Abstract
Background:
Sternocostoclavicular joint (SCCJ) swelling is an underdiagnosed, albeit important entity in clinical practice. The present study was conducted in order to identify the incidence and common causes of this entity.
Methods:
Patients presenting to the Orthopaedic Clinic with a swelling of the sternocostoclavicular joint, during the study period of two years were included, and detailed history was obtained from the patient. Baseline investigations (total and differential leukocyte count, ESR, CRP, X-ray and CT) wereperformed. Magnetic resonance imaging,FNAC or joint aspiration was performed whenever clinically or radiologically indicated.
Results:
A total of 21 patients were enrolled into the study for a duration of 2 years. Patients mainly presented with both pain and swelling of the SCCJ with predominant right sided involvement. Osteoarthritis was the most frequent diagnosis followed by infections, primary bone/cartilage tumor, and metastasis.
Conclusions:
Although most of the patients with SCCJ swelling have a benign etiology, it is not wise to dismiss thisswelling as degenerative changes. Serious conditions like septic arthritis or neoplasia, may masquerade with similar presentations such as osteoarthritis. It would be therefore imperative to rule out all of these potentially life threatening conditions using thorough clinic-radiological workups.
Key words: Infection, Inflammatory, Neoplasia, Sternocostoclavicular, Swelling
Introduction
Abnormalities of the sternocostoclavicular joint (SCCJ) although common, is still the most underdiagnosed entity in Orthopaedics. The reason for this may be the mild nature of symptoms and thus less emphasis given to them both by the patient as well the treating physician. Nevertheless it is prudent to examinethis joint and investigate these symptoms early, as abnormalities of the SCCJ are common and may point towardsdiagnosis of a specific inflammatory, infectious or neoplastic disorder. Also, the failure to recognize and treat some of these conditions could result in chronic discomfort and disability in patients.
Common causes of SCCJ swelling include degenerative osteoarthritis, septic arthritis, rheumatoid arthritis, crystal deposition disorders, metastatic disease and post-operative involvement after surgery on the neck (1). In addition, certain rare disorders like palmoplantar pustulosis and Friedrich’s disease with a predilection for this joint have been described (2). Although, across the literature numerous cases of SCCJ swelling with varied etiology have been reported in patients, studies with a group of patients from a single population is lacking (3-5). Therefore, the present study was carried out to screen the patients presenting with SCCJ swelling in the Orthopaedic Clinic of a large tertiary care center in the south of India. We aimed to describe the epidemiological profile, and identifyclinical and diagnostic characteristics thatcan help in identifying some of the serious conditions amongst the benign ones. We also tried to search for attributing factors leading to such swellings in our population.
Methods
This prospective observational study was carried out in the Department of Orthopaedics, JIPMER, Puducherry, India, during a two year period from January 2011 to December 2012. During this period, any patient presenting to the Orthopaedics Clinic with a swelling of SCCJ joint were enrolled into the study after giving theirformal consent. Detailed history including any history of trauma or fall, fever, skin eruptions, morning stiffness, pain in other joints, diabetes, alcohol intake, drug abuse and any history suggestive of contact with a tuberculosis patient or previous history of head and neck surgery was obtained from the patient using a performa (Appendix 1). Baseline investigations including total and differential leukocyte count, ESR, CRP, X-ray and CT were performed. In cases with inconclusive findings on the CT scan, or to see the extent of infections and tumors, MRI was done in a few patients. In some patients with unclear clinico-radiological findings, whenever indicated an FNAC or joint aspiration was performed to reach a final diagnosis. All attempts were made to reach a conclusive diagnosis in thepatients and any onein whom a definitive diagnosis could not be made were excluded from the study
Results
A total of 21 patients were enrolled in the study for a duration of 2 years. Out of the 21 patients, 15 (71.4%) were females and 6 (28.6%) were males. The average age of presentation was 45 years (12-69 years). Of the 21 patients, 16 (76%) of them presented with both pain and swelling of the SCCJ, whereas 5(23.8%) presented only with swelling. Right SCCJ was involved in 17(81.1%) patients, whereas the left side was involved in 4(19%) patients. Constitutional symptoms were present in 2(9.5%) patients. On examination, tenderness of the joint was observed in 10 (47.6%) cases, pain on shoulder movement in 3 patients (14.3%) and thickening of the medial end of the clavicle was observed in 3 (14.3%) patients.
The frequency of final diagnosis is depicted in Table 1. Osteoarthritis constituted 52.4%, infections 19%, primary bone/cartilage tumor 9.5%, and metastasis to the joint was 9.5% of the total cases. One patient had rheumatoid involvement of the joint and another one was diagnosed with radiation induced arthritis.
Table 1.
Final diagnosis of sternoclavicular joint swelling (n=21)
| S. No | Diagnosis | Frequency |
|---|---|---|
| Osteoarthitis | 11 (52.4%) | |
| Infection | 4 (19%) | |
| Metastasis | 2 (9.5%) | |
| Primary bone/cartilage tumour | 2 (9.5%) | |
| Rheumatoid arthritis | 1 (4.8%) | |
| Radiation induced arthritis | 1 (4.8%) |
Osteoarthritis could be attributed to occupational exposure in three patients: one with a history of milking cows and coir rope making, another a professional biker, and third being an agricultural laborer.
Out of 4 cases of infections, 3 were diagnosed as having tuberculosis and one with a pseudomonas infection. Of the 3 patients with tuberculosis, one patient had a positive history of contact with tuberculosis from his father. The patient with pseudomonas infection of the clavicular end presented with pain and discharging sinus of short duration.
Out of the two primary tumors of the clavicular end, one was identifiedas a malignant bone tumor (adamantinoma) and one as a benign cartilaginous tumor (enchondroma). Metastasis was found in two patients, of which one was consistent with bronchogenic adenocarcinoma and for the second patient the kidney (RCC) was the primary site. The patient withradiation induced arthritis had a history of soft tissue sarcoma in the region thatwas excised followed by the administration of radiotherapy. The MRI showed the changes were consistent with the diagnosis.
Rheumatoid arthritis involving SCCJ was observed in one patient who also had accompanying Hashimoto’s thyroiditis.
Discussion
Sternocostoclavicular joint swelling can be caused by a number of pathological conditions including infections, inflammatory arthritis and tumors. In the present study, we observed the pattern of presentation and the distribution of diseases causing SCCJ swelling in our population.
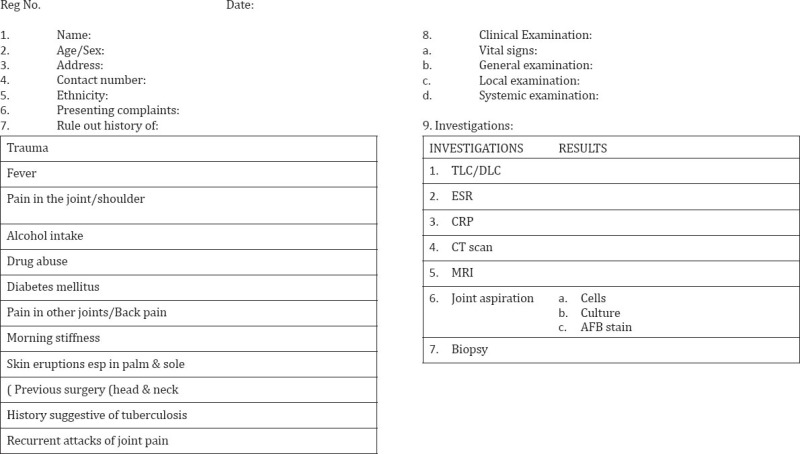
We observed 52.4% of our patients to have degenerative osteoarthritis of the SCCJ. Of these patients, barring one with involvement of the left sided joint, all the others had right sided arthropathy, and all our patients were right hand dominant individuals [Figure 1; 2]. This is consistent with the previous reports, where in more symptoms are observed on the dominant side (1, 6). Mean age of presentation was 48 years and women were affected more than men (63.6% vs 36.3%). Occupational exposure leading to microtrauma and degeneration could be related in three patients (cow milker, coir rope maker, biker and agricultural laborer working with a sickle to clear weeds).
Figure 1.

Patients presenting with right sternocostoclavicular joint swelling.
Figure 2.
(a) MRI and (b) CT images showing osteoarthritis of right sternocostoclavicular joint.
Tubercular involvement of the joint was observed in three patients. Of these, two were females and one was a male child of 12 years. The child had a positive history of contact with tuberculosis from his father. The right side was involved in twopatients and left sided involvement was observed in one of these patients. All the three patients had elevated ESR (mean:-38) with negative CRP. A CT scan showed amass lesion in the manubrium sterni with bony destruction and subsequent FNA showedcaseating granuloma. All three patients responded well to anti-tubercular treatment. Although rare, tuberculosis of the clavicle has been reported by various research teams (7). Similar findings were reported by Dhillon et al. in their case series of nine patients suffering from tubercular SCCJ arthropathy (8).
Septic arthritis of the SCCJ was observed in a 42-year male patient who presented with discharging sinus lastingfive days preceded by swelling and pain of one month. An imaging study showed sternal erosions with soft tissue destruction [Figure 3]. Culture of pus showedpseudomonas aeruginosa sensitive to cloxacillin. Blood culture was negative for any growth. No predisposing factor could be elicited for the infection. Similar cases of septic arthritis in 27 previously healthy patients were also described by Bar-Natan et al. (9). Staphylococcus Aureus was the predominant organism in this series with an incidence of 7% for gram negative rods (pseudomonas). Similar findings were observed by Ross et al. in their review of 180 cases of non-healthy patients (10). On the other hand pseudomonas aeruginosa was the most common organism in the series reported by Roca et al., although the predisposing factor in the form of heroin abuse was present (11).
Figure 3.

CT image showing features of pyogenic infection of right sternocostoclavicular joint.
Of the four tumors diagnosed in our patients, two had a primary tumor and two had secondary metastasis to the SCCJ. Of the primary tumor, one was enchondroma diagnosed in a 60-year-old female, and another was adamantinoma in a young 26-year-old female patient. Metastasis was found in two patients, of which one was consistent with bronchogenic adenocarcinoma and in the second patient the primary site was the kidney. Both metastatic and primary tumors of the SCCJ have been described although metastasis is much more common than a primary bone tumor (12). Secondaries have been reported to originate from the upper aerodigestive tract, thyroid, kidney and prostate (13). Recently, a 16-year-old girl with non-ossifying fibroma has been reported by Gilbert et al. (14). The experience from our study highlights the fact that both benign and malignant tumours of SCCJ are not uncommon, and all four patients in our series presented with minimal symptoms of mild swelling and pain of recent onset. This reiterates the need to evaluate SCCJ swelling seriously.
One patient withradiation induced arthritis had a history of soft tissue sarcoma in the region, which was excised followed by administering radiotherapy. A MRI showed the changes consistent with the diagnosis. Moreover, there are reports of cases presenting with SCCJ swelling after head and neck surgery including radical neck dissection (15-17).
Rheumatoid arthritis involving the SCCJ was observed in one patient, who also had accompanying Hashimoto’s thyroiditis. Rodriguez et al. observed 89 out of 103 cases of SCCJ involvement in patients withrheumatoid arthritis and found the synovitis and hyperperfusion related to the disease activity score (18). However, more studies with screening of the SCCJ in rheumatoid arthritis needs to be done in our population to establish a pattern.
In a series of 25 patients described by Steinheim et al., it was observed that SCCJ arthropathy in these patients was transient and self-limiting (19). We, however, found that SCCJ arthropathy had varied causes in our population, starting from degenerative changes to primary bone tumor. It would therefore be wise to evaluate all the patients of SCCJ arthropathy with great concern. The complications of delayed diagnosis and treatment of serious conditions like septic arthritis or tumor can lead to the increase in morbidity and mortality. To prevent missing out on any serious or systemic disorder we found it extremely useful to follow a protocol based assessment as per the performaand be wary of any red flag signs as described below:
-
1)
Swelling of shorter duration (< 3 weeks)
-
2)
Swelling associated with debilitating pain or sinus
-
3)
Rapid increase in size of swelling
-
4)
Referred pain to shoulder
-
5)
Extremes of age
-
6)
Involvement of non-dominant side
Our experience from this study was that although most of the patients with a sternocostoclavicular joint swelling have a benign etiology, it is still not wise to dismiss all SCCJ swellings as degenerative changes. There are conditions like septic arthritis and neoplasia, which masquerade with similar presentation as osteoarthritis. It would be therefore imperative to rule out all of these potentially life threatening conditions using thorough clinico-radiological workup. The treating orthopaedician should be aware of all these pathologies which can inflict this joint
Appendix 1. Screening performa for sternocostoclavicular joint swelling
References
- 1.Le Loët X, Vittecoq O. The sternocostoclavicular joint: normal and abnormal features. Joint Bone Spine. 2002;69(2):161–9. doi: 10.1016/s1297-319x(02)00362-7. [DOI] [PubMed] [Google Scholar]
- 2.Levy M, Goldberg I, Fischel RE, Frisch E, Maor P. Friedrich's disease. Aseptic necrosis of the sternal end of the clavicle. J Bone Joint Surg Br. 1981;63(4):539–41. doi: 10.1302/0301-620X.63B4.7298679. [DOI] [PubMed] [Google Scholar]
- 3.Mandal SK, Ganguly J, Sil K, Mondal SS. Diagnostic dilemma in a case of osteolytic lesions. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-201682. doi: 10.1136/bcr-2013-201682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mondal S, Sinha D, Nag A, Ghosh A. Unilateral sternocostoclavicular hyperostosis in a patient with ankylosing spondylitis: A case report with color Doppler ultrasonogram findings. Indian J Radiol Imaging. 2013;23(3):278–80. doi: 10.4103/0971-3026.120280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aggarwal AN, Dhammi IK, Singh AP, Kumar S, Goyal MK. Tubercular osteomyelitis of the clavicle: a report of four cases. J Orthop Surg (Hong Kong) 2009;17(1):123–6. doi: 10.1177/230949900901700128. [DOI] [PubMed] [Google Scholar]
- 6.Thongngarm T, McMurray RW. Osteoarthritis of the sternoclavicular joint. J Clin Rheumatol. 2000;6(5):269–71. doi: 10.1097/00124743-200010000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Khan SA, Zahid M, Asif N, Hasan AS. Tuberculosis of the sternoclavicular joint. Indian J Chest Dis Allied Sci. 2002;44(4):271–3. [PubMed] [Google Scholar]
- 8.Dhillon MS, Gupta RK, Bahadur R, Nagi ON. Tuberculosis of the sternoclavicular joints. Acta Orthop Scand. 2001;72(5):514–7. doi: 10.1080/000164701753532862. [DOI] [PubMed] [Google Scholar]
- 9.Bar-Natan M, Salai M, Sidi Y, Gur H. Sternoclavicular Infectious Arthritis in Previously Healthy Adults. Semin Arthritis Rheum. 2002;32(3):189–95. doi: 10.1053/sarh.2002.37284. [DOI] [PubMed] [Google Scholar]
- 10.Ross JJ, Shamsuddin H. Sternoclavicular septic arthritis: review of 180 cases. Medicine (Baltimore) 2004;83(3):139–48. doi: 10.1097/01.md.0000126761.83417.29. [DOI] [PubMed] [Google Scholar]
- 11.Rocha PP, Yoshika TT. Primary skeletal infections in heroin users: a clinical characterization, diagnosis and therapy. Clin Ortho Related Res. 1979;144:238–48. [PubMed] [Google Scholar]
- 12.Kofoed H, Thomsen P, Lindenberg S. Serous synovitis of the sternoclavicular joint: Differential diagnostic aspects. Scand J Rheumatol. 1985;14(1):61–4. doi: 10.3109/03009748509102019. [DOI] [PubMed] [Google Scholar]
- 13.Yood RA, Goldenberg DL. Sternoclavicular joint arthritis. Arthritis Rheum. 1980;23(2):232–9. doi: 10.1002/art.1780230215. [DOI] [PubMed] [Google Scholar]
- 14.Gilbert NF, Deavers MT, Madewell JE, Lewis VO. A 16-year-old Girl With Pain and Swelling in the Medial Clavicle. Clin Orthop Relat Res. 2008;466(12):3158–62. doi: 10.1007/s11999-008-0160-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lamb CEM. Sternoclavicular joint enlargement following block dissection. Br J Surg. 1976;63(6):488–92. doi: 10.1002/bjs.1800630622. [DOI] [PubMed] [Google Scholar]
- 16.Cantlon GE, Gluckman JL. Sternoclavicular joint hypertrophy following radical neck dissection. Head Neck Surg. 1983;5(3):218–21. doi: 10.1002/hed.2890050306. [DOI] [PubMed] [Google Scholar]
- 17.Gluth MB, Simpson CB, Wirth MA. Sternoclavicular Joint Swelling After Surgery of the Head and Neck Region: A Case Report and Differential Diagnostic Review. Am J Otolaryngol. 2001;22(5):367–70. doi: 10.1053/ajot.2001.26501. [DOI] [PubMed] [Google Scholar]
- 18.Rodríguez-Henríquez P, Solano C, Peña A, León-Hernández S, Hernández-Díaz C, Gutiérrez M, et al. Sternoclavicular joint involvement in rheumatoid arthritis: clinical and ultrasound findings of a neglected joint. Arthritis Care Res (Hoboken) 2013;65(7):1177–82. doi: 10.1002/acr.21958. [DOI] [PubMed] [Google Scholar]
- 19.Sternheim A, Chechik O, Freedman Y, Steinberg EL. Transient sternoclavicular joint arthropathy, a self-limited disease. J Shoulder Elbow Surg. 2014;23(4):548–52. doi: 10.1016/j.jse.2013.08.013. [DOI] [PubMed] [Google Scholar]


