Abstract
Objective. To determine the impact of incorporating standardized colleague simulations on pharmacy students’ confidence and interprofessional communication skills.
Design. Four simulations using standardized colleagues portraying attending physicians in inpatient and outpatient settings were integrated into a required course. Pharmacy students interacted with the standardized colleagues using the Situation, Background, Assessment, Request/Recommendation (SBAR) communication technique and were evaluated on providing recommendations while on simulated inpatient rounds and in an outpatient clinic. Additionally, changes in student attitudes and confidence toward interprofessional communication were assessed with a survey before and after the standardized colleague simulations.
Assessment. One hundred seventy-one pharmacy students participated in the simulations. Student interprofessional communication skills improved after each simulation. Student confidence with interprofessional communication in both inpatient and outpatient settings significantly improved.
Conclusion. Incorporation of simulations using standardized colleagues improves interprofessional communication skills and self-confidence of pharmacy students.
Keywords: interprofessional, standardized colleague, communication, SBAR, simulation
INTRODUCTION
Interprofessional education (IPE) and practice are strategies to achieve the goals of effective, patient-centered, timely, efficient, and equitable health care.1 Poor interprofessional communication is linked to medical errors.2-4 Future health professionals will be required to work together in interprofessional teams; therefore, IPE is included in the curriculum of health professions as a core component of their education.5,6 The American Association of Colleges of Pharmacy (AACP), in addition to several other national health professions associations in the fields of nursing, medicine, and public health, are committed to continued collaboration, expansion of leadership initiatives, member engagement, and attention to sustainability related to IPE and practice.6-8
Students should be prepared to work in interprofessional teams by being actively engaged in collaboration and learning with other health professionals.9-11Interprofessional educational strategies are effective when realistic patient care scenarios are presented and accurately reflect the professional role of each participant.10-12 To this end, high-fidelity simulations using human-patient simulators and standardized patients have been developed to deliver clinically realistic scenarios in a controlled learning environment. Simulations are an effective educational tool to expose students to a situation that could vary widely during practice experiences.13-16 Limited published information is available regarding standardized colleague simulations as an effective educational method to teach communication skills.17-19
A traditional simulation incorporates a standardized patient who presents with the need for a medical intervention; the standardized colleague represents a health care provider who receives information/recommendations from another health care professional (in this case a pharmacy student). A standardized colleague simulation role can include an interprofessional health care provider or another pharmacist. Standardized colleagues interact with students in a simulated health care environment to foster interprofessional communication by engaging in dialogue and responding to students in a standardized manner. They also provide feedback on student behaviors from the perspective of the health care professional they portray. Use of the standardized colleague model is beneficial as an introductory experience to interprofessional communication, but additional activities with real health professions students should also be incorporated into the curriculum. When interprofessional student groups communicate early in their training, the majority may simply accept recommendations, and conflicts may not arise. The standardized colleague communicates in a uniform style and can question students and raise conflict to determine how students respond.
Simulations using standardized colleagues can utilize any clinical scenario, communication style, and inpatient or outpatient health care setting. In addition, many interprofessional communication tools can be incorporated such as providing recommendations on hospital rounds when the interprofessional health care providers are together working as a synchronous team. Often in an outpatient setting, the team members provide interprofessional care asynchronously (ie, they are not all together at the same time), and a useful communication technique for this situation is called SBAR (Situation-Background-Assessment-Request/Recommendation).20
The standardized colleague activity fulfills the Accreditation Council for Pharmacy Education’s (ACPE) Standard 11 through active-learning strategies and practice-based exercises that develop critical-thinking and problem-solving skills. The council further advocates the use of simulation, including standardized colleagues, as an active-learning means to deliver pharmacotherapy and interprofessional communication content. Moreover, ACPE’s Standard 12 and the Center for the Advancement of Pharmaceutical Education (CAPE) Outcomes encourage pharmacy students to participate in IPE.21,22 In addition to pharmacy accreditation standards, the Interprofessional Education Collaborative national competencies have been proposed to guide the development of IPE.6 The authors used this competency document and focused on the specific domain of interprofessional communication to serve as the framework for this activity.6
Standardized colleague simulations were incorporated as required activities for third-year pharmacy students at the South Carolina College of Pharmacy (SCCP) in the Clinical Assessment course. Specific learning objectives were: (1) to develop an accurate pharmacotherapy plan for a specific patient; (2) to demonstrate appropriate interprofessional communication skills when interacting with a physician in an outpatient setting by displaying confidence, using the SBAR technique and concisely conveying the pharmacotherapy plan; and (3) to demonstrate appropriate interprofessional communication skills when interacting with a physician in an inpatient setting by recommending evidence-based pharmacotherapy and a monitoring plan and concisely conveying the pharmacotherapy plan to secure consensus from the health care team during hospital rounds.
Objectives of the study were to use standardized colleague simulations and the SBAR communication technique to expose pharmacy students to a standardized attending physician in inpatient and outpatient health care settings to evaluate student satisfaction with the IPE activity. Additional objectives were to determine the impact of such simulations on pharmacy students’ interprofessional communication skills and on the students’ confidence in their interprofessional communication.
DESIGN
The college offers a traditional 4-year doctor of pharmacy (PharmD) program to 180 students per class on 3 campuses. Students receive the same didactic curriculum at all campuses via distance education. This paper only addresses the standardized colleague simulations at the Medical University of South Carolina and University of South Carolina campuses (n=171).
Clinical Assessment is a required applications-based course offered during the spring of the third year of the PharmD curriculum. The course consists of lectures and weekly laboratory sessions that utilize active-learning strategies. Pharmacy students enrolled in Clinical Assessment have completed 2 semesters of pharmacotherapy courses, including modules, focused on cardiovascular, anticoagulation, respiratory, and infectious disease topics. Prior to the standardized colleague simulations, students are required to view a 60-minute recorded lecture, including video demonstrations that discuss interprofessional communication concepts such as SBAR and how to convey recommendations to an interprofessional team on rounds.
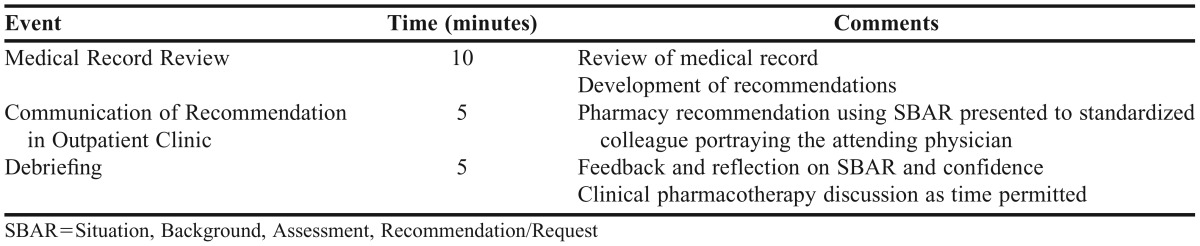
Four laboratory sessions using standardized colleague simulations were incorporated throughout the spring semester to allow students to apply interprofessional communication skills in various clinical situations. Two simulations were in an outpatient setting where students used the SBAR communication tool to deliver recommendations to a standardized colleague, who portrayed an attending physician in a primary care clinic. The 2 outpatient simulations included a patient in the anticoagulation clinic who needed warfarin therapy to be bridged with a low-molecular weight heparin and a patient in the pharmacotherapy clinic taking warfarin and who was recently prescribed sulfamethoxazole/trimethoprim. The other 2 simulations were in an inpatient setting where students used skills to convey evidence-based recommendations to a standardized colleague, an attending physician on internal medicine rounds. The 2 inpatient simulations included a patient admitted for new-onset atrial fibrillation and uncontrolled diabetes and a patient admitted for pneumonia and poorly controlled HIV. The timing of the standardized colleague interaction, specific logistics, and pharmacotherapy issues differed for the inpatient and outpatient scenarios (Tables 1 and 2). However, for all simulations, students were required to review the patients’ medical records, interact with and convey recommendations to the standardized attending physician, receive a performance evaluation, and participate in debriefing of their interprofessional communication skills. The focus of the debriefing session was on interprofessional communication skills rather than the clinical content of the simulation (ie, more than half the time was spent on communication skills).
Table 1.
Logistics of Standardized Colleague Inpatient Rounding Experience
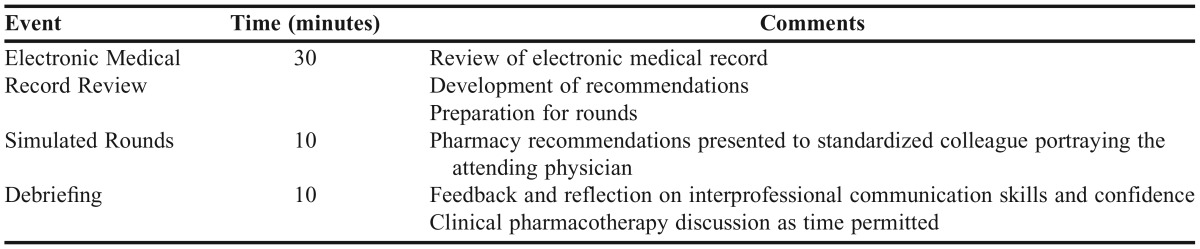
Table 2.
Logistics of Standardized Colleague Outpatient SBAR Experience
Clinical faculty members at SCCP played the role of the attending physicians and were familiar with a “typical physician interaction.” Faculty members were instructed to portray an experienced attending physician accustomed to pharmacy colleagues rounding with them; however, they were told to provide some resistance to a few of the recommendations and to seek evidence before accepting a recommendation. One week prior to each laboratory session, faculty members were sent an e-mail that contained a short orientation video, an overview of logistics, a facilitator guide and standardized colleague script, and the patient case and analytical checklist. Each standardized physician was instructed to follow the script, portray a specific persona, and ask certain questions (eg, during the inpatient rounds simulation, they asked students to provide evidence for atrial fibrillation rate vs rhythm control and the mechanism of action of digoxin). However, the scripts had sufficient flexibility to allow them to interact, ask additional questions, or provide comments based on specific student recommendations. The standardized colleagues were also trained on the evaluation tool and given a simple debriefing guide to help with delivering consistent feedback regarding the students’ interprofessional communication skills. When possible, standardized colleagues were assigned to the same students each week to allow for consistency in evaluations.
The overall time for students to complete the simulations was approximately 20 minutes for outpatient settings and 60 minutes for inpatient settings. Outpatient cases were limited to a 1-page document, whereas inpatient cases were more complex and presented as an electronic medical record with multiple pages of information. Additionally, time for communicating recommendations and debriefing was shorter for the outpatient scenarios because the task was limited to one specific recommendation rather than multiple recommendations, which was the case in the inpatient settings. Students did not have additional preparation requirements and were not provided with the clinical scenario ahead of time.
Faculty members committed an average of 24 hours for the semester to develop simulations and standardized colleague training guides and evaluations, train the standardized colleagues, and participate in simulations. Other SCCP faculty time commitments varied depending on the number of simulations they participated in. Each week, 3 days were devoted to the laboratory activities. All standardized colleague encounters took place in the Clinical Assessment laboratory spaces on each campus. On average, most faculty members volunteered to portray a standardized colleague for 3 sessions, translating to approximately 9 hours for the semester, and total of 13 faculty members participated.
The learning objectives of the standardized colleague simulations were evaluated using several methods. Changes in student attitudes toward interprofessional collaboration and self-confidence in interprofessional communication were assessed using a survey instrument before and after the simulations. Student performance and interprofessional communication skills were evaluated after each simulation with an objective structured learning experience (OSLE) and an assessment rubric. Student satisfaction with the standardized colleague simulations was qualitatively evaluated by assessing student comments from the postcourse evaluations. These assessment measures were directly related to the objectives of the study and the learning objectives of the activity.
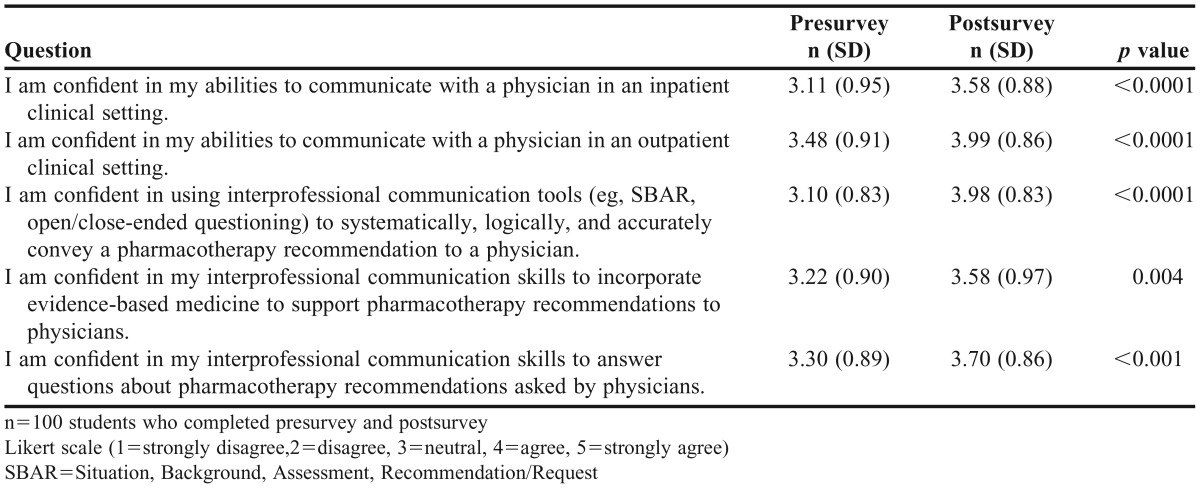
The survey assessing student confidence was administered one week prior to the first standardized colleague simulation (presurvey) and one week after the final simulation (postsurvey). No validated questionnaires assessing confidence regarding interprofessional communication specific to the study needs were available in the literature; therefore, the investigators developed their own. The survey was developed, reviewed by 3 additional faculty members, piloted with a small group of students, and revised accordingly. The lengthy psychometrically validated surveys assessing student perception or readiness for interprofessional collaboration23,24 would not have provided information relevant to the standardized colleague simulation scenarios, specifically interprofessional communication. Students were asked to complete the anonymous and voluntary surveys using SurveyMonkey software (SurveyMonkey, Inc., Palo Alto, CA). Each student was provided an anonymous code in order to match responses before and after the experience, and they had one week to complete each survey. Responses were collected using a 5-item Likert scale (1=strongly disagree to 5=strongly agree). The study and survey were approved as exempt research by the Institutional Review Board for Research with Human Subjects at both the Medical University of South Carolina and the University of South Carolina.
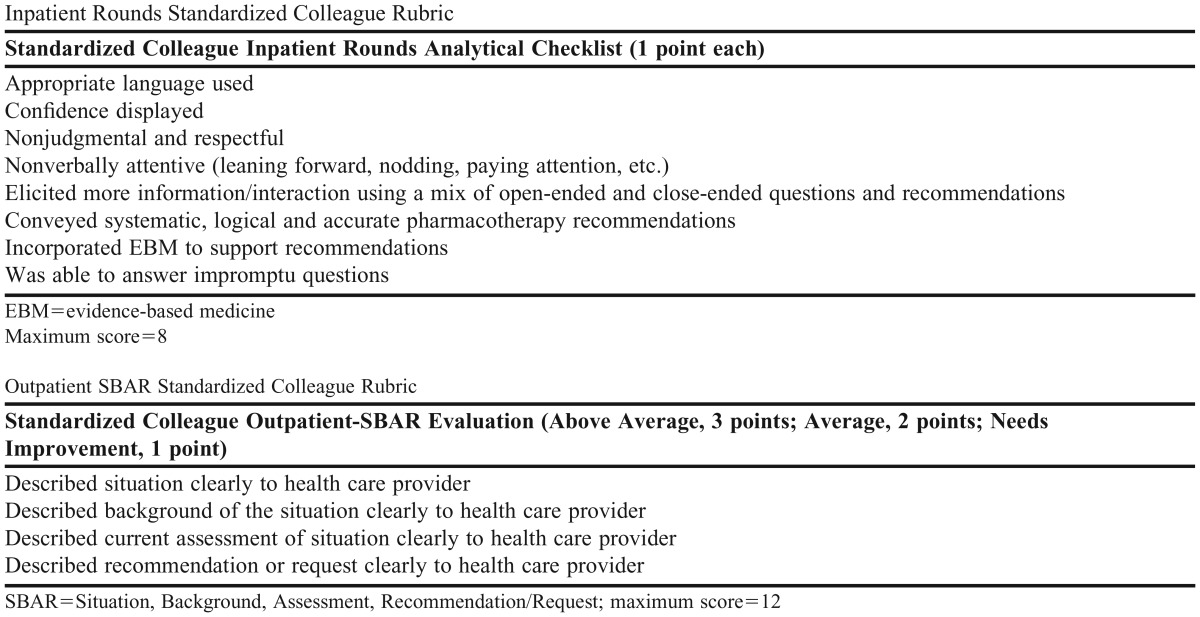
To assess student performance, 4 OSLEs were designed around each standardized colleague simulation. The 2 outpatient OSLEs used a rubric that assessed interprofessional communication using the SBAR technique. The investigators modified an existing rubric from a college of nursing program for this purpose.25 The 2 inpatient OSLEs used a rubric that assessed interprofessional communication while students were on hospital rounds. The investigators modified an existing rubric from a college of pharmacy program.19 The rubrics and the simulation focused on assessing interprofessional communication and not on accuracy of clinical recommendations. See Appendix 1 for inpatient and outpatient OSLE rubrics. After each student completed the OSLE, the standardized colleague completed the evaluation rubric and provided verbal comments and debriefings. Student OSLE performance for each of the simulations was formative, and students were graded (pass/fail) based on participation for the course.
Qualitative student satisfaction data were collected from the comment section of the postcourse evaluation. Themes were collected in order to gauge the value of the simulations and to gather information for future improvement. Statistical analyses were performed using SAS v9.2 (SAS, Inc., Cary, NC). Presurvey and postsurvey results and OSLE rubrics were analyzed using Wilcoxon signed rank test. Descriptive statistics were used for assessment of qualitative student comments.
EVALUATION AND ASSESSMENT
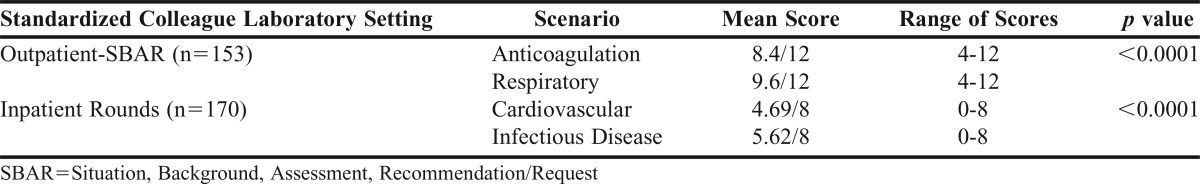
One hundred seventy-one students completed all 4 standardized colleague simulations; however, matched scores were only available for 153 students in the outpatient settings and 170 students in the inpatient settings. Students demonstrated an improvement of their interprofessional communication skills as evidenced by their OSLE evaluations. For the outpatient-SBAR simulations, the mean score increased from 8.4 to 9.6 out of 12 possible points from the first simulation to the second simulation (p<0.0001). Student performance also improved for the inpatient rounds simulations. Mean scores increased from 4.69 to 5.62 out of 8 possible points from the first simulation to the second simulation (p<0.0001). See Table 3 for complete results of student OSLE performance.
Table 3.
Evaluation of Pharmacy Student Interprofessional Communication Using Standardized Colleagues in Outpatient and Inpatient Simulated Health Care Settings
One hundred students completed the presurvey and postsurvey, representing a 58% response rate (125 students completed the presurvey, and 150 students completed the postsurvey; unmatched surveys were not assessed). Pharmacy student self-confidence in interprofessional communication significantly improved in both inpatient and outpatient settings after participating in the simulations as evidenced by all 5 questions (p<0.0001). See Table 4 for complete results.
Table 4.
Changes in Pharmacy Student Confidence Toward Interprofessional Communication with Simulated Physicians
Student comments regarding the standardized colleague simulations were collected from postsemester evaluations. More than 80% of comments were positive and enthusiastic about this learning activity. The most common themes included students’ desire for more standardized colleague simulations during the course and for standardized colleague simulations to be incorporated earlier (first or second year) in the curriculum. The most common constructive comment received from students was to standardize use of the evaluation tool among faculty members who portrayed the standardized colleagues. Students noted subjectivity and variability on the assessment rubric regarding students’ interprofessional communication, specifically during the inpatient rounds simulations.
DISCUSSION
Incorporating standardized colleague simulations into a clinical assessment course was beneficial to the college and the students. The simulations helped fulfill pharmacy accreditation standards and collaborative IPE competencies for the SCCP.6 In addition, student performance and self-confidence in interprofessional communication improved with use of a standardized colleague. Overall, students were satisfied with the simulations.
As pharmacy students graduate and become pharmacists practicing collaboratively within health care teams, enhancement of interprofessional clinical communication is imperative to increase safety and quality outcomes for patients.26 Standardized colleague simulations is one approach to help prepare health professions students for interprofessional interaction and patient-care activities upon graduation. However, limited information is reported in the pharmacy literature.18,19,26
Foley and colleagues conducted a small-scale pilot program that trained lay people to portray standardized physicians. Twenty-eight registered professional nurses comprised the intervention group, each of whom engaged in two 15-minute videotaped case scenarios with the standardized physician. Communication and collaboration skills were evaluated and compared to the control group, which did not participate in any sessions. Although no significant difference was noted between the 2 groups when comparing presurvey and postsurvey scores, the authors did note there were positive changes in 4 of the survey items in the intervention group.18
Meyer and colleagues used standardized colleagues to train pharmacy and nursing students. Clinical faculty members from the school of medicine were trained as standardized colleagues. Various patient cases were used to simulate challenging interprofessional communication scenarios. Students completed a self-evaluation that focused on their confidence and comfort in communication skills. Both nursing and pharmacy students demonstrated a significant increase in comfort and confidence from baseline to 6 months, leading the authors to conclude that standardized colleagues can enhance students’ abilities to communicate effectively in challenging situations.19
Our standardized colleague simulations add to the current literature, as it went beyond a simple description and assessed student performance, attitudes, and confidence. Assessment of student performance was standardized by using an OSLE evaluation with a grading rubric. Providing these multiple and sustained simulation experiences, as opposed to a one-time simulation, strengthened the instructional design because students completed the experience, received and reflected on feedback, and improved their performance. Use of standardized colleagues was a unique instructional design approach to teach interprofessional communication even though the only learners participating were pharmacy students. This concept is an approach that can overcome common barriers to IPE such as coordinating different student schedules or lack of access to other colleges of health professions.
This study is not without limitations. Student performance on interprofessional communication improved; however, the overall OSLE performance evaluation scores were low (eg, average scores of 70-80%). Student performance assessment focused on communication and not clinical content. There remains a philosophical debate about assessing one and not the other. In clinical practice, it is important to deliver sound clinical recommendations using appropriate interprofessional communication skills. In addition, interprofessional communication during the inpatient standardized colleague simulations improved marginally, and the educational significance of these results is questionable. Performance evaluations rated students much lower on the inpatient simulation scenarios than on the outpatient scenarios. Possible explanations for these findings include students not feeling as comfortable with interprofessional communication in this setting because many of them had not experienced rounds with a health care team. Another possibility may be the degree of difficulty of the inpatient clinical content, which may have hindered students’ ability to provide satisfactory interprofessional communication. Lastly, the 2 inpatient scenarios covered a range of challenging clinical topics not directly related to each other. Pharmacy faculty members portrayed the standardized colleague and could have introduced bias. Improvements could be made to training the standardized colleagues, specifically regarding completion of the evaluation rubrics (eg, observe practice videos to use the evaluation tool and compare inter-rater reliability). By providing examples of full-credit vs partial-credit responses, the consistency with which students were graded would be improved. These issues and specific differences of interprofessional communication within different health care settings could be the focus of future research.
In addition to student performance, self-confidence was evaluated before and after the simulations. Validated questionnaires were not used to collect survey data, and this may have limited the reproducibility of the results. Despite a large number of responses, the overall response rate was 58% and must be considered when generalizing the results. The matching of responses hindered the response rate, but strengthened the study design. Furthermore, the results only included student responses from a single institution in one academic year.
The standardized colleague simulation is still used in the required course for third-year pharmacy students. Based on student satisfaction data, improving training of standardized colleagues is underway so OSLE evaluation rubrics will be completed with more consistency. Incorporating more simulations using standardized colleagues earlier in the curriculum is being considered as is incorporation of an inpatient “rounding team” scenario. In addition, developing standardized colleague simulations using health professionals other than physicians (eg, nurses, physical therapists) is ongoing. Other schools of pharmacy could consider implementing required standardized colleague simulations to help fulfill ACPE standards and national IPE competencies. However, other institutions should carefully consider the amount of resources required for this activity, such as number of faculty members and volunteer hours.
SUMMARY
Incorporating standardized colleague simulations into a required course improved pharmacy students’ self-confidence and performance regarding interprofessional communication. This activity fulfilled national IPE competencies and pharmacy education standards. Specifically, this activity fulfilled a curricular need for and introduction to interprofessional communication training; however, using standardized colleagues eliminated many barriers surrounding IPE, including schedule availability of students at other colleges. Other schools of pharmacy could consider implementing similar simulations in order to fulfill curricular needs.
ACKNOWLEDGMENTS
The authors would like to thank all of the faculty members who helped in the development and portrayal of the simulated standardized colleagues.
Appendix 1. Inpatient Rounds and Outpatient-SBAR Standardized Colleague Student Evaluation Tools.
REFERENCES
- 1.Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm. Washington, DC: National Academy Press; 2001. http://www.nap.edu/openbook.php?isbn=0309072808. Accessed December 21, 2012. [Google Scholar]
- 2.To err is human: building a safer health system. Washington, DC: National Academy Press; 1999. http://www.nap.edu/openbook.php?record_id=9728&page=R1. Accessed December 21, 2012. [Google Scholar]
- 3.Reason J. Human error: models and management. BMJ. 2000;320(7237):768–770. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smallwood RA. Learning from adverse events. Int J Qual Health Care. 2000;12(5):359–361. doi: 10.1093/intqhc/12.5.359. [DOI] [PubMed] [Google Scholar]
- 5.Center for Advancement of Interprofessional Education (CAIPE) http://www.caipe.org.uk/about-us/defining-ipe/. Accessed December 21, 2012.
- 6.Interprofessional Education Collaborative [Internet] Core Competencies for Interprofessional Collaborative Practice. c2011 [cited 2012 Jan 19]. http://www.aacn.nche.edu/education-resources/IPECReport.pdf. Accessed December 21, 2012.
- 7.American Association of Colleges of Pharmacy. Task Force on Interprofessional Education 2007-2008. Annual Report. www.aacp.org/governance/councilfaculties/Documents/COF_InterprofessionalEducation2008.pdf. Accessed December 21, 2012.
- 8.Association of American Medical Colleges. Learn, Serve, Lead: The Mission, Vision and Strategic Priorities of the AAMC. Washington, DC; Association of American Medical Colleges; March 2010. https://members.aamc.org/eweb/upload/Learn%20Serve%20Lead.pdf. Accessed December 21, 2012.
- 9.Freeth D, Reeves S. Learning to work together: using the presage, process, product (3P) model to highlight decisions and possibilities. J Interprof Care. 2004;18(1):43–56. doi: 10.1080/13561820310001608221. [DOI] [PubMed] [Google Scholar]
- 10.Hammick M, Olckers L, Campion-Smith C. Learning in interprofessional teams: AMEE Guide no 38. Med Teach. 2009;31(1):1–12. doi: 10.1080/01421590802585561. [DOI] [PubMed] [Google Scholar]
- 11.Oandasan I, Reeves S. Key elements for interprofessional education. Part 1: the learner, the educator and the learning context. J Interprof Care. 2005;19(Suppl 1):21–38. doi: 10.1080/13561820500083550. [DOI] [PubMed] [Google Scholar]
- 12.Kilminster S, Hale C, Lascelles M, et al. Learning for real life: patient focused interprofessional workshops offer added value. Med Educ. 2004;38(7):717–726. doi: 10.1046/j.1365-2923.2004.01769.x. [DOI] [PubMed] [Google Scholar]
- 13.Hill AE, Davidson BJ, Theodoros DG. A review of standardized patients in clinical education: implications for speech-language pathology programs. Int J Speech-Lang Pathol. 2010;12(3):259–270. doi: 10.3109/17549500903082445. [DOI] [PubMed] [Google Scholar]
- 14.Seybert AL, Kobulinsky LR, McKaveney TM. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westberg S, Adams J, Thiede K, Stratton T, Bumgardner M. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70(2) doi: 10.5688/aj700234. Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shrader S, McRae L, King WM, Kern D. A simulated interprofessional rounding experience in a clinical assessment course. Am J Pharm Educ. 2011;75(4) doi: 10.5688/ajpe75461. Article 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Day HD. Standardized Colleagues: Modernizing Interprofessional Training. http://hdl.handle.net/10755/151931. Accessed December 21, 2012.
- 18.Foley ME, Nespoli G, Conde E. Using standardized patients and standardized physicians to improve patient-care quality: results of a pilot study. J Contin Educ Nurs. 1997;28(5):198–204. doi: 10.3928/0022-0124-19970901-05. [DOI] [PubMed] [Google Scholar]
- 19.Meyer S, Day H, Burn H. We need to talk: Facilitating improved interprofessional communication through the use of standardized colleagues. University of Pittsburgh Provost Newsletter. http://www.pitt.edu/∼facaffs/acie/documents/ACIE%20Report%20Meyer-Burns-Day.pdf. [Google Scholar]
- 20.Institute for Healthcare Improvement. http://www.ihi.org/explore/SBARCommunicationTechnique/Pages/default.aspx. Accessed December 21, 2012.
- 21.Accreditation Council for Pharmacy Education. Accreditation standards. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed December 21, 2012.
- 22.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education. http://www.aacp.org/resources/education/cape/Open%20Access%20Documents/CAPEoutcomes2013.pdf. Accessed June 8, 2014.
- 23.Luecht RM, Madsen MK, Petterson BJ. Assessing professional perceptions: design and validation of an interdisciplinary education perception scale. J Allied Health. 1990;19(2):181–190. [PubMed] [Google Scholar]
- 24.Parsell G, Bligh J. The development of a questionnaire to assess the readiness of healthcare students for interprofessional learning (RIPLS) Med Educ. 1999;33(2):95–100. doi: 10.1046/j.1365-2923.1999.00298.x. [DOI] [PubMed] [Google Scholar]
- 25.Institute for Healthcare Improvement. Reinventing nursing education. http://www.ihi.org/knowledge/Pages/ImprovementStories/ReinventingNursingEducation.aspx Accessed December 21, 2012.
- 26.Hume AL, Kirwin J, Bieber HL, et al. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy. 2012;32(11):e326–337. doi: 10.1002/phar.1215. [DOI] [PubMed] [Google Scholar]


