Abstract
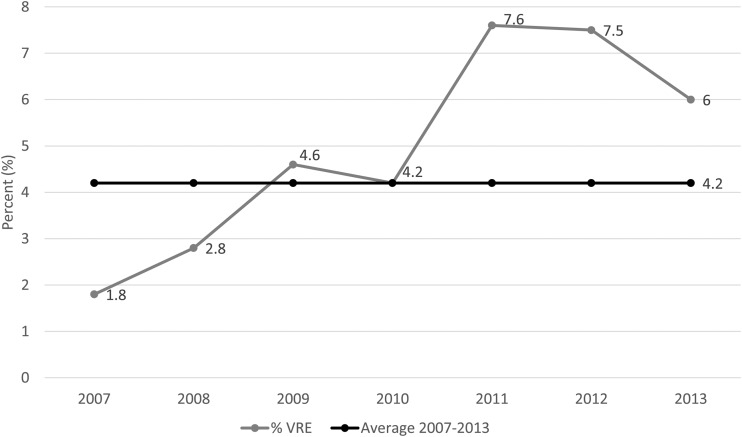
Of 1,927 Enterococcus species isolates collected across Canada from 2007 to 2013, 80 (4.2%) were identified as vancomycin-resistant enterococci (VRE). VRE infections during this time tripled in Canadian hospitals, from 1.8% to 6.0% (P = 0.03). All VRE were Enterococcus faecium, with 90% possessing vanA. The prevalence of vanB decreased from 37.5% in 2007 to 0% in 2013 (P < 0.05). The VRE were multidrug resistant, but 70.6%, 86.3%, and 100% were susceptible to doxycycline, linezolid, and daptomycin, respectively.
TEXT
Vancomycin-resistant enterococci (VRE) are an important cause of nosocomial infections worldwide and may cause significant mortality in immunosuppressed populations (1). Since the first description of VRE in 1986, the incidence of VRE infections has significantly increased, particularly in parts of Asia, Europe, and the United States (2, 3). The annual VRE burden in U.S. hospitals was estimated in 2004 to range from a conservative 20,931 infections (95% confidence interval [CI], 12,596 to 29,266), to a more liberal 85,586 infections (95% CI, 55,986 to 115,186 [4]). The number of U.S. hospitalizations with VRE discharges more than doubled between 2000 and 2006, with a reported prevalence as high as 65% in U.S. hospitals (2, 5). In contrast, the prevalence of VRE in Canadian hospitals remains low, although it has been increasing steadily since the first description of these organisms in 1993 (6). The Canadian Nosocomial Infection Program (CNISP) was the first to report the prevalence of VRE in Canadian hospitals, which was reported at 0.1% in 1996 (7). The Canadian National Intensive Care Unit (CAN-ICU) study reported the prevalence in Canadian ICUs to have increased from 1.8% in 2007 to 4.6% in 2009 (8). A second report from the CNISP studying the epidemiology of VRE in bloodstream infections (BSI) described a significant increase in bacteremia caused by VRE in eastern and central Canada since 2007 (9). Only a few studies have been performed on the epidemiology of VRE in Canadian hospitals and have focused on specific scenarios (i.e., ICUs and BSI) since its first report in 1996. As such, the purpose of this study was to update and assess the epidemiology of VRE isolated from various clinical specimens in Canadian hospitals from 2007 to 2013.
From 2007 through 2013, 10 to 15 tertiary care centers across Canada submitted consecutive pathogens to an ongoing national surveillance study (CANWARD), obtained from samples from patients attending hospital clinics, emergency rooms, medical and surgical wards, and intensive care units. Each site submitted isolates (one isolate per patient) from blood (n = 100 to 360), respiratory (n = 100 to 200), urine (n = 25 to 100), and wound (n = 25 to 50) specimens. The number of isolates submitted differed by study year (10). All isolates were deemed clinically significant by the participating laboratories. Statistical analysis was performed with GraphPad QuickCalcs using the chi-square analysis. A total of 1,927 Enterococcus species isolates were submitted as part of the CANWARD study. Of the 1,927 Enterococcus species isolated, 4.2% (80/1,927) were identified as VRE and had an MIC of ≥32 μg/ml for vancomycin using the Clinical and Laboratory Standards Institute (CLSI) broth microdilution method (11). Over the study period, the national prevalence of VRE tripled from 1.8% in 2007 to 6.0% in 2013 (P = 0.03) and peaked at 7.9% in 2011 (Fig. 1). This observation is consistent with other studies documenting the increasing prevalence of VRE in Canadian ICUs and VRE as a cause of BSI in Canadian hospitals (8, 9). Similarly, the prevalence of VRE in a single hospital in China in 2012 to 2013 was reported at 4.4% (12). In contrast, the prevalence of VRE in Canadian hospitals was much lower than that seen with significant increases observed in other countries; in the United States, the prevalence of VRE in elderly increased significantly from 6% in 1998 to 25% in 2009 (13), and in Taiwan, there was an increase in the prevalence of VRE blood isolates from 3.9% in 2003 to 18.9% in 2010 (3).
FIG 1.
The prevalence of Enterococcus spp. (n = 1,927) with vancomycin resistance (n = 80) observed in Canada from 2007 to 2013.
The majority of the VRE isolates obtained in the current study were from central (Ontario and Quebec, 58.8% [n = 47]) and western Canada (British Columbia, Alberta, Saskatchewan, and Manitoba, 40% [n = 32]), with only one isolate (1.2%) coming from eastern Canada (New Brunswick and Nova Scotia). The observed distribution of VRE in Canadian hospitals is consistent with that in other studies (7, 9). Interestingly, it appears that VRE emerged in central and western Canada (6, 7) but remains a rare finding in eastern Canada >2 decades after its first description in Canadian hospitals. The majority of the isolates originated from blood (68.8%), followed by wound (15.0%), urine (13.7%), and respiratory specimens (2.5%). Although it would appear from the data that VRE are a significant cause of invasive infections in Canadian hospitals, this most likely reflects the methodology of the CANWARD study, as more blood isolates are requested than other specimen sources. The patient demographics for this study are summarized in Table 1. Most VRE were identified from medical wards (45.0%), followed by ICUs (32.5%), surgery wards (12.5%), emergency rooms (6.3%), and hospital clinics (3.8%). In comparison to vancomycin-susceptible enterococci (VSE), VRE were more commonly isolated from patients in ICUs (P = 0.0016), whereas VSE were more commonly isolated from patients in hospital clinics (P = 0.01) and emergency rooms (P = 0.0019). In addition, VRE were more commonly isolated from patients 18 to 64 years old (P = 0.03), whereas VSE were more commonly isolated from patients ≤17 years old (P = 0.05).
TABLE 1.
Summary of demographics of patients with VRE and VSE infections in Canadian hospitals
| Demographic | No. (%) of patients witha: |
P valueb | |
|---|---|---|---|
| VRE (n = 80) | VSE (n = 1,847) | ||
| Gender | |||
| Female | 40 (50) | 777 (42.1) | >0.05 |
| Male | 40 (50) | 1,070 (57.9) | >0.05 |
| Age group (yr) | |||
| ≤17 | 1 (1.3) | 178 (9.6) | 0.05 |
| 18–64 | 42 (52.5) | 740 (40.1) | 0.03 |
| ≥65 | 37 (46.3) | 929 (50.3) | >0.05 |
| Location | |||
| Hospital clinic | 3 (3.8) | 237 (12.8) | 0.01 |
| Emergency room | 5 (6.3) | 353 (19.1) | 0.0019 |
| ICU | 26 (32.5) | 325 (17.6) | 0.0016 |
| Medical ward | 36 (45.0) | 683 (37.0) | >0.05 |
| Surgical ward | 10 (12.5) | 249 (13.5) | >0.05 |
VRE, vancomycin-resistant enterococci; VSE, vancomycin-susceptible enterococci.
P ≤ 0.05 is considered statistically significant.
All 80 VRE isolates were confirmed to be E. faecium using the previously described ddl gene PCR to identify Enterococcus species (14). In contrast, the first CNISP report in 1996 found that 11.3% of the VRE isolates were E. faecalis. In addition, a recent report from a hospital in China found the prevalence of vancomycin-resistant E. faecalis in 2012 to 2013 to be higher, at 6.5%, than that of vancomycin-resistant E. faecium, at 2.7% (15). A recent CNISP study evaluating VRE in BSI in Canada from 1999 to 2009 also isolated E. faecium only, and the results were similar to those of the current study (9). Vancomycin-resistant E. faecalis is now considered a rare finding in Canadian hospitals. Genotypes were determined by using a PCR for vanA and vanB genes (9). Of the VRE, 90% carried the vanA gene, while the remainder carried vanB. The proportion of VRE possessing the vanB determinant decreased over the study period from 37.5% in 2007 to 0% in 2013 (P < 0.05). Remarkably, the first report in 1996 found that 96% of VRE harbored the vanB gene and may be accounted for by the spread of VRE in a single facility (7). Consequently, it appears that vanA genotypes are now the predominant genetic proponent in vancomycin resistance in enterococci in Canada. The predominance of the vanA genotype in VRE isolates has been documented in Europe, Canada, and the United States (2, 9).
Susceptibility testing was performed using CLSI broth microdilution methods (11). The antimicrobial susceptibility profiles are summarized in Table 2. All VRE were resistant to ciprofloxacin, levofloxacin, and vancomycin, as expected. Of the VRE, 70.6%, 86.3%, and 100% were susceptible to doxycycline, linezolid, and daptomycin, respectively. In comparison, 44.7%, 58.1%, 51.6%, 95.5%, and 100% of vancomycin-susceptible enterococci were susceptible to ciprofloxacin, levofloxacin, doxycycline, linezolid, and daptomycin, respectively. Interestingly, linezolid susceptibility for both VRE (86.3%) and VSE (95.5%) was lower than that reported in high VRE prevalence settings, such as the United States and China (14, 15). Furthermore, all enterococcal isolates in this study that were linezolid nonsusceptible fell in the intermediate category (MIC, 4 μg/ml) and did not display frank resistance. Future studies are required to elucidate the mechanism of linezolid nonsusceptibility in these isolates.
TABLE 2.
Antimicrobial susceptibility profiles of vancomycin-resistant and -susceptible E. faecium isolates from CANWARD study
| Antimicrobial used | Susceptibility profile (%)a |
MIC range (μg/ml) | MIC50 (μg/ml) | MIC90 (μg/ml) | ||
|---|---|---|---|---|---|---|
| S | I | R | ||||
| Vancomycin-resistant enterococci | ||||||
| Ciprofloxacin | 100 | >16 | >16 | >16 | ||
| Levofloxacin | 100 | >32 | >32 | >32 | ||
| Vancomycin | 100 | >32 | >32 | >32 | ||
| Doxycycline | 70.6 | 8.8 | 20.6 | ≤0.12 to 16 | 2 | 16 |
| Linezolid | 86.3 | 13.8 | 0.5 to 4 | 2 | 4 | |
| Daptomycin | 100 | ≤0.06 to 2 | 1 | 2 | ||
| Vancomycin-susceptible enterococci | ||||||
| Ciprofloxacin | 44.7 | 12.8 | 42.5 | ≤0.06 to >16 | 2 | >16 |
| Levofloxacin | 58.1 | 0.8 | 41.1 | ≤0.06 to >32 | 2 | >32 |
| Vancomycin | 100 | ≤0.25 to 4 | 1 | 2 | ||
| Doxycycline | 51.6 | 32.7 | 15.7 | ≤0.12 to 32 | 4 | 16 |
| Linezolid | 95.5 | 4.5 | ≤0.12 to 4 | 2 | 2 | |
| Daptomycin | 100 | ≤0.06 to 4 | 0.5 | 2 | ||
S, susceptible; I, intermediate; R, resistant.
In summary, the prevalence of VRE infections has tripled between 2007 and 2013 in Canadian hospitals, from 1.8% to 6.0%. The majority of the VRE isolates were vanA-positive E. faecium. The proportion of VRE possessing vanB decreased over the study period. Although treatment options are limited for infections caused by VRE, most remain susceptible to linezolid and daptomycin.
REFERENCES
- 1.Arias CA, Contreras GA, Murray BE. 2010. Management of multidrug-resistant enterococcal infections. Clin Microbiol Infect 16:555–562. doi: 10.1111/j.1469-0691.2010.03214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deshpande LM, Fritsche TR, Moet GJ, Biedenbach DJ, Jones RN. 2007. Antimicrobial resistance and molecular epidemiology of vancomycin-resistant enterococci from North America and Europe: a report from the SENTRY antimicrobial surveillance program. Diagn Microbiol Infect Dis 58:163–170. doi: 10.1016/j.diagmicrobio.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 3.Lu CL, Chuang YC, Chang HC, Chen YC, Wang JT, Chang SC. 2012. Microbiological and clinical characteristics of vancomycin-resistant Enterococcus faecium bacteraemia in Taiwan: implication of sequence type for prognosis. J Antimicrob Chemother 67:2243–2249. doi: 10.1093/jac/dks181. [DOI] [PubMed] [Google Scholar]
- 4.Reik R, Tenover FC, Klein E, McDonald LC. 2008. The burden of vancomycin-resistant enterococcal infections in U.S. hospitals, 2003 to 2004. Diagn Microbiol Infect Dis 62:81–85. doi: 10.1016/j.diagmicrobio.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Ramsey AM, Zilberberg MD. 2009. Secular trends of hospitalization with vancomycin-resistant enterococcus infection in the United States, 2000–2006. Infect Control Hosp Epidemiol 30:184–186. doi: 10.1086/593956. [DOI] [PubMed] [Google Scholar]
- 6.Kibsey PC, Willey B, Low DE. 1993. Vancomycin multi-resistant Enterococcus faecium: first Canadian isolate, abstr K5. Abstr Can Assoc Clin Microbiol Infect Dis, 21 to 25 November 1993, Vancouver, British Columbia, Canada. [Google Scholar]
- 7.Ofner-Agostini ME, Conly J, Paton S, Kureishi A, Nicolle L, Mulvey M, Johnson W, Johnston L, Canadian Hospital Epidemiology Committee. 1997. Vancomycin-resistant enterococci (VRE) in Canada—results of the Canadian Nosocomial Infection Surveillance Program 1996 VRE point prevalence surveillance project. Can J Infect Dis 8:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhanel GG, Decorby M, Nichol KA, Baudry PJ, Karlowsky JA, Lagace-Wiens PR, McCracken M, Mulvey MR, Hoban DJ. 2008. Characterization of methicillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci and extended-spectrum beta-lactamase-producing Escherichia coli in intensive care units in Canada: results of the Canadian National Intensive Care Unit (CAN-ICU) study (2005–2006). Can J Infect Dis Med Microbiol 19:243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCracken M, Wong A, Mitchell R, Gravel D, Conly J, Embil J, Johnston L, Matlow A, Ormiston D, Simor AE, Smith S, Du T, Hizon R, Mulvey MR, Canadian Nosocomial Infection Surveillance Program. 2013. Molecular epidemiology of vancomycin-resistant enterococcal bacteraemia: results from the Canadian Nosocomial Infection Surveillance Program, 1999–2009. J Antimicrob Chemother 68:1505–1509. doi: 10.1093/jac/dkt054. [DOI] [PubMed] [Google Scholar]
- 10.Zhanel GG, Adam HJ, Baxter MR, Fuller J, Nichol KA, Denisuik AJ, Lagace-Wiens PR, Walkty A, Karlowsky JA, Schweizer F, Hoban DJ, Canadian Antimicrobial Resistance Alliance. 2013. Antimicrobial susceptibility of 22746 pathogens from Canadian hospitals: results of the CANWARD 2007–11 study. J Antimicrob Chemother 68(Suppl 1):i7–i22. doi: 10.1093/jac/dkt022. [DOI] [PubMed] [Google Scholar]
- 11.Clinical and Laboratory Standards Institute. 2014. Performance standards for antimicrobial susceptibility testing; 24th informational supplement. CLSI M100-S24 Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 12.Jia XQ, Pang F, Chen JZ, Jiang LX. 2015. Prevalence and clinical distribution of multidrug-resistant bacteria (3537 isolates) in a tertiary Chinese hospital (January 2012–December 2013). Pathol Biol (Paris) 63:21–23. doi: 10.1016/j.patbio.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Denkinger CM, Grant AD, Denkinger M, Gautam S, D'Agata EM. 2012. Increased multi-drug resistance among the elderly on admission to the hospital—a 12-year surveillance study. Arch Gerontol Geriatr 56:227–230. doi: 10.1016/j.archger.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Boyd DA, Willey BM, Fawcett D, Gillani N, Mulvey MR. 2008. Molecular characterization of Enterococcus faecalis N06-0364 with low-level vancomycin resistance harboring a novel d-Ala-d-Ser gene cluster, vanL. Antimicrob Agents Chemother 52:2667–2672. doi: 10.1128/AAC.01516-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang M, Xie Y, He C, Chen ZX, Guo L, Yang Q, Liu JY, Du Y, Ou QS, Wang LL. 2014. Molecular characteristics of vancomycin-resistant Enterococcus faecium from a tertiary care hospital in Chengdu, China: molecular characteristics of VRE in China. Eur J Clin Microbiol Infect Dis 33:933–939. doi: 10.1007/s10096-013-2029-z. [DOI] [PubMed] [Google Scholar]