Abstract
We report a very rare case of primary endobronchial peripheral T-cell lymphoma (PTCL) not otherwise specified (NOS), which presented as an endobronchial tumor obstructing the main airway. An 81-year-old man was referred to our hospital for a 1-month history of productive cough and wheeze. Computed tomography revealed chronic pyothorax with calcified foci in the right lung and a mass inside the bronchus intermedius. Flexible bronchoscopy identified an endobronchial tumor obstructing the bronchus intermedius. The biopsy specimen showed an infiltration composed predominantly of small atypical lymphocytes. Immunohistochemical analyses demonstrated that the proliferating cells were positive for CD3, CD4, and CD5 and negative for CD8 and CD20. Pathological tests confirmed that the case was PTCL-NOS. PTCL-NOS should be considered in the differential diagnosis of endobronchial tumors.
Keywords: Bronchoscopy, endobronchial tumor, pulmonary lymphoma, pyothorax, T-cell lymphoma
Introduction
Peripheral T-cell lymphoma (PTCL) is one of the subtypes of T-cell lymphoma (TCL); it comprises a heterogeneous group of nodal and extranodal mature TCLs. Among the PTCLs, a subset is specifically defined as PTCL not otherwise specified (PTCL-NOS). PTCL-NOS do not correspond to any of the known T-cell entities. Primary pulmonary lymphoma (PPL) is a distinct entity that arises de novo in lung tissue [1]. We report an extremely rare case of primary endobronchial PTCL-NOS that presented as a tumor obstructing the main airway.
Case Report
An 81-year-old Japanese man was referred to our hospital for a 1-month history of productive cough and wheeze. He was a smoker (approximately 56 packs per year) and had a medical history of pulmonary tuberculosis at the age of 17 years. He had been diagnosed with chronic pyothorax and treated with intravenous injection of antibiotics 1 year prior to being seen at our facility. Upon examination, his body temperature was 37.2°C and a physical examination revealed wheeze and reduced air entry in the right mid-lung. No superficial lymph nodes were palpated. Blood assays revealed leukocytosis (12,500 leukocytes per microliter) and normal lactate dehydrogenase values (223 IU/L). Carcinoembryonic antigen and soluble interleukin-2 receptor values were slightly elevated to 5.8 ng/mL and 575 U/mL, respectively. A chest X-ray showed hypolucency of the right middle lung field, which suggested fluid accumulation. Computed tomography (CT) revealed chronic pyothorax with calcified foci in the right-hand portion of the right lung and a mass inside the bronchus intermedius (Fig. 1A). No mediastinal lymphadenopathy was detected. Flexible bronchoscopy identified an endobronchial tumor obstructing the bronchus intermedius (Fig. 1B). The biopsy specimen showed an infiltration composed predominantly of small atypical lymphocytes (Fig. 2A). Immunohistochemical analyses demonstrated that the proliferating cells were positive for CD3 (Fig. 2B), CD4, CD5 (Fig. 2C), and CD7 and negative for CD8 (Fig. 2D), CD20 (Fig. 2E), and CD30. The Ki-67 labeling index was low. Based on these findings, we diagnosed the tumor as PTCL-NOS. Positron emission tomography (PET) with [18F] fluoro-2-deoxyglucose and CT revealed uptake at the endobronchial tumor, with a maximum standardized uptake value of 20.6 (Fig. 1C). There was no evidence of abnormal uptake at the pyothorax, mediastinal lymph node, or other extrathoracic organs. His disease was considered stage IE, and the patient was treated with systemic chemotherapy (pirarubicin, cyclophosphamide, vincristine, and prednisone). After the first course of the chemotherapy, the endobronchial tumor markedly diminished on chest CT (Fig. 1D) and bronchoscopy. However, because of complication with refractory pyothorax, fenestration surgery was undertaken in a definitive fashion. Systemic chemotherapy was not delivered thereafter; however, the patient is free of recurrence 1 year after diagnosis.
Figure 1.
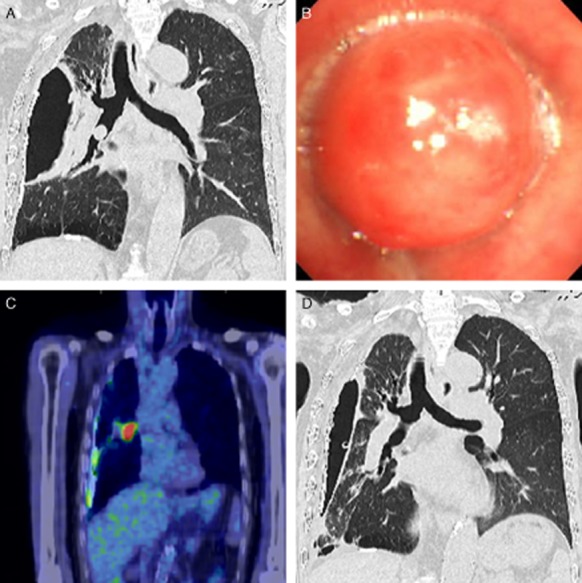
Imaging findings of the case. (A) Computed tomography (CT) revealed chronic pyothorax with calcified foci on the right and a mass inside the bronchus intermedius. (B) Flexible bronchoscopy identified an endobronchial tumor obstructing the bronchus intermedius. (C) Positron emission tomography with [18F] fluoro-2-deoxyglucose and CT revealed uptake at the endobronchial tumor. (D) CT after the chemotherapy demonstrated that the endobronchial tumor markedly diminished.
Figure 2.
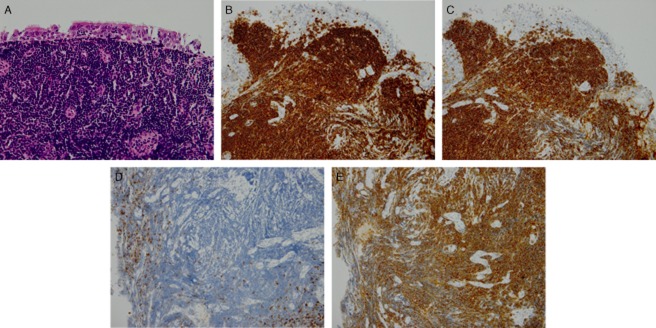
Biopsy specimen showed an infiltration comprised predominantly of small atypical lymphocytes (hematoxylin-eosin, 40×) (A). Immunohistochemical analyses demonstrated that the proliferating cells were positive for CD3 (B) and CD5 (C), and negative for CD8 (D) and CD20 (E).
Discussion
PPL is defined as lymphomas that affect the lungs (parenchyma, bronchi, and/or trachea) with no evidence of extrapulmonary extension in 3-month follow-up [2]. It is a rare condition that comprises only 3–4% of extranodal non-Hodgkin lymphomas (NHL), less than 1% of all NHLs [2], and 0.5–1% of primary pulmonary malignancies [3]. The majority of the reported cases have been of the B-cell type, so-called mucosa-associated or bronchus-associated lymphoid tissue lymphomas [4]. The current patient presented with a solitary endobronchial tumor, which is an extremely rare manifestation of PPL. Solomonov et al. reported that in a series of 441 patients with newly diagnosed NHL over a 7-year period, eight patients presented with a primary endobronchial B-cell lymphoma [1]. To our knowledge, this is the first report of PTCL-NOS presenting as a primary endobronchial tumor. PTCL-NOS is a diagnosis made based on the results of a tissue biopsy that demonstrates evidence of a TCL that does not meet the criteria for other subtypes of TCL including anaplastic large-cell lymphoma, angioimmunoblastic TCL, extranodal NK/TCL, nasal type, subcutaneous panniculitis-like TCL, enteropathy-associated TCL, and hepatosplenic TCL. The differential diagnosis is based on histologic examination and immunophenotype evaluation such as immunohistochemical panel (CD20, CD3, CD10, BCL6, Ki-67, CD5, CD30, CD2, CD4, CD8, CD7, CD56, CD57, CD21, CD23, ALK) or cell surface marker analysis by flow cytometry (kappa/lambda, CD45, CD3, CD5, CD19, CD10, CD20, CD30, CD4, CD8, CD7, CD2), and in difficult or equivocal cases, polymerase chain reaction-based assay for molecular detection of a clonal T-cell receptor rearrangement. The limitation of the current case was that the pathological diagnosis was based on small specimen through flexible bronchoscopy, so not all these markers were examined. However, we are confident of the diagnosis based on multiple immunohistochemical analyses.
The current case was complicated by chronic pyothorax. Pyothorax-associated lymphoma is a category in which a lymphoproliferative disorder develops in the pleural cavity after a long-standing history of pyothorax; it represents an entity distinct from other malignant lymphomas [5]. In our case, PET/CT revealed a hypermetabolic mass at the endobronchial tumor, but there was no abnormal uptake at the pyothorax. Endoscopic examination showed a smooth-surfaced, round tumor with a stalk; these features do not correspond to an outer parietal invasion. However, the coronal CT showed dense scar-like tissue between the wall of pyothorax and bronchus intermedius. These findings might suggest the relationship between the lymphoma and pyothorax. We think that the chronic inflammation could have contributed to the development of the disease.
In conclusion, we have reported upon what is, to the best of our knowledge, the first case of PTCL-NOS, which was confined to the bronchus. PTCL-NOS should be considered in the differential diagnosis of endobronchial tumor.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Acknowledgments
We thank Drs. Kyotaro Ohno, Yasuharu Sato, and Prof. Tadashi Yoshino, Department of Pathology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, for detailed pathological analyses.
References
- Solomonov A, Zuckerman T, Goralnik L, et al. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am. J. Hematol. 2008;83:416–419. doi: 10.1002/ajh.21112. [DOI] [PubMed] [Google Scholar]
- Chilosi M, Zinzani PL. Poletti V. Lymphoproliferative lung disorders. Semin. Respir. Crit. Care Med. 2005;26:490–501. doi: 10.1055/s-2005-922032. [DOI] [PubMed] [Google Scholar]
- Cadranel J, Wislez M. Antoine M. Primary pulmonary lymphoma. Eur. Respir. J. 2002;20:750–762. doi: 10.1183/09031936.02.00404102. [DOI] [PubMed] [Google Scholar]
- Cordier JF, Chailleux E, Lauque D, et al. Primary pulmonary lymphomas. A clinical study of 70 cases in nonimmunocompromised patients. Chest. 1993;103:201–208. doi: 10.1378/chest.103.1.201. [DOI] [PubMed] [Google Scholar]
- Aozasa K, Takakuwa T. Nakatsuka S. Pyothorax-associated lymphoma: a lymphoma developing in chronic inflammation. Adv. Anat. Pathol. 2005;12:324–331. doi: 10.1097/01.pap.0000194627.50878.02. [DOI] [PubMed] [Google Scholar]


