Abstract
Objective
To compare self-reported and measured energy intake in weight-restored patients with anorexia nervosa (AN), weight-stable obese individuals (OB), and normal weight controls (NC).
Method
Forty participants (18 AN, 10 OB, and 12 NC) in a laboratory meal study simultaneously completed a prospective food record.
Results
AN patients significantly (p = .018) over-reported energy intake (16%, 50 kcal) and Bland-Altman (B-A) analysis indicated bias toward over-reporting at increasing levels of intake. OB participants significantly (p = .016) under-reported intake (19%, 160 kcal) and B-A analysis indicated bias toward under-reporting at increasing levels of intake. In NC participants, NS (p = .752) difference between reported and measured intake was found and B-A analysis indicated good agreement between methods at all intake levels.
Discussion
Self-reported intake should be cautiously interpreted in AN and OB. Future studies are warranted to determine if over-reporting is related to poor outcome and relapse in AN, or under-reporting interferes with weight loss efforts in OB.
Keywords: anorexia nervosa, obesity, food record, caloric intake
Introduction
Food records and dietary recalls are commonly used to assess the energy intake of individuals, for both clinical and research purposes. A potential source of error in the assessment of energy intake is misreporting, both under and over. Methods like the doubly labeled water technique and the Gold-berg cut-off1 are often used to identify the misreporting of energy intake; however, the direct comparison of reported intake to observed and measured intake may be the most discriminating and informative approach.
Studies validating the accuracy of foods records and dietary recalls against observed and measured intake suggest that normal weight, overweight, and obese adults either under-report,1-7 over-report,5,8 or accurately report5,9,10 their measured energy intake. It has been suggested that patients with anorexia nervosa (AN) provide more accurate self-reports of food and energy intake.11-13 Indeed, numerous studies have reported the results of 24-h recalls12-15 and food records15-22 in patients with AN. However, to our knowledge, only two studies have been conducted to validate self-report measures of food intake against observed and measured food intake in patients with AN15,23 and both were conducted at low body weight, before weight restoration.
The objectives of the study were: (1) to compare self-reported energy intake, determined from a prospective food record, to observed and measured energy intake in three groups of study participants: weight-restored patients with AN, healthy, normal weight controls (NC), and weight-stable obese individuals (OB); (2) to determine the reporting within and among participant groups.
Method
Subjects were 40 AN, OB, and NC participants in a laboratory meal study conducted by the Eating Disorders Research Unit at the New York State Psychiatric Institute (NYSPI), Columbia University Medical Center, between January 2008 and October 2010. The NYSPI/Columbia University, Department of Psychiatry Institutional Review Board approved this study, and all participants were provided informed consent before study entry.
Patients with AN were females between the ages of 18–45 years meeting Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV)24 criteria for AN except amenorrhea.25 Patients were excluded if they had comorbid substance abuse or significant DSM-IV Axis I psychiatric disorders other than major depression. All were free from medications, except acetaminophen and ibuprofen, for a minimum of 2 weeks before study. Patients were hospitalized on the inpatient Eating Disorder Service at the NYSPI. Treatment consisted of a structured behavioral program aimed at normalizing body weight and eating patterns.26 The meal study was conducted after restoring body weight to a minimum of 90% of ideal body weight, as defined by the Metropolitan Life actuarial tables27; this weight is approximately equal to a body mass index (BMI in kg/m2) of 20. NC (BMI 19–21 kg/m2) were healthy females between the ages of 18–45 years who were matched to AN participants on age, ethnicity, and race. Obese individuals (BMI 30–40 kg/m2) were male and female participants between the ages of 18–60 years who participated in a placebo-controlled study of the effects of sibutramine on eating behavior.
All meal studies were conducted on the Biological Studies Unit at the NYSPI. On the morning of the study (~8 am), AN and NC participants ate a standardized breakfast of ~300 kcal; OB participants consumed 16 fl. oz. of Optifast 800 (Nestle Nutrition) as their standardized breakfast. Thereafter, all participants refrained from eating and drinking, except water, until the test meal at ~1 pm.
The laboratory meal consisted of 25 food items placed on a table28: grilled chicken, fried chicken, macaroni and cheese, tuna fish, pickles, French fries, tossed salad, chocolate sandwich cookies, chocolate bar, vanilla ice cream, donuts, popcorn, fruit salad, whole wheat bread, white bread slices, butter, mustard, mayonnaise, ketchup, Italian salad dressing, salt, pepper, iced tea, bottled water, and diet cola. Participants were instructed: “This is your lunch for the day. Eat as much or as little as you would like.” Participants, alone in the room while consuming the meal, were continuously monitored via a one-way, closed circuit TV. Participants had up to 60 min to eat their meal. Food and beverage items were weighed before and after the test meal using an Acculab 7200 electronic digital balance (readability 0.1g) to quantify observed intake.
Participants completed a prospective 4-day food record that included the observed laboratory test meal. A trained research assistant provided detailed verbal and written instructions on estimation of food portions, and a pictorial. A registered dietitian reviewed completed records for accuracy and completeness. Self-reported intake at the laboratory test meal was determined from the food record.
Observed kcal intake and self-reported kcal intake were determined by nutrient analysis software (University of Minnesota Nutrition Data System for Research, Regents of the University of Minnesota, Nutrition Coordinating Center, version 2009). Outcome measures included self-reported kcal intake (reported kcal), observed kcal intake (observed kcal), the difference between reported and observed kcal intake (reported kcal – observed kcal), and reported kcal intake as a percent of observed caloric intake (reported kcal/observed kcal × 100).
Statistical analyses were performed using SPSS, version 18.0 (Chicago, IL) and significance was set at the p < .05 level. Descriptive statistics were used to determine the mean (±SD) age and BMI (in kg/m2) of participant groups. The paired samples t-test was used to compare self-reported and observed kcal intake within the AN, NC, and OB groups. One-way analysis of variance (ANOVA) was used to compare differences among participant groups in BMI, the difference between reported and observed kcal intake, and percent of kcal that were over-reported or under-reported. The Tukey Honestly Significant Difference (HSD) test was planned for all post hoc analyses; however, if Levene’s test of homogeneity of variances was found to be significant (p < .05), then the Welch F-ratio and Games-Howell post hoc analyses were alternatively reported. Bland-Altman (B-A) plots29 were constructed to determine agreement between the food record (reported intake) and the laboratory test meal (observed intake) in all participant groups. As described by Bland and Altman, the limits of agreement were set as two standard deviations of the difference above and below the mean difference. A regression line was fitted to better visualize the magnitude and directionality of instrument bias.
Results
All AN (n = 18) and NC (n = 12) participants were female and Caucasian. Obese participants (n = 10) included two males and eight females; four were African American, two were Hispanic, and four were Caucasian.
The mean age was 27.1 ± 8.5 years (range: 17–44 years) for AN patients, 24.1 ± 3.7 years (range: 19–32) for controls, and 37.3 ± 9.6 years (range: 21–54) for OB individuals. One-way ANOVA was used to compare age across participant groups. The assumption of homogeneity of variance was violated, and the Welch-F-ratio is alternatively reported. Age differed significantly among the participant groups (F (2, 19.403) = 8.431, p = .002). Results of Games-Howell post hoc analyses found no statistically significant difference in the mean ages of AN patients and healthy controls (p = .406). Obese individuals were, however, significantly older than the control (p = .004) and AN (p = .03) participants.
The mean BMI was 19.7 ± 0.9 for weight-restored AN patients, 20.3 ± 0.9 for control subjects, and 33.9 ± 2.4 for obese participants. One-way ANOVA was used to compare BMI across participant groups. Once again, the assumption of homogeneity of variance was violated and the Welch-F-ratio is reported. The effect of diagnosis on BMI was significant (F (2, 18.09) = 158.639, p = .000). Games-Howell post hoc analyses indicated that BMI in the weight-restored AN group and the NC group was significantly different from that of the OB group (p = .00 and p = .00, respectively); however, no statistically significant difference in BMI was observed between weight-restored AN and NC groups (p = .198).
Reported versus observed kcal intakes, and their mean difference, are summarized in Table 1. In the AN group, self-reported kcal intake ranged from 4.7 to 999.2 kcal, whereas observed kcal intake ranged from 2.7 to 830.2 kcal; the food record significantly (p = .018) over-reported actual kcal intake by a mean of 50 kcal (116%). Self-reported kcal intake in the NC group ranged from 352.6 to 1296.9 kcal, whereas observed kcal intake ranged from 355.2 to 1110.5 kcal. The food record over-reported actual kcal intake by a mean of 20 kcal (106%), but this was not statistically significant (p = .752). Lastly, self-reported kcal intake in OB participants ranged from 221.2 to 1174.5 kcal, whereas observed kcal intake ranged from 185.8 to 1160.6 kcal. The food record significantly (p = .016) under-reported actual kcal intake by a mean of 160 kcal (81%).
TABLE 1. Reported versus observed energy (kcal) intake.
| Reported (kcal) |
Observed (kcal) |
Difference Between Reported and Observed (kcal)a |
Percent kcal over-reported or under-reportedb |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group | n | Mean | SD | Mean | SD | p c | Mean | SD | Mean | SD |
| AN | 18 | 491 | 290 | 440 | 254 | .018 | 50 | 81 | 116 | 27 |
| NC | 12 | 738 | 310 | 718 | 255 | .752 | 20 | 210 | 106 | 40 |
| OB | 10 | 542 | 269 | 702 | 309 | .016 | −160 | 172 | 81 | 21 |
One-way ANOVA indicates a significant between-group difference: Welch-F (2, 15.843) = 6.419, p = .009; Games-Howell post hoc analyses: Significant difference between AN and OB groups (p = .009); NS difference between AN and NC groups (p = .882); NS difference between NC and OB groups (p = .094).
One-way ANOVA indicates a significant between-group difference: F (2, 37) = 4.184, p = .023; Tukey post hoc analyses: Significant difference between AN and OB groups (p = .018); NS difference between AN and NC groups (p = .678); NS difference between NC and OB groups (p = .148).
Paired samples t-test between reported kcal and observed kcal.
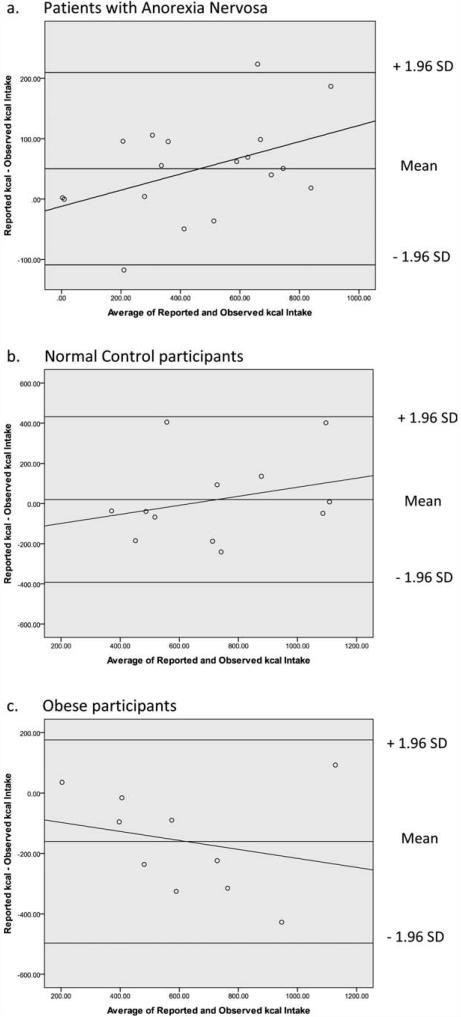
Bland-Altman plots (Fig. 1) suggest a systematic difference between self-reported and observed kcal intake in AN and OB participants. At increasing levels of kcal intake, AN patients were biased towards over-reporting and OB participants were biased toward under-reporting. In contrast, there was no systematic difference between self-reported and observed kcal in NC participants, and good agreement between the methods was observed at kcal intake levels.
FIGURE 1.
Bland-Altman analysis of self-reported kcal intake (food record) and observed kcal intake (laboratory meal) in (a) anorexia nervosa (AN), (b) normal control (NC), and (c) obese (OB) participants. The food record over-reported kcal intake in the AN and NC group, but under-reported kcal intake in the OB group. Bias toward over-reporting at increasing levels of kcal intake was found in the AN group, whereas bias toward under-reporting at increasing levels of kcal intake was found in the OB group; no systematic bias was observed in the NC group.
Discussion
This study is the first to compare self-reported energy intake, obtained from a food record, to observed and measured energy intake in weight restored patients with AN. Our sample of 18 AN patients significantly over-reported energy intake by 16%, and B-A analysis indicated bias toward over-reporting at increasing levels of kcal intake. Two prior studies have compared self-reported intake to observed intake in low weight AN patients, each with opposite outcomes. In a study of 30 low-weight AN patients, Hadigan et al.,23 compared a 1-month Burke diet history with a 1-day observed intake and found that AN patients significantly over-estimated energy intake; the percentage of over-reporting was not provided. It is noteworthy that observed food intake was calculated by estimating the percent of portions consumed for each item, rather than by the direct measurement, i.e., weighing of foods consumed. In contrast, Van der Ster Wallin et al.15 compared a 24-h recall of food intake with that which was both observed and measured in 15 low weight AN patients. No significant difference was found and the researchers concluded that the 24-h recall was a valid method for the assessment of food intake in patients with AN.
In contrast to the AN patients, our 10 OB participants significantly under-reported their energy intake by 19%, and B-A analysis indicated bias toward under-reporting at increasing levels of kcal intake. These results support the findings of Macdiarmid and Blundel3 who observed that under-reporting was more common among obese individuals and the magnitude of under-reporting varied as a direct function of the quantity of food consumed. In general, studies suggest a positive association between low-energy reporting and high BMI.7 Similar to our findings, Lichtman et al.6 reported that, 24-h after an observed and measured laboratory test meal, 10 obese adults under-reported their intake by ~20%. Likewise, Poppitt et al.2 found that 18 obese adult females under-reported a 1-day observed and measured energy intake by 12.4%. Conversely, two studies found that obese individuals accurately self-reported their energy intake. Conway et al.10 found no significant difference between actual and recalled energy intakes in 42 adult males, and concluded that obese men recalled food intake as accurately as nonobese men. Similarly, Conway et al.9 studied recalled versus actual food intake in 49 adult females and found that while normal weight and overweight women significantly over-reported energy intake, obese women accurately self-reported energy intake.
An accurate estimate of energy intake is typically with 10% of estimated values.8 In our 12 NC participants, reported kcal intake was 106% of observed intake, and B-A analysis found good agreement between these methods. It is noteworthy, however, that prior studies provide no clear-cut consensus on the accuracy of self-reported energy intake in normal weight adults. Conway et al.9 found significant over-reporting of energy intake in 14 normal weight women. Similarly, Myers et al.5 found significant energy over-reporting in a sample of 19 female college students. In contrast, Poppitt et al.2 observed that 15 normal weight adult females significantly under-reported their energy intake by 12.6%, and Hadigan et al.23 found that 28 normal weight adult females significantly under-reported their energy intake by 24.1%.
This study is unique in that it uses that same methodological approach in AN, OB, and NC participants. Nevertheless, there are several important limitations to this study. First and foremost, the sample size was small and results should be interpreted with caution. Second, accuracy was determined from one meal only and a study that included several meals, or multiple study days, may have yielded a different outcome. Third, the ability to accurately self-report food intake may differ in laboratory versus naturalistic settings, and results may have been influenced by the provision of buffet-style versus individual food portions. Finally, this study was a secondary analysis of data from two separate studies. Although food records were included in the methods of both studies, the decision to validate these records against the laboratory test meal was made post hoc.
Conclusion
Accurate determination of food and energy intake is central to the nutritional assessment process, the formulation of dietary recommendations and prescriptions, and the routine monitoring of interventions in individuals with AN and obesity. This study contributes to a relatively small body of literature that addresses the accuracy of commonly used self-report diet measures, like food records, in normal weight and obese individuals. From a clinical perspective, our findings suggest that food records should be interpreted judiciously in obese individuals; future studies that assess the degree to which under-reporting interferes with successful weight loss efforts are warranted. This study is the first to report on the accuracy of self-reported energy intake in weight-restored AN patients. Additional studies are needed to replicate these findings, and to determine if energy over-reporting is related to clinical outcome and risk for relapse after weight restoration in patients with AN.
Acknowledgments
Supported by the Irving Institute for Clinical and Translational Research; Clinical Trials Pilot Award; the Irving Scholars Program at Columbia University; AstraZeneca.
Footnotes
Author contributions: Designed research: Schebendach and Mayer; Conducted research: Schebendach and Mayer; Analyzed data or performed statistical analysis: Schebendach, Porter, and Wolper; Wrote manuscript: Schebendach and Mayer; Significant advice or consultation: Walsh; Critical revision of manuscript for important intellectual content: Walsh; Primary responsibility for final content: Schebendach and Mayer; We also thank the patients and staff of the General Clinical Research Unit, including Mary Bongiovi, Dan Richter, and Arlene Bolson without whose participation and support this study could not have happened.
References
- 1.Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van’t Veer PS. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009;101:S73–S85. doi: 10.1017/S0007114509990602. [DOI] [PubMed] [Google Scholar]
- 2.Poppitt SD, Swann D, Black AE, Prentice AM. Assessment of selective under-reporting of food intake by both obese and non-obese women in a metabolic facility. Int J Obes Relat Metab Disord. 1998;22:303–311. doi: 10.1038/sj.ijo.0800584. [DOI] [PubMed] [Google Scholar]
- 3.Macdiarmid J, Blundell Assessing dietary intake: Who, what and why of under-reporting. Nutr Res Rev. 1998;11:231–253. doi: 10.1079/NRR19980017. [DOI] [PubMed] [Google Scholar]
- 4.Hallfrisch J, Steele P, Cohen L. Comparison of seven-day diet record with measured food intake of twenty-four subjects. Nutr Res. 1982;2:263–273. [Google Scholar]
- 5.Myers RJ, Klesges RC, Eck LH, Hanson CL, Klem ML. Accuracy of self-reports of food intake in obese and normal-weight individuals: Effects of obesity on self-reports of dietary intake in adult females. Am J Clin Nutr. 1988;48:1248–1251. doi: 10.1093/ajcn/48.5.1248. [DOI] [PubMed] [Google Scholar]
- 6.Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, Weisel H, Heshka S, Mattews DE, Heymsfield SB. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Eng J Med. 1992;327:1893–1898. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 7.Livingstone MBE, Black AE. Markers of the validity of reported energy intake. J Nutr. 2003;133:895S–920S. doi: 10.1093/jn/133.3.895S. [DOI] [PubMed] [Google Scholar]
- 8.Ard JD, Desmond RA, Allison DB, Conway JM. Dietary restraint and disinhibition do not affect accuracy of 24-hour recall in a multiethnic population. J Am Diet Assoc. 2006;106:434–437. doi: 10.1016/j.jada.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003;77:1171–1178. doi: 10.1093/ajcn/77.5.1171. [DOI] [PubMed] [Google Scholar]
- 10.Conway JM, Ingwersen LA, Moshfegh AJ. Accuracy of dietary recall using the USDA five-step multiple-pass method in men: An observational validation study. J Am Diet Assoc. 2004;104:595–603. doi: 10.1016/j.jada.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Russell G. The present status of anorexia nervosa. Psycholl Med. 1978;7:363. doi: 10.1017/s0033291700004323. [DOI] [PubMed] [Google Scholar]
- 12.Beaumont PJ, Chambers TL, Rouse L, Abraham SF. The diet composition and nutritional knowledge of patients with anorexia nervosa. J Hum Nutr. 1981;35:265–273. doi: 10.3109/09637488109143052. [DOI] [PubMed] [Google Scholar]
- 13.Huse DM, Lucas AR. Dietary patterns in anorexia nervosa. Am J Clin Nutr. 1984;40:251–254. doi: 10.1093/ajcn/40.2.251. [DOI] [PubMed] [Google Scholar]
- 14.Thibault L, Roberge AG. The nutritional status of subjects with anorexia nervosa. Int J Vitam Nutr Res. 1987;57:447–452. [PubMed] [Google Scholar]
- 15.van der Ster Wallin G, Norring C, Lennernas MA, Holmgren S. Food selection in anorectics and bulimics: Food items, nutrient content and nutrient density. J Am Coll Nutr. 1995;14:271–277. doi: 10.1080/07315724.1995.10718507. [DOI] [PubMed] [Google Scholar]
- 16.Windauer U, Lennerts W, Talbot P, Touyz SW, Beumont PJ. How well are ‘cured’ anorexia nervosa patients? An investigation of 16 weight-recovered anorexic patients. Br J Psychiatry. 1993;163:195–200. doi: 10.1192/bjp.163.2.195. [DOI] [PubMed] [Google Scholar]
- 17.van der Ster Wallin G, Norring C, Holmgren S. Selective dieting patterns among anorectics and bulimics at the onset of eating disorder. Eur Eat Disord Rev. 1994;2:221–232. [Google Scholar]
- 18.Nova E, Varela P, López-Vidriero I, Toro O, Ceñal MJ, Casas J, Marcos A. A one-year follow-up study in anorexia nervosa. Dietary pattern and anthropometrical evolution. Eur J Clin Nutr. 2001;55:547–554. doi: 10.1038/sj.ejcn.1601181. [DOI] [PubMed] [Google Scholar]
- 19.Affenito SG, Dohm FA, Crawford PB, Daniels SR, Striegel-Moore RH. Macronutrient intake in anorexia nervosa: The National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 2002;141:701–705. doi: 10.1067/mpd.2002.129840. [DOI] [PubMed] [Google Scholar]
- 20.Misra M, Tsai P, Anderson EJ, Hubbard JL, Gallagher K, Soyka LA, Miller KK, Herzog DB, Klibanski A. Nutrient intake in community-dwelling adolescent girls with anorexia nervosa and in healthy adolescents. Am J Clin Nutr. 2006;84:698–706. doi: 10.1093/ajcn/84.4.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schebendach JE, Mayer LES, Devlin MJ, Attia E, Contento IR, Wolf RL, Walsh BT. Dietary energy density and diet variety as predictors of outcome in anorexia nervosa. Am J Clin Nutr. 2008;87:810–816. doi: 10.1093/ajcn/87.4.810. [DOI] [PubMed] [Google Scholar]
- 22.Dellava JE, Hamer RM, Kanodia A, Reyes-Rodríguez ML, Bulik CM. Diet and physical activity in women recovered from anorexia nervosa: A pilot study. Int J Eat Disord. 2011;44:376–382. doi: 10.1002/eat.20865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hadigan CM, Anderson EJ, Miller KK, Hubbard JL, Herzog DB, Klibanski A, Grinspoon SK. Assessment of macronutrient and micronutrient intake in women with anorexia nervosa. Int J Eat Disord. 2000;28:284–292. doi: 10.1002/1098-108x(200011)28:3<284::aid-eat5>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association, editor. Diagnostic and Statistical Manual of Mental Disorders. 4th ed APA Press; Washington, D.C.: 1994. [Google Scholar]
- 25.Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? Intl J Eat Disord. 2009;42:581–589. doi: 10.1002/eat.20720. [DOI] [PubMed] [Google Scholar]
- 26.Attia E, Walsh BT. Behavioral management for anorexia nervosa. N Eng J Med. 2009;360:500–506. doi: 10.1056/NEJMct0805569. [DOI] [PubMed] [Google Scholar]
- 27.Metropolitan Life Insurance Co . New weight standards for men and women. Vol. 40. Stat Bull Metrop Life Insur Co; 1959. pp. 1–11. [Google Scholar]
- 28.Mayer LE, Schebendach J, Bodell LP, Shingleton RM, Walsh BT. Eating behavior in anorexia nervosa: Before and after treatment. Int J Eat Disord. 2011 Apr 14; doi: 10.1002/eat.20924. Epub ahead of print (DOI:10.1002/eat.20924) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]