Abstract
A blend of three monoclonal antibodies has completely protected monkeys against a lethal dose of Ebola virus. Unlike other post-infection therapies, the treatment works even at advanced stages of the disease.
The filoviruses known as Ebola virus and Marburg virus are among the most deadly of pathogens, with fatality rates of up to 90% (ref. 1). Early this year, a new strain of the Zaire species of Ebola virus emerged2 in the West African country of Guinea and quickly spread to Liberia, Sierra Leone and Nigeria. The outbreak persists despite the best efforts of local and international authorities, and is now the largest filovirus outbreak on record, with no end in sight. There are no licensed vaccines or post-exposure treatments against Ebola, so moving the most promising interventions forward is a matter of utmost urgency. On page 47 of this issue, Qiu et al.3 report that rhesus monkeys can be completely protected from lethal Ebola infection using ZMapp — a blend of three monoclonal antibodies. Crucially, the treatment protected monkeys even when it was administered as late as 5 days after exposure to the virus, at a time when the animals were severely ill.
Since the discovery of Ebola virus (Fig. 1) in 1976, researchers have been actively developing treatments to combat infection. Studies over the past decade have found that modulators of blood coagulation4,5, an antisense oligonucleotide called AVI-6002 (ref. 6) and a vaccine7 based on vesicular stomatitis virus (VSV) all afforded partial protection of monkeys against Ebola when administered within an hour of virus exposure. The VSV-based vaccine was used in 2009 to treat a laboratory worker in Germany shortly after she was accidentally pricked with a needle possibly contaminated by an Ebola-infected animal8. The worker survived, but it is unclear whether this was because she had not been exposed to Ebola or because the vaccine protected her.
Figure 1.
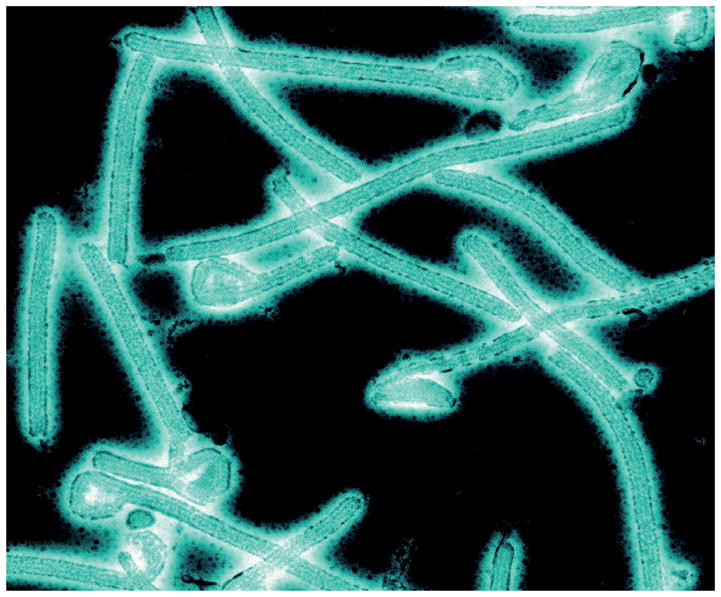
The Ebola virus.
Subsequent advances have been made in developing treatments that can completely protect monkeys against Ebola. These include small ‘interfering’ RNAs (known as TKM-Ebola9) and various combinations of antibodies10–12. But these treatments need to be administered within 2 days of exposure to the virus. So although these approaches were highly important and can be used to treat known exposures, the need for treatments that protect at later times after infection was paramount.
Further development and improvement of the antibody-based strategies led to a cocktail of monoclonal antibodies13 that protected 43% of monkeys when given as late as 5 days after Ebola exposure — a time at which the clinical signs of disease are apparent. Another therapy that combines monoclonal antibodies with interferon-α (a protein that stimulates an antiviral response) provides almost complete protection of macaques when given 3 days after exposure14, at which point the virus can be detected but clinical signs are only just beginning to be seen in some animals.
Qiu et al. now report ZMapp, an antibody therapy that does not require interferon-α, and which was developed by two collaborating teams of researchers who had worked on some of the previously reported antibody treatments. ZMapp was made by testing different combinations of chimaeric monoclonal antibodies (in which fragments of human antibodies are attached to antibody fragments from mice). The optimal formulation contains two antibodies from a previously reported blend14 and a third from a different cocktail13.
To test the therapy, Qiu et al. administered a lethal dose of Ebola virus to three groups of six animals, and then treated them with three doses of ZMapp. The first group received therapy at 3, 6 and 9 days post-infection; the second group at 4, 7 and 10 days; and the third group at 5, 8 and 11 days. Remarkably, all the animals survived, and were found to have undetectable viral loads by 21 days after infection. It should be noted that the authors used the Kikwit variant of the virus in these experiments, because the Guinean strain from the current West African outbreak was not available in time for this part of their study. However, they went on to show that ZMapp inhibits replication of the Guinean strain in cell culture.
The development of ZMapp and its success in treating monkeys at an advanced stage of Ebola infection is a monumental achievement. On this basis, the treatment has been used in the current Ebola outbreak to treat several patients on compassionate grounds15. Of these, two US health-care workers have recovered — but whether ZMapp had any effect is unknown, because at the time of writing, about 45% of patients in this outbreak survive without treatment16. As of 26 August, two other patients treated with ZMapp have not survived, but this might be because the treatment was initiated too late in the course of the disease.
The diversity of strains and species of Ebola and Marburg viruses remain an obstacle for all candidate treatments. Lethal disease in humans is caused by three different species of Ebola virus (Sudan, Bundibugyo and Zaire) and two genetically distinct lineages of Marburg virus. Treatments that protect against one species of Ebola — Zaire, in the case of ZMapp — will probably not protect against a different species of the virus, and might not protect against a different strain within a species.
Although the need for treatments for filovirus infections is unquestionable, the most effective way to manage and control future outbreaks might be through preventive vaccines, some of which have been tailored to protect against multiple species and strains. During outbreaks, single-injection vaccines are needed to ensure rapid use and protection. At least five preventive vaccines have been shown to completely protect monkeys against Ebola and Marburg infection17. But only VSV-based vaccines have been reported to completely protect monkeys against Ebola (Zaire) virus after a single injection18 — notably, the wild-type virus, rather than a cultured variant that has also been used in research, and which produces slower disease progression in macaques.
Antibody therapies and several other strategies mentioned here should ultimately be included in an arsenal of interventions for controlling future Ebola outbreaks. Although ZMapp in particular has been administered for compassionate use, the next crucial step will be to formally assess its safety and effectiveness. Testing the latter is clearly difficult, because intentional infection of human subjects in clinical trials is not possible. US regulations, however, could allow the treatment to be licensed for widespread use on the basis of safety testing in humans and efficacy testing in animals. In the long run, the manufacture of ZMapp could require investment in infrastructure for making monoclonal antibodies at an industrial scale — assuming that funding is available to pay the production costs.
References
- 1.Feldmann H, Sanchez A, Geisbert TW. In: Fields Virology. 6. Knipe DM, Howley PM, editors. Lippincott Williams & Wilkins; 2013. pp. 923–956. [Google Scholar]
- 2.Baize S, et al. N Engl J Med. 2014 http://dx.doi.org/10.1056/NEJMoa1404505.
- 3.Qiu X, et al. Nature. 2014;514:47–53. doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geisbert TW, et al. Lancet. 2003;362:1953–1958. doi: 10.1016/S0140-6736(03)15012-X. [DOI] [PubMed] [Google Scholar]
- 5.Hensley LE, et al. J Infect Dis. 2007;196(Suppl 2):S390–S399. doi: 10.1086/520598. [DOI] [PubMed] [Google Scholar]
- 6.Warren TK, et al. Nature Med. 2010;16:991–994. doi: 10.1038/nm.2202. [DOI] [PubMed] [Google Scholar]
- 7.Feldmann H, et al. PLoS Pathog. 2007;3:e2. doi: 10.1371/journal.ppat.0030002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Günther S, et al. J Infect Dis. 2011;204(Suppl 3):S785–S790. doi: 10.1093/infdis/jir298. [DOI] [PubMed] [Google Scholar]
- 9.Geisbert TW, et al. Lancet. 2010;375:1896–1905. doi: 10.1016/S0140-6736(10)60357-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dye JM, et al. Proc Natl Acad Sci USA. 2012;109:5034–5039. doi: 10.1073/pnas.1200409109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olinger GG, Jr, et al. Proc Natl Acad Sci USA. 2012;109:18030–18035. doi: 10.1073/pnas.1213709109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiu X, et al. Sci Transl Med. 2012;4:138ra81. doi: 10.1126/scitranslmed.3003876. [DOI] [PubMed] [Google Scholar]
- 13.Pettitt J, et al. Sci Transl Med. 2013;5:199ra113. doi: 10.1126/scitranslmed.3006608. [DOI] [PubMed] [Google Scholar]
- 14.Qiu X, et al. Sci Transl Med. 2013;5:207ra143. doi: 10.1126/scitranslmed.3006605. [DOI] [PubMed] [Google Scholar]
- 15.Check Hayden E, Reardon S. Nature. 2014 http://dx.doi.org/10.1038/nature.2014.15698.
- 16.www.afro.who.int/en/clusters-a-programmes/dpc/epidemic-a-pandemic-alert-and-response/outbreak-news/4260-ebola-virus-disease-west-africa-22-august-2014.html
- 17.Marzi A, Feldmann H. Expert Rev Vaccines. 2014;13:521–531. doi: 10.1586/14760584.2014.885841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reported at the Filovirus Medical Countermeasure Workshop; 22–23 August 2013; https://respond.niaid.nih.gov/conferences/mcmworkshop/Pages/default.aspx. [Google Scholar]


