Abstract
Background
Carvedilol is a third-generation β-blocker indicated for congestive heart failure and high blood pressure. The aim of this study was to investigate the dose proportionality of the carvedilol sustained-release (SR) formulation in healthy male subjects.
Methods
An open-label, single dose-ascending, 10-sequence, 3-period balanced incomplete block study was performed using healthy male subjects. In varying sequences, each subject received three of five carvedilol SR formulations (8, 16, 32, 64, or 128 mg once). The treatment periods were separated by a washout period of 7 days. Serial blood samples were collected up to 48 h after dosing. The plasma concentrations of carvedilol were determined by using validated liquid chromatography–tandem mass spectrometry. Pharmacokinetic parameters including the area under the plasma concentration–time curve (AUC) from time 0 to the last measurable time (AUClast), AUC extrapolated to infinity (AUCinf), and the measured peak plasma concentration (Cmax) were obtained by noncompartmental analysis. Dose proportionality was evaluated if the ln–ln plots of AUClast, AUCinf, and Cmax versus dose were linear and the 90% confidence intervals (CIs) of the slopes were within 0.9195 and 1.0805. Tolerability was assessed by vital signs, electrocardiogram, clinical laboratory tests, and monitoring of adverse events (AEs) throughout the study.
Results
A total of 31 subjects were enrolled, and 30 completed the study. The assessment of dose proportionality meets the statistical criteria; the point estimates of slope were 1.0104 (90% CI: 0.9849–1.0359) for AUClast, 1.0003 (90% CI: 0.9748–1.0258) for AUCinf, and 0.9901 (90% CI: 0.9524–1.0277) for Cmax, respectively. All AEs were mild, and none of the subjects dropped out due to AEs.
Conclusion
In this study, exposure to carvedilol was proportional over the therapeutic dose range of 8–128 mg. The carvedilol SR formulation was well tolerated.
Keywords: dose linearity, carvedilol, sustained release, healthy subjects
Introduction
Carvedilol is a third-generation β-blocker indicated in the treatment of congestive heart failure and high blood pressure.1–3 In addition to its β-blocking properties, it has blocking effect at α1-adrenoreceptor, and exhibits low levels of intrinsic sympathomimetic activity (ISA).4 The lack of ISA reduces side effects and makes carvedilol better tolerated than the other β-blockers.5
Carvedilol was developed as an immediate-release (IR) formulation in 1995.6 It is rapidly absorbed with time to maximum concentration (tmax) at 1–2 h, and then declines with a terminal half-life of approximately 7–10 h; thus, twice-daily dosing is recommended. It is extensively metabolized primarily by CYP2D6, and greater than 98% of the drug is bound to plasma proteins, primarily albumin.7,8
A new sustained-release (SR) formulation of carvedilol was approved in 2006 by the Food and Drug Administration (FDA) for all of the same indications as twice-daily carvedilol based on several clinical trials.9,10 The tmax of carvedilol SR formulation was reached approximately 4–6 h after drug administration, and the maximum concentration (Cmax) and area under the plasma concentration–time curve (AUC) did not differ for the IR and SR formulations in patients.11,12 In a previous report, drug-taking compliance with carvedilol SR was comparable to carvedilol IR formulations, and there were no differences in adverse events (AEs) among patients switching from carvedilol IR to SR formulations.13
In Korea, the SR formulation of carvedilol was also developed by Chong Kun Dang Pharmaceutical Corp. (Seodaemun-gu, Seoul, Republic of Korea). From a study to compare the pharmacokinetics between carvedilol IR 25 mg twice daily and SR 64 mg once daily, the Cmax and AUC were found equivalent. As a drug label, the therapeutic dose range of IR carvedilol was 3.125–50 mg twice daily,14 but the therapeutic dose range of SR formulations is expected to be 8–128 mg once daily.
The aim of this study was to investigate the pharmacokinetics and dose proportionality of the carvedilol SR formulation across the dose range of 8–128 mg in healthy male subjects.
Materials and methods
Subjects
Healthy male volunteers aged 20–55 years and having a body mass index (BMI) of 19–26 kg/m2 were eligible for this study. Volunteers were considered to be in good health based on medical history, physical examinations, vital signs (systolic blood pressure [SBP], diastolic blood pressure [DBP], heart rate [HR], and body temperature), 12-lead electrocardiogram (ECG), clinical laboratory tests (hematology, blood chemistry, and urinalysis), serology (human immunodeficiency virus antibody, hepatitis B surface antigen, hepatitis C virus, and syphilis high quality reagin test), and urine drug screening (amphetamine, cocaine, opiate, barbiturates, benzodiazepine, tetrahydrocannabinol, and methadone) within 4 weeks of the first administration of the study drug. Volunteers with a sitting SBP ≥140 or <90 mmHg, DBP ≥90 or <60 mmHg, or HR of >95 or <55 beats per minute were excluded. Volunteers with known allergy or hypersensitivity to carvedilol, or with a history of drug abuse were also excluded from the study.
The study protocol was approved by the Korean Food and Drug Administration (KFDA) and the institutional review board of Asan Medical Center (AMC), Seoul, Republic of Korea. All volunteers provided written informed consent prior to screening tests. This trial was registered with the identifier number NCT01369472 at ClinicalTrials.gov.
Study design
This study was designed as an open-label, single dose-ascending, 10-sequence, 3-period balanced incomplete block study (Figure 1). Subjects were randomly assigned to one of ten sequences and received three of five carvedilol SR formulations (8, 16, 32, 64, or 128 mg once). All treatments were given after consuming a standardized meal. The study drug was administered 30 min after the start of the meal with 240 mL of water. After the drug administration, the subjects were required to fast for 4 h. Following a 1-week washout interval, subjects received alternate formulations.
Figure 1.
Study flow with carvedilol SR dosages.
Abbreviation: SR, sustained release.
For each treatment period, subjects were admitted in the Clinical Trial Center (CTC) at AMC from day 1 through day 2 (24 h after dosing). On days 2 (36 h after dosing) and 3 (48 h after dosing), subjects were asked to revisit the CTC to assess the tolerability and pharmacokinetics of carvedilol. The schedule for the second and third treatment period procedures was the same as in the first period. Follow-up visits were performed within 6–8 days after the last treatment.
For pharmacokinetic analysis, sequential blood samples were collected prior to and at 1, 2, 4, 5, 6, 8, 12, 16, 24, 36, and 48 h after dosing. All blood samples for the determination of carvedilol concentrations were drawn into a heparinized tube and separated by centrifugation at 1,800× g centrifugation for 8 min at 4°C and stored at −70°C until analysis.
Tolerability was assessed by vital signs (SBP, DBP, HR, and body temperature), 12-lead ECG, clinical laboratory tests (hematology, blood chemistry, and urinalysis), physical examinations, and monitoring of AEs. SBP and DBP were recorded at predose baseline and at 4, 8, 12, 24, and 48 h after each study drug administration. The clinical importance of any AEs, vital signs, or laboratory test results was evaluated by the study investigators.
Determination of carvedilol concentrations
Plasma concentrations of carvedilol were determined using a validated high-performance liquid chromatography (HPLC) coupled with the tandem mass spectrometry method. The internal standard (IS) was venlafaxine. The sample extracts were analyzed using HPLC (Agilent 1200; Agilent, Waldbronn, Germany) and a Synergi 4 μ Polar-RP 80 Å column (4.0 μm, 100×2.0 mm; Phenomenex, Torrance, CA, USA) with mobile phase consisting of ammonium formate and acetonitrile with methanol (40:60, v/v).
The MS system (4000 QTRAP®; AB Sciex, Redwood City, CA, USA) was operated in positive ion electrospray mode with multiple reaction monitoring (MRM). For carvedilol and IS, the precursor-to-production reactions monitored were m/z 407.2→100.2 and 278.0→58.0, respectively.
Calibration curves covered the concentration range of 0.1–200 ng/mL (R2 >0.999). Using this assay, interday accuracy ranged from 100.35% to 110.73%, and interday precision, expressed as percent coefficient of variation (%CV), ranged from 3.82% to 12.92%. In addition, intraday accuracy and precision (%CV) ranged from 102.31% to 106.93%, and from 3.10% to 10.02%, respectively.
Pharmacokinetic assessment and statistical analysis
The plasma concentration–time profiles of carvedilol of each subject were analyzed by a noncompartmental method using WinNonlin® 6.1 (Pharsight Corporation, Mountain View, CA, USA). All analyses were made using actual times of sampling. The peak plasma concentration (Cmax) and time at Cmax (tmax) were determined from the observed values. The terminal elimination rate constant (λz) was estimated by linear regression of the terminal log-linear portion of the plasma concentration–time curves. The area under the time–concentration curve (AUC) from time 0 to the last measurable time (AUClast) was calculated by the trapezoidal rule, and the AUC extrapolated to infinity (AUCinf) was obtained AUClast + Clast/λz (Clast: the last quantifiable concentration). The t½β was calculated for each participant as ln(2)/λz.
All statistical analyses were performed using SAS® 9.3 (SAS Korea, Gangnam-gu, Seoul, Republic of Korea) and WinNonlin® 6.1 (Pharsight Corporation, Mountain View, CA, USA). Demographic data and pharmacokinetic parameters were summarized using descriptive statistics.
The dose proportionality of carvedilol over the dose range 8–128 mg was assessed by fitting a power model. The power model assumes a linear relationship between natural log-transformed pharmacokinetic exposure parameter (AUClast, AUCinf, and Cmax) and natural log-transformed dose; ln(PK) = β0 + β1 − ln(dose). The proportionality constant (β1) and its corresponding 90% confidence interval (CI) were compared with the modified acceptance range; lower limit as 1+(ln(0.8)/ln(r)) and upper limit as 1+(ln(1.25)/ln(r)), where r was the maximal dose ratio for the study.15–17 In this study, the maximal dose ratio was 16 (128/8), so the acceptance range was 0.9195–1.0805.
In addition to the power model, analysis of variance (ANOVA) model with factors for sequence, subject within sequence, period, and treatment were used to investigate the natural log-transformed, dose-normalized pharmacokinetic parameters including AUClast, AUCinf, and Cmax.18 P-values <0.05 were deemed to indicate statistical significance.
Results
Study participants
A total of 31 healthy Korean volunteers were enrolled, and 30 subjects completed the study. One subject was dropped by the principal investigator for taking concomitant medication without notice. The mean (standard deviation) age of study participants was 25.06±3.55 years, the mean weight was 68.67±7.64 kg, and the mean height was 174.57±6.23 cm.
Pharmacokinetic analysis
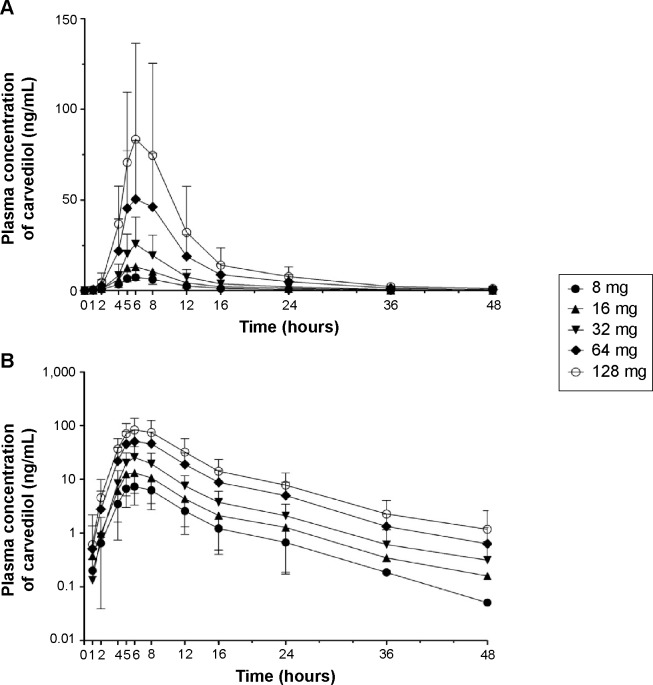
Thirty subjects, who completed the study, were included for pharmacokinetic analysis. The mean plasma carvedilol concentration–time profile is presented in Figure 2. The geometric mean Cmax increased from 6.93 to 77.04 ng/mL, and the geometric mean AUCinf increased from 60.84 to 703.29 ng·h/mL with an increase in the carvedilol dose from 8 mg to 128 mg (Table 1). Regarding the carvedilol dose, the median tmax was about 6.0 h, and the geometric mean half-life ranged from 6.73 to 7.67 h at each dose level.
Figure 2.
Mean (SD) plasma concentration–time curves of carvedilol SR formulations: (A) linear; (B) log-linear.
Abbreviations: SD, standard deviation; SR, sustained release.
Table 1.
Pharmacokinetic parameters of carvedilol SR by each dose group
| Parametera | AUClast (ng·h/mL) | AUCinf (ng·h/mL) | Cmax (ng/mL) | t½β (h) | tmax (h) |
|---|---|---|---|---|---|
| 8 mg | 58.29 (66.83)b | 60.84 (65.11) | 6.93 (63.19) | 6.73 (42.75) | 5.98 (4.0, 8.0) |
| 16 mg | 100.3 (69.92) | 104.16 (68.85) | 12.26 (53.52) | 6.96 (39.41) | 6.0 (5.0, 8.0) |
| 32 mg | 184.11 (62.74) | 188.78 (62.95) | 22.6 (65.83) | 7.38 (41.33) | 6.0 (5.0, 15.98) |
| 64 mg | 413.51 (68.59) | 423.02 (68.32) | 46.31 (64.04) | 7.74 (47.67) | 6.02 (5.0, 8.02) |
| 128 mg | 689.35 (62.76) | 703.29 (63.95) | 77.04 (66.99) | 7.67 (41.93) | 6.02 (5.0, 11.98) |
Notes:
n=18.
Data presented as geometric mean CV, except for tmax, for which median (min, max) is shown.
Abbreviations: AUClast, area under the plasma concentration–time curve from time 0 to last measurable time point; AUCinf, area under the plasma concentration–time curve from time 0 to infinity; Cmax, measured peak plasma concentration; CV, coefficient of variation; t½β, terminal half-life; tmax, time to reach peak concentration; SR, sustained release.
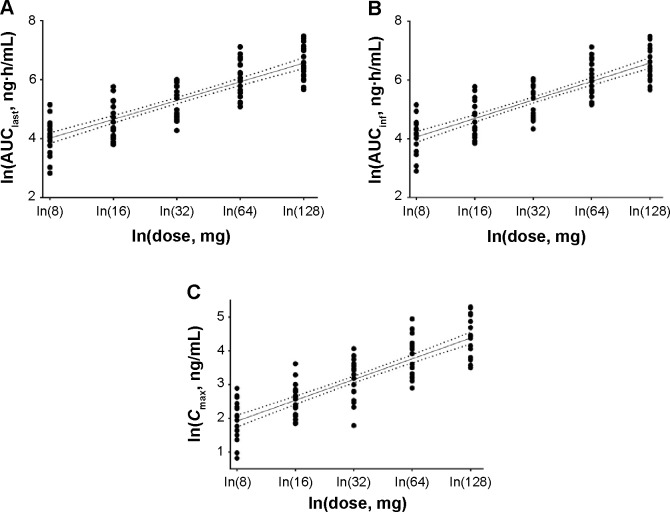
Carvedilol AUClast, AUCinf, and Cmax were proportional to dose. The plots of the function fitted for the power model with 90% CIs were presented for AUClast, AUCinf, and Cmax in Figure 3. The estimate of the proportionality constant (90% CI) for AUClast, AUCinf, and Cmax were 1.0104 (0.9849–1.0359), 1.0003 (0.9748–1.0258), and 0.9901 (0.9524, 1.0277), respectively. The estimates and 90% CIs all fell within the prespecified range (0.9195–1.0805). When analyzed using the ANOVA model, the dose-adjusted AUClast, AUCinf, and Cmax were not statistically different among all treatments (Tables 2 and 3). Thus, carvedilol systemic exposure was concluded to be dose proportional over the therapeutic dose range of 8–128 mg.
Figure 3.
Relationship between the extent of systemic exposure and dose following single administration of carvedilol SR formulation ranging from 8 to 128 mg.
Notes: Mean (SD) plasma concentration–time curves of carvedilol SR formulations. (A) AUClast, (B) AUCinf, (C) Cmax. The circles are observed values, the solid lines are the fitted values based on the power model, and the dotted lines are the 90% confidence intervals.
Abbreviations: AUClast, area under the plasma concentration–time curve from time 0 to last measurable time point; AUCinf, area under the plasma concentration–time curve from time 0 to infinity; Cmax, measured peak plasma concentration; SD, standard deviation; SR, sustained release.
Table 2.
Summary of analysis of variance for dose-normalized pharmacokinetic parameters of carvedilol
| Parameters | Source | Degree of freedom | Sum of squares | Mean square | F value | P-value |
|---|---|---|---|---|---|---|
| AUClast/dose | Sequence | 9 | 5.166555 | 0.574062 | 0.6 | 0.7818 |
| Subject (sequence) | 20 | 22.15506 | 1.107753 | 62.3 | <0.0001 | |
| Period | 2 | 0.017512 | 0.008756 | 0.49 | 0.6138 | |
| Dose | 4 | 0.022278 | 0.00557 | 0.31 | 0.8679 | |
| Error | 54 | 0.960124 | 0.01778 | |||
| AUCinf/dose | Sequence | 9 | 5.254612 | 0.583846 | 0.62 | 0.7679 |
| Subject (sequence) | 20 | 21.89227 | 1.094613 | 61.41 | <0.0001 | |
| Period | 2 | 0.015427 | 0.007714 | 0.43 | 0.6509 | |
| Dose | 4 | 0.025575 | 0.006394 | 0.36 | 0.8368 | |
| Error | 54 | 0.962456 | 0.017823 | |||
| Cmax/dose | Sequence | 9 | 3.48442 | 0.387158 | 0.46 | 0.8864 |
| Subject (sequence) | 20 | 19.564 | 0.9782 | 25.29 | <0.0001 | |
| Period | 2 | 0.000868 | 0.000434 | 0.01 | 0.9889 | |
| Dose | 4 | 0.071528 | 0.017882 | 0.46 | 0.7631 | |
| Error | 54 | 2.088889 | 0.038683 |
Abrreviations: AUClast, area under the plasma concentration–time curve from time 0 to last measurable time point; AUCinf, area under the plasma concentration–time curve from time 0 to infinity; Cmax, measured peak plasma concentration.
Table 3.
Summary of geometric mean ratio for dose-normalized pharmacokinetic parameters of carvedilol
| Parameter
|
AUClast/dose
|
AUCinf/dose
|
Cmax/dose
|
|||
|---|---|---|---|---|---|---|
| Dose (mg) | GMR | P-value | GMR | P-value | GMR | P-value |
| 16 vs 8 | 0.9388 | 0.3220 | 0.9329 | 0.2771 | 0.9619 | 0.6785 |
| 16 vs 32 | 0.9804 | 0.7387 | 0.9853 | 0.8035 | 0.9314 | 0.4186 |
| 16 vs 64 | 1.0109 | 0.8946 | 1.0234 | 0.7779 | 0.9602 | 0.7368 |
| 32 vs 8 | 0.9576 | 0.6219 | 0.9468 | 0.5346 | 1.0328 | 0.8030 |
| 32 vs 64 | 1.0312 | 0.6061 | 1.0387 | 0.5245 | 1.0310 | 0.7278 |
| 64 vs 8 | 0.9287 | 0.5114 | 0.9116 | 0.4124 | 1.0018 | 0.9915 |
| 128 vs 8 | 0.9127 | 0.5153 | 0.9004 | 0.4558 | 0.9296 | 0.7240 |
| 128 vs 16 | 0.9722 | 0.8022 | 0.9652 | 0.7531 | 0.9664 | 0.8369 |
| 128 vs 32 | 0.9531 | 0.5845 | 0.9510 | 0.5678 | 0.9001 | 0.4171 |
| 128 vs 64 | 0.9828 | 0.7848 | 0.9878 | 0.8466 | 0.9280 | 0.4259 |
Abbreviations: AUClast, area under the plasma concentration–time curve from time 0 to last measurable time point; AUCinf, area under the plasma concentration–time curve from time 0 to infinity; Cmax, measured peak plasma concentration; GMR, geometric mean ratio; vs, versus.
Tolerability
Overall, carvedilol was well tolerated. Twelve subjects experienced a total of 13 AEs, among which 11 events in 11 subjects were considered “possibly related” to the study drug (Table 4). All AEs were of mild severity, and resolved without sequelae. No death or serious AE occurred during the entire course of the study. Likewise, there were no clinically significant abnormalities in physical examinations, or ECGs.
Table 4.
Summary of adverse events
| Adverse eventsa | 8 mg (n=18) | 16 mg (n=19) | 32 mg (n=18) | 64 mg (n=18) | 128 mg (n=18) | Total |
|---|---|---|---|---|---|---|
| Dizzinessb | 0 (0) | 1 (1) | 0 (0) | 1 (1) | 4 (4) | 6 (6) |
| Headacheb | 0 (0) | 0 (0) | 1 (1) | 1 (1) | 1 (1) | 3 (3) |
| Light-headednessb | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 1 (1) |
| Paresthesiab | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 1 (1) |
| Bilirubin total increased | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) |
| Blepharospasm | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (1) |
Notes:
Data presented as number of subjects (number of events);
drug-related adverse events.
Decreases in mean systolic and diastolic blood pressure were observed 4–12 h after the study drug administration compared with baseline (Figure 4); however, the changes were not clinically significant. The lowest mean SBP values were 106.1 mmHg at 8 mg and 97.6 mmHg at 128 mg group, which were measured 8 h after administration, respectively. The lowest mean DBP values were 62.8 mmHg at 8 mg and 56.3 mmHg at 128 mg group, which were measured 8 h after administration, respectively.
Figure 4.
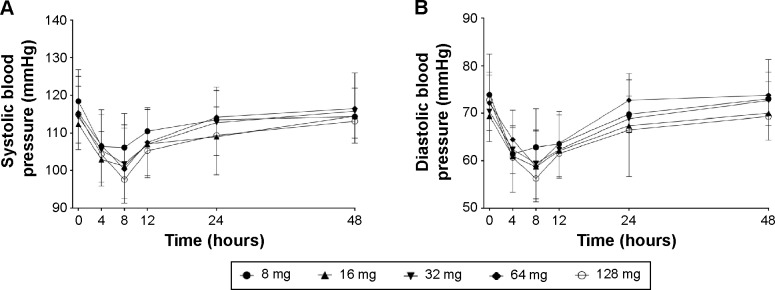
Mean (SD) (A) systolic and (B) diastolic blood pressure after administration of carvedilol SR formulation in healthy male volunteers.
Abbreviations: SD, standard deviation; SR, sustained release.
Discussion
The current study was designed to evaluate the dose proportionality and pharmacokinetics of single-dose carvedilol SR formulations in healthy male subjects. Carvedilol systemic exposure was dose proportional over the dose range of 8–128 mg. The pharmacokinetic parameters are consistent with former reports.9 These results demonstrate that there is a predictable and consistent dose–response relationship among the five different dose levels of carvedilol SR formulations.
A comparison of three or more formulations of a study drug shows that a balanced incomplete block design has some advantages over a complete crossover design. First, the subject is less likely to drop out. Second, the trial execution timeline is reduced. Third, the total blood sampling volume of the subject is also decreased. Fourth, statistical analysis is simple such that the balance is preserved.19,20
Carvedilol is a racemic mixture of two enantiomers, R(+)-carvedilol and S(−)-carvedilol.21 Both enantiomers have α1-blocking activity, but S(−)-carvedilol primarily has a β-adrenoreceptor blocking activity.22 The S(−)-carvedilol is metabolized faster than the R(+)-carvedilol in human cytochrome P450 enzymes.23 Thus, the Cmax and AUC for the R(+)-carvedilol were shown to be two to three times larger than those of S(−)-carvedilol in healthy subjects.24
In this study, we additionally measured the concentration of R(+)-carvedilol and S(−)-carvedilol, respectively. The pharmacokinetic parameters of R(+)-carvedilol and S(−)-carvedilol were presented at Table 5. In S(−)-carvedilol, the data for the 8-mg dose group were not presented because the concentration–time profiles were not consistently well described. The estimates of the proportionality constant (90% CI) for AUClast and Cmax of R(+)-carvedilol 8–128 mg were 1.0861 (1.0439–1.1283), and 1.0493 (0.9913, 1.1074), respectively. The estimates of the proportionality constant (90% CI) for AUClast and Cmax of S(−)-carvedilol 16–128 mg were 1.0956 (1.0023–1.1889), and 1.0103 (0.9000, 1.1206), respectively. Although the data for the lowest-dose group (8 mg) of S(−)-carvedilol were excluded because of insufficient data to obtain pharmacokinetic parameters, the racemic mixtures of carvedilol were also proportional to dose.
Table 5.
Pharmacokinetic parameters of R(+)- and S(−)-carvedilol by each dose group
| Parametera |
R(+)-carvedilol
|
S(−)-carvedilolb
|
||||
|---|---|---|---|---|---|---|
| AUClast (ng·h/mL) | Cmax (ng/mL) | tmax(h)c | AUClast (ng·h/mL) | Cmax (ng/mL) | tmax(h)c | |
| 8 mg | 43.81 (94.11) | 6.31 (81.52) | 5.95 (4.00, 8.00) | – | – | – |
| 16 mg | 88.09 (80.93) | 12.44 (68.91) | 5.98 (4.00, 8.02) | 34.7 (106.35) | 4.96 (100.56) | 6.00 (4.95, 8.02) |
| 32 mg | 189.28 (84.52) | 25.84 (95.34) | 5.98 (4.00, 15.97) | 71.15 (84.18) | 9.52 (84.55) | 5.99 (4.00, 15.97) |
| 64 mg | 367.22 (92.24) | 44.73 (88.5) | 6.04 (5.00, 8.00) | 160.28 (78.34) | 18.09 (78.59) | 6.05 (5.98, 8.00) |
| 128 mg | 606.98 (81.75) | 76.1 (88.85) | 6.01 (5.00, 12.00) | 272.9 (66.12) | 31.8 (71.17) | 7.99 (5.00, 12.00) |
Notes:
n=18.
The 8 mg dose group of S(−)-carvedilol was not presented due to insufficient data.
Data presented as geometric mean and CV, except for tmax, for which median (min, max) is shown.
Abbreviations: AUClast, area under the plasma concentration–time curve from time 0 to last measurable time point; Cmax, measured peak plasma concentration; CV, coefficient of variation; tmax, time to reach peak concentration.
The most common AEs were dizziness and headache, which were likely due to the pharmacologic effects of lowering blood pressure in healthy volunteers. These AEs were similar and consistent with the known safety profile of carvedilol.25 Moreover, all AEs were mild and resolved without treatment, and the decreased blood pressures also resolved within 24 h without any clinically related symptoms.
Because all of the subjects in the current study were male, sex differences in the pharmacokinetics of carvedilol were not investigated. As a recent report, bioavailability of carvedilol in female subjects was slightly higher than that in male subjects, but these differences could be explained by the lower body weight of females.26 On the other hand, as drug label, there were no age- or gender-related differences in response to carvedilol.14 Thus, dose adjustment based on clinical status of patients would be helpful.
Conclusion
In conclusion, exposure to carvedilol was proportional over the therapeutic dose range of 8–128 mg in this study. Based on the results, a predictable and linear increase in systemic exposure of carvedilol can be expected. The carvedilol SR formulation was well tolerated.
Acknowledgments
The study was funded by Chong Kun Dang Pharmaceutical Corp. (Seoul, Republic of Korea).
Footnotes
Disclosure
Chin Kim is an employee of Chong Kun Dang Pharmaceutical Corp. The other authors report no conflicts of interest in this work.
References
- 1.Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med. 1996;334(21):1349–1355. doi: 10.1056/NEJM199605233342101. [DOI] [PubMed] [Google Scholar]
- 2.Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet. 2003;362(9377):7–13. doi: 10.1016/S0140-6736(03)13800-7. [DOI] [PubMed] [Google Scholar]
- 3.Moser M, Frishman W. Results of therapy with carvedilol, a beta-blocker vasodilator with antioxidant properties, in hypertensive patients. Am J Hypertens. 1998;11(1 Pt 2):15S–22S. doi: 10.1016/s0895-7061(97)00424-x. [DOI] [PubMed] [Google Scholar]
- 4.McTavish D, Campoli-Richards D, Sorkin EM. Carvedilol. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy. Drugs. 1993;45(2):232–258. doi: 10.2165/00003495-199345020-00006. [DOI] [PubMed] [Google Scholar]
- 5.Yoshikawa T, Port JD, Asano K, et al. Cardiac adrenergic receptor effects of carvedilol. Eur Heart J. 1996;17(Suppl B):8–16. doi: 10.1093/eurheartj/17.suppl_b.8. [DOI] [PubMed] [Google Scholar]
- 6.Frishman WH. Carvedilol. N Engl J Med. 1998;339(24):1759–1765. doi: 10.1056/NEJM199812103392407. [DOI] [PubMed] [Google Scholar]
- 7.Morgan T. Clinical pharmacokinetics and pharmacodynamics of carve-dilol. Clin Pharmacokinet. 1994;26(5):335–346. doi: 10.2165/00003088-199426050-00002. [DOI] [PubMed] [Google Scholar]
- 8.Zhou HH, Wood AJ. Stereoselective disposition of carvedilol is determined by CYP2D6. Clin Pharmacol Ther. 1995;57(5):518–524. doi: 10.1016/0009-9236(95)90036-5. [DOI] [PubMed] [Google Scholar]
- 9.Tenero DM, Henderson LS, Baidoo CA, et al. Pharmacokinetic properties of a new controlled-release formulation of carvedilol. Am J Cardiol. 2006;98(7A):5L–16L. doi: 10.1016/j.amjcard.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Fonarow GC. Profile of carvedilol controlled-release: a new once-daily formulation of carvedilol. Expert Opin Pharmacother. 2006;7(18):2533–2546. doi: 10.1517/14656566.7.18.2533. [DOI] [PubMed] [Google Scholar]
- 11.Henderson LS, Tenero DM, Baidoo CA, et al. Pharmacokinetic and pharmacodynamic comparison of controlled-release carvedilol and immediate-release carvedilol at steady state in patients with hypertension. Am J Cardiol. 2006;98(7A):17L–26L. doi: 10.1016/j.amjcard.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 12.Packer M, Lukas MA, Tenero DM, Baidoo CA, Greenberg BH, Study G. Pharmacokinetic profile of controlled-release carvedilol in patients with left ventricular dysfunction associated with chronic heart failure or after myocardial infarction. Am J Cardiol. 2006;98(7A):39L–45L. doi: 10.1016/j.amjcard.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Udelson JE, Pressler SJ, Sackner-Bernstein J, et al. Adherence with once daily versus twice daily carvedilol in patients with heart failure: the compliance and quality of life study comparing once-daily controlled-release carvedilol CR and twice-daily immediate-release carvedilol IR in patients with heart failure (CASPER) trial. J Card Fail. 2009;15(5):385–393. doi: 10.1016/j.cardfail.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 14.Dilatrend® (carvedilol) [Product Information] NSW, Australia: Roche Products Pty Limited; [Accessed February 10, 2015]. Available from: http://www.roche-australia.com/content/dam/internet/corporate/roche/en_AU/files/cardiac_agents/dilatrend-pi.pdf. [Google Scholar]
- 15.Smith BP, Vandenhende FR, DeSante KA, et al. Confidence interval criteria for assessment of dose proportionality. Pharm Res. 2000;17(10):1278–1283. doi: 10.1023/a:1026451721686. [DOI] [PubMed] [Google Scholar]
- 16.Hummel J, McKendrick S, Brindley C, French R. Exploratory assessment of dose proportionality: review of current approaches and proposal for a practical criterion. Pharm Stat. 2009;8(1):38–49. doi: 10.1002/pst.326. [DOI] [PubMed] [Google Scholar]
- 17.Sheng Y, He Y, Huang X, Yang J, Wang K, Zheng Q. Systematic evaluation of dose proportionality studies in clinical pharmacokinetics. Curr Drug Metab. 2010;11(6):526–537. doi: 10.2174/138920010791636185. [DOI] [PubMed] [Google Scholar]
- 18.Bass A, Stark JG, Pixton GC, et al. Dose proportionality and the effects of food on bioavailability of an immediate-release oxycodone hydrochloride tablet designed to discourage tampering and its relative bioavailability compared with a marketed oxycodone tablet under fed conditions: a single-dose, randomized, open-label, 5-way crossover study in healthy volunteers. Clin Ther. 2012;34(7):1601–1612. doi: 10.1016/j.clinthera.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 19.Westlake WJ. The use of balanced incomplete block designs in comparative bioavailability trails. Biometrics. 1974;30(2):319–327. [PubMed] [Google Scholar]
- 20.Chow SC, Liu JP. Design and Analysis of Bioavailability and Bioequivalence Studies. 3rd ed. Boca Raton, FL: CRC Press; 2009. [Google Scholar]
- 21.Neugebauer G, Akpan W, Kaufmann B, Reiff K. Stereoselective disposition of carvedilol in man after intravenous and oral administration of the racemic compound. Eur J Clin Pharmacol. 1990;38(Suppl 2):S108–S111. doi: 10.1007/BF01409476. [DOI] [PubMed] [Google Scholar]
- 22.Nichols AJ, Sulpizio AC, Ashton DJ, Hieble JP, Ruffolo RR., Jr The interaction of the enantiomers of carvedilol with alpha 1- and beta 1- adrenoceptors. Chirality. 1989;1(4):265–270. doi: 10.1002/chir.530010404. [DOI] [PubMed] [Google Scholar]
- 23.Oldham HG, Clarke SE. In vitro identification of the human cytochrome P450 enzymes involved in the metabolism of R(+)- and S(−)-carvedilol. Drug Metab Dispos. 1997;25(8):970–977. [PubMed] [Google Scholar]
- 24.Gehr TW, Tenero DM, Boyle DA, Qian Y, Sica DA, Shusterman NH. The pharmacokinetics of carvedilol and its metabolites after single and multiple dose oral administration in patients with hypertension and renal insufficiency. Eur J Clin Pharmacol. 1999;55(4):269–277. doi: 10.1007/s002280050628. [DOI] [PubMed] [Google Scholar]
- 25.Mori Y, Nishikawa Y, Iizuka T, et al. Artist(R) tablets (carvedilol) for hypertensive patients in Japan: results of a drug use survey. Drugs R D. 2011;11(2):171–190. doi: 10.2165/11592450-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abbas M, Khan AM, Riffat S, Tipu MY, Nawaz HA, Usman M. Assessment of sex differences in Pharmacokinetics of carvedilol in human. Pak J Pharm Sci. 2014;27(5):1265–1269. [PubMed] [Google Scholar]