Abstract
Objective: The US Food and Drug Administration (FDA) issued a warning stating that patients older than 60 years are not recommended to receive doses of citalopram exceeding 20 mg daily due to concerns of corrected QT (QTc) prolongation. The purpose of this study is to assess the impact of the FDA warning on prescribing patterns of citalopram in patients 60 years of age and older.
Method: This is a retrospective cohort study of hospitalized patients 60 years of age and older prescribed citalopram from October 24, 2010, to August 24, 2011 and from November 24, 2011, to September 24, 2012. Records were examined for the presence of baseline risk factors for QTc prolongation and torsades de pointes.
Results: The issuance of an FDA warning was not associated with an observable change in prescribing patterns of citalopram. A total of 98.8% of patients had at least 1 risk factor for QTc prolongation. No significant difference in the total number of risk factors was seen between groups (P = .915). No differences were seen in risk factors prewarning and postwarning, except a higher percentage had left ventricular hypertrophy (P = .001) or history of syncope (P = .043) prior to the warning. More subjects were prescribed concomitant proarrhythmic medications (P = .009) after the FDA warning was issued. Similar percentages of each group were receiving daily dosages > 20 mg of citalopram (P = .600).
Conclusions: The issuance of an FDA warning did not produce observable changes in prescribing patterns of citalopram. Modifiable risk factors and optimal dosing may be targets of interventions aimed at promoting safer use of citalopram.
Clinical Points
■ Electrolytes and concomitant QTc-prolonging medications may be the most appropriate targets for intervention for reducing QTc prolongation risk.
■ The maximum recommended daily citalopram dose for patients greater than 60 years old is 20 mg.
In 2011, the US Food and Drug Administration (FDA) issued a warning with citalopram indicating concerns about the potential for corrected QT (QTc) interval prolongation at doses exceeding 40 mg daily for patients under 60 years of age and 20 mg daily for patients over the age of 60 years.1 The FDA warning cited concerns regarding increased serum concentrations and the resultant increased risk of QT interval prolongation.2
The main basis for the FDA warning was an analysis of an unpublished multicenter, double-blind, placebo-controlled crossover study of 119 subjects.1 In this study, subjects received three 22-day treatments in a random order, separated by at least 14 days. The 3 treatments consisted of (1) citalopram 20 mg daily for 9 days, followed by citalopram 40 mg daily for 4 days and citalopram 60 mg for 9 days; (2) 8 days of placebo, followed by a single dose of moxifloxacin 400 mg (an antibiotic known to prolong the QTc interval), followed by 12 days of placebo and an additional dose of moxifloxacin; and (3) 22 days of placebo. Researchers observed greater QTc prolongation in the group of subjects prescribed 60 mg daily (18.5 ms) compared with those prescribed 20 mg daily (8.5 ms).3 The 40-mg daily dose of citalopram was not studied, but the prolongation of the QTc interval compared to placebo was estimated to be 12.6 ms on the basis of serum concentrations. By comparison, subjects taking moxifloxacin 400 mg daily exhibited a QTc prolongation of 13.4 ms compared to subjects taking placebo.1
The FDA warning did not provide data about baseline characteristics of subjects included in the study. According to a study summary made available by Forest Laboratories, the mean ± SD age of the sample was 31.5 years ± 8.01 years.3 The percentage of the 119 subjects 60 years of age or older is unknown. Other than suggesting a dosage reduction to 20 mg in patients 60 years of age and older, the FDA warning provided no clear guidance as to how to address the use of citalopram in older adults at risk for QTc prolongation.2
The purpose of this study is to assess the impact of the FDA warning on prescribing patterns of citalopram in patients 60 years of age and older.
METHOD
This study was a single-center, retrospective cohort design. Subjects were eligible for inclusion if they were at least 60 years of age; were admitted to the study institution from October 24, 2010, to August 24, 2011 and November 24, 2011, to September 24, 2012; and received citalopram (at any dose and duration) during the index hospital admission at Vidant Medical Center in Greenville, North Carolina. The time periods of data collection reflect a 10-month interval before and after the warning. Data collection for the postwarning period was begun 3 months following the date of the FDA warning to allow for its dissemination. Patients were hospitalized in both medical and psychiatric settings. For patients with multiple admissions meeting the inclusion criteria, only the most recent hospital admission was included in the data collection. Excluded patients were those who did not have a documented history and physical with active problem list for the index hospital admission (ie, same-day surgical patients).
The primary endpoint was the percentage of patients prescribed citalopram at a dose greater than 20 mg. The secondary endpoint was the number of risk factors per subject for QTc interval prolongation, which included left ventricular dysfunction, left ventricular hypertrophy, ischemic heart disease, bradycardia (less than 60 bpm, based on first recorded heart rate at admission), reported history of syncope, reported family history of sudden death at age less than 40 years in a first-degree relative, reported alcohol dependence, liver disease, metabolic/endocrine disorders (diabetes, hypothyroidism, pituitary insufficiency, obesity), QTc-prolonging medication overdose during index hospitalization, central nervous system (CNS) disorders (CNS trauma, CNS infection, stroke) during index hospitalization, hypomagnesemia (measured by the first magnesium value during index hospital admission in mg/dL), hypokalemia (measured by the first potassium value during index hospital admission in mEq/L), and proarrhythmic medications based on the Arizona CERT—Center for Education and Research on Therapeutics website at index hospital admission. Other secondary endpoints were the percentage of patients with individual risk factors for QTc prolongation, the percentage of patients undergoing electrocardiogram (ECG) monitoring during index hospital admission, and incidence of QTc interval prolongation.
Data Collection
Using a standardized data abstraction form, 1 investigator (study author K.R.F.) reviewed medical records and recorded demographic data including age, gender, admitting diagnosis, and admission date. If performed during the index hospitalization, the QTc values were calculated by machine using Bazett’s formula4 and averaged over 12 leads. Charts were examined for nonmodifiable risk factors for QTc prolongation, including cardiovascular (left ventricular dysfunction, left ventricular hypertrophy, ischemic heart disease, heart rate < 60 bpm, past history of syncope, or a family history of sudden death at age < 40 years) and other noncardiovascular conditions (alcohol dependence, liver disease, metabolic or endocrine disorders, medication overdose, or central nervous system disorders).5 The following additional modifiable risk factors for QTc prolongation also were recorded: lowest potassium and magnesium values and concomitant proarrhythmic medications. Concomitant proarrhythmic medications were identified per the Arizona CERT—Center for Education and Research on Therapeutics website.6
The Investigational Review Board of East Carolina University, Greenville, North Carolina, and Vidant Medical Center reviewed study methodology under expedited review and granted a waiver of consent for the conduct of the study. No protected health information or patient-specific identifiers were recorded.
Statistical Analysis
The primary endpoint was the percentage of subjects prescribed a daily dose of citalopram > 20 mg. A χ2 test was used compare the difference in these percentages from the pre- and post-FDA alert study periods. The χ2 tests were used to compare secondary endpoints including ECG monitoring and percent of subjects with each risk factor pre- and post- FDA warning. The number of risk factors for QTc prolongation was analyzed via a Mantel-Haenszel test statistic. The QTc interval data are reported using descriptive statistics. Analysis was completed using JMP (SAS Institute Inc, Cary, North Carolina). All statistical tests were 2-sided, with a α of .05 defining statistical significance.
RESULTS
The initial search yielded 1,039 potentially eligible subjects. From these 1,039 subjects, a total of 447 (238 in the prewarning group and 209 in the postwarning group) were included in the study. All subjects were chosen by random number assignment. Demographics were similar between groups, with a mean sample age of 72.7 years and male gender percentage of 40.3% (Table 1).
Table 1.
Demographic Information of Study Participants
| Variable | Overall Sample (N = 447) | Prewarning Group (n = 238)a | Postwarning Group (n = 209)b |
| Age, mean ± SD | 72.7 ± 9.0 | 73.1 ± 8.2 | 72.3 ± 8.8 |
| Men, n (%) | 180 (40.3) | 100 (42.0) | 80 (38.2) |
| Body mass index, mean ± SD, kg/m2 | 30.1 ± 12.9 | 30.2 ± 15.7 | 30.0 ± 8.6 |
Patients prescribed citalopram from October 24, 2010, to August 24, 2011.
Patients prescribed citalopram from November 24, 2011, to September 24, 2012.
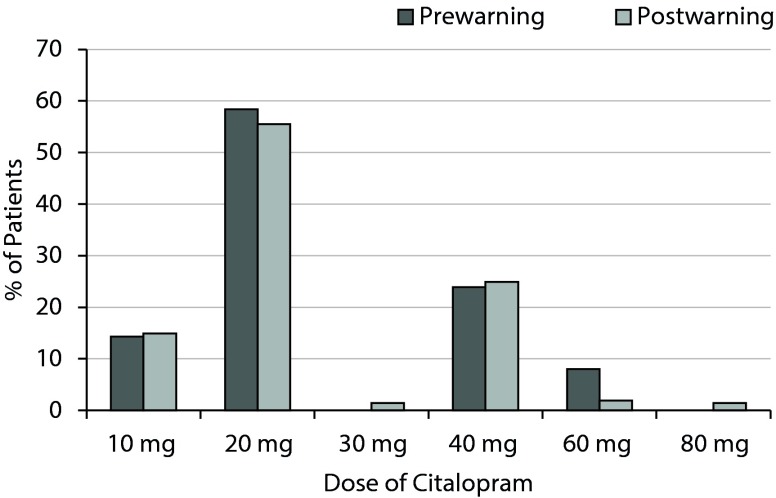
There was no statistically significant difference in percentage of patients prescribed citalopram at a daily dose greater than 20 mg. There were 65 subjects in the prewarning group (27.3%) and 62 subjects in the postwarning group (29.7%) who received a daily dosage greater than 20 mg (χ2 = 0.303, P = .600) (Table 2). The daily dose for citalopram ranged from 10 to 80 mg, with the highest percentages of patients receiving a daily dose of either 20 mg or 40 mg (Figure 1).
Table 2.
Comparison of Citalopram Daily Dosagesa
χ2 = 0.30, P = .600.
Patients prescribed citalopram from October 24, 2010, to August 24, 2011.
Patients prescribed citalopram from November 24, 2011, to September 24, 2012.
Figure 1.
Citalopram Daily Dosages of Patients in the Prewarninga and Postwarning Groupsb
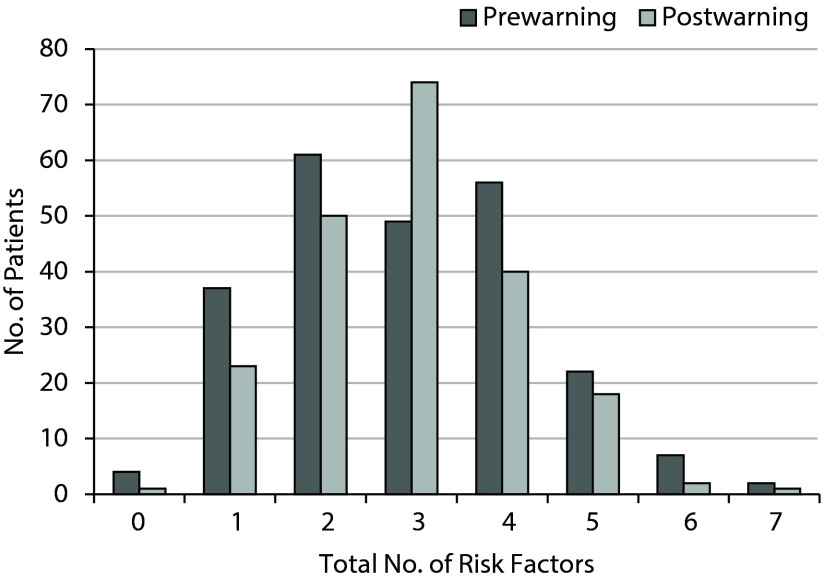
There were no significant differences between groups in terms of prevalence of risk factors (P = .915) (Figure 2). Subjects ranged in number of prespecified risk factors for QTc prolongation from 0 to 7 risk factors, with a median of 3. Approximately 98% of all subjects in the study had at least 1 risk factor for QTc prolongation, 39.4% had 0 to 2 risk factors, 57.9% had 3 to 5 risk factors, and 2.7% had ≥ 6 risk factors for QTc prolongation.
Figure 2.
Total Risk Factors for QTc Prolongation of Patients in the Prewarninga and Postwarning Groupsb
No subjects in the sample were identified as having a family history of sudden death at age < 40 years. One subject was identified as overdosing on a QTc-prolonging medication (trazodone) in the prewarning group. Prior to the FDA warning, a higher percentage of patients had left ventricular hypertrophy (26.1% prewarning compared to 13.9% postwarning, P = .001) or history of syncope (8% prewarning compared to 3.3% postwarning, P = .043). A higher percentage of patients in the postwarning group were taking concomitant proarrhythmic medications (77.3% prewarning compared to 87.1% postwarning, P = .009). No other significant differences were seen in prespecified risk factors for QTc prolongation (Table 3).
Table 3.
Comparison of Individual Risk Factors for QTc Prolongationa
| Risk Factor | Prewarning (n = 238)b | Postwarning (n = 209)c | χ2 | P Value |
| Left ventricular dysfunction | 25 (10.5) | 21 (10.0) | 0.025 | 1.00 |
| Left ventricular hypertrophy | 62 (26.1) | 29 (13.9) | 10.173 | .001 |
| Ischemic heart disease | 79 (33.2) | 77 (3.8) | 0.652 | .428 |
| Bradycardia | 29 (12.2) | 30 (14.4) | 0.457 | .576 |
| History of syncope | 19 (8.0) | 7 (3.3) | 4.362 | .043 |
| Overdose on QTc-prolonging medication | 1 (0.4) | 0 (0) | 1.263 | 1.00 |
| Ethanol dependence | 17 (7.1) | 14 (6.7) | 0.034 | 1.00 |
| Liver disease | 6 (1.3) | 2 (0.4) | 1.549 | .293 |
| CNS disorders (CNS trauma, CNS infection, stroke) | 20 (8.4) | 17 (8.1) | 0.011 | 1.00 |
| Metabolic disorders (diabetes, hypothyroidism, obesity) | 157 (65.9) | 143 (68.4) | 0.304 | .615 |
| Hypokalemia | 19 (8.6) | 20 (9.9) | 0.213 | .737 |
| Hypomagnesemia | 13 (10.8) | 10 (8.1) | 0.488 | .518 |
| Proarrhythmic medications | 184 (77.3) | 182 (87.1) | 7.160 | .009 |
Values are presented as n (%).
Patients prescribed citalopram from October 24, 2010, to August 24, 2011.
Patients prescribed citalopram from November 24, 2011, to September 24, 2012.
Abbreviation: CNS = central nervous system, QTc = corrected QT.
Ninety-five percent of subjects had a serum potassium level (normal range in the study institution: 3.5–5.0 mEq/L) and 55% of subjects had a serum magnesium level (normal range in the study institution: 1.6–2.6 mg/dL) measured during their index hospital admission. If these serum measurements were not obtained during the index hospital admission, the risk factor was treated as not being present.
Overall, 332 of the subjects included in this study underwent ECG testing during their index hospital admission (74.3%). Statistically more subjects underwent ECG testing during index hospitalization in the postwarning period: 166 patients in the prewarning group (69.3%) compared to 166 patients in the postwarning group (79.4%) (χ2 = 5.9065, P = .017). There was no statistical difference between groups in terms of prevalence of prolonged QTc interval. Among 235 subjects who had an ECG and were taking citalopram 20 mg, the mean QTc interval was statistically the same as for 96 subjects who had an ECG and were taking > 20 mg of citalopram. There was an association between QTc interval and number of risk factors, with a mean ± SD QTc interval of 455.6 ± 31.2 ms, 460.1 ± 40.2 ms, and 485.5 ± 37.7 ms for individuals with 0 to 2, 3 to 5, and > 6 risk factors for QTc prolongation, respectively.
DISCUSSION
This is the first study to look at changes in citalopram prescribing following an FDA alert of QTc prolongation at daily doses > 20 mg in patients older than 60 years of age. In this sample of 447 medical inpatients 60 years of age and older prescribed citalopram at any dose, there was no significant difference in the percentage of subjects prescribed a daily dose of citalopram greater than 20 mg prior to and following the FDA alert. There were also no statistically significant differences seen between groups in total number of risk factors pre- and post-FDA warning. A high percentage of subjects (98.8%) had at least 1 risk factor for QTc prolongation. We did find a statistically higher percentage with left ventricular hypertrophy or history of syncope prior to the warning and a higher percentage prescribed proarrhythmic medications after the warning.
Prior to the FDA alert in 2011, studies of therapeutically dosed citalopram demonstrated an associated reduction in heart rate but no other ECG changes7; however, QTc prolongation has been reported in case reports of citalopram overdose.8 In these cases, degree of QTc prolongation correlated with predicted serum drug concentration and elimination of the drug. A systematic review of literature associating citalopram with QTc prolongation and torsades de points identified 9 cases, 5 of which involved an overdose. In the remaining 4 cases, patients had several risk factors for QTc prolongation, including concurrent use of QTc-prolonging medications (olanzapine, amiodarone), sinus bradycardia, hypokalemia, advanced age, and hypomagnesemia. Three of the 9 cases involved patients over the age of 60 years.8
Since issuance of the FDA warning, 2 additional studies examining QTc prolongation with antidepressants have been published.9,10 The first study was designed to quantify the impact on the QTc interval of the selective serotonin reuptake inhibitors and other antidepressants in conjunction with methadone, an opiate known to prolong the QTc interval.9 The study included 38,397 subjects who had ECGs available and had received an antidepressant or methadone. Mean age in the study was 58.3 years, with a standard deviation of 16.2 years. There was a dose-response association with QTc prolongation for citalopram (adjusted β = 0.10, SE = 0.04, P < .01), escitalopram (adjusted β = 0.58, SE = 0.15, P < .001), and amitriptyline (adjusted β = 0.11, SE = 0.03, P < .001) but not for other antidepressants. The QTc-prolonging effect of citalopram was further demonstrated by within-subject paired observations demonstrating a statistically significant dose-response curve (10–20 mg citalopram was associated with an increase of 7.8 ± 3.6 ms in QTc; 20–40 mg citalopram was associated with an increase of 10.3 ± 4.0 ms in QTc).9 This study confirms QT prolongation with higher doses of citalopram as well as with amitriptyline, which does not carry an FDA warning (though it is widely known to exhibit effects on cardiac conduction).
The second study, a retrospective cohort design using data from the Veterans Health Administration from 2004 through 2009, evaluated depressed patients who were prescribed either citalopram (n = 618,450) or sertraline (n = 365,898), a comparison SSRI antidepressant with no associated FDA warning.10 Patients at least 60 years of age comprised 41.2% of subjects in the citalopram group and 42.3% of subjects in the sertraline group. Outcomes included ventricular arrhythmias and cardiac, noncardiac, and all-cause mortality. The QTc intervals were not reported. The study failed to demonstrate an increased risk of ventricular arrhythmia, all-cause mortality, or noncardiac mortality with citalopram, which yielded findings similar to those with sertraline. The authors of this study raised questions regarding the merit of the FDA warning for citalopram.10
Prescribers may need education to increase awareness of risk factors for QTc prolongation, such as congenital long QT syndrome, uncompensated heart failure, bradycardia, hypokalemia, hypomagnesemia, and concomitant medications, when prescribing citalopram or other medications associated with QTc-prolonging risk. Considering that 13% of subjects in the sample had a QTc measured at > 500 ms, modifiable risk factors including concomitant proarrhythmic medications and electrolyte monitoring may be important targets of interventions aimed at optimizing the safe use of citalopram. In this study, 82.8% of subjects were concomitantly prescribed proarrhythmic medications, with a significantly higher percentage of subjects receiving these medications after issuance of the warning. One possibility is that prescribers are not recognizing concomitant proarrhythmic drugs, or they are unaware of the FDA warning regarding increased risk of QTc prolongation. Another possibility is that prescribers generally reach for citalopram because it has been associated with lower rates of pharmacodynamic interactions, and they may be unaware of possible risks for QTc prolongation and torsades de pointes.
In regard to electrolyte imbalances, hypomagnesemia and hypokalemia are 2 common modifiable risk factors for QTc prolongation and torsades de points.7,11,12 Although 95% of subjects had a serum potassium level measured during their index hospital admission, only slightly more than half of the subjects had a serum magnesium value available. Approximately 14% of patients with values available had a potassium or magnesium value below the normal laboratory limit. Increased recognition and correction of electrolyte imbalances may be an important step to include in mitigating adverse cardiac effects in patients taking citalopram.
A risk assessment could be added to the electronic medical record with reassessment to determine the risk for QTc prolongation based on modifiable and nonmodifiable risk factors. The Mayo Clinic in Rochester, Minnesota, recently implemented an institution-wide computer-based QT alert system that generates a medication- and disease-based pro-QTc score, which has been demonstrated to be an independent predictor of mortality.13 The pro-QTc score included female sex, QT-affecting clinical diagnoses and conditions, QT-prolonging electrolyte disturbances, and QT-prolonging medication(s) present on the International Registry for Drug-Induced Arrhythmias Arizona Classification.6 Each QT-prolonging data point, drug, or medical condition was considered equipotent and was designated 1 point for the purposes of the study. In addition, all ECGs performed were screened, and the physician was alerted if the QTc was 500 ms or greater. Similarly, implementation of a computerized physician order entry set was found to be beneficial in reducing the 24-hour cumulative dose of intravenous haloperidol, a QTc-prolonging medication, and increasing the likelihood of a follow-up ECG and obtainment of a magnesium laboratory value.14 However, in an era of information overload and prescriber “alert fatigue,”15 it will be important to determine a strategy that will have the greatest impact on behavior and patient safety.
A significantly higher percentage of patients prescribed citalopram underwent ECG monitoring after publication of the FDA warning, though without additional information about their medical condition, it is not possible to draw any conclusions about the effect of the warning itself. The FDA does not give guidance on how often an ECG should be obtained for QTc measurements in patients receiving citalopram. Due to a relatively low rate of QTc prolongation with citalopram in general, the cost of routine ECG monitoring may limit its utility. We would recommend obtaining an ECG before starting citalopram or continuing citalopram at a dose higher than the FDA recommendation.
The FDA recommendations have not been extended to other SSRIs including escitalopram despite the structural similarities to citalopram. A study of escitalopram found dose-dependent increases of QTc with escitalopram that were substantially less marked (4.5 ms and 10.7 ms for 10 and 30 mg, respectively), though the mean age and standard deviation of the sample was significantly younger than the sample used in the citalopram study.16 The percentage of the 113 subjects in this study 60 years of age or older is unknown, though with a mean± SD age of 27.3 ± 7.53 years, it is unlikely to be a high proportion of the sample.16 Case reports have linked other SSRIs with QTc prolongation, but no prospective study (including 5 studies of fluoxetine and 5 studies of paroxetine) has shown a statistically significant effect on the QTc interval.17 The International Registry for Drug-Induced Arrhythmias Arizona Classification currently lists citalopram on its “Torsades List,” escitalopram on its “Possible Torsades List,” and paroxetine, fluoxetine, and sertraline on its “Conditional Torsades List.”6
Additionally, sertraline has been safely studied in cardiac patients; both with acute myocardial infarction/unstable angina and heart failure,18,19 and escitalopram was reported to be as safe as placebo on numerous cardiovascular safety measures (arrhythmias, QTc prolongation, ST-segment depression) in nondepressed acute coronary syndrome patients.20
Our study has several limitations. It is a retrospective cohort study, and prescribers chose medications and dosages based on clinical impressions, which could have included risk assessment with respect to the QTc interval. The study focused on patients admitted to the hospital, and hospital providers may be likely to maintain the same dosage of antidepressant during hospitalization without reassessing risk factors for QTc prolongation. The daily dosage of citalopram was recorded cross-sectionally at admission, and dose increases and decreases were not captured. Laboratory monitoring was not standardized at admission, so not all patients received the same screening at baseline. For example, those individuals with a cardiac complaint at admission may have been more likely to have a magnesium level drawn and an ECG performed. At the same time, missing values were treated as “risk factor not present,” so it is possible our study underestimates the proportion of patients with hypomagnesemia taking citalopram at higher-than-recommended doses and/or in the presence of multiple concomitant risk factors for QTc prolongation. Pre- and post-citalopram dosage ECG data are not available to facilitate an assessment of QTc change as it relates to citalopram administration. It is unknown if the prescribers at the institution received any other education, such as a grand rounds presentation, regarding the new dosage limitations besides the issuance of the FDA warning. We do know that no formal education program was provided by the pharmacy department to the prescribers at the institution.
CONCLUSION
Patterns of citalopram prescribing for patients 60 years of age and older remained stable at the study institution before and after the issuance of the FDA warning, which recommended a maximum dosage of 20 mg per day in this population. Nearly 30% of subjects were prescribed doses in excess of 20 mg daily. No significant differences were seen in the prevalence of risk factors for QTc prolongation prewarning and postwarning, except a higher percentage had left ventricular hypertrophy or history of syncope prior to the warning and a higher percentage were taking concomitant proarrhythmic medications after it was issued. A significantly higher percentage of subjects received ECG monitoring after the warning, though relationship to the FDA warning cannot be determined.
Given the risks of QTc prolongation with high-dose citalopram and the theoretical risk of torsades de points and sudden cardiac death, it is important to recognize and modify risk factors. Electrolytes and concomitant QTc-prolonging medications may be the most appropriate targets for intervention. Prescribers may not recognize concomitant proarrhythmic drugs when prescribed, or they may be unaware of the FDA warning regarding increased risk of QTc prolongation with citalopram. Prescribers might benefit from educational interventions designed to increase awareness of the importance of identifying nonmodifiable and modifiable risk factors at baseline and obtaining an ECG for QTc determination before contemplating a high dose of citalopram (as well as other medications associated with QTc prolongation). Risk assessment tools and QTc alert systems have been implemented in other institutions and may be strategies to consider in institutions that have not yet adopted them. An alert system through computerized physician order entry to immediately notify prescribers of concomitant QTc-prolonging medications at the time of entry may decrease the incidence of prescribing these agents, but such a strategy may also lead to “alert fatigue.”
Drug names: amiodarone (Nexterone, Cordarone, and others), citalopram (Celexa and others), escitalopram (Lexapro and others), fluoxetine (Prozac and others), haloperidol (Haldol and others), methadone (Methadose and others), moxifloxacin (Avelox and others), olanzapine (Zyprexa), paroxetine (Paxil, Pexeva, and others), sertraline (Zoloft and others), trazodone (Oleptro and others).
Potential conflicts of interest: None reported.
Funding/support: None reported.
References
- 1.US Food and Drug Administration. FDA drug safety communication: abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide) August 24, 2011. http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Updated March, 28, 2012. Accessed August 1, 2012.
- 2.Marcum ZA, Vande Griend JP, Linnebur SA. FDA drug safety communications: a narrative review and clinical considerations for older adults. Am J Geriatr Pharmacother. 2012;10(4):264–271. doi: 10.1016/j.amjopharm.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evaluation of the effects of sequential multiple-dose regimens of citalopram on cardiac repolarization in healthy subjects. http:// http://www.forestclinicaltrials.com/default.aspx. Accessed October 1, 2014.
- 4.Bazett JC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:353–370. [Google Scholar]
- 5.Al-Khatib SM, LaPointe NM, Kramer JM, et al. What clinicians should know about the QT interval. JAMA. 2003;289(16):2120–2127. doi: 10.1001/jama.289.16.2120. [DOI] [PubMed] [Google Scholar]
- 6.Arizona Cert–Center for Education and Research on Therapeutics. http://www.crediblemeds.org. Accessed December 1, 2012.
- 7.Alvarez PA, Pahissa J. QT alterations in psychopharmacology: proven candidates and suspects. Curr Drug Saf. 2010;5(1):97–104. doi: 10.2174/157488610789869265. [DOI] [PubMed] [Google Scholar]
- 8.Vieweg WV, Hasnain M, Howland RH, et al. Citalopram, QTc interval prolongation, and torsade de pointes: how should we apply the recent FDA ruling? Am J Med. 2012;125(9):859–868. doi: 10.1016/j.amjmed.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Castro VM, Clements CC, Murphy SN, et al. QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ. 2013;346(3):f288. doi: 10.1136/bmj.f288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zivin K, Pfeiffer PN, Bohnert AS, et al. Evaluation of the FDA warning against prescribing citalopram at doses exceeding 40 mg. Am J Psychiatry. 2013;170(6):642–650. doi: 10.1176/appi.ajp.2013.12030408. [DOI] [PubMed] [Google Scholar]
- 11.Meyer-Massetti C, Cheng CM, Sharpe BA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8–E16. doi: 10.1002/jhm.691. [DOI] [PubMed] [Google Scholar]
- 12.Muzyk AJ, Rayfield A, Revollo JY, et al. Examination of baseline risk factors for QTc interval prolongation in patients prescribed intravenous haloperidol. Drug Saf. 2012;35(7):547–553. doi: 10.2165/11599960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Haugaa KH, Bos JM, Tarrell RF, et al. Institution-wide QT alert system identifies patients with a high risk of mortality. Mayo Clin Proc. 2013;88(4):315–325. doi: 10.1016/j.mayocp.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Muzyk AJ, Rivelli SK, Jiang W, et al. A computerized physician order entry set designed to improve safety of intravenous haloperidol utilization: a retrospective study in agitated hospitalized patients. Drug Saf. 2012;35(9):725–731. doi: 10.1007/BF03261969. [DOI] [PubMed] [Google Scholar]
- 15.van der Sijs H, Aarts J, Vulto A, et al. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;13(2):138–147. doi: 10.1197/jamia.M1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evaluation of the effects of sequential multiple-dose regimens of escitalopram on cardiac repolarization in healthy subjects. http://www.forestclinicaltrials.com/default.aspx. Accessed October 1, 2014.
- 17.Beach SR, Celano CM, Noseworthy PA, et al. QTc prolongation, torsades de pointes, and psychotropic medications. Psychosomatics. 2013;54(1):1–13. doi: 10.1016/j.psym.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Glassman AH, O’Connor CM, Califf RM, et al. Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288(6):701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 19.Jiang W, O’Connor C, Silva SG, et al. SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with CHF (SADHART-CHF): a randomized, double-blind, placebo-controlled trial of sertraline for major depression with congestive heart failure. Am Heart J. 2008;156(3):437–444. doi: 10.1016/j.ahj.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanash JA, Hansen BH, Hansen JF, et al. Cardiovascular safety of one-year escitalopram therapy in clinically nondepressed patients with acute coronary syndrome: results from the DEpression in patients with Coronary ARtery Disease (DECARD) trial. J Cardiovasc Pharmacol. 2012;60(4):397–405. doi: 10.1097/FJC.0b013e3182677041. [DOI] [PubMed] [Google Scholar]