Abstract
Background
Surgical education remains an important mission of academic medical centers. Financial pressures, however, may favor improved operating room (OR) efficiency at the expense of surgical education. We aim to characterize resident impact on the duration of procedural time using common pediatric otolaryngologic cases which do not necessitate a surgical assistant and assess whether other factors modify the extent to which residents impact OR efficiency.
Study Design
We retrospectively reviewed resident and attending surgeon total OR and procedural times for isolated tonsillectomy, adenoidectomy, tonsillectomy with adenoidectomy (T&A) and bilateral myringotomy with tube insertion between 2009 and 2013. We included cases supervised or performed by one of four teaching surgeons in children with ASA < 3. Regression analyses were used to identify predictors of procedural time.
Results
We identified a total of 3,922 procedures. Residents had significantly longer procedure times for all four procedures compared to an attending surgeon (range: 4.9 to 12.8 minutes, p<0.001). These differences were proportional to case complexity. When comparing mean procedural times, similar differences between the resident surgeon and attending surgeon cohorts were appreciated (p<0.0001). In T&A patients, older patient age, and attending surgeon identity were also significant predictors of increased mean procedural time (p<0.05).
Conclusions
Resident participation contributes to increased procedure time for common otolaryngology procedures. While residents may increase operative times, addressing other system-wide issues may decrease impact of time needed for education and added efficiencies of resident participation may exist throughout the perioperative period. Our model is applicable to surgical education across specialties.
Level of Evidence
4
Keywords: residency education, training, procedure length, operative time, cost
Introduction
The United States has witnessed a tremendous rise in health care costs over the past several decades.1 Increases in operating room (OR) costs, in particular, have risen with the advent of operative techniques requiring the use of expensive technologies and more skilled surgical support staff.2 Not surprisingly, hospital administrators and health care payors have begun to critically assess health care workflow to identify potential inefficiencies and reduce costs. The Patient Protection and Affordable Care Act will further increase pressure to reduce costs through “bundling” of reimbursements for a patient's entire operative course, including pre- and post-operative care, as well as measures such as pay-for-performance which prescribes compensation based on outcomes and penalize for complications.3
Alongside these changes in health policy and the increased emphasis on cost reduction and efficiency, surgical residency training has undergone a substantial transformation. Recent changes, including the implementation of the 80-hour work week, institution of Accreditation Council for Graduate Medical Education (ACGME) core competencies, and most recently the institution of the Next Accreditation System, which includes the development of the Milestones project, which aims to provide more objective measurements throughout the course of residency training.4 Despite these changes, the intra-operative one-on-one mentor-apprentice model remains at the core of surgical training, facilitating the acquisition of technical skills needed to safely and effectively operate.5
Critical teaching time in the OR, however, is arguably in direct conflict with the growing emphasis on improving OR efficiency and cost reduction. Surgical simulation and cadaveric dissection have been used as potential solutions to training time lost in the operating room and as a way to augment technical instruction.6,7 Ultimately, trainees must gain experience in the OR working with real patients to prepare for the multifactorial stresses and challenges of an operative procedure they will be required to perform independently after completing residency. Thus, quantifying and identifying the impact of resident training on OR efficiency is important to understanding and potentially addressing divergent financial and educational goals of the current health care system.
Only a handful of studies have directly examined the “cost” of intra-operative resident education. For example, one study examining operative times for four distinct general surgery cases including laparoscopic cholecystectomy, hernia repair, colectomy, and carotid endarterectomy found that residents significantly increased total operating room time for these procedures.8 Similarly, literature from the fields of ophthalmology and otolaryngology literature suggests that residents increase operating room time for cataract surgery and a variety of otolaryngology procedures.9,10 Analogous work has been carried out in orthopedic, cardiothoracic, and transplant surgery.11-15 However, these studies are limited by their design: many were carried out in variable hospital systems, had the involvement of numerous attending surgeons, or had limited sample size. In addition, nearly all these studies include procedures that necessitate a surgical assistant, risking the introduction of confounders due to the ill-defined role of resident surgeons. Past studies also assessed total operating room time, rather than procedure time; however, operating room time is dependent on more than just the presence of a resident – it is influenced by multiple factors including ancillary staff efficiency and anesthesiology care. Finally, none of these studies used regression analysis to compare the potential inefficiency introduced by resident participation compared to other patient and non-patient related factors.
To build upon previous literature and to address these limitations, we retrospectively reviewed the entire case log of the Massachusetts Eye and Ear Infirmary (MEEI) from 2009 to 2013, focusing on four common, isolated pediatric otolaryngology procedures (tonsillectomy alone, adenoidectomy alone, tonsillectomy with adenoidectomy (T&A), and bilateral myringotomy with tympanostomy tube insertion). These procedures were supervised by one of four teaching surgeons. We focused our analyses on these common pediatric otolaryngology procedures because these cases do not require a surgical assistant. Thus, in contrast to past work, our study offers a highly controlled environment in which to characterize the impact of resident involvement on operative times. By focusing on thousands of cases at a single institution with a small group of attendings and choosing procedures that are relatively simple and completed solely by the resident surgeon, we have modeled the impact of residents on procedure times. We also perform a multivariable regression analysis to identify additional factors that influence operative times. Together, our study builds upon previous studies, offers a refined model of investigation into the impact of resident involvement on operative times, and provides insight into surgical education across specialties.
Methods
The Massachusetts Eye and Ear Infirmary (MEEI) operating room log was queried for patients who underwent isolated cases of tonsillectomy alone, adenoidectomy alone, tonsillectomy and adenoidectomy (T&A), or bilateral myringotomy with tympanostomy tube placement between January 2009 and December 2013. Cases supervised or performed by one of four academic surgeons, patient age ≤ 18 years old, and American Society of Anesthesiology (ASA) classification of less than three.
Cases were grouped by procedure type and by primary operator (resident surgeon versus attending surgeon). A case was designated as a resident surgeon procedure if a resident at MEEI was listed as the primary operator, while cases with an attending listed as the primary surgeon were placed in the attending surgeon cohort. These cases are typically performed at the PGY2 level during a dedicated 12-week pediatric otolaryngology rotation at our institution. All four attending surgeons included in this analysis had an academic appointment at MEEI and each regularly taught residents.
Descriptive analyses were performed to characterize patient demographics (age, gender, ASA class), indication for procedure, and operative times including total OR time and procedure time (defined as the time from when the surgeon begins the procedure to when the surgeon declares the procedure to be complete; excludes induction of anesthesia, patient positioning and prepping, and extubation time). Patient demographics, case characteristics, and operative times were compared between resident and attending surgeons for each of the four procedures to ensure that other factors intrinsic to the patient population or the procedure were not contributing to potential differences between attending and resident surgeon operative times. Means were compared by student's t-test and proportions compared by chi-square test.
A multivariable linear regression analysis was performed to determine the contribution of a resident surgeon to procedural time for T&A while adjusting for patient demographics and other case characteristics. All independent variables listed previously were included in a complete case analysis. Surgeon identity was used as a proxy for all fixed effects associated with difference in surgeon volume. Statistical analyses were performed with STATA v.13 (StataCorp LP, College Station, TX). This study was granted institutional review board approval by the Massachusetts Eye and Ear Infirmary Human Studies Committee.
Results
Operative procedure distribution
A total of 9,574 cases were reviewed and 3,922 met the inclusion criteria, consisting of tonsillectomy alone (n = 264), adenoidectomy alone (n = 446), T&A (n = 1,741), and bilateral myringotomy with tympanostomy tube placement (n = 1,471) (Table 1). Residents performed 41.7% of cases (n = 1,636) as primary operator, while 58.3% (n = 2,286) had an attending as the primary surgeon (Table 1).
Table 1. Case characteristics.
| All Patients (N=3,922) | |
|---|---|
| Attending | |
| A | 1,324 (33.8) |
| B | 1,427 (36.4) |
| C | 662 (16.9) |
| D | 509 (13.0) |
| Primary operator | |
| Resident | 1,636 (41.7) |
| Attending | 2,286 (58.3) |
| Procedure | |
| Tonsillectomy and adenoidectomy | 1,741 (44.4) |
| Tonsillectomy alone | 264 (6.7) |
| Adenoidectomy alone | 446 (11.4) |
| Bilateral tympanostomy tube placement under general anesthesia | 1,471 (37.5) |
Patient characteristics and indication for the procedure
We first examined cases of T&A, initially comparing the mean age of the patients. Mean age was similar in the AS and RS cohorts (6.3 years old vs. 6.1 years old, respectively, p = 0.27) (Table 2a, online supplement). Gender ratios were also similar with 51.8% male patients in the AS cohort compared to 53.4% in the RS group (p = 0.52) (Table 2a, online supplement). We limited our analyses to patients with ASA < 3, and accordingly, the distribution of ASA class 1 or 2 patients was similar in both cohorts (25.7% ASA I and 74.3% ASA II for the AS group vs. 22.6% ASA I and 77.4% ASA II for the RS cohort, p = 0.13) (Table 2a, online supplement). Indications for surgery including adenotonsillar hypertrophy, obstructive sleep apnea (OSA), infection, and other indications were similarly distributed among the AS and RS groups (p = 0.448) (Table 2a, online supplement). Similar analyses carried out in cases of isolated tonsillectomy as well as adenoidectomy alone revealed similar results, with no differences in mean age, gender ratio, or ASA classification (Table 3a-4a, online supplement). There was no statistically significant distribution in the indication for tonsillectomy alone when comparing the AS and RS groups (Table 3a, online supplement); however, for isolated adenoidectomy, the RS cohort had lower proportion of surgeries that were indicated for adenoid hypertrophy and a higher proportion of cases indicated for obstructive sleep apnea, infection, nasal/sinus disease, and other indications (Table 4a, online supplement).
Table 2.
Mean total operating room times by procedure for attending surgeons and resident surgeon. Difference = resident surgeon time minus attending surgeon time. Two-sided p-value denotes level of significance between attending surgeon and resident surgeon.
| Total OR Time, Mean (SD), Minutes | |||||
|---|---|---|---|---|---|
| Procedure | Total Patients | Attending Surgeon | Resident Surgeon | Difference (mins) | P-value |
| Tonsillectomy and adenoidectomy | 1,741 | 40.4 (13.2) | 53.2 (15.3) | + 12.8 | <0.0001 |
| Tonsillectomy alone | 264 | 41.5 (13.4) | 52.0 (14.6) | + 10.5 | <0.0001 |
| Adenoidectomy alone | 446 | 38.5 (15.5) | 44.4 (20.3) | + 5.9 | 0.0005 |
| Bilateral tympanostomy tubes | 1,471 | 16.7 (6.3) | 21.6 (9.4) | + 4.9 | <0.0001 |
Table 3.
Mean procedure times by procedure for attending surgeons and resident surgeon. Difference = resident surgeon time minus attending surgeon time. Two-sided p-value denotes level of significance between attending surgeon and resident surgeon.
| Mean Surgical Time (SD), Minutes | |||||
|---|---|---|---|---|---|
| Procedure | Total Patients | Attending Surgeon | Resident Surgeon | Difference (mins) | P-value |
| Tonsillectomy and adenoidectomy | 1,741 | 15.5 (10.4) | 27.3 (12.4) | + 11.8 | <0.0001 |
| Tonsillectomy alone | 264 | 15.0 (9.5) | 23.9 (10.7) | + 8.9 | <0.0001 |
| Adenoidectomy alone | 446 | 11.4 (11.5) | 16.6 (9.6) | + 5.2 | <0.0001 |
| Bilateral tympanostomy tubes | 1,471 | 6.9 (4.5) | 10.8 (5.7) | + 3.9 | <0.0001 |
Table 4.
Multivariable analysis predicting outcome of mean procedural time for T&A cases.
| Variable | Coefficient | Standard Error | P-Value |
|---|---|---|---|
| Age (per 1 year increase) | +0.4 | 0.1 | <0.0001 |
| Male (vs. female) | +0.4 | 0.5 | 0.428 |
| Race | 0.9187 | ||
| White | REF | ||
| Black | +0.2 | 1.3 | 0.883 |
| Other/unknown | +0.2 | 0.5 | 0.688 |
| ASA (II vs. I) | -0.4 | 0.6 | 0.516 |
| Indication | 0.2147 | ||
| Tissue hypertrophy | REF | ||
| OSA | +0.5 | 0.6 | 0.436 |
| Infection | -0.2 | 0.9 | 0.818 |
| Other | +4.1 | 2.1 | 0.049 |
| Year | 0.0879 | ||
| 2009 | REF | ||
| 2010 | -1.5 | 0.7 | 0.032 |
| 2011 | +0.1 | 0.8 | 0.933 |
| 2012 | +0.4 | 0.8 | 0.608 |
| 2013 | -0.2 | 0.8 | 0.767 |
| Day of week | <0.0001 | ||
| Monday | -0.2 | 1.2 | 0.891 |
| Tuesday | +2.4 | 0.9 | 0.009 |
| Wednesday | +2.9 | 1.0 | 0.003 |
| Thursday | +0.4 | 0.9 | 0.648 |
| Friday | REF | ||
| Case start time | 0.3735 | ||
| 6am-9am | REF | ||
| 9am-12pm | +0.5 | 0.5 | 0.387 |
| 12pm-3pm | -0.8 | 1.1 | 0.445 |
| 3pm to 6pm | +5.4 | 4.8 | 0.269 |
| Resident surgeon (vs. attending surgeon) | +11.1 | 0.5 | <0.0001 |
| Attending surgeon identity | -- | -- | <0.0001 |
We compared patient characteristics and procedural indications for cases of bilateral myringotomy with tympanostomy tube placement. Differences in mean age in the AS and RS cohorts were highly significant, although absolute differences were small (8.9 years old for AS group compared to 7.9 years old for the RS cohort, p = 0.0009) (Table 5a, online supplement). The gender ratio was similar in both groups, with 59.1% males in the AS cohort compared to 63.4% for the RS group (p = 0.105) (Table 5a, online supplement). ASA classification tended towards a greater proportion of ASA class I cases in the AS group with 74.5% ASA I and 25.5% ASA II compared to 66.0% ASA I and 34.0% ASA II in the RS group (p = 0.001) (Table 5a, online supplement). The indications for surgery, including infection, Eustachian tube dysfunction, and other indications, were similarly distributed between both the AS and RS cohorts (p = 0.621) (Table 5a, online supplement). Thus, with few exceptions, patient characteristics and indications for a procedure were similarly distributed among the AS and RS cohorts.
Table 5. Previous studies evaluating “cost” of resident participation in the operating room.
| Study | Speciality | Procedures | Study Design | Sample size (n) | # of instuttions | # of Attendings | Difference in resident vs. attending (percent difference) | Cost |
|---|---|---|---|---|---|---|---|---|
| Babineau (2004) | General Surgery | Hernia repair, lap cholecystectomy, carotid endarterectomy | RA vs. AA | unknown | 1 | 4 | 8 to 60 (21 to 52%) | $5-20 / min |
| Bridges (1999) | Multiple | 62 different procedures (general, pediatric, vascular, plastic, urology, trauma) | RA vs. None | 14,452 | 1 | >50 | -32 to 88 min (-17 to 88%) | $4 / min |
| Farnworth (2001) | Orthopedic Surgery | Athroscopic ACL reconstruction | RS. vs. AS | 53 | 1 | 20 | 62 min (49%) | $16 / min |
| Hosler (2012) | Optholmology | Cataract surgery | RA vs. RS vs. AS | 947 | 1 | 4 | 13 min (46%) | $8 / min |
| Hwang (2010) | General Surgery | Bowel resection, lap cholecystectomy, hernia repair (exlucluding inguninal, femorla, umbilicial hernias), mastectomy, appendectomy | RA vs. None | 2,723 | 1 | 8 | 15 to 33 min (24 to 31%) | $25 / min |
| Papadria (2012) | General Surgery | lap appendectomy, lap cholecystectomy, open inguinal hernia | RA vs. None | 115,535 | 1,574 (ACS-NQSIP participants) | Unknown | 12 to 20 min (30 to 33%) | N/A |
| Pollei (2013) | Otolaryngology | cricopharyngeal myotomy, tonsillectomy, parotidectomy, septoplasty, tympanomastoidectomy, thyroidectomy | RS vs. AS | 642 | 1 | 3 | 12 to 20 min (30 to 33%) | $42 / min |
| Puram (2013) | Otolaryngollgy | tonsillectomy, adenoidectomy, tonsillectomy and adenoidectomy, bilateral myringotomy with tympanostomy tube placement | RS vs. AS | 3,922 | 1 | 4 | 5 to 13 min (46 to 76%) | N/A |
| von Strauss (2012) | General Surgery | Lab cholecystectomy | RS vs. AS | 9,045 | 46 | Unknown | 24 min (43%) | $23 / min |
RA = resident assistant; RS = resident surgeon; AA = attending assistant; AS = attending surgeon; min = minutes.
Mean total operating room time and procedural time
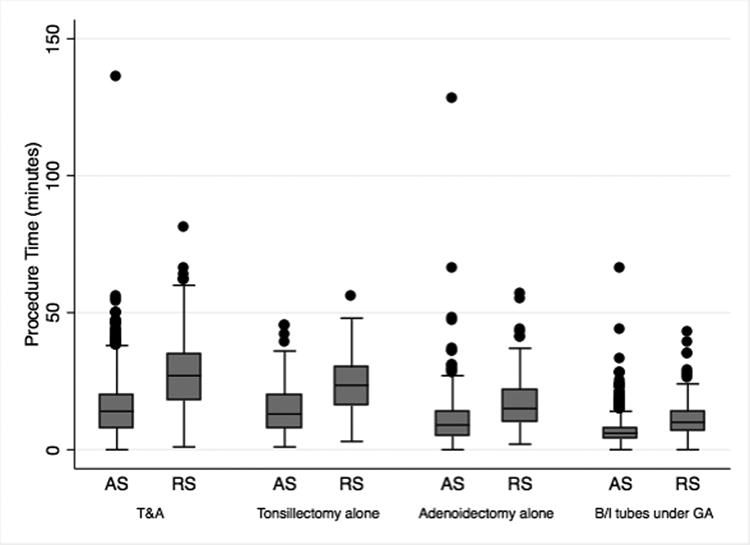
Total OR times were significantly longer for RS as compared to AS for all procedures (Table 2). When comparing the AS and RS cohorts, differences in total OR time were highly significant, with residents adding 12.8 min for T&A, 10.5 min for tonsillectomy alone, 5.9 min for adenoidectomy alone, and 4.9 min for bilateral tympanostomy tube placement (p < 0.001) (Table 2). To determine whether resident surgeons operated more slowly than attendings, we also specifically compared procedure times for T&A, tonsillectomy alone, adenoidectomy alone, and bilateral tympanostomy tube placement. These analyses revealed similar, highly significant differences in procedure time between the AS and RS cohorts (p < 0.0001) (Table 3). On average, residents added 11.8 min for T&A, 8.9 min for tonsillectomy alone, 5.2 min for adenoidectomy alone, and 3.9 min for bilateral tympanostomy tube placement (p < 0.001) (Table 3 and Figure 1).
Figure 1. Mean procedural times for attending surgeons (AS) and resident surgeons (RS) stratified by procedure type.
Additional factors modifying mean procedural time
Having identified resident surgeon involvement as a factor that significantly lengthens OR and procedural times, we turned our attention to determining whether other factors might also influence the mean procedural time of cases included in our analyses. Using multivariable linear regression analyses, we identified several additional predictors of procedural time for T&A cases, including older patient age (p < 0.0001), and attending surgeon identity (p < 0.0001) (Table 4). Gender, race, ASA classification, indication for procedure, year of the procedure, and case start time were not significantly associated with longer procedural times (Table 4). Thus, although involvement of a resident surgeon lengthens mean OR and procedural times, other factors also contribute to the overall efficiency of the operating room experience.
Discussion
Our data suggest that resident surgeons had significantly longer procedure times for all procedures analyzed, with the added operative time compared to an attending surgeon ranging from 4.9 to 12.8 minutes. Time differences between the RS and AS cohort increased proportionally to case complexity. Total operating room times were similar to those previous reported in the literature, confirming that our case experience was similar to national averages and thus generalizable.16 We also appreciated similar differences between RS and AS groups when examining procedural time, suggesting that the duration of the procedure as opposed to pre-operative preparation such as prepping the patient or post-operative factors such as extubation times explained differences in total OR time. Importantly, in our largest subgroup of T&A patients, multivariable linear regression analyses identified several additional factors including older patient age, and attending surgeon identity as statistically significant predictors of increased mean procedural time.
Careful selection of our inclusion and exclusion criteria narrowed our list of 9,574 cases to 3,922 cases meeting criteria. Although these criteria significantly reduced the number of cases analyzed, our criteria provided a relatively homogenous population, which could then be divided into cases completed by a RS or AS and subsequently compared. The few isolated differences in patient age, ASA classification, and indication for procedure is insufficient to explain differences in procedural and total OR times between RS and AS.
Although other studies have examined the impact of resident surgeons on a variety of surgical procedures across specialties,8-15 these studies have drawbacks that potentially limit the conclusions. In addition to being limited by small samples sizes, many of these studies combine procedures carried out at different institutions with numerous attending surgeons (Table 5). As a result, the role of the resident and his or her contribution in the OR is unclear. In fact, many of the previous studies make no distinction between resident assistants and resident surgeons, while the few studies that explicitly compare resident surgeons to attending surgeons analyze procedures that require an assistant (Table 5). Further, these studies did not account for additional factors that may influence operative efficiency.
Our study of 3,922 procedures at MEEI offers the largest analysis to date at a single institution with a small group of attending surgeons that are experienced in teaching residents at comparable training level. Further, by choosing a handful of common pediatric otolaryngology cases, our analysis focuses on procedures that are technically completed by an individual surgeon due to small size of the operative field; thus, we offer a rigorously controlled environment in which the role of residents in the OR can be reasonably investigated. Additionally, we were able to demonstrate that multiple factors beyond resident participation also contribute to longer procedural times. Finally, our analyses specifically measure actual procedural time, a distinction from past studies, which largely use total operating room time.
When evaluating our data, it is important to provide a balanced assessment of the “cost” of resident education. If one provides the percentage increase of time due resident participation, residents increase procedure lengths by 45.6 to 76.1%, on average, depending on the type of case. While these differences appear striking, the percentages correspond to a range of 3.9-11.8 minutes. This additional time difference is arguably minimal in the context of training future surgeons and it is unclear whether this additional time teaching directly results in lost case volume. Several previous studies focused on the financial cost of resident education by multiplying the cost of one minute in the OR by the increase in time attributed to resident involvement.9,10,12 These cost analyses are highly variable: Based on past studies, estimated cost per minute in the OR ranged from $4 to $42 per minute (Table 5). These differential costs highlight the variability across hospital systems and regions and identify a potential oversimplification of actual OR or “opportunity” costs.17 It is also unclear whether the time saved by limiting resident participation would translate into real differences in cost. Babineau and colleagues offer a sophisticated economic analysis of these various costs, arguing that even if the time of resident involvement was “saved,” the vast majority of OR costs are fixed and thus would not change.8 The few semivariable or semifixed costs such as the cost of overtime (semivariable) and the cost of OR staff (semifixed) represent small contributions to a typical OR budget (< 1.7%).8 Thus, in order to leverage time saved into financial savings, a hospital would have to eliminate unnecessary OR staff or increase operative volume to fill the added time available. In addition, without intra-operative resident support, cases that require sophisticated surgical assistance would require hiring of surgical assistants, such as physician assistants, who are typically paid by the surgical department; in contrast, United States-based resident salaries are largely provided indirectly by Medicare and the Department of Health and Human Services.18
Finally, cost calculations as described in the literature do not take into account potential time savings by resident participation in the perioperative care of the patient that may, in fact, allow increased case volume. At most institutions, the surgical resident ensures pre-operative paper work is completed, transports the patient to the OR, ensures proper imaging is available intra-operatively, and positions the patient on the operating table. Without the resident, nearly all the aforementioned tasks would have to be completed by the attending surgeon or an OR assistant such as the circulating nurse, scrub technician, or the perioperative care team (anesthesiologist, post-anesthesia care unit (PACU) nurse, etc.), all of whom are already performing other necessary tasks before the procedure. After the case, the resident performs a similar set of tasks, including writing orders, prescriptions, medication reconciliation, and post-operative instructions, and drafting an operative note. Therefore, analysis of total OR time and procedure length may not fully capture potential time saved due to resident involvement.
The main limitations of this study are its descriptive approach, variability in patient cohorts, and focus on a cross-section of operative procedures. Further, at our institution, junior otolaryngology residents (PGY2) largely perform these cases, and it is unclear if the difference between attending and resident surgeon would have decreased as residents gain experience. The strengths include the consistency of surgical environment in analyses, the choice of procedures that capture consistent resident involvement, and the large sample size. In the future, it will be essential to carry out studies examining additional operative procedures, with the goal of better determining the impact of resident training on procedure length. An important part of this analysis will be including multivariable regression to identify factors that modify the impact of resident training on operative time. In addition, further research should clarify the costs saved through resident-directed pre- and post-operative care, thereby providing insight into the overall costs of surgical residency training. Large-scale single institution analyses of more complex surgical procedures can clarify the impact of resident involvement on highly sophisticated techniques and procedures. However, by focusing on simple, lower complexity cases, our analysis has taken the first steps towards modeling the impact of residency training on operative times.
Conclusions
Resident participation in the operating room increases total OR time and procedure time for some of the most common pediatric procedures in the United States. We investigated and found that difference in operative time between resident surgeons and attending surgeons is proportional to the complexity of the case, with additional factors such as attending surgeon identity, and older patient age also influencing procedure times. While residents may increase procedure length, addressing other system-wide issues during the perioperative period may decrease the impact of time needed for education. Our model and findings are broadly applicable to surgical education across specialties. Future studies should cultivate robust cost-benefit analyses that may provide insight into incorporating residents into the operating room while simultaneously minimizing payor costs and maximizing efficiency.
Supplementary Material
Acknowledgments
We would like to thank Fran McDonald, Senior System Analyst, of the Massachusetts Eye and Ear Infirmary for her thoughtful approach to data acquisition and analysis.
Footnotes
Conflict of Interest: None
Financial Disclosure: None
References
- 1.Moses H, Matheson D, Dorsey E, George B, Sadoff D, Yoshimura S. The anatomy of health care in the United States. JAMA. 2013;310:1947–63. doi: 10.1001/jama.2013.281425. [DOI] [PubMed] [Google Scholar]
- 2.Kanich D, Byrd J. How to increase efficiency in the operating room. Surg Clin North Am. 1996;76:161–73. doi: 10.1016/s0039-6109(05)70429-1. [DOI] [PubMed] [Google Scholar]
- 3.Korda H, Eldridge G. Payment incentives and integrated care delivery: levers for health system reform and cost containment. Inquiry. 2011-2012;48:277–87. doi: 10.5034/inquiryjrnl_48.04.01. [DOI] [PubMed] [Google Scholar]
- 4.Van Eaton E, Tarpley J, Solorzano C, Cho C, Weber S, Termuhlen P. Resident education in 2011: Three key challenges on the road ahead. Surgery. 2011;149:465–73. doi: 10.1016/j.surg.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Cox S, Swanson M. Identification of teaching excellence in operating room and clinic settings. Am J Surg. 2000;183:251–5. doi: 10.1016/s0002-9610(02)00787-0. [DOI] [PubMed] [Google Scholar]
- 6.Nagendran M, Gurusamy K, Aggarwal R, Loizidou M, Davidson B. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev. 2013;8:CD006575. doi: 10.1002/14651858.CD006575.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mowry S, Hansen M. Resident participation in cadaveric temporal bone dissection correlates with improved performance on a standardized skill assessment instrument. Otol Neurotol. 2014;35:77–83. doi: 10.1097/MAO.0b013e31829c1106. [DOI] [PubMed] [Google Scholar]
- 8.Babineau T, Becker J, Gibbons G, et al. The “cost” of operative training for surgical residents. Arch Surg. 2004;139:366–70. doi: 10.1001/archsurg.139.4.366. [DOI] [PubMed] [Google Scholar]
- 9.Hosler M, Scott I, Kunselman A, Wolford K, Oltra E, Murray W. Impact of resident participation in cataract surgery on operative time and cost. Ophthalmology. 2012;119:95–8. doi: 10.1016/j.ophtha.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 10.Pollei T, Barrs D, Hinni M, Bansberg S, Walter L. Operative time and cost of resident surgical experience: effect of instituting an otolaryngology residency program. Otolaryngol Head Neck Surg. 2013;148:912–8. doi: 10.1177/0194599813482291. [DOI] [PubMed] [Google Scholar]
- 11.Hwang C, Wichterman K, Alfrey E. The cost of resident education. J Surg Res. 2010;163:18–23. doi: 10.1016/j.jss.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Farnworth L, Lemay D, Wooldridge T, et al. A comparison of operative times in arthroscopic ACL reconstruction between orthopaedic faculty and residents: the financial impact of orthopaedic surgical training in the operating room. Iowa Orthop J. 2001;21:31–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Bridges M, Diamond D. The financial impact of teaching surgical residents in the operating room. Am J Surg. 1999;177:28–32. doi: 10.1016/s0002-9610(98)00289-x. [DOI] [PubMed] [Google Scholar]
- 14.Papandria D, Rhee D, Ortega G, et al. Assessing trainee impact on operative time for common general surgical procedures in ACS-NSQIP. J Surg Educ. 2012;69:149–55. doi: 10.1016/j.jsurg.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Von Strauss Und Torney M, Dell-Kuster S, Mechera R, Rosenthal R, Langer I. The cost of surgical training: analysis of operative time for laparoscopic cholecystectomy. Surg Endosc. 2012;26:2579–86. doi: 10.1007/s00464-012-2236-1. [DOI] [PubMed] [Google Scholar]
- 16.Bhattacharyya N. Benchmarks for the durations of ambulatory surgical procedures in otolaryngology. Ann Otol Rhinol Laryngol. 2011;120:727–31. doi: 10.1177/000348941112001106. [DOI] [PubMed] [Google Scholar]
- 17.Sasor S, Flores R, Wooden W, Tholpady S. The cost of intraoperative plastic surgery education. J Surg Educ. 2013;70:655–9. doi: 10.1016/j.jsurg.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Dower C. Health Policy Brief: Graduate Medical Education. Health Affairs. 2012 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


