Abstract
Objective
The current pilot study examined the feasibility, acceptability, and initial outcome of an intensive and more condensed version of Parent-Child Interaction Therapy (90 minute sessions for 5 days/week over the course of 2 weeks).
Method
Using an open trial design, 11 children (M child age = 5.01 years) and their mothers completed a baseline period of 2 weeks, a treatment period of 2 weeks, and a post-treatment evaluation. A follow-up evaluation was also conducted 4 months following treatment completion. Across all assessments, mothers completed measures of child behavior and parenting stress, and observational data was collected during three 5-minute standard situations that vary in the degree of parental control (child-led play, parent-led play, & clean-up).
Results
All 11 families completed the intervention with extremely high attendance and reported high satisfaction. Results across both mother report and observations showed that: a) externalizing behavior problems were stable during the baseline period; b) treatment was effective in reducing externalizing behavior problems (ds = 1.67-2.50), improving parenting skills (ds = 1.93-6.04), and decreasing parenting stress (d = .91); and c) treatment gains were maintained at follow-up (ds = .53-3.50).
Conclusions
Overall, preliminary data suggest that a brief and intensive format of a parent-training intervention is a feasible and effective treatment for young children with externalizing behavior problems with clinical implications for improving children's behavioral impairment in a very brief period of time.
Keywords: parent training, PCIT, externalizing behavior problems, child, brief treatment
Early externalizing behavior problems (EBP), including aggression, defiance, inattention, hyperactivity, and impulsivity, have been the focus of considerable theoretical and empirical work (e.g., Broidy et al., 2003; Campbell, 2002; Dodge & Pettit, 2003; Moffitt, 1993; Hinshaw, 2002). In addition to the high prevalence, ranging from 15 to 34% (Nolan, Gadow, & Sprafkin, 2001; Upshur, Wenz-Gross, & Reed, 2009; Kupersmidt, Bryant, & Willoughby, 2000), these problems in early childhood are moderately stable and predictive of other, more serious externalizing and internalizing disorders in later childhood and adolescence (Olson, Bates, Sandy & Schilling, 2002; Mesman, Bongers, & Koot, 2001; Moffitt, Caspi, Dickson, Silva, & Stanton, 1996). For example, two-thirds of preschoolers with elevated behavior problems have been found to receive subsequent mental health diagnoses of Attention-Deficit/Hyperactivity Disorder (ADHD) or another disruptive disorder by age nine, which necessitates costly special education services (Campbell & Ewing, 1990; Redden et al., 2003). Given the deleterious outcomes associated with EBP, as well as the staggering public health costs that accompany special education placements (Pelham, Foster, & Robb, 2007), significant efforts have been made towards developing effective early intervention programs.
Behavioral parent-training interventions are the treatment of choice for young children with EBP (Eyberg, Nelson, & Boggs, 2008; Pelham & Fabiano, 2008), and interventions with considerable evidence include the Triple P-Positive Parenting Program (Sanders, Markie-Dadds, Tully, & Bor, 2000), Incredible Years (Webster-Stratton & Reid, 2003), Helping the Noncompliant Child (McMahon & Forehand, 2003), and Parent-Child Interaction Therapy (PCIT; Zisser & Eyberg, 2010). While these parent training programs are effective, they often last three to four months (Reyno & McGrath, 2006) with some programs such as PCIT not ending until parents reach “mastery criteria,” making them considerably longer for some families (Hembree-Kigin & McNeil, 1995; Harwood & Eyberg, 2006; Reyno & McGrath, 2006). Given the high levels of functional impairment associated with children's EBP and corresponding parental distress (Johnson & Reader, 2002), increasing attention has been gathered on the viability of shortening the delivery of these evidence based programs to maximize rapid improvement.
For example, PCIT has been effective in a relatively shorter fixed dose (e.g., 12 sessions versus 16 or more depending on meeting master criteria) in families at risk or with a history of maltreatment (Thomas & Zimmer-Gembeck, 2012). Additionally, meta-analytic work has demonstrated that early intervention programs with fewer treatment sessions are more effective than those with a higher number of treatment sessions (Bakermans-Kranenburg, Van IJzendoorn, & Juffer, 2003). There is some evidence for the efficacy of even briefer interventions for children's externalizing behavior problems, including a three-session adaptation of the Family Check-Up (FCU; Dishion & Kavanagh, 2003), which uses motivational interviewing to target parenting practices. In comparison to no treatment control, FCU was found to be successful in decreasing destructive behavior (Shaw et al., 2006; Dishion et al., 2013), increasing proactive and positive parenting (Gardner, Shaw, Dishion, Burton, & Supplee, 2007; Dishion et al., 2008), and decreasing maternal depression (Shaw et al., 2009). Abbreviated, four-session interventions have also been successfully implemented within primary care settings, including the Triple P-Positive Parenting Program (Turner & Sanders, 2006) and PCIT (Berkovits, O'Brien, Carter, & Eyberg, 2010). While these brief primary care settings interventions as well as FCU are effective compared to no intervention, their short number of sessions limit the implementation of all treatment components traditionally included in behavioral parent training (e.g., time out) and shown to be important for long term success (Kaminski, Valle, Filene, & Boyle, 2008).
In contrast, a more intensive model, in which all components of treatment are implemented and mastered within a shorter time frame, may serve to reduce functional impairment (e.g., child's behavioral difficulties at school) more quickly, enhance family motivation in a more focused treatment period, thereby increasing participant engagement and perhaps increasing the effect of the intervention (Foa & Steketee, 1987). Providing intervention in a shorter but more focused way has been examined in the internalizing disorders literature. For example, Cognitive-behavioral therapy (CBT) has been successfully used in a brief and intensive manner (90 minute sessions held five days per week for three weeks) to treat pediatric OCD with similar gains compared to CBT delivered once a week for the same time interval (Storch et al., 2007a). Phobia treatment also has been successfully implemented within a very brief period ranging from two weeks to as little as three hours (Davis III, Ollendick, & Öst, 2009; Mörtberg, Berglund, & Sundin, 2005; Mörtberg, Karlsson, Fyring, & Sundin, 2006). Indeed, intensive interventions ostensibly offer opportunity for massed practice and full mastery of intervention criteria prior to termination (Abramowitz, Foa, & Franklin, 2003), but within a condensed time frame, which may be more appealing to some families (Storch et al., 2007b). However, an intensive and brief intervention for EBP has not been examined in the literature. A brief yet intensive parent training intervention would have significant clinical implications as it would potentially alleviate the functional impairment that can result from early externalizing behavior problems (e.g., getting kicked out of preschool) in a more rapid fashion.
The current study is the first to determine the feasibility of implementing a shorter and more intensive form of PCIT to address young children's EBP. In a similar manner to the intensive OCD treatment model described above (Storch et al., 2007a), intensive PCIT (I-PCIT) was delivered in 90-min sessions across five days per week for two weeks. PCIT was chosen as the PT program because PCIT: a) has well established efficacy in reducing young children's EBP (Eisenstadt, Eyberg, McNeil, Newcomb, & Funderburk, 1993; Eyberg, et al., 2001; Hood & Eyberg, 2003; Schuhmann, Foote, Eyberg, Boggs, & Algina, 1998); b) contains all of the treatment components recognized by Kaminski and colleagues’ meta-analysis (Kaminski et al., 2008) as yielding the largest effect sizes (i.e., increasing positive parent-child interactions, promoting consistency and use of time out, and requiring parents to practice new skills with their child during PT sessions); c) aims to strengthen the parent-child relationship, which can be accomplished in a brief intervention (Bakermans-Kranenburg et al., 2003); d) is a competency-based model that emphasizes skill acquisition rather than a fixed set of sessions; and e) includes a unique delivery technique (i.e., wireless headset for the therapist to coach the parent in vivo during interactions with the child) similar to an exposure-based approach in which parents observe “in vivo” changes in their child behavior during sessions. We expected that I-PCIT would be feasible, as evidenced by high treatment attendance, and lead to high parental satisfaction, as well as statistically and clinically significant reductions in children's EBP.
Method
Participants
Participants were 11 children who displayed elevated EBP and whose mothers provided consent to participate in the study. Children were referred to an outpatient child clinic from pediatricians/mental health professionals (36%), school personnel (28%), or were self-referred (36%). The mean age of the participating children was 5 years (range: 3 to 8 years of age), and most of the children were boys (91%) and Hispanic (73%). Ninety-one percent of children were from a two-parent biological family, had at least one parent with a college degree or higher, and had a middle class level of family income (3.5 to 4 ratio of income to poverty). None of the children were currently receiving or had ever taken psychotropic medication or participated in a previous psychosocial treatment.
For study inclusion, the mother had to rate their child above the clinically significant range (T-score ≥ 60) on a measure of child EBP (Eyberg Child Behavior Inventory; Eyberg & Pincus, 1999), be willing to come to treatment every day (Monday – Friday) during a two-week period, and both mother and child had to be able to speak and understand English. Exclusion criteria included an intellectual disability (full scale IQ < 70 based on the WPPSI-III; Wechsler, 2002), Autistic Disorder, or a psychotic disorder for the child or the inability of parents to attend sessions daily. Of the 14 families that contacted our clinic, one child did not meet criteria at the screening evaluation due to scores below the clinically significant range on the measure of EBP, and two families were not able to come to treatment daily during a two week period.
Study Design and Procedure
This study was approved by the University's Institutional Review Board. An open trial was implemented to determine the feasibility, acceptability, and initial outcome of I-PCIT. All families participated in an initial baseline assessment two weeks prior to the start of treatment, followed by a pre-treatment assessment immediately preceding the first treatment session. Following the baseline and pre-treatment assessments, families participated in the intervention for 2 weeks, providing a direct comparison to the 2-week baseline period. Each intervention was conducted by two co-therapists, who were clinical psychology graduate students. All therapists involved in the intervention were formally trained in PCIT, and supervision occurred daily with a licensed clinical psychologist. A post-treatment assessment was conducted within 1 week after the completion of treatment, and a follow-up assessment was conducted 4 months after completion of treatment. Every family completed all assessments. Across all assessments, mothers completed various behavioral and parenting questionnaires, and participated in observations of three 5-minute standard parent-child interaction situations that vary in the degree of parental control (child-led play, parent-led play, and clean-up).
Intervention Description and Adaptation
PCIT is a manualized parent-training intervention with extensive research demonstrating its efficacy (Nixon, Sweeney, Erickson, & Touyz, 2003; Schumann et al., 1998) and long-term maintenance (Boggs et al., 2004; Hood & Eyberg, 2003; Nixon, Sweeney, Erikson, & Touyz, 2004) in treating young children with disruptive behavior disorders. With foundations in attachment and social learning theories, PCIT was designed to alter the pattern of parent-child interaction and thereby change child disruptive behavior. Treatment progresses through two distinct phases: Child-Directed Interaction (CDI) resembles traditional play therapy, and Parent-Directed Interaction (PDI) resembles clinical behavior therapy.
During CDI, parents follow their child's lead in play by using the non-directive PRIDE (i.e., do skills): Praising the child, Reflecting the child's statements, Imitating the child's play, Describing the child's behavior, and using Enjoyment. They learn to apply PRIDE skills to the child's appropriate play and ignore undesirable behaviors, and are taught to avoid verbalizations that take the lead away from the child during the play (i.e., don't skills), including questions, commands, and negative statements (e.g., criticism). During PDI, parents set limits to reduce child noncompliance and negative behavior. They learn to use effective commands and consistently follow through with timeout for noncompliance. Parents are also taught variations of the PDI procedure to deal with aggressive behavior and public misbehavior. During all sessions, the therapist coaches each parent in vivo through a one-way mirror (using a wireless headset) in their use of the CDI and PDI skills with their child.
The adaptation of PCIT in the current study involved only changing the length of the intervention; no changes to the core skills and principles of treatment were made. Specifically, families attended 90-minute sessions, 5 days a week for 2 weeks. During the first session, a “teach” session of CDI was conducted, in which the mother learned and briefly practiced skills with the therapist. This was followed by four coaching sessions in which the therapist actively coached the mother towards mastery of the interaction skills. During the second week, a teach session of PDI was conducted followed by four coaching sessions in which the therapist actively coached the mother on using effective commands and implementing the time out procedures. CDI continued to be assessed and coached along with PDI skills in the PDI phase of treatment. Given the time-limited structure of the intervention, all families received 10 total sessions, and CDI and PDI mastery criteria was not required for treatment completion.
Measures
EBP
Mothers completed the Eyberg Child Behavior Inventory (ECBI; Eyberg & Ross, 1978), a 36-item questionnaire that is designed to assess the presence of externalizing or conduct problems in children ages 2 through 16 years. Mothers were asked to rate each behavior on a 7-point intensity scale that indicates how often the behaviors currently occur. The ECBI requires approximately 10 minutes to complete and can be scored by hand in two minutes. The ECBI has been found to have high reliability and validity across age and socioeconomic status (Colvin, Eyberg, & Adams, 1999; Eyberg & Robinson, 1983). The total raw intensity scale score was used in the current study as the main measure of EBP (α's = .85-.93).
Parenting Skills and Child Compliance
The Dyadic Parent-Child Interaction Coding System (DPICS), a behavioral coding system with documented reliability and validity (Eyberg, Nelson, Duke, & Boggs, 2005), was used to measure the quality of parent-child interactions across all assessments. Several categories of parent and child behaviors may be selected and are coded by recording the frequency of each occurrence in real time using a video coding system. The current study focused on the extent to which I-PCIT was effective in changing parenting skills and child compliance. Consistent with prior PCIT research (Bagner, Sheinkopf, Vohr, & Lester, 2010; Chaffin et al., 2004), we created a composite of do skills (behavior descriptions, reflections, praises) and don't skills (questions, commands, and negative talk) reflecting behaviors parents are taught during treatment to use and not use during a child-led play. Children's average compliance levels across the parent directed play and clean-up situations were also calculated (i.e., ratio of number of complies to number of commands). Undergraduate student coders, who were masked to whether children were receiving treatment or not, were trained to 80% agreement with a criterion tape and coded 37% of the observations a second time to assess reliability. Reliability for the do and don't skills as well as rates of compliance were excellent (r's range from .71 to .99).
Parenting Stress
Mothers completed the Parenting Stress Index-Short Form (PSI-SF; Abidin, 1983). The PSI-SF is a 36-item self-report instrument for parents of children ages 1 month to 12 years containing three subscales (Parent Distress, Parent-Child Dysfunctional Interaction, Difficult Child) with Cronbach's alphas of .87, .80, and .85, respectively, and 6-month test-retest reliabilities of .85, .68, and .78, respectively (Abidin, 1983). The PSI and the PSI-SF total scores are highly correlated with one another (.94). On the long form of the PSI, higher scores have been associated with increased severity of conduct-disordered behavior (Ross, Blanc, McNeil, Eyberg, & Hembree-Kigin, 1998). The PSI-SF total raw score was used to assess the effects of I-PCIT on overall parenting stress (α's = .90-.97).
Discipline Strategies
Mothers completed the Parenting Scale (PS; Arnold, O'Leary, Wolff, & Acker, 1993), a 30-item self-report measure that assesses parental discipline practices of children as young as 18 months. The effectiveness of discipline techniques is measured based on three factor scores (Laxness, Over-Reactivity, Verbosity) and a total score yielding good internal consistency (α = .83, .82, .63 and .84, respectively). The PS total score correlated .73 with observed parent dysfunctional discipline practices (Arnold, et al., 1993) and .53 with maternal report of self-confidence (Morawska & Sanders, 2007). The three scales of the PS were used to assess the effects of I-PCIT on parenting practices (α's =.62-.86 for laxness; .55-.84 for over-reactivity; .61-.71 for verbosity).
Treatment Satisfaction
The Therapy Attitude Inventory (TAI; Brestan, Jacobs, Rayfield, & Eyberg, 1999) is a 10-item parent-report measure that assesses parent satisfaction with treatment. Test-retest reliability over a four month period and correlations between the TAI and both parent-rating scales and observational measures of treatment change have been demonstrated (Brestan et al., 1999). The TAI total score was administered at the post-intervention assessment to assess parent satisfaction with the intervention.
Data Analysis Plan
Given the open trial design and four assessment points, we conducted multiple repeated measures ANOVAs. Although we did not have a between-subjects factor, within-subjects follow-up contrast tests, with a Bonferroni correction to minimize type 1 error, were conducted to first establish the baseline period (i.e., no significant differences from the initial to pre-treatment assessments) followed by contrasts between the pre-treatment and post-treatment as well as follow-up assessments. Cohen's d effect size estimates ([pre-treatment – post-treatment/follow-up]/pooled SD) were provided for all treatment and follow-up analyses.
Results
Preliminary Analyses, Intervention Feasibility and Acceptability
Preliminary analyses indicated no significant associations between demographic variables and the treatment outcome variables (i.e., parenting measures, child EBP). All 11 families completed the intervention with impressive attendance over the course of 10 sessions. Of the possible 110 treatment sessions, only one session was missed by a single family and rescheduled. All sessions were videotaped and therapists completed fidelity checklists each session. Twenty percent of sessions were randomly selected for fidelity reliability probes (coded by a masked research assistant). Accuracy, defined as the percent with which the therapist adhered to key elements of each session detailed in the PCIT treatment manual, was 99% (range = 97 to 100%). Parents also reported high satisfaction and acceptance with the intervention on the TAI (M = 48.10 out of a possible 50, range from 43 to 50).
Parenting Outcomes
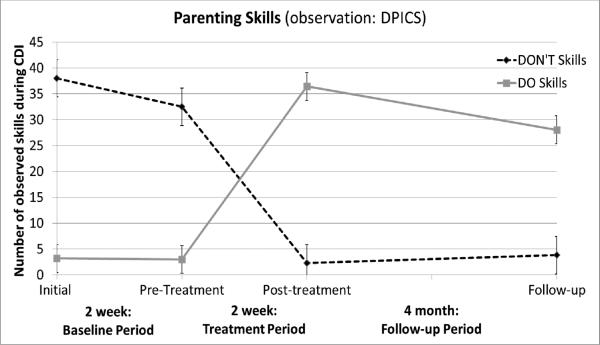
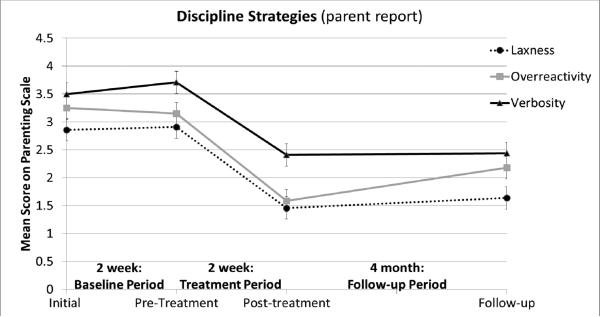
As indicated in Table 1, all parenting outcomes were stable during the baseline period, and no statistically significant differences occurred between the initial baseline and pre-treatment assessments. Significant changes were observed from pre-treatment to post-treatment for parenting skills (Cohen's d = 6.04 and 3.51 for do skills and don't skills, respectively), discipline strategies (d = 2.28, 1.93, and 2.35 for Laxness, Verbosity, and Overreactivity, respectively), and parenting stress (d = .91 for total stress). Significant changes were also evidenced from pre-treatment to the follow-up assessment in terms of parenting skills (d = 3.50 and 3.21 for do skills and don't skills, respectively), discipline strategies (d = 1.78, 1.97, and 1.09 for Laxness, Verbosity, and Overreactivity, respectively), and parenting stress (d =.53 for total stress). Overall, and as expected, mothers significantly improved their parenting skills, displaying higher levels of do skills and lower levels of don't skills during child-led play (Figure 1). Additionally, parents also exhibited significantly more effective discipline strategies, as measured by reported decreased levels of laxness, verbosity, and overreactivity (Figure 2), and lowered stress levels following I-PCIT (see Table 1 for summary).
Table 1.
Summary of results
| Initiala | Pre-treatmentb | Post-treatmentc | Follow-upd | F score | pValue | |
|---|---|---|---|---|---|---|
| Parenting Measures | ||||||
| DPICS: “Do skills” (O) | 3.20 (1.05) | 3.00 (.95) | 36.45 (2.16) | 28.09 (2.91) | 91.64*** | 1.00ab,< .001ac, <.001bc, <.001 <.001ad, bd, .11cd |
| DPICS: “Don't skills” (O) | 38.00 (3.91) | 32.55 (3.64) | 2.27 (.524) | 3.82 (1.14) | 31 79*** | .938ab, <.001ac, <.001bc, <.001b <.001bd, .927cd |
| PS: Discipline Strategies: Laxness (P) | 2.86 (.262) | 2.90 (.246) | 1.46 (.111) | 1.65 (.175) | 14.62** | 1.00ab, <.001bc <.001ac, .001bd, .001ad, , .883cd |
| PS: Discipline Strategies: Verbosity (P) | 3.50 (.275) | 3.71 (.222) | 2.41 (.204) | 2.44 (.151) | 63.87*** | .829ab,<.001bc .002ac,, .001abc.019ad,, 1.00cd |
| PS: Discipline Strategies: Overreactivity (P) | 3.25 (.180) | 3.15 (.265) | 1.59 (.100) | 2.18 (.272) | 20.21*** | 1.00ab, .001bc, <.001ac .006bd, , .004ad, .163cd |
| PSI: Parenting Stress total raw score (P) | 86.00 (5.38) | 79.64 (6.17) | 61.00 (6.16) | 66.91 (8.18) | 15.27** | .369ab, .002bc, .002ac, .168bd, .034ad,1.00cd |
| Child Behavior Measures | ||||||
| ECBI: Externalizing behavior problems (P) | 154.36 (8.86) | 146.64 (7.77) | 91.73 (4.91) | 102.91 (9.46) | 13.01** | 1.00ab, .001bc, .001ac, .004bd, .003ad, 1.00cd |
| DPICS: Compliance% (O) | 51.93 (5.26) | 50.43 (8.11) | 86.27 (4.22) | 81.30 (3.22) | 10.24** | 1.00ab, .036bc, .006ac, .014bd, .001ad,1.00cd |
Note. Values enclosed in parentheses represent standard errors. DPICS = Dyadic Parent Interaction Coding System, PS = Parenting Scale, PSI = Parenting Stress Index Short-Form, ECBI = Eyberg Child Behavior Inventory, O = observational measure, P = Parent report measure. P-values are reported for contrast tests between assessment periods (e.g., ab = comparison of initial and pre-treatment assessments).
Figure 1.
Results of parenting skills (observational). Note. CDI = Child Directed Interaction, Interaction Coding System. DPICS = Dyadic Parent
Figure 2.
Results for discipline strategies (parent report).
Child Behavior Outcomes
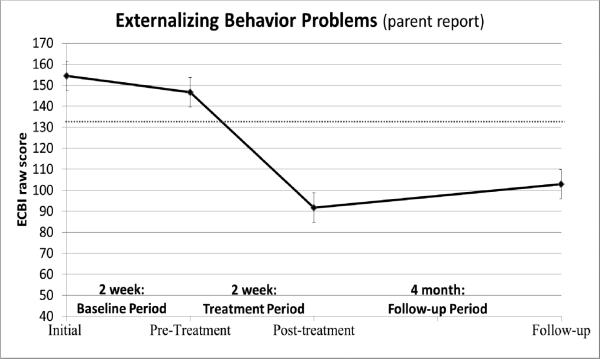
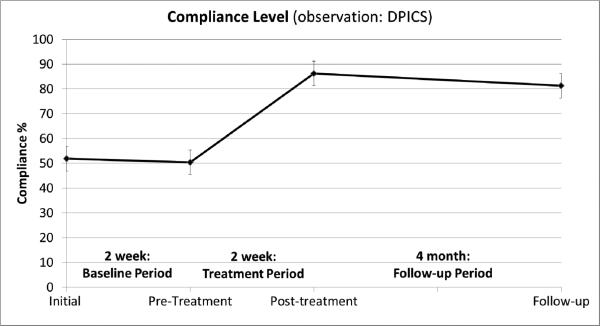
Similar to the parenting outcomes and as displayed in Table 1, child EBP, as reported by mothers and as observed during parent-directed and clean-up tasks, were stable during the baseline period (i.e., no statistically significant differences between the initial and pre-treatment assessments). Significant changes were observed from pre-treatment to post-treatment in terms of both parent reported externalizing behavior problems (Cohen's d = 2.50) and observed compliance (d = 1.67). Significant changes were also observed from pre-treatment to the follow-up assessment (parent report of EBP d = 1.51, and observed compliance d = 1.51). Consistent with our hypotheses, parents reported decreased levels of child EBP (Figure 3) and increased levels of compliance were observed during structured assessments following I-PCIT (Figure 4). In terms of the clinical significance of our findings, none of the 11 children were rated above the clinical cut-off according to the ECBI (T-score > 60) at the post-treatment assessment, and only one child was rated above the clinical cut-off during the follow-up assessment.
Figure 3.
Results for externalizing behavior problems (parent) report. Note. ECBI = Eyberg Child Behavior Inventory, Clinical cut-off score (132) is depicted by dashed grey line.
Figure 4.
Results for child compliance level across parent-directed and clean up tasks. DPICS = Dyadic Parent Interaction Coding System.
Comparing to Traditional PCIT
We also compared the current study's effect sizes to those found in traditional PCIT, both single group and independent group comparisons, as reported by a meta-analysis (Thomas & Zimmer-Gembeck, 2007). The effect sizes (pre- to post-treatment) found for child behavior outcomes in the current study are larger than those reported in traditional PCIT: observed compliance d = .61-.94 (traditional PCIT) vs. d = 1.67 (current study I-PCIT); parent report of EBP d = 1.31-1.45 (traditional PCIT) vs. d = 2.50 (current study I-PCIT). The maintenance of such gains (pre-treatment to 3-4 month follow-up) were also larger in the current study versus traditional PCIT: observed compliance d = 0.30 (traditional PCIT) versus d = 1.51 (current study I-PCIT); parent report of EBP d = 1.10 (traditional PCIT) versus d = 1.51 (current study I-PCIT).
Lastly, the effect sizes (pre- to post-treatment) found for parenting outcomes (observed do and don't skills and parenting discipline practices) in the current study (d = 1.93-6.04) were also larger than those reported in traditional PCIT (d = 1.11-3.11) and were better maintained at the 3-4 month follow-up: d = 1.09-3.50 (current study I-PCIT) versus d = 0.61-0.94 (traditional PCIT).
Discussion
The current study examined in an open trial the feasibility, acceptability, and initial outcome of a shorter and intensive version (90 minute sessions held 5 days/week for 2 weeks) of PCIT, an evidence-based parent-training intervention for childhood EBP. First, it is important to note that 85% of parents approached about the study were willing to enroll in the brief and intensive version of PCIT rather than the traditional PCIT format, which averages 12 to 14 sessions over 3 to 4 months. I-PCIT was feasible and acceptable to all enrolled families with an impressive 100% attendance rate and 0% attrition rate. Parents who completed the program were also highly satisfied with treatment (M = 48.10 out of a possible 50 on the TAI). In the context of our small sample size, our excellent attendance and zero drop-out rate fare well when compared to drop-out of approximately 40% in standard PCIT (Boggs et al., 2004; Werba et al., 2006), and even more impressive relative to other evidenced-based PT programs with attrition rates approaching 50% (Reyno & McGrath, 2006). Given the success within the internalizing literature of conducting shorter and intensive family-based behavioral treatment (exposure and response prevention) for childhood OCD (Storch et al., 2007a), our open trial results indicate that a similar format can be easily adapted for parent-training models that focus on externalizing problems.
Second, we found significant improvements in mothers’ parenting skills as indicated by both observational measures and self-report. Specifically, mothers were able to learn and implement greater use of positive do skills, such as labeled praises and behavioral descriptions, and fewer directive and negative verbalizations when interacting with their children in a child-led play situation. These improvements in parenting skills are consistent with research on standard PCIT over the course of four months (Bagner & Eyberg, 2007; Bagner et al., 2010). Additionally, parents reported an improvement in their parenting discipline strategies, including a reduction in laxness, making consequences more concrete rather than overly explaining, and staying calmer when implementing discipline. In addition to changes in parenting skills, mothers reported reduced overall parenting stress. Importantly, especially given the brief, 2-week period of treatment, improvements in mothers’ parenting skills, discipline strategies, and parenting stress were maintained 4 months after treatment completion. Although various PT models have been successful in targeting these parenting factors (Beauchaine, Webster-Stratton, & Reid, 2005; Eddy & Chamberlain, 2000), our study contributes to the literature by showing that these important parenting mechanisms can be changed within a short period of time.
In addition to demonstrating changes in parenting, our results also indicated that children's EBP significantly improved as measured by both observation and parent report. During the baseline period, children were compliant with only 50% of parents’ commands but improved their rate of compliance to 86% immediately after treatment, and maintained gains at 80% at 4-month follow-up. Consistent with the results on parent report of child EBP from the Family Check-Up (FCU; Shaw et al., 2006; Gardner et al., 2007), our findings suggest that a brief but intensive intervention can be successful in both reducing young children's EBP, while extending findings to observed child compliance.
Other work using brief versions of PT (e.g., Turner & Sanders, 2006; Berkovits et al., 2010) yield findings consistent with those reported here. However, these other studies primarily targeted preschool children with subclinical EBP, with the Berkovits et al. (2010) study ruling out children exhibiting clinically elevated EBP, and the Turner & Sanders (2006) study acknowledging “low overall level of disruptive child behavior” when compared to previous Triple P outcome studies. Additionally, the Turner & Sanders (2006) study did not find significant improvements in observed measures of both parenting and child behavior. Finally, the brief versions of treatment in both studies were implemented weekly over the course of four to eight weeks in comparison to the two weeks in the current study. All children in the current study presented with clinically significant levels of EBP pre-treatment, providing initial support that brief, intensive PT interventions may be helpful for children experiencing more severe behavior problems. Additionally, our findings mark the first successful demonstration of a shorter and intensive version of an evidence-based parent-training intervention in yielding positive changes in parenting and child behavior based on parent-report and observation and maintaining over a four month follow-up. In fact, the effect sizes found in the current study at both the post-treatment and 3-4 month follow-up assessments are larger than those reported in traditional PCIT studies (see Thomas & Zimmer-Gembeck, 2007).
Compared to studies of children with subclinical or absent EBPs, the severity of behavior in the present study may have influenced parental willingness to engage in treatment by providing increased motivation to use PCIT strategies, both at home and in the clinic, in an effort to remediate difficult behavior. Further, families in the current study all reported increased motivation to participating in treatment due to setting up an a priori time frame over a short period of time that is solely dedicated to helping their child. Such enhanced motivation has also been reported within the intensive internalizing treatment literature (Foa & Steketee, 1987; Storch et al., 2007a). The unique in vivo training aspect of PCIT also may play a role in enhancing family motivation because parents observe changes in their own skills and the impact their changes can have on improving their child's behavior and reducing their functional impairment. Similar to exposure and response prevention in treatment for OCD, parents in PCIT experience putting their child in time out and the considerable decrease in the length and severity of the time out situation each day, which may increase parental confidence at home. It will be important for future studies to examine whether the intensive format of PCIT does in fact influence parent motivation and confidence, and whether this intensive format can be effective with other parent-training programs that use video modeling rather than in-vivo training (e.g., Incredible Years).
There were some limitations to the current study that need to be addressed. First, with no control group, threats to validity, such as regression to the mean, cannot be completely ruled out so caution should be used in interpreting our results. Although randomized control trials (RCTs) have increasingly become the “gold standard” of intervention research, especially when establishing the efficacy and effectiveness of a particular treatment (e.g., Chambless & Ollendick, 2001), there has been increasing recognition of the benefits of conducting well-controlled single-case experimental studies or smaller open trials that contain a within-design baseline (such as the one in the present study) when assessing the practicality and utility of clinical interventions (Morgan & Morgan, 2001), or when determining the processes and patterns associated with change (Borckardt et al., 2008; Westen & Bradley, 2005). . Indeed, single-case research has been noted as integral to establishing evidence-based practices (Horner et al., 2005). For example, while it does not resolve several problems of non-randomization, the fact that the current study found no significant changes in any measure of parenting factors or child behavior during the 2-week baseline period, which was equivalent to the time frame of treatment, indicates that at least the passage of time did not seem to affect treatment outcome. A randomized controlled trial comparing I-PCIT to both a control group and standard PCIT would provide further confidence in these findings and would be important to address a potential self-selection bias for parents choosing an intensive treatment.
Second, while the small sample size that accompanies an open trial is a limitation, our findings were statistically significant, with large effect sizes that are comparable to larger trials of standard PCIT. A third limitation was the homogeneity of the sample, which was largely Hispanic (73%) and middle SES. However, Hispanic children represent the fastest growing group in the U.S. but are understudied in child intervention research (La Greca, Silverman, & Lochman, 2009). Of course, it is important to recognize that the excellent attendance and attrition rates also may have been related to other sample demographics as middle to upper SES intact families tend to have better attendance and completion rates across PT studies (Lundahl, Risser, & Lovejoy, 2006). Moving forward with the development of I-PCIT, it will be important to examine whether I-PCIT can be effective for higher risk families, such as those from lower SES who often have more treatment barriers (Bagner & Graziano, 2013). Furthermore, the present study was conducted in a university-based clinic setting with a high availability of mental health providers. Future research should seek to determine the feasibility of disseminating such services in other (e.g., traditional outpatient and/or medical) settings in which clinician time and availability may be more limited. Notably, other intensive therapies, such as those for pediatric OCD, suggest the feasibility and efficacy of delivering interventions across different settings (Franklin et al., 1998; Whiteside & Jacobsen, 2010)
A final limitation was the lack of data on children's behavior at school to measure generalization of treatment effects. Anecdotally, some parents who completed I-PCIT commented that their child's preschool teacher reported improvements in behavior, and findings generalizing effects of standard PCIT to the school setting have been reported (Funderburk et al., 1998; McNeil, Eyberg, Eisenstadt, Newcomb, & Funderburk, 1991). It will be important for future studies to examine the extent to which improvements seen within the course of a brief and intensive treatment generalizes to the school environment.
Regarding clinical implications, mental health professionals should be aware that some families may prefer and be able to learn specialized behavioral parent-training skills in a brief and intensive format. Hence, it may be useful to offer families a choice in the format of parent training to increase treatment compliance. Of course, the feasibility of delivering this type of intense yet brief treatment also may be dependent on families’ insurances which vary greatly in terms of the number of sessions covered as well as how many visits are allowed on a weekly basis. The small open trial presented here precludes conducting any significant cost-effective analyses, but it will be important for future work to continue to explore how brief PT programs can be administered to a larger number of parents while maintaining their efficacy. Barring any financial factors, it is important to note that the summer, winter, or spring breaks for most schools may be a particularly feasible time for families to attend therapy in a more intensive manner. In fact, the Summer Treatment Program (STP) for children with ADHD, which provides treatment 5 days a week for 8 weeks, bodes one of the best PT attendance rates at over 95% among elementary (Pelham et al., 2010) and 92% among preschool age children (Graziano et al., 2014).
Although certain parent training programs such as PCIT require that parents achieve a “mastery criteria” prior to moving onto other sessions (which may result in longer treatment periods), our data as well as data from other briefer PCIT studies (e.g., Berkovits et al., 2010; Nixon et al., 2003), suggest that a time limited approach is equally effective. While we are not suggesting that the “mastery criteria” in traditional PCIT be removed, it is important to recognize that no study, to our knowledge, has examined the incremental validity in outcomes for parents who achieved “mastery criteria” versus those that fall just short. The live coaching and feedback provided to parents regarding their parenting skills is what makes PCIT unique and while the spirit of achieving a “mastery criteria” is well intended, it may be just as important to offer families the flexibility of moving towards the second phase of PCIT prior to achieving this criteria.
In summary, the current study focused on a novel and relatively unexplored research question by examining the feasibility, acceptability, and initial outcome of a shorter and intensive form of an established parent-training program (i.e., PCIT) to improve young children's EBP. All families completed the intervention with close to perfect attendance and reported very high satisfaction with treatment. Large effect sizes following I-PCIT were demonstrated across both mother report and observations of parent-child interactions, and these gains were maintained at a 4-month follow up. While conducting an RCT is the next step in validating our findings, it appears that a briefer and intensive parent-training intervention may be effective for young children with EBP.
References
- Abidin RR. Parenting stress index: Manual, administration booklet,[and] research update. Pediatric Psychology Press; Charlottesville, VA: 1983. [Google Scholar]
- Abramowitz JS, Foa EB, Franklin ME. Exposure and ritual prevention for obsessive-compulsive disorder: Effects of intensive versus twice-weekly sessions. Journal of Consulting and Clinical Psychology. 2003;71:394–398. doi: 10.1037/0022-006x.71.2.394. [DOI] [PubMed] [Google Scholar]
- Arnold DS, O'Leary SG, Wolff LS, Acker MM. The Parenting Scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment. 1993;5:137–144. doi: 10.1037//1040-3590.5.2.137. [Google Scholar]
- Bagner DM, Eyberg SM. Parent–child interaction therapy for disruptive behavior in children with mental retardation: A randomized controlled trial. Journal of Clinical Child and Adolescent Psychology. 2007;36:418–429. doi: 10.1080/15374410701448448. [DOI] [PubMed] [Google Scholar]
- Bagner DM, Graziano PA. Barriers to success in parent training for young children with developmental delay: The role of cumulative risk. Behavior Modification. 2013;37:356–377. doi: 10.1177/0145445512465307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Sheinkopf SJ, Vohr BR, Lester BM. Parenting intervention for externalizing behavior problems in children born premature: An initial examination. Journal of Developmental and Behavioral Pediatrics. 2010;31:209–216. doi: 10.1097/DBP.0b013e3181d5a294. doi: 10.1097/DBP.0b013e3181d5a294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, Van IJzendoorn MH, Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin. 2003;129:195–215. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- Baumrind D. The influence of parenting style on adolescent competence and substance use. The Journal of Early Adolescence. 1991;11:56–95. doi: 10.1177/0272431691111004. [Google Scholar]
- Beauchaine TP, Webster-Stratton C, Reid MJ. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: A latent growth curve analysis. Journal of Consulting and Clinical Psychology. 2005;73:371–388. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- Berkovits MD, O'Brien KA, Carter CG, Eyberg SM. Early identification and intervention for behavior problems in primary care: A comparison of two abbreviated versions of parent-child interaction therapy. Behavior Therapy. 2010;41:375–387. doi: 10.1016/j.beth.2009.11.002. doi: 10.1016/j.beth.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Boggs SR, Eyberg SM, Edwards DL, Rayfield A, Jacobs J, Bagner D, Hood KK. Outcomes of parent-child interaction therapy: A comparison of treatment completers and study dropouts one to three years later. Child & Family Behavior Therapy. 2004;26(4):1–22. doi: 10.1300/J019v26n04_01. [Google Scholar]
- Borckardt JJ, Nash MR, Murphy MD, Moore M, Shaw D, O'Neil P. Clinical practice as natural laboratory for psychotherapy research. American Psychologist. 2008;63:1–19. doi: 10.1037/0003-066X.63.2.77. doi: 10.1037/0003-066X.63.2.77. [DOI] [PubMed] [Google Scholar]
- Breslau J, Miller E, Breslau N, Bohnert K, Lucia V, Schweitzer J. The impact of early behavior disturbances on academic achievement in high school. Pediatrics. 2009;123:1472–1476. doi: 10.1542/peds.2008-1406. doi: 10.1542/peds.2008-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brestan E, Jacobs J, Rayfield A, Eyberg SM. A consumer satisfaction measure for parent-child treatments and its relationship to measures of child behavior change. Behavior Therapy. 1999;30:17–30. doi: 10.1016/S0005-7894(99)80043-4. [Google Scholar]
- Broidy LM, Nagin DS, Tremblay RE, Bates JE, Brame B, Dodge KA, Laird R. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: A six-site, cross-national study. Developmental Psychology. 2003;39:222–245. doi: 10.1037//0012-1649.39.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell S. Behavior problems in preschool children: Clinical and developmental issues. 2nd ed. Guilford Press; New York, NY: 2002. [Google Scholar]
- Campbell S. Behavior problems in preschool children: A review of recent research. Journal of Child Psychology and Psychiatry. 2006;36:113–149. doi: 10.1111/j.1469-7610.1995.tb01657.x. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, Bonner BL. Parent-child interaction therapy with physically abusive parents: efficacy for reducing future abuse reports. Journal of Consulting and Clinical Psychology. 2004;72:500–510. doi: 10.1037/0022-006X.72.3.500. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Funderburk B, Bard D, Valle LA, Gurwitch R. A combined motivation and parent-child interaction therapy package reduces child welfare recidivism in a randomized dismantling field trial. Journal of Consulting and Clinical Psychology. 2011;79:84–95. doi: 10.1037/a0021227. doi: 10.1037/a0021227. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Valle LA, Funderburk B, Gurwitch R, Silovsky J, Bard D, Kees M. A motivational intervention can improve retention in PCIT for low-motivation child welfare clients. Child Maltreatment. 2009;14:356–368. doi: 10.1177/1077559509332263. doi: 10.1177/1077559509332263. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annual Review of Psychology. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Chacko A, Fabiano GA, Wymbs BT, Pelham WE. Enhancements to the behavioral parent training paradigm for families of children with ADHD: Review and future directions. Clinical Child and Family Psychology Review. 2004;7:1–27. doi: 10.1023/b:ccfp.0000020190.60808.a4. doi: 10.1023/B:CCFP.0000020190.60808.a4. [DOI] [PubMed] [Google Scholar]
- Colvin A, Eyberg SM, Adams CD. Restandardization of the eyberg child behavior inventory. Retrieved December. 1999;3:2012. from http://www.pcit.org. [Google Scholar]
- Davis TE, III, Ollendick TH, Öst LG. Intensive treatment of specific phobias in children and adolescents. Cognitive and Behavioral Practice. 2009;16:294–303. doi: 10.1016/j.cbpra.2008.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denham SA. Social-emotional competence as support for school readiness: What is it and how do we assess it? Early Education and Development. 2006;17:57–89. doi: 10.1207/s15566935eed1701_4. [Google Scholar]
- Dishion TJ, Brennan L, Shaw D, McEachern A, Wilson M, Booil J. Prevention of problem behavior through annual family check-ups in early childhood: Intervention effects from home to early elementary school. Journal of Abnormal Child Psychology. doi: 10.1007/s10802-013-9768-2. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Kavanagh K. Intervening in adolescent problem behavior: A family-centered approach. Guilford Press; New York, NY: 2003. [Google Scholar]
- Dodge KA, Pettit GS. A biopsychosocial model of the development of chronic conduct problems in adolescence. Developmental Psychology. 2003;39:349–371. doi: 10.1037//0012-1649.39.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy JM, Chamberlain P. Family managment and deviant peer association as mediators of the impact of treatment condition on youth antisocial behavior. Journal of Consulting and Clinical Psychology. 2000;68:857–863. doi: 10.1037/0022-006X.68.5.857. doi: 10.1037//0022-006X.68.5.857. [DOI] [PubMed] [Google Scholar]
- Eisenstadt TH, Eyberg S, McNeil CB, Newcomb K, Funderburk B. Parent-child interaction therapy with behavior problem children: Relative effectiveness of two stages and overall treatment outcome. Journal of Clinical Child Psychology. 1993;22:42–51. [Google Scholar]
- Eyberg SM, Funderburk BW, Hembree-Kigin TL, McNeil CB, Querido JG, Hood KK. Parent-child interaction therapy with behavior problem children: One and two year maintenance of treatment effects in the family. Child & Family Behavior Therapy. 2001;23(4):1–20. [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2008;37:215–237. doi: 10.1080/15374410701820117. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Duke M, Boggs SR. Manual for the dyadic parent-child interaction coding system. (3rd edition) 2005 Available online at www.pcit.org.
- Eyberg SM, Robinson EA. Conduct problem behavior: Standardization of a behavioral rating. Journal of Clinical Child & Adolescent Psychology. 1983;12:347–354. [Google Scholar]
- Eyberg SM, Ross AW. Assessment of child behavior problems: The validation of a new inventory. Journal of Clinical Child & Adolescent Psychology. 1978;7:113–116. [Google Scholar]
- Fernandez MA, Eyberg SM. Predicting treatment and follow-up attrition in parent-child interaction therapy. Journal of Abnormal Child Psychology. 2009;37:431–441. doi: 10.1007/s10802-008-9281-1. doi: 10.1007/s10802-008-9281-1. [DOI] [PubMed] [Google Scholar]
- Foa EB, Steketee G. Behavioral treatment of phobics and obsessive-compulsives. In: Jacobson NS, editor. Psychotherapists in clinical practice: Cognitive and behavioral perspectives. Guilford; New York, NY: 1987. pp. 78–120. [Google Scholar]
- Franklin ME, Kozak MJ, Cashman LA, Coles ME, Rheingold AA, Foa EB. Cognitive-behavioral treatment of pediatric obsessive-compulsive disorder: an open clinical trial. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:412–419. doi: 10.1097/00004583-199804000-00019. [DOI] [PubMed] [Google Scholar]
- Funderburk BW, Eyberg SM, Newcomb K, McNeil CB, Hembree-Kigin T, Capage L. Parent-child interaction therapy with behavior problem children: Maintenance of treatment effects in the school setting. Child and Family Behaviour Therapy. 1998;20:17–38. [Google Scholar]
- Gardner F, Shaw DS, Dishion TJ, Burton J, Supplee L. Randomized prevention trial for early conduct problems: effects on proactive parenting and links to toddler disruptive behavior. Journal of Family Psychology. 2007;21:398–406. doi: 10.1037/0893-3200.21.3.398. doi: 10.1037/0893-3200.21.3.398. ISSN: 0893-3200. [DOI] [PubMed] [Google Scholar]
- Graziano PA, Bagner DM, Sheinkopf SJ, Vohr BR, Lester BM. Evidence-based intervention for young children born premature: Associated changes in physiological regulation. Infant Behavior and Development. 2012;35:417–428. doi: 10.1016/j.infbeh.2012.04.001. doi: 10.1016/j.infbeh.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graziano P, Slavec J, Hart K, Garcia A, Pelham W. Improving school readiness in preschoolers with behavior problems: Results from a summer treatment program. Journal of Psychopathology and Behavioral Assessment. in press. [Google Scholar]
- Gunn WB, Jr, Blount A. Primary care mental health: A new frontier for psychology. Journal of Clinical Psychology. 2009;65:235–252. doi: 10.1002/jclp.20499. doi: 10.1002/jclp.20499. [DOI] [PubMed] [Google Scholar]
- Harwood MD, Eyberg SM. Child-directed interaction: Prediction of change in impaired mother–child functioning. Journal of Abnormal Child Psychology. 2006;34:323–335. doi: 10.1007/s10802-006-9025-z. doi: 10.1007/s10802-006-9025-z. [DOI] [PubMed] [Google Scholar]
- Hembree-Kigin TL, McNeil CB. Parent-Child Interaction Therapy. Plenum Publishers; New York: 1995. [Google Scholar]
- Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. Journal of Consulting and Clinical Psychology. 2002;70:1086–1098. doi: 10.1037//0022-006x.70.5.1086. doi: 10.1037//0022-006X.70.5.1086. [DOI] [PubMed] [Google Scholar]
- Hood KK, Eyberg SM. Outcomes of parent-child interaction therapy: Mothers' reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology. 2003;32:419–429. doi: 10.1207/S15374424JCCP3203_10. [DOI] [PubMed] [Google Scholar]
- Horner RH, Carr EG, Halle J, McGee G, Odom S, Wolery M. The use of single-subject research to identify evidence-based practice in special education. Exceptional Children. 2005;71:165–179. [Google Scholar]
- Johnson J, Reader S. Assessing stress in families of children with ADHD: Preliminary development of the Disruptive Behavior Stress Inventory (DBSI). Journal of Clinical Psychology in Medical Settings. 2002;9:51–62. doi: 10.1007/s10880-008-9140-9. [DOI] [PubMed] [Google Scholar]
- Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Cchild Psychology. 2008;36:567–589. doi: 10.1007/s10802-007-9201-9. doi: 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Kupersmidt JB, Bryant D, Willoughby MT. Prevalence of aggressive behaviors among preschoolers in Head Start and community child care programs. Behavioral Disorders. 2000;26:42–52. [Google Scholar]
- La Greca AM, Silverman WK, Lochman JE. Moving beyond efficacy and effectiveness in child and adolescent intervention research. Journal of Consulting and Clinical Psychology. 2009;77:373–382. doi: 10.1037/a0015954. doi: 10.1037/a0015954. [DOI] [PubMed] [Google Scholar]
- Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: modreators and follow-up effects. Clinical Psychology Review. 2006;26:86–104. doi: 10.1016/j.cpr.2005.07.004. doi:10.1016/j.cpr.2005.07.004. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Child, parent and family dysfunction as predictors of outcome in cognitive-behavioral treatment of antisocial children. Behaviour Research and Therapy. 1995;33:271–281. doi: 10.1016/0005-7967(94)00053-m. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Gouze KR, Binns HJ, Keller J, Pate L. Predictors and correlates of completing behavioral parent training for the treatment of oppositional defiant disorder in pediatric primary care. Behavior Therapy. 2010;41:198–211. doi: 10.1016/j.beth.2009.02.006. doi: 10.1016/j.beth.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil CB, Eyberg S, Eisenstadt TH, Newcomb K, Funderburk B. Parent-child interaction therapy with behavior problem children: Generalization of treatment effects to the school setting. Journal of Clinical Child and Adolescent Psychology. 1991;20:140–151. [Google Scholar]
- McMahon RJ, Forehand RL. Helping the noncompliant child: Family-based treatment for oppositional behavior. 2nd ed. Guilford Press; New York, NY: 2003. [Google Scholar]
- Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. The role of psychosocial and family factors in adherence to antiretroviral treatment in human immunodeficiency virus-infected children. The Pediatric infectious disease journal. 2004;23:1035–1041. doi: 10.1097/01.inf.0000143646.15240.ac. [DOI] [PubMed] [Google Scholar]
- Mesman J, Bongers IL, Koot HM. Preschool developmental pathways to preadolescent internalizing and externalizing problems. Journal of Child Psychology and Psychiatry. 2001;42:679–689. [PubMed] [Google Scholar]
- Moffitt TE. The neuropsychology of conduct disorder. Development and psychopathology. 1993;5:135–135. [Google Scholar]
- Moffitt TE, Caspi A, Dickson N, Silva P, Stanton W. Childhood-onset versus adolescent-onset antisocial conduct in males: Natural history from age 3 to 18 years. Development and Psychopathology. 1996;8:399–424. doi: 10.1017/S0954579400007161. [Google Scholar]
- Morawska A, Sanders MR. Concurrent predictors of dysfunctional parenting and maternal confidence: Implications for parenting interventions. Child: Care, Health and Development. 2007;33:757–767. doi: 10.1111/j.1365-2214.2007.00758.x. doi: 10.1111/j.1365-2214.2007.00758.x. [DOI] [PubMed] [Google Scholar]
- Morgan DL, Morgan RK. Single-participant research design: bringing science to managed care. American Psychologist. 2001;56:119–127. doi: 10.1037/0003-066X.56.2.119. [PubMed] [Google Scholar]
- Mörtberg E, Berglund G, Sundin Ö. Intensive cognitive behavioural group treatment for social phobia: A pilot study. Cognitive and Behavioral Therapy. 2005;34:41–49. doi: 10.1080/16506070510010657. [PubMed] [Google Scholar]
- Mörtberg E, Karlsson A, Fyring C, Sundin Ö. Intensive cognitive-behavioral group treatment (CBGT) of social phobia: A randomized controlled study. Journal of Anxiety Disorders. 2006;20:646–660. doi: 10.1016/j.janxdis.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Sweeney L, Erickson DB, Touyz SW. Parent-child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. Journal of Consulting and Clinical Psychology. 2003;71:251–260. doi: 10.1037/0022-006x.71.2.251. doi: 10.1037/0022-006X.71.2.251. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Sweeney L, Erickson DB, Touyz SW. Parent–child interaction therapy: One-and two-year follow-up of standard and abbreviated treatments for oppositional preschoolers. Journal of Abnormal Child Psychology. 2004;32:263–271. doi: 10.1023/b:jacp.0000026140.60558.05. [DOI] [PubMed] [Google Scholar]
- Nolan EE, Gadow KD, Sprafkin J. Teacher reports of DSM-IV ADHD, ODD, and CD symptoms in school children. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:241–249. doi: 10.1097/00004583-200102000-00020. [DOI] [PubMed] [Google Scholar]
- Olson SL, Bates JE, Sandy JM, Schilling EM. Early developmental precursors of impulsive and inattentive behavior: From infancy to middle childhood. Journal of Child Psychology and Psychiatry. 2002;43:435–447. doi: 10.1111/1469-7610.00035. doi: 10.1111/1469-7610.0003. [DOI] [PubMed] [Google Scholar]
- Pelham, Fabiano GA. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:184–214. doi: 10.1080/15374410701818681. doi: 10.1080/15374410701818681. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Ambulatory Pediatrics. 2007;7(1):121–131. doi: 10.1016/j.ambp.2006.08.002. doi: 10.1016/j.ambp.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greiner AR, Waschbush DA, Fabiano G, Burrows-MacLean L. Summer treatment programs for Attention-Deficit/Hyperactivity Disorder. In: Weisz J, Kazdin A, editors. Evidence-based psychotherapies for children and adolescents. The Guilford Press; New York: 2010. pp. 277–294. [Google Scholar]
- Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems--a meta-analytic review. Journal of Child Psychology and Psychiatry. 2006;47:99–111. doi: 10.1111/j.1469-7610.2005.01544.x. doi: 10.1111/j.1469-7610.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- Robinson G, Kaye N, Bergman D, Moreaux M, Baxter C. State profiles of mental health and substance abuse services in Medicaid (SAMHSA Publication No. NMH05-0202) Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2005. [Google Scholar]
- Ross CN, Blanc HM, McNeil CB, Eyberg SM, Hembree-Kigin TL. Parenting stress in mothers of young children with oppositional defiant disorder and other severe behavior problems. Child Study Journal. 1998;28:93–110. [Google Scholar]
- Sanders MR, Markie-Dadds C, Tully LA, Bor W. The Triple P-positive parenting program: A comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology. 2000;68:624–640. doi: 10.1037//002-006x.68.4.624. [PubMed] [Google Scholar]
- Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, Algina J. Efficacy of parent-child interaction therapy: Interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology. 1998;27:34–45. doi: 10.1207/s15374424jccp2701_4. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Dishion TJ, Supplee L, Gardner F, Arnds K. Randomized trial of a family-centered approach to the prevention of early conduct problems: 2-year effects of the family check-up in early childhood. Journal of Consulting and Clinical Psychology. 2006;74:1–9. doi: 10.1037/0022-006X.74.1.1. doi: 10.1037/0022-006X.74.1.1. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Dishion TJ, Connell AM, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early child problem behavior. Development and Psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Bagner DM, Geffken GR, Adkins JW, Murphy TK, Goodman MD. Sequential cognitive-behavioral therapy for children with obsessive-compulsive disorder with an inadequate medication response: A case series of five patients. Depression and Anxiety. 2007;24:375–381. doi: 10.1002/da.20260. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Mann G, Duke D, Munson M, Goodman WK. Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: Comparison of intensive and weekly approaches. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:469–478. doi: 10.1097/chi.0b013e31803062e7. doi: 10.1097/chi.0b013e31803062e7. [DOI] [PubMed] [Google Scholar]
- Thomas R, Zimmer-Gembeck MJ. Parent-Child interaction therapy: An evidence-based treatment for child maltreatment. Child Maltreatment. 2012;17:253–266. doi: 10.1177/1077559512459555. [DOI] [PubMed] [Google Scholar]
- Thomas R, Zimmer-Gembeck MJ. Behavioral outcomes of Parent-Child Interaction Therapy and triple P—Positive Parenting Program: A review and meta-analysis. Journal of Abnormal Child Psychology. 2007;35:475–495. doi: 10.1007/s10802-007-9104-9. doi: 10.1007/s10802-007-9104-9. [DOI] [PubMed] [Google Scholar]
- Turner KMT, Sanders MR. Help when it's needed first: A controlled evaluation of brief, preventive behavioral family intervention in a primary care setting. Behavior Therapy. 2006;37:131–142. doi: 10.1016/j.beth.2005.05.004. doi: 10.1016/j.beth.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid M. The incredible years parents, teachers, and children training series: A multifaceted treatment approach for young children with conduct problems. In: Kazdin AE, Weisz JR, editors. Evidenced-based psychotherapies for children and adolescents. Guilford; New York, NY: 2003. pp. 224–240. [Google Scholar]
- Webster-Stratton, Reid MJ, Stoolmiller M. Preventing conduct problems and improving school readiness: evaluation of the Incredible Years Teacher and Child Training Programs in high-risk schools. Journal of Child Psychology and Psychiatry. 2008;49:471–488. doi: 10.1111/j.1469-7610.2007.01861.x. doi: 10.1111/j.1469-7610.2007.01861.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. The Wechsler Preschool and Primary Scale of Intelligence. 3rd ed The Psychological Corporation; San Antonio, TX: 2002. [Google Scholar]
- Weisz JR, Thurber CA, Sweeney L, Proffitt VD, LeGagnoux GL. Brief treatment of mild-to-moderate child depression using primary and secondary control enhancement training. Journal of Consulting and Clinical Psychology. 1997;65:703–707. doi: 10.1037//0022-006x.65.4.703. [DOI] [PubMed] [Google Scholar]
- Werba BE, Eyberg SM, Boggs SR, Algina J. Predicting outcome in parent-child interaction therapy: Success and attrition. Behavior Modification. 2006;30:618–646. doi: 10.1177/0145445504272977. doi: 10.1177/0145445504272977. [DOI] [PubMed] [Google Scholar]
- Westen D, Bradley R. Empirically supported complexity: rethinking evidence-based practice in psychotherapy. Current Directions in Psychological Science. 2005;14:266–271. doi: 10.1111/j.0963-7214.2005.00378.x. [Google Scholar]
- Whiteside SP, Johnson AB. An uncontrolled examination of a 5-day intensive treatment for pediatric OCD. Behavior Therapy. 2010;41:410–422. doi: 10.1016/j.beth.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Zisser A, Eyberg SM. Treating oppositional behavior in children using parent-child interaction therapy. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. 2nd ed. Guilford; New York, NY: 2010. pp. 179–193. [Google Scholar]