Abstract
Background
Previous studies assessing second primary malignancies (SPMs) after uterine cancer have been conducted in Western populations with conflicting results. This study aimed to define the incidence and risk of SPMs in Taiwanese patients with an initial diagnosis of uterine cancer.
Methods
Using population-based data from the Taiwan Cancer Registry for the period 1979–2008, we quantified standardized incidence ratios (SIRs) among 11,571 women with an initial diagnosis of uterine cancer.
Results
Among the 11,571 women, 555 (4.80 %) developed at least one SPM during 69,987 person-years of follow-up. There was a 71 % increased risk of SPM following uterine cancer (SIR = 1.71, 95 % CI, 1.57–1.86), with higher risks in the vagina/vulva (SIR = 9.06), small intestine (SIR = 8.45), ovary (SIR = 4.15), urinary bladder (SIR = 2.31), kidney (SIR = 2.24), colorectum (SIR = 2.24), lung (SIR = 1.96), and breast (SIR = 1.43). The risk of SPM was found to be the highest within the first 5 years after diagnosis of uterine cancer, with surveillance bias possibly contributing to the extremely high risk observed in the first follow-up year. The overall risk and pattern of SPM development observed in this study differed from those previously reported in Western populations, possibly because of the methodology and shorter follow-up period employed in this study. The cumulative incidence of SPMs was significantly higher in older patients (≥50 years) than in younger patients (P < 0.001).
Conclusions
To our knowledge, this is the first study in an Asian population to report 71 % increased risk in SPMs in women previously diagnosed with uterine cancer. A younger age at diagnosis of uterine cancer conferred an increased risk of second malignancies, and SPMs worsened survivorship in patients who survived uterine cancer.
Keywords: Uterine cancer, Second primary malignancy, Standardized incidence ratios
Background
Uterine cancer is the sixth most common malignancy in women worldwide [1]. In Western countries, it is the most common gynecological malignancy, with a continuously rising incidence rate [1-3]. For example, the incidence of endometrial cancer reportedly increased by 21 % from 2008–2012 in the United States [3]. The incidence in Asian countries has been lower but has markedly increased in recent decades [4, 5]. In Taiwan, the incidence of uterine cancer has more rapidly increased than other malignancies from 3.43–15.07 per 100,000 between 1996 and 2010 [6, 7]. It is noteworthy that age at onset of uterine cancer among Asian patients has been reported to peak at 45–55 years, at least 10–15 years earlier than that reported in Western patients [4]. A similar trend in age at breast cancer diagnosis has been reported in Asian patients [8]; however, the mechanisms underlying the lower age at onset for both cancers remain unclear. Further evaluation of the risk of second primary malignancies (SPMs) following uterine cancer may provide some insights to its etiology.
Similar to the United States, uterine cancers in Taiwan comprise ~90 % adenocarcinomas, 8 % sarcomas, and other unspecified types [9, 10]. The 5-year overall survival rate for uterine cancers recorded in the Surveillance, Epidemiology, and End Results (SEER) database (1988–2001) was found to be 87.9 %. Of all patients in this database, 75.3 % had stage I disease, and these patients had a five-year survival rate of 97.4 % [9]. Considering the increasing incidence and survival rate of patients with uterine cancer worldwide, SPMs have become an increasingly important clinical issue. Nevertheless, most studies about SPMs after uterine cancer have been conducted in Western populations [11-18]. The most comprehensive evaluation of the SEER database has demonstrated markedly elevated SIRs for several specific sites; however, the overall SIR was not found to be increased [19]. Similarly, two large SEER studies based on 90,502 and 98,205 patients with primary endometrial cancer from 1973–2004 and 1973–2007, respectively, revealed that the overall risk of SPMs did not differ from the general population [14, 18]. In contrast, a nationwide Swedish population-based study reported a 54 % increased risk in overall SPMs [13], and other studies have reported a higher risk of developing SPMs after uterine cancers in patients with a young age at diagnosis [17], African ancestry [18], Lynch syndrome (LS), family history of breast or ovarian cancer [12, 13, 17], and in those receiving radiotherapy [15, 16].
There are racial disparities in the SEER database [18]. The overall risk of SPMs after endometrial cancer was found to be higher in Americans of an African descent (SIR = 1.19; 95 % CI, 1.08–1.31) and lower in Caucasians (SIR = 0.85; 95 % CI, 0.84–0.87) compared with the general population. Furthermore, the pattern of SPMs was found to differ between African American and Caucasian populations. Therefore, there is a clinical requirement for studies assessing SPMs following uterine cancers in Asian populations, which, to our knowledge, have not been previously reported. To achieve this objective, we conducted a retrospective population-based study using a database from the Taiwan Cancer Registry (TCR) that included a total of 12,509 patients with an initial diagnosis of uterine cancer between 1979 and 2008.
Methods
Data sources
We quantified the incidence of SPMs among the 12,509 patients with an initial diagnosis of uterine cancer (International Classification of Diseases, 9th Revision (ICD-9) codes: 179 and 182) reported in TCR (http://crs.cph.ntu.edu.tw/) from January 1, 1979–December 31, 2008. This TCR was founded in 1979 and is financed by the Ministry of Health and Welfare for estimating the incidence of cancer in Taiwan. It is a population-based cancer registry that covered 22 million people in 2003. Furthermore, the hospitals with more than 50 beds are required to submit information regarding patients with newly diagnosed cancer to TCR, which reimburses the hospitals based on the reported number of cases for reducing the possibility of under-reporting. All cancer registry databases in TCR have been systemically converted to ICD-9 codes [20] and linked with death certificates from the national death database. Therefore, individuals not identified by this process were considered to be alive for the purpose of the current study (passive follow-up). Coding of multiple primaries followed the principles of International Association of Cancer Registries (IACR) and International Agency for Research on Cancer (IARC) [21-23]. Informed consent was not required because all registry records are anonymous and accessible to the public. The study was approved by the Ethics Committee of the Chang Gung Memorial Hospital.
Since 1996, 80 %–90 % of patients with uterine cancer have received hysterectomy as the standard treatment in Taiwan, limiting the risk of secondary cervical cancer [6, 7]. One hundred and three patients with a second cervical cancer (ICD-9: 180) were excluded from the analysis as discrimination between cervical cancer, endometrial cancer extending to the cervix, and cervical recurrence was challenging in patients who did not receive hysterectomy. Thus, this study evaluated the risk of secondary non-cervical cancers. We aimed to accurately determine the age at onset, estimate the person-years of follow-up, and minimize potentially unconfirmed cancer diagnoses in this study cohort. A total of 835 patients were excluded from analysis because they met one or more of the following criteria: (1) missing birth date (7 cases); (2) missing follow-up date or death status (128 cases); (3) SPM diagnosis or death occurring less than 1 month after diagnosis of uterine cancer (684 cases); or (4) age under 20 years (18 cases). Thus, 11,571 patients were included in the analysis.
Statistical analysis
SIRs and the corresponding 95 % CIs were calculated [24] for all types of SPMs except for uterine corpus to quantify the rate of second malignancy development after diagnosis of uterine cancer. SIRs were calculated as the ratio of the observed number (O) of SPMs to the expected number (E), assuming the patients had the same incidence of cancer as the general female population. The number of person-years at risk was defined as the number of years from the date of diagnosis of uterine cancer to the date of death, date of SPM diagnosis, or end of the study period (December 31, 2008), whichever occurred first. The person-years of observation for each 5-year age group, 5-year period (1979–1983, 1984–1988, 1989–1993, 1994–1998, 1999–2003, and 2004–2008), and the time from entry to the cohort (≤1, 1–5, 5–10, or >10 years) were multiplied by cancer incidence rates for the Taiwanese female population. The corresponding products were summed over all ages and calendar years to yield the expected numbers of SPMs at each site. SIR confidence intervals were based on an assumed Poisson distribution of SPM cases. An approximate χ2 test was used for evaluating differences between two SIRs and trends in SIRs.
Survival curves of patients with uterine cancer diagnosed at age <50 and ≥50 years were calculated using the Kaplan–Meier method. Differences between the two age groups were examined by the log-rank test. Further, the Cox model with a time-dependent covariate [25, 26], allocating follow-up time for each patient to the non-SPM group until SPM occurrence, was used for comparing the survival between patients with and without SPM. All statistical tests were two-sided, and a P value of less than 0.05 was considered statistically significant.
Results
Patient characteristics
Of the 11,571 women with an initial diagnosis of uterine cancer (4,445 diagnosed at age <50 years and 7,126 at age ≥50 years) and the complete data available for analysis, 555 (4.80 %) developed SPM during 69,987 person-years of follow-up (Table 1). Of all the enrolled patients, 10.47 % were diagnosed with uterine sarcoma, and the remaining with endometrial cancer. Overall, uterine cancer was diagnosed at a mean age of 52.93 years, and the mean age at SPM diagnosis was 61.23 years. The average follow-up time was 6.05 years, including 9,638 cases (83 %) followed up for at least one year, 2,678 (23 %) for 5–10 years, and 2,518 (22 %) for >10 years. The average interval between the first and second cancers was 6.27 years, with a standard deviation of 5.53 years.
Table 1.
Characteristics of population-based cohort of 11,571 patients first diagnosed as uterine cancer (ICD-9: 179, 182) in Taiwan 1979-2008
| All | <50 years olda | ≥50 years olda | |
|---|---|---|---|
| No. with uterine cancer | 11,571 | 4,445 (38.42 %) | 7,126 (61.58 %) |
| No. who developed a SPM (%) | 555 (4.80 %) | 163 (3.67 %) | 392 (5.50 %) |
| Average age at diagnosis of uterine cancer ± SD (years) | 52.93 ± 11.69 | 41.63 ± 6.22 | 59.98 ± 8.26 |
| Average age at diagnosis of SPM ± SD (years) | 61.23 ± 11.78 | 48.59 ± 8.57 | 66.50 ± 8.49 |
| Average interval between first and second cancers ± SD (years) | 6.27 ± 5.53 | 6.61 ± 5.68 | 6.14 ± 5.47 |
| Average follow-up (years) | 6.05 ± 5.55 | 7.00 ± 5.84 | 5.46 ± 5.27 |
SD standard deviation, SPM second primary malignancy
aAge at uterine cancer diagnosis. An age of 50 years was selected for comparison as this is the average menopausal age in Taiwanese women
Risk of second primary malignancies stratified by site
SIRs and the corresponding 95 % CIs for SPMs at all sites, except the uterine corpus, were calculated. Patient ages at initial uterine cancer and SPM diagnoses are presented in Table 2. Irrespective of the site, the overall SIR for developing SPM was 1.71 (95 % CI, 1.57–1.86). Regarding SPM sites, the risk of developing genital malignancies, including ovarian, vaginal, and vulvar, was the highest (SIR = 4.91; 95 % CI, 3.71–6.37), followed by the urinary system (SIR = 2.27; 95 % CI, 1.64–3.06) and digestive system (SIR = 1.71; 95 % CI, 1.49–1.96). In particular, there was an increased risk of vaginal/vulvar (SIR = 9.06), small intestinal (SIR = 8.45), ovarian (SIR = 4.15), urinary bladder (SIR = 2.31), kidney (SIR = 2.24), colorectal (SIR = 2.24), lung (SIR = 1.96), and breast (SIR = 1.43) cancers (Table 2).
Table 2.
Observed (O) and expected (E) numbers of second primary cancers after diagnosis of an initial uterine cancer (ICD-9 179, 182) in Taiwan 1979-2008
| SPM site (ICD-9 code) | Age of uterine cancer (years) (mean ± SD) | Age of SPM (years) (mean ± SD) | O | E | SIR (O/E) | (95 % CI) |
|---|---|---|---|---|---|---|
| Head and neck | 57.89 ± 11.95 | 63.67 ± 12.94 | 9 | 10.51 | 0.86 | (0.39, 1.63) |
| Oral & pharynx (141, 143-5, 146,148-9) | 49.50 ± 5.92 | 54.25 ± 8.96 | 4 | 4.81 | 0.83 | (0.22, 2,13) |
| Nasopharynx (147) | 71.67 ± 8.33 | 77.00 ± 6.93 | 3 | 4.48 | 0.67 | (0.13, 1.96) |
| Larynx (161) | 57 | 70 | 1 | 0.41 | 2.45 | (0.03, 13.64) |
| Major salivary glands (142) | 51 | 55 | 1 | 0.80 | 1.24 | (0.02, 6.92) |
| Digestive system | 56.21 ± 10.12 | 63.28 ± 10.41 | 212 | 124.06 | 1.71 | (1.49, 1.96) |
| Esophagus (150) | 58.00 ± 1.41 | 65.50 ± 7.78 | 2 | 1.57 | 1.28 | (0.14, 4.61) |
| Stomach (151) | 59.92 ± 9.06 | 66.88 ± 8.59 | 25 | 17.09 | 1.46 | (0.95, 2.16) |
| Small intestine (152) | 50.33 ± 10.45 | 56.50 ± 11.34 | 12 | 1.42 | 8.45 | (4.36, 14.77) |
| Colorectum (153,154) | 54.70 ± 10.43 | 61.22 ± 10.42 | 119 | 53.05 | 2.24 | (1.86, 2.68) |
| Liver (155) | 60.16 ± 6.81 | 69.09 ± 6.72 | 45 | 39.42 | 1.14 | (0.83, 1.53) |
| Biliary system (156) | 63.67 ± 15.95 | 71.67 ± 13.43 | 3 | 4.82 | 0.62 | (0.13, 1.82) |
| Pancreas (157) | 48.50 ± 12.57 | 54.17 ± 12.98 | 6 | 6.69 | 0.90 | (0.33, 1.95) |
| Genital system | 49.48 ± 12.52 | 52.57 ± 13.82 | 56 | 11.42 | 4.91 | (3.71,6.37) |
| Ovary (183) | 48.40 ± 11.54 | 49.75 ± 11.43 | 40 | 9.65 | 4.15 | (2.95, 5.64) |
| Vagina and vulva (184) | 52.19 ± 14.75 | 59.63 ± 16.92 | 16 | 1.77 | 9.06 | (5.17, 14.71) |
| Urinary system | 55.95 ± 13.10 | 64.14 ± 12.18 | 43 | 18.94 | 2.27 | (1.64, 3.06) |
| Urinary bladder (188) | 53.89 ± 15.02 | 62.28 ± 14.42 | 18 | 7.79 | 2.31 | (1.37, 3.65) |
| Kidney (189) | 57.44 ± 11.62 | 65.48 ± 10.38 | 25 | 11.16 | 2.24 | (1.45, 3.31) |
| Lung and bronchus (162) | 58.63 ± 10.19 | 64.97 ± 10.99 | 72 | 36.81 | 1.96 | (1.53, 2.46) |
| Sarcoma (171) | 48.50 ± 16.81 | 52.50 ± 16.45 | 6 | 6.77 | 0.89 | (0.32, 1.93) |
| Skin (173) | 52.50 ± 11.57 | 59.14 ± 12.38 | 14 | 11.85 | 1.18 | (0.65, 1.98) |
| Breast (174) | 53.41 ± 10.20 | 59.23 ± 10.46 | 95 | 66.51 | 1.43 | (1.16, 1.75) |
| Brain (191) | 52.00 ± 9.02 | 54.75 ± 9.25 | 4 | 2.25 | 1.78 | (0.48, 4.55) |
| Thyroid (193) | 55.46 ± 10.61 | 59.77 ± 11.50 | 13 | 9.84 | 1.32 | (0.70, 2.26) |
| Leukemia (204-8) | 51.33 ± 7.12 | 58.00 ± 9.80 | 9 | 5.07 | 1.77 | (0.81, 3.37) |
| Lymphoma (200-3) | 61.00 ± 7.62 | 67.57 ± 6.58 | 7 | 8.39 | 0.83 | (0.33, 1.72) |
| Others | 50.27 ± 13.00 | 56.93 ± 13.80 | 15 | 12.54 | 1.20 | (0.67, 1.97) |
| Total | 55.01 ± 11.45 | 60.54 ± 12.08 | 555 | 324.95 | 1.71 | (1.57, 1.86) |
Bold denotes statistical significance
SD standard deviation, SIR standardized incidence ratio, SPM second primary malignancy, O observed numbers of SPMs, E expected numbers of SPMs, CI confidence interval
Risk of second primary malignancies stratified by age at diagnosis of uterine cancer
For the eight sites with an increased risk of SPMs, SIRs were further stratified according to age at diagnosis of uterine cancer (<50 and ≥50 years, Table 3, left half). Overall, patients <50 years at onset had a slightly higher risk of developing SPM than those aged ≥50 years (SIR = 2.44 vs. 1.98, P = 0.06). The age-based trend was the most prominent for small intestinal, colorectal, and ovarian SPMs (P = 0.005, 0.001, and 0.018, respectively), whereas the risk of lung, breast, vaginal, urinary bladder, and kidney SPMs was similar between age groups.
Table 3.
Risk for significant second primary cancers by age at diagnosis of uterine cancer (left half) and follow-up interval (right half), respectively
| SPM site (ICD-9 code) | Agea (years) | O | E | SIR (O/E) | 95 % CI | Intervalb (years) | O | E | SIR (O/E) | 95 % CI |
|---|---|---|---|---|---|---|---|---|---|---|
| Small intestine (152) | <50 | 7 | 0.27 | 26.06 | (10.44, 53.71) | ≤5 | 6 | 0.23 | 25.95 | (9.48-56.49) |
| ≥50 | 5 | 1.15 | 4.34 | (1.40, 10.14) | ≤1 | 0 | 0.03 | 0 | NA | |
| 1-5 | 6 | 0.20 | 29.47 | (10.76-64.15) | ||||||
| 5-10 | 3 | 0.38 | 7.97 | (1.60-23.30) | ||||||
| ≥10 | 3 | 0.81 | 3.69 | (0.74-10.79) | ||||||
| Colorectum (153,154) | <50 | 36 | 9.68 | 3.72 | (2.60, 5.15) | ≤5 | 58 | 9.00 | 6.45 | (4.89-8.33) |
| ≥50 | 83 | 43.36 | 1.91 | (1.52, 2.37) | ≤1 | 12 | 1.07 | 11.25 | (5.81-19.66) | |
| 1-5 | 46 | 7.93 | 5.8 | (4.25-7.74) | ||||||
| 5-10 | 29 | 14.05 | 2.06 | (1.38-2.96) | ||||||
| ≥10 | 32 | 30.00 | 1.07 | (0.73-1.51) | ||||||
| Lung (162) | <50 | 13 | 6.24 | 2.08 | (1.11, 3.56) | ≤5 | 36 | 6.22 | 5.78 | (4.05-8.00) |
| ≥50 | 59 | 30.57 | 1.93 | (1.47, 2.49) | ≤1 | 7 | 0.74 | 9.42 | (3.77-19.40) | |
| 1-5 | 29 | 5.48 | 5.29 | (3.54-7.59) | ||||||
| 5-10 | 24 | 9.73 | 2.47 | (1.58-3.67) | ||||||
| ≥10 | 12 | 20.85 | 0.58 | (0.30-1.01) | ||||||
| Breast (174) | <50 | 34 | 29.38 | 1.16 | (0.80, 1.62) | ≤5 | 52 | 13.71 | 3.79 | (2.83-4.97) |
| ≥50 | 61 | 37.13 | 1.64 | (1.26, 2.11) | ≤1 | 12 | 1.40 | 8.56 | (4.42-14.96) | |
| 1-5 | 42 | 12.31 | 3.25 | (2.32-4.43) | ||||||
| 5-10 | 21 | 20.05 | 1.05 | (0.65-1.60) | ||||||
| ≥10 | 22 | 32.75 | 0.67 | (0.42-1.02) | ||||||
| Ovary (183) | <50 | 23 | 3.68 | 6.25 | (3.96, 9.38) | ≤5 | 37 | 1.84 | 20.12 | (14.16-27.73) |
| ≥50 | 17 | 5.97 | 2.85 | (1.66, 4.56) | ≤1 | 30 | 0.20 | 152.87 | (103.12-218.25) | |
| 1-5 | 7 | 1.64 | 4.26 | (1.71-8.78) | ||||||
| 5-10 | 1 | 2.78 | 0.36 | (0.00-2.00) | ||||||
| ≥10 | 2 | 5.03 | 0.40 | (0.04-1.44) | ||||||
| Vagina (184) | <50 | 6 | 0.38 | 15.68 | (5.73, 34.14) | ≤5 | 7 | 0.29 | 24.43 | (9.79-50.34) |
| ≥50 | 10 | 1.38 | 7.22 | (3.46, 13.29) | ≤1 | 6 | 0.04 | 172.12 | (62.85-374.65) | |
| 1-5 | 1 | 0.25 | 3.97 | (0.05-22.11) | ||||||
| 5-10 | 3 | 0.46 | 6.58 | (1.32-19.23) | ||||||
| ≥10 | 6 | 1.02 | 5.86 | (2.14-12.75) | ||||||
| Bladder (188) | <50 | 5 | 1.07 | 4.69 | (1.51, 10.95) | ≤5 | 7 | 1.22 | 5.74 | (2.30-11.82) |
| ≥50 | 13 | 6.72 | 1.93 | (1.03, 3.31) | ≤1 | 3 | 0.15 | 19.69 | (3.96-57.52) | |
| 1-5 | 4 | 1.07 | 3.75 | (1.01-9.59) | ||||||
| 5-10 | 4 | 1.99 | 2.01 | (0.54-5.14) | ||||||
| ≥10 | 7 | 4.58 | 1.53 | (0.61-3.15) | ||||||
| Kidney (189) | <50 | 4 | 1.68 | 2.38 | (0.64, 6.10) | ≤5 | 7 | 1.82 | 3.86 | (1.54-7.95) |
| ≥50 | 21 | 9.47 | 2.22 | (1.37, 3.39) | ≤1 | 6 | 0.22 | 27.70 | (10.12-60.30) | |
| 1-5 | 1 | 1.60 | 330.63 | (0.01-3.48) | ||||||
| 5-10 | 9 | 2.93 | 3.07 | (1.40-5.82) | ||||||
| ≥10 | 9 | 6.40 | 1.41 | (0.64-2.67) | ||||||
| Total | <50 | 128 | 52.37 | 2.44 | (2.04, 2.91) | ≤5 | 210 | 34.33 | 6.12 | (5.32,7.00) |
| ≥50 | 269 | 135.77 | 1.98 | (1.75, 2.23) | ≤1 | 76 | 3.84 | 19.80 | (15.60-24.75) | |
| 1-5 | 134 | 30.50 | 4.39 | (3.68-5.21) | ||||||
| 5-10 | 94 | 52.37 | 1.79 | (1.45, 2.20) | ||||||
| ≥10 | 93 | 101.45 | 0.92 | (0.74, 1.12 |
Bold indicates statistical significance
SIR standardized incidence ratio, SPM second primary malignancy, O observed numbers of SPMs, E expected numbers of SPMs, CI confidence interval
aAge at diagnosis of uterine cancer
bFollow-up interval after the diagnosis of uterine cancer
Risk of second primary malignancies stratified by follow-up interval
SIRs stratified according to the follow-up interval from the initial diagnosis of uterine cancer were examined for the eight sites with an elevated risk of SPM (Table 3, right half). The follow-up period was divided into 4 intervals: ≤1, 1–5, 5–10, and ≥10 years. Overall, SIR was found to markedly decrease over time. The increased risk of SPM at all selected sites was the greatest in the first year and diminished with time (SIR = 19.80, 4.39, 1.79, and 0.92 for ≤1, 1–5, 5–10, and ≥10 years follow-up, respectively, P < 0.001). Furthermore, an increased risk of breast, ovarian, and bladder SPM was observed in only the first 5 years, whereas an increased risk of small intestinal, colorectal, lung, and kidney SPM remained after up to 10 years of follow-up. The vagina/vulva was the only location with a markedly increased risk of SPM, lasting for ≥10 years of follow-up.
Cumulative incidence rates of all second cancers
The estimated overall risk of developing SPM in uterine cancer survivors was calculated, with death treated as a competing risk. For all SPMs, the cumulative risk in the younger group (<50 years) at 5, 10, 15, 20, and 25 years after uterine cancer was estimated to be 1.96 %, 3.85 %, 6.47 %, 9.15 %, and 13.24 %, respectively (Fig. 1). In contrast, the cumulative incidence was higher in older patients (≥50 years) than in younger patients (3.42 %, 6.42 %, 10.07 %, 12.84 %, and 20.51 % at 5, 10, 15, 20, and 25 years, respectively). A significant difference between the two cumulative incidence curves indicated that the risk of all SPMs differed between age groups (P < 0.001; Fig. 1).
Fig. 1.
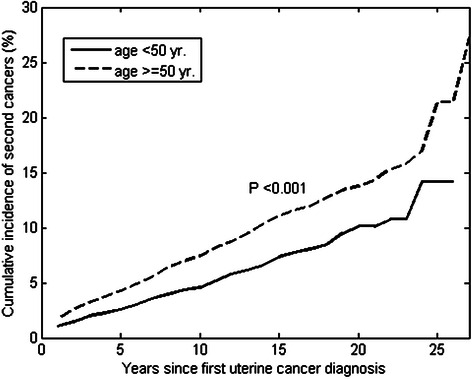
Cumulative incidence rates of all the second cancers after uterine cancer stratified by age
Overall survival and impact of second primary malignancies in patients with uterine cancer
The median overall survival was 25.08 years, and the five-year survival rate was 81 % (Fig. 2a). The patients diagnosed with uterine cancer at an age <50 years had a higher survival than those diagnosed at a later age (Fig. 2a, P < 0.001). For the 555 patients with SPMs, the median survival time after SPM diagnosis was 3.77 years (Fig. 2b), with 1–, 5–, 10–, and 15-year survival rates of 74 %, 47 %, 36 % and 28 %, respectively. Of these patients, the younger age group had a higher survival after diagnosis of any SPM (median survival time, 10.14 vs. 2.40 years; P < 0.001).
Fig. 2.
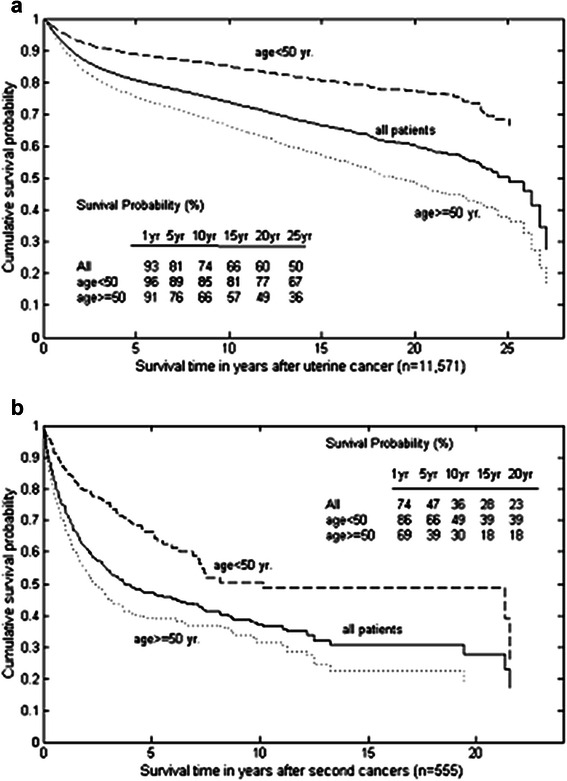
(a): Survival of all the patients with uterine cancer stratified by age at diagnosis of uterine cancer; (b): survival after second primary cancers stratified by age
The Cox model with a time-dependent covariate was employed for assessing the impact of SPMs on survival (Table 4). After adjusting for age at diagnosis of uterine cancer, we found that the SPM development was associated with a markedly increased risk of death (adjusted hazard ratio = 1.74, P < 0.001). This result suggests older patients (≥50 years) at initial uterine cancer diagnosis who subsequently develop SPM are at the highest risk of death.
Table 4.
Cox regression analysis of overall survival, with second cancer as a time-dependent covariate
| Hazard ratio | P-value | ||
|---|---|---|---|
| Age diagnosis age <50 | 1 | <0.001 | |
| ≥50 | 2.457 | ||
| Second cancers without | 1 | <0.001 | |
| with | 1.771 | ||
Discussion
Patients in the present study had a median overall survival of 25.08 years, consistent with the reported survival of patients in the SEER database. In our study, patients with SPMs had a median survival of 3.77 years following SPM diagnosis, and the average interval between the first and second cancers was 6.27 years (SD = 5.53 years). The highest risk of developing SPM was observed in the first 5 years after diagnosis of uterine cancer, largely because of an extremely increased risk in the first year (Table 3). The close follow-up during the first year following the diagnosis may have contributed to an earlier detection of second malignancies, leading to a surveillance bias. Moreover, recommendations regarding screening should consider this observed latency pattern. Screening and preventive strategies for SPMs are essential for reducing mortality rates. However, no universal guidelines for SPM surveillance in patients with uterine cancer have been established to date. A major obstacle has been contradictory results from studies examining SPMs. For example, a nationwide Swedish population-based study reported a 54 % increased risk for all SPMs (SIR = 1.54; 95 % CI, 1.48–1.61) in 19,128 patients with primary endometrial cancer, revealing an increased risk of subsequent malignancy at 11 sites, including the ovary, urinary bladder, small intestine, connective tissue, colon or rectum, female genitalia, kidney, skin (squamous cell), breast, and bone marrow (particularly, leukemia). However, the strong decline in SPM development with the length of follow-up found in our study was not observed in the Swedish data [13]. A complete evaluation of the US SEER data revealed no increase in the overall risk of SPMs (SIR = 0.99, excluding female genital sites; 95 % CI, 0.97–1.01). However, our study corroborated findings of the SEER database regarding the association between age at onset and risk of SPM. Further, despite SIRs being generally lower in the SEER database than those reported in Taiwan, the same SPM sites were found to have increased SIRs [19]. Another study using the SEER database also found no overall increased risk of SPMs (SIR = 0.85; 95 % CI, 0.84–0.87) and reported no increased risk of breast, ovarian, or colorectal SPM [18]. In our study, there was a 71 % increased risk of SPM following uterine cancer (SIR = 1.71; 95 % CI, 1.57–1.86), with a higher risk of small intestinal, colorectal, ovarian, vaginal/vulvar, breast, urinary bladder, kidney, and lung cancers. In general, treatments for uterine cancer in Taiwan are similar to those used in Western countries, particularly the US, as Taiwanese clinicians generally follow American guidelines. Hence, the discrepancies in results in this study and those using the US SEER data may be because of follow-up time, surveillance bias, and methodology rather than differences in treatment regimes. First, the follow-up period in our study (69,987 person-years) was shorter than that in the US (705,002 person-years) and Swedish (255,211 person-years) studies [13, 19]. Second, a close follow-up in the first 5 years, particularly the first year, may have contributed to an earlier detection of SPM and lead to surveillance bias. Last, differences may have been because of the study methodology rather than intrinsic differences between the two countries. For example, the influence of migration on Taiwan is minimal compared with that on the US. The population in Taiwan is relatively stable, and mostly, Taiwanese emigrants return to Taiwan for medical treatments as the National Health Insurance Plan in Taiwan provides great medical care at a lower cost.
The mechanisms underlying SPM development are unclear; however, an association between hereditary factors, common environmental risk factors, and effects of treatment modalities between the first and second malignancy may be responsible. In the present study, the risk of SPMs in the small intestine, colon or rectum, ovary, and urinary bladder was found to be higher in patients with a younger age (<50 years) at the initial diagnosis of uterine cancer, suggesting an underlying genetic association. The discovery of metachronous cancers in a young patient suggests a hereditary cause. The most well-known example is LS, an autosomal dominant disease caused by germ-line mutations in DNA mismatch repair genes [27, 28]. LS is associated with an increased risk of colorectal, endometrial, and ovarian cancers, with the risk of endometrial cancer equaling or exceeding that of colorectal cancer. Diagnosis of gynecological cancer precedes colorectal cancer in over half of the women with LS. It has been recently reported that women with LS diagnosed with a primary endometrial cancer have an increased risk of SPMs, including colorectal, kidney, renal pelvic, ureteral, urinary bladder, ovarian, and breast cancers [29, 30]. In addition to LS, patients with genetic polymorphisms in DNA repair enzyme genes, such as ERCC1 and XPF, have also been reported to be at an increased risk of developing multiple cancers [31, 32].
The incidence of estrogen-related cancers, including that of the breast and ovary and endometrial carcinomas of the uterus, is rapidly increasing in Taiwan [4]. Although the underlying mechanisms remain unelucidated, they are believed to involve a complex association between genetic, endocrinal, and environmental factors. Xenoestrogens are widely dispersed into the environment because of increasing industrialization. Marked exposure levels of nonylphenol, ubiquitously found in water supplies and food, and bisphenol A, found in considerable amounts in polycarbonate plastics, can be detected in the Taiwanese population. The average daily intake of nonylphenol in Taiwan has been reported to be 4–and 8.5-folds higher than that in Germany and New Zealand, respectively [33]. These organic compounds, which have estrogenic effects and can cause precocious puberty and early menarche [34], resulting in an increased cumulative life-long exposure to estrogen, have been implicated in carcinogenesis [35].
Regarding SPM sites, we found that the organs within and closer to irradiated fields (vagina/vulva, small intestine, ovary, kidney, bladder, ureter, and colorectum) were at a higher risk of SPM than those not directly exposed to radiation (lung and breast). Pelvic radiotherapy for endometrial cancer is associated with a marked increase in the risk of SPM in the urinary system (kidney, ureter, bladder, and urethra), colon and rectum, vagina/vulva, sarcoma, breast, and lung [14, 16]. Radiation has also been reported to induce local immunosuppression which may activate high-risk human papillomavirus infection and increase the risk of vaginal and vulvar cancer [36, 37]. Beyond the radiation field, radiotherapy may increase the risk of lung and breast cancers through the bystander effect, in which the non-exposed cells receive signals from irradiated cells (radiation-induced genomic instability) and confer predisposition to malignancy [38]. We found that the risk of developing these SPMs was the highest within the first five years after diagnosis of uterine cancer. Considering the long latency required for carcinogenesis, the higher risk of SPMs occurring within a short period after the first cancer contradicts the hypothesis that radiotherapy is the sole SPM initiator. Factors other than radiotherapy, such as heritable factors, may influence the risk of SPM. Further, a higher than expected incidence of the second cancer, strongly associating with radiation and occurring in relatively short latency periods, has been reported in numerous studies about uterine corpus cancer [13, 16, 19]. However, this was not observed in our study.
The major limitation of this study is the lack of information regarding potential confounders. For example, data on the received treatments, staging at initial diagnosis, and treatment-related complications were not included. Information regarding bilateral oophorectomy is known to influence the estimated risk of second ovarian cancer, particularly in young patients with early stage diseases who may have undergone hysterectomy with ovary preservation or those who may undergo hysterectomy without oophorectomy for presumed uterine myoma or adenomyosis prior a histological diagnosis of malignancy. Hence, the calculated SIR of second ovarian cancer may have been underestimated. Moreover, SIRs in the first follow-up year were extremely high for second ovarian and vaginal/vulvar cancers (SIR = 152.87; 95 % CI, 103.12–218.25 and SIR = 172.12; 95 % CI, 62.85–374.65, respectively Table 3). This may have been because of a high prevalence of synchronous malignancies involving anatomically related organs as 22 of 30 s ovarian and 4 of 6 s vaginal/vulvar cancers occurred within 6 months of diagnosis of uterine cancer.
Conclusions
The present study suggests the higher incidence of SPM in women previously diagnosed with uterine cancer may be because of genetic, environmental, and therapy-related factors. The overall risks and patterns of SPMs in Taiwan differ from those reported in the United States suggesting the relative influence of each factor differs according to the patient demographics, study methodology, and follow-up period. Therefore, surveillance guidelines for SPMs should be developed using data specific to local populations.
Acknowledgments
We are grateful to the staff of the Taiwan Cancer Registry, Health Promotion Administration, Ministry of Health and Welfare, Taiwan. This work was supported by grant NSC 102-2314-B-182-062-MY2 from the National Science Council, Taiwan and grant CMRPD1C0051-53 from Chang Gung Memorial Hospital, Linkou, Taiwan.
Abbreviations
- CI
Confidence interval
- E
Expected number
- IACR
International Association of Cancer Registries
- IARC
International Agency for Research on Cancer
- ICD-9
International Classification of Diseases, 9th Revision
- O
Observed number
- LS
Lynch syndrome
- SEER
Surveillance, Epidemiology, and End Results
- SIR
Standardized incidence ratio
- SPM
Second primary malignancy
- TCR
Taiwan Cancer Registry
Footnotes
Kuan-Der Lee and Chao-Yu Chen contributed equally to this work.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors (ICMJE), were completely responsible for all content and editorial decisions, retained a full control over all content contained in this manuscript, and were involved with all stages of manuscript development. KD and MC were involved in the study concept and design. Moreover, KD, CY, and MC drafted the manuscript. SH and MC performed the statistical analysis. CH provided critical revisions of the manuscript for important intellectual content. HJ, TY, and DT were involved in the drafting, intellectual input and final approval of the manuscript.
Contributor Information
Kuan-Der Lee, Email: kdlee@cgmh.org.tw.
Chao-Yu Chen, Email: b9002031@adm.cgmh.org.tw.
Huei-Jean Huang, Email: hueijean.huang@gmail.com.
Ting-Yao Wang, Email: tywang.onco@gmail.com.
David Teng, Email: david.d.teng@gmail.com.
Shih-Hao Huang, Email: shi.hao@msa.hinet.net.
Chyong-Huey Lai, Phone: 886-3-3281200, Email: sh46erry@ms6.hinet.net.
Min-Chi Chen, Phone: 886-3-2118800, Email: mcc@mail.cgu.edu.tw.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Duncan ME, Seagroatt V, Goldacre MJ. Cancer of the body of the uterus: trends in mortality and incidence in England, 1985-2008. BJOG. 2012;119:333–9. doi: 10.1111/j.1471-0528.2011.03201.x. [DOI] [PubMed] [Google Scholar]
- 3.Sorosky JI. Endometrial cancer. Obstet Gynecol. 2012;120:383–97. doi: 10.1097/AOG.0b013e3182605bf1. [DOI] [PubMed] [Google Scholar]
- 4.Lin CH, Chen YC, Chiang CJ, Lu YS, Kuo KT, Huang CS, et al. The emerging epidemic of estrogen-related cancers in young women in a developing Asian country. Int J Cancer. 2012;130:2629–37. doi: 10.1002/ijc.26249. [DOI] [PubMed] [Google Scholar]
- 5.Ushijima K. Current status of gynecologic cancer in Japan. J Gynecol Oncol. 2009;20:67–71. doi: 10.3802/jgo.2009.20.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cancer Registry Annual Report, 1996 Taiwan: Department of Health, Executive Yuan 1996. (http://www.hpa.gov.tw/BHPNet/Web/Stat/Statistics.aspx).
- 7.Cancer Registry Annual Report, 2010 Taiwan: Department of Health, Executive Yuan 2012. (http://www.hpa.gov.tw/BHPNet/Web/Stat/Statistics.aspx).
- 8.Lee KD, Chen SC, Chan CH, Lu CH, Chen CC, Lin JT, et al. Increased risk for second primary malignancies in women with breast cancer diagnosed at young age: a population-based study in Taiwan. Cancer Epidemiol Biomarkers Prev. 2008;17:2647–55. doi: 10.1158/1055-9965.EPI-08-0109. [DOI] [PubMed] [Google Scholar]
- 9.Kosary CL. Cancer of the corpus uteri. In: Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD, Horner M-J, editors. SEER survival monograph: cancer survival among adults: U.S. SEER program, 1998–2001, patient and tumor characteristics. Bethesda, MD: National Cancer Institute, SEER Program; 2007. pp. 123–32. [Google Scholar]
- 10.Huang CY, Chen CA, Chen YL, Chiang CJ, Hsu TH, Lin MC, et al. Nationwide surveillance in uterine cancer: survival analysis and the importance of birth cohort: 30-year population-based registry in Taiwan. PLoS One. 2012;7:e51372. doi: 10.1371/journal.pone.0051372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Annegers JF, Malkasian GD., Jr Patterns of other neoplasia in patients with endometrial carcinoma. Cancer. 1981;48:856–9. doi: 10.1002/1097-0142(19810801)48:3<856::AID-CNCR2820480332>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 12.Re A, Taylor TH, DiSaia PJ, Anton-Culver H. Risk for breast and colorectal cancers subsequent to cancer of the endometrium in a population-based case series. Gynecol Oncol. 1997;66:255–7. doi: 10.1006/gyno.1997.4766. [DOI] [PubMed] [Google Scholar]
- 13.Hemminki K, Aaltonen L, Li X. Subsequent primary malignancies after endometrial carcinoma and ovarian carcinoma. Cancer. 2003;97:2432–9. doi: 10.1002/cncr.11372. [DOI] [PubMed] [Google Scholar]
- 14.Kumar S, Shah JP, Bryant CS, Awonuga AO, Imudia AN, Ruterbusch JJ, et al. Second neoplasms in survivors of endometrial cancer: impact of radiation therapy. Gynecol Oncol. 2009;113:233–9. doi: 10.1016/j.ygyno.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 15.Zwahlen DR, Ruben JD, Jones P, Gagliardi F, Millar JL, Schneider U. Effect of intensity-modulated pelvic radiotherapy on second cancer risk in the postoperative treatment of endometrial and cervical cancer. Int J Radiat Oncol Biol Phys. 2009;74:539–45. doi: 10.1016/j.ijrobp.2009.01.051. [DOI] [PubMed] [Google Scholar]
- 16.Lonn S, Gilbert ES, Ron E, Smith SA, Stovall M, Curtis RE. Comparison of second cancer risks from brachytherapy and external beam therapy after uterine corpus cancer. Cancer Epidemiol Biomarkers Prev. 2010;19:464–74. doi: 10.1158/1055-9965.EPI-09-0892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uccella S, Cha SS, Melton LJ, 3rd, Bergstralh EJ, Boardman LA, Keeney GL, et al. Risk factors for developing multiple malignancies in patients with endometrial cancer. Int J Gynecol Cancer. 2011;21:896–901. doi: 10.1097/IGC.0b013e318219711f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Felix AS, Linkov F, Maxwell GL, Ragin C, Taioli E. Racial disparities in risk of second primary cancers in endometrial cancer patients: Analysis of SEER Data. Int J Gynecol Cancer. 2011;21:309–15. doi: 10.1097/IGC.0b013e31821a62dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK, et al. New malignancies among cancer survivors: SEER cancer registries, 1973-2000. Bethesda MD: National Cancer Institute, NIH Publ. No. 05-5302; 2006. [Google Scholar]
- 20.Slee VN. The International Classification of Diseases: ninth revision (ICD-9) Ann Intern Med. 1978;88:424–6. doi: 10.7326/0003-4819-88-3-424. [DOI] [PubMed] [Google Scholar]
- 21.Parkin DM. CS: Cancer incidence in five continents. Lyon: IARC Sci Publ, Electronic Publication; 1997. p. 7. [Google Scholar]
- 22.IARC/ENCR/IACR Working Group International rules for multiple primary cancers. Asian Pacific J Cancer Prev. 2005;6:104–6. [PubMed] [Google Scholar]
- 23.International Agency for Research on Cancer . International Rules for Multiple Primary Cancers (ICD-O Third Edition). Internal Report No. 2004/02. Lyon: IARC; 2004. [Google Scholar]
- 24.Breslow NE, Day NE. Statistical methods in cancer research. Volume II--The design and analysis of cohort studies. IARC Sci Publ 1987. [PubMed]
- 25.Cox D. Regression models and life tables. J Roy Stat Soc Ser. 1972;34:187–220. [Google Scholar]
- 26.Cox D. Partial likelihood. Biometrika. 1975;62:269–76. doi: 10.1093/biomet/62.2.269. [DOI] [Google Scholar]
- 27.Vasen HF, Watson P, Mecklin JP, Lynch HT. New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology. 1999;116:1453–6. doi: 10.1016/S0016-5085(99)70510-X. [DOI] [PubMed] [Google Scholar]
- 28.Lu KH, Dinh M, Kohlmann W, Watson P, Green J, Syngal S, et al. Gynecologic cancer as a “sentinel cancer” for women with hereditary nonpolyposis colorectal cancer syndrome. Obstet Gynecol. 2005;105:569–74. doi: 10.1097/01.AOG.0000154885.44002.ae. [DOI] [PubMed] [Google Scholar]
- 29.Win AK, Lindor NM, Winship I, Tucker KM, Buchanan DD, Young JP, et al. Risks of colorectal and other cancers after endometrial cancer for women with Lynch syndrome. J Natl Cancer Inst. 2013;105:274–9. doi: 10.1093/jnci/djs525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crispens MA. Endometrial and ovarian cancer in lynch syndrome. Clin Colon Rectal Surg. 2012;25:97–102. doi: 10.1055/s-0032-1313780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He J, Xu Y, Qiu LX, Li J, Zhou XY, Sun MH, et al. Polymorphisms in ERCC1 and XPF genes and risk of gastric cancer in an eastern Chinese population. PLoS One. 2012;7 doi: 10.1371/journal.pone.0049308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crew KD, Gammon MD, Terry MB, Zhang FF, Zablotska LB, Agrawal M, et al. Polymorphisms in nucleotide excision repair genes, polycyclic aromatic hydrocarbon-DNA adducts, and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2007;16:2033–41. doi: 10.1158/1055-9965.EPI-07-0096. [DOI] [PubMed] [Google Scholar]
- 33.Lu YY, Chen ML, Sung FC, Wang PS, Mao IF. Daily intake of 4-nonylphenol in Taiwanese. Environ Int. 2007;33:903–10. doi: 10.1016/j.envint.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 34.Ozen S, Darcan S. Effects of environmental endocrine disruptors on pubertal development. J Clin Res Pediatr Endocrinol. 2011;3:1–6. doi: 10.4274/jcrpe.v3i1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernandez SV, Russo J. Estrogen and xenoestrogens in breast cancer. Toxicol Pathol. 2010;38:110–22. doi: 10.1177/0192623309354108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fujimura M, Ostrow RS, Okagaki T. Implication of human papillomavirus in postirradiation dysplasia. Cancer. 1991;68:2181–5. doi: 10.1002/1097-0142(19911115)68:10<2181::AID-CNCR2820681016>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 37.Barzon L, Pizzighella S, Corti L, Mengoli C, Palu G. Vaginal dysplastic lesions in women with hysterectomy and receiving radiotherapy are linked to high-risk human papillomavirus. J Med Virol. 2002;67:401–5. doi: 10.1002/jmv.10077. [DOI] [PubMed] [Google Scholar]
- 38.Lorimore SA, Coates PJ, Wright EG. Radiation-induced genomic instability and bystander effects: inter-related nontargeted effects of exposure to ionizing radiation. Oncogene. 2003;22:7058–69. doi: 10.1038/sj.onc.1207044. [DOI] [PubMed] [Google Scholar]


