fractures (16.7%). Road traffic accidents were the leading cause of fractures in our series [Table 3]. There were three patients with diabetes and so they were started on insulin injections. Seven patients were smokers and were encouraged to either cut back or stop smoking altogether. There were three patients who developed superficial wound infection at the tibial incision and they were treated with a change of antibiotics after doing a culture sensitivity report. No patient had ankle stiffness or developed deep infection/osteomyelitis or wound dehiscence or any case of ankle instability. All patients started full weight bearing at 12-14 weeks. The average time to union of the tibial plafond was found to be 19 weeks with a range of 16-24 weeks. There was no case of nonunion in our series; however, two cases of delayed union were seen. The average time to union in the fibula was 14 weeks in our study with the shortest being 12 weeks and the longest was 16 weeks. There was no case of delayed union or nonunion in case of fibular fracture in our series. The rest of the postop period was uneventful in all the other patients.
Table 1.
Demographic Data
| Age in years | Males | Females |
|---|---|---|
| 20-35 | 6(20%) | 2(6.66%) |
| 35-50 | 9(30%) | 5(16.66%) |
| >50 | 3(10%) | 5(16.66) |
| Total | 18(60%) | 12(40%) |
Table 2.
Side of injury
| Side | No of patients | percentage |
|---|---|---|
| Right | 19 | 63.33% |
| Left | 11 | 36.66% |
Table 3.
Mode of trauma
| Injury | No of patients | Percentage |
|---|---|---|
| Road traffic accident | 22/30 | 73.33% |
| Slips and twisting injury | 6/30 | 20% |
| Others | 2/30 | 6.66% |
Discussion
Fractures of the tibial plafond constitute about 10% of all lower extremity fractures. The fracture can be caused by low energy rotational forces or high energy axial force. They are often associated with severe, closed soft tissue trauma or open injuries (13). Different methods of treatment includes plaster cast immobilization, lag screw fixation, ORIF with plates and external fixation with or without limited internal fixation for distal tibial fractures, and ORIF with plates for distal tibial fractures.
The average time to union of the tibia plafond was found to be 19 weeks in our study with a range of 16-24 weeks, superficial wound infection in three (10%) patients and 2 (6.67%) cases of delayed union were reported in our study. Borg et al. studied 21 patients with tibial plafond fractures and noted that the average time to union was 5.44 months, postop infection developed in 14.3% of patients and delayed/non-union in 19% patients (18). Bahari et al. in 42 patients noted union in 22.4 weeks, postop infection was reported in 7.14% patients and delayed union in 5.3% patients (19). Redfern et al. studied 20 patients and noted that the average time to union was 23 weeks, postop infection was reported in 5% patients, and no case of non union (20). Lau et al. noted the average time to union 18.7 weeks, postop infection was reported in 16.7% patients and delayed/non-union in 10.4% patients (21).
Reudi and Allgower treated 75 patients with open reduction and internal fixation with a medial buttress plate for the tibial plafond fracture and fibular fracture was stabilized with plates. They reported good or excellent results, but lately satisfactory results have been found in only 82%, 37% and 40% respectively in type 1, type 2 and type 3 fractures. Infection rate after type 3 fractures have been reported as high as 37% (13). Mcferran et al. reported 54% incidence of local complications in fractures treated with plates and screws in both the tibia and fibula. Borens et al. reported excellent to good results in those fractures treated with reduction and plating through the MIPPO technique (14). A study of 37 patients had encouraging results with a mean Olerud and Molander score (OMS) of 87, a good radiological outcome in 97%, and a low complication rate; with only one case of loss of fixation and two with infection (15).
Appleton et al. noted average union time in fibula fractures of 110.68 days and nonunion in 4 cases (5.12%) and delayed union in 5 cases ( 6.41%). The average time to union in the fibula was 14 weeks in our study with the shortest being 12 weeks and the longest being 16 weeks. There was no case of delayed or nonunion in our series.
The use of the dual plating technique has been associated with increased soft tissue complications like local wound infections and wound necrosis, which, in some cases, required free tissue transfer to salvage the limb [Figure 3]. The complication rate following ORIF for fibula in the elderly is up to 40% (15). Tenny and Wiss evaluated tibial plafond fractures treated with open reduction and plate fixation noting poor results in 50% of the cases with 37% developing deep infection (22). It is also considerably higher in patients with systemic diseases, particularly diabetes and neuropathy and in those with compromised local soft tissues and those who smoke (16,17). In our series there were no local complications pertaining to the fibular fracture, no superficial or deep infection highlighting the importance of using the minimally invasive approach, and using an intramedullary nail. The MIPPO technique avoids much soft tissue dissection and subsequently less chances of local wound complications and bone healing problems. Rush nail is excellent in achieving reduction of the fracture and avoids much soft tissue complications. We have concluded in our study that the use of rush nail in the fibula to achieve stability, and reduction of the distal tibial fracture using the medial buttress plate through the MIPPO technique is a good method in simple, closed fractures of both the distal leg bones [Figure 4]. This technique reduces the chances of local wound complications and bone healing can subsequently improve.
Figure 3.

Exposed implant, seen in a patient of distal tibia & fibula fracture managed by dual plating.
Figure 4.
Radiograph showing stable fixation of fracture with a plate and rush nail.
References
- 1.Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures: An increasing problem? Acta Orthop. 1998;69(1):43–7. doi: 10.3109/17453679809002355. [DOI] [PubMed] [Google Scholar]
- 2.Koval KJ, Lurie J, Zhou W, Sparks MB, Cantu RV, Sporer SM, et al. Ankle fractures in the elderly: What you get depends on where you live and who you see. J Orthop Trauma. 2005;19(9):635–9. doi: 10.1097/01.bot.0000177105.53708.a9. [DOI] [PubMed] [Google Scholar]
- 3.Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Increasing number and incidence of low-trauma ankle fractures in elderly people: Finnish statistics during 1970-2000 and projections for the future. Bone. 2002;31(3):430–3. doi: 10.1016/s8756-3282(02)00832-3. [DOI] [PubMed] [Google Scholar]
- 4.Canale ST, Beaty JH. Campbell operative orthopedics. 12th ed. Maryland Heights, Missouri: Mosby; 2013. [Google Scholar]
- 5.Höiness P, Engebretsen L, Strömsöe K. The influence of perioperative soft tissue complications on the clinical outcome in surgically treated ankle fractures. Foot Ankle Int. 2001;22(8):642–8. doi: 10.1177/107110070102200805. [DOI] [PubMed] [Google Scholar]
- 6.McKenna PB, O›Shea K, Burke T. Less is more: Lag screw only fixation of lateral malleolar fractures. Int Orthop. 2007;31(4):497–502. doi: 10.1007/s00264-006-0216-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beauchamp CG, Clay NR, Thexton PW. Displaced ankle fractures in patients over 50 years of age. J Bone Joint Surg Br. 1983;65(3):329–32. doi: 10.1302/0301-620X.65B3.6404905. [DOI] [PubMed] [Google Scholar]
- 8.Appleton P, McQueen M, Court-Brown C. The fibula nail for treatment of ankle fractures in elderly and high risk patients. Tech Foot Ankle. 2006;5(3):204–8. [Google Scholar]
- 9.Lee YS, Huang HL, Lo TY, Huang CR. Lateral fixation of AO type-B2 ankle fractures in the elderly: The Knowles pin versus the plate. Int Orthop. 2007;31(6):817–21. doi: 10.1007/s00264-006-0260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith G, Wallace R, Findlater G, White T. Gothenburg: Procs Seventh SICOT/SIROT Anuual International Conference; 2010. The fibular nail: A biomechanical study. [Google Scholar]
- 11.Ramasamy PR, Sherry P. The role of a fibular nail in the management of Weber type B ankle fractures in elderly patients with osteoporotic bone: A preliminary report. Injury. 2001;32(6):477–85. doi: 10.1016/s0020-1383(01)00030-4. [DOI] [PubMed] [Google Scholar]
- 12.Rajeev A, Senevirathna S, Radha S, Kashayap NS. Functional outcomes after fibula locking nail for fragility fractures of the ankle. J Foot Ankle Surg. 2011;50(5):547–50. doi: 10.1053/j.jfas.2011.04.017. [DOI] [PubMed] [Google Scholar]
- 13.Rüedi T. Fractures of the lower end of the tibia into the ankle joint: results 9 years after open reduction and internal fixation. Injury. 1973;5(2):130–4. doi: 10.1016/s0020-1383(73)80089-0. [DOI] [PubMed] [Google Scholar]
- 14.Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL, Borens O, Kloen P, Richmond J, et al. Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg. 2009;129(5):649–59. doi: 10.1007/s00402-006-0219-1. [DOI] [PubMed] [Google Scholar]
- 15.Anderson SA, Li X, Franklin P, Wixted JJ. Ankle fractures in the elderly: Initial and long-term outcomes. Foot Ankle Int. 2008;29(12):1184–8. doi: 10.3113/FAI.2008.1184. [DOI] [PubMed] [Google Scholar]
- 16.Nåsell H, Ottosson C, Törnqvist H, Lindé J, Ponzer S. The impact of smoking on complications after operatively treated ankle fractures: A follow-up study of 906 patients. J Orthop Trauma. 2011;25(12):748–55. doi: 10.1097/BOT.0b013e318213f217. [DOI] [PubMed] [Google Scholar]
- 17.Wukich DK, Joseph A, Ryan M, Ramirez C, Irrgang JJ. Outcomes of ankle fractures in patients with uncomplicated versus complicated diabetes. Foot Ankle Int. 2011;32(2):120–30. doi: 10.3113/FAI.2011.0120. [DOI] [PubMed] [Google Scholar]
- 18.Borg T, Larsson S, Lindsjo U. Percutanous plating of distal tibial fractures- preliminary results in 21 patients. Injury. 2004;35(6):608–14. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 19.Bahari S, Lenehan B, Khan H, McElwain JP. Minimally invasive percutaneous plate fixation of distal tibia fractures. Acta Orthop Belg. 2007;73(5):635–40. [PubMed] [Google Scholar]
- 20.Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimal invasive plate osteosynthesis. Injury. 2004;35(6):615–20. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32(5):697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993;292:108–17. [PubMed] [Google Scholar]


