Introduction
From 2000 to 2011, the rate of death from unintentional drug poisoning in the USA more than doubled from 4.1 per 100,000 to 10.6 per 100,000, respectively [1]. Further, from 1999 to 2011, drug overdose deaths involving opioids quadrupled from 4030 to 16,917 [1]. Nationally, since 2009, more people have died each year from drug poisoning than from motor vehicle crashes [1]. In fact, overdose is the leading cause of adult unintentional injury death in Rhode Island, which is one of 30 states where overdose mortality exceeded motor vehicle collision mortality in 2010 [2].
The major driver of the increase in drug overdose deaths is pharmaceutical opioids. In 2010, 60 % of the unintentional drug poisoning deaths in the USA were caused by pharmaceuticals, and 75 % of the fatal pharmaceutical overdoses were caused by opioids [3]. Nationally, heroin use doubled from 2003 to 2012, and from 2002 to 2011, drug poisoning deaths involving heroin more than doubled from 2089 to 4397, respectively [4, 5]. In Rhode Island, overdose deaths caused by illicit drugs increased so much during 2011–2013 that it overtook fatal pharmaceutical overdoses, which remained steady during the same time period [6].
Fentanyl (N-(1-(2-phenethyl)-4-piperidinyl-N-phenyl-propanamide) is a synthetic opioid first synthesized by Janssen Pharmaceuticals in the 1960s and used medicinally since 1968. It is estimated to be between 80 and 100 times more potent than morphine [7, 8] and has over 200 chemical derivatives, some of which have been used recreationally or implicated in heroin adulteration in the past. The first fentanyl derivatives synthesized in the early 1970s showed similar pharmacokinetics but significantly different potencies. By the early 1980s, clandestinely produced synthetic fentanyl and fentanyl derivatives were becoming available on the black market [7, 9]. The speed of onset and potency of these drugs made them attractive to opioid users but also made them more dangerous. Fentanyl derivatives can be a few to hundreds of times more potent than heroin, and if users unknowingly obtain and administer packages sold as heroin but containing a more potent fentanyl derivative, this can lead to inadvertent overdose and death [10].
Several epidemics of overdose deaths caused by illicitly manufactured fentanyl- and fentanyl derivative-adulterated heroin have occurred in the USA since the 1970s, leaving more than 1000 dead in their wakes. The first epidemic was identified in California in 1978 and was associated with a compound later identified as the fentanyl analog 3-methylfentanyl, branded by the street name “China White.” This drug is several hundred times more potent than morphine and accounted for more than 100 deaths in California [7–9, 11]. This same drug resurfaced in 1988 in Pennsylvania, where it was implicated in the deaths of 16 persons [12, 13]. In 1991, covertly manufactured fentanyl was sold as heroin on the streets of New York City in small envelopes labeled “Tango and Cash.” Because of difficulties in cutting the drug, these samples contained highly variable amounts of fentanyl and their use resulted in 12 deaths [14]. More recently, from 2005 to 2007, an outbreak of fentanyl-contaminated heroin caused 1013 deaths across several states [15].
The Rhode Island State Health Laboratory preliminarily identified acetyl fentanyl, a fentanyl analog, as the cause of ten overdose deaths during March–April 2013. Acetyl fentanyl (N-phenyl-N-[1-(2-phenylethyl)-4-piperidinyl]-acetamide, monohydrochloride) is an illicit synthetic opioid that is four to five times more potent than heroin; it is not FDA approved, not prescribed by physicians, and not commercially available. The objectives of this investigation were to (1) determine if these drug overdose deaths represented an increase above baseline, (2) characterize the acetyl fentanyl overdose decedents, and (3) identify potential risk factors for acetyl fentanyl overdose death relative to those for other illicit drug overdose deaths.
Methods
Data Collection
We collected data from the Rhode Island Office of State Medical Examiners (OSME), which investigates all Rhode Island deaths resulting or suspected of resulting from an external cause, such as drug overdose. The OSME database includes information collected during medical examiner investigations (including scene investigations, medical record review, and examinations) to determine the cause and manner of death for homicidal, suicidal, accidental (including trauma), sudden, and unexpected natural or undetermined deaths. OSME maintains comprehensive electronic and written records on all autopsies, including toxicology and pathology reports, death certificates, and case investigation summaries. This investigation was exempt from review by CDC’s Internal Review Board.
We extracted data from the OSME database for the 15 months leading up to and including the occurrence of acetyl fentanyl-related overdoses (March 2012–May 2013) to determine the baseline incidence of illicit drug overdose deaths in Rhode Island and determine if any other acetyl fentanyl overdose deaths had previously occurred in the state. We used the OSME database variable “manner sub type” to include records of all illicit drug overdose deaths, defined as deaths caused by illicit drugs alone or in combination with alcohol and/or prescription drugs. We excluded from the baseline incidence analysis overdose deaths caused only by prescription drugs and/or alcohol.
The case definition for acetyl fentanyl overdose deaths identified in the Rhode Island OSME database was death in a person who had an immunoassay screen positive for fentanyl and gas chromatography/mass spectrometry (GC/MS) confirmatory results showing a mass spectrum consistent with acetyl fentanyl or 4-anilino-n-phenethylpiperdine (ANPP), a compound believed to be a precursor of acetyl fentanyl. The concentration of acetyl fentanyl or ANPP was unknown because at the time, no laboratory test existed to quantify these drugs. Acetyl fentanyl overdose deaths are a subgroup of illicit drug overdose deaths.
To characterize the acetyl fentanyl overdose deaths in detail, we conducted in-depth reviews of complete medical examiner charts, post-mortem toxicology results, and hospital medical records (when available) of each acetyl fentanyl overdose death identified. We developed standard data collection forms to systematically abstract information on multiple variables including demographics, date of death, illicit drug use history (if noted in medical examiner records or medical records), scene investigation findings, place of death, autopsy findings, toxicology data, past medical history and prescribed medications (when available), and route of drug administration.
Laboratory Methods
All cases submitted to the Forensic Toxicology Laboratory (FTL) at the Rhode Island State Health Laboratories requiring drug analysis undergo preliminary testing by enzyme-linked immunosorbent assay (ELISA) method. ELISA is a competitive binding process involving antigen-antibody complexes. While very sensitive, these tests can be non-specific, resulting in false-positive results. Therefore, all positive screening results require confirmation by an appropriate method.
The Rhode Island ELISA drug screening method is comprised of a panel of 16 assays. FTL used Immunalysis Direct ELISA kits (Alere, San Diego, CA) with a Tecan Freedom EVO automated system. Multi-constituent whole blood controls (purchased through Utak Laboratories) serve as the blank, cut-off, and low and high positive controls. FTL analyzes these quality control samples before case specimens with the negative and cut-off samples run in duplicate. The fentanyl assay uses a 2 ng/ml cut-off control, a 1 ng/ml low control, and a 20 ng/ml high positive control. FTL analyzes all forensic specimens in duplicate and the instrument software calculates the average absorbance reading and corresponding drug concentration. The preferred post-mortem specimen for ELISA testing is heart blood, but specimen preference and availability may vary according to case history. For the acetyl fentanyl overdose decedents studied here, FTL analyzed post-mortem heart blood and ante-mortem blood specimens due to availability.
Following lab protocol, when case specimens screened positive by the ELISA fentanyl assay, FTL used GC/MS following liquid basic-back-n-butyl chloride extraction [16]. The GC/MS instrument employed in the toxicology laboratory is an Agilent 6890 GC (Agilent Technologies, Inc., Wilmington, DE) equipped with a 5973 MSD run in the electron impact mode. The internal standard used is SKF-525A (Proadifen). The preferred post-mortem specimen for confirmatory testing is femoral blood drawn in a gray-top tube (containing potassium oxalate and sodium fluoride) but is dependent on case history.
The Forensic Drug Chemistry Laboratory analyzed physical evidence collected by law enforcement using GC/MS confirmatory testing. The quality control sample was the DEA-provided acetyl fentanyl reference standard that was analyzed in the same batch as the physical evidence samples.
Statistical Analysis
To describe the acetyl fentanyl overdose deaths and other illicit drug overdose deaths, we calculated frequencies and proportions for all sociodemographic and death-related characteristics obtained from OSME records. In addition, we conducted descriptive analysis of acetyl fentanyl death data abstracted from autopsy reports, toxicology results, and hospital medical records.
To assess if risk factors for acetyl fentanyl overdose deaths differed from those for other illicit drug overdose deaths, we compared OSME data on acetyl fentanyl overdose deaths to OSME data on overdose deaths caused by other illicit drugs that occurred during March 2012–May 2013. Other illicit drugs were defined as drugs not manufactured for pharmaceutical purposes or medical treatment and include cocaine, heroin, methamphetamine, and designer drugs such as MDMA, synthetic cannabinoids, and bath salts. Within the other illicit drug overdose deaths, we coded each death as dichotomous yes/no for the mention of both heroin and opiate in the cause of death field. Using Fisher’s exact test, Wilcoxon rank sum test, and chi-squared test, we compared characteristics of the acetyl fentanyl overdose deaths to four comparison groups of other illicit drug overdose deaths that occurred during March 2012–May 2013: (1) all other illicit drug overdose deaths, (2) those mentioning “heroin,” (3) those mentioning “opiate,” and (4) those mentioning heroin or opiate.
We used a dichotomous comparison to compare the baseline incidence of illicit drug overdose deaths from March 1, 2012–February 28, 2013, to the illicit drug overdose deaths in March 2013, the month during which acetyl fentanyl deaths began occurring. We analyzed all data using SAS 9.3 (SAS Institute, Cary, NC, USA), Microsoft Office Excel 2010 (Microsoft Corp., Redmond, WA, USA), and ESRI® ArcMap™, ArcGIS version 10.1 SP 1 (ESRI®, Redlands, CA, USA). We considered p < 0.05 statistically significant.
Results
Illicit Drug Overdose Death Incidence
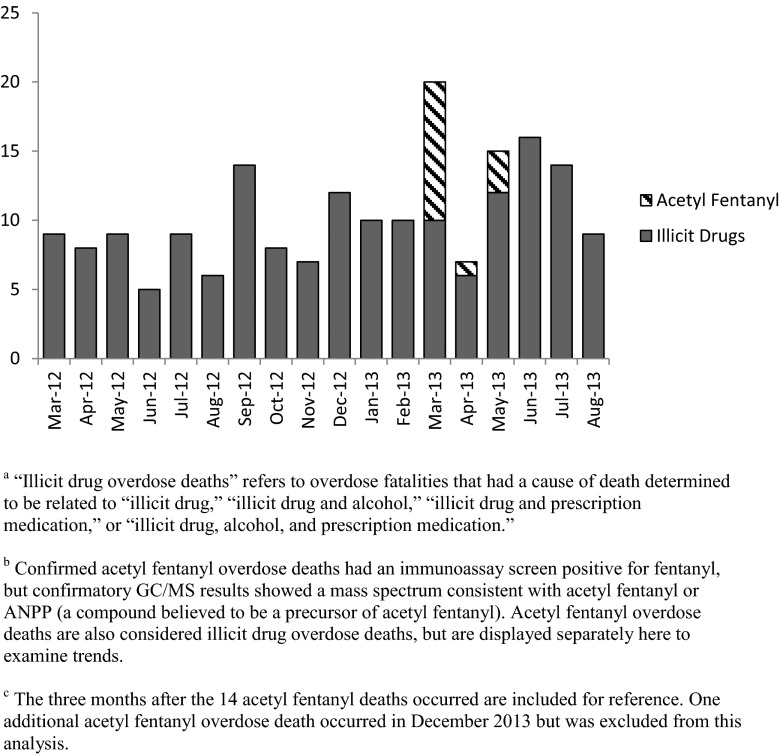
During the 12 months leading up to the appearance of acetyl fentanyl in Rhode Island, an average of 8.9 illicit drug overdose deaths per month occurred in Rhode Island (Fig. 1). In March 2013, 20 illicit drug overdose deaths occurred, representing a significant increase of illicit drug overdose deaths compared to the monthly average of the previous year (p = 0.0003). Of the 20 illicit drug overdose deaths in March 2013, 10 were acetyl fentanyl overdose deaths. In addition, four more acetyl fentanyl overdose deaths occurred during the study period: one in April and three in May.
Fig. 1.
Illicit drug overdose deathsa and acetyl fentanyl overdose deathsb by month, Rhode Island, March 2012–August 2013c
Description of Acetyl Fentanyl Overdose Deaths
During March–May 2013, 14 acetyl fentanyl overdose deaths occurred in Rhode Island. Prior to March 7, 2013, no cases identified by the medical examiner and tested by the Rhode Island FTL showed positive results for either acetyl fentanyl or ANPP. Table 1 summarizes demographic and event-related characteristics of the acetyl fentanyl overdose decedents. The majority of acetyl fentanyl decedents were male (n = 10; 71 %), and all were white. Four (29 %) acetyl fentanyl decedents were aged 50–59 years and five (36 %) were aged 20–29 years. Eight acetyl fentanyl decedents were reported to be not married (57 %). Law enforcement found drug paraphernalia at the scene of incident of nine acetyl fentanyl deaths (64 %) and evidence of track marks in three decedents (21 %). Eleven (79 %) acetyl fentanyl decedents had a known history of drug use, while seven (50 %) had a history of opioid use. None of the acetyl fentanyl overdose decedents showed evidence of naloxone administration by a non-medical professional (i.e., bystander, police officer, etc.).
Table 1.
Selected characteristics of acetyl fentanyl overdose decedents and overdose event, Rhode Island, March–May 2013 (n = 14)
| Characteristic | n (%) |
|---|---|
| Gender | |
| Female | 4 (29) |
| Male | 10 (71) |
| Race/ethnicity | |
| White | 14 (100) |
| Black | 0 (0) |
| Hispanic | 0 (0) |
| Age (years) | |
| <20 | 1 (7) |
| 20–29 | 5 (36) |
| 30–39 | 3 (21) |
| 40–49 | 1 (7) |
| 50–59 | 4 (29) |
| 60+ | 0 (0) |
| Marital status | |
| Single | 8 (57) |
| Married | 0 (0) |
| Divorced/widowed | 2 (14) |
| Unknown | 4 (29) |
| History of drug use | |
| Yes | 11 (79) |
| Unknown | 3 (21) |
| History of opioid abuse | 7 (50) |
| Place of death | |
| Emergency department | 7 (50) |
| Home | 4 (29) |
| Public place | 1 (7) |
| Hospital (not emergency department) | 2 (14) |
| Scene characteristics | |
| Drug paraphernalia | 9 (64) |
| Died alone (not in hospital) | 3 (21) |
| Evidence of tracks | 3 (21) |
| Non-professional resuscitation attempted | 1 (7) |
| Trauma | 1 (7) |
| Naloxone administration by non-medical professional | 0 (0) |
Law enforcement found needles at the scene of five (36 %) deaths, suggesting intravenous drug use. Investigators also found other drug paraphernalia at the scenes, such as crack pipes and cut straws, suggesting that acetyl fentanyl may have been smoked or snorted. Several drug packets found at the scenes of overdose deaths were tested. Two of three samples tested positive for acetyl fentanyl and negative for heroin; the third sample tested positive for heroin only. A sample obtained from a law enforcement drug seizure in May 2013 in a Rhode Island town where several deaths occurred tested positive for acetyl fentanyl and ANPP.
Table 2 shows a summary of substances of abuse identified by GC/MS confirmatory testing among the acetyl fentanyl overdose decedents. Thirteen acetyl fentanyl decedents tested positive for acetyl fentanyl. Eight decedents tested positive for both acetyl fentanyl and ANPP; five tested positive for acetyl fentanyl and no ANPP, and one tested positive for ANPP without acetyl fentanyl. Other drugs of abuse found in the toxicology testing were cocaine (57 %), morphine (an indication of heroin) (36 %), ethanol (36 %), and benzodiazepines (21 %) (Table 2).
Table 2.
Substances testing positive by gas chromatography/mass spectrometry among the acetyl fentanyl overdose decedents, Rhode Island, March–May 2013
| Case patient | Acetyl fentanyl | ANPP | Fentanyl | Cocaine | Morphinea | Ethanol | Benzodiazepinesb |
|---|---|---|---|---|---|---|---|
| 1 | Positive | Positive | Positive | Positive | |||
| 2 | Positive | Positive | Positive | Positive | |||
| 3 | Positive | Positive | Positive | Positive | Positive | ||
| 4 | Positive | ||||||
| 5 | Positive | Positive | |||||
| 6 | Positive | Positive | Positive | ||||
| 7 | Positive | Positive | Positive | ||||
| 8 | Positive | Positive | |||||
| 9 | Positive | Positive | Positive | ||||
| 10 | Positive | Positive | Positive | ||||
| 11 | Positive | Positive | Positive | ||||
| 12 | Positive | Positive | Positive | Positive | |||
| 13 | Positive | NA | Positive | Positive | |||
| 14 | Positive | NA | Positive | Positive | |||
| Total | 13 (93 %) | 9 (64 %) | 0 () | 8 (57 %) | 5 (36 %) | 5 (36 %) | 3 (21 %) |
Each of the following substances tested positive in one acetyl fentanyl decedent (not necessarily the same decedent): oxycodone, hydrocodone, hydroxyzine, sertraline, trazodone, lamotrigine, bupropion, doxepin, and desmethylcitalopram. Three tested positive for cetirizine and diphenhydramine. Substances testing positive represent at least one positive test from one of the following samples: femoral blood, heart blood, ante-mortem blood, or urine
aHeroin converts quickly to morphine in the blood, so morphine is an indication of heroin
bThese tested positive for diazepam, clonazepam, alprazolam, or their metabolites
Risk Factor Analysis
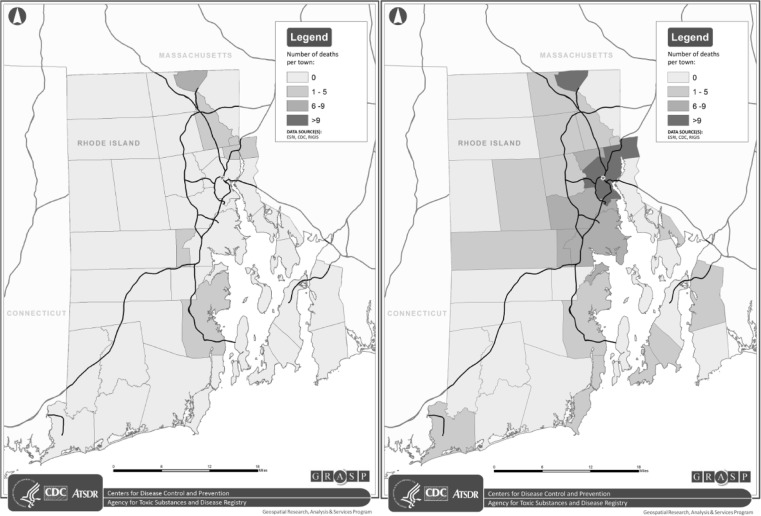
When comparing acetyl fentanyl overdose deaths to all other illicit drug overdose deaths that occurred in Rhode Island during March 2012–May 2013, the proportion of acetyl fentanyl overdose deaths that occurred in Woonsocket, Rhode Island, was significantly higher than the proportion of other illicit drug overdose deaths that occurred there (p < 0.001) (Table 3). Figure 2 shows the geographic distribution of the acetyl fentanyl deaths compared to the March 2012–March 2013 non-acetyl fentanyl illicit drug overdose deaths. A comparison of gender, race/ethnicity, age, and marital status revealed no significant differences between acetyl fentanyl overdose decedents and the comparison group. For the comparison groups, heroin, opiate, and heroin or opiate city where overdose death occurred was also the only significantly different characteristic (data not shown).
Table 3.
Associations between selected variables in bivariate models comparing acetyl fentanyl overdose deaths and non-acetyl fentanyl illicit drug overdose deaths, Rhode Island
| Acetyl fentanyl overdose deaths (n = 14) | Non-acetyl fentanyl illicit drug overdose deathsa (n = 135)b | p valuec | |
|---|---|---|---|
| n (%) | n (%) | ||
| Gender | |||
| Female | 4 (29) | 31 (23) | 0.74 |
| Male | 10 (71) | 104 (77) | |
| Race/ethnicity | |||
| White | 14 (100) | 100 (87) | 0.76 |
| Black | 0 (0) | 4 (3) | |
| Hispanic | 0 (0) | 11 (10) | |
| Age | |||
| Mean (SD) | 36.4 (13) | 41.7 (12) | 0.15 |
| 1–19 | 1 (7) | 2 (1) | |
| 20–29 | 5 (36) | 28 (21) | |
| 30–39 | 3 (21) | 29 (21) | |
| 40–49 | 1 (7) | 37 (27) | |
| 50–59 | 4 (29) | 32 (24) | |
| 60+ | 0 (0) | 7 (5) | |
| Marital status | |||
| Single | 8 (57) | 55 (41) | 0.52 |
| Married | 0 (0) | 13 (10) | |
| Divorced/widowed | 2 (14) | 14 (10) | |
| Missing | 4 (29) | 53 (39) | |
| Incident city | |||
| Woonsocket | 6 (43) | 10 (9)d | <0.001 |
aNon-acetyl fentanyl illicit drug overdose deaths that occurred during March 2012–March 2013
bDue to missing data, total numbers do not always sum to the total
c p value calculated using Fisher exact test for gender, race/ethnicity, and marital status. Wilcoxon rank sum test used for age, and Mantel-Haenszel chi-square for incident city
dMissing “Incident city” for 27 of the non-acetyl fentanyl illicit drug overdose deaths
Fig. 2.
Left: Acetyl fentanyl overdose deaths (n = 14) that occurred during March–May 2013. Right: Non-acetyl fentanyl illicit drug overdose deaths (n = 108; missing incident city for 27 non-acetyl fentanyl illicit drug overdose deaths) that occurred during March 2012–May 2013
Discussion
During March–May 2013, 14 acetyl fentanyl overdose deaths occurred in Rhode Island. This outbreak of acetyl fentanyl overdose deaths is the first time acetyl fentanyl has been identified in drug overdose deaths in the USA. The proportion of acetyl fentanyl overdose deaths that occurred in Woonsocket, Rhode Island, was significantly higher than the proportion of other illicit drug overdose deaths that occurred there.
Woonsocket, RI, has a population of about 40,000 persons, and there are several inpatient and outpatient treatment facilities there [17]. The concentration of acetyl fentanyl overdose deaths in Woonsocket allowed law enforcement agencies to identify the potential source of acetyl fentanyl. Several arrests were made which may have contributed to the stop of acetyl fentanyl overdose deaths. Another possible contributing factor to the stop of acetyl fentanyl overdose deaths is that users became aware of the acetyl fentanyl source and self-adjusted their dose to avoid overdosing.
The Rhode Island FTL preliminarily identified the unknown compound found during GC/MS testing as acetyl fentanyl by comparing the testing results to existing mass spectral libraries because no chemical standard existed at that time for more direct comparison. FTL worked closely with the Drug Enforcement Administration (DEA), whose staff synthesized acetyl fentanyl, allowing FTL to confirm the identity of the unknown substance as acetyl fentanyl. As a result of this investigation, an acetyl fentanyl chemical standard is now commercially available, a national reference laboratory offers acetyl fentanyl confirmatory testing, and methods to quantify acetyl fentanyl and its metabolite in human urine have been developed [18].
The Rhode Island FTL screens all suspicious deaths for a panel of 16 drugs of abuse, one of which is fentanyl. Rhode Island FTL uses the extensive screening panel to rule out drugs of abuse so that they do not have to outsource expensive confirmatory testing to reference laboratories. Testing practices across jurisdictions (i.e., states, counties, cities) vary, depending on public health budgets and priorities. National data are not available for the number of jurisdictions that screen for fentanyl, but anecdotal evidence suggests the percentage is low. GC/MS confirmatory testing can be expensive, so laboratories often do not confirm positive ELISA results by GC/MS. Acetyl fentanyl cross-reacted with the fentanyl ELISA. Consequently, without fentanyl screening and confirmatory GC/MS testing in Rhode Island, the cause of this outbreak may have gone unidentified. Similarly, acetyl fentanyl deaths may have occurred outside of Rhode Island and gone unidentified. As a result of this investigation, Pennsylvania confirmed at least one acetyl fentanyl overdose death and attributed at least 50 fatalities to either fentanyl or acetyl fentanyl during the first half of 2013 [19]. Similarly, Jefferson Parish outside of New Orleans reported five acetyl fentanyl overdose deaths in 2013 [20], and more recently, North Carolina reported three acetyl fentanyl overdose deaths in 2014 [21]. In December 2013, one additional acetyl fentanyl overdose death occurred in Rhode Island. When this manuscript went to press, no additional acetyl fentanyl overdose deaths had occurred in Rhode Island.
Among the acetyl fentanyl overdose decedents, the variety of illicit substances identified by toxicology testing suggests that polysubstance abuse was common. It also brings into question whether or not acetyl fentanyl was mixed with heroin, similar to how fentanyl and other fentanyl analogs were in previous fatal overdose outbreaks. The presence of other opioids (morphine—most likely representing a metabolite from intravenously administered heroin) could indicate that acetyl fentanyl was mixed with heroin. However, 64 % of acetyl fentanyl decedents tested negative for other opioids, indicating that acetyl fentanyl was not sold as a mixture with heroin and that acetyl fentanyl was not used in conjunction with heroin by the majority of acetyl fentanyl decedents. Results from drug samples that found acetyl fentanyl alone or with ANPP support this, but only four drug samples from scenes of death or seizures were tested, so we cannot say that acetyl fentanyl was never sold in a mixture with heroin.
Prescription drug abuse is the primary driver of the ongoing opioid overuse epidemic in the USA [22–24]. A recent study showed that among persons who abuse prescription opioids, past-year heroin use increased significantly over the past decade [25]. This increase in heroin use puts a larger number of people at risk for overdose from heroin or heroin contaminated with or replaced by more potent opioids, such as acetyl fentanyl. During January–March 2014, the lay press in Connecticut, Maryland, Pennsylvania, and Rhode Island reported spikes in overdose deaths caused by fentanyl mixed with heroin [26–29], similar to illicitly produced fentanyl that killed 1013 people in the multistate outbreak from 2005 to 2007 [15].
While acetyl fentanyl is estimated to be up to five times more potent than heroin (about 15 times more potent than morphine) [8, 30, 31], it is less potent than fentanyl and other fentanyl analogs (Table 4). Fentanyl and α-methylfentanyl are roughly 50 times more potent than morphine, and 3-methylfentanyl is between 50 and 500 times more potent than morphine [8]. Acetyl fentanyl may have been sold alone due to its relatively low potency, while in past outbreaks, fentanyl, 3-methylfentanyl, and α-methylfentanyl have mostly been found mixed with heroin, likely due to their higher potency [7–9, 11–15].
Table 4.
Effective dose values (ED50), lethal dose (LD50) values, and analgesic potency ratios to morphine and fentanyl for fentanyl analogs (adapted from Higashikawa and Suziki, 2008)
| Compound | ED50 (mg/kg) | LD50 (mg/kg) | Potency ratio to morphine | Potency ratio to fentanyl |
|---|---|---|---|---|
| Morphine | 0.33 | 470 | 1 | 0.02 |
| Fentanyl | 0.0061 | 62 | 54.1 | 1 |
| Acetyl fentanyl | 0.021 | 9.3 | 15.7 | 0.29 |
| α-Methylfentanyl | 0.0058 | 8.6 | 56.9 | 1.1 |
| 3-Methylfentanyl | 0.00058–0.0068 | – | 48.5–569 | 0.9–10.5 |
In the past, public health messages designed to deter drug users from using more potent heroin or heroin contaminated with fentanyl or fentanyl analog have sometimes had the opposite effect of attracting users. In 1991, during the Tango and Cash epidemic in New York City, 24 of 28 drug users reported searching for Tango and Cash, the brand of heroin contaminated with fentanyl [32]. Heroin overdoses can actually create a demand for a specific heroin because it is viewed as more potent [33]. Understanding this, and dealing with an unknown substance, the Rhode Island Department of Health (RIDH) was very careful in crafting their public health messages. In their initial press release and interviews with the media, before the substance had been confirmed as acetyl fentanyl, RIDH referred to the substance as a “new synthetic drug” and did not mention specifically where the overdose deaths were occurring [34]. They also included information on available drug treatment resources and about a pilot program that provides naloxone, an opioid receptor antagonist and antidote for opioid poisoning. RIDH did not announce the name of the substance until they confirmed that it was acetyl fentanyl, and RIDH continued to exclude information about where overdose deaths were occurring [35]. It is possible that this communication strategy prevented heroin users from seeking out or finding this new synthetic drug, potentially saving lives.
Since 1999, in an effort to reduce mortality from opioid overdoses, some states have implemented programs to increase the availability of naloxone (an opioid receptor antagonist and antidote for opioid poisoning) to at-risk intravenous drug users and their families and friends [34, 36–38]. An evaluation of one program in Massachusetts showed that opioid overdose death rates were reduced in communities where overdose education and nasal naloxone distribution programs were implemented [37]. As of December 2014, 27 states and the District of Columbia had naloxone distribution programs [39, 40]. In 2006, Rhode Island implemented Preventing Overdose and Naloxone Intervention (PONI) as a pilot program [39]. PONI trained intravenous drug users, family members, and inmates at the Adult Correctional Institutes how to administer naloxone. However, the current investigation found that none of the persons who died from acetyl fentanyl overdose received naloxone by a non-medical professional. More recently, to give more first responders access to naloxone, officials in Rhode Island and Vermont have distributed naloxone to law enforcement agents and trained them to administer it [41, 42]. Evaluating programs that provide law enforcement officials with naloxone and train them how to administer it will be important to understand whether the programs successfully reduce the number of opioid-related overdose deaths.
Overdose Good Samaritan Laws are another strategy employed by some states in an attempt to save lives in the event of drug overdoses. These laws encourage bystanders who observe a drug overdose to contact emergency responders and protect the caller from civil or criminal repercussions [40]. As of December 2014, 21 states and the District of Columbia have Overdose Good Samaritan Laws [40]. Rhode Island currently has an Overdose Good Samaritan Law, but citizens are not always aware of the protection and are often reluctant to alert the authorities when they witness a drug overdose because they fear prosecution [43, 44].
This investigation had several limitations. Using non-acetyl fentanyl illicit drug overdose deaths as a comparison group may not have been optimal, but that group was the most readily available for this investigation. To identify risk factors associated with acetyl fentanyl overdose death, a more ideal comparison group would have been acetyl fentanyl users who did not die. Because testing for fentanyl and its analogs is not part of routine clinical testing (e.g., overdose patients seen in emergency departments), such a comparison population was not available. Additionally, cases where not matched to persons in the comparison group. We conducted in-depth reviews of charts of all acetyl fentanyl overdose deaths, but medical records were not available for all cases. For the non-acetyl fentanyl illicit drug overdose death comparison group, toxicology results for other substances of abuse were not readily available for comparison to the acetyl fentanyl overdose deaths. Comparing substances present in toxicology reports for the acetyl fentanyl deaths with substances in reports for the comparison groups could indicate additional risk factors (e.g., number and type of concurrent substances used) for acetyl fentanyl overdose death. Persons who died of acetyl fentanyl overdose may have been missed if they had a delayed death caused by trauma or overdose, and there were no anti-mortem blood samples available. However, OSME collaborated with hospitals to avoid this, and at least one of the 14 acetyl fentanyl overdose deaths was a delayed death. Also, if biological samples did not cross-react with the fentanyl ELISA, death caused by acetyl fentanyl could have been missed. However, it seems unlikely that acetyl fentanyl would not cross-react with the fentanyl ELISA because of the strong cross-reaction that was seen among persons that died from acetyl fentanyl overdose.
Conclusions
We report the first outbreak of acetyl fentanyl overdose deaths in the USA. During March to May 2013, 14 acetyl fentanyl overdose deaths occurred in Rhode Island; nearly half of them occurred in Woonsocket. Acetyl fentanyl is a new street drug that is approximately four times more potent than heroin. The extensive testing done by the Rhode Island Forensic Toxicology Laboratory, and its thorough investigation of this new compound, was instrumental in identifying acetyl fentanyl. Testing of biological samples from the persons who died from acetyl fentanyl overdose and drug samples obtained by law enforcement revealed that acetyl fentanyl was not likely mixed with heroin, as other fentanyl analogs have been in past overdose death outbreaks. Rather, data from this study suggests that acetyl fentanyl was sold alone. Screening suspected opioid overdose deaths for fentanyl and performing confirmatory testing when the screen is positive to distinguish between fentanyl and acetyl fentanyl overdoses would help identify overdose deaths associated with acetyl fentanyl in other states.
Acknowledgments
Funding Source
This study is part of the regular duties of the Centers for Disease Control and Prevention.
Conflict of Interest
None
References
- 1.Centers for Disease Control and Prevention NCHS. Underlying cause of death 1999–2011 on CDC WONDER online database, released 2014. Data are from the Multiple Cause of Death Files, 1999–2011, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. 2011.
- 2.Levi J, Segal L, Fuchs Miller A. Prescription drug abuse: strategies to stop the epidemic 2013; 2013:64.
- 3.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. J Am Med Assoc. 2013;309(7):657–9. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 4.SAMHSA. Results from the 2012 National Survey on Drug Use and Health: summary of national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration 2013 Contract No.: HHS Publication No. (SMA) 13-4795.
- 5.Centers for Disease Control and Prevention Rates of drug poisoning deaths involving heroin,* by selected age and racial/ethnic groups—United States, 2002 and 2011. MMWR Morb Mortal Wkly Rep. 2014;63(27):595. [Google Scholar]
- 6.Rhode Island Department of Health. Fatal drug overdoses. http://www.health.ri.gov/data/death/drugoverdoses/2013.
- 7.Ayres WA, Starsiak MJ, Sokolay P. The bogus drug: three methyl & alpha methyl fentanyl sold as “China White”. J Psychoactive Drugs. 1981;13(1):91–3. doi: 10.1080/02791072.1981.10471455. [DOI] [PubMed] [Google Scholar]
- 8.Higashikawa Y, Suzuki S. Studies on 1-(2-phenethyl)-4-(N-propionylanilino)piperidine (fentanyl) and its related compounds. VI. Structure-analgesic activity relationship for fentanyl, methyl-substituted fentanyls and other analogues. Forensic Toxicol. 2008;26(1):1–5. doi: 10.1007/s11419-007-0039-1. [DOI] [Google Scholar]
- 9.Baum RM. New variety of street drugs poses growing problem. Chem Eng News. 1985;63(36):7–16. doi: 10.1021/cen-v063n036.p007. [DOI] [Google Scholar]
- 10.Stogner JM. The potential threat of acetyl fentanyl: legal issues, contaminated heroin, and acetyl fentanyl “disguised” as other opioids. Ann Emerg Med. 2014;64(6):637–9. doi: 10.1016/j.annemergmed.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 11.Kram TC, Cooper DA, Allen AC. Behind the identification of China White. Anal Chem. 1981;53(12):1379A–86. doi: 10.1021/ac00235a790. [DOI] [PubMed] [Google Scholar]
- 12.Hibbs J, Perper J, Winek CL. An outbreak of designer drug-related deaths in Pennsylvania. J Am Med Assoc. 1991;265(8):1011–3. doi: 10.1001/jama.1991.03460080081037. [DOI] [PubMed] [Google Scholar]
- 13.Martin M, Hecker J, Clark R, Frye J, Jehle D, Lucid EJ, et al. China White epidemic: an eastern United States emergency department experience. Ann Emerg Med. 1991;20(2):158–64. doi: 10.1016/S0196-0644(05)81216-8. [DOI] [PubMed] [Google Scholar]
- 14.Nieves E. Toxic heroin has killed 12, officials say. The New York Times. 1991 February 4, 1991.
- 15.Centers for Disease Control and Prevention Nonpharmaceutical fentanyl-related deaths—multiple states, April 2005–March 2007. MMWR Morb Mortal Wkly Rep. 2008;57(29):793–6. [PubMed] [Google Scholar]
- 16.Foerster EH, Mason MF. Preliminary studies on the use of n-butyl chloride as an extractant in a drug screening procedure. J Forensic Sci. 1974;19(1):155–62. [PubMed] [Google Scholar]
- 17.Rhode Island Department of Health. Agencies licensed to provide substance abuse treatment services. 2014. http://www.bhddh.ri.gov/serviceproviders/BH_ProviderSubAbuseList.pdf?7. Accessed 8 Aug 2014.
- 18.Patton AL, Seely KA, Pulla S, Rusch NJ, Moran CL, Fantegrossi WE, et al. Quantitative measurement of acetyl fentanyl and acetyl norfentanyl in human urine by LC-MS/MS. Anal Chem. 2014;86(3):1760–6. doi: 10.1021/ac4036197. [DOI] [PubMed] [Google Scholar]
- 19.Pennsylvania Department of Drug and Alcohol Programs. Department of Drug and Alcohol Programs warns about acetyl fentanyl. 2013.
- 20.Robin N. New street drug kills 5 in Jefferson Parish. 2013.
- 21.McDonald T. NC health officials warn of new street drug that killed 3 this year. News Observer 2014.
- 22.Manchikanti L, Helm S, 2nd, Fellows B, Janata JW, Pampati V, Grider JS, et al. Opioid epidemic in the United States. Pain Phys. 2012;15(3 Suppl):ES9–38. [PubMed] [Google Scholar]
- 23.Warner M, Chen LH, Makuc DM. Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006. NCHS data brief. 2009. 22:1–8. [PubMed]
- 24.Centers for Disease Control and Prevention Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–92. [PubMed] [Google Scholar]
- 25.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132(1–2):95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Owens D. Deadly heroin-fentanyl mix on streets prompts police warnings. The Courant 2014.
- 27.Press A. Md. has 37 deaths from heroin, fentanyl overdoses. 2014.
- 28.Conlon LFK. Cancer painkiller mixed with heroin blamed for 22 Pennsylvania deaths. 2014.
- 29.Freyer FJ. RI overdose deaths rise to 69 for 2014; illicit drugs and fentanyl key factors. Providence J. 2014.
- 30.Soine WH. Clandestine drug synthesis. Med Res Rev. 1986;6(1):41–74. doi: 10.1002/med.2610060103. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention Acetyl fentanyl overdose fatalities—Rhode Island, March–May 2013. MMWR Morb Mortal Wkly Rep. 2013;62(34):703–4. [PMC free article] [PubMed] [Google Scholar]
- 32.Fernando D. Fentanyl-laced heroin. J Am Med Assoc. 1991;265(22):2962. doi: 10.1001/jama.1991.03460220050029. [DOI] [PubMed] [Google Scholar]
- 33.Preble ECJ. Taking care of business: the heroin users life on the street. Int J Addict. 1969;4:1–24. [Google Scholar]
- 34.Rhode Island Department of Health. HEALTH Investigating New Synthetic Drug. 2013. http://www.health.ri.gov/news/.
- 35.Rhode Island Department of Health. HEALTH identifies new synthetic drug as acetyl fentanyl. online 2013.
- 36.Seal KH, Thawley R, Gee L, Bamberger J, Kral AH, Ciccarone D, et al. Naloxone distribution and cardiopulmonary resuscitation training for injection drug users to prevent heroin overdose death: a pilot intervention study. J Urban Health Bull N Y Acad Med. 2005;82(2):303–11. doi: 10.1093/jurban/jti053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Green TC, Heimer R, Grau LE. Distinguishing signs of opioid overdose and indication for naloxone: an evaluation of six overdose training and naloxone distribution programs in the United States. Addiction. 2008;103(6):979–89. doi: 10.1111/j.1360-0443.2008.02182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yokell MA, Green TC, Bowman S, McKenzie M, Rich JD. Opioid overdose prevention and naloxone distribution in Rhode Island. Med Health Rhode Island. 2011;94(8):240–2. [PMC free article] [PubMed] [Google Scholar]
- 40.Davis C. Legal interventions to reduce overdose mortality: naloxone access and overdose good samaritan laws: The Network for Public Health Law2014 December 2014.
- 41.Niedowski E. Rhode Island takes emergency steps on overdoses. 2014.
- 42.Wood P. Arundel police officers to carry drug to counteract heroin overdose. The Baltimore Sun 2014.
- 43.Tobin KE, Davey MA, Latkin CA. Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addiction. 2005;100(3):397–404. doi: 10.1111/j.1360-0443.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- 44.Tracy M, Piper TM, Ompad D, Bucciarelli A, Coffin PO, Vlahov D, et al. Circumstances of witnessed drug overdose in New York City: implications for intervention. Drug Alcohol Depend. 2005;79(2):181–90. doi: 10.1016/j.drugalcdep.2005.01.010. [DOI] [PubMed] [Google Scholar]