Abstract
Objective
Depression is a common psychological problem in adolescence. Recent research suggests that group cognitive-behavioral interventions can reduce and prevent symptoms of depression in youth. Few studies have tested the effectiveness of such interventions when delivered by school teachers and counselors (as opposed to research team staff).
Method
We evaluated the effectiveness of the Penn Resiliency Program for adolescents (PRP-A), a school-based group intervention that targets cognitive behavioral risk factors for depression. We randomly assigned 408 middle school students (ages 10-15) to one of three conditions: PRP-A, PRP-AP (in which adolescents participated in PRP-A and parents were invited to attend a parent intervention component), or a school-as-usual control. Adolescents completed measures of depression and anxiety symptoms, cognitive style, and coping at baseline, immediately after the intervention, and at 6-month follow-up.
Results
PRP-A reduced depression symptoms relative to the school as usual control. Baseline levels of hopelessness moderated intervention effects. Among participants with average and high levels of hopelessness, PRP (A and AP) significantly improved depression symptoms, anxiety symptoms, hopelessness, and active coping relative to control. Among participants with low baseline hopelessness, we found no intervention effects. PRP-AP was not more effective than PRP-A alone. We found no intervention effects on clinical levels of depression or anxiety.
Conclusion
These findings suggest that cognitive-behavioral interventions can be beneficial when delivered by school teachers and counselors. These interventions may be most helpful to students with elevated hopelessness.
Depression is one of the most common psychological disorders and is one of the most debilitating and costly public health problems (Kessler et al., 2003; Kessler et al., 2005; Mathers, Boerma, & Ma Fat, 2008). Thus, there is a great need for depression prevention programs that are effective and that can be implemented widely. Because rates of depression increase dramatically during adolescence (Hankin et al., 1998), the second decade of life is a particularly important window for these prevention efforts. Fortunately, the past 15 years have seen a dramatic increase in the development and evaluation of interventions designed to prevent depression in youth. Most of these interventions are based on cognitive-behavioral (CB) therapy for depression (Beck, 1976; Ellis, 1962; Seligman, 1991). These interventions target many of the risk factors for adolescent depression that John Abela and his colleagues identified, such as pessimistic explanatory style, hopelessness, rumination, and other maladaptive thinking and coping styles (e.g., Abela, 2001; Abela, Brozina, and Haigh, 2002; Abela & Hankin, 2011; Abela, Vanderbilt, & Rochon, 2004; Hankin & Abela, 2005). CB programs also teach a variety of coping and problem-solving strategies that may help adolescents to respond adaptively to the wide range of stressors that are common during this developmental period.
Recent reviews indicate that, on average, depression prevention programs that target high-risk adolescents reduce depressive symptoms (Horowitz & Garber, 2006; Stice, Shaw, Bohon, Marti, & Rohde, 2009). Some programs prevent the onset of depressive disorders (e.g., Garber et al., 2009; Stice, Rohde, Gau, & Wade, 2010; for a review, see Cjuipers, van Straten, Smit, Mihalpoulos, & Beekman, 2008). Currently, there is less evidence for the effectiveness of depression prevention programs that are delivered universally to all youth regardless of risk status (Horowitz & Garber, 2006; Stice et al., 2009).
Although most depression prevention programs are intended for delivery by school counselors, teachers, and other community providers, most of the research on depression prevention has relied on researchers and professional interventionists (hired by the research team) to lead prevention groups. Recent reviews provide more evidence for the benefits of depression prevention programs when delivered by these exogenous providers than when delivered by people who actually work in the settings for which they are intended. For example, in their meta-analytic review of depression prevention research, Stice and colleagues reported that, though statistically significant, effect sizes for community provider group leaders were “trivial” (Stice et al., 2009, page 495). Clearly, this is a problem. To realize the promise of wide-scale prevention, we need programs that can be delivered effectively by staff within the community settings for which they are intended.
The Penn Resiliency Program (PRP), which is the focus of this research, is a CB intervention for young adolescents that is intended for delivery in schools. PRP is one of the most widely researched depression prevention programs. It has been tested as a targeted intervention, with high risk youth, and as a universal intervention. PRP group leaders have included researchers and community providers. A recent meta-analytic review of 17 controlled studies of PRP found that PRP significantly reduced depressive symptoms for at least 12 months post-intervention. PRP significantly reduced depression when delivered by researchers and also when delivered by community providers (Brunwasser, Gillham, & Kim, 2009). A major aim of the present study was to test PRP’s effectiveness when delivered by school teachers and counselors.
A second limit of existing depression prevention programs (and of treatments for depression in youth) is that, on average, effect sizes are small and fade over time (Horowitz & Garber, 2006; Stice et al., 2009; Weisz, McCarty, & Valeri, 2006). One strategy for boosting and sustaining effects is to include parents in prevention efforts. Some of the most important risk and protective factors for depression reside within the family environment. For example, childhood and adolescent depression is linked to parental depression, family conflict, and parental intrusiveness and criticism (Abela, Zinck, Kryger, Zilber, & Hankin, 2009; Asarnow, Goldstein, & Guthrie, 1993; Beardslee, Versage, & Gladstone, 1998; Downey & Coyne, 1990; Goodman & Gotlib, 1999). Factors in the family environment that protect against depression include family cohesiveness and parenting characterized by warmth and support (Parker, 1993). In addition, children may, in part, learn pessimistic and maladaptive thinking styles and coping strategies from their parents (Garber & Flynn, 2001).
These findings suggest a variety of targets for parent and family interventions: reducing parental depression, improving the family environment, increasing parenting skills, and helping parents to use and model more adaptive thinking and coping styles. Several of the most promising depression prevention programs include parent and/or family components (e.g., Beardslee et al., 1997; Clarke et al., 2001; Compas et al., 2009; Young, Mufson, & Gallop, 2010), although few studies have tested the added benefit of including parents versus working with adolescents alone. An evaluation of the Resourceful Adolescent Program (RAP), a school-based CB program for adolescents, found no added benefit of parent groups beyond the effects of adolescent groups (Shochet et al., 2001). Parent attendance was poor, however; only about 35% of parents attended any of the sessions. This may reflect the difficulties of running parent interventions through schools.
The parent component to PRP (PRP for parents) is a group intervention designed to help parents apply the cognitive-behavioral skills in their own lives and support their children’s use of these skills. In a pilot study, the combination of PRP for adolescents and PRP for parents reduced adolescents’ depression and anxiety symptoms, and prevented clinical levels of anxiety symptoms relative to a school-as-usual control (Gillham, Reivich, et al., 2006). On average, parents attended 63% of sessions and 90% of parents attended at least one session suggesting that the parent intervention was feasible. The study did not examine whether the parent program increased PRP’s effects, however.
The present study examined PRP’s effects in adolescents. We had three major aims: First, we examined PRP’s effects when delivered by school teachers and counselors. We expected PRP would reduce symptoms of depression and improve cognitive styles and coping skills targeted by the intervention. We also examined PRP’s effect on anxiety because some of the skills (e.g., challenging catastrophic thoughts, relaxation) may help to reduce anxiety. PRP has prevented anxiety symptoms in past research (e.g., Gillham, Reivich, et al., 2006; Roberts, Kane, Bishop, Matthews, & Thomson, 2004). Second, we examined whether the combination of PRP for adolescents + PRP for parents was more beneficial than PRP alone. Finally, because past research suggests depression prevention programs may be most effective for participants at highest risk, we examined whether baseline symptoms and other risk factors moderated PRP’s effects on depression.
Method
Participants
This study was approved by the University of Pennsylvania’s Institutional Review Board and by school administrators in each of the participating school districts. Figure 1 shows the participant flow from recruitment through the 6-month follow-up. Starting in 2003, we recruited three consecutive cohorts of students. Each year, the research team sent letters and consent forms describing the project to parents of students (ages 10-14) in five middle schools in two school districts in a suburban metropolitan area in the Northeastern United States. We sent recruitment materials to parents of approximately 8,000 students.
Figure 1.
Participant flow from recruitment through 6-month follow-up
A total of 1,025 students and their parents consented to participate in the screening phase and 1,016 of these students completed the screening questionnaires: the Children’s Depression Inventory (CDI; Kovacs, 2001), the Reynolds Adolescent Depression Scale, 2nd Edition (RADS-2; Reynolds, 2002), and the Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1985). At screening, the average CDI score was 7.87 (SD = 6.88, range 0 to 39); the average RADS-2 score was 55.12 (SD = 15.13, range 29 to 100); and the average RCMAS score was 8.97 (SD = 6.89, range 0 to 28). These scores are in the average range (between the 32nd and 54th percentiles) for middle school students based on standardization sample norms for each of these measures (Kovacs, 2001; Reynolds, 2002; Reynolds & Richmond, 1985).
Each year (in each school), we first offered places in the study to youth who reported high levels of depression symptoms on the CDI and/or RADS-2 (based on percentile equivalents from the standardization manuals) and then enrolled additional participants as space permitted. (The RCMAS was administered during the screening assessment to gather information about participants’ anxiety symptoms but it was not used to select participants into the intervention phase.) In some schools in some years, we were able to include all students who completed the screening assessment. We invited 655 students and their parents to participate in the intervention phase. Of these, 417 (64%) consented to participate. Average screening scores for these students were 11.12 (SD = 7.66, range 0 to 39) on the CDI; 63.53 (SD = 14.67, range 29 to 100) on the RADS-2, and 12.17 (SD = 7.04, range 0 to 38) on the RCMAS. These mean scores correspond approximately to the 62nd-73rd percentile for the CDI, the 62nd percentile for the RADS-2, and the 49th to 73rd percentile for the RCMAS based on the standardization samples (ranges reflect differences in norms by age and sex) (Kovacs, 2001; Reynolds, 2002; Reynolds & Richmond, 1985). Thus, the mean screening scores for our sample were slightly higher than average, although still well within one standard deviation of the standardization sample means. Participants’ scores covered the full range from no symptoms to high levels of symptoms.
A total of 412 of these students completed the baseline questionnaires and 401 completed baseline interviews screening for likely depression and anxiety disorders. Following baseline and prior to randomization, 3 students withdrew from the study and 1 student assigned to one of the PRP intervention conditions was excluded because there were too few students to create an intervention group for the student’s grade level. The remaining 408 students (214 boys and 194 girls) entered the intervention phase. At baseline, these 408 students were in between 10 and 15 years old and in 6th, 7th, or 8th grade. The majority (N = 374, 92%) were between 11 and 13 years old. See Table 1 for additional sample characteristics.
Table 1.
Sample Characteristics at Baseline (N = 408)
| N | % | ||
|---|---|---|---|
| Sex | |||
| Boys | 214 | 52 | |
| Girls | 194 | 48 | |
| Missing Data | 0 | ||
| Grade | |||
| 6 | 202 | 49 | |
| 7 | 118 | 29 | |
| 8 | 88 | 22 | |
| Missing Data | 0 | ||
| Race | |||
| Native American | 1 | <1 | |
| Asian | 16 | 4 | |
| Pacific Islander/Native Hawaiian | 1 | <1 | |
| African American | 48 | 12 | |
| European American | 312 | 77 | |
| Latino/a | 12 | 3 | |
| Other | 16 | 4 | |
| Missing Data | 2 | ||
| Parents’ Marital Status | |||
| Married | 267 | 74 | |
| Separated | 14 | 4 | |
| Divorced | 49 | 13 | |
| Widowed | 3 | <1 | |
| Never Married | 24 | 7 | |
| Other | 4 | 1 | |
| Missing Data | 47 | ||
| Mothers’ Education | |||
| Some high school | 9 | 2 | |
| High school graduate | 76 | 19 | |
| Some College | 77 | 19 | |
| College Graduate | 152 | 38 | |
| Advanced Degree | 90 | 22 | |
| Missing Data | 4 | ||
| Fathers’ Education | |||
| Some high school | 20 | 5 | |
| High school graduate | 104 | 26 | |
| Some College | 74 | 19 | |
| College Graduate | 110 | 28 | |
| Advanced Degree | 87 | 22 | |
| Missing Data | 13 | ||
We assessed clinical levels of depression and anxiety symptoms using the depression, social anxiety, and generalized anxiety sections of the NIMH Diagnostic Interview Schedule for Children version IV (NIMH DISC-IV: Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). Of the 401 students who completed the baseline interviews, 15 reported clinical levels of depression, 15 reported clinical levels of anxiety, and 6 reported clinical levels of both depression and anxiety. In total, 36 (9%) of students reported clinical levels of depression and/or anxiety. We contacted parents of these students and provided them with referrals if requested. Participants who reported clinical levels of symptoms at baseline were not excluded from the study and their data are included in analyses. Analyses excluding their data revealed similar results.
Randomization and Study Conditions
Within each school each year, we stratified students by sex and then used a computer-generated random numbers sequence to randomly assign participants to one of three study conditions: the Penn Resiliency Program for adolescents (PRP-A), the PRP for adolescents and parents (PRP-AP), and usual care control.
Students assigned to the PRP-A or PRP-AP conditions participated in the PRP intervention for adolescents. Students in both active intervention conditions participated in groups together. The PRP is a structured program that includes two major components. In the first component, based on cognitive-behavioral therapy for depression (Beck, 1976; Ellis, 1962; Seligman, 1991), students learn about the connection between interpretations and feelings and behaviors. Students learn to identify thinking styles, especially maladaptive styles that increase risk for hopelessness and depression. Students learn to challenge unrealistic pessimistic beliefs by considering alternatives and examining evidence. In the second component, students learn a variety of skills for solving interpersonal and other problems and for coping with stress. Students learn strategies for assertiveness, negotiation, creative problem-solving, decision making, and relaxation. PRP adolescent groups met for about 90 minutes after school once a week for 10-12 sessions, depending on the school calendar. (In most schools, most years, the adolescent program ran for 10 sessions.) When PRP ran for more than 10 sessions, the additional session(s) were devoted to additional review of key concepts and skills or to catch up on uncovered material from previous sessions. During the follow-up phase, adolescents in the PRP-A and PRP-AP conditions were invited to participate in 6 group booster sessions. Adolescent booster sessions started 5 months after the PRP group ended and were offered about once every 6 months during the follow-up phase.
Parents of adolescents assigned to the PRP-AP condition participated in the PRP for parents (Gillham, Reivich, et al., 2006), which is designed to teach parents the core PRP skills, including the cognitive skills and assertiveness. The major goals of the program are to help parents 1) use the skills in their own lives and 2) understand and support their children’s use of the skills. PRP parent groups met for about 90 minutes in the evening about once every two weeks for 6-7 sessions, depending on the school calendar. (In most schools, most years, the parent program ran for 6 sessions). When the parent groups ran for 7 sessions, the final session was devoted to additional review of key concepts and skills. Parents in the PRP-AP condition were invited to attend 3 booster sessions. Parent booster sessions were held 1 month, 5 months, and 17 months after the parent group ended. These sessions reviewed PRP content, helped participants think about the relevance of PRP skills to their recent experiences, and encouraged participants to apply the PRP skills.
Group leaders were teachers and counselors at the participating schools. Leaders participated in a 6-day (approximately 30-hour) group training and attended 90-minute group supervision meetings with members of the research team about once every 2-3 weeks during the intervention phase. There were 2 major components to the initial training. The first 2 days were devoted to teaching the skills at the adult level. Group leaders practiced applying PRP skills to their own lives. The goal of this section was to promote a deep understanding of the skills and competence with the cognitive-behavioral model. The last 4 days were devoted to supervised practice of the PRP curriculum.
Intervention Integrity
We assessed intervention integrity for the first two cohorts of adolescent groups (because of funding and staffing limits, we were unable to code intervention integrity for parent groups or for cohort 3). Group leaders audio-recorded their PRP sessions. Two trained research assistants independently rated sessions 1-9 for each intervention group in cohorts 1 and 2 on the presentation of concepts, skills, and activities using the PRP intervention integrity checklist that our team has used in past research (Gillham et al., 2007; Gillham, Hamilton, Freres, Patton, & Gallop, 2006). Coders received extensive training from a developer of the PRP program and had to demonstrate reliability by coding practice sessions (recordings of PRP sessions from past studies). A total of 164 sessions were coded with 17 sessions lost due to recording malfunctions. For each content item, raters used a 7-point scale ranging from 1 (no coverage) to 4 (satisfactory coverage) to 7 (excellent coverage). We measured consistency in the coders’ ratings using intraclass correlation coefficients (ICCs). The average ICC across all intervention groups and intervention sessions was .79.
We computed three integrity scores for each group: (1) the degree covered score, calculated by averaging the scores on each item across sessions, (2) the percentage covered score, calculated by averaging the percentage of items covered to any degree (rated >= 2) across the sessions, and (3) the percentage covered adequately score, calculated by averaging the percentage of items covered satisfactorily (rated >= 4) across the sessions. The 3 integrity scores were highly correlated (rs ranging from .90 to .97). The average degree covered score was 3.25 (SD = 0.48). On average, group leaders covered 68% of the integrity items to some degree (rated >= 2) and 47% of the items satisfactorily (rated >= 4), which is considerably below the level achieved in previous trials that assessed intervention adherence (Gillham et al., 2007; Gillham, Hamilton, et al., 2006). We did not evaluate intervention integrity for parent groups.
Attendance
Students in the PRP-A and PRP-AP conditions attended an average of 5.80 (SD = 3.64) sessions (out of 10), and 84% of students attended at least one session. Previous studies of PRP as an after school program report similar attendance rates (e.g., Gillham et al., 2007; Gillham, Reivich et al., 2006). Students’ attendance did not differ significantly between the two active intervention conditions, t(277) = 0.62, ns. On average, parents assigned to PRP-AP attended 3.20 (SD = 2.28) sessions (out of 6), and 77% of students had parents who attended at least one session. In the PRP-AP condition, students’ attendance and parent attendance were significantly correlated, r(N = 142) = 0.51, p <.001.
About half (44%) of the students attended the 5-month booster sessions. Attendance rates were similar for adolescents in PRP-A and PRP-AP. Parents of 27% of the students in PRP-AP attended the first parent booster session and parents of 21% of students in PRP-AP attended the second parent booster session. Parents most frequently cited scheduling conflicts as the reason they and their children were unable to attend intervention and booster sessions.
Assessment Schedule and Measures
Students completed assessments at baseline and approximately two weeks (post) and every 6-12 months after the PRP groups ended. We followed participants for 3 years. This paper focuses on initial findings, through the 6-month follow-up, for adolescents’ depression and anxiety symptoms and cognitive-behavioral skills targeted by PRP. Families were paid $25 for each assessment completed by the adolescent only (k = 2) and $50 for the 4 assessments completed by both the adolescent and parent(s) (k = 4). Families completing all 6 assessments earned a $60 bonus. Thus, participating families could earn up to $310.
Depression symptoms
Our primary measure of depression symptoms was the Children’s Depression Inventory (CDI; Kovacs, 2001), which has been used in most previous studies of PRP (Brunwasser et al., 2009). In a few studies, effects of depression prevention programs have varied depending on the questionnaire used to measure symptoms (Merry, McDowell, Wild, Bir, & Cunliffe, 2004; Muñoz et al., 1995). Therefore, we used the Reynolds Adolescent Depression Scale, 2nd Edition (RADS-2; Reynolds, 2002) to examine whether PRP’s effect on depression would extend to other measures. The CDI and RADS-2 are widely used measures of depressive symptoms in children and adolescents. Both measures have demonstrated adequate reliability and validity in previous research (Kovacs, 2001; Reynolds, 2002). Higher scores on the CDI and RADS-2 reflect higher levels of depressive symptoms. At the request of school administrators, we removed items that ask about suicidal thoughts and self-injurious behaviors (CDI item 9 and RADS-2 item 14). Because previous depression prevention studies have sometimes found different effects for different measures of depression, we examined these measures separately.
Anxiety symptoms
Students completed the Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1985), a widely used measure of anxiety in children and adolescents. The RCMAS measures several types of anxiety symptoms including worrying, social anxiety, difficulty concentrating, and physiological symptoms. The RCMAS has demonstrated good internal consistency and correlates with other measures of anxiety (Reynolds & Richmond, 1985). Higher scores on the RCMAS reflect higher levels of anxiety symptoms.
Clinical levels of symptoms
We used the depressive disorders, social phobia, and generalized anxiety modules of the computer-assisted NIMH Diagnostic Interview Schedule for Children (DISC-IV; Shaffer et al., 2000) to assess clinical levels of depression, social phobia and/or generalized anxiety at baseline and at the 6-month follow-up. The DISC-IV is a highly structured interview that assesses symptoms of DSM-IV psychological disorders (American Psychiatric Association, 1994) and is designed for delivery by lay people. The DISC-IV depression scale has demonstrated good test-retest reliability in clinical samples, although reliability is lower for the anxiety scales (Shaffer et al., 2000). Clinical levels of depression and anxiety symptoms on the DISC-IV have been found to correlate with scores from self-report questionnaires and to predict clinician diagnoses (e.g., Katon et al., 2007; Katon, Richardson, Russo, Lozano, & McCauley, 2006; Lambert, McCreary, Joiner, Schmidt, & Iaolongo, 2004; Roberts, Parker, & Dagnone, 2005), although some studies have reported poor agreement with clinicians’ diagnoses (e.g., Lewczyk, Garland, Hurlburt, Gearity, & Hough, 2003). Interviews were conducted by research assistants who received NIMH Diagnostic Interview Schedule for Children Version IV training from a member of the DISC-IV development team. Interviewers were not informed of students’ condition assignments.
Cognitive style
Youth completed the negative events scale from the Children’s Attributional Style Questionnaire (CASQ-N; Seligman et al., 1984). This scale assesses the internality, stability, and globality of causal attributions for negative events. The CASQ has demonstrated moderate internal consistency and moderate to high test-retest reliability (Seligman et al., 1984). In longitudinal studies, CASQ scores predict subsequent depression symptoms (e.g., Abela, 2001; Nolen-Hoeksema, Girgus, & Seligman, 1992). High scores on the CASQ-N reflect pessimistic explanatory styles.
Hopelessness
Students completed the Hopelessness Scale for Children (HSC; Kazdin, French, Unis, Esveldt-Dawson, & Sherick, 1983). The HSC has demonstrated good internal consistency (Kazdin et al., 1983; Kazdin, Rodgers, & Colbus, 1986). In past studies, HSC scores have correlated with symptoms of depression and reports of suicidal intent (e.g., Kazdin et al., 1983, 1986). Higher scores on the HSC reflect higher levels of hopelessness.
Coping
We used the Active Coping scale from the Children’s Coping Strategies Checklist-Revision 1 (CCSC-R1; Program for Prevention Research, 1999; Ayers et al., 1996) to measure students’ use of coping skills covered in PRP. The CCSC Active Coping scale measures problem-focused coping (cognitive decision making, direct problem solving, and seeking understanding) and positive cognitive restructuring (positive and optimistic thinking, perceptions of control). The CCSC scales have demonstrated good internal consistency and correlate with other measures of coping (Ayers et al., 1996). Higher scores on the Active Coping scale reflects higher use of problem-focused coping and cognitive restructuring strategies.
Statistical Analyses
Power analysis
Our goal was to detect small-to-medium intervention effects (d >= 0.35) on continuous measures allowing for 20% attrition. We planned an initial cell size >= 125 (final cell size of n>= 100) to achieve a power of >= 0.80 to detect a difference at alpha = 0.05, two-tailed).
Inspection and transformation of data
We evaluated assumptions of normality of continuous measures by examining histograms and calculating skewness and kurtosis scores at each assessment point. CDI and HSC scores were skewed and kurtotic so we used square root transformations for these data. We report raw scores in tables to ease interpretation.
Baseline differences and attrition
We used analyses of variance (ANOVA) and chi-square analyses to test for between-condition differences on psychological variables and demographic characteristics assessed at baseline. Similar analyses tested for differences between students who did and did not complete the follow-up assessment. We examined the possibility of differential attrition by testing for between-condition differences among students who did not complete the follow-up assessment.
Intervention effects
We conducted analyses based on intent-to-treat, including all participants for whom we had data. Mixed-model (MM) ANOVAs tested intervention effects on continuous outcomes (depression and anxiety symptoms, cognitive style, coping). These analyses predicted outcome score over time from condition with scores from baseline covaried. Screening scores were also covaried in analyses of depression and anxiety symptoms. Examination of the model fit statistics, such as the Akaike Information Criterion and the Bayesian Information Criterion, as well as the likelihood ratio tests, for several covariance structures indicated that the unstructured covariance structure was appropriate. When the MM ANOVAs revealed a significant or marginal (p < .10) main effect of condition, t tests (using test statements) compared the estimated marginal means for each pair of conditions. To determine whether effects were significant at post and/or 6-month follow-up, we followed up significant and marginal MM ANOVAs with analyses of covariance (ANCOVAs) predicting outcome at the given assessment from condition, with baseline score covaried (and screening score covaried, if available).
We calculated effect sizes based on Cohen’s d (Cohen, 1992) using the difference in estimated marginal means. For MM ANOVAs, we divided the difference in estimated marginal means by the square root of the covariance estimate following recommendations by Raudenbush and Xiao-Feng (2001). For ANCOVAs, we divided the difference in estimated marginal means by the pooled standard deviation. We standardized effect sizes so that positive effect sizes reflect a benefit of PRP-A relative to control, of PRP-AP relative to PRP-A, or of PRP-AP relative to control. We used two-tailed alphas. We report significant effects and nonsignificant trends (p < .10, referred to as tendencies within).
We used generalized linear mixed models (GLMM) through the lme4 package in the R Software Environment to evaluate the impact of the intervention on categorical outcomes (clinical levels of depression and anxiety) (Bates, Maechler, & Bolker, 2011; R Development Core Team, 2010). Three binary outcome variables were created indicating whether participants exceeded cutoffs for (1) a likely depressive disorder, (2) a likely anxiety disorder, and (3) either a likely depression or anxiety disorder. We entered baseline diagnostic status and baseline hopelessness symptoms as covariates in these analyses.
We conducted additional outcome analyses (not reported here) controlling for characteristics that differed between conditions at baseline. Those analyses yielded similar findings.
Moderator analyses
We examined whether intervention effects on depression symptoms (on the CDI) were moderated by students’ sex and level of baseline depression symptoms (moderators identified in previous depression prevention studies) and by the cognitive and behavioral risk factors that strongly predicted depression in our sample. To reduce the number of potential moderators examined, we conducted a series of analyses (not reported here) to identify the cognitive and behavioral variables that strongly predicted subsequent depression in the control group. We conducted separate MM ANOVAs predicting depression symptoms across post and follow-up from the risk factor of interest, with screening and baseline depression symptoms covaried. We then entered significant predictors into a single MM ANOVA. When examined singly, hopelessness (HSC) and low levels of active coping (CCSC) predicted higher levels of subsequent depression. Only hopelessness predicted depression symptoms in the combined analysis (details of these analyses are available from the authors). Therefore, we examined baseline hopelessness as a potential moderator of intervention effects.
We evaluated whether covariates moderated the impact of the intervention on depressive symptoms by including two-way interactions in the MM analyses. MM ANOVAs predicted depression symptoms from condition, proposed moderator (centered, if continuous), and the condition by moderator interaction, with screening and baseline levels of depression symptoms covaried.
We used the online utility described in Preacher, Curran, and Bauer (2006) to probe the nature of significant two-way interaction effects between continuous covariates and condition assignment. The online utility uses R software (R Development Core Team, 2010) to calculate and plot slopes of the dependent variable on the focal predictor (in this case, condition assignment) at different levels of the continuous moderator (e.g., levels of hopelessness). We evaluated the significance of the slope between condition and depressive symptoms at low (25th percentile), average (mean), and high (75th percentile) levels of the continuous variable. The interaction utility also provides cutoff scores identifying the specific levels of the continuous moderator at which there is a significant relationship between the predictor and outcome variables of interest. Knowing the “region of significance” helps interpret the nature of the interaction.
Finally, we conducted additional analyses to examine 1) whether variables that moderated intervention effects on depressive symptoms also moderated effects on other outcomes, and 2) whether intervention effects were significant for subgroups of participants (e.g., students scoring above or below the cut-off scores on significant moderator variables).
Dose effects
We examined whether higher intervention doses (high integrity and high attendance) were associated with greater improvements in depression and anxiety symptoms. We examined attendance using MM ANOVAs predicting outcome score from attendance with screening and baseline scores covaried. Analyses examining adolescent attendance included data from the PRP-A and PRP-AP conditions. Analyses examining parent attendance included data from PRP-AP alone. We measured the impact of intervention integrity by predicting depressive symptoms from the degree covered, percentage covered, and percentage covered adequately scores (see description in the Method section) with screening and baseline scores covaried.
Hypotheses
We predicted that 1) PRP-A would improve students’ cognitive style and active coping skills, reduce symptoms of depression and anxiety, and prevent clinical levels of depression and anxiety; 2) PRP-AP would lead to greater benefits on these outcomes than PRP-A alone, and 3) the PRP interventions would be most effective for students at higher risk for depression (girls and participants with higher baseline depression symptoms and higher hopelessness). We also examined whether higher intervention integrity and attendance predicted greater reductions in depression and anxiety.
Results
Overview
PRP-A reduced hopelessness and depressive symptoms (on the CDI) and tended to reduce anxiety symptoms relative to control. We found no added benefit of the PRP parent intervention. PRP-A was more beneficial to students who reported elevated levels of hopelessness at baseline. We now describe these findings in detail.
Baseline Differences and Attrition
At baseline, PRP-A and PRP-AP differed in the proportion of adolescents from different racial groups, χ2(6, N = 278) = 13.64, p <.05. PRP-A included more students of Asian and African American descent and fewer students of European descent than PRP-AP. There were no other differences between conditions on baseline measures of demographic characteristics or psychological functioning.
Of the 408 students who began the intervention phase, 372 (91%) completed the post assessment and 349 (86%) completed the 6-month follow-up assessment. Completion rates were similar in all three conditions. Completion rates varied by race/ethnicity, χ2 (6, N = 406) = 21.93, p<.01. Asian American, African American, and European American students were more likely than Latino/a students to complete the follow-up assessment. Students whose fathers’ had higher levels of education were more likely to complete the follow-up than students whose fathers had lower levels of education, χ2 (5, N = 395) = 15.21, p <.01. Students who completed the follow-up assessment did not differ from non-completers on other demographic characteristics or on psychological variables assessed at baseline.
Among students who did not complete the follow-up assessment, those in PRP-AP scored lower on the RADS-2 than controls (p < .05). We found no other differences between conditions.
Baseline Scores
Table 2 presents descriptive statistics and correlations among measures of psychological functioning at baseline. Consistent with past research, pessimistic explanatory style, and hopelessness were associated with higher levels of depression. Active coping was associated with lower levels of depression. Girls reported higher levels of anxiety than boys, t(406) = 2.09, p <.05 and t (405) = 1.69, p <.10. There were no sex differences on other measures at baseline.
Table 2.
Descriptive statistics and correlations at baseline
| Descriptive statistics | Correlations | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | N | 1. | 2. | 3. | 4. | 5. | |
| 1. Depression (CDI) | 10.49 | 8.40 | 407 | -- | ||||
| 2. Depression (RADS) | 60.23 | 16.98 | 408 | .88 | -- | |||
| 3. Anxiety (RCMAS) | 10.79 | 7.46 | 408 | .83 | .81 | -- | ||
| 4. Explanatory style (CASQ-CN) | 7.93 | 3.27 | 405 | .63 | .59 | .56 | -- | |
| 5. Hopelessness (HSC) | 4.28 | 3.25 | 407 | .63 | .63 | .57 | .56 | -- |
| 6. Active Coping (CCSC) | 2.65 | 0.61 | 404 | −.52 | −.50 | −.41 | −.43 | −.50 |
All correlations significant at p <.001
Intervention Effects: PRP-A versus Control
Table 3 reports descriptive statistics by condition, the results of MM ANOVAs, and the results of ANCOVAs that followed significant and marginally significant (p < .10) MM ANOVAs.
Table 3.
Intervention effects: Full sample
| Measure | Assessment | Descriptive Statistics | Pairwise comparison | |||||
|---|---|---|---|---|---|---|---|---|
| PRP-A Mean (SD) |
PRP-AP Mean (SD) |
Control Mean (SD) |
PRP-A vs Control | PRP-AP vs PRP-A | PRP-AP versus Control | |||
| Depression (CDI) | ||||||||
| Screening | 10.64 (7.76) | 11.64 (7.71) | 10.97 (7.57) | |||||
| N = 137 | N = 141 | N = 129 | ||||||
| Baseline | 10.20 (8.52) | 10.25 (7.93) | 11.05 (8.79) | |||||
| N = 137 | N = 142 | N = 129 | ||||||
| Post | 7.37 (7.13) | 8.51 (8.19) | 9.45 (8.59) | ANCOVA | p=.012 | p = .404 | p = .091 | |
| N = 127 | N = 126 | N = 118 | d = 0.20 (0.05, 0.35) | d = −0.07 (−0.22, 0.09) | d = 0.13 (−0.03, 0.29) | |||
| Follow-up | 6.97 (6.98) | 6.97 (7.71) | 8.18 (8.88) | ANCOVA | p=.747 | p=.285 | p=.164 | |
| N = 114 | N = 121 | N = 113 | d = 0.03 (−0.16, 0.22) | d = 0.10 (−0.09, 0.29) | d = 0.13 (−0.05, 0.32) | |||
| MM ANOVA | t(364) = −2.09, p=.037 | t(366) = 0.30, p=.762 | t(362) = −1.78, p=.076 | |||||
| d = 0.23 (0.01, 0.44) | d = −0.03 (−0.24, 0.18) | d = 0.20 (−0.02, 0.41) | ||||||
| Depression (RADS-2) | ||||||||
| Screening | 63.16 (15.12) | 63.75 (15.15) | 63.63 (13.73) | |||||
| N = 137 | N = 141 | N = 129 | ||||||
| Baseline | 59.78 (17.16) | 59.67 (16.58) | 61.62 (17.29) | |||||
| N = 137 | N = 142 | N = 129 | ||||||
| Post | 54.03 (15.55) | 55.81 (17.10) | 56.76 (17.07) | ANCOVA | -- | -- | -- | |
| N = 127 | N = 127 | N = 118 | ||||||
| Follow-up | 53.42 (15.54) | 53.14 (16.36) | 55.25 (17.97) | ANCOVA | -- | -- | -- | |
| N = 114 | N = 122 | N = 113 | ||||||
| MM ANOVA | t(367) = −1.25, p=.211 | t(369) = 0.28, p=.780 | t(366) =−0.98, p=0.328 | |||||
| d = 0.14 (−0.08, 0.36) | d = −0.03 (−0.25, 0.19) | d = 0.11 (−0.11, 0.33) | ||||||
| Anxiety (RCMAS) | ||||||||
| Screening | 12.18 (7.02) | 12.16 (7.13) | 12.32 (7.11) | |||||
| N = 137 | N = 141 | N = 129 | ||||||
| Baseline | 10.74 (7.47) | 10.40 (7.20) | 11.27 (7.75) | |||||
| N = 137 | N = 141 | N = 129 | ||||||
| Post | 8.30 (6.93) | 8.89 (7.23) | 9.53 (7.69) | ANCOVA | p=.053 | p=.335 | p=.322 | |
| N = 127 | N = 127 | N = 118 | d = 0.16 (0.00, 0.32) | d = −0.08 (−.023, 0.08) | d = 0.08 (−0.08,0.24) | |||
| Follow-up | 7.53 (6.95) | 8.08 (6.98) | 8.28 (7.61) | ANCOVA | p=.391 | p=.431 | p=.932 | |
| N = 113 | N = 122 | N = 112 | d = 0.08 (−0.11, 0.28) | d = −0.08 (−0.27, 0.11) | d = 0.00 (−0.18, 0.20) | |||
| MM ANOVA | t(367) = −1.86, p=.064 | t(369) =0.77, p=.269 | t(365) = −1.11, p=.439 | |||||
| d = 0.21 (−0.01, 0.43) | d = −0.12 (−0.34, 0.09) | d = 0.09 (−0.11, 0.31) | ||||||
| Explanatory style (CASQ-CN) | ||||||||
| Baseline | 8.06 (3.21) | 7.62 (3.22) | 8.12 (3.39) | |||||
| N = 137 | N = 141 | N = 127 | ||||||
| Post | 7.58 (3.51) | 6.95 (3.78) | 8.08 (3.79) | ANCOVA | -- | -- | -- | |
| N = 126 | N = 124 | N = 117 | ||||||
| Follow-up | 7.35 (3.24) | 7.45 (4.00) | 7.87 (3.80) | ANCOVA | -- | -- | -- | |
| N = 112 | N = 120 | N = 113 | ||||||
| MM ANOVA | t(365) = −1.02, p=.309 | t(368) = −0.36, p=.720 | t(365) = −1.37, p=.171 | |||||
| d = 0.11 (−0.10, 0.33) | d = 0.04 (−0.17, 0.25) | d = 0.15 (−0.07, 0.37) | ||||||
| Hopelessness (HSC) | ||||||||
| Baseline | 4.17 (3.13) | 4.17 (3.14) | 4.53 (3.48) | |||||
| N = 137 | N = 142 | N = 128 | ||||||
| Post | 3.35 (2.69) | 3.89 (2.90) | 4.30 (3.53) | ANCOVA | p=.021 | p=.100 | p=.486 | |
| N = 127 | N = 127 | N = 118 | d = 0.24 (0.03, 0.44) | d = −0.17 (−0.36, 0.03) | d = 0.07 (−0.13, 0.27) | |||
| Follow-up | 3.26 (2.75) | 3.55 (2.51) | 3.98 (3.23) | ANCOVA | p=.079 | p=.374 | p=.366 | |
| N = 113 | N = 121 | N = 113 | d = 0.21 (−0.02, 0.45) | d = −0.11 (−0.34, 0.13) | d = 0.11 (−0.12, 0.34) | |||
| MM ANOVA | t(370) = −2.31 p=.021 | t(373) = 1.47, p=.142 | t(367) = −0.88, p=.380 | |||||
| d = 0.26 (0.04, 0.48) | d = −0.16 (−0.38, 0.05) | d = 0.10 (−0.12, 0.32) | ||||||
| Active Coping (CCSC) | ||||||||
| Baseline | 2.65 (0.60) | 2.62 (0.62) | 2.69 (0.62) | |||||
| N = 134 | N = 141 | N = 129 | ||||||
| Post | 2.62 (0.61) | 2.70 (0.59) | 2.65 (0.62) | ANCOVA | -- | -- | -- | |
| N = 126 | N = 126 | N = 118 | ||||||
| Follow-up | 2.66 (0.59) | 2.67 (0.62) | 2.66 (0.58) | ANCOVA | -- | -- | -- | |
| N = 113 | N = 120 | N = 113 | ||||||
| MM ANOVA | t(360) = 0.46, p=.647 | t(364) = 0.88, p=.380 | t(358) = 1.32, p=.184 | |||||
| d = 0.05 (−0.16, 0.26) | d = 0.09 (−0.11, 0.30) | d = 0.14 (−0.07, 0.35) | ||||||
Depression and anxiety symptoms
PRP-A significantly reduced depression symptoms on the CDI, but not the RADS, and tended to reduce anxiety symptoms. Follow-up ANCOVAs indicated that PRP-A significantly reduced depression symptoms on the CDI at post, but not at the 6-month follow-up. We found no significant intervention effects on clinical levels of symptoms on the DISC-IV (see Table 4).
Table 4.
Clinical levels of symptoms at follow-up*
| PRP-A Number (%) scoring positive |
N | PRP-AP Number (%) scoring positive |
N | Control Number (%) scoring positive |
N | |
|---|---|---|---|---|---|---|
| Depression and/or Anxiety |
7 (6.1%) | 115 | 4 (3.4%) | 116 | 8 (7.0%) | 114 |
| Depression | 4 (3.5%) | 115 | 1 (0.9%) | 116 | 4 (3.5%) | 114 |
| Anxiety | 4 (3.5%) | 115 | 3 (2.6%) | 116 | 7 (6.1%) | 114 |
There were no significant intervention effects on clinical levels of symptoms
Cognitive style and coping
PRP-A significantly reduced hopelessness. Follow-up ANCOVAs suggested that PRP-A significantly reduced hopelessness at post and tended to reduce hopelessness at the 6-month follow-up. PRP-A did not improve explanatory style or active coping.
Intervention Effects: PRP-AP
The addition of the PRP parent intervention did not lead to greater improvements than the PRP adolescent intervention alone on any of the measures examined (see Table 3).
Moderation by Baseline Risk
Given that there were no significant differences between the 2 active intervention conditions (PRP-A and PRP-AP), we combined these conditions when evaluating moderators. Students’ sex and baseline levels of depression and anxiety symptoms did not moderate intervention effects on depression symptoms (CDI).
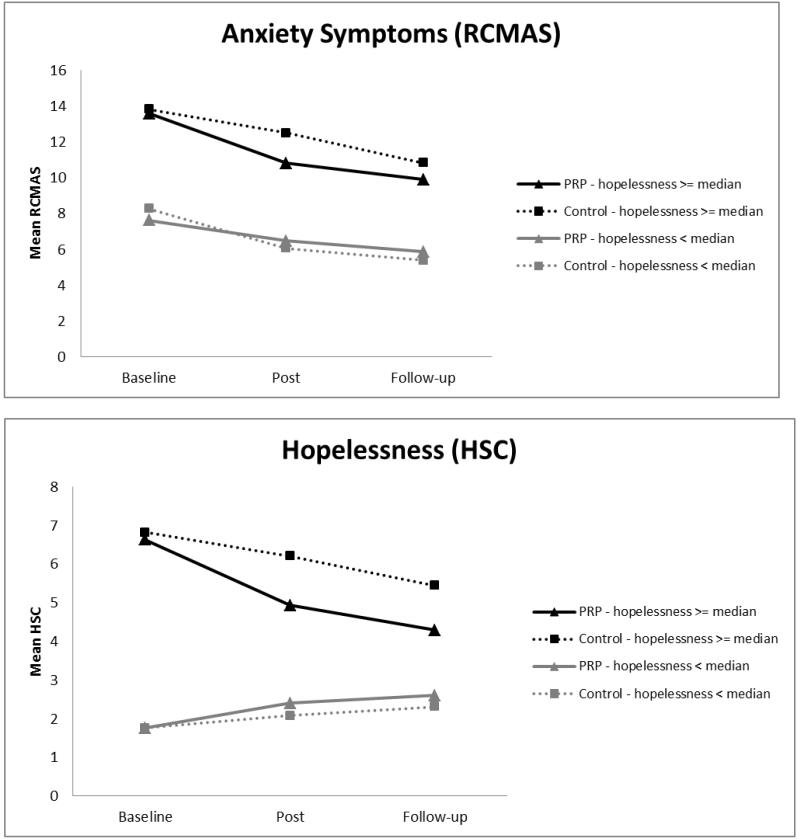
Baseline levels of hopelessness significantly moderated intervention effects on depressive symptoms (CDI), t(366) = −2.14, p < .05. The region of significance showed that at levels of hopelessness greater than or equal to the median score, the slope of CDI symptoms on condition was significant (see Figure 2). We therefore used the median hopelessness score as a cutoff indicating whether students had low versus average or high baseline hopelessness scores. Baseline hopelessness also moderated intervention effects on depression symptoms on the RADS-2, anxiety, and hopelessness, and tended to moderate intervention effects on active coping, for RADS-2: t(364) = −2.31, p < .05; RCMAS: t(364) = −2.40, p < .05; HSC: t(367) = −3.60, p < .001; and CCSC-Active Coping: t(356) = 1.93, p = .054 (see Figures 3A to 3E). Baseline hopelessness did not moderate intervention effects on clinical levels of depression or anxiety symptoms.
Figure 2.
Interaction of Condition and Hopelessness
Figure 3.
A to E Intervention effects for subgroups with average and high versus low hopelessness
A. Depression symptoms (CDI)
B. Depression symptoms (RADS-2)
C. Anxiety symptoms (RCMAS)
D. Hopelessness (HSC)
E. Active Coping (CCSC)
Among students who reported average or high levels of hopelessness at baseline, PRP significantly reduced depression symptoms (on both the CDI and RADS-2), anxiety symptoms, and hopelessness. PRP also increased active coping (see Table 5). Among students with low baseline hopelessness, there were no significant intervention effects on any outcome.
Table 5.
Intervention effects: Subgroup with average and high baseline hopelessness
| Measure | Assessment | Descriptive Statistics | Comparison | ||
|---|---|---|---|---|---|
| PRP (A+AP) Mean (SD) |
Control Mean (SD) |
PRP vs Control | |||
| Depression (CDI) | |||||
| Screening | 14.37 (8.13) | 13.14 (8.23) | |||
| N = 138 | N = 70 | ||||
| Baseline | 14.47 (8.62) | 14.57 (9.46) | |||
| N = 138 | N = 70 | ||||
| Post | 11.16 (8.68) | 13.25 (9.67) | ANCOVA | F(1,183) = 8.36, p=.004 | |
| N = 123 | N = 64 | d = 0.28 (0.09, 0.48) | |||
| Follow-up | 9.75 (8.51) | 11.77 (10.21) | ANCOVA | F(1,170) = 3.17, p=.077 | |
| N = 113 | N = 61 | d = 0.21 (−0.02, 0.44) | |||
| MM ANOVA | t(181) = −2.84, p=.005 | ||||
| d = 0.37 (0.11, 0.63) | |||||
| Depression (RADS-2) | |||||
| Screening | 70.00 (14.44) | 66.60 (14.58) | |||
| N = 138 | N = 70 | ||||
| Baseline | 68.41 (16.51) | 68.24 (17.99) | |||
| N = 138 | N = 70 | ||||
| Post | 60.95 (16.91) | 64.31 (17.80) | ANCOVA | F(1,183) = 5.50, p=.020 | |
| N = 123 | N = 64 | d = 0.27 (0.04, 0.49) | |||
| Follow-up | 58.62 (17.20) | 61.81 (19.68) | ANCOVA | F(1,170) = 2.49, p=.117 | |
| N = 113 | N = 61 | d = 0.20 (−0.05, 0.45) | |||
| MM ANOVA | t(184) = −2.21, p=.029 | ||||
| d = 0.31 (0.03, 0.57) | |||||
| Anxiety (RCMAS) | |||||
| Screening | 14.77 (6.86) | 14.31 (7.18) | |||
| N = 138 | N = 70 | ||||
| Baseline | 13.58 (7.08) | 13.83 (8.24) | |||
| N = 138 | N = 70 | ||||
| Post | 10.82 (16.91) | 12.50 (8.44) | ANCOVA | F(1,183 = 6.78, p=.010 | |
| N = 123 | N = 64 | d = 0.27 (0.07, 0.48) | |||
| Follow-up | 9.91 (7.51) | 10.83 (8.59) | ANCOVA | F(1,169) = 1.44, p=.231 | |
| N = 113 | N = 60 | d = 0.14 (−0.09, 0.38) | |||
| MM ANOVA | t(184) = −2.13, p=.031 | ||||
| d = 0.30 (0.02, 0.57) | |||||
| Explanatory style (CASQ-CN) | |||||
| Baseline | 9.34 (3.11) | 9.35 (3.34) | |||
| N = 138 | N = 70 | ||||
| Post | 8.66 (3.72) | 9.41 (3.87) | ANCOVA | -- | |
| N = 123 | N = 64 | ||||
| Follow-up | 8.42 (3.76) | 8.78 (4.01) | ANCOVA | -- | |
| N = 113 | N = 61 | ||||
| MM ANOVA | t(183) = −1.05, p=.292 | ||||
| d = 0.14 (−0.12, 0.40) | |||||
| Hopelessness (HSC) | |||||
| Baseline | 6.63 (2.61) | 6.82 (3.08) | |||
| N = 138 | N = 70 | ||||
| Post | 4.93 (2.96) | 6.21 (3.58) | ANCOVA | F(1,184) = 7.58, p=.007 | |
| N = 123 | N = 64 | d = 0.39 (0.11, 0.67) | |||
| Follow-up | 4.29 (2.85) | 5.45 (3.52) | ANCOVA | F(1,170) = 5.73, p=.018 | |
| N = 112 | N = 61 | d = 0.37 (0.06, 0.67) | |||
| MM ANOVA | t(185) = −2.85, p=.005 | ||||
| d = 0.39 (0.12, 0.66) | |||||
| Active Coping (CCSC) | |||||
| Baseline | 2.39 (0.58) | 2.42 (0.63) | |||
| N = 134 | N = 70 | ||||
| Post | 2.55 (0.56) | 2.43 (0.61) | ANCOVA | F(1,180) = 4.76, p=.030 | |
| N = 122 | N = 64 | d = 0.28 (0.03, 0.53) | |||
| Follow-up | 2.57 (0.61) | 2.49 (0.60) | ANCOVA | F(1,168) = 1.75, p=.187 | |
| N = 112 | N = 61 | d = 0.19 (−0.10, 0.48) | |||
| MM ANOVA | t(178) = 2.20, p=.029 | ||||
| d = 0.24 (0.02, 0.45) | |||||
Dose Effects
Intervention attendance and integrity were not related to depression or anxiety symptom outcomes.
Discussion
PRP-A significantly reduced hopelessness and depressive symptoms (on the CDI) and tended to reduce anxiety symptoms. These findings demonstrate that PRP is beneficial to adolescents when delivered by school teachers and counselors. This is important given the limited evidence for the effectiveness of depression prevention programs when delivered by community providers (Stice et al., 2009). Our findings add to a small but growing body of literature showing that prevention programs can be effective when delivered by school staff (e.g., Arnarson & Craighead, 2011). Our findings are particularly promising because most of our group leaders were teachers without any previous training in conducting therapy, let alone cognitive-behavioral interventions. If prevention programs can be delivered effectively by teachers, this holds great promise for wide-scale prevention.
While encouraging, the average effects were small, did not persist at 6-month follow-up, and did not translate into the prevention of depression or anxiety disorders. There may have been little room for an intervention effect in our sample during the 6-month follow-up period. PRP is designed to prevent the increase in depressive symptoms that occurs during the middle and high school years, but this increase did not occur in the control in our sample. Instead, mean depression symptom scores decreased in all 3 conditions, and by follow-up the control group scored well within the average range on depression and anxiety symptoms (Kovacs, 2001; Reynolds, 2002; Reynolds & Richmond, 1985). Few participants reported clinical levels of symptoms during interviews and there was a significant decrease in the percentage of students screening positively for depression and anxiety disorders from baseline to follow-up in the full sample (β = −0.50, SE = 0.23). In past studies, intervention effects have sometimes increased after the post and 6-month follow-up as depression symptoms begin to rise in the control group (e.g., Gillham, Reivich, Jaycox, & Seligman, 1995). This study will follow participants for 3 years, and it will be important to examine whether the program leads to lasting benefits and prevents the onset of disorders over time.
PRP was most effective for adolescents with average and above average levels of baseline hopelessness. In this subgroup, PRP significantly reduced depression symptoms, anxiety symptoms, and hopelessness, and increased active coping. Effect sizes were moderate for many of these outcomes. In contrast, among adolescents with low hopelessness, PRP had no significant effects. This pattern of findings is consistent with the conclusions of recent meta-analytic reviews that depression prevention programs are more beneficial to participants at high risk (Horowitz & Garber, 2006; Stice et al., 2009). Previous studies of PRP and of school-based CB depression prevention programs have not specifically targeted adolescents with elevated hopelessness and this may be a particularly important subgroup for future prevention efforts, especially since hopelessness is a strong predictor of subsequent depressive symptoms in this sample and in past research (e.g., Abela, Brozina, & Haigh, 2002; Hankin, Abramson, & Siler, 2001). At baseline, adolescents with elevated hopelessness were less likely than those with low hopelessness to use adaptive coping strategies. Thus, these adolescents may find PRP’s cognitive and behavioral skills useful. Although adolescents with low levels of hopelessness did not benefit from PRP in the current study, it is possible that their presence in the groups was beneficial to their peers. Adolescents who are more hopeful may model adaptive cognitive and coping styles. They may help their peers generate more realistic and optimistic alternatives. Many of our group leaders have suggested that this is an important part of the PRP group process. Peers can often provide more relevant and compelling models of adaptive coping than teachers or counselors.
The parent program did not boost PRP’s effectiveness; the addition of the parent program did not lead to greater benefits on any outcome than PRP-A alone. We found no significant differences in effects of the PRP-A and PRP-AP conditions and the findings were in the opposite direction from expected. While disappointing, the failure to find added benefits of the parent program is consistent with an earlier study that found no added benefit for a different PRP parent component (Gillham, 1994) and with the previous evaluation of the parent component to RAP (Shochet et al., 2001). Although parent attendance was better than for the original RAP study, it was lower than in the previous study of PRP for parents (Gillham, Reivich, et al., 2006). Most parents attended one session but few attended most sessions and only a quarter attended the booster sessions. Thus, many parents did not receive key intervention content. School counselors told us that attendance rates were typical for other programs they ran for parents and that boosting parent attendance at school functions is an ongoing challenge given the many other family and work responsibilities that parents have to juggle. Future work on PRP may do work within these constraints by distilling some of the core concepts into one or two key lessons, the time commitment that most parents were able to manage. Video or computer modules could make program content more available to parents (and adolescents), although it would be difficult to capture PRP’s interactive components through this modality.
Attendance difficulties may also have constrained the adolescent program’s effects. The after-school format posed challenges as many adolescents missed sessions because of conflicts with sports and other extracurricular activities. Future studies of PRP should examine the intervention when delivered during the school day. This will boost attendance and will ensure that PRP is evaluated in the specific contexts for which it is intended. PRP would fit well within advisory period or health classes. The CB skills such as critical thinking (evaluating thoughts and considering alternatives), assertiveness, problem-solving, and decision making fit well with many states’ educational objectives for the middle school years (Dusenbury, Zadrazil, Mart, & Weissberg, 2011).
PRP’s effects also may have been constrained by low adherence to the intervention. On average, group leaders only covered about half of the PRP content at a satisfactory level. In contrast, in past effectiveness studies that measured integrity, group leaders covered 80% of the content satisfactory level (Gillham et al., 2007; Gillham, Hamilton, et al., 2006) and one study found no significant benefits of PRP for groups with integrity below 80% (Gillham, Hamilton, et al., 2006). Group leader training procedures did not change substantially between these studies, so it is unclear why adherence was worse in the present study. Poor intervention integrity may be tied to attendance problems. Group leaders often had to return to topics covered in previous sessions to allow students who were absent to catch up on the material. This would frequently cause groups to fall behind and then move through the intervention material too quickly or skip topics in order to get back on schedule. Future research on PRP should examine whether intervention adherence (and outcomes) can be improved by enhancing group leader training and supervision. The PRP group leader training model places a heavy emphasis on the initial training period. Research on the dissemination of other school-based CB programs suggests effective dissemination may require more intense supervision and support while group leaders are delivering the intervention (Lochman et al., 2009), which may make it more difficult to disseminate interventions. An alternative approach is to use video, computer, and other media to deliver some of the key intervention components (Connor-Smith, Jensen, & Weisz, 2002)
Although intervention integrity and attendance did not predict improvements in depression or anxiety symptoms, our analyses only examined the overall level of integrity for each group and the total number of sessions each participant attended. These analyses may fail to capture more complex dosage effects (for example, if some PRP lessons or skills are more important than others or if attendance, integrity, and group process interact). Additionally, we treated integrity as a group-level construct in our analyses, meaning that all participants within a group received the same integrity score regardless of their attendance. A more nuanced analysis would combine attendance and group integrity into a single, subject-level dosage variable. This would also result in greater statistical power. Adolescents may benefit most if they are part of a cohesive group with high integrity that they and their peers attend regularly. Our research group is just beginning to explore these more complex relationships between group integrity, group process, attendance, and outcome.
PRP-A’s effects on depression symptoms differed by measure. PRP-A significantly reduced depression symptoms on the CDI but not the RADS-2. In depression prevention studies that include more than one self-report measure, this kind of discrepancy is common (e.g., Horowitz, Garber, Ciesla, Young, & Mufson, 2007; Merry et al., 2004; Muñoz et al., 1995). Self-report measures of depression differ in the degree to which they emphasize different types of symptoms (for example, DSM-IV diagnostic criteria versus somatic complaints and other symptoms that frequently occur with depression) and the degree to which they focus on the frequency, intensity, and duration of symptoms. The different findings by measure raise the possibility that depression prevention programs have stronger effects for some symptoms than others. Although an examination of specific items or subscales on the CDI and RADS-2 is beyond the scope of this project, one intriguing possibility is that CB interventions like PRP are most beneficial for sad mood, hopelessness, motivational deficits, unrealistic worry, feelings of worthlessness, and other difficulties that are predicted by the Hopelessness Theory of depression (Abramson, Metalsky, & Alloy, 1989). Research by Abela and colleagues suggests that cognitive vulnerabilities and maladaptive response styles are most predictive of these symptoms (Abela, Gagnon, & Auerbach, 2007). Research that examines effects on specific types of symptoms may help to identify where programs are having their strongest impact, and also identify symptoms and difficulties for which other skills or other interventions may be needed.
In the context of this special issue, we consider the connections between John Abela’s seminal work on risk factors for depression in youth and research on cognitive behavioral depression prevention programs, including PRP. Abela’s research on risk factors provides a strong foundation for CB depression prevention programs. It suggests that depression can be prevented through interventions that improve adolescents’ cognitive styles, reduce maladaptive response styles such as rumination, and increase adaptive problem solving and coping strategies. It is encouraging that PRP-A reduces hopelessness and that it also improves coping in adolescents with average and above average levels of hopelessness.
Abela’s work also raises challenging questions and rich possibilities for prevention research. Much of his work emphasized nuance and complexity, as well as the importance of considering the individual’s experience, even when examining quantitative data from large longitudinal studies. His Weakest Link theory suggests the value of attending to each adolescent’s greatest area of cognitive vulnerability (Abela & Sarin, 2002). For some adolescents this will be pessimistic explanatory style, for others it may be the tendency to infer negative consequences or to view the self as deeply flawed following negative events. Research by Abela and his colleagues suggests that adolescents’ risk for depression is related to their weakest cognitive vulnerability (Abela, McGirr, & Skitch, 2007). Interventions that improve an adolescent’s weakest link may be particularly beneficial. Interventions that can improve the various weakest links in large groups of adolescents may have the greatest potential for wide-spread prevention.
Abela’s work suggests limits to examining different responses to stress (e.g., active coping, rumination, distraction) as separate outcomes. Adolescents’ risk for depression may be more closely connected to their tendency to employ adaptive as opposed to maladaptive responses, particularly rumination (Abela, Aydin, & Auerbach, 2007). Future work on PRP will do well to examine this response ratio. In addition, it is important to evaluate whether adolescents’ responses are appropriate to a given stressor and context.
Abela’s research reminds us that most cognitive-behavioral models of depression are vulnerability-stress models. Adolescents with maladaptive cognitive and response styles are at particularly high risk for depression when they encounter negative life events (Abela, 2001; Abela & Hankin, 2008, 2011; Auerbach, Abela, Zhu, & Yao, 2010). In the absence of stress, cognitive and response styles may not be linked to depression. Abela and colleagues have pushed risk factor researchers to examine vulnerability-stress interaction. Prevention researchers would do well to consider this interaction as well. Prevention effects may be most visible among participants who experience stressful events during the follow-up period. The assessment of life events may enable researchers to better to detect the benefits of prevention programs that are delivered universally. In examining the role of life stress, it will be important to consider increases in stress relative to each individual’s average or baseline (Abela, Aydin, & Auerbach, 2006; Abela, McGirr, & Skitch, 2007). Given the evidence that maladaptive cognitive styles, coping styles, and depressive symptoms contribute to difficulties in relationships and achievement (Hammen, 1991; Shih, Abela, & Starrs, 2009), decreases in life events could be an important outcome of depression prevention programs.
These observations suggest several limits of the current study and of research on CB depression prevention programs in general. Our program evaluation is rudimentary in comparison to Abela and colleagues’ research on risk factors for depression. In addition, our findings are limited by their reliance on self-report measures. In other work, we are examining whether teachers, parents, and other observers notice improvements in children’s coping behavior, depression, and anxiety symptoms. The present study also did not control for non-specific intervention ingredients (group leader attention, peer support, etc.). Thus, it is not clear that intervention effects observed in this study are due to the particular cognitive and behavioral skills covered in PRP. In addition, most of the participants in our sample were of European American descent and had parents who had completed college, although many previous studies have tested PRP with adolescents from other socioeconomic, racial, and cultural backgrounds (Brunwasser et al., 2009).
Implications for Research, Policy, and Practice
Our research group hopes to develop effective prevention programs that target psychosocial risk factors for depression during adolescence. Research by John Abela and colleagues provides a strong foundation for this work. Adolescents’ cognitive styles and responses to stress can increase risk for (or protect against) depression. Our findings suggest that cognitive-behavioral depression prevention programs that target these risk factors reduce depression symptoms and tend to reduce anxiety symptoms. These programs may be most helpful to adolescents with higher levels of cognitive vulnerability, particularly hopelessness. Our findings also suggest that prevention programs are beneficial (at least in the short term) when delivered by school teachers and counselors. Additional research is needed to determine whether these benefits can endure and translate into the prevention of depression and anxiety disorders.
By incorporating insights from Abela’ seminal work on risk factors for depression in children and adolescence, prevention researchers can develop more powerful program evaluations that examine cognitive styles, coping skills, and stressful life events as potential moderators, mediators, and intervention outcomes. Such research can increase our understanding of how existing prevention programs work and for whom they work best. Ultimately, such research can inform the development of more powerful prevention programs.
Acknowledgments
This project was supported by National Institute of Mental Health grant MH52270. Clinical trials registration #: NCT00360451. We would like to thank the adolescents, parents, school counselors, and teachers who participated in this project.
Footnotes
The Penn Resiliency Program materials are available for use in research. Materials can be requested by info@pennproject.org
Disclosures: Drs. Gillham and Reivich are authors of the Penn Resiliency Program. T Pennsylvania has licensed the Penn Resiliency Program to Adaptiv Learning Systems. Drs. Reivich and Seligman own Adaptiv stock and could profit from the sale of this program. None of the other authors of this study has a financial relationship with Adaptiv.
Contributor Information
Jane E. Gillham, Department of Psychology, Swarthmore College and Positive Psychology Center, University of Pennsylvania
Karen J. Reivich, Positive Psychology Center, University of Pennsylvania, reivich@sas.upenn.edu
Steven M. Brunwasser, Positive Psychology Center, University of Pennsylvania, stevenbr@psych.upenn.edu
Derek R. Freres, Positive Psychology Center, University of Pennsylvania, dfreres@sas.upenn.edu
Norma D. Chajon, Positive Psychology Center, University of Pennsylvania, nchajon@darienps.org
V. Megan Kash-MacDonald, Positive Psychology Center, University of Pennsylvania, v.kash-macdonald@ucl.ac.uk
Tara M. Chaplin, Positive Psychology Center, University of Pennsylvania, tara.chaplin@yale.edu
Rachel M. Abenavoli, Positive Psychology Center, University of Pennsylvania, rma5183@psu.edu
Samantha L. Matlin, Positive Psychology Center, University of Pennsylvania, samantha.matlin@yale.edu
Robert J. Gallop, Department of Mathematics and Applied Statistics, West Chester University, rgallop@wcupa.edu
Martin E.P. Seligman, Department of Psychology and Positive Psychology Center, University of Pennsylvania, seligman@psych.upenn.edu
References
- Abela JRZ. The hopelessness theory of depression: A test of the diathesis-stress and causal mediation components in third and seventh grade children. Journal of Abnormal Child Psychology. 2001;29:241–254. doi: 10.1023/a:1010333815728. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Aydin C, Auerbach RP. Operationalizing the “vulnerability” and “stress” components of the hopelessness theory of depression: A multi-wave longitudinal study. Behaviour Research and Therapy. 2006;44:1565–1583. doi: 10.1016/j.brat.2005.11.010. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Aydin CM, Auerbach RP. Responses to depression in children: Reconceptualizing the relation among response styles. Journal of Abnormal Child Psychology. 2007;35:913–927. doi: 10.1007/s10802-007-9143-2. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Brozina K, Haigh EP. An examination of response styles theory of depression in third- and seventh-grade children: A short-term longitudinal study. Journal of Abnormal Child Psychology. 2002;30:515–527. doi: 10.1023/a:1019873015594. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Gagnon H, Auerbach RP. Hopelessness depression in children: An examination of the symptom component of the Hopelessness Theory. Cognitive Therapy and Research. 2007;31:401–417. [Google Scholar]
- Abela JRZ, Hankin BL. Cognitive vulnerability to depression in children and adolescents: A psychopathology perspective. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. Guilford Press; New York, NY, US: 2008. pp. 35–78. [Google Scholar]
- Abela JRZ, Hankin BL. Rumination as a vulnerability factor to depression during the transition from early to middle adolescence: A multiwave longitudinal study. Journal of Abnormal Psychology. 2011;120:259–271. doi: 10.1037/a0022796. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, McGirr A, Skitch SA. Depressogenic inferential styles, negative events, and depressive symptoms in youth: An attempt to reconcile past inconsistent findings. Behaviour Research and Therapy. 2007;45:2397–2406. doi: 10.1016/j.brat.2007.03.012. [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Sarin S. Cognitive vulnerability to hopelessness depression: A chain is only as strong as its weakest link. Cognitive Therapy and Research. 2002;26:811–829. [Google Scholar]
- Abela JRZ, Vanderbilt E, Rochon A. A test of the integration of the response styles and social support theories of depression in third and seventh grade children. Journal of Social and Clinical Psychology. 2004;23:653–674. [Google Scholar]
- Abela JRZ, Zinck S, Kryger S, Zilber I, Hankin BL. Contagious depression: Negative attachment cognitions as a moderator of the temporal association between parental depression and child depression. Journal of Clinical Child & Adolescent Psychology. 2009;38:16–26. doi: 10.1080/15374410802575305. [DOI] [PubMed] [Google Scholar]
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Arnarson EO, Craighead WE. Prevention of depression among Icelandic adolescents: A 12-month follow-up. Behaviour Research and Therapy. 2011;49:170–174. doi: 10.1016/j.brat.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Goldstein MJ, Thompson M, Guthrie D. One-year outcomes of depressive disorders in child psychiatric in-patients: Evaluation of the prognostic power of a brief measure of expressed emotion. Journal of Child Psychology and Psychiatry. 1993;23:129–137. doi: 10.1111/j.1469-7610.1993.tb00975.x. [DOI] [PubMed] [Google Scholar]
- Auerbach RP, Abela JRZ, Zhu X, Yao S. Understanding the role of coping in the development of depressive symptoms: Symptom specificity, gender differences, and cross-cultural applicability. British Journal of Clinical Psychology. 2010;49:547–561. doi: 10.1348/014466509X479681. [DOI] [PubMed] [Google Scholar]
- Ayers TS, Sandler IM, West SG, Roosa MW. A dispositional and situational assessment of children’s coping: Testing alternative models of coping. Journal of Personality. 1996;64:923–958. doi: 10.1111/j.1467-6494.1996.tb00949.x. [DOI] [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B. lme4: Linear mixed-effects models using S4 classes (R package version 0.999375-39) [computer software] 2011 Retrieved from http://CRAN.R-project.org/package=lme4.
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;34:129–137. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Wright EJ, Salt P, Drezner K, Gladstone TRG, Versage EM, Rothberg PC. Examination of children’s responses to two preventive intervention strategies over time. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:196–204. doi: 10.1097/00004583-199702000-00010. [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. International Universities Press; New York: 1976. [Google Scholar]
- Brunwasser SM, Gillham JE, Kim E. A meta-analytic review of the Penn Resiliency Program’s effects on depressive symptoms. Journal of Consulting and Clinical Psychology. 2009;77:1042–1054. doi: 10.1037/a0017671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cjuipers P, van Straten A, Smit F, Mihalopoulos C, Beekman A. Preventing the onset of depressive disorders: A meta-analytic review of psychological interventions. American Journal of Psychiatry. 2008;165:1272–1280. doi: 10.1176/appi.ajp.2008.07091422. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, O’Connor E, Seeley J. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Archives of General Psychiatry. 2001;58:1127–1134. doi: 10.1001/archpsyc.58.12.1127. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Keller G, Champion JE, Rakow A, Reeslund KL, McKee L, Fear JM, Colletti JM, Hardcastle E, Merchant MJ, Roberts E, Sterba SK, Cole DA. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology. 2009;77:1007–1020. doi: 10.1037/a0016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor-Smith JK, Jensen AL, Weisz JR. Act & Adapt: A Video Series to Guide the PASCET Program. University of California; Los Angeles: 2002. [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Dusenbury L, Zadrazil J, Mart A, Weissberg R. State learning standards to advance social and emotional learning: The state scan of social and emotional learning standards, preschool through high school. Department of Psychology, University of Illinois at Chicago. 2011 Available at http://casel.org/wp-content/uploads/2011/05/Forum-Brief-on-the-State-Scan-5-10-2011.pdf.
- Ellis A. Reason and emotion in psychotherapy. Lyle Stuart; New York: 1962. [Google Scholar]
- Garber J, Clarke GN, Weersing VR, Beardslee WR, Brent DA, Gladstone TRG, DeBar LL, Lynch FL, D’Angelo E, Hollon SD, Shamseddeen W, Iyengar S. Prevention of depression in at-risk adolescents: A randomized controlled trial. Journal of the American Medical Association. 2009;301:2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Flynn C. Predictors of depressive cognitions in young adolescents. Cognitive Therapy and Research. 2001;25:353–376. [Google Scholar]
- Gillham JE. Preventing depressive symptoms in school children. Dissertation Abstracts International: Section B. Sciences and Engineering. 1994;55(09):4119. [Google Scholar]
- Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: A randomized controlled study of the Penn Resiliency Program. Journal of Abnormal Child Psychology. 2006;34:203–219. doi: 10.1007/s10802-005-9014-7. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté AJ, Samuels B, Elkon AGL, Litzinger S, Lascher M, Gallop R, Seligman MEP. School-based prevention of depressive symptoms: A randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program. Journal of Consulting and Clinical Psychology. 2007;75:9–19. doi: 10.1037/0022-006X.75.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatté A, Seligman MEP. School-based prevention of depression and anxiety symptoms in early adolescence: A pilot of a parent intervention component. School Psychology Quarterly. 2006;21:323–348. [Google Scholar]
- Gillham JE, Reivich KJ, Jaycox LH, Seligman MEP. Preventing depression in schoolchildren: Two year follow-up. Psychological Science. 1995;6:343–351. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abela JRZ. Depression from childhood through adolescence and adulthood: A developmental vulnerability and stress perspective. In: Hankin BL, Abela JRZ, editors. Development of psychopathology: A vulnerability-stress perspective. Sage; Thousand Oaks, CA: 2005. pp. 245–288. [Google Scholar]
- Hankin BL, Abramson LY, Siler M. A prospective test of the hopelessness theory of depression in adolescence. Cognitive Therapy and Research. 2001;25:607–632. [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KA. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10 year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L. Prevention of depressive symptoms in adolescents: A randomized trial of cognitive-behavioral and interpersonal prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:693–706. doi: 10.1037/0022-006X.75.5.693. [DOI] [PubMed] [Google Scholar]
- Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. Journal of Adolescent Health. 2007;41:455–463. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Medical Care. 2006;44:1064–1072. doi: 10.1097/01.mlr.0000237421.17555.8f. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, French NH, Unis AS, Esveldt-Dawson K, Sherick RB. Hopelessness, depression, and suicidal intent among psychiatrically disturbed inpatient children. Journal of Consulting and Clinical Psychology. 1983;51:504–510. doi: 10.1037//0022-006x.51.4.504. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Rodgers A, Colbus D. The hopelessness scale for children: Psychometric characteristics and concurrent validity. Journal of Consulting and Clinical Psychology. 1986;54:241–245. doi: 10.1037//0022-006x.54.2.241. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (NCS-R) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory manual. Multi-Health Systems; North Tonawanda, NY: 2001. [Google Scholar]
- Lambert SF, McCreary BT, Joiner TE, Schmidt NB, Ialongo NS. Structure of anxiety and depression in urban youth: An examination of the tripartite model. Journal of Consulting and Clinical Psychology. 2004;72:904–908. doi: 10.1037/0022-006X.72.5.904. [DOI] [PubMed] [Google Scholar]
- Lewcyzk CM, Garland AF, Hurlburt MS, Gearity J, Hough RL. Comparing DISC-IV and clinician diagnoses among youths receiving public mental health services. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:349–356. doi: 10.1097/00004583-200303000-00016. [DOI] [PubMed] [Google Scholar]
- Lochman JE, Boxmeyer C, Powell N, Qu L, Wells K, Windle M. Dissemination of the Coping Power Program: Importance of intensity of counselor training. Journal of Consulting and Clinical Psychology. 2009;77:397–409. doi: 10.1037/a0014514. [DOI] [PubMed] [Google Scholar]
- Mathers C, Boerma T, Ma Fat D. The global burden of disease: 2004 update. Department of Health Statistics and Informatics, World Health Organization; Switzerland: 2008. [Google Scholar]
- Merry S, McDowell H, Wild CJ, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based prevention program. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:538–547. doi: 10.1097/00004583-200405000-00007. [DOI] [PubMed] [Google Scholar]
- Muñoz RF, Ying Y-W, Bernal G, Pérez-Stable EJ, Sorensen JL, Hargreaves WA, Miranda J, Miller LS. Prevention of depression with primary care patients: A randomized controlled trial. American Journal of Community Psychology. 1995;23:199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS, Seligman M.E.y. Predictors and consequences of childhood depressive symptoms: A five-year longitudinal study. Journal of Abnormal Psychology. 1992;101:405–422. doi: 10.1037//0021-843x.101.3.405. [DOI] [PubMed] [Google Scholar]
- Parker G. Parental rearing style: Examining for links with personality vulnerability factors for depression. Social Psychiatry and Psychiatric Epidemiology. 1993;28:97–100. doi: 10.1007/BF00801738. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Program for Prevention Research . Manual for the Children’s Coping Strategies Checklist & the How I Coped Under Pressure Scale. Program for Prevention Research, Arizona State University; 1999. Unpublished manuscript. [Google Scholar]
- R Development Core Team . R: A Language and Environment for Statistical Computing (version 2.12.0) [computer software] R Foundation for Statistical Computing; Vienna, Austria: 2010. Available from http://www.R-project.org/ [Google Scholar]
- Raudenbush SW, Xiao-Feng L. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods. 2001;6:387–401. [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. Revised Children’s Manifest Anxiety Scale: Manual. Western Psychological Services; Los Angeles: 1985. [Google Scholar]
- Reynolds WM. Reynolds Adolescent Depression Scale (2nd Ed.) Psychological Assessment Resources, Inc.; Odessa, FL: 2002. [Google Scholar]
- Roberts C, Kane R, Bishop B, Matthews H, Thomson H. The prevention of depressive symptoms in rural school children: A follow-up study. International Journal of Mental Health Promotion. 2004;6:4–16. [Google Scholar]
- Roberts N, Parker KCH, Dagnone M. Comparison of clinical diagnoses, NIMH-DISC-IV diagnoses and SCL-90-R ratings in an adolescent psychiatric inpatient unit: A brief report. Canadian Child and Adolescent Psychiatry Review. 2005;14:103–105. [PMC free article] [PubMed] [Google Scholar]
- Seligman MEP. Learned optimism. Knopf.; New York: 1991. [Google Scholar]
- Seligman MEP, Peterson C, Kaslow NJ, Tenenbaum RL, Alloy LB, Abramson LY. Attributional style and depressive symptoms among children. Journal of Abnormal Psychology. 1984;93:235–241. doi: 10.1037//0021-843x.93.2.235. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shih JH, Abela JRZ, Starrs C. Cognitive and interpersonal predictors of stress generation in children of affectively ill parents. Journal of Abnormal Child Psychology. 2009;37:195–208. doi: 10.1007/s10802-008-9267-z. [DOI] [PubMed] [Google Scholar]
- Shochet IM, Dadds MR, Holland D, Whiteford K, Harnett PH, Osgarby SM. The efficacy of a universal school-based program to prevent adolescent depression. Journal of Clinical Child Psychology. 2001;30:303–315. doi: 10.1207/S15374424JCCP3003_3. [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau JM, Wade E. Efficacy trial of a brief cognitive-behavioral depression prevention program for high-risk adolescents: Effects at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2010;78:856–867. doi: 10.1037/a0020544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young JF, Mufson L, Gallop R. Preventing depression: A randomized trial of interpersonal psychotherapy-adolescent skills training. Depression and Anxiety. 2010;27:426–433. doi: 10.1002/da.20664. [DOI] [PMC free article] [PubMed] [Google Scholar]