Abstract
Setting standards for medically based running analyses is necessary to ensure that runners receive a high-quality service from practitioners. Medical and training history, physical and functional tests, and motion analysis of running at self-selected and faster speeds are key features of a comprehensive analysis. Self-reported history and movement symmetry are critical factors that require follow-up therapy or long-term management. Pain or injury is typically the result of a functional deficit above or below the site along the kinematic chain.
Introduction
While the interest in the sport of running has increased exponentially worldwide (54), the medically based running-specific assessments, analyses, and medical care for the running population have not kept pace with the demand. Approximately 20% of Americans run for fitness, but the estimates of people who participate in recreational running are far greater than those of competitive runners (14). While there are “running assessment” or “gait analysis” services available across the country to help runners achieve optimal performance, the athlete faces the challenge of trying to select the programs that will provide the detail and medical oversight necessary for the best long-term outcomes. The programs that provide physician supervision and complementary expertise from physiologists, therapists, sports dietitians, and psychologists that may be required to assess and treat the runner appropriately may not be apparent. Programs may not indicate preparedness for emergency situations (emergency action plan) with access to medical professionals or nearby facilities for emergency care. Selecting a quality program from which a running analysis can be obtained therefore can be challenging for the consumer. Standards for conducting a comprehensive, medically based running analysis are presented here to help practitioners develop the best possible integrative programs for patients. These analyses can be defined as those guided by the best available scientific evidence of safe running practices, those that integrate musculoskeletal care with running form optimization and programming.
The medically based running analysis is very useful for the following: 1) confirming suspicions of poor running form and training techniques that contribute to current pain symptoms, 2) ruling out other medical conditions that underlie running-related pain or injury, and 3) helping prevent injury from occurring in healthy runners. The running analysis therefore should include a comprehensive medical review, a complete training history, a physician examination if the runner is symptomatic, biomechanical analysis and interpretation, and physical therapy consultation to propose programs for correcting biomechanical aberrations of running motion. Sports dietitians should be part of the care team, particularly in cases of recurrent chronic injury, body weight-related injuries, and suspected malnutrition. Other specialists such as sport psychologists, pain specialists, orthopedic surgeons, and endocrinologists need to be involved depending on the nature and chronicity of the symptoms. The analysis should include a medical and training history, physical examination by a physician and physical therapist, motion capture of running form, and review of factors that can influence performance (physical variables such as shoes, psychological variables such as anxiety or worry, and other individual issues such as dietary deficiencies or hormone imbalance). Once completed, the results should be reviewed and a plan should be outlined to address the deficits identified. An important point to note is that all runners should undergo a careful history review process (52), but not all runners may require a gait analysis initially (if the injury is acute and is contrary to medical advice). The running analysis components may be combined together or separated temporally depending on the nature of the case.
Medical and Training History
An initial encounter with a runner involves a medical review and a training history. This review process of physical examination factors is performed to make an initial medical diagnosis if needed and to identify possible modifiers and risk factors that may predispose the runner to injury or worsen a current problem. These collective factors are found in Table 1. A Physical Activity Readiness Questionnaire should be included in the initial visit to ensure that major potential risks for participating in exercise have been addressed (2).
Table 1.
Factors included in the medical history review and training history. Consider review over the last 6 months.
| Factor | Follow-Up Questions |
|---|---|
| Medical history review | |
| Demographics | |
| Past and current medical conditions | Bone health and menstrual history |
| History of previous running injuries (39) | |
| Dietary change | Energy intake and macro- or micronutrient pattern change |
| Development of musculoskeletal pain | If so, in which location and of what intensity? What makes it feel better or worse? |
| When do symptoms feel worst? | Before, during, or after the run, exacerbating factors, and pain type |
| Reasons for engaging in running | Weight management, social outlet, stress management, and fitness or health |
|
| |
| Potential triggers for injury | |
| Training status | Recreational, competitive, or elite |
| Cross-training | If so, what sport(s)? |
| Current weekly sessions, mileage, and runs per week | |
| Average distances for long run | |
| Typical running surface and route characteristics | |
| Shoe type and orthotic use (39) | How long has orthotics been used? |
| Wear pattern on shoe | |
| Barefoot running | |
| Currently doing speed work? | If so, how many times per week? |
| Currently training for a race? | If so, what distance and when? |
| Changes in running volume, frequency, terrain or surface, and shoes | |
| Perceived foot strike pattern | |
| Recent changes to training regimen, volume, and cross-training? | If so, describe. |
| Rapid increase in mileage (more than 10% per week) or sudden start of a program with inadequate transition (56) | |
| Participation in other endurance sports that use similar muscle groups as running | |
| Novice runner or slow running times (30,40) | |
| Increased weekly mileage (16,53) | |
| Increased number of days or sessions of running per week (27,53,56) | |
| Changed running gait because of pain or discomfort | |
| New shoes or inserts (23) | |
| Poorly fitting, tight, or worn shoes (28) | |
| Changed from a standard running shoe to minimalist shoes or barefoot (7,8) | |
| Change from rear foot to mid- or forefoot strike | |
| Added speed work or track work to routine | |
| Increased the pace of running | |
| Added hill training to routine (23) | |
| Changed running terrain | |
| For female runners, had irregular menstrual cycles (23) | |
Recent training history from approximately the last 3 to 6 months is highly valuable for creating a profile of the participant. Current training modes, training frequency, and duration are important areas for assessment of injury risk (8,16,27) and determining the volume of running and other activities to determine the cumulative effects of exercise stress (55). If a runner currently is training 7d·wk−1 or performs more than 1 running session a day, this is excessive volume that will not permit bony and soft tissues to recover between exercise sessions. Some evidence shows that less than 2 d·wk−1 of rest can increase risk of overuse injury by 5.2-fold (46). Tissues fatigue, and injury ensues. If a runner presents with a history of previous injuries such as stress fractures, this is a predictor for future stress fractures (25). Running experience, current pace, competition goals, and preferred running surface may reveal issues that are contributing to musculoskeletal pain. Participation in speed work may indicate significant stress to the hamstrings and lower back. Both recreational and elite runners can develop pain symptoms, but the experienced runner may tolerate more pain and have performance decline before seeking medical care and a running analysis. Recreational runners have a higher risk for developing exercise-related leg pain if their weekly volume is <24 km·wk−1 or <3 years of training (42) compared with more experienced runners.
Running surface or modifications to the running surface can change gait mechanics that lead to injury. For example, running the same route on a beveled road always places strain on the lower extremity that lands on the lateral side of the road (e.g., the iliotibial band and medial knee compartment). Research indicates that compared with running on asphalt roads, running on sand can increase the risk for soft tissue injuries such as midportion Achilles tendinopathy (27). The addition of hills to a running program introduces new musculoskeletal stressors that can include eccentric loading to the knee extensors. Changes in running program parameters and timing of these program changes can reveal possible reasons for onset of pain. For example, a sudden increase in running volume over a few weeks or one intense long run can trigger pain onset in various areas of the lower extremity or connective tissues (tendons) around the feet (26). Therefore a thorough review of running activity is important to guide recommendations in the analysis.
Documentation of the use of additional gear such as water bottles, electronic devices, and strollers can add valuable insight on biomechanics, symptoms, or pain perception. When any equipment that changes normal muscle activation patterns of gait and gait symmetry is introduced into running, the risk for onset of pain or injury increases. For example, our current pilot research is indicating that handheld water bottles cause motion restriction on the holding side and compensatory gait change on the contralateral side of the lower body. Alternating the hand that holds the gear or using belts or packs may help address this issue.
The use of orthotics (32,57), shoe posting in the insoles (47), and shoe mileage (28) can help provide explanations to patterns found in the running kinematics or kinetics. Rigid orthotics or heel lifts are provided commonly to runners for foot pain, or runners purchase commercial orthotics for running shoes to improve cushioning. While orthotics can help serve as a temporary bridge for foot support during rehabilitation, these inserts are not intended to be a long-term addition to a shoe. Prior orthotic use is a predictor of medial tibial stress syndrome (39). Overuse and overreliance on shoe inserts can prevent normal foot motion during the load bearing phase of gait and can decondition the muscles of the feet (1). Orthotics can perpetuate musculoskeletal pain and can even contribute to medial tibial stress fractures (24). Shoes with high mileage and obvious wear in the soles prevent normal loading mechanics of the foot and lower extremity. For example, a runner who has worn away the lateral heel of the shoe sole will be forced to land in exaggerated supination with each step, thereby increasing soft tissue stress in the midfoot.
Minimalist running approaches (1,5,6) and shoe type (18,29) are factors that may influence injury risk. Recent research has stimulated healthy debate among running experts regarding the injury risk related to foot strike pattern. Some studies report that heel striking is related to 2.5 times higher rates of repetitive bony and soft tissue injuries compared with forefoot striking (11). Forefoot striking does increase the plantarflexor moments and stress or strain rates to the Achilles tendon and the forces acting on the metatarsal heads (1). Foot strike may be facilitated partly by the type of shoe wear. Cushioned shoes or shoes with a high heel to toe drop encourage heel striking, whereas shoes with a minimal or no drop or no shoes facilitate mid- to forefoot striking. While comparative long-term injury rates for heel and forefoot striking are not yet clear, it is known that runners who rapidly switch from heel strike to forefoot strike with minimal transition time can develop musculo-skeletal injuries such as metatarsal stress fractures and plantar fasciitis. Similarly when runners change from a cushioned shoe to a shoe with minimal style without a safe transition for a few weeks to a few months, there is risk for injuries such as metatarsal stress fractures (7,19). Areas of the shoe soles that are worn show how the runner lands and pushes at foot strike and toe-off, respectively. Asymmetries of shoe wear patterns may be important indicators of asymmetric motion during running. It has been suggested that the materials in an average running shoe begin to break down over 350 to 400 miles. A history of the shoes worn and wear patterns is therefore important in the running analysis.
When musculoskeletal pain symptoms are present during or after running, a physician with running expertise should examine the runner before any further testing. Based on the nature of the pain and the self-reported history, imaging may be required to determine the presence and severity of musculoskeletal injury. A goal of this history review and imaging process is to reveal triggering factors of a running program that increase the risk for injury. These events may include 1) rapid changes in running volume mileage (22,41) (progression of more than 10% per week) (4), frequency, or form mileage with minimal transition time for adaptation (56), 2) recent change in running terrain or surface, 3) recent change in shoe wear or removal of shoes (19,44), 4) prolonged use of an orthotic in a shoe for longer than 2 months, and 5) no participation in sports other than running (34). Examination of the soles of the current and previous pair of running shoes provides insight about the locations of foot loading and leg dominance (28).
Additional Assessments
Running is essentially a repetitive series of single-legged squats performed over time. Before any gait analysis, a physician and a physical therapist therefore should perform a variety of physical tests to evaluate the runner’s ability to control dynamic motion symmetrically (33). Test maneuvers can include functional ability of different lower extremity motions and muscle strength and flexibility of the lower extremities, core, and spine (Table 2) (31,36). These assessments may be grouped into weight bearing and non-weight bearing categories. The physician and therapist will determine whether the runner is able to perform tests with equal range of motion (ROM) (43), strength and endurance, and limb segment alignment (31,36). Deficits can be identified, and physical therapy plans can be put into place to equalize right- and left-sided capability.
Table 2.
Static and dynamic physical examination maneuvers in a medically based running analysis.
| Weight bearing tests |
| Navicular drop (39) |
| Posture |
| Lumbar flexion and extension ROM |
| Thoracic rotation ROM |
| Single-leg squat |
|
|
| Weight bearing functional movement screen tests |
| Deep squat |
| Hurdle step |
| Inline lunge |
| Trunk rotary stability |
| Functional dorsiflexion tests (standing lunge test) |
| Balance assessment (single-leg test with eyes open and closed, Y balance) |
| Jump rope |
| Walking gait assessment |
| Heel and toe walking |
|
|
| Non-weight bearing tests |
| Static foot alignment |
| First metatarsal ray mobility |
| Ankle flexion/extension and inversion/eversion ROM |
| Subtalar inversion and eversion ROM |
| Hip mobility |
| Flexibility |
| Gastrocnemius and soleus, hamstring, iliotibial band, iliopsoas, and rectus femoris |
| Patellar position and tracking |
| Strength |
| Ankle inversion and eversion, hip flexion, hip extension, hip external rotation |
| Abduction |
| Functional rolling assessment |
Weight bearing tests can include static anthropometric tests such as leg lengths and toe-out angles at stance. These complement the load bearing responses such as navicular drop (43) and foot posture indices (33). Postural assessment of the runner from the shoulders to the feet is important to determine pelvic tilt, shoulder height symmetry, and spinal curvature that may induce asymmetric loading during gait analysis. Shoulder protraction or upward pelvic tilt that appears similar to a “sitting” posture will inhibit the ability of the runner to perform normal pelvis and trunk rotation during gait. Characterizing the natural alignment of the hips and knees (valgus, neutral, or varus) and the ankle inversion and eversion during stance is important for identification of possible areas to target during motion analysis.
Functional movement screens are vital in helping the care team determine strengths and weaknesses in motion control during running. Movement screens should include one- and two-legged squats with no shoes, hurdle stepping, inline lunges, and trunk rotary stability to the runner’s control of motion. While the act of single-legged load bearing during a gait cycle is complex, these movements can induce similar stresses. Careful observation by a trained eye of how the runner descends during a series of 10 to 12 dual-leg or single-leg squats can reveal whether the runner has adequate hip flexor, core, and gluteal strength to control motion during the stance phase of gait and reveal compensatory motions in cases of strength deficits. The runner should be able to descend into squatting in a controlled manner. Proper execution includes no pelvis tilt and no valgus knees. If the runner demonstrates severe knee valgus, cannot descend more than a few inches, or loses balance during descent, there is a lack of dynamic stability. This is important because hip strength is correlated inversely with pelvic and hip motion during the stance phase of running (15). Execution of these functional motions should occur with the runner performing an “abdominal brace,” where the abdominal and lumbar muscles are coactivated to support the spine (51). Walking gait tests, heel or toe walking, and jumping rope provide insight on natural ambulation patterns and ability of the participant to lift the knees during motion. The feet should not scuff the ground during these motions.
Non-weight bearing tests complement the results obtained from the weight bearing functional tests and include foot alignment and first metatarsal mobility, joint ROM, flexibility, and strength of the major lower extremity muscle groups. Patellar tracking is useful in determining whether pain symptoms are related to patellofemoral alignment. If the patella tracks laterally during a squatting motion or gait, this indicates that there is inadequate vastus medialis strength and relatively high iliotibal band tension. Right and left symmetry are evaluated and used in designing rehabilitation plans to correct imbalances or joint pain.
Motion Capture of Running Activity
Measurement of running mechanics can reveal mechanisms underlying injury or provide a platform to make improvements in running mechanical efficiency. Biomechanics of healthy uninjured runners can be compared with previously injured runners or those with pain to determine key differences in kinematics (3,13). There are several techniques that can be used to capture running motion. Among these choices, the ideal and accurate one is to use optical motion capture system with special markers (Fig. 1). This typical technique involves the placement of retroreflective (passive) or light-emitting (active) markers on anatomical landmarks attached to the subject. The markers are placed on specific landmarks of the body and can be used to create a stick figure model of the participant for kinematic calculations. New markerless systems require less setup and involve a participant running in the video capture area. The filmed runner is processed into a three-dimensional figure using a series of shapes that creates a hull (37). There is the potential sacrifice of resolution and reliability calculations if the camera number is not adequate (37). For the system to be able to reconstruct the three-dimensional position of the markers based on the two-dimensional view of each camera, each marker has to be seen by at least two cameras at the same time.
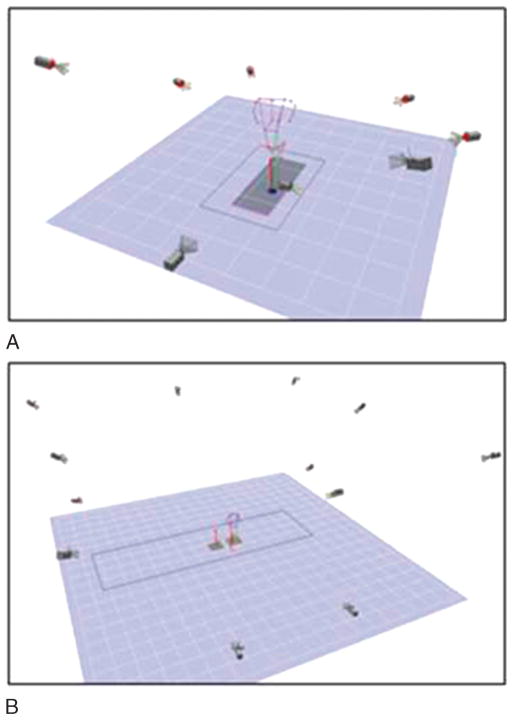
Figure 1.
A. Biomechanical testing setup for a running analysis: a force plated treadmill with a subset of seven cameras. Cameras are represented by rectangular prism shapes. The red arrow indicates the ground reaction force vector, and the stick figure is generated by marker system and digitizing. The force and kinematic data are synchronized by the capture and analysis software. B. A commercial treadmill testing setup in which the deck feet are placed over two force plates embedded in the floor. A 12-camera system is shown here, and cameras are represented by rectangular prism shapes. The ground reaction force vector arrows indicate the time of foot contact that can be synchronized with the kinematic data. For both setups, a reference camera is used to document the testing session.
Access to the technologies described previously is not always possible for the medical care team. However some basic systems such as dual high-speed cameras can be coupled with other imaging applications and software to provide some key information about running gait to the patient. For example, video capture obtained from iPad devices or smartphones can be processed in applications that calculate joint angles from different views at various points in the gait cycle. Advantages of this technique include real-time feedback to the patient during the assessment.
The convention of identifying the start of the gait cycle is to use the point of foot strike of one foot to the foot strike of the same foot (9,10,38). Joint angles and all other temporal-spatial parameters occurring during the gait cycle can be calculated by a postprocess software. Emerging evidence indicates that upper body motion can affect the motion of the lower body significantly (35). Measures and observations should include trunk, upper arm, and forearm motion. This three-dimensional data capture can be complemented with high-speed filming (at least 60 frames per second is recommended). Full-view data captures of the runner from each side, back, and front will provide the best information. Review of high-speed filming is useful for real-time, rapid feedback that the runner can see when the test is complete. High-speed filming also permits the team to observe slowly the runner’s normal running gait. Once collected, the data can be processed and the kinematics of the gait can be computed by a specific customized program.
Type of Treadmill for Running Assessment
The type of treadmill used for an analysis is based on the resources of the program and the needs of the athlete. Low to moderately priced commercial-grade treadmills are used often in the laboratory or clinic setting. In our experience, treadmills that can incline and reach 16.0 to 19.2 km·h−1 are perfectly suitable for running analyses. Features such as a 4-hp motor and continuous duty, weight limit of 182 kg, and strong, thick decking can accommodate almost all runners. Floor force plates are common in many motion laboratories and in some clinical settings. Assessment of ground reaction forces can be captured with these force plates. The data from the treadmill and force plates can be merged to generate information about the athlete (Fig. 1a). An important point to note is that the mechanics of treadmill running may not always match overground running. Some investigators have shown very close lower body kinematics and kinetics in all three planes of motion during treadmill and overground running (12,45). However other research revealed that minor increases in peak ankle eversion and small decreases in hip flexion at foot strike are lower during treadmill running than those during overground running (50). Therefore it is important to be aware that some runners may demonstrate slightly different motion when on a treadmill compared with their motion when on the ground.
Instrumented treadmills with embedded force plates are used to collect overground trials of running to collect ground reaction forces during running. While these treadmills are expensive and not common, these can be very useful for tracking changes before and after rehabilitation programs or for research measures. Ground reaction force data can be matched temporally with the kinematic data capture (Fig. 1b) Advantages of this setup include a direct matching of data that allows the clinical team to determine the effect of a kinematic pattern on the forces applied to the body during running at times when specific kinematic patterns occur. Five minutes of running on a treadmill is sufficient to allow familiarization with the equipment and adopt the typical gait pattern used for data collection (12). In addition, a 5-min window is ample time for the runner to achieve a steady state in metabolism (20).
Key Features to Observe in the Motion Capture
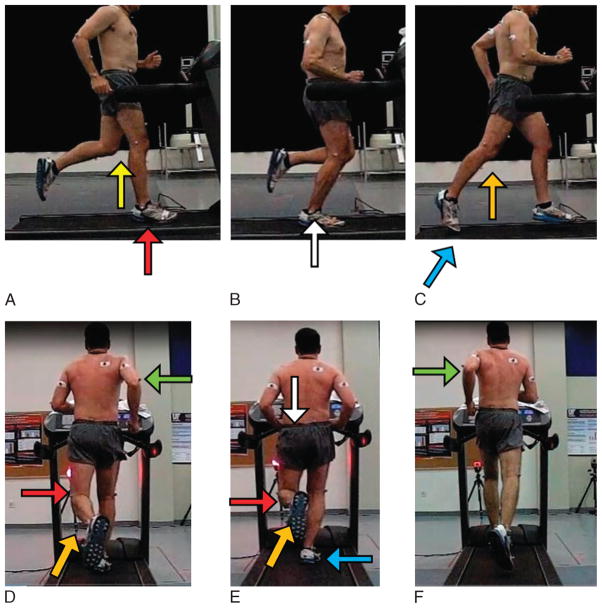
Motion capture data should be viewed from all three planes (sagittal, frontal, and transverse). High-speed camera videos should be reviewed minimally from the sagittal view and the posterior view. Transverse views from the motion analysis are important for determining the amount of rotation of the pelvis relative to the trunk. Still photos from the high-speed filming obtained in the sagittal view are from a sample recreational runner (Fig. 2a–c), and arrows represent some key points to review.
Figure 2.
A–F. Key points to compare during a typical gait cycle. A recreational male runner is shown a sample interpretation of the running form from a high-speed film capture. Arrows represent key issues to review in the still images. The trailing leg is defined as the leg behind the center of mass. Sagittal view, foot contact: foot strike pattern, knee bend, distance between knees, and trunk lean. Sagittal view, midstance phase: trailing leg lift, supporting leg knee bend. Sagittal view, toe off: distance the trailing leg remains on the treadmill belt, trailing leg knee bend. Posterior view, foot contact: crossover of trailing leg compared to the midline of the body, supporting foot toe-out angle. Posterior view, midstance phase: pelvic drop, knee angles, and time the trailing foot remains on the treadmill belt. Posterior view, toe off: symmetry of motion of hips compared to beginning of gait cycle, symmetry of arm motion.
The foot strike location (heel, midfoot, or forefoot) and where the heel lands relative to the hips (Fig. 2a, arrow) can be observed in this plane. A review of the film also can reveal whether the shoulder, hip, and ankle are aligned at foot strike. The pelvis and trunk should act as a unit. There should be a slight forward lean of the trunk-pelvic unit. At midstance, the shoulders should be aligned with the hips in the same vertical plane (Fig. 2b, white arrow) (48). The trunk should not bend forward in a disjointed fashion from the pelvis. The foot strike location indicates the type of impact stresses experienced by the runner (Fig. 2a, red arrow). A heel strike with an extended leg can generate very high impact forces on the lower extremity, whereas quiet midfoot or forefoot strikes are related with lower peak impact forces. The distance between the knees of the supporting leg and the trailing leg at midstance should be minimal (Fig. 2b, yellow arrow). Another feature to note is the length of time the striking foot spends on the treadmill belt (Fig. 2c). If the foot appears to be launching the body forward, the foot has remained on the treadmill belt too long (Fig. 2c, light blue arrow). The striking leg should not develop a full knee extension right before push-off (Fig. 2c, orange arrow), as shown in this example. The amount of knee lift during the swing phase and the foot lift after toe-off should be noted. Symmetry between the right and left sagittal views is important.
The posterior view can provide additional information about the running form (Fig. 2d–f). The key features are the foot inversion or eversion angle at foot contact and midstance (Fig. 2e, light blue arrow). Excessive values of either foot motion place negative stresses on the foot and knee and strain the muscles and ligaments of the foot. Knee angles and the presence of knee contact during the gait cycles during the stance phase indicate whether there is weakness of the hip flexors and extensors (Fig. 2d and e; knee angles, red arrow). The supporting foot should not collapse at the arch and cause a valgus knee. Determination of whether the trailing foot crosses over the midline of the body can be seen in images in Figure 2d and f (orange arrows). The motion of the markers at the pelvis can be used to show whether there is symmetry of hip motion in the vertical and transverse planes. Specifically pelvic drop after foot contact (Fig. 2e, white arrow) can indicate weakness of the hip musculature in the supporting leg. Trunk and pelvis rotation should be coordinated, with forward motion of one side of the pelvis coordinated with the forward movement of the trunk on the ipsilateral side. There should be an opposite rotation of the pelvis relative to the trunk. Shoulder height and arm drive should be symmetrical throughout the gait cycle (Fig. 2d and f, green arrows). Asymmetric arm and shoulder motion may compensate for flexibility variations in trunk and pelvic rotation.
Transverse plane motion is very useful to determine where there are limitations in rotation in the body segments. While this is not collected typically in a high-speed film, the digitized data reveal some key features. From the superior view, it can be observed whether the pelvis and trunk segments cyclically cross. If the pelvis and trunk segments are not crossing and the pelvis and torso act as one stiff segment, this could be indicative of guarded gait (injury or pain history) or poor flexibility of the muscles in the hips and lumbopelvic region. Asymmetry of trunk or arm rotation can indicate relative thoracolumbar or hip tightness on one side or the other.
Additional Speed Testing
Running at self-selected speeds can provide the average running motion of the participant. Inclusion of trials at faster or slower speeds may be required if speed variations trigger pain because changing speed changes the normal kinematic patterns and kinetics during running (49). Differences in muscle activation patterns and ground reaction forces exist when jogging and running at speeds ranging from 2 to 5 m·s−1 (21) and beyond. Inclusion of a “speed work” or faster pace is useful if this is an intensity that mechanically triggers or worsens joint pain. Changes in testing speed therefore may be used as needed for the specific case.
When to Involve Other Experts
A running analysis is focused on the aspects of the patient’s health that are affected by running. During testing, findings may reveal issues deeper than gait mechanics, shoes, orthotics, and muscle activation. Alternatively if the runner’s symptoms do not resolve with the recommended conservative approaches, other expert opinions should be sought. Psychological conditions often are unnoticed and untreated in runners. If the runner reveals that there is a history of psychological issues or expresses answers to questions in a depression survey that indicate harm to self, there should be plans in place to refer these individuals for further care.
During the evaluation, the runner may report that running or exercise elicits severe and/or repeatable lower extremity pain (>7 points out of 10 on a 0 to 10 pain scale). The pain may be the result of mechanical or nonmechanical factors such as nerve entrapments, regional pain syndromes, stress fractures, or other musculoskeletal issues. Ancillary diagnostic testing may be very helpful to rule out nonmechanical mechanisms for pain. Pain specialists or neurologists may be consulted if the presence of pain symptoms is disproportionate to the stressors placed on the tissues or if pain is severe and unrelenting during or after running.
Depending on the particular runner and symptoms, the participant can be recommended for follow-up testing and consultation with medical specialists. Radiological imaging, compartment testing, bone scans, vascular tests, hormone profiles, nutritional analysis, and neurological examinations may identify anatomical or disease conditions that may be causing pain (17). Primary care physicians can facilitate this additional testing. Radiological findings may reveal the need for orthopedic surgical intervention, such as osteochondral defects on the knee or ankle. Hip symptoms consistent with labral tears will require consults with an orthopedic surgeon. Physical therapists and athletic trainers are vital to the continuum of care and should work closely with the physicians to provide tailored rehabilitation programs that address the functional deficits and correct asymmetries. In some cases, chronic or recurring musculoskeletal injuries may have a multifaceted etiology with endocrine and/or nutritional factors. In young girls or women or older runners with low body weight, hormonal or dietary deficiencies may contribute to stress reactions or fractures. Endocrinologists can be consulted to determine whether there are endocrine issues underlying the injury.
Sports dietitians are a valuable part of the running health care team. Dietitians should be involved in helping runners achieve personal goals such as weight loss and weight management and optimizing recovery from endurance events. Dietitians provide expertise regarding recovery from over-training syndromes and performance concerns. Importantly dietitians also should be consulted for helping runners over-come female athlete triad issues and helping older runners achieve adequate energy intake.
Conclusions
Setting standards for medically based running analyses is necessary to ensure that patients are being provided with service of appropriate quality and depth. A comprehensive analysis should include a medical and training history and a battery of physical and functional tests. Motion analysis of running at self-selected and faster speeds (if needed) is appropriate for identification of possible mechanical reasons underlying musculoskeletal pain symptoms and for injury prevention. Attention to details in self-reported history and movement symmetry can reveal important issues that require follow-up therapy or adjustments. The pain or injury site may be the end product of a kinematic problem on the contralateral side or deficits above or below the site along the kinematic chain. Other medical experts should be included in the care of the runner, should issues that are outside the scope of the treating practitioner arise.
Acknowledgments
This article was recruited and shepherded through the review process by section editor Jonathan T. Finnoff, DO, FACSM, for the Training, Prevention, and Rehabilitation section. Publication was delayed by the peer review process, and the article missed the intended issue.
Footnotes
The authors declare no conflicts of interest and do not have any financial disclosures to report.
References
- 1.Altman AR, Davis IS. Barefoot running: biomechanics and implications for running injuries. Curr Sports Med Rep. 2012;11:244–50. doi: 10.1249/JSR.0b013e31826c9bb9. [DOI] [PubMed] [Google Scholar]
- 2.American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 9. Lippincott Williams and Williams; Philadelphia: 2013. [DOI] [PubMed] [Google Scholar]
- 3.Azevedo LB, Lambert MI, Vaughan CL, et al. Biomechanical variables associated with Achilles tendinopathy in runners. Br J Sports Med. 2009;43:288–92. doi: 10.1136/bjsm.2008.053421. [DOI] [PubMed] [Google Scholar]
- 4.Ballas MT, Tytko J, Cookson D. Common overuse running injuries: diagnosis and management. Am Fam Physician. 1997;55:2473–84. [PubMed] [Google Scholar]
- 5.Bonacci J, Saunders PU, Hicks A, et al. Running in a minimalist and light-weight shoe is not the same as running barefoot: a biomechanical study. Br J Sports Med. 2013;47:387–92. doi: 10.1136/bjsports-2012-091837. [DOI] [PubMed] [Google Scholar]
- 6.Bonacci J, Vicenzino B, Spratford W, Collins P. Take your shoes off to reduce patellofemoral joint stress during running. Br J Sports Med. 2013 doi: 10.1136/bjsports-2013-092160. [DOI] [PubMed] [Google Scholar]; Br J Sports Med. 2014 Mar;48(6):425–8. doi: 10.1136/bjsports-2013-092160. [DOI] [PubMed] [Google Scholar]
- 7.Cauthon DJ, Langer P, Coniglione TC. Minimalist shoe injuries: three case reports. Foot (Edinb) 2013;23:100–3. doi: 10.1016/j.foot.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Chang WL, Shih YF, Chen WY. Running injuries and associated factors in participants of ING Taipei Marathon. Phys Ther Sport. 2012;13:170–4. doi: 10.1016/j.ptsp.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Chumanov ES, Wille CM, Michalski MP, Heiderscheit BC. Changes in muscle activation patterns when running step rate is increased. Gait Posture. 2012;36:231–5. doi: 10.1016/j.gaitpost.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciacci S, Di Michele R, Merni F. Kinematic analysis of the braking and propulsion phases during the support time in sprint running. Gait Posture. 2010;31:209–12. doi: 10.1016/j.gaitpost.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Daoud AI, Geissler GJ, Wang F, et al. Foot strike and injury rates in endurance runners: a retrospective study. Med Sci Sports Exerc. 2012;44:1325–34. doi: 10.1249/MSS.0b013e3182465115. [DOI] [PubMed] [Google Scholar]
- 12.Fellin RE, Manal K, Davis IS. Comparison of lower extremity kinematic curves during overground and treadmill running. J Appl Biomech. 2010 Nov;26(4):407–14. doi: 10.1123/jab.26.4.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferber R, Noehren B, Hamill J, Davis IS. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010;40:52–8. doi: 10.2519/jospt.2010.3028. [DOI] [PubMed] [Google Scholar]
- 14.Fields KB. Running injuries — changing trends and demographics. Curr Sports Med Rep. 2011;10:299–303. doi: 10.1249/JSR.0b013e31822d403f. [DOI] [PubMed] [Google Scholar]
- 15.Ford KR, Taylor-Haas JA, Genthe K, Hugentobler J. Relationship between hip strength and trunk motion in college cross-country runners. Med Sci Sports Exerc. 2013;45:1125–30. doi: 10.1249/MSS.0b013e3182825aca. [DOI] [PubMed] [Google Scholar]
- 16.Fredericson M, Misra AK. Epidemiology and aetiology of marathon running injuries. Sports Med. 2007;37:437–9. doi: 10.2165/00007256-200737040-00043. [DOI] [PubMed] [Google Scholar]
- 17.Gallo RA, Plakke M, Silvis ML. Common leg injuries of long-distance runners: anatomical and biomechanical approach. Sports Health. 2012;4:485–95. doi: 10.1177/1941738112445871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giandolini M, Horvais N, Farges Y, et al. Impact reduction through long-term intervention in recreational runners: midfoot strike pattern versus low-drop/low-heel height footwear. Eur J Appl Physiol. 2013;113:2077–90. doi: 10.1007/s00421-013-2634-7. [DOI] [PubMed] [Google Scholar]
- 19.Giuliani J, Masini B, Alitz C, Owens BD. Barefoot-simulating footwear associated with metatarsal stress injury in 2 runners. Orthopedics. 2011;34:e320–3. doi: 10.3928/01477447-20110526-25. [DOI] [PubMed] [Google Scholar]
- 20.Gruber AH, Umberger BR, Braun B, Hamill J. Economy and rate of carbohydrate oxidation during running with rearfoot and forefoot strike patterns. J Appl Physiol (1985) 2013;115:194–201. doi: 10.1152/japplphysiol.01437.2012. [DOI] [PubMed] [Google Scholar]
- 21.Hammer SR, Delp SL. Muscle contributions to fore-aft and vertical body mass center accelerations over a range of running speeds. J Biomech. 2013;46:780–7. doi: 10.1016/j.jbiomech.2012.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hespanhol LC, Junior, Pena Costa LO, Lopes AD. Previous injuries and some training characteristics predict running-related injuries in recreational runners: a prospective cohort study. J Physiother. 2013;59:263–9. doi: 10.1016/S1836-9553(13)70203-0. [DOI] [PubMed] [Google Scholar]
- 23.Hockenbury RT. Forefoot problems in athletes. Med Sci Sports Exerc. 1999;31:S448–58. doi: 10.1097/00005768-199907001-00006. [DOI] [PubMed] [Google Scholar]
- 24.Hubbard TJ, Carpenter EM, Cordova ML. Contributing factors to medial tibial stress syndrome: a prospective investigation. Med Sci Sports Exerc. 2009;41:490–6. doi: 10.1249/MSS.0b013e31818b98e6. [DOI] [PubMed] [Google Scholar]
- 25.Kelsey JL, Bachrach LK, Procter-Gray E, et al. Risk factors for stress fracture among young female cross-country runners. Med Sci Sports Exerc. 2007;39:1457–63. doi: 10.1249/mss.0b013e318074e54b. [DOI] [PubMed] [Google Scholar]
- 26.Kindred J, Trubey C, Simons SM. Foot injuries in runners. Curr Sports Med Rep. 2011;10:249–54. doi: 10.1249/JSR.0b013e31822d3ea4. [DOI] [PubMed] [Google Scholar]
- 27.Knobloch K, Yoon U, Vogt PM. Acute and overuse injuries correlated to hours of training in master running athletes. Foot Ankle Int. 2008;29:671–6. doi: 10.3113/FAI.2008.0671. [DOI] [PubMed] [Google Scholar]
- 28.Kong PW, Candelaria NG, Smith D. Comparison of longitudinal biomechanical adaptation to shoe degradation between the dominant and non-dominant legs during running. Hum Mov Sci. 2011;30:606–13. doi: 10.1016/j.humov.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 29.Lilley K, Stiles V, Dixon S. The influence of motion control shoes on the running gait of mature and young females. Gait Posture. 2013;37:331–5. doi: 10.1016/j.gaitpost.2012.07.026. [DOI] [PubMed] [Google Scholar]
- 30.Lisman P, O’Connor FG, Deuster PA, Knapik JJ. Functional movement screen and aerobic fitness predict injuries in military training. Med Sci Sports Exerc. 2013;45:636–43. doi: 10.1249/MSS.0b013e31827a1c4c. [DOI] [PubMed] [Google Scholar]
- 31.Loudon JK, Parkerson-Mitchell AJ, Hildebrand LD, Teague C. Functional movement screen scores in a group of running athletes. J Strength Cond Res. 2014;28:909–13. doi: 10.1097/JSC.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 32.Maclean CL, Davis IS, Hamill J. Influence of running shoe midsole composition and custom foot orthotic intervention on lower extremity dynamics during running. J Appl Biomech. 2009;25:54–63. doi: 10.1123/jab.25.1.54. [DOI] [PubMed] [Google Scholar]
- 33.Magrum E, Wilder RP. Evaluation of the injured runner. Clin Sport Med. 2010;29:331–45. doi: 10.1016/j.csm.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Malisoux L, Ramesh J, Mann R, et al. Can parallel use of different running shoes decrease running-related injury risk? Scand J Med Sci Sports. 2013 doi: 10.1111/sms.12154. [DOI] [PubMed] [Google Scholar]
- 35.Miller RH, Caldwell GE, Van Emmerik RE, et al. Ground reaction forces and lower extremity kinematics when running with suppressed arm swing. J Biomech Eng. 2009;131:124502. doi: 10.1115/1.4000088. [DOI] [PubMed] [Google Scholar]
- 36.Minick KI, Kiesel KB, Burton L, et al. Interrater reliability of the functional movement screen. J Strength Cond Res. 2010;24:479–86. doi: 10.1519/JSC.0b013e3181c09c04. [DOI] [PubMed] [Google Scholar]
- 37.Mundermann L, Corazza S, Andriacchi TP. Markerless motion capture for biomechanical applications. In: Rosenhahn B, Klette R, Metaxas D, editors. Human Motion — Understanding, Modeling, Capture, and Animation. Springer; Dordecht, Netherlands: 2008. pp. 377–98. [Google Scholar]
- 38.Nakayama Y, Kudo K, Ohtsuki T. Variability and fluctuation in running gait cycle of trained runners and non-runners. Gait Posture. 2010;31:331–5. doi: 10.1016/j.gaitpost.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 39.Newman P, Witchalls J, Waddington G, Adams R. Risk factors associated with medial tibial stress syndrome in runners: a systematic review and meta-analysis. Open Access J Sports Med. 2013;4:229–41. doi: 10.2147/OAJSM.S39331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parker DT, Weitzenberg TW, Amey AL, Nied RJ. Group training programs and self-reported injury risk in female marathoners. Clin J Sport Med. 2011;21:499–507. doi: 10.1097/JSM.0b013e3182377080. [DOI] [PubMed] [Google Scholar]
- 41.Rasmussen CH, Nielsen RO, Juul MS, Rasmussen S. Weekly running volume and risk of running-related injuries among marathon runners. Int J Sports Phys Ther. 2013;8:111–20. [PMC free article] [PubMed] [Google Scholar]
- 42.Reinking MF, Austin TM, Hayes AM. A survey of exercise-related leg pain in community runners. Int J Sports Phys Ther. 2013;8:269–76. [PMC free article] [PubMed] [Google Scholar]
- 43.Reinking MF, Hayes AM. Intrinsic factors associated with exercise-related leg pain in collegiate cross-country runners. Clin J Sport Med. 2006;16:10–4. doi: 10.1097/01.jsm.0000188041.04760.d2. [DOI] [PubMed] [Google Scholar]
- 44.Rice H, Nunns M, House C, et al. High medial plantar pressures during barefoot running are associated with increased risk of ankle inversion injury in Royal Marine recruits. Gait Posture. 2013;38:614–8. doi: 10.1016/j.gaitpost.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 45.Riley PO, Dicharry J, Franz J, et al. A kinematics and kinetic comparison of overground and treadmill running. Med Sci Sports Exerc. 2008;40:1093–100. doi: 10.1249/MSS.0b013e3181677530. [DOI] [PubMed] [Google Scholar]
- 46.Ristolainen L, Kettunen JA, Waller B, et al. Training-related risk factors in the etiology of overuse injuries in endurance sports. J Sports Med Phys Fitness. 2014;54:78–87. [PubMed] [Google Scholar]
- 47.Rodrigues P, Chang R, TenBroek T, Hamill J. Medially posted insoles consistently influence foot pronation in runners with and without anterior knee pain. Gait Posture. 2013;37:526–31. doi: 10.1016/j.gaitpost.2012.09.027. [DOI] [PubMed] [Google Scholar]
- 48.Schache AG, Blanch P, Rath D, et al. Three-dimensional angular kinematics of the lumbar spine and pelvis during running. Hum Mov Sci. 2002;21:273–93. doi: 10.1016/s0167-9457(02)00080-5. [DOI] [PubMed] [Google Scholar]
- 49.Schache AG, Blanch PD, Dorn TW, et al. Effect of running speed on lower limb joint kinetics. Med Sci Sports Exerc. 2011;43:1260–71. doi: 10.1249/MSS.0b013e3182084929. [DOI] [PubMed] [Google Scholar]
- 50.Sinclair J, Richards J, Taylor PJ, et al. Three-dimensional kinematic comparison of treadmill and overground running. Sports Biomech. 2013;12:272–82. doi: 10.1080/14763141.2012.759614. [DOI] [PubMed] [Google Scholar]
- 51.Stanton T, Kawchuk G. The effect of abdominal stabilization contractions on posteroanterior spinal stiffness. Spine (Phila Pa 1976) 2008;33:694–701. doi: 10.1097/BRS.0b013e318166e034. [DOI] [PubMed] [Google Scholar]
- 52.Strakowski JA, Jamil T. Management of common running injuries. Phys Med Rehabil Clin N Am. 2006;17:537–52. doi: 10.1016/j.pmr.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 53.Tenforde AS, Sayres LC, McCurdy ML, et al. Overuse injuries in high school runners: lifetime prevalence and prevention strategies. PM R. 2011;3:125–31. doi: 10.1016/j.pmrj.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 54.Verhagen E. Prevention of running-related injuries in novice runners: are we running on empty? Br J Sports Med. 2012;46:836–7. doi: 10.1136/bjsports-2012-091505. [DOI] [PubMed] [Google Scholar]
- 55.Vleck VE, Bentley DJ, Millet GP, Cochrane T. Triathlon event distance specialization: training and injury effects. J Strength Cond Res. 2010;24:30–6. doi: 10.1519/JSC.0b013e3181bd4cc8. [DOI] [PubMed] [Google Scholar]
- 56.Wilder RP, Sethi S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81. doi: 10.1016/S0278-5919(03)00085-1. [DOI] [PubMed] [Google Scholar]
- 57.Williams DS, 3rd, McClay Davis I, Baitch SP. Effect of inverted orthoses on lower-extremity mechanics in runners. Med Sci Sports Exerc. 2003;35:2060–8. doi: 10.1249/01.MSS.0000098988.17182.8A. [DOI] [PubMed] [Google Scholar]