Abstract
Objective
Internalizing mental illness stigma is related to poorer well-being, but less is known about the factors that predict levels of internalized stigma. This study explored how experiences of discrimination relate to greater anticipation of discrimination and devaluation in the future, and how anticipation of stigma, in turn predicts greater stigma internalization.
Method
Participants were 105 adults with mental illness who self-reported their experiences of discrimination based on their mental illness, their anticipation of discrimination and social devaluation from others in the future, and their level of internalized stigma. Participants were approached in several locations and completed surveys on laptop computers.
Results
Correlational analyses indicated that more experiences of discrimination due to one’s mental illness were related to increased anticipated discrimination in the future, increased anticipated social stigma from others, and greater internalized stigma. Multiple serial mediator analyses showed that the effect of experiences of discrimination on internalized stigma was fully mediated by increased anticipated discrimination and anticipated stigma.
Conclusion and Implications for Practice
Experiences of discrimination over the lifetime may influence not only how much future discrimination people with mental illness are concerned with but also how much they internalize negative feelings about the self. Mental health professionals may need to address concerns with future discrimination and devaluation in order to decrease internalized stigma.
Keywords: Stigma, Discrimination, Anticipated Stigma, Internalized Stigma
The impact of stigma on mental health and life outcomes for individuals living with mental illness has been well documented. Mental illness stigma has been associated with less treatment utilization (Fung & Tsang, 2010), poorer treatment outcomes (Corrigan & Rao, 2012), reduced relationship quality (Brohan, Elgie, Sartorius, & Thornicroft, 2010), and greater discrimination in employment, housing, and educational contexts (Link, Struening, Rahav, & Nuttbrock, 1997). Self-stigma is defined as the internalization of the negative stereotypes, attitudes, and perceptions held of individuals who are members of a socially devalued group (Corrigan, 2004). An individual who has internalized stigma not only believes the stereotypes to be true, but also believes the stereotypes to be true of him or herself. In the case of mental illness stigma, images of the mentally ill as dangerous, unpredictable, flawed, or possessing a weakness of character become self-defining resulting in fears of rejection, discrimination, and diminished self-concept (Corrigan & Rao, 2012). The actual experience of discrimination may provide evidence or proof that people with mental illness are in fact devalued and are likely to be targets of mistreatment. Although discrimination may play a significant role in the internalization process, discrimination alone is not sufficient to explain the likelihood of internalizing mental illness stigma (Krajewski, Burazeri, & Brand, 2013). We know that some individuals who experience mental illness discrimination do so at a significant personal cost whereas others seem relatively unscathed or even in some cases, derive a sense of empowerment and purpose by the experience (Brohan, Elgie, Sartorius, & Thornicroft, 2010). It is also the case that the expectation of being mistreated or socially devalued may result in stigma internalization even in the absence of actual mental illness discrimination (Corrigan & Rao, 2012).
The focus of the current study is to more clearly delineate the relationships among mental illness discrimination, anticipated discrimination, anticipated social stigma, and stigma internalization. A number of studies have examined the aforementioned constructs but typically only one or two in a single investigation. Studies that have assessed experiences of discrimination along with anticipated stigma tend to find high levels of both among individuals suffering from serious mental illness although levels of anticipated stigma are generally much higher than actual experiences of discrimination (Angermeyer, Beck, & Holzinzer, 2004; Cechnicki, Angermeyer, & Bielanska, 2011; Thornicroft, Brohan, Sartorius, & Leese, 2009). Many of these studies, however, do not distinguish between anticipated discrimination and anticipated social stigma. For example, Thornicroft, et al., (2009) as part of the global INDIGO study examined experiences of discrimination and anticipated discrimination among individuals diagnosed with schizophrenia in 27 different countries. While the authors measured a range of actual instances of discrimination (32 situations/experiences), their measure of anticipated discrimination was limited to four items and included both anticipated discrimination (e.g., future discrimination looking for work) and anticipated social stigma (e.g., fear of revealing one’s diagnosis and limiting one’s involvement in close relationships because of fears of rejection). Others have operationalized anticipated social stigma as the expectation of both future discrimination and social/interpersonal devaluation (Angermeyer, Beck, & Holzinzer, 2004; Cechnicki, Angermeyer, & Bielanska, 2011). In the current work, we differentiate between anticipated discrimination – worry about acute acts of discrimination that are likely to happen infrequently such as getting fired from a job or not being rented an apartment due to one’s mental illness– and anticipated social stigma. Anticipated social stigma encompasses worries about more “day-to-day” devaluation and interpersonal distancing such as getting treated with less respect than others and people not wanting to get involved in relationships (Quinn & Chaudoir, 2009).
Research has examined the link between mental illness discrimination and internalized stigma but has not yet accounted for the effects of anticipated stigma (Drapalski, et al., 2013; Lysaker et al., 2012). Drapalski and colleagues (2013), using a sample comprised of individuals with serious mental illness, found a significant association between discrimination and internalized stigma (as measured by stereotype endorsement and isolation/withdrawal), but did not find an association between internalized stigma and self-concept, which would be expected if stigma internalization is the application of stereotypes to the self. Lysaker and colleagues (2012) examined the stability of discrimination and internalized stigma over time in a sample of individuals diagnosed with schizophrenia and found that discrimination and internalized stigma at baseline did not predict discrimination and internalized stigma 12 months later. Neither study took into account the effects of anticipated experiences on the relationship between discrimination and internalization. Consistent with the stereotyping and discrimination literature more broadly, the extent to which a specific experience of mental illness discrimination and/or series of experiences leads to internalized mental illness stigma may be contingent, at least in part, on the degree of effort devoted to worrying about, anticipating, and avoiding similar experiences in the future (Corrigan, Larson, & Rüsch, 2009; Link & Phelan, 2001). Farrelly and colleagues (2014) did examine the relationships among experienced discrimination, anticipated discrimination, and internalized stigma in a sample of individuals with serious mental illness, however, the analyses focused almost exclusively on anticipated and experienced discrimination rather than internalized stigma.
In the current work, we attempt to address some of the unanswered questions in the literature by proposing that the relationship between experienced discrimination and internalization is mediated by anticipated discrimination and stigma. Specifically, we hypothesize that experiences of discrimination will be associated with greater anticipation of discrimination in the future. As individuals anticipate experiencing more discrimination as a consequence of their mental illness, we expect them to also anticipate more social stigma. In turn, as levels of stigma anticipation increase, we expect greater stigma internalization. Much of the literature on mental illness stigma has focused on serious mental illness or specific disorders such as schizophrenia. A focus on serious mental illness is understandable as many of the negative stereotypes, cultural taboos, and myths about mental illness are framed around individuals with serious mental illness, and individuals with serious mental illness will likely suffer the greatest disease burden without treatment. However, the impact of stigma can be felt across the spectrum of mental disorders, conditions, and levels of impairment. As a barrier to treatment, anticipated discrimination and stigma may be especially impactful among individuals who are experiencing less severe mental illness or psychiatric impairment as they are less likely to experience discrimination and yet may remain vulnerable to stigma internalization. In the current study, we did not target specific diagnoses or co-morbidity among participants but rather allowed participants to self-identify as having a mental illness
Method
Recruitment
Data were collected as part of a parent grant on identity components and well-being targeting a variety of different concealable stigmatized identities. The study was approved by both the institutional review boards of the University of Connecticut and the Department of Mental Health and Addiction Services (DMHAS) of the State of Connecticut. Participants (N=735) were recruited over three years (2009–2011) from three locations in and around Hartford, Connecticut. Participants were approached by research assistants and told about the study. If participants were interested, they were taken to a private room and completed the survey on a laptop computer. (Full information on the recruitment procedure can be found at Quinn et al., 2014).
Participants
As part of the initial screening questions, participants were given a list of experiences and identities (e.g., domestic violence, mental illness) and asked to check off any identity that they had and regularly kept hidden from others in their lives. If they checked off more than one identity of interest for the parent grant, they were asked to select the identity that was most important to them. The current report focuses on the 105 participants who indicated that they regularly kept a mental illness concealed from others, and that it was most important to them. The computer program was set up such that all of the stigma questions asked about the specific identity people indicated. Thus, in the current data, all participants responded to questions about mental illness. Full demographic information is presented in Table 1. These participants were on average 33 years old. The sample was ethnicity/race was 28.6% Hispanic ethnicity, 38.1% Black, and 30.5% White. The sample was also very poor, with a median annual income of only $5000 or less. At the end of the survey, participants were provided with a checklist of psychiatric diagnoses and conditions and asked to check all that apply. Major depression (40%), anxiety (35.2%), and bipolar disorder (28.6%) were the most frequent diagnoses reported although many participants checked off multiple disorders, including schizophrenia, obsessive-compulsive disorder, personality disorder, self-mutilation, and trauma disorders. Eighty-one percent of the participants reported that they had sought treatment for their mental illness.
Table 1.
Demographic information, including age, sex, education, income, employment status, race/ethnicity, and treatment.
| N | % | |
|---|---|---|
| Age (M, SD) | 33.02 (11.52) | |
|
| ||
| Sex (Female) | 41 | 39 |
|
| ||
| Education | ||
| Did not complete high school | 34 | 32 |
| Completed high school | 25 | 24 |
| Some college | 27 | 26 |
| Completed Bachelor’s degree | 3 | 3 |
|
| ||
| Annual income | ||
| Less than $5,000 | 53 | 51 |
| Between $5,000 and $10,000 | 20 | 19 |
| Between $10,000 and $15,000 | 12 | 12 |
| $15,000 or more | 19 | 18 |
|
| ||
| Employed at time of participation | 23 | 22 |
|
| ||
| Ethnicity (Hispanic) | 30 | 29 |
|
| ||
| Race (Could choose more than one) | ||
| Asian/Pacific Islander | 2 | 2 |
| Black/African American | 40 | 38 |
| Native American | 3 | 3 |
| White | 32 | 31 |
| Other | 26 | 25 |
|
| ||
| Have received treatment for mental illness? | 85 | 81 |
|
| ||
| Treatment Type | ||
| Medical services | 48 | 56.5 |
| Professional counseling | 24 | 28.2 |
| Other | 13 | 15.3 |
Measures
Anticipated Discrimination and Experienced Discrimination due to Mental Illness
Anticipated and experienced discrimination was measured with a modified version of the lifetime discrimination scale, used in the national MIDUS survey, as reported by Kessler, Mickelson, & Williams (1999). For anticipated discrimination, participants were presented with the stem, “If others knew about your mental illness, how likely would each of the following be to occur” with the 11 items asked on a 1 (Not at all Likely) to 7 (Very Likely) scales. This scale had a mean of 3.28 (SD = 1.50) and high internal reliability in the current study (Cronbach’s alpha = 0.90). After completing the scale, participants were asked, “Have you actually experienced any of those things due to revealing your mental illness?” If participants indicated “yes”, they were asked to check off all they had experienced due to their mental illness. The 11 items are presented in Table 3, with percentages of people who indicated they had experienced each type of discrimination. The measure of experienced discrimination is the sum of the experiences participants indicated (M = 1.25, SD = 1.82).
Anticipated Stigma
Anticipated stigma is the extent to which people are worried about negative interpersonal reactions and devaluations from others if they reveal their mental illness or others become aware of the mental illness. The anticipated stigma scale was composed of 9 items from the “day-to-day” discrimination scale (Kesser et al., 1999) combined with 6 more items focused on relationship devaluation. The scale begins with the stem “If others knew of your mental illness, how likely do you think the following would be to occur?” with items such as, “Treated with less respect than other people” and “People not wanting to get to know you better,” answered on 1 (Very Unlikely) to 7 (Very Likely) scales. The full 15-item scale—which has been used previously for multiple types of stigmatized identities (e.g., Quinn et al., 2014)—had a mean of 4.09 (SD = 1.54) and exhibited high internal reliability in the current study (Cronbach’s alpha = 0.93).
Internalized Stigma
Internalized stigma is measured in many different ways in the literature. We sought to clearly measure negative feelings about the self due to mental illness. Our scale had 4 items; 3 were modified from Berger, Ferrans, and Lashley’s (2001) stigma scale: “Having experiences with mental illness makes me feel like a bad person,” “I feel I am not as good as others because of my mental illness,” and “I feel guilty because of my mental illness” with an additional item modified from Link’s (1987) devaluation-discrimination scale: “I feel that my mental illness is a sign of personal failure.” All items were measured on 1 (Strongly Disagree) to 7 (Strongly Agree) scales. The 4-item scale had a mean of 3.73 (SD = 1.70) and displayed good internal reliability in the current study (Cronbach’s alpha = 0.82).
Results
Initial findings indicate that a large proportion of participants in the current sample have experienced discrimination, and anticipate discrimination and stigma, due to their mental illness. As shown in Table 2, about half of the participants report experiencing discrimination due to their mental illness. The most common types of discrimination reported were not get hired for a job (26%), getting hassled by the police (23%), getting fired from a job (16%), and getting poorer medical treatment/service (13%). The degree to which participants anticipated specific discriminatory experiences was not always consistent with the likelihood of having experienced that event. The two experiences rated with the highest mean anticipated discrimination if one’s mental illness were revealed were not getting hired for a job (M = 4.00) and not getting promoted for a job (M = 3.82). While a quarter of participants reported the experience of not being hired because of their mental illness, less than 5% reported not being promoted due to their mental illness. Lifetime rates of experience of discrimination were correlated with greater anticipated discrimination and greater anticipation of social stigma. As expected anticipated discrimination, anticipated stigma, and internalized stigma were all quite highly correlated with bivariate correlations between 0.50 and 0.52.
Table 2.
Descriptive information for Experienced and Anticipated Discrimination, Anticipated Stigma, and Internalized Stigma.
| Experienced Discrimination | Anticipated Discrimination | Anticipated Stigma | |
|---|---|---|---|
| Anticipated Discrimination | 0.41** | ||
| Anticipated Stigma | 0.36** | 0.52** | |
| Internalized Stigma | 0.24** | 0.51** | 0.50** |
| Not get hired for a job | 26% | 4.00 (2.13) | |
| Not be given a job promotion | 5% | 3.82 (2.12) | |
| Fired from a job | 16% | 3.57 (2.17) | |
| Discouraged by a teacher from continuing education | 8% | 3.38 (2.15) | |
| Denied a scholarship | 2% | 2.96 (2.02) | |
| Prevented from renting or buying a home | 7% | 2.99 (2.11) | |
| Denied a bank or car loan or credit card | 9% | 3.27 (2.21) | |
| Forced out of neighborhood by neighbors | 9% | 2.91 (2.12) | |
| Denied (or given poorer) medical care | 13% | 3.09 (2.12) | |
| Denied (or given poorer) services (e.g., by plumber, mechanic, etc.) | 9% | 2.81 (1.92) | |
| Hassled by police | 23% | 3.25 (2.28) | |
| Have not experienced any of above | 53% |
Note: The first three rows display the bivariate correlations between Experienced Discrimination, Anticipated Discrimination, Anticipated Stigma, and Internalized Stigma. For the following rows, the first column displays the percentage of participants who experienced a given type of discrimination, while the second column displays the average amount of anticipated discrimination for each type.
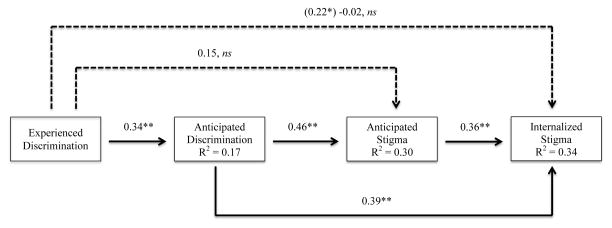
It was hypothesized that experiences of discrimination would be related to internalized stigma, and that this association would be mediated by anticipated discrimination and anticipated social stigma. To test this hypothesis we conducted multiple serial mediator analyses using Hayes’ Process program (2013). This analytic procedure was chosen because it uses a bootstrapping technique that computes 95% confidence intervals around indirect effects (i.e., the mediation effects) in a simultaneous serial mediational model. As shown in Figure 1, and consistent with previous research, we found evidence for a direct effect of experiences of discrimination on internalized stigma (unstandardized regression coefficient, b = 0.22, p < 0.05)—as the amount of experienced discrimination increases, the level of internalized stigma increases. However, when anticipated discrimination and anticipated social stigma were included in the model as mediators, the direct effect of experienced discrimination on internalized stigma became non-significant (b = −0.02, ns). The indirect effect of experienced discrimination on internalized stigma—mediated through anticipated discrimination and anticipated social stigma—was significant (95% CI: 0.03, 0.41). These findings indicate that anticipated discrimination and anticipated stigma fully mediated the effect of experienced discrimination on internalized stigma. Moreover, anticipated discrimination had a significant direct effect on internalized stigma (b = 0.39, p < 0.01). Overall, the full model accounted for 34% of the variance in internalized stigma. Taken together, people who reported more experiences with discrimination because of their mental illness also anticipated more discrimination in the future. People who anticipate more discrimination also believe it to be more likely that others will devalue them (anticipated stigma) if they reveal their mental illness. Finally, the more people anticipated stigma, the more they internalized the stigma associated with mental illness.
Figure 1.
This serial multiple mediation model (with unstandardized regression weights) displays the effect of experienced discrimination on internalized stigma as mediated by anticipated discrimination and anticipated stigma. Anticipated discrimination and anticipated stigma fully mediate the relationship between experienced discrimination and internalized stigma.
Discussion
Past research on mental illness stigma has found that experiencing discrimination is associated with internalizing the negative stereotypes of mental illness (i.e., self-stigma); however, little is known about the role that anticipation of discrimination and stigma play in this relationship. The current research sought to fill this gap in the mental illness literature. Consistent with hypotheses and past research, experiencing more discrimination due to one’s mental illness was associated with greater internalized stigma. Importantly, this relationship was fully mediated by the extent to which people with a mental illness anticipated discrimination (i.e., acute instances of discrimination) and anticipated social stigma (i.e., the day-to-day experiences of social distancing and devaluation). These findings indicate that experiencing discrimination may not directly lead people to internalize the negative stereotypes of mental illness. It may be the case that people internalize the negative stereotypes when, after experiencing discrimination, they then start to anticipate more discrimination and more social stigma. Given that the current study used cross-sectional data—which makes claims about temporal precedence difficult—future research may benefit from exploring whether reducing anticipation of discrimination and stigma can weaken the relationship between experienced discrimination and internalized stigma for people living with a mental illness. Moreover, although we made a case for the direction of causality to go from experienced discrimination to anticipated discrimination to anticipated stigma to internalization, it is impossible with cross-sectional data to test this directional path. Only a longitudinal study, following people as they experience (or do not experience) discrimination and examining changes in anticipated discrimination and stigma over time, would be able to definitely test the direction of causality. In addition, it is likely that there are bidirectional relationships that we could not capture. For example, once internalized stigma is heightened people may anticipate more discrimination and stigma from others.
The current research has certain methodological features that, we believe, strengthen the impact and generalizability of the findings. First, the current study utilized an ethnically diverse sample of participants with a range of mental illness conditions and experiences. While the sample was ethnically diverse, it was disproportionately low income. Specifically, our sample consists largely of adults from low socio-economic backgrounds—nearly a third of participants had less than a high school education with a median income well below the poverty line. This may explain why discriminatory experiences associated with employment, treatment, and police encounters garnered the strongest expectation of future discrimination and were also the most frequently reported experiences of actual discrimination; whereas the least endorsed experiences of discrimination were those experiences that are also less likely to occur in a highly impoverished community sample (e.g., denied a scholarship, prevented from buying a house). Future research should explore whether the relationships between experiences of discrimination, anticipation of discrimination and stigma, and stigma internalization function similarly for those who are more economically advantaged. Second, participants in the current study had a wide range of mental illnesses, which indicates that the current study’s findings may generalize across mental illnesses. With that said, because our sample was relatively small (n = 105), we did not have the statistical power to explore whether these processes were stronger or weaker for people with certain mental illnesses as opposed to others—future research should explore this possibility. Finally, the current research contributes to the mental illness literature by how it differentiated and measured key variables. Specifically, whereas past research typically confounds anticipated discrimination with anticipated stigma—constructs that are similar, but differ by their level of acuteness and frequency—the current research made a deliberate effort to measure these constructs separately.
Past research has found that stigma due to mental illness is associated with less treatment utilization (Fung & Tsang, 2010) and poorer treatment outcomes (Corrigan & Rao, 2012). Whether or not stigma served as a potential barrier to treatment was unclear in the current study. Most of the participants reported receiving mental health treatment, although we do not know the extent of treatment. While not specific to mental health providers, 13% of our participants reported experiencing discrimination from medical providers as a consequence of their mental illness as well as moderate levels of anticipating future discrimination from medical providers. There is growing evidence that stigma (both anticipated and internalized) affects areas other than treatment utilization including treatment engagement, compliance, interpersonal relationships, perceptions of care, and treatment effectiveness (Tucker, et al., 2013). Thus, future work that explicitly investigates the roles of discrimination and anticipated stigma as barriers to treatment, more widely defined, may be particularly useful. Assessing both actual and anticipated discrimination regarding one’s mental illness may inform interventions designed to reduce mental illness stigma and increase treatment engagement. Interventions designed to reduce mental illness stigma have been geared toward two domains: public service campaigns designed to challenge stereotypes and misconceptions about mental illness and to shift social norms (e.g., California Mental Health Services Authority; Wayne, et al., 2013) and targeted education and training programs that focus on individual attitude and behavior change (e.g., Corrigan & Penn, 1999). Both domains are important as they target social norms and individual experiences as a consequence of those norms. Internalized stigma, however, is direct application of stereotypes and social devaluation to the self and may require more than education and training to address. Many targeted interventions such as cognitive behavior therapies or schema-based therapies focus on reducing internalized stigma by challenging maladaptive beliefs (e.g., “mental illness makes me a bad person”) or redefining the self (e.g., “my mental illness is only one part of who I am”). While many of these targeted interventions do include elements of anticipated stigma and social stigma, they often frame discrimination as a behavioral consequence (e.g., “how to respond if someone treats you poorly because of your mental illness”) rather than incorporating discrimination and anticipated discrimination into the internalized belief system. That is, actual, perceived, and/or anticipated mental illness discrimination may impact symptoms and treatment engagement indirectly through internalized stigma or independent of internalized stigma. For some individuals, mental illness discrimination (or anticipation of such discrimination) may validate negative evaluations of the self (internalized stigma) whereas for others, such discrimination may validate social devaluation of one’s group (individuals with mental illness) but not of the self. Incorporating elements of anticipated discrimination and social stigma into treatments broadly may provide a more accurate assessment of individuals’ experiences and serve as differential targets of intervention (e.g., Fung, Tsang, & Cheung, 2011; Stathi, Tsantila, & Crisp, 2012; Yanos, et al., 2014).
Acknowledgments
Research funded by the National Institute of Mental Health (NIMH) of the National Institutes of Health under award number R01MH082916.
Footnotes
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Angermeyer MC, Beck M, Deitrich M, Holzinger A. The stigma of mental illness: Patients’ anticipation experiences. International Journal of Social Psychiatry. 2004;50:153–162. doi: 10.1177/0020764004043115. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Brohan E, Elgie R, Sartorius N, Thornicroft G. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: The GAMIAN-Europe study. Journal of Affective Disorders. 2010;122:232–238. doi: 10.1016/j.schres.2010.02.1065. [DOI] [PubMed] [Google Scholar]
- Cechnicki A, Angermeyer MC, Bielanska A. Anticipated and experienced stigma among people with schizophrenia: Its nature and correlates. Social Psychiatry. 2011;46:643–650. doi: 10.1007/s00127-010-0230-2. [DOI] [PubMed] [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. American Psychologist. 2004;59:614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Larson JE, Rüsch N. Self-stigma and the “why try” effect: Impact on life goals and evidence-based practices. World Psychiatry. 2009;8:75–81. doi: 10.1002/j.2051-5545.2009.tb00218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Penn DL. Lessons from social psychology on discrediting psychiatric stigma. The American Psychologist. 1999;54:765–776. doi: 10.1037//0003-066x.54.9.765. [DOI] [PubMed] [Google Scholar]
- Corrigan P, Rao D. On the self-stigma of mental illness: Stages, Disclosure, and strategies for change. Canadian Journal of Psychiatry. 2012;57:464–469. doi: 10.1177/070674371205700804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drapalski AL, Lucksted A, Perin PB, Askre JM, Brown CH, DeForge BR, Boyd JE. A model of internalized stigma and its effects on people with mental illness. Psychiatric Services. 2013;64:264–269. doi: 10.1176/appi.ps.001322012. [DOI] [PubMed] [Google Scholar]
- Farrelly S, Clement S, Gabbidon J, Jeffrey D, Dockery D, Lassman F, Brohan E, Henderson C, Williams RC, Williams P, Howard LM, Thornicroft G. Anticipated and experienced discrimination amongst people with schizophrenia, bipolar disorder and major depressive disorder: A cross sectional study. BioMed Central Psychiatry. 2014;14:1–8. doi: 10.1186/1471-244X-14-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung K, Tsang H. Self-stigma, stages of change, and psychological treatment adherence among Chinese people with schizophrenia: A path analysis. Social Psychiatry and Psychiatric Epidemiology. 2010;45:561–568. doi: 10.1007/s00127-009-0098-1. [DOI] [PubMed] [Google Scholar]
- Fung KM, Tsang HW, Cheung WM. Randomized controlled trial of the self-stigma reduction program among individuals with schizophrenia. Psychiatry Research. 2011;189:208–214. doi: 10.1016/j.psychres.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis. New York, NY: Gilford Press; [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–230. [PubMed] [Google Scholar]
- Krajewski C, Burazeri G, Brand H. Self-stigma, perceived discrimination and empowerment among people with mental illness in six countries: Pan European stigma study. Psychiatry Research. 2013;210:1136–1146. doi: 10.1016/j.psychres.2013.08.013. [DOI] [PubMed] [Google Scholar]
- Link BG. Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review. 1987;52:96–112. [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnosis of mental illness and substance abuse. Journal of Health and Social Behavior. 1997;38:177–190. [PubMed] [Google Scholar]
- Lysaker PH, Tunze C, Yanos PT, Roe D, Ringer J, Rand K. Relationship between stereotyped beliefs about mental illness, discrimination experiences, and distressed mood over 1 year among persons with schizophrenia enrolled in rehabilitation. Social Psychiatric Epidemiology. 2012;47:849–855. doi: 10.1007/s00127-011-0396-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM, Chaudoir SR. Living with a concealable stigmatizing identity: The impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. Journal of Personality and Social Psychology. 2009;97:634–651. doi: 10.1037/a0015815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM, Williams MK, Quintana F, Gaskins JL, Overstreet NM, Pishori A, Earnshaw VA, Perez G, Chaudoir SR. Examining effects of anticipated stigma, centrality, salience, internalization, and outness on psychological distress for people with concealable stigmatized identities. PLoS One. 2014 doi: 10.1371/journal.pone.0096977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusch N, Corrigan PW, Wassel A, Michaels P, Olschweski M, Wilkniss S, Batia K. A stress-coping model of mental illness stigma: Predictors of cognitive stress appraisal. Schizophrenia Research. 2009;110:59–64. doi: 10.1016/j.schres.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stathi S, Tsantila K, Crisp RJ. Imaging intergroup contact can combat mental illness stigma by reducing anxiety, avoidance, and negative stereotyping. Journal of Social Psychology. 2012;152:746–757. doi: 10.1080/00224545.2012.697080. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: A cross-sectional survey. Lancet. 2009;373:408–415. doi: 10.1016/S0140-6736(08)61817-6. [DOI] [PubMed] [Google Scholar]
- Tucker JR, Hammer JH, Vogel DL, Bitman RL, Wade NG, Maier EJ. Disentangling self-stigma: Are mental illness and help-seeking self-stigmas different? Journal of Counseling Psychology. 2013;60:520–531. doi: 10.1037/a0033555. [DOI] [PubMed] [Google Scholar]
- Wayne C, Welch S, Berry SH, Collentine AM, Collins R, Lebron D, Shearer AL. California’s historic effort to reduce the stigma of mental illness: The mental health services act. American Journal of Public Health. 2013;103:786–794. doi: 10.2105/AJPH.2013.301225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanos PT, Drapalski AL, Lucksted A, Roe D, Lysaker P. Interventions targeting mental health self-stigma: A review and comparison. Psychiatric Rehabilitation Journal. 2014 Oct 13; doi: 10.1037/prj0000100. Advance online publication: http://dx.doi.org/10.1037/prj0000100. [DOI] [PMC free article] [PubMed]