Abstract
The design of humeral implants for shoulder arthroplasty has evolved over the years. The new-generation modular shoulder prostheses have an anatomical humeral stem that replicates the three-dimensional parameters of the proximal humerus. An anatomical reconstruction is the best way to restore stability and mobility of the prosthetic shoulder and improve implant durability. However, a perfect anatomical match is not always possible in, for example, patients with post-traumatic osteoarthritis of the shoulder and deformities in the metaphyseal region. To avoid stem-related complications while retaining the advantages of the fourth generation of shoulder implants, different stemless implants have been developed. The stemless shoulder prosthesis is a new concept in shoulder arthroplasty. The authors review the indications, surgical technique, clinical and radiological midterm results, and complications of these humeral implants.
Keywords: shoulder, arthroplasty, stemless, osteoarthritis, post-traumatic
Introduction
Shoulder arthroplasty dates back to 1893, when the French surgeon Jules-Émile Péan implanted a platinum and rubber prosthesis to replace a glenohumeral joint that had been destroyed by tuberculosis. Thereafter, little progress in design and functionality was made until 1951, when Neer developed an unconstrained Vitallium prosthesis for the treatment of severe proximal humerus fracture. The humeral component for anatomical shoulder arthroplasty initially designed by Neer was a monoblock with a smooth surface fixed with polymethylmethacrylate (1,2). The first-generation components met the needs of many patients, but offered only a mid-range of sizes and did not precisely reproduce the proximal humerus geometry. The design of new-generation components was prompted by several studies analyzing the relative variability of some anatomical parameters. Boileau and Walch (3), in 1997, described the enormous anatomical variability of the proximal end of the humerus, with version, for example, varying between +5° and −55°. According to this study, the total shoulder arthroplasty can only be an “unconstrained prosthesis which best reproduces the normal articulation and matches the anatomy, kinematics and stability of the joint”.
The new generation of humeral components are commonly referred to as adaptable and modular. Depending on the design used, these components allow correct placement of the prosthetic humeral head, with positioning referenced to the stem in the anteroposterior and mediolateral directions (offset or eccentric). Some implants also allow various degrees of head inclination.
The use of modern anatomically designed shoulder implant systems in combination with glenoid resurfacing provides significant pain relief and improvement of function in the long term (4,5). However, in existing modern shoulder prosthesis systems, the clinical outcome and long-term survival of the prosthesis can be affected, in particular, by problems with the soft tissues and complications involving the glenoid component (6–9). By contrast, complications relating to the humeral component (such as loosening and stress shielding of the humeral stem or periprosthetic fractures) are much less common (having an incidence of approximately 1% according to the literature) (6, 8–11). As regards the long-term outcome of shoulder replacement, the failure rate increases over time and is directly in line with hip and knee replacement failure rates (7). A well-fixed humeral component may need to be removed for several reasons including infection, component malposition, humeral fracture, and glenoid exposure. The removal of a well-fixed humeral component during the course of revision shoulder arthroplasty is a significant challenge (12). In order to reduce these complications, many manufacturers progressively shortened humeral stem implants. For example, the Tornier Ascend (Tornier, Edina, MN, USA) has stem lengths ranging from 66 to 98 mm, and the Biomet Mini (Biomet, Warsaw, IN, USA) has a stem length of 70 mm. Stem shortening, coupled with elimination of humeral cement, potentially allows easier stem removal and improved bone quality in the event of subsequent revision. Stemless arthroplasty, with complete humeral stem elimination and reliance on metaphyseal fixation, provides even greater bone preservation for possible revision (13).
Stemless shoulder arthroplasty implants
The stemless shoulder prosthesis was introduced as a new, modern shoulder replacement system designed to reduce the potential risks associated with using a stemmed humeral implant. Today, five stemless shoulder implants are available on the worldwide market:
- the Arthrex Eclipse stemless shoulder arthroplasty (Arthrex, Naples, FL, USA), which was first introduced in Europe in 2005;
- the Total Evolutive Shoulder System (TESS), the world’s first stemless shoulder arthroplasty system, first implanted in Europe in 2004 (Biomet Inc, Warsaw, IN);
- the Mathys Affinis Short stemless arthroplasty (Mathys, Bettlach, Switzerland), introduced on the market in 2009;
- the Tornier Simpliciti, available, only for the European market, since 2010;
- the recently introduced Zimmer Sidus stemless shoulder system (Zimmer, Warsaw, IN, USA).
Indications and contraindications
The indications for an anatomical stemless shoulder prosthesis include pain and/or decreased function due to osteoarthritis (OA) (Fig. 1), rheumatoid arthritis, osteonecrosis, instability arthropathy, post-infectious arthropathy or post-traumatic arthritis not treated successfully with non-surgical means (13). The characteristic feature of this type of prosthesis is the cementless metaphyseal fixation of the implant by some mechanism. Its essential advantage is the fixation of the humeral component without the need to prepare the humeral diaphysis. In short, the humeral head can be positioned regardless of the shape of the humeral diaphysis. As well as in patients with primary OA, this fixation technique is particularly useful in patients with post-traumatic OA of the shoulder and extra-articular deformities of the proximal humerus, which can make the placement of a conventional stemmed prosthesis difficult or impossible (13,14). Similarly, a stemless prosthesis can easily be placed on a humerus that has hardware, such as an intramedullary nail or screws, that would impede the passage of a conventional stem.
Fig. 1.
Preoperative AP radiograph of a 67-year-old woman showing concentric degenerative arthritis.
The contraindications for an anatomical stemless shoulder prosthesis include four-part humerus fractures and inadequate bone stock.
Results: literature review
Because stemless arthroplasty implants have been available to surgeons worldwide for only a relatively short time, there are few published reports on this technique in the literature.
The Biomet TESS implant was the first system on the market. In 2010, Huguet et al. (14) reported the results of 63 Biomet TESS implants with a minimum follow-up of three years. The most recent post-operative radiographs indicated no subsidence or loosening of the corolla and no evidence of osteolysis, stress shielding, or radiolucent lines surrounding the corolla itself. The authors achieved an anatomical reconstruction in all patients, even in post-traumatic arthritis cases in which no tuberosity osteotomy was required. In 2011, Kadum et al. (15) reported on a group of 56 patients treated for a variety of shoulder conditions, including OA, post-traumatic arthritis, rotator cuff arthropathy, and proximal humeral fracture. This group was implanted with the Biomet TESS by standard hemiarthroplasty, primary total shoulder arthroplasty, or reverse arthroplasty, either with or without the optional intramedullary stem attachment to the corolla. Unfortunately, given the marked heterogeneity of the patient group, little can be concluded from this study.
In 2013, Razmjou et al. (16) presented a prospective longitudinal study comparing clinical and radiological outcomes of three different prosthetic designs, the Neer II system, the Bigliani-Flatow, and a stemless prosthesis, i.e. the TESS. The three types of total shoulder arthroplasty prosthesis used in this study all provided significant improvement in pain and function and were associated with high patient satisfaction. The incidence of lucent lines around the glenoid component was higher in the Neer II group; no evidence of lucent lines or stress shielding was seen in the TESS group.
In the same year, Berth and Pap (17) reported their prospective, randomized, longitudinal study comparing the results of the Biomet TESS stemless implant with the Mathys Affinis stemmed prosthesis. According to these authors, the use of the stemless shoulder prosthesis yielded good results which, at a mid-term follow-up, were comparable with those provided by a standard anatomical shoulder prosthesis. In addition, the authors concluded that the metaphyseal fixation allows precise and simple reconstruction of the proximal humerus with bone stock preservation and adequate glenoid exposure.
In 2011, Schoch et al. (18) published, in German, the first preliminary (average follow-up: 2.3 years) report regarding the Eclipse implant. The authors’ only practical conclusions were that it is possible to implant the prosthesis independent of the diaphysis of the humerus and malposition of the humeral with rare complications.
The second report on the Arthrex Eclipse prosthesis was by Brunner et al. in 2012 (19). The authors presented the results obtained in 233 patients treated for various indications (primary OA, fracture deformity, instability, rheumatoid arthritis, avascular necrosis, post-infectious OA, and cuff tear arthropathy). In this study the Eclipse prosthesis showed a secure bony fixation and ingrowth and stem-related complications were avoided.
Discussion
The indications for a stemless shoulder arthroplasty are exactly the same as those for any stemmed prosthesis used in the treatment of arthritis, and hence stemless replacements can be used in the treatment of OA, rheumatoid arthritis, osteonecrosis, instability arthropathy, and post-traumatic or post infectious arthropathy. The only limitation for implantation of a stemless prosthesis is a humeral head bone stock deficit (13–17,19).
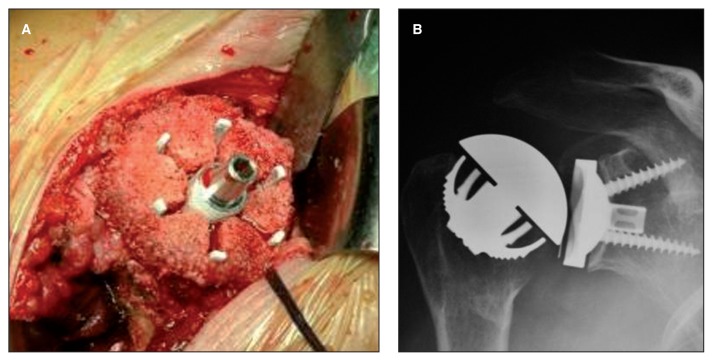
Another advantage of stemless shoulder prostheses is humeral bone stock preservation (Fig. 2). This potentially results in better starting conditions if any revision surgery is needed, and reduces the potential risk of typical complications such as intraoperative humeral fracture in those cases requiring humeral stem removal (20). Furthermore, in comparison with humeral head resurfacing, adequate exposure of the glenoid to allow glenoid component implantation is much easier to achieve (13,15).
Fig. 2.
A: Intraoperative photograph of the metaphyseal corolla (Total Evolutive Shoulder System, Biomet) in place showing complete seating of the component with considerable bone preservation. B: AP radiograph, three years postoperatively, showing the implant matching the patient’s anatomy and the humeral head centered on the prosthetic glenoid.
In conclusion, stemless shoulder arthroplasty has been proven to be at least as successful as stemmed implants with certain advantages for treatment in young people. The preliminary clinical reports are promising, but given their short-term duration and the heterogeneity of the patients concerned, they must be interpreted with caution.
References
- 1.Neer CS., 2nd Articular replacement for the humeral head. J Bone Joint Surg Am. 1955;37-A:215–228. [PubMed] [Google Scholar]
- 2.Neer CS., 2nd Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 1974;56:1–13. [PubMed] [Google Scholar]
- 3.Walch G, Boileau P. Prosthetic adaptability: a new concept for shoulder arthroplasty. J Shoulder Elbow Surg. 1999;8:443–451. doi: 10.1016/s1058-2746(99)90074-5. [DOI] [PubMed] [Google Scholar]
- 4.Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14:471–479. doi: 10.1016/j.jse.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Sperling JW, Cofield RH, Rowland CM. Minimum fifteen-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elbow Surg. 2004;13:604–613. doi: 10.1016/S1058274604001296. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Bohsali KI, Wirth MA, Rockwood CA., Jr Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88:2279–2292. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 7.Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: are they fewer or different? J Shoulder Elbow Surg. 2006;15:19–22. doi: 10.1016/j.jse.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Farng E, Zingmond D, Krenek L, Soohoo NF. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:557–563. doi: 10.1016/j.jse.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Wirth MA, Rockwood CA., Jr Complications of total shoulder replacement arthroplasty. J Bone Joint Surg Am. 1996;78:603–616. doi: 10.2106/00004623-199604000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Athwal GS, Sperling JW, Rispoli DM, Cofield RH. Periprosthetic humeral fractures during shoulder arthroplasty. J Bone Joint Surg Am. 2009;91:594–603. doi: 10.2106/JBJS.H.00439. [DOI] [PubMed] [Google Scholar]
- 11.Kumar S, Sperling JW, Haidukewych GH, Cofield RH. Periprosthetic humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am. 2004;86-A:680–689. doi: 10.2106/00004623-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Sahota S, Sperling JW, Cofield RH. Humeral windows and longitudinal splits for component removal in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1485–91. doi: 10.1016/j.jse.2014.02.004. pii: S1058–2746(14)00113-X. [DOI] [PubMed] [Google Scholar]
- 13.Churchill RS. Stemless shoulder arthroplasty: current status. J Shoulder Elbow Surg. 2014;23:1409–1414. doi: 10.1016/j.jse.2014.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Huguet D, DeClercq G, Rio B, Teissier J, Zipoli B TESS Group. Results of a new stemless shoulder prosthesis: radiologic proof of maintained fixation and stability after a minimum of three years’ follow-up. J Shoulder Elbow Surg. 2010;19:847–852. doi: 10.1016/j.jse.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Kadum B, Mafi N, Norberg S, Sayed-Noor AS. Results of the Total Evolutive Shoulder System (TESS): a single-centre study of 56 consecutive patients. Arch Orthop Trauma Surg. 2011;131:1623–1629. doi: 10.1007/s00402-011-1368-4. [DOI] [PubMed] [Google Scholar]
- 16.Razmjou H, Holtby R, Christakis M, Axelrod T, Richards R. Impact of prosthetic design on clinical and radiologic outcomes of total shoulder arthroplasty: a prospective study. J Shoulder Elbow Surg. 2013;22:206–214. doi: 10.1016/j.jse.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 17.Berth A, Pap G. Stemless shoulder prosthesis versus conventional anatomic shoulder prosthesis in patients with osteoarthritis: a comparison of the functional outcome after a minimum of two years follow-up. J Orthop Traumatol. 2013;14:31–37. doi: 10.1007/s10195-012-0216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schoch C, Huth J, Aghajev E, Bauer G, Mauch F. Die metaphysär verankerte Prothese bei posttraumatischer und primärer Omarthrose. Obere Extremität. 2011;6:275–281. [Google Scholar]
- 19.Brunner UH, Fruth M, Rückl K, Magosch P, Tauber M, Resch H, et al. Die schaftfreie Eclipse-Prothese-Indikation und mittelfristige Ergebnisse. Obere Extremität. 2012;7:22–28. [Google Scholar]
- 20.Vanhees M, Jaspars KC, van Riet R, Verborgt O, Declercq G. Stemless revision of a failed hemiarthroplasty: case report and surgical technique. J Shoulder Elbow Surg. 2013;22:e14–18. doi: 10.1016/j.jse.2013.05.014. [DOI] [PubMed] [Google Scholar]