Abstract
Objective
The aim of this study was to examine associations between childhood adversity, parental bonding, gender, depressive symptoms, and quality of life in non-treatment-seeking adults from the community.
Method
Effects of differential parental rearing were compared in adults who reported a high degree of childhood maltreatment (n = 72) and those who reported no significant adverse events in childhood (n = 69). Subjects completed retrospective measures of childhood maltreatment and perceived parenting style, as well as measures of current depressive symptoms and quality of life.
Results
The subjects without childhood maltreatment were younger and endorsed less current depressive symptomatology than did subjects with childhood maltreatment. While the subjects without a history of maltreatment reported more “optimal” bonding experiences with their parents, the maltreatment group members were more likely to characterize their early parental bonding experiences in terms of “affectionless control” (p < .001 for both maternal and paternal parenting), “affectionate constraint” (p = .025 for maternal parenting and p = .004 for paternal parenting), or “weak or absent” bonding (p < .001 for both maternal and paternal parenting). Results of a multiple regression analysis revealed that overall quality of paternal care (p = .015) and current level of depressive symptoms (p < .001) were significant independent predictors of adult quality of life. Gender effects between subjects providing parental bonding data were limited to the group with childhood maltreatment.
Conclusion
These findings extend previous work documenting a relationship between early life maltreatment and suboptimal parental bonding, suggesting gender-specific effects of maternal and paternal care. Effects of childhood maltreatment on quality of life in adulthood appear to be linked with the quality of childhood paternal care and the occurrence of depressive symptomatology in adulthood, suggesting possible targets for primary or secondary prevention.
Keywords: Parental bonding, Quality of life, Childhood maltreatment
Introduction
Bowlby (1969, 1973, 1980) construed attachment as the strong emotional connection, which develops between a child and his care provider within the first 6 or 7 months of his birth as a result of the shared interaction between them. Any form of separation from the attachment figure or involvement in a stress-inducing situation triggers the attachment behavioral system that results in the child seeking protection and attempting to re-establish proximity with the caregiver. The caregiver provides a safe foundation from which the child can explore the world (George, 1996; Main, 1996).
Ainsworth, Blehar, Waters, and Walls (1978) identified three styles of attachment in a controlled laboratory setting. Interaction patterns of infants were observed using the strange situation procedure that entails brief separations from the mother and contact with an unfamiliar person. They noted that a securely attached infant with a good bonding relationship with the mother gets slightly upset when she departs, and readily reaches out for her on her return. Mothers of securely attached children tend to provide consistent care, and are highly responsive to their children’s needs. A child with an insecure (anxious/ambivalent) attachment becomes extremely upset in the absence of the mother or in the presence of a stranger; however, the child tends to be annoyed and becomes defiant towards the mother on her return. Mothers of these children tend to be inconsistent and unpredictable in provision of care. On the other hand, a child exhibiting an insecure (anxious/avoidant) style of attachment exhibits minimal anguish when the mother leaves, and disregards her on her return. Mothers of such children tend to be irritable and indifferent or overstimulating. Main and Solomon (1990) identified a fourth style of attachment called disorganized/disoriented wherein children appear to be fearful of care providers, and exhibit a confused attachment pattern. A large percentage of maltreated infants tend to manifest this insecure attachment style (Carlson, Cicchetti, Barnett, & Braunwald, 1989).
According to Bowlby (1973), early attachment experiences provide a template or an internal working model for later adult attachment which serves as a foundation for expectations and conduct in subsequent relationships (e.g., Collins & Read, 1990; George, 1996; Roisman, Collins, Sroufe, & Byron, 2005). The formation of this template is influenced by the child’s perception of the caregiver’s accessibility in the time of distress and the child’s sense of self influenced by his perception of how willing the caregiver or others would be to help him in the time of need. Several researchers have developed models of adult attachment (Bartholomew & Horowitz, 1991; George, Kaplan, & Main, 1987; Hazan & Shaver, 1987).
Accordingly, early life experiences have a powerful impact on future growth and development. While experiences during this vulnerable period affect many spheres of function, secure attachment to parental figures and positive bonding experiences during childhood have been specifically reported to be associated with greater welfare (Salzman, 1996), increased coping resources (Buelow, Lyddon, & Johnson, 2002), and higher perceived support in one’s community (Blain, Thompson, & Whiffen, 1993). On the other hand, insecure attachment has been found to be related to psychopathology (Bogaerts, Vanhuele, & Declercq, 2005; Difilippo & Overholser, 2002; Myhr, Sookman, & Pinard, 2004), adjustment difficulties (Rice, FitzGerald, Whaley, & Gibbs, 1995), and suicidality (Violato & Arato, 2004).
Measurement of parental bonding
Parker, Tupling, and Brown (1979) reviewed the attachment literature (Ainsworth, Bell, & Stayton, 1975; Bowlby, 1969; Rutter, 1972) and several factor analytic studies (e.g., Raskin, Boothe, Reatig, Schulterbrandt, & Odle, 1971; Roe & Siegelman, 1963; Schaefer, 1965) to identify key parental characteristics that influence the parent-child bond. While noting that positive bonding experiences are contingent on several factors, including nurturance, affection, ease of access, protection, support, and encouragement from caregivers, and are influenced by parent-child attributes and characteristics of their relationship, they proposed that bonding experiences with parents may be influenced by two main factors, specifically, care and psychological control or overprotection. Parker et al. (1979) developed the Parental Bonding Instrument (PBI) as a self-report questionnaire completed by offspring who report on their childhood experiences of these two dimensions of parental behaviors and attitudes. The care factor has two poles, measuring parental warmth, affection, and involvement versus coldness, rejection, detachment, and aloofness, respectively. The second factor, overprotection, is also bipolar, and measures psychological control, infringement, and imposition versus encouragement of autonomy and self-sufficiency.
The PBI allows the classification of parental bonding styles into four quadrants reflecting the combinations of the two dimensions. The first quadrant is referred to as the “optimal” bonding quadrant and is reflective of individuals who report ideal parenting in their formative years, with high parental care and encouragement of autonomy (i.e., low overprotection). The second quadrant is called “affectionate constraint” and includes individuals who describe their parents as caring but with a tendency to exert psychological control and discourage autonomy (i.e., high overprotection). The third quadrant, called “affectionless control” is reflective of individuals who report poor care and experienced excessive control, infringement of rights and intrusion from their parents (i.e., high overprotection). The final quadrant encompasses individuals with “weak” or “absent” bonding and is characterized by low scores on both the care and overprotection factors. It is important to note that while the PBI assesses reported parental behaviors that impact the formation of the child’s attachment style, it does not directly evaluate the child’s attachment behavior (Gittleman, Klein, Smider, & Essex, 1998).
Parental bonding and adult quality of life and functioning
Bonding is viewed as an essential developmental task that is critical for adequate functioning. A large number of empirical studies have found associations of parental care and overprotection with domains of adult functioning, including dysfunctional self-cognitions (Ingram, Overbey, & Fortier, 2001), emotional functioning (Canetti, Bachar, Galili-Weisstub, Kaplan, & Shalev 1997; Wark, Kruczek, & Boley, 2003), and loneliness (Wiseman, Mayseless, & Sharabany, 2006), as well as overall satisfaction and quality of life (Canetti et al., 1997; Datta, Marcoen, & Poortinga, 2005; Lung, Huang, Shu, & Lee, 2004). Attachment style may moderate the effects of parenting behaviors on later functioning. Gittleman et al. (1998) found that presence of a secure attachment protected against the adverse consequences of poor parental conduct.
Parental bonding and psychopathology
A number of studies have investigated the association between parental bonding and subsequent development of psychiatric disorders (e.g., Enns, Cox, & Clara, 2002; Lung, Lee, & Shu, 2002; Russ, Heim, & Westen, 2003; Turgeon, O’Connor, Marchand, & Freeston, 2002; Wiborg & Dahl, 1997; Zweig-Frank & Paris, 1991). Adverse parenting experiences in childhood have been linked to a broad range of symptoms of adult psychopathology (Enns et al., 2002; Mancini, D’Olimpio, Prunetti, Didonna, & Genio, 2000). Specifically, poor parental bonding is thought to interfere with the development of appropriate coping skills, rendering the individual vulnerable to stress and prone to affective illness (Kraaij et al., 2003; Matheson et al., 2005). In the National Comorbidity Study, Enns et al. (2002) noted that the only “clear pattern of specificity” is between inferior parental bonding and nonmelancholic depression (Parker & Hadzi-Pavlovic, 1992; Parker et al., 1997). While the affectionless control quadrant characterized by low care and high overprotection has been implicated as a risk factor for depression (e.g., Sato et al., 1998), many studies have found that in comparison with overprotection, lack of adequate parental care in childhood (e.g., Duggan, Sham, Minne, Lee, & Murray, 1998; Mackinnon, Henderson, & Andrews, 1993), particularly mother care (e.g., Oakley-Browne, Joyce, Wells, Bushness, & Hornblow, 1995; Rey, 1995; Sakado et al., 2000) is the crucial factor predisposing to depressive symptomatology.
Childhood maltreatment and parental bonding: determinants of quality of life?
Though many investigations have documented links between childhood adversity or poor parenting and psychiatric or functional problems, few studies have examined the role of parental bonding in comparative groups of abused and non-abused subjects. In general, the studies that have been conducted have exclusively examined the impact of childhood sexual abuse on parental rearing (e.g., Fitzgerald, Shipman, Jackson, McMahon, & Hanley, 2005; Schreiber & Lyddon, 1998) or the presence of psychiatric symptoms (e.g., Berger et al., 1995; Douglas, 2000; Jurmann, 1999; Romans, Gendall, Martin, & Mullen, 2001). However, few studies have addressed how associations between parental bonding and symptoms of depression affect quality of life in individuals with a history of childhood maltreatment compared to those without such histories. The relationships between childhood maltreatment, parental bonding experiences, and symptoms of depression, three factors that have been highly associated with quality of life, have not been examined concurrently. In addition, there has been a lack of emphasis on how parental bonding might mitigate negative outcomes in cases of childhood maltreatment.
In order to fill this gap in the literature, the present study examined differences in perceived parental bonding quality and depressive symptoms in subjects who reported significant childhood maltreatment (e.g., emotional neglect, emotional abuse, physical neglect, physical abuse, sexual abuse) compared with a group who did not report significant maltreatment in childhood. The aim of this study was to determine whether parental bonding and the severity of depressive symptoms are intermediates in the relationship between childhood maltreatment and quality of life in adulthood. Specifically, based on the literature discussed above, it was hypothesized that parental bonding would account for a significant proportion of the variance in this relationship. In addition, given the associations of both childhood maltreatment and parental bonding with depression, it was hypothesized that adult depressive symptoms would further account for some of the association between maltreatment and quality of life.
Method
Subjects
Adults aged 18–65 were invited to participate in one of four thematically and methodologically similar studies of early life adversity and adult neurobiology that recruited participants from 2002 to 2005. Advertisements for (1) healthy adults; (2) adults suffering from depression; and (3) individuals with a history of early life stress were posted (e.g., newspapers, fliers, media, web-based) in and around Providence, RI. These studies employed identical baseline assessment procedures, including a battery of self-report retrospective measures of childhood maltreatment and perceived parenting style, current depressive symptoms, and current quality of life. Potential participants were initially screened over the phone, and if exclusion criteria were not met, they were then invited to participate in the aforementioned studies. Participants provided voluntary written informed consent on forms approved by the Butler Hospital Institutional Review Board. Participants took part in a comprehensive semi-structured diagnostic interview, the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First, Spitzer, Gibbon, & Williams, 2002). Exclusion criteria included (a) any significant acute or chronic medical or neurological condition; (b) current use of psychotropic medications; (c) any history of bipolar or psychotic disorders; and (d) any current alcohol or substance dependence.
Measures
Subjects were assessed with the following measures: (1) Structured Clinical Interview for DSM-IV Axis I Disorders (First et al., 2002); (2) Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998; Bernstein et al., 2003); (3) Parental Bonding Instrument (PBI; Parker et al., 1979); (4) Inventory of Depressive Symptomatology-Self Report (IDS-SR; Rush, Gullion, Basco, Jarrett, & Trivedi, 1996); and the (5) Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q; Endicott, Nee, Harrison, & Blumenthal, 1993).
Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First et al., 2002). The SCID is a semi-structured, diagnostic interview designed to assess the symptoms of DSM-IV Axis I disorders.
The Childhood Trauma Questionnaire (CTQ) is a retrospective measure of child abuse and neglect that has demonstrated high internal consistency and good test–retest reliability (Bernstein & Fink, 1998; Bernstein et al., 1994). The CTQ has five scales (emotional abuse, physical abuse, sexual abuse, emotional neglect and physical neglect), each of which allows individuals to be divided into categories of none, low, moderate, or severe abuse. The CTQ was used as an assessment measure of participants’ exposure to early adverse experiences.
Parental Bonding Instrument (PBI; Parker et al., 1979). The PBI examines parental behaviors and attitudes that contribute to the development of bonding experiences in childhood. It has two bipolar dimensions of parental care and overprotection. The PBI has good reliability and validity (Parker, 1990). The PBI has been shown to be stable over a 20-year period in a nonclinical population, and is resistant to the effects of life experiences and mood state (Wilhelm, Niven, Parker, & Hadzi-Pavlovic, 2005).
The Inventory of Depressive Symptomatology - Self-Report (IDS-SR) is a self-report measure of depressive signs and symptoms (Rush et al., 1986). The items provide information about vegetative symptoms, cognitive changes, mood disturbance, “endogenous” features, and anxiety symptoms. The IDS-SR has good internal reliability, strong internal consistency, and adequate construct validity (Rush et al., 1996).
Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q; Endicott et al., 1993). The Q-LES-Q is a 93-item, self-report measure that assesses the degree of satisfaction and pleasure that participants experience in a variety of areas of life functioning. The Q-LES-Q is rated on a 5-point scale, which provide information for several summary scale scores, including physical health, subjective feelings, work, household duties, school/course work, leisure time activities, social relationships, and general activities. Reported test–retest reliability (inter-class coefficient) ranges from .63 to .89 and internal consistency for the Q-LES-Q (Cronbach’s α) has been reported to range from .90 to .96 (Bishop, Walling, Dott, Folkes, & Bucy, 1999). The item from the Q-LES-Q regarding “overall life satisfaction and contentment during the past week” was used as a measure of quality of life. This item was very highly correlated (.91) with the 14-item General Activities subscale of the Q-LES-Q (Endicott et al., 1993) in the present sample. For this measure, a higher score is indicative of greater satisfaction with current quality of life.
Childhood abuse grouping
Subject groups were defined for this study based on CTQ data using the norms published for the 28-item CTQ (version 3). Subjects meeting a “moderate to severe” threshold score on any of the five CTQ subscales (emotional abuse ≥13; physical abuse ≥10; sexual abuse ≥8, emotional neglect ≥15; physical neglect ≥10) were classified into the maltreatment group, whereas individuals meeting the “none” threshold score on all of the five CTQ subscales (emotional abuse ≤8; physical abuse ≤7; sexual abuse ≤5, emotional neglect ≤9; physical neglect ≤7) were designated as the control group. In an effort to make the groups as homogeneous as possible, subjects with intermediate scores suggesting mild abuse were excluded from this analysis.
Subject characteristics
The maltreatment group was comprised of 72 participants (22 men and 50 women), while the control group had 69 subjects (27 men and 42 women). A total of 42 participants, who had intermediate scores on the CTQ were excluded. The subjects in the maltreatment group were significantly older than subjects in the control group (mean ± SD: 36.8 ± 14.1 vs. 25.5 ± 9.7 years, p < .001). Also, current self-rated depressive symptom scores on the IDS-SR were significantly higher in the maltreatment group than in the control group (22.3 ± 13.9 vs. 8.5 ± 9.1, p < .001). Consistent with this, more individuals with a history of maltreatment then subjects without such histories met diagnostic criteria for current major depressive disorder (34.2% vs. 7.2 %, p < .001) and current anxiety disorder (28.5% vs. 7.2%, p < .01); differences in current substance-related disorder were not significant. More maltreated then control subjects met diagnostic criteria for lifetime major depressive disorder (37.1% vs. 14.4%, p < .01), lifetime anxiety disorder (11.5% vs. 31.4%, p < .01), and lifetime substance-related disorder (28.5% vs. 7.2%, p < .01). Overall, a greater proportion of maltreated versus control subjects met criteria for a current (57.1% vs. 20.2%, p < .001) or lifetime Axis I disorder (65.7% vs. 26.0%, p < .001).
PBI quadrant classification
Previously published quadrant classification techniques for characterization of the overall quality of maternal and paternal bonding were used. A summary data point was determined by the intersection of each respondent’s scores for the PBI care factor and the PBI overprotection factor. Published cutoff scores (Parker, 1979; Parker & Hadzi-Pavlovic, 1992) for paternal care and maternal care (≥24 and 27, respectively) and for paternal overprotection and maternal overprotection (≥12.5 and 13.5, respectively) were used to define the plot intersection and resultant quadrants. Quadrant labels defined by Parker et al. (1979) were used to summarize and characterize the overall quality of bonding assessed for each subject. This 2 times 2 categorization based on the intersection of PBI care and overprotection scores results in a single classification of bonding for each parent: “optimal bonding” (high care/low overprotection), “affectionate constraint” (high care/high overprotection), “affectionless control” (low care/high overprotection), or “weak bonding” (low care/low overprotection). Categorical quadrant determinations for bonding with each parent were used for subsequent statistical comparisons between control and maltreatment groups.
Statistical analyses
Categorical and continuous data describing subject characteristics (age, gender, current or lifetime history of Axis I disorders) were compared between groups with χ2 or t tests, as appropriate. Chi-square tests were used to compare the proportion of control and maltreated subjects represented in each quadrant for maternal bonding and for paternal bonding. Partial correlation coefficients were generated to examine the relationships between childhood adversity (total score), gender, and PBI data (total scores for care and overprotection scales for each parent rated by subject) after controlling for age and depression (IDS-SR score). A standard linear regression model was used to evaluate predictors of adult quality of life. Bivariate correlational analyses were also conducted to examine the relationships between childhood adversity (CTQ total score), gender, age, depression score, and the PBI factors prior to doing the regression analysis. Finally, t tests were performed to compare male and female subject data within each of the maltreatment and control groups on the four PBI summary scores (maternal care, maternal overprotection, paternal care, paternal overprotection) and to compare ratings of mothers versus ratings of fathers for the entire subject sample.
Data were analyzed using SPSS version 11.5. All statistical tests were two-tailed, with significance set at p < .05. A Holm’s modified Bonferroni approach was adopted to control for experimentwise error (Holm, 1979), as this correction is more powerful than more traditional approaches (i.e., Tukey test and the Bonferroni correction) when guarding against artificial inflation of Type I error rates (Jaccard, 1998).
Results
Parental bonding experiences
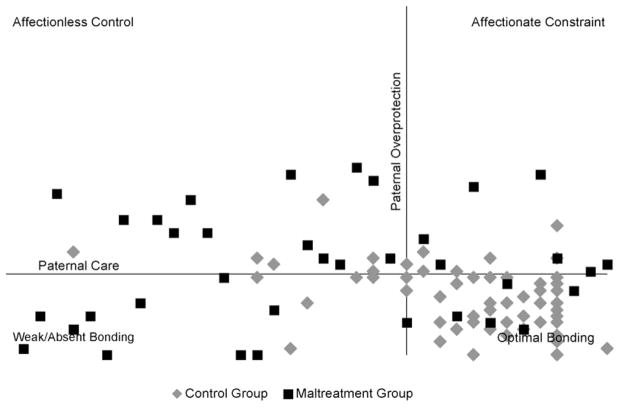
Figures 1 and 2 show the distributions of maltreated and control subjects’ data plotted across the PBI summary quadrants for maternal bonding and paternal bonding, respectively. An analysis using a two-way contingency table was used to evaluate whether the nature of reported maternal bonding experiences (i.e., affectionless control, affectionate constraint, weak/absent bonding, optimal bonding) differs between individuals who report a history of maltreatment and those who do not. Maltreatment and type of maternal bonding were found to be significantly related, Pearson χ2 (3, N = 138) = 76.3, p < .001, Cramér’s V = .74. Of all the individuals reporting each type of maternal bonding, the proportion who reported a history of maltreatment was as follows: .91 for affectionless control, .35 for affectionate constraint, .84 for weak bonding, and .10 for optimal bonding. Pairwise comparisons and probabilities of maltreated individuals reporting non-optimal maternal bonding versus optimal maternal bonding were computed. These results showed that maltreated individuals were 9.1 times more likely to fall in the maternal affectionless control quadrant than the optimal bonding quadrant (.91/.10; p < .001), 3.5 times more likely to report maternal parenting that fell in the affectionate constraint quadrant than the optimal bonding quadrant (.35/.10); p = .025, and 8.4 times more likely to endorse weak maternal bonding experiences than optimal bonding experiences (84/.10; p < .001).
Figure 1.
Quadrants characterize overall quality of maternal bonding as defined by Parker et al. (1979).
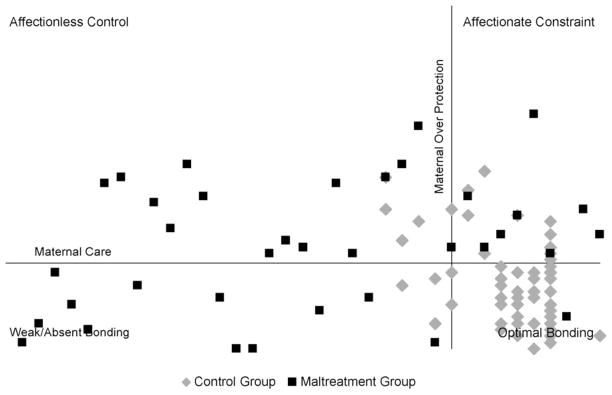
Figure 2.
Quadrants characterize overall quality of paternal bonding as defined by Parker et al. (1979).
A second two-way contingency table analysis was conducted to determine if paternal bonding experiences differed between individuals with and without a history of maltreatment. Once again, maltreatment and type of paternal bonding were significantly associated, Pearson χ2 (3, N = 135) = 70.4, p < .001, Cramér’s V = .67. Among those reporting each type of parental bonding, the proportion that reported maltreatment was .85 for affectionless control, .44 for affectionate constraint, .76 for weak bonding, and .11 for optimal bonding. Maltreated individuals were 7.7 times more likely to report paternal bonding experiences that were characteristic of affectionless control compared to optimal bonding (.85/.11; p < .001), 4.0 times more likely to endorse affectionate paternal constraint compared to optimal paternal bonding (.80/.13; p = .004), and 6.9 times more likely to report weak paternal bonding experiences compared to optimal parental bonding (.76/.11; p < .001).
After controlling for age and IDS-SR scores using partial correlations, CTQ total score was negatively correlated with PBI maternal care [r(130) = −.65, p < .001] and paternal care [r(127) = −.55, p < .001] scores and positively correlated with maternal overprotection [r(130) = .34, p < .001] and paternal overprotection [r(127) = .35, p < .001] scores.
Quality of life
Age, CTQ total score, current depressive symptoms (IDS-SR score), and the PBI parental care and parental overprotection scales were highly correlated with adult quality of life as measured by the Q-LES-Q (Table 1). All of these variables were entered into a multiple regression equation to test for independent contributions to the prediction of quality of life. In a significant regression model [R = .80, F (7, 114) = 29.63, p < .001], only IDS-SR and paternal care emerged as significant predictors. In this model, paternal care was positively associated, and depressive symptoms negatively associated, with adult quality of life (Table 2). The overall model explained 65% of the variance in quality of life scores (R2 = .65, adjusted R2 = .62). Squared semipartial correlations showed that depression scores on the IDS-SR uniquely accounted for 31% of the variance, and paternal care contributed only 1.5% in unique variance. The combination of the independent variables contributed the remaining 32.5%. Childhood maltreatment did not contribute unique variance to the model predicting quality of life, despite the bivariate relationship between these two variables. Multicollinearity as assessed in the regression model by tolerance values was not present. The regression analyses were repeated without individuals with current major depression in order to determine if these results held in a sample without clinical levels of depression. The regression analysis was significant [R = .71, F (7, 96) = 13.91, p < .001], with depressive symptoms and paternal care still remaining significant predictors of quality of life (p < .001 and p = .024, respectively). No other variables were significant.
Table 1.
Bivariate correlations for study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 CTQ | – | ||||||||
| 2 Age | .39* | – | |||||||
| 3 Gender | .11 | −.05 | – | ||||||
| 4 IDS-SR | .49* | .39* | .07 | – | |||||
| 5 PBI - maternal care | −.74* | −.32* | −.25* | −.44* | – | ||||
| 6 PBI - paternal care | −.65* | −.31* | .11 | −.36* | .45* | – | |||
| 7 PBI - maternal overprotection | .42* | .10 | .10 | .30* | −.46* | −.25* | – | ||
| 8 PBI - paternal overprotection | .51* | .25* | .05 | .46* | −.37* | −.43* | .56* | – | |
| 9 Q-LES-Q | −.43* | −.40* | .00 | −.79* | .35* | .39* | −.18* | −.40* | – |
Note: N = 141; CTQ: Childhood Trauma Questionnaire (total score); IDS-SR: Inventory for Depressive Symptomatology, Self-report version; PBI: Parental Bonding Instrument; Q-LES-Q: Quality of Life Enjoyment and Satisfaction Questionnaire;
p < .01.
Table 2.
Standard linear regression on Q-LES-Q rating “overall satisfaction with quality of life”
| Variables | Standardized regression coefficients (B) | t | p |
|---|---|---|---|
| Age | −.006 | −1.30 | .197 |
| IDS-SR | −.056 | −10.45 | .000** |
| CTQ | −.005 | −.19 | .852 |
| PBI - maternal care | −.008 | −.74 | .462 |
| PBI - paternal care | .020 | 2.46 | .015* |
| PBI - maternal overprotection .005 | .54 | .589 | |
| PBI - paternal overprotection | −.004 | −.34 | .732 |
Note: IDS-SR: Inventory for Depressive Symptomatology, Self-report version; CTQ: Childhood Trauma Questionnaire (total score); PBI: Parental Bonding Instrument;
p ≤ .05,
p ≤ .01.
Gender effects
PBI data from both maltreatment and control groups were initially pooled to explore gender effects. The first gender effect analysis examined differences in how subjects described bonding with their female parent in comparison to their male parent. Mean scores for maternal care were significantly higher than those for paternal care [24.81 ± 8.57 vs. 22.32 ± 9.3, t (134) = 3.08, p < .01]. The mean score for maternal overprotection was also somewhat higher than the mean score for paternal overprotection [13.42 ± 8.31 vs. 12.21 ± 7.29, t (134) = 1.91, p ≤ .05].
The next gender effects analysis examined differences related to the gender of the subject within each group. Significant gender differences emerged only for the parental care factor in the maltreatment group. Men with a history of maltreatment reported receipt of greater maternal care than did women with similar histories of maltreatment [31.03 ± 3.04 vs. 30.73 ± 2.66, t(67) = 3.26, p < .01]. In contrast, women in the maltreatment group reported receipt of greater care from their fathers than did men in the same group [27.00 ± 7.15 vs. 29.02 ± 4.77, t(64) = −2.73, p < .01]. No gender differences were found in the reporting of parental overprotection in the maltreatment group. Similarly, no gender effects were found in the control group for parental care or overprotection.
Discussion
The present study examined the nature of parental bonding experiences and the quality of life in individuals with and without a history of childhood maltreatment. Specifically, our aim was to evaluate the more complex relationships between parental bonding, severity of depressive symptoms, childhood maltreatment, and their effect on adult quality of life. As expected, the results of this study suggest a strong association between childhood maltreatment and parental bonding. Fewer adults who report having been exposed to significant childhood maltreatment in the form of abuse and/or neglect reported having optimal parental bonding experiences than did their non-exposed counterparts. Other researchers have noted that abused individuals report poor parental bonding experiences (e.g., Byrne, Velamor, Cernovsky, Cortese, & Losztyn, 1990; Craissati, McClurg, & Browne, 2002). This finding is not surprising given that poor parental care and excessive psychological control or intrusive behavior probably increase susceptibility for, and may even contribute to adverse experiences such as abuse and neglect in childhood (Enns et al., 2002; Hill et al., 2000). In contrast, more capable parents, such as those who were likely to have been rated by our adult subjects as providers of higher quality bonding experiences, are likely to be better able to safeguard their children from adverse circumstances (Enns et al., 2002; Harris, Brown, & Bifulco, 1986).
The results of the present study also showed that other factors, namely the severity of depressive symptoms and the quality of paternal care, are better predictors of quality of life than childhood maltreatment itself. Although childhood maltreatment was associated with quality of life in the bivariate analyses, the multivariate model revealed that this effect was accounted for by shared variance with these other predictor variables. Current levels of depressive symptomatology were most highly predictive of quality of life satisfaction, with 31% of the variance accounted for by this factor. Given the strength of the associations of depressive symptoms with both childhood maltreatment and quality of life, it appears that this factor provides the link between childhood maltreatment and current quality of life. While none of our subjects was seeking or receiving treatment for major depression, a relatively small portion of each group (34.2% of subjects with a history of maltreatment and 7.2 %, of control subjects) met criteria for the disorder. It is possible that adult depressive symptoms in this sample are a consequence of exposure to early life stress (Bifulco, Brown, & Adler, 1991; Brown & Harris, 1993; Lynskey & Fergusson, 1997). Alternatively, depressed mood and affect may have negatively biased subjects’ recall and perceptions of childhood events and primary relationships. However, this hypothesis has been rejected in numerous studies (e.g., Gerlsma, Das, & Emmelkamp, 1993; Gotlib, Mount, Cordy, & Whiffen, 1988; Lizardi & Klein, 2005; Wilhelm et al., 2005), including one that investigated the effect of treatment for depression on the stability of perception of parental rearing over time (De Rubertis, Levy, Busch, Miller, & Kocsis, 2002). Since the present study used a community sample, the association between depression and parental bonding is not likely to have been confounded by the “help-seeking” behavior of a clinical sample, the importance of which has been highlighted by several investigators (e.g., Mackinnon, Henderson, Scott, & Duncan-Jones, 1989; Parker, Hadzi-Pavlovic, Greenwald, & Weissman, 1995).
Quality of paternal care had a small but significant unique influence on adult quality of life, whereas maternal care was not a unique predictor. This finding is distinct from those of other studies, which have highlighted maternal care in the subsequent development of mental disorders (Enns et al., 2002; Oakley-Browne et al., 1995; Rey, 1995), and is contrary to our hypothesis that maternal care would be the strongest PBI predictor of adult quality of life. It is possible that poor paternal care reflects a variety of stressors in the childhood psychosocial environment whose effects persist into adulthood. For example, Fosse and Holen (2002) investigated the childhood environment of adult psychiatric outpatients, comparing those who had been bullied with those who had not. They found that men who had been bullied tended to have grown up without their biological parents or their biological fathers in their formative years, and that bullied women reported having had more adverse experiences during childhood. Hill et al. (2000) observed that the presence of an ideal caring father restricts exposure to adverse circumstances in childhood. Olweus (1993) also found a link between childhood victimization and presence of a disparaging and uninvolved father. He suggested that the absence of an adequate paternal role model (along with the presence of a controlling mother, a temperamental predisposition, and physical weakness) results in the child becoming less self-assured and lacking in confidence, thus becoming an easy target for offensive peers or other abusive individuals.
Consistent with the findings of Parker et al. (1979) in the general population, our pooled subjects described their mothers as more caring and overprotective than their fathers. In addition, maltreated men perceived their fathers as less caring than did maltreated women, whereas maltreated women perceived their mothers as less caring than did maltreated men. It is possible that both men and women perceived their same-gender parent as deficient because they failed to protect them, or may even have contributed to the adverse experiences in childhood.
Limitations
The first limitation of the present study is the use of retrospective measures that involve retrospective and subjective judgments about parental behavior, particularly given the large age range in this study. However, as noted earlier, the PBI has been shown to be independent of mood state (De Rubertis et al., 2002; Gerlsma et al., 1993; Lizardi & Klein, 2005; Wilhelm et al., 2005). The PBI has also demonstrated adequate test–retest reliability for up to 90 months (Lizardi & Klein, 2005) and as long as two decades (Wilhelm et al., 2005). A second limitation is that the mean age and IDS-SR depressive symptom scores were significantly different between the maltreatment and control groups; however, these factors were controlled in the statistical analyses. Third, the inclusion of individuals who met diagnostic criteria for current mild or moderate major depression in this community sample could have compromised our findings, but exclusion of these subjects would have introduced a bias by selecting a supra-normal or uniquely resilient subject group who had been exposed to significant early life adversity and reported little or no adult emotional sequelae. Indeed, subjects who report low parental care or high overprotection (a more common pattern in individuals with early life adversity) are more likely to be depressed (Sato et al., 1998). Fourth, our maltreatment group was comprised of individuals with moderate to severe neglect (12.5%), abuse (31.9%), or both (55.5%). Since other investigators have reported a differential impact of neglect and type of abuse on psychological adjustment and mental disorders (Briere & Runtz, 1990; Gauthier, Stollak, Messe, & Aronoff, 1996), it would be valuable in future work to study homogenous groups of subjects with specific types of neglect (e.g., emotional or physical) or abuse (e.g., emotional, physical, or sexual) in order to independently evaluate the roles of these variables on quality of life in adulthood. Finally, another limitation of the present study is that the sample used was largely self-selected, since these participants responded to advertisements. This could have reduced the representativeness of our sample compared to the general population and thus, affected the generalizabilty of these results to the community at large.
Implications
There are several implications stemming from the results of the current study. First, as expected, childhood maltreatment and negative parental bonding experiences are both associated with poorer quality of life in adulthood and depressive symptoms, and thus, both should be considered targets of intervention for children in terms of facilitating healthy outcomes in adulthood. Secondly, the quality of paternal care was found to be a significant predictor of quality of life in adulthood, even above a history of childhood maltreatment. These results indicate that more attention should be paid to relationships between fathers and their children with regard to protecting children from potential adverse experiences in childhood and contributing to the promotion of their positive adjustment. In addition, the results of the current study demonstrate that depressive symptoms are the best predictor of quality of life in adulthood, independent of childhood maltreatment and levels of parental care. Hence, interventions targeting depressive symptoms in adulthood may help mitigate the negative effects on quality of life that are also associated with early adverse childhood experiences. Research on these topics may contribute to the development of more efficacious prevention and intervention programs for individuals with a history of maltreatment.
In summary, this study underscores the complexity of the relationships between childhood maltreatment and parental bonding, and their sequelae. The findings suggest that childhood maltreatment in itself does not predetermine quality of life in adulthood. Quality of perceived care provided by one’s father emerged as a critical variable. Depression score was found to be the strongest predictor of quality of life. Given that childhood maltreatment increases the risk of depression (Brown & Harris, 1993), childhood maltreatment appears to impact quality of life somewhat indirectly.
Acknowledgments
The authors gratefully acknowledge Kelly Colombo for assistance with data management. Thanks are also due to Butler Hospital Mood Disorder Research Program staff Kelly Grover, B.A., Lauren Wier, B.S., John Carvalho, B.A., and Sandra Tavares, R.N. for their help in collecting the data.
Footnotes
This work was supported in part by a Pfizer/Society for Women’s Health Research (SWHR) 2004 Research Scholar Award to Linda L. Carpenter, M.D. and an Investigator-Initiated Research Grant from Pfizer.
References
- Ainsworth MDS, Bell SM, Stayton DJ. Infant-mother attachment and social development, socialization as a product of reciprocal responsiveness to signals. In: Richards M, editor. The integration of the child in a social world. Cambridge: Cambridge University Press; 1975. [Google Scholar]
- Ainsworth MDS, Blehar MC, Waters E, Wall S, editors. Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Erlbaum; 1978. [Google Scholar]
- Bartholomew K, Horowitz LM. Attachment styles among young adults: A test of a four-category model. Journal of Personality and Social Psychology. 1991;61(2):226–244. doi: 10.1037//0022-3514.61.2.226. [DOI] [PubMed] [Google Scholar]
- Berger D, Ono Y, Saito S, Tezuka I, Takahashi Y, Uno M. Relationship of parental bonding to child abuse and dissociation in eating disorders in Japan. Acta Psychiatrica Scandinavica. 1995;91(4):278–282. doi: 10.1111/j.1600-0447.1995.tb09782.x. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report. San Antonio: Harcourt Brace & Company; 1998. [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Saparetto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Adler Z. Early sexual abuse and clinical depression in adult life. British Journal of Psychiatry. 1991;159:115–122. doi: 10.1192/bjp.159.1.115. [DOI] [PubMed] [Google Scholar]
- Bishop SL, Walling DP, Dott SG, Folkes CC, Bucy J. Refining quality of life: Validating a multidimensional factor measure in the severe mentally ill. Quality of Life Research. 1999;(8):151–160. doi: 10.1023/a:1026489331009. [DOI] [PubMed] [Google Scholar]
- Blain MD, Thompson JM, Whiffen VE. Attachment and perceived social support in late adolescence: The interaction between working models of self and others. Journal of Adolescent Research. 1993;8(2):226–241. [Google Scholar]
- Bogaerts S, Vanheule S, Declercq F. Recalled parental bonding, adult attachment style, and personality disorders in child molesters: A comparative study. Journal of Forensic Psychiatry & Psychology. 2005;16(3):445–458. [Google Scholar]
- Bowlby J. Attachment and loss: Volume I: Attachment. London: Hogarth Press; 1969. [Google Scholar]
- Bowlby J. Attachment and loss: Volume II: Separation. New York: Basic Books; 1973. [Google Scholar]
- Bowlby J. Attachment and loss: Volume III: Loss. New York: Basic Books; 1980. [Google Scholar]
- Briere J, Runtz M. Differential adult symptomatology associated with three types of child abuse histories. Child Abuse & Neglect. 1990;14:357–364. doi: 10.1016/0145-2134(90)90007-g. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO. Aetiology of anxiety and depressive disorders in an inner-city population. 1. Early adversity. Psychological Medicine. 1993;23:143–154. doi: 10.1017/s0033291700038939. [DOI] [PubMed] [Google Scholar]
- Buelow S, Lyddon WJ, Johnson JT. Client attachment and coping resources. Counseling Psychology Quarterly. 2002;15(2):145–152. [Google Scholar]
- Byrne CP, Velamor VR, Cernovsky ZZ, Cortest L, Losztyn S. A comparison of borderline and schizoid patients for childhood life events and parent-child relationships. Canadian Journal of Psychiatry. 1990;35:590–595. doi: 10.1177/070674379003500705. [DOI] [PubMed] [Google Scholar]
- Canetti B, Bachar E, Galili-Weisstub E, Kaplan DA, Shalev AY. Parental bonding and mental health in adolescence. Adolescence. 1997;32(126):381–394. [PubMed] [Google Scholar]
- Carlson V, Cicchetti D, Barnett D, Braunwald K. Disorganized/disoriented attachment relationships in maltreated infants. Developmental Psychology. 1989;25(4):525–531. [Google Scholar]
- Collins NL, Read SJ. Adult attachment, working models, and relationship quality in dating couples. Journal of Personality and Social Psychology. 1990;58(4):644–663. doi: 10.1037//0022-3514.58.4.644. [DOI] [PubMed] [Google Scholar]
- Craissati J, McClurg G, Browne K. The parental bonding experiences of sex offenders: A comparison between child molesters and rapists. Child Abuse & Neglect. 2002;26(9):909–921. doi: 10.1016/s0145-2134(02)00361-7. [DOI] [PubMed] [Google Scholar]
- Datta P, Marcoen A, Poortinga YH. Recalled early maternal bonding and mother- and self-related attitudes in young adult daughters: A cross-cultural study in India and Belgium. International Journal of Psychology. 2005;40(5):324–338. [Google Scholar]
- De Rubertis ST, Levy KN, Busch FN, Miller NL, Kocsis JH. Perceptions of parental bonding in chronically depressed patients treated with desipramine. Paper presented at the 30th Annual Hunter College Psychology Conference; New York. Apr, 2002. Paper retrieved March 22, 2005 from http://urban.hunter.cuny.edu/~klevy/pdf/DeRubetis. [Google Scholar]
- Difilippo JM, Overholser JC. Depression, adult attachment and recollections of parental caring during childhood. Journal of Nervous and Mental Disease. 2002;190(10):663–669. doi: 10.1097/00005053-200210000-00002. [DOI] [PubMed] [Google Scholar]
- Douglas AR. Reported anxieties concerning intimate parenting in women sexually abused as children. Child Abuse & Neglect. 2000;24(3):425–434. doi: 10.1016/s0145-2134(99)00154-4. [DOI] [PubMed] [Google Scholar]
- Duggan C, Sham P, Minne C, Lee A, Murray R. Quality of parenting and vulnerability to depression: Results from a family study. Psychological Medicine. 1998;28(1):185–191. doi: 10.1017/s0033291797006016. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of Life Enjoyment and Satisfaction Questionnaire: A new measure. Psychopharmacology Bulletin. 1993;29(2):321–326. [PubMed] [Google Scholar]
- Enns MW, Cox BJ, Clara I. Parental bonding and adult psychopathology: Results from the US national comorbidity survey. Psychological Medicine. 2002;32(6):997–1008. doi: 10.1017/s0033291702005937. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for the DSM-IV-TR Axis I disorders-Patient edition (SCID-I/P, 11/2002 revision) New York: New York State Psychiatric Institution; 2002. [Google Scholar]
- Fitzgerald MM, Shipman KL, Jackson JL, McMahon RJ, Hanley HM. Perceptions of parenting versus parent-child interactions among incest survivors. Child Abuse & Neglect. 2005;29(6):661–681. doi: 10.1016/j.chiabu.2004.10.012. [DOI] [PubMed] [Google Scholar]
- Fosse GK, Holen A. Childhood environment of adult psychiatric outpatients in Norway having been bullied in school. Child Abuse & Neglect. 2002;26(2):129–137. doi: 10.1016/s0145-2134(01)00312-x. [DOI] [PubMed] [Google Scholar]
- Gauthier L, Stollak G, Messe L, Aronoff J. Recall of childhood neglect and physical abuse as differential predictors of current psychological functioning. Child Abuse & Neglect. 1996;20(7):549–559. doi: 10.1016/0145-2134(96)00043-9. [DOI] [PubMed] [Google Scholar]
- George C. A representational perspective of child abuse and prevention: Internal working models of attachment and caregiving. Child Abuse & Neglect. 1996;20(5):411–424. doi: 10.1016/0145-2134(96)00016-6. [DOI] [PubMed] [Google Scholar]
- George C, Kaplan N, Main M. Adult Attachment Interview. Berkeley, CA: University of California; 1987. Unpublished Interview. [Google Scholar]
- Gerlsma C, Das J, Emmelkamp PMG. Depressed patients’ parental representations: Stability across changes in depressed mood and specificity across diagnoses. Journal of Affective Disorders. 1993;27:173–181. doi: 10.1016/0165-0327(93)90005-5. [DOI] [PubMed] [Google Scholar]
- Gittleman MG, Klein MH, Smider NA, Essex MJ. Recollections of parental behaviour, adult attachment and mental health: Mediating and moderating effects. Psychological Medicine. 1998;28(6):1443–1455. doi: 10.1017/s0033291798007533. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Mount JH, Cordy NI, Whiffen VE. Depression and perceptions of early parenting: A longitudinal investigation. British Journal of Psychiatry. 1988;152:24–27. doi: 10.1192/bjp.152.1.24. [DOI] [PubMed] [Google Scholar]
- Harris T, Brown GW, Bifuco A. Loss of parent in childhood and adult psychiatric disorder: The role of lack of adequate parental care. Psychological Medicine. 1986;16:641–659. doi: 10.1017/s0033291700010394. [DOI] [PubMed] [Google Scholar]
- Hazan C, Shaver P. Conceptualizing romantic love as an attachment process. Journal of Personality and Social Psychology. 1987;52:511–524. doi: 10.1037//0022-3514.52.3.511. [DOI] [PubMed] [Google Scholar]
- Hill J, Davis R, Byatt M, Burnside E, Rollinson L, Fear S. Childhood sexual abuse and affective symptoms in women: A general population study. Psychological Medicine. 2000;30(6):1283–1291. doi: 10.1017/s0033291799003037. [DOI] [PubMed] [Google Scholar]
- Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6:65–70. [Google Scholar]
- Ingram RE, Overby T, Fortier M. Individual differences in dysfunctional automatic thinking and parental bonding: Specificity of maternal care. Personality and Individual Differences. 2001;30(3):401–412. [Google Scholar]
- Jaccard J. Interaction effects in factorial analysis of variance. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Jurmann ID. Childhood sexual abuse, parental bonding, and binge eating. Dissertation Abstracts International. 1999;59(8-B) [Google Scholar]
- Kraaij V, Garnefski N, de Wilde EJ, Dijkstra A, Gebhardt W, Maes S. Negative life events and depressive symptoms in late adolescence: Bonding and cognitive coping as vulnerability factors? Journal of Youth and Adolescence. 2003;32(3):185–193. [Google Scholar]
- Lizardi H, Klein DN. Long-term stability of parental representations in depressed outpatients utilizing the Parental Bonding Instrument. Journal of Nervous and Mental Disease. 2005;193(3):183–188. doi: 10.1097/01.nmd.0000154838.16100.36. [DOI] [PubMed] [Google Scholar]
- Lung FW, Lee FY, Shu BC. The relationship between life adjustment and parental bonding in military personnel with adjustment disorder in Taiwan. Military Medicine. 2002;167(8):678–682. [PubMed] [Google Scholar]
- Lung FW, Huang YL, Shu BC, Lee FY. Parenting rearing style, premorbid personality, mental health, and quality of life in chronic regional pain: A causal analysis. Comprehensive Psychiatry. 2004;45(3):206–212. doi: 10.1016/j.comppsych.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Fergusson DM. Factors protecting against the development in young adults exposed to childhood sexual abuse. Child Abuse & Neglect. 1997;21(12):1177–1190. doi: 10.1016/s0145-2134(97)00093-8. [DOI] [PubMed] [Google Scholar]
- Mackinnon AJ, Henderson AS, Duncan JP. The parental bonding instrument: An epidemiological study in a general population sample. Psychological Medicine. 1989;19(4):1023–1034. doi: 10.1017/s0033291700005754. [DOI] [PubMed] [Google Scholar]
- Mackinnon AJ, Henderson AS, Andrews G. Parental ‘affectionless control’ as an antecedent to adult depression: a risk factor defined. Psychological Medicine. 1993;23:135–141. doi: 10.1017/s0033291700038927. [DOI] [PubMed] [Google Scholar]
- Main M. Introduction to the specials section on attachment and psychopathology. 2. Overview of the field of attachment. Journal of Consulting and Clinical Psychology. 1996;64(2):237–243. doi: 10.1037//0022-006x.64.2.237. [DOI] [PubMed] [Google Scholar]
- Main M, Solomon J. Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation. In: Greenberg MT, Cicchetti D, Cummings EM, editors. Attachment in the preschool years. Chicago: University of Chicago Press; 1990. pp. 51–86. [Google Scholar]
- Mancini F, D’Olimpio F, Prunetti E, Didonna F, Genio MD. Parental bonding: Can obsessive symptoms and general distress be predicted by perceived rearing practices? Clinical Psychology & Psychotherapy. 2000;7:201–208. [Google Scholar]
- Matheson K, Kelly O, Cole B, Tannenbaum B, Dodd C, Anisman H. Parental bonding and depressive affect: The mediating role of coping resources. British Journal of Social Psychology. 2005;44(3):371–395. doi: 10.1348/014466605X37477. [DOI] [PubMed] [Google Scholar]
- Myhr G, Sookman D, Pinard G. Attachment security and parental bonding in adults with obsessive-compulsive disorder: A comparison with depressed out-patients and healthy controls. Acta Psychiatrica Scandinavica. 2004;109(6):447–456. doi: 10.1111/j.1600-0047.2004.00271.x. [DOI] [PubMed] [Google Scholar]
- Oakley-Browne MA, Joyce PR, Wells JE, Bushnell JA, Hornblow AR. Adverse parenting and other childhood experience as risk factors for depression in women aged 18–44 years. Journal of Affective Disorders. 1995;34(1):13–23. doi: 10.1016/0165-0327(94)00099-u. [DOI] [PubMed] [Google Scholar]
- Olweus D. Victimization by peers antecedents and long-term consequences. In: Rubin KH, Asendorpf JB, editors. Social withdrawal, inhibition, and shyness in childhood. Hillsdale, NJ: Lawrence Erlbaum; 1993. pp. 315–341. [Google Scholar]
- Parker G. Parental characteristics in relation to depressive disorders. British Journal of Psychiatry. 1979;134:138–147. doi: 10.1192/bjp.134.2.138. [DOI] [PubMed] [Google Scholar]
- Parker G. The Parental Bonding Instrument: A decade of research. Social Psychiatry and Psychiatric Epidemiology. 1990;25(6):281–282. doi: 10.1007/BF00782881. [DOI] [PubMed] [Google Scholar]
- Parker G, Hadzi-Pavlovic D. Parental representations of melancholic and non-melancholic depressives: Examining for specificity to depressive type and evidence for additive effects. Psychological Medicine. 1992;22:657–665. doi: 10.1017/s0033291700038101. [DOI] [PubMed] [Google Scholar]
- Parker G, Tupling H, Brown LB. A Parental Bonding Instrument. British Journal of Medical Psychology. 1979;52:1–10. [Google Scholar]
- Parker G, Hadzi-Pavlovic D, Greenwald S, Weissman M. Low parental care as a risk factor to lifetime depression in a community sample. Journal of Affective Disorders. 1995;33:173–180. doi: 10.1016/0165-0327(94)00086-o. [DOI] [PubMed] [Google Scholar]
- Parker G, Gladstone G, Wilhelm K, Mitchell P, Hadzi-Pavlovic D, Austin M. Dysfunctional parenting: Over-representation in non-melancholic depression and capacity of such specificity to refine sub-typing depression measures. Psychiatry Research. 1997;73(1–2):57–71. doi: 10.1016/s0165-1781(97)00113-3. [DOI] [PubMed] [Google Scholar]
- Raskin A, Boothe HH, Reatig NA, Schulterbrandt JG, Odle D. Factor analyses of normal and depressed patients’ memories of parental behavior. Psychological Reports. 1971;29:871–879. doi: 10.2466/pr0.1971.29.3.871. [DOI] [PubMed] [Google Scholar]
- Rey JM. Perceptions of poor maternal care are associated with adolescent depression. Journal of Affective Disorders. 1995;34(2):95–100. doi: 10.1016/0165-0327(95)00005-8. [DOI] [PubMed] [Google Scholar]
- Rice KG, FitzGerald DP, Whaley T, Gibbs CL. Cross-sectional and longitudinal examination of attachment, separation-individuation, and college student adjustment. Journal of Counseling & Development. 1995;73(4):463–474. [Google Scholar]
- Roe A, Siegelman M. A parent-child questionnaire. Child Development. 1963;34:355–369. doi: 10.1111/j.1467-8624.1963.tb05143.x. [DOI] [PubMed] [Google Scholar]
- Roisman GI, Collins WA, Sroufe LA, Byron E. Predictors of young adults’ representations of and behavior in their current romantic relationship: Prospective tests of the prototype hypothesis. Attachment & Human Development. 2005;7(2):105–121. doi: 10.1080/14616730500134928. [DOI] [PubMed] [Google Scholar]
- Romans SE, Gendall KA, Martin JL, Mullen PE. Child sexual abuse and later disordered eating: A New Zealand epidemiological study. International Journal of Eating Disorders. 2001;29(4):380–392. doi: 10.1002/eat.1034. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger J, Burns C. The Inventory for Depressive Symptomatology (IDS): Preliminary findings. Psychiatry Research. 1986;18:65–87. doi: 10.1016/0165-1781(86)90060-0. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): Psychometric properties. Psychological Medicine. 1996;26(3):477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Russ E, Heim A, Westen D. Parental bonding and personality pathology assessed by clinician report. Journal of Personality Disorders. 2003;17(6):522–536. doi: 10.1521/pedi.17.6.522.25351. [DOI] [PubMed] [Google Scholar]
- Rutter M. Maternal deprivation reassessed. Harmondsworth; Penguin: 1972. [Google Scholar]
- Sakado K, Kuwabara H, Sato T, Uehara T, Sakado M, Someya T. The relationship between personality, dysfunctional parenting in childhood, and lifetime depression in a sample of employed Japanese adults. Journal of Affective Disorders. 2000;60(1):47–51. doi: 10.1016/s0165-0327(99)00150-0. [DOI] [PubMed] [Google Scholar]
- Salzman JP. Primary attachment in female adolescents: Association with depression, self-esteem, and maternal identification. Psychiatry: Interpersonal and Biological Processes. 1996;59(1):20–33. doi: 10.1080/00332747.1996.11024748. [DOI] [PubMed] [Google Scholar]
- Sato T, Sakado K, Uehara T, Narita T, Hirano S, Nishioka K, Kasahara Y. Dysfunctional parenting as a risk factor to lifetime depression in a sample of employed Japanese adults: Evidence for the ‘affectionless control’ hypothesis. Psychological Medicine. 1998;28(3):737–742. doi: 10.1017/s0033291797006430. [DOI] [PubMed] [Google Scholar]
- Schaefer ES. A configurational analysis of children’s report of parent behavior. Journal of Consulting Psychology. 1965;29:552–557. doi: 10.1037/h0022702. [DOI] [PubMed] [Google Scholar]
- Schreiber R, Lyddon WJ. Parental bonding and current psychological functioning among childhood sexual abuse survivors. Journal of Counseling Psychology. 1998;45(3):358–362. [Google Scholar]
- Turgeon L, O’Connor KP, Marchand A, Freeston MH. Recollections of parent-child relationships in patients with obsessive-compulsive disorder and panic disorder with agoraphobia. Acta Psychiatrica Scandinavica. 2002;105(4):310–316. doi: 10.1034/j.1600-0447.2002.1188.x. [DOI] [PubMed] [Google Scholar]
- Violato C, Arato J. Childhood attachment and adolescent suicide: A stepwise discriminant analysis in a case-comparison study. Individual Differences Research. 2004;2(3):162–168. [Google Scholar]
- Wark MJ, Kruczek T, Boley A. Emotional neglect and family structure: Impact on student functioning. Child Abuse & Neglect. 2003;27(9):1033–1043. doi: 10.1016/s0145-2134(03)00162-5. [DOI] [PubMed] [Google Scholar]
- Wiborg IM, Dahl AA. The recollection of parental rearing styles in patients with panic disorder. Acta Psychiatrica Scandanavia. 1997;96:58–63. doi: 10.1111/j.1600-0447.1997.tb09905.x. [DOI] [PubMed] [Google Scholar]
- Wilhelm K, Niven H, Gordon P, Hadzi-Pavlovic D. The stability of the Parental Bonding Instrument over a 20-year period. Psychological Medicine. 2005;35(3):387–393. doi: 10.1017/s0033291704003538. [DOI] [PubMed] [Google Scholar]
- Wiseman H, Mayseless O, Sharabany R. Why are they lonely? Perceived quality of early relationships with parents, attachment, personality predispositions and loneliness in first-year university students. Personality and Individual Differences. 2006;40(2):237–248. [Google Scholar]
- Zweig-Frank H, Paris J. Parents’ emotional neglect and overprotection according to the recollections of patients with borderline personality disorder. American Journal of Psychiatry. 1991;148(5):648–651. doi: 10.1176/ajp.148.5.648. [DOI] [PubMed] [Google Scholar]