Abstract
Acute respiratory distress syndrome (ARDS) is one of the severe complications of influenza H1N1/09 infection, resulting in high mortality. Effective treatment strategies for ARDS are needed. This report presents two cases of ARDS due to influenza in Vietnam. Both cases were similar in terms of starting symptoms, the rapid progression to ARDS, and the treatment strategy, direct hemoperfusion with a polymyxin-B-immobilized fiber column (PMX-DHP) and oseltamivir. However, the clinical course of disease and the outcomes were different. For case 1, treatment was initiated on day 4 following the onset of hypoxemia due to ARDS. Symptoms improved rapidly after treatment and the patient was discharged on day 12. For case 2, treatment was initiated on day 9 after the onset of symptoms. Despite intensive therapy, the patient died on day 18. In conclusion, treatment with PMX-DHP and oseltamivir is effective on ARDS due to influenza but only if initiated early.
Keywords: Acute respiratory distress syndrome (ARDS), influenza, oseltamivir, PaO2/FiO2, polymyxin-B-immobilized fiber column (PMX-DHP)
Introduction
In the post-pandemic period of influenza H1N1/09, the intensive care unit (ICU) at our hospital has continued to receive patients with acute respiratory distress syndrome (ARDS) caused by influenza H1N1/09 from the local hospitals in Vietnam. However, effective treatment strategies for ARDS due to influenza are yet to be confirmed. Direct hemoperfusion with a polymyxin-B-immobilized fiber column (PMX-DHP) is a treatment method that selectively absorbs and removes blood endotoxins in cases of severe sepsis and septic shock [1]. This report presents two cases of ARDS due to influenza H1N1/09, who received the same treatment (PMX-DPH) but had different outcomes.
Case Report
Case 1
A 20-year-old Vietnamese female had flu-like symptoms on April 11, 2013. Four days later, she visited a local hospital with exacerbated dyspnea. Her chest X-ray revealed diffuse infiltrations. She was clinically diagnosed with pneumonia due to influenza and administered oseltamivir (150 mg/day). She was immediately transferred to the ICU in our hospital. Her Glasgow score was 15 and she presented cyanosis, dyspnea, and tachycardia. Arterial gas analysis (AGA) showed severe hypoxemia (PaO2/FiO2 [ratio of arterial oxygen partial pressure to fractional inspired oxygen], 170) under 15 L/min of supplemental oxygen administered via a mask (Table 1). A chest radiograph showed diffuse infiltrations (Fig. 1A1). Echocardiography was normal (ejection fraction/EF, 65%). She tested negative twice for influenza H1N1/09 virus by a real-time reverse-transcription polymerase chain reaction (RT-PCR) assay on a sputum sample, but later tested positive in a serological test. Bacteria were not detected in sputum or blood cultures.
Table 1.
Laboratory findings at the time of ICU admission
| Case 1 | Case 2 | |
|---|---|---|
| Blood gas analysis | ||
| pH | 7.44 | 7.34 |
| PaCO2 | 33 | 53 |
| PaO2 | 88 | 72 |
| HCO3 | 22.4 | 28.6 |
| Base excess | −1.8 | 2.8 |
| Blood cell count | ||
| RBC (104/μL) | 4.76 | 5.34 |
| Hemoglobin (g/dL) | 10.1 | 15.4 |
| Hematocrit (%) | 29 | 45 |
| WBC (103/μL) | 7.85 | 8.16 |
| Neutrophil (%) | 59.7 | 90 |
| Lymphocyte (%) | 33.8 | 7.1 |
| Platelet (104/μL) | 179 | 342 |
| Respiratory condition | ||
| PaO2/FiO2 | 170 | 89 |
| Respiratory support | Oxygenation by mask | BiPAP |
ICU, intensive care unit; PaO2/FiO2, ratio of partial pressure arterial oxygen and fraction of inspired oxygen; RBC, red blood cell; WBC, white blood cell.
Figure 1.
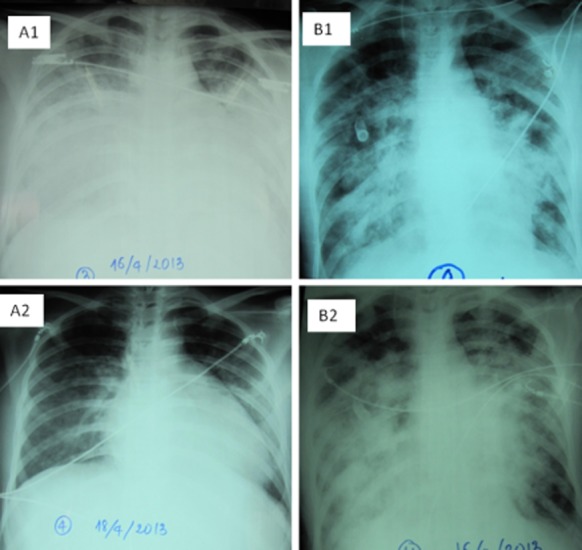
Chest radiographs at the time of ICU admission. Case 1 showed diffuse infiltrations (A1) and at the time of discharge from ICU showed resolution of shadows (A2). Chest radiographs at the time of ICU admission on case 2 (B1) showed bilateral severe infiltrations and at the time before death showed worsening shadows (B2).
She was diagnosed with ARDS. Ventilation support was initiated using biphasic positive airway pressure (BiPAP) along with the empirical treatments of oseltamivir and antibiotics (imipenem, levofloxacin). Twelve hours later, her PaO2/FiO2 ratio was 182. PMX-DHP was initiated and performed for 14 h on day 4 after the onset of symptoms. The PaO2/FiO2 improved to 375 on day 5 (Fig. 2). On day 8, she was weaned from BiPAP to a nasal cannula. The PaO2/FiO2 improved to 380 with no oxygenation and her chest radiograph improved on day 9 (Fig. 1A2). She was discharged from hospital on day 12.
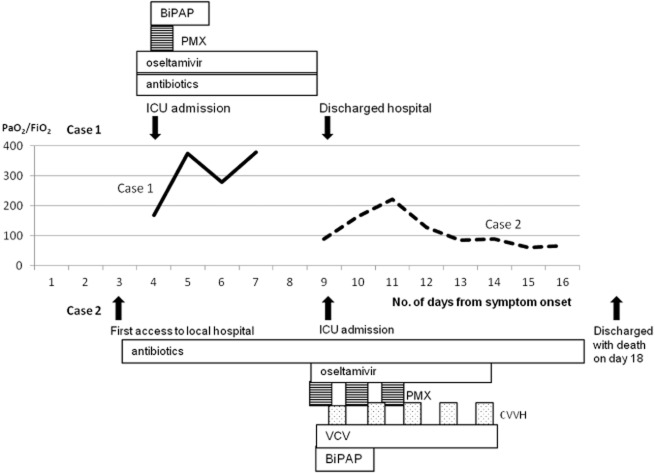
Figure 2.
Clinical course of case 1 in upper part and case 2 in lower part. Case 1 admitted to the ICU on 4 days after symptom onset with 170 of PaO2/FiO2. After PMX-DPH, the PaO2/FiO2 on case 1 (solid line) improved, weaned from oxygen supplement therapy, and discharged ICU on 12 days from symptom onset. Case 2 admitted to the ICU on 9 days after symptom onset with 89 of PaO2/FiO2. Although PaO2/FiO2 of case 2 (dotted line) improved after three consecutive days to 222, it dropped to less than 100. Finally, case 2 died on day 18 from symptom onset. BiPAP, biphasic positive airway pressure; CVVH, continuous veno-venous hemofiltration; PaO2/FiO2, partial pressure arterial oxygen and fraction of inspired oxygen; PMX, polymyxin-B-immobilized fiber column; VCV, volume control ventilation.
Case 2
A 23-year-old Vietnamese male had flu-like symptoms on April 3, 2013. On day 3, he visited a local hospital because of exacerbated dyspnea. The chest radiograph revealed diffuse infiltrations. He was admitted to the local hospital and was treated with antibiotics (amikacin, ceftriaxone) with the diagnosis of bacterial pneumonia. His condition deteriorated. On day 9, he was transferred to our ICU and his Glasgow score was 15. AGA (under BiPAP) showed severe hypoxemia (PaO2/FiO2 of 89; Table 1). A chest radiograph revealed diffuse infiltrations (Fig. 1B1). Echocardiography was normal (EF, 65%). Treatment with oseltamivir (300 mg/day) was initiated based on the possibility of influenza infection, along with broad spectrum antibiotics (imipenem, levofloxacin). On day 10, the PaO2/FiO2 had dropped to 78. PMX-DHP was initiated and performed three times at 8-h intervals (Fig. 2). He also received continuous veno-venous hemofiltration (five times) as a non-renal indication between PMX-DHP treatments. Volume control ventilation was also initiated. On day 11, the PaO2/FiO2 had improved to 166. On day 12, it was 222, but on day 13, it had dropped to 128 (Fig. 2). On day 14, bacterial infection was detected in blood cultures. The chest radiograph showed no improvement (Fig. 1B2). On day 16, the PaO2/FiO2 had dropped further to 68, and on day 18, the patient died of respiratory failure. A positive result for influenza H1N1/09 virus by RT-PCR on a sputum sample was obtained during ICU admission.
Discussion
This report highlights that the early initiation of PMX-DPH and oseltamivir treatment is critical to obtaining a successful outcome in the treatment of ARDS due to influenza H1N1/09 virus infection.
PMX-DHP can be used for non-renal indication [2]. Previously, we reported our trial of PMX-DHP treatment on ARDS due to avian influenza (H5N1) that resulted in successful outcomes if initiated early (No. 7998/BYT-K2DT, 2011) [3]. Hypercytokinemia is one of the main causes of severe pneumonia associated with H5N1 infection. Improvement in the PaO2/FiO2 related to the removal of serum cytokines as well as activated neutrophils and monocytes by PMX-DHP [3], [4]. Also, some successful cases of PMX treatment for ARDS with influenza H1N1/09 infection have been reported that were associated with decreased blood cytokine levels [4].
In the present report, both cases were similar in terms of the starting symptoms and the rapid progression to ARDS. The different outcomes resulted from the timing of treatment. For case 1, treatment with PMX-DHP and oseltamivir was initiated on day 4, compared with day 9 for case 2.
Case 1 was admitted to our ICU with moderate ARDS, which would usually be difficult to cure with antiviral agents alone, even if treatment was initiated early [5]. We treated with PMX-DPH in addition to oseltamivir, and observed a dramatic improvement in the PaO2/FiO2. By contrast, for case 2, physicians in the local hospital did not suspect influenza infection, but instead treated the patient for bacterial pneumonia. It is therefore important to raise awareness among physicians regarding the rapid progression of this disease. Information on the clinical aspects of rapid progression of pneumonia with diffuse infiltrates, such as chest X-ray observations and laboratory findings (i.e. no leukocytosis and thrombocytopenia), would assist their clinical diagnosis.
In conclusion, early treatment with PMX-DHP and oseltamivir may improve oxygenation, especially, in a case of moderate ARDS due to influenza H1N1/09, resulting in a successful outcome. The result assists the clinical decision making. The further investigations are warranted.
Acknowledgments
Authors thank the medical doctors in the ICU of Bach Mai Hospital and the provincial hospitals who were involved in providing clinical care to patients. The authors also thank Shinyu Izumi and Jin Takasaki for their technical support for using PMX. This study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI26293115.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
References
- Hisataka S. Extracorporeal endotoxin removal for the treatment of sepsis: endotoxin adsorption cartridge (Toraymyxin) Ther. Apher. Dial. 2003;7:108–114. doi: 10.1046/j.1526-0968.2003.00005.x. [DOI] [PubMed] [Google Scholar]
- Cruz DN, Antonelli M, Fumagalli R, et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA. 2009;301(23):2445–2452. doi: 10.1001/jama.2009.856. [DOI] [PubMed] [Google Scholar]
- Kudo K, Binh NG, Manabe T, et al. Clinical preparedness for severe pneumonia with highly pathogenic avian influenza A (H5N1) Respir. Investig. 2012;50:140–150. doi: 10.1016/j.resinv.2012.08.005. [DOI] [PubMed] [Google Scholar]
- Takeda S, Munakata R, Abe S, et al. Hypercytokinemia with 2009 pandemic H1N1 (pH1N1) influenza successfully treated with polymyxin B-immobilized fiber column hemoperfusion. Intensive Care Med. 2010;36(5):906–907. doi: 10.1007/s00134-010-1830-8. [DOI] [PubMed] [Google Scholar]
- Higuera Iglesias AL, Kudo K, Manabe T, et al. Reducing occurrence and severity of pneumonia due to pandemic H1N1 2009 by early oseltamivir administration: a retrospective study in Mexico. PLoS ONE. 2011;6(7):e21838. doi: 10.1371/journal.pone.0021838. doi: 10.1371/journal.pone.0021838. [DOI] [PMC free article] [PubMed] [Google Scholar]