Abstract
Between now and 2030, every country will experience population ageing—a trend that is both pronounced and historically unprecedented. Over the past six decades, countries of the world had experienced only a slight increase in the share of people aged 60 years and older, from 8% to 10%. But in the next four decades, this group is expected to rise to 22% of the total population—a jump from 800 million to 2 billion people. Evidence suggests that cohorts entering older age now are healthier than previous ones. However, progress has been very uneven, as indicated by the wide gaps in population health (measured by life expectancy) between the worst (Sierra Leone) and best (Japan) performing countries, now standing at a difference of 36 years for life expectancy at birth and 15 years for life expectancy at age 60 years. Population ageing poses challenges for countries’ economies, and the health of older populations is of concern. Older people have greater health and long-term care needs than younger people, leading to increased expenditure. They are also less likely to work if they are unhealthy, and could impose an economic burden on families and society. Like everyone else, older people need both physical and economic security, but the burden of providing these securities will be falling on a smaller portion of the population. Pension systems will be stressed and will need reassessment along with retirement policies. Health systems, which have not in the past been oriented toward the myriad health problems and long-term care needs of older people and have not sufficiently emphasised disease prevention, can respond in different ways to the new demographic reality and the associated changes in population health. Along with behavioural adaptations by individuals and businesses, the nature of such policy responses will establish whether population ageing will lead to major macroeconomic difficulties.
Introduction
Increased longevity is one of the most remarkable success stories in human history. However, coupled with decreased fertility rates, it raises serious concerns about the economic consequences of longer lives and an increased proportion of people aged 60 and older in the populations of rich and poor countries alike. These concerns—which are typically premised on a world of static policy and institutions, continuing low fertility trends, constant age-specific savings and labour-participation rates, and constant age-specific health and functional statuses—range from macroeconomic slow downs to heightened financial strain on pensions, health, and other social-protection systems.1–3
In view of the rapid and accelerating pace of population ageing, merely tweaking existing institutions and policies is unlikely to be a sufficient response to the challenges posed. No historical examples are available to guide decision making; therefore, countries will need to rely on fresh analyses rather than historical examples of policy change. Deep and fundamental reforms, the achievement of which will be fraught with political difficulties,4,5 are needed both to tackle entrenched expectations of early retirement and unsustainably generous pension entitlements, and to reduce the emphasis of most health systems on the provision of expensive treatment and care rather than on disease prevention.
In our Series paper, we seek to dispel misconceptions about the large negative effects of population ageing on macro economic performance, and on the financial integrity of pension and health-care systems. As long as key stakeholders do not adhere statically to existing approaches, we conclude that population ageing will not necessarily, or even probably, cause widespread economic distress. Population ageing during the coming decades will naturally lead to and need changes in labour and capital markets, retirement policies and pensions, and the organisation and financing of health systems.6–8 However, some actions, if initiated now, would offset any potential macroeconomic difficulties.9
Effective responses should take account of national differences, because many factors play a part in establishing the economic effects of population ageing. Health, long-term care, and pension systems are diverse; government commitment to funding health care and pension programmes varies in form, intensity, and effectiveness; labour-force participation and savings rates have an enormous spread; income per person varies widely; and societal treatment of older people and traditions for family responsibility vary across cultures and over time.
Although universal health insurance is normal in many high-income countries (HICs), the situation is varied in low-income and middle-income countries (LMICs) where older people and their families are often at high risk of incurring catastrophic, out-of-pocket, health expenditures. Of course, the nature of health insurance varies widely throughout the world, so straightforward comparisons of coverage rates do not tell the whole story. With respect to the costs of long-term care, some industrialised countries have established explicit and comprehensive long-term care programmes,10 although substantial scope exists for improved organisation and coordination of services.11 In other countries, such as the UK, long-term care is fragmented, largely means tested, and often of poor quality.12 In most LMICs, formal long-term care is weak, with the burden typically falling on families, whose capacity for the provision of physical care and companionship is diminishing because of small family sizes, increased participation of women in the workforce, and increased geographical mobility.
Responses to population ageing should also recognise the contributions that older people make to society. In addition to their potential capacity to work, older people embody a large reserve of human capital, especially in education and work experience. A lifetime of experiences can make older adults wiser and more adept at assessing and addressing a wide array of situations, in addition to mentoring young people, which could serve to mitigate some of the economic drawbacks posed by population ageing.
Main economic concerns
Those who contend that an increase in the population share at older ages will drive many undesirable macroeconomic phenomena13 typically base their argu ments on five points:
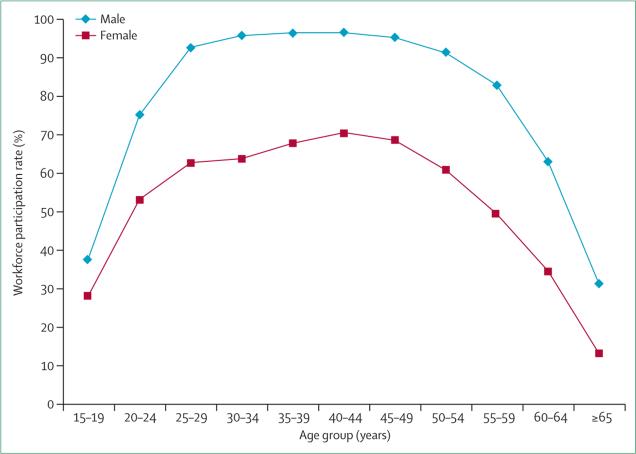
First, older people do not work as much as young and middle-aged adults, which means that an economy populated mainly by such people will tend to create less output (on a per-person basis) than an economy with a higher proportion of individuals at prime working ages. Cross-country differences aside, workforce participation typically peaks at about age 40 years, and falls to less than 50% by age 65 years for men and by age 55 years for women (figure 1). This decrease might be partly offset by a workforce that is effectively enlarged by increased investments in education, training, and health. Additionally, declines in fertility can result in an increased number of women working because of reduced childcare responsibilities, which will contribute to economic growth.15
Figure 1. Employment by age.
Age-specific workforce participation14 M=male. F=female. Combined figures for all countries in 2012.
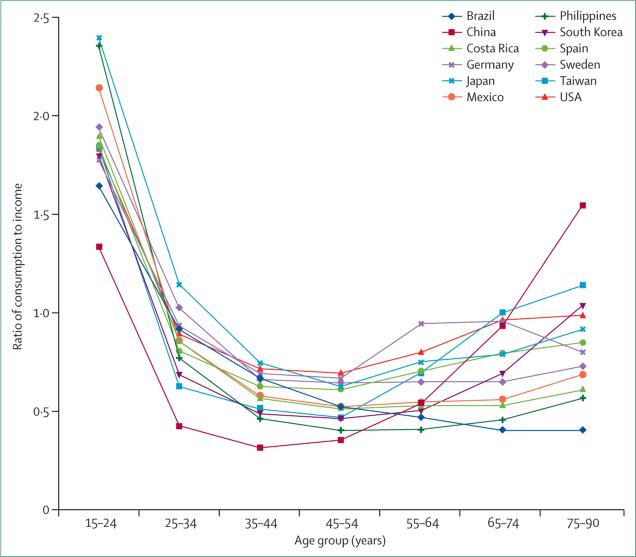
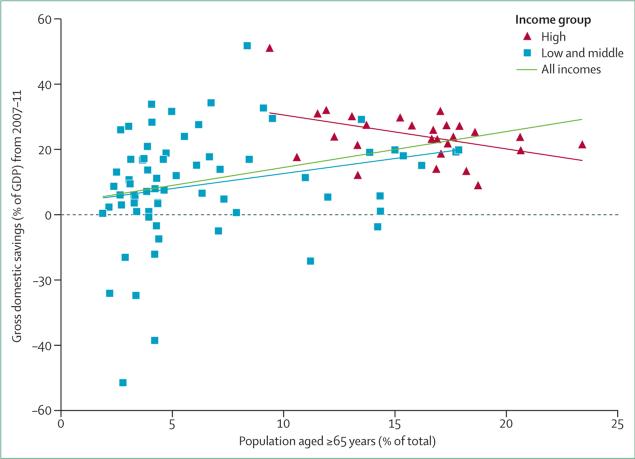
Second, consumption accounts for a higher proportion of income in older adults than for those at the prime working ages. Theoretically, as the older share of the population rises, average savings rates will tend to fall, potentially leading to a scarcity of investment capital (figure 2). However, the negative relation between the proportion of the population aged more than 65 years and the savings rate is not nearly as clear as might be expected (figure 3). In HICs, the association is indeed negative, but the outlier (Singapore) and the spread of data diminish its importance. By contrast with HICs, LMICs show a slight positive association between age and savings rates, although there is much heterogeneity, and outliers affect the association substantially. These findings undercut the concerns of major reductions in savings rates as population ageing progresses. (This slight association does not conflict with the stronger associations shown in figure 2, which shows consumption rates for specific age groups but does not show the share of the population in each age group.) Higher-than-expected savings rates at older ages could show uncertainty about longevity, the concomitant need to pay for long-term care, and the desire to leave bequests.
Figure 2. Age-specific consumption as a share of income, by age and country.
Income includes labour income, asset income, and net public transfers.16
Figure 3. Savings by age in developed and developing countries.
Gross domestic savings versus the share of the population aged at least 65 years, grouped by high, middle, and low-income countries.17 Blue=regression line for low-income and middle-income countries. Red=regression line for high-income countries. Black=regression line for all countries combined. GDP=gross domestic product. Gross domestic savings are calculated as the GDP for each country minus the final consumption expenditure (total consumption). Data exclude countries with a population of less than 1 million, or oil rents of more than 2·5% of the GDP (average for 2007–11).
Third, an increasing proportion of older people tends to raise the demands on pension schemes. This finding is especially relevant when effective pension coverage is high and when a system aims to guarantee a minimum level of protection, irrespective of earnings history, as for most HICs. Population ageing introduces new difficulties for the fiscal integrity of public and private pension systems, such as a low share of workers contributing to the system and longer periods of benefit receipt associated with increased longevity. In LMICs the difficulties tend to be different—some are encountering population ageing before they have secured comprehensive social security coverage and before they have the resources to support large cohorts of retired people.18
The link between population ageing and pension costs is not as direct as widely claimed. Both HICs and LMICs often have powerful incentives for early retirement. In LMICs with high levels of informal employment and low levels of social security coverage, pension systems are dominated by expensive and reform-resistant, civil-service schemes. In some countries, pension obligations have become enormous–eg, in Brazil, public spending on pensions equals 13% of the national gross domestic product (GDP), and a similar proportion is spent in Italy and France.19 However, in other countries such as the UK, the cost of public-sector pensions is falling as a share of GDP, which is partly attributable to increased privatisation and delayed retirement. The researchers of a thorough review of pension policy reforms—including movement toward or away from pay-as-you-go systems—concluded that no one system is best, and that reforms should be tailored to each country.20,21
Fourth, disease and disability in older adults represent a substantial loss to national production. The supply of a workforce is depleted by mortality and morbidity, which are concentrated factors in older people. Capital is also depleted, because of the diversion of savings to spending on health and long-term care. Calculations based on a macroeconomic model (EPIC) developed by WHO22 suggest that sizeable costs are associated with noncommunicable diseases (NCDs), which predominate in older adults.23,24 However, large cross-country differences in the age-specific prevalence of most NCDs suggest that the effects of ageing can be modified.
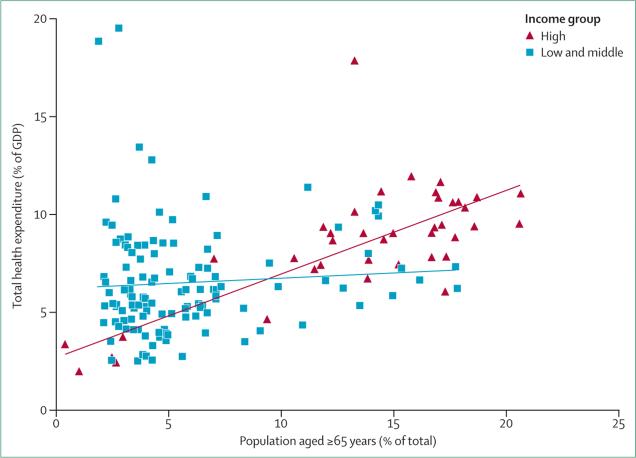
Fifth, older people place a large burden on health and long-term care systems, especially in high-income countries, and contribute reduced revenue to their support. The positive correlation between health-care expenditure and the proportion of elderly people in a population (figure 4) is partly because countries with older populations tend to have higher incomes and thus can spend more on health than younger populations. But even with controls set for income, this association still holds. Increased health-care spending at older ages is largely driven by much higher outlays in the final years of life, with substantial heterogeneity.25
Figure 4. Health expenditure outlays by age.
Total health expenditure as a share of gross domestic product versus the percentage of the population aged at least 65 years.17 GDP=gross domestic product.
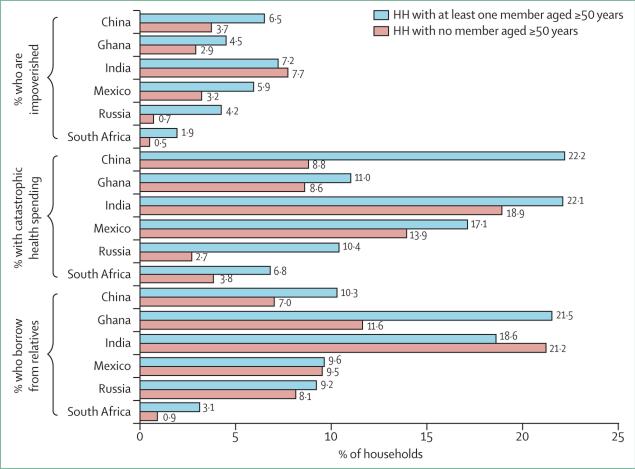
Higher costs later in life are associated with health and long-term care of older people. The potential burden on informal social care systems in LMICs—for which a great deal of health spending is private26—is shown in a study of six such countries (the WHO Survey on Global Ageing and Adult Health [SAGE], figure 5),27 in which households with members aged at least 50 years had higher rates of impoverishment and catastrophic health expenditures than households without older members. These raised demands on financial resources are associated with increased borrowing from relatives, amplifying the economic burden on the wider family and household.28
Figure 5. Financial status of households with and without older people.
Financial effects of having an older person as a member of a household, by household type and country.27 HH=household. Impoverished expenditures: a non-poor household is judged to be impoverished by health payments if it becomes poor after paying for health care. Catastrophic expenditures: out-of-pocket health payments of at least 40% of non-subsistence spending.28 Impoverishment figures are not indexed to country-specific poverty line calculations.
Population ageing in LMICs is likely to aggravate existing strains on formal health systems. It will also magnify the needs for long-term care, as traditional family-based approaches become less feasible because of declines in fertility and socioeconomic changes. Most LMICs have long had young populations, so their health systems are attuned to issues that predominantly affect the young and working-age populations. As populations age, the distribution of health disorders changes, with an increased prevalence of cancer, fractures, cardiovascular diseases, depression, and dementia29,30 and many comorbidities that need a wide range of potentially interacting treatments.31–33 Complicating this situation, the epidemiological transition is also driven by risks accumulated during the life course, when not successfully counteracting risks in early life and young adulthood will mean an older adult population with possibly increased levels of ill health and disability.34
If allowed to become overburdened, health and long-term care systems in HICs might develop the same gaps in provision for older people as in LMICs. Our analysis of SAGE data35 for six LMICs shows that less than 10% of older adults with depression and about 45% of those with angina were being treated for their disorders—these figures do not include the substantial numbers of older people who were unaware of their health problems.
Behavioural and public policy responses
Many behavioural changes and public policy responses to population ageing have the potential to mitigate the concerns we have outlined, especially with respect to diminished economic growth.1,7,8,13,36,37 The mix of interventions chosen (eg, raised taxes for workers or their employers, decreased benefits for retirees, or raising the age of retirement) will naturally affect the distribution of costs between possible payers.
General economic and social trends, including changes in wages and relative prices of different goods and services and technological innovations, will naturally mitigate some of the pressures associated with population ageing.1 For example, an increased number of women working, higher savings in expectation of longer lifespans, and fewer but healthier and better-educated young people can boost rates of income growth per person in the face of low fertility and population ageing.15,38–40 Smoking cessation, a reduction in excessive alcohol consumption, adherence to healthier diets,41 engagement in more physical activity, and taking advantage of adult vaccines such as those for influenza, pneumococcal disease, human papillomavirus, and shingles, are also behavioural responses that would promote improved health in older people.
Many public and private options exist to address the economic challenges raised by population ageing. Such reforms (some of which do not focus specifically on older populations) could improve work productivity, earnings, and tax contributions from older individuals, especially if coupled with diminished incentives for early retirement. To the extent that stronger health systems prevent disease, or detect and treat it at an earlier stage, health and long-term care spending could also be diminished. A key adaptation is emphasis on disease prevention. Many low-cost interventions, ranging from those designed to encourage behavioural change42 to therapeutic measures,43–46 could improve or maintain health in elderly people. Similarly, policies and population-based inter ventions geared to prevent or delay health disorders and improve wellbeing assume a particular importance for older people.4
Approaches that show promise47,48 focus on the prevention or postponement of disability by lowering risk factors;49–53 such measures, even if initiated in middle and older ages, might decrease disability, risk of disease, and lifetime medical expenditures.42,54–57 For example, a straightforward intervention such as a reduction in salt intake is proposed as an important contributor to the decreased blood pressure noted from 2003 to 2011 in England.58 A reduction in the risk factor of high blood pressure could, in turn, reduce the associated outcomes of stroke and ischaemic heart disease mortality.
A distinction between individual and social perspectives, and between the short or medium term, and the long term, is important. For example, in the short term, a medicine that extends lifespan and productivity late in life will tend to improve the wellbeing of older people and save costs to society. However, in the long term, whether such a medicine is cost saving or a burden to society will depend on several factors–ie, (1) the implications of the medicine for the length and quality of the additional years of life, (2) employment, earnings, and pension recipiency during those additional years; (3) the cost of the medicine; and (4) any medical and non-medical care costs associated with other health disorders that could eventually ensue.
The five most common non-communicable diseases (cardiovascular disease, cancer, chronic respiratory disease, diabetes, and mental health disorders) constitute an increasing share of the burden of disease in all countries.59 NCDs are strongly associated with age and are driven by behavioural risk factors that increasingly characterise LMIC populations, or poor people within high-income countries, including unhealthy diet, physical inactivity, tobacco use, and excess consumption of alcohol. Poverty exacerbates some of these risk factors, and can be reinforced by any resultant NCDs.
NCDs are often costly to treat, partly because many of them (such as hypertension) are chronic, with patients requiring care and treatment for many years.60,61 However, prevention and control of NCDs can often pay for itself because the investments needed to diminish their prevalence can be less than the economic losses caused by their sequelae.62,63 Measures that can most cost effectively reduce NCDs apply to the whole population and include behaviour-change campaigns, some screening and treatment interventions, and policies that address the social determinants of disease.23,24 However, unless effective treatment can be accessed, early diagnosis will offer little benefit.
In most LMICs, the provision of quality coverage to all older people to protect against catastrophic spending and impoverishment due to health-care issues is a long way off. In these settings, basic packages of cost-effective health services suited to the needs of older people should be developed, and primary health-care programmes should be reoriented to the changing demographic and epidemiological patterns, with increased focus on integrated-service delivery. Generally, there is wide scope to reform health-care financing mechanisms, to enhance their fairness and sustainability, and to promote risk pooling and operational efficiency. Such reform has the potential to reduce fiscal pressures associated with population ageing and improve access to services, especially for disadvantaged groups.
The need to establish effective financing mechanisms is especially acute in most LMICs, where levels of health insurance coverage vary in terms of the share of older populations enrolled, the services included, and the degree of protection they offer from catastrophic expenditures.64,65 Additionally, the implications of health insurance for health outcomes depend on their integration with other policies. For example, WHO SAGE data35 show that a scarcity of health awareness in older people and of available health services (particularly in rural areas), and low treatment effectiveness, meant that insurance coverage was not associated with higher rates of hypertension control.63
As for covering the costs of long-term care, some HICs have been striving to reduce institutional care while supporting self-care and other services that enable older people to remain in their own homes or a home-like environment.66,67 The importance of informal care and the types of support that can be given to informal caretakers, who remain the main source of care for older people worldwide, are also increasingly recognised.68 Of course, any effort to estimate the costs of long-term care– and in particular to do so on a comparative basis–faces the great difficulty of taking into account the extended care by families, which predominates in many parts of the world and which generally is not factored into calculations of national economic output. For example, if a family that formerly took care of older members at home begins to pay for institutional care, health and long-term care costs as accounted for in GDP calculations will rise, even though the amount of care provided might not change. In addition to an integration of such services11 and improvements in their quality, regulation is much needed, especially in LMICs, where there is a predominance of small-scale, unregulated, private sector providers.69 HICs and LMICs alike can learn from the example of Japan's Government-initiated, mandatory, public, long-term care insurance policy, which during the past decade has ushered in increased use of formal care at a reduced cost to households.10 This system is highly tailored to the social and policy environment in Japan—eg, only formal services are provided, but recipients can choose their services and providers.
The management of complex chronic conditions can be improved by training more health workers and physicians in geriatric care, developing supportive information systems, and financing mechanisms that encourage integration rather than fragmentation.47,70 The creation of cadres of geriatricians or, in their absence, enhancement of the skills of family doctors, is an important objective of the UN International Action Plan on Ageing.71 More broadly, LMICs need more health-care workers at all levels of training—such as nurses and community health workers—especially in rural areas, where large numbers of older adults reside. Such an influx could help with mainstream care for older people within primary health-care systems in countries where such services are heavily focused on infectious disease and maternal and child health.
Medical curriculae, in order to stay responsive to the health needs of older populations, should also address the challenges of managing many interacting disorders.72 According to a 2002 study, only about 50% of 72 high-income and low-income countries had national curriculae in geriatric medicine in their medical schools, and in only 41% of these countries was geriatric medicine training mandatory.73 Advances in geriatric sciences could bring many benefits to older people74–76 but the number of geriatricians is low or decreasing in many countries, although advances in multidisciplinary training in Europe are encouraging.74,77
Although a larger elderly share of the population can lead to a proportionally smaller workforce, policy and behavioural changes can make this workforce more effective. Increased investment in the training, education, and health of workers can help to counter the decreasing workforce resulting from reduced fertility. If such investment results in higher human capital (the skills and capacities that people have that could be put to productive use) held by the workforce, the productivity and standards of living could in fact increase.40,78 Better health, cognition, and education will generally translate into more productive working adults, and this effective enlargement of the workforce will help to counteract the shrinkage associated with population ageing.
In the interest of improving market efficiency, substantial scope exists for the improvement of individuals’ financial literacy, so that they can make better choices about the forms, accessibility, and security of their wealth. Older people make these choices with much uncertainty about individual longevity, real rates of return, and benefits derived from government pro grammes, and they are making these choices during phases of their lifecycle in which cognitive function is reduced.
In principle, international migration could ameliorate the effects of population ageing, because LMIC populations that are still mainly youthful can fill job vacancies and provide care workers to countries whose populations are ageing rapidly. Many potential workers wish to move permanently or temporarily to another country to work, but many of them are either ineligible for any form of legal movement or face decades-long waiting lists. These barriers to immigration in part show growing anti-immigrant sentiments in HICs. The absence of mechanisms for social welfare entitlements to be portable across countries is another barrier to increased immigration.
Several items have been proposed for migration policies that would meet both the demand of LMIC workers for employment, and care needs in HICs. These include proposals for bilateral guest–worker agreements between such countries.79 However, in view of present political views in most HICs, increased immigration will probably not appreciably offset the workforce issues posed by population ageing except in a handful of countries.80
A common argument is that people will respond naturally to longer and healthier lifespans by planning on lengthened working lives. However, most of the world's social security systems still offer retirement pensions between age 60 and 65 years, with often strong incentives for early retirement. An analysis of data from public pension systems in 43 high-income and middle-income countries between 1965 and 2005 showed that life expectancy for men in those countries rose by an average of nearly 9 years during this period, but the mean legal retirement age rose by less than half a year.8
More freedom of choice for people with respect to the timing of their retirement, perhaps by removing any tax disincentives associated with working past the legal retirement age, would increase the workforce supply and alleviate some fiscal pressures. But the realisation of long working lives presupposes suitable opportunities for older workers and a desire to continue working. Many HICs (such as Australia, France, Greece, Ireland, and the UK) are gradually raising the statutory retirement age, although the acceleration of such reforms (as in the UK) might be driven by cost-cutting objectives associated with the post-2008 global financial crisis rather than goals that enhance the workforce supply. Additionally, raising of the retirement age has created social and political tension in some HICs, especially in view of the high rates of unemployment during the past 5 years. Nevertheless, further moves in the direction of later ages of retirement seem probable. For example, Sweden is considering raising the retirement age to 75 years. Norway has taken a different approach: new cohorts of older people will receive a pension calculated as the accumulated pension entitlement divided by a life-expectancy divisor. Thus, as life expectancy rises, the annual pension will decrease.2,81
By expanding the horizon over which the benefits of investments in education, training, job searches, and health can accrue, raising of the legal age of retirement will also tend to promote higher productivity, income, and tax contributions. In the USA, workforce-participation rates of older individuals have been increasing for the past two decades, especially in those with high levels of education.82
An increase in the age of retirement would have little effect on work participation in older individuals who are not working because of poor health. However, our analysis of large, nationally representative samples of individual-level data from a similar set of health and retirement surveys undertaken in 15 wealthy, industrial countries in 201083 shows that more than half of those aged at least 60 years who are not working do not identify health disorders as the reason for that status. The countries analysed were Austria, Belgium, Czech Republic, Denmark, England, France, Germany, Greece, Italy, Netherlands, Poland, Spain, Sweden, Switzerland, and the USA. As the health status of older individuals improves or deteriorates over time, the effect of a later retirement age on workforce participation could be amplified, or muted.
Especially in HICs, market mechanisms will naturally induce changes in business practices in response to population ageing. Businesses can adjust their human resources practices to cater to older employees’ desires for flexible roles and schedules, with the inclusion of options for reduced or flexible hours, the provision of on-site health-care facilities, and retraining of older workers for jobs that are less physically demanding.84
Businesses could also invest in worker-wellness programmes to enhance attendance and productivity and to avoid unnecessary health-care costs as the workforce ages. They could also restructure pay scales to acknowledge the changing capabilities of older workers, and take advantage of new opportunities that will accompany population ageing (eg, the design and marketing of products and services customised to older people to equip them with more capital and better technology). In other words, many economies have some powerful self-correction mechanisms that are likely to come into play.36
New technologies also offer many ways of bringing health care to underserved older populations more efficiently, especially in rural areas. Mobile clinics can offer an array of services that previously were offered mainly in stationary clinics and hospitals. Some innovations use low-cost laptop computers with sensors to read vital signs and do electrocardiograms, which can send images to trained physicians at other locations and create electronic health records. Low-cost ambulance services (such as Riders for Health)85 provide a means to get rural residents to tertiary care facilities. Mexico's Medicall,86 India's MeraDoctor,87 and the US Healthtap88 are examples of companies that allow people to access doctors’ services by telephone or through the internet, and avoid the need to travel and deal with long and uncertain waiting times. Older people in poorer countries could face major barriers to accessing such interventions, including low literacy and poor access to telephones and the internet. However, many LMICs have much scope to extend the effective use of more straightforward technologies, including interventions to improve detection and management of high blood pressure.
Conclusions
Various behavioural, policy, financial, and other mechanisms—both in the health arena and beyond—could lessen the potential negative effects of population ageing on macroeconomic performance. A top priority should be to invest in good health, because to not do so will hurt economic outcomes in countries at all levels of development.89,90 Establishment of universal access to health care as a central objective of the post-2015 development agenda could be a major step in the direction of safeguarding economic wellbeing.
Matters are complicated by ill health taking on a new and more demanding character, as NCDs add to, and progressively outweigh, the health and economic burdens of infectious disease.91 Additionally, expen diture for health and long-term care at a household level could rise greatly, at least for some families, and with it the risk of impoverishment in countries that do not make reasonable progress toward affordable and universal access to these services.92 Countries will also need to address older-age income security more effectively than they do now. Longer periods of retirement will need more fiscally robust pension systems that can serve the needs of an increasingly large sector of the population.
Population ageing poses some daunting macroeconomic challenges, but many options are available to address them. These options include behavioural responses by individuals, such as higher savings rates and educational attainment in expectation of longer lives, and increased workforce participation from women, immigrants, and older people. Businesses can respond by adjusting human resources practices and adopting technological innovations that meet the needs of older workers. Policy responses might include a delay in retirement age, or finding incentives for delayed retirement; a redesign of pension finance; slowing the growth of benefits; and investing in education to enlarge the effective workforce. These myriad responses can interact and reinforce each other, with longer working lives promoting higher income taxes and receipts, improving both the private and public ability to provide health and long-term care. Additionally, the earlier the policy and institutional reforms are initiated, the smoother will be the macroeconomic adjustment path to accommodating an older population.
The responses set out in this Series paper do not only mitigate the potential economic effect of population ageing, but also tend to enhance the wellbeing of older people, which is an end in its own right. Indeed, many of the necessary responses to population ageing have the potential to benefit people of all ages and might be understood in terms of a more general reorientation of global development toward more efficient, equitable, and sustainable outcomes.
Key messages.
Population ageing raises concerns about the economic security of older people, health spending, labour supply, tax receipts, savings, and growth of income per person
Assertions about the strong negative effects of population ageing on macroeconomic performance are overblown, because countervailing behavioural changes and policy responses are possible
An important and continuing behavioural change—fertility decline—is mitigating the effects of population ageing because it is associated with rising labour force participation by women, increased human capital investment in children, and a decrease in youth dependency
The increasing rate of longevity is sparking another behavioural change—higher rates of savings in expectation of long periods of retirement
Public and private policy responses include a change in retirement policies, emphasis on disease prevention and early detection rather than treatment, a focus on non-communicable diseases, and making better use of technology
Acknowledgments
We thank Elizabeth Cafiero, Alyssa Lubet, Andrew Mason, Roddy McKinnon, Elizabeth Mitgang, Marija Ozolins, Klaus Prettner, and Laura Wallace for their valuable comments and assistance. Daniel Chisholm and Jonathan Weiss also provided comments on an early version of this report.
DEB and LR were funded by a grant from the US National Institute on Aging (# 2P30AG024409-10) supporting Harvard University's Center for the Global Demography of Aging. SC and PK were supported by the US National Institute on Aging through Interagency Agreements (OGHA04034785; YA1323-08-CN-0020; Y1-AG-1005-0) and through research grants R01-AG034479 and R21-AG034263. JPS was supported by NIA grant R37AG025529.
Footnotes
Contributors
All of the authors made substantial contributions to the content and writing of this Series paper.
Declaration of interests
All other authors declare no competing interests.
References
- 1.Bloom DE. 7 billion and counting. Science. 2011;33:562–69. doi: 10.1126/science.1209290. [DOI] [PubMed] [Google Scholar]
- 2.Organisation for Economic Co-operation and Development (OECD) Pensions at a glance 2011: retirement-income systems in OECD countries. Paris: 2011. [Aug 28, 2014]. http://www.oecd-ilibrary.org./finance-and-investment/pensions-at-a-glance-2011_pension_glance-2011-en. [Google Scholar]
- 3.McKee M, Suhrcke M, Lessof S, Figueras J, Duran A, Menabde N. Health systems, health, and wealth: a European perspective. Lancet. 2009;373:349–51. doi: 10.1016/S0140-6736(09)60098-2. [DOI] [PubMed] [Google Scholar]
- 4.Rechel B, Doyle Y, Grundy E, McKee M. How can health systems respond to population ageing? Policy Brief No. 10. Joint Observatory/HEN series on Health Systems and Policy Analysis. Copenhagen: World Health Organization, 2009, on behalf of the European Observatory on Health Systems and Policies.
- 5.Fahy N, McKee M, Busse R, Grundy E. How to meet the challenge of ageing populations. BMJ. 2011;342:d3815. doi: 10.1136/bmj.d3815. [DOI] [PubMed] [Google Scholar]
- 6.Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature. 2008;451:716–19. doi: 10.1038/nature06516. [DOI] [PubMed] [Google Scholar]
- 7.Lee R, Mason A. The price of maturity. Finance Dev. 2011;48:7–11. [PMC free article] [PubMed] [Google Scholar]
- 8.Bloom DE, Canning D, Fink G. Implications of population aging for economic growth. Oxf Rev Econ Policy. 2010;26:583–612. [Google Scholar]
- 9.National Research Council . Aging and the macroeconomy: long-term implications of an older population. National Academies Press; Washington DC: 2012. [PubMed] [Google Scholar]
- 10.Tamiya N, Noguchi H, Nishi A, et al. Population ageing and wellbeing: lessons from Japan's long-term care insurance policy. Lancet. 2011;378:1183–92. doi: 10.1016/S0140-6736(11)61176-8. [DOI] [PubMed] [Google Scholar]
- 11.Kendrick S, Conway M. Demographic and social change: implications for use of acute care services in Scotland. Eur J Population. 2006;22:281–307. [Google Scholar]
- 12.Parliament of the United Kingdom House of Commons Health Committee. [Aug 28, 2014];Social Care. 2012 http://www.publications.parliament.uk/pa/cm201012/cmselect/cmhealth/1538/1538.pdf.
- 13.Lee R, Mason A. Some macroeconomic consequences of global population aging. Demography. 2010;47(suppl):S151–72. doi: 10.1353/dem.2010.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Labour Organization [Aug 26, 2014];ILO Database on Labour Statistics. 2012 http://laborsta.ilo.org/2012.
- 15.Bloom DE, Canning D, Fink G, Finlay J. Fertility, female labor force participation, and the demographic dividend. J Econ Growth. 2009;14:79–101. [Google Scholar]
- 16.Lee R, Mason A. Population aging and the generational economy: a global perspective. Edward Elgar Publishing; Cheltenham: 2011. [Google Scholar]
- 17.World Bank [Sept 2, 2014];World development indicators 2013. http://databank.worldbank.org/data/download/WDI-2013-ebook.pdf.
- 18.Bloom DE, McKinnon R. The design and implementation of public pension systems in developing countries: issues and options. In: Harper S, Hamblin K, editors. International handbook on ageing and public policy. Edward Elgar; Cheltenham: 2014. pp. 108–30. [Google Scholar]
- 19.Tick tock: Brazil's pension system [Aug 28, 2014];The Economist (London) 2012 Mar 24; http://www.economist.com/node/21551093.
- 20.Turner A. Pension challenges in an aging world. Finance Dev. 2006;43:36–39. [Google Scholar]
- 21.Barr N, Diamond P. Reforming pensions: principles, analytical errors and policy directions. ISSR. 2009;62:5–29. [Google Scholar]
- 22.Abegunde D, Stanciole A. WHO Working Paper. World Health Organization; Geneva: 2006. An estimation of the economic impact of chronic noncommunicable diseases in selected countries. [Google Scholar]
- 23.Bloom DE, Cafiero ET, Jané-Llopis E, et al. The global economic burden of non-communicable disease. World Economic Forum; Geneva: 2011. [Google Scholar]
- 24.Bloom DE, Chisholm D, Jane-Llopis E, Prettner K, Stein A, Feigl A. From burden to ‘best buys’: reducing the economic impact of non-communicable diseases in low- and middle-income countries. World Economic Forum; Geneva: 2011. [Google Scholar]
- 25.Mcgrail K, Green B, Barer M, Evans R, Hertzman C, Normand C. Age, costs of acute and long-term care and proximity to death: evidence for 1987–88 and 1994–95 in British Columbia. Age Ageing. 2000;29:249–53. doi: 10.1093/ageing/29.3.249. [DOI] [PubMed] [Google Scholar]
- 26.Hopkins S. Health expenditure comparisons: low, middle and high income countries. Open Health Serv Policy J. 2010;3:111–17. [Google Scholar]
- 27.WHO [Sept 2, 2014];Study on global AGEing and adult health 2012. www.who.int/healthinfo/systems/sage/en/
- 28.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–17. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 29.Tallis R. The ultimate aims of medicine and the future of old age. Asian J Gerontol Geriatr. 2006;1:157–62. [Google Scholar]
- 30.Caughey GE, Vitry AI, Gilbert AL, Roughead EE. Prevalence of comorbidity of chronic diseases in Australia. BMC Public Health. 2008;8:221. doi: 10.1186/1471-2458-8-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dubois C-A, McKee M, Nolte E. Analysing trends, opportunities and challenges. In: Dubois C-A, McKee M, Nolte E, editors. Human resources for health in Europe. Open University Press; Maidenhead: 2006. pp. 15–40. [Google Scholar]
- 32.Hillman K. The changing role of acute-care hospitals. Med J Aust. 1999;170:325–28. [PubMed] [Google Scholar]
- 33.Saltman RB, Figueras J. European health care reform: analysis of current strategies. World Health Organization, Regional Office for Europe; Copenhagen: 1997. [Google Scholar]
- 34.Gruenberg EM. The failures of success. Milbank Mem Fund Q Health Soc. 1977;55:3–24. [PubMed] [Google Scholar]
- 35.Kowal P, Chatterji S, Naidoo N, et al. SAGE collaborators Data resource profile: WHO study on global AGEing and adult health (SAGE). Int J Epidemiol. 2012;41:1639–49. doi: 10.1093/ije/dys210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beard JR, Biggs S, Bloom DE, et al. Global population ageing: peril or promise? World Economic Forum; Geneva: 2012. [Google Scholar]
- 37.Bloom DE, Canning D, Finlay JE. Population aging and economic growth in Asia. In: Ito T, Rose A, editors. The economic consequences of demographic change in east Asia. University of Chicago Press; Chicago: 2010. pp. 61–89. [Google Scholar]
- 38.Lee R, Mason A. Fertility, human capital, and economic growth over the demographic transition. Eur J Popul. 2010;26:159–82. doi: 10.1007/s10680-009-9186-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bloom D, Canning D, Mansfield R, Moore M. Demographic change, social security systems, and savings. J Monet Econ. 2007;54:92–114. doi: 10.1016/j.jmoneco.2006.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Prettner K, Bloom DE, Strulik H. Declining fertility and economic well-being: do education and health ride to the rescue? Labour Econ. 2013;22:70–79. doi: 10.1016/j.labeco.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Basu S, Babiarz K, Ebrahim S, Vellakkal S, Stuckler D, Goldhaber-Fiebert J. Palm oil taxes and cardiovascular disease mortality in India: economic-epidemiologic model. BMJ. 2013;347:f6048. doi: 10.1136/bmj.f6048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nagai M, Kuriyama S, Kakizaki M, et al. Impact of walking on life expectancy and lifetime medical expenditure: the Ohsaki Cohort Study. BMJ Open. 2011;1:e000240. doi: 10.1136/bmjopen-2011-000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lonn E, Bosch J, Teo KK, Pais P, Xavier D, Yusuf S. The polypill in the prevention of cardiovascular diseases: key concepts, current status, challenges, and future directions. Circulation. 2010;122:2078–88. doi: 10.1161/CIRCULATIONAHA.109.873232. [DOI] [PubMed] [Google Scholar]
- 44.Yusuf S, Pais P, Afzal R, et al. Effects of a polypill (Polycap) on risk factors in middle-aged individuals without cardiovascular disease (TIPS): a phase II, double-blind, randomised trial. Lancet. 2009;373:1341–51. doi: 10.1016/S0140-6736(09)60611-5. [DOI] [PubMed] [Google Scholar]
- 45.Soliman EZ, Mendis S, Dissanayake WP, et al. A polypill for primary prevention of cardiovascular disease: a feasibility study of the World Health Organization. Trials. 2011;12:3. doi: 10.1186/1745-6215-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.PILL Collaborative Group An international randomised placebo-controlled trial of a four-component combination pill (polypill) in people with raised cardiovascular risk. PLoS One. 2011;6:e19857. doi: 10.1371/journal.pone.0019857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oxley H. OECD Health Working Papers 42. OECD; Paris: 2009. Policies for healthy ageing: an overview. [Google Scholar]
- 48.Nutbeam D, Kickbusch I. Advancing health literacy: a global challenge for the 21st century. Health Promot Int. 2000;15:183–84. [Google Scholar]
- 49.Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–208. doi: 10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Daviglus ML, Liu K, Pirzada A, et al. Cardiovascular risk profile earlier in life and Medicare costs in the last year of life. Arch Intern Med. 2005;165:1028–34. doi: 10.1001/archinte.165.9.1028. [DOI] [PubMed] [Google Scholar]
- 51.Gandjour A. Aging diseases–do they prevent preventive health care from saving costs?. Health Econ. 2009;18:355–62. doi: 10.1002/hec.1370. [DOI] [PubMed] [Google Scholar]
- 52.Gandjour A, Lauterbach K. Does prevention save costs? Considering deferral of the expensive last year of life. J Health Econ. 2005;24:715–24. doi: 10.1016/j.jhealeco.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 53.Doyle Y, McKee M, Rechel B, Grundy E. Meeting the challenge of population ageing. BMJ. 2009;337:892–94. doi: 10.1136/bmj.b3926. [DOI] [PubMed] [Google Scholar]
- 54.Do R, Xie C, Zhang X, et al. The effect of chromosome 9p21 variants on cardiovascular disease may be modified by dietary intake: evidence from a case/control and a prospective study. PLoS Med. 2011;9:e1001106. doi: 10.1371/journal.pmed.1001106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marín GH, Homar C, Niedfeld G, Matcovick G, Mamonde M, Grupo Interdisciplinario para la Salud (GIS) Evaluation of the state intervention project to improve quality of life and reduce the complications associated with aging: “add health to your years”. Gac Sanit. 2009;23:272–77. doi: 10.1016/j.gaceta.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 56.Shi Z, Hu X, Yuan B, et al. Vegetable-rich food pattern is related to obesity in China. IntJ Obes. 2008;32:975–84. doi: 10.1038/ijo.2008.21. [DOI] [PubMed] [Google Scholar]
- 57.Chakravarty EF, Hubert HB, Krishnan E, Bruce BB, Lingala VB, Fries JF. Lifestyle risk factors predict disability and death in healthy aging adults. Am J Med. 2012;125:190–97. doi: 10.1016/j.amjmed.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.He FJ, Pombo-Rodrigues S, MacGregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014;4:e004549. doi: 10.1136/bmjopen-2013-004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.WHO . Global status report on noncommunicable diseases, 2010–2011. World Health Organization; Geneva, Switzerland: 2011. [Google Scholar]
- 60.Beaulieu N, Bloom DE, Bloom LR, Stein R. Breakaway: the global burden of cancer–challenges and opportunities. Economist Intelligence Unit; New York: Aug, 2009. [Sept 2, 2014]. http://graphics.eiu.com/upload/eb/EIU_LIVESTRONG_Global_Cancer_Burden.pdf. [Google Scholar]
- 61.Gakidou E, Nordhagen S, Obermeyer Z. Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PLoS Med. 2008;5:e132. doi: 10.1371/journal.pmed.0050132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chow C, Teo K, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–68. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 63.Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low and middle income countries: prevalence, awareness and control. Int J Epidemiol. 2014;43:116–28. doi: 10.1093/ije/dyt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu X, Tang S, Yu B, et al. Can rural health insurance improve equity in health care utilization? A comparison between China and Viet Nam. IntJ Equity Health. 2012;11:10. doi: 10.1186/1475-9276-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Strauss J, Hong H, Lei X, Li L, Park A, Yang L, et al. Health care and insurance among the elderly in China: evidence from the CHARLS Pilot. In: Smith James P, Majmundar Malay., editors. Aging in Asia. Findings from new and emerging data initiatives. National Academies Press (US); Washington DC: 2012. pp. 342–70. [PubMed] [Google Scholar]
- 66.Coyte PC, Goodwin N, Laporte A. How can the settings used to provide care to older people be balanced? World Health Organization; Copenhagen: 2008. [Google Scholar]
- 67.Häkkinen U, Martikainen P, Noro A, Nihtilä E, Peltola M. Aging, health expenditure, proximity of death and income in Finland. Health Econ Policy Law. 2008;3:165–95. doi: 10.1017/S174413310800443X. [DOI] [PubMed] [Google Scholar]
- 68.Fernández JL, Forder J, Trukeschitz B, Rokosová M, McDaid D. How can European States design efficient, equitable and sustainable funding systems for long-term care for older people? World Health Organization on behalf of the European Observatory on Health Systems and Policies, Joint HEN/European Observatory on Health Systems and Policies Policy Brief; Copenhagen: 2009. [Google Scholar]
- 69.Redondo N, Lloyd-Sherlock P. Institutional care for older people in developing countries: Repressing rights or promoting autonomy? The case of Buenos Aires, Argentina. J Pop Ageing. 2010;2:41–56. [Google Scholar]
- 70.Nolte E, McKee M. A health system perspective. Open University Press; Maidenhead: 2008. Caring for people with chronic conditions. [Google Scholar]
- 71.UN . Guiding framework and toolkit for practitioners and policy makers. United Nations Department of Economic and Social Affairs; New York: 2008. Madrid international plan of action on ageing 2002. [Google Scholar]
- 72.Ryan D, Wilden J. Modern medical education: meeting the demands of an ageing population. In: Beard JR, Biggs S, Bloom DE, et al., editors. Global population ageing: peril or promise? World Economic Forum; Geneva: 2012. [Sept 2, 2014]. pp. 74–77. http://www3.weforum.org/docs/WEF_GAC_GlobalPopulationAgeing_Report_2012.pdf. [Google Scholar]
- 73.WHO . Global survey on geriatrics in the medical curriculum. World Health Organization; Geneva: 2002. [Google Scholar]
- 74.O'Neill D. Building capacity in gerontology and geriatric medicine in primary and secondary care is part of the solution. BMJ. 2011;342:d3815. [Google Scholar]
- 75.Ellis G, Whitehead MA, O'Neill D, Langhorne P, Robinson D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2011;7:CD006211. doi: 10.1002/14651858.CD006211.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stuck AE, Illiffe S. Comprehensive geriatric assessment for older adults. BMJ. 2011;343:d6799. doi: 10.1136/bmj.d6799. [DOI] [PubMed] [Google Scholar]
- 77.Economist Intelligence Unit . Health care strategies for an ageing society. The Economist; London: 2009. Addressing the lack of expertise. pp. 20–22. [Google Scholar]
- 78.Lee R, Mason A. Fertility, human capital, and economic growth over the demographic transition. Eur J Popul. 2010;26:159–182. doi: 10.1007/s10680-009-9186-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pritchett L. Bilateral guest worker agreements: a win-win solution for rich countries and poor people in the developing world. Center for Global Development; 2007. [Sept 2, 2014]. http://www.cgdev.org/publication/bilateral-guest-worker-agreements-win-win-solution-rich-countries-and-poor-people. [Google Scholar]
- 80.Zlotnik H. International migration and population ageing. In: Beard JR, Biggs S, Bloom DE, et al., editors. Global population ageing: peril or promise? Vol. 2012. World Economic Forum; Geneva: [Sept 2, 2014]. pp. 97–102. http://www3.weforum.org/docs/WEF_GAC_GlobalPopulationAgeing_Report_2012.pdf. [Google Scholar]
- 81.The Norwegian Labour and Welfare Service . National Insurance Retirement Pensions. Norwegian Labour and Welfare Service; Oslo: 2011. [Google Scholar]
- 82.Aaron H, Burtless G, editors. Closing the deficit: how much can later retirement help? The Brookings Institution; Washington, DC: 2013. [Google Scholar]
- 83.Zamarro G, Meijer E, Fernandes M. Labor force participation and retirement. In: Borsch-Supan A, et al., editors. Health, Ageing, and Retirement in Europe (2004–2007)–starting the longitudinal dimension. MEA; Mannheim: [Google Scholar]
- 84.Loch CH, Sting FJ, Bauer N, Mauermann H. How BMW Is defusing the demographic time bomb. Harvard Business Review (Boston) 2010 Mar;:1–5. [PubMed] [Google Scholar]
- 85. [Sept 2, 2014];Riders for Health. 2012 http://www.riders.org/
- 86. [Sept 2, 2014];Medicall. 2012 http://www.medicallhome.com.
- 87. [Sept 2, 2014];MeraDoctor. 2012 http://meradoctor.com.
- 88. [Sept 2, 2014];Healthtap. 2014 http://www.healthtap.com.
- 89.Suhrcke M, McKee M, Stuckler D, Sauto Arce R, Tsolova S, Mortensen J. The contribution of health to the economy in the European Union. Public Health. 2006;120:994–1001. doi: 10.1016/j.puhe.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 90.Bloom DE, Canning D. The health and wealth of nations. Science. 2000;287:1207–09. doi: 10.1126/science.287.5456.1207. [DOI] [PubMed] [Google Scholar]
- 91.Egger G. Health and economic growth: medicine, environment and economics at the crossroads. Am J Prev Med. 2009;37:78–83. doi: 10.1016/j.amepre.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 92.The Lancet. Striving for universal health coverage. 2010;376:1799. doi: 10.1016/S0140-6736(10)62148-4. [DOI] [PubMed] [Google Scholar]