Abstract
The Malawi Longitudinal Study of Families and Health (MLSFH) is one of very few long-standing, publicly available longitudinal cohort studies in a sub-Saharan African (SSA) context. It provides a rare record of more than a decade of demographic, socioeconomic and health conditions in one of the world’s poorest countries. The MLSFH was initially established in 1998 to study social network influences on fertility behaviours and HIV risk perceptions, and over time the focus of the study expanded to include health, sexual behaviours, intergenerational relations and family/household dynamics. The currently available data include MLSFH rounds collected in 1998, 2001, 2004, 2006, 2008, 2010 and 2012 for up to 4000 individuals, providing information about socioeconomic and demographic characteristics, sexual behaviours, marriage, household/family structure, risk perceptions, social networks and social capital, intergenerational relations, HIV/AIDS and other dimensions of health. The MLSFH public use data can be requested on the project website: http://www.malawi.pop.upenn.edu/.
Key Messages.
Social networks exerted systematic and strong influences on HIV risk perceptions and the probability of spousal communication about HIV/ AIDS risks.
Rural Malawians have relatively accurate risk perceptions about a newborn child dying within its first year of life, and related frequent life outcomes/events; however, mortality expectations that measured the respondents’ own risk of death over a 1-, 5- or 10-year horizon were substantially overestimated compared with life table estimates.
Conditional cash transfers (CCTs) significantly increase the demand for learning one’s HIV status, but do not seem to affect reported sexual behaviours.
MLSFH data on self-reported functional limitations showed that disabilities among mature adults were common, and that the physical health may have been an important limiting factor for individuals’ social and economic activities.
Why was the cohort set up?
The Malawi Longitudinal Study of Families and Health (MLSFH) is one of a very few long-standing longitudinal cohort studies in a poor sub-Saharan African (SSA) context. The MLSFH cohorts were selected to represent the rural population of Malawi, where the vast majority of Malawians live in conditions that are similar to those in the rural areas of other countries with high HIV prevalence: health conditions are poor, health facilities and schools are overburdened and under-staffed, standards of living are low and nutritional needs of adults, children and the elderly are often not met. The MLSFH was initially established in 1998 to study social network influences on fertility behaviours and HIV risk perceptions, and over time the focus of the MLSFH expanded to include health (including HIV/AIDS), sexual behaviours, intergenerational relations and family/household dynamics. The MLSFH is a collaboration of the University of Pennsylvania with the College of Medicine and the Demography Unit, Chancellor College, both at the University of Malawi. It subsumes earlier research under the Malawi Diffusion and Ideational Change Project (MDICP). The data collection and research conducted by MLSFH was approved by the Institutional Review Board (IRB) at the University of Pennsylvania and, in Malawi, by the College of Medicine Research Ethics Committee (COMREC) or the National Health Sciences Research Committee (NHSRC).
Who is in the cohort?
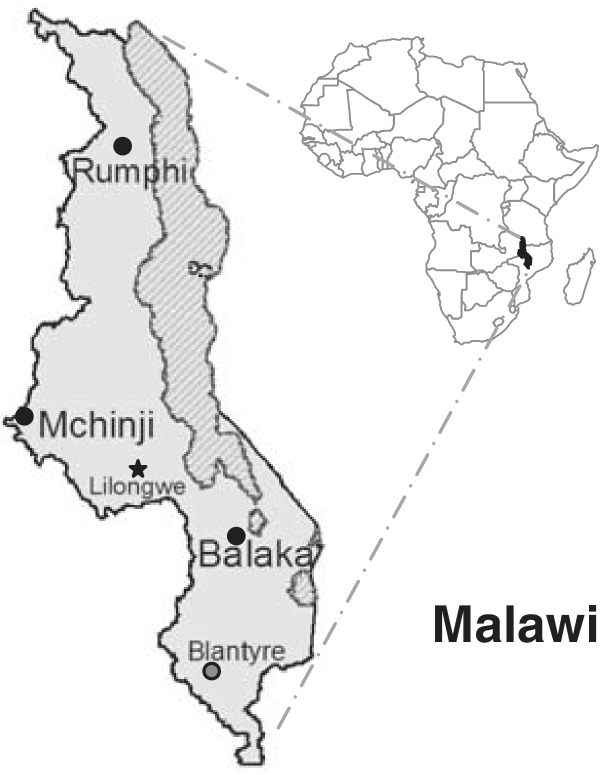
The MLSFH is based in three districts in Malawi—Rumphi in the north, Mchinji in the centre and Balaka in the south (Figure 1)—and major MLSFH data collection has been conducted in 1998, 2001, 2004, 2006, 2008, 2010 and 2012 (Figure 2). The target sample for the initial MLSFH round in 1998 consisted of 1721 ever-married women aged 15–49 years. A total of 1532 ever-married women aged 15–49 were surveyed, including also 1065 of their spouses (Figure 2). The initial target sample was established using a cluster random sampling strategy (Mchinji and Rumphi) and by drawing a subset of an earlier representative population survey (Balaka). Details of the initial sampling procedure are described in Appendix A2.1 (available as Supplementary data at IJE online). The initial sample characteristics closely matched the characteristics of the rural population of the 1996 Malawi Demographic and Health Survey (MDHS) (Appendix A2.1, available as Supplementary data at IJE online). In 2001, respondents were re-interviewed, along with any new spouses since 1998. In 2004, in addition to re-interviewing the 1998 and 2001 study population and new spouses, the MLSFH added a sample of approximately 1000 adolescents aged 15–24 to compensate for the ageing of the initial MLSFH sample and the underrepresentation of unmarried individuals at adolescent and young adult ages. During the 2008 MLSFH round, a sample of parents of the original MLSFH respondents was added to the MLSFH to increase the suitability of the MLSFH for studying intergenerational aspects and the health of older individuals in Malawi. This study population was re-interviewed in 2010. Table 1 provides summary statistics for the 2010 MLSFH study population. The 2012 MLSFH round was restricted to mature adults, defined as individuals aged 45 and over (Appendix A6.8, available as Supplementary data at IJE online).
Figure 1.
MLSFH study locations in Malawi
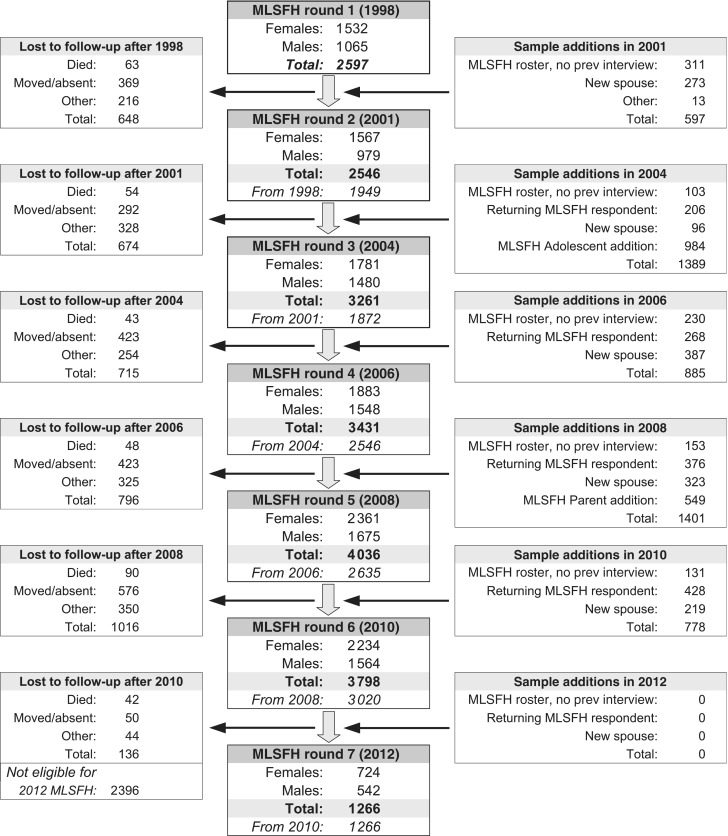
Figure 2.
MLSFH sample flow 1998–2012. MLSFH sampling and related relevant data collection procedures are described in Appendix A2. Only MLSFH mature adults, defined as individuals aged 45 and older, who were interviewed in both 2008 and 2010, were eligible for the 2012 MLSFH (Appendix A6.8). MLSFH study instruments are described in Table 3. In addition to the major MLSFH waves noted above, the MLSFH also conducted a migration follow-up in 2007 (Appendix A2.2), a 2006–07 MLSFH Incentive Study (Appendix A6.6) that collected repeated sexual diaries and a 2009 MLSFH Biomarker Study collecting biomarkers for cardiovascular risk, organ/metabolic function and inflammation (Appendix A6.7). The MLSFH survey data are complemented by extensive qualitative and ethnographic data that have been collected during 1998–2012. Prev, previous
Table 1.
Summary statistics for the MLSFH Round 6 (2010) study population
| Females | Males | Total | |
|---|---|---|---|
| mean (SD) | mean (SD) | mean (SD) | |
| Number of observations | 2,234 | 1,564 | 3,798 |
| Respondent’s age in 2010(years) | 41.43 | 43.42 | 42.25 |
| (16.83) | (16.63) | (16.78) | |
| Age group in 2010 (years) | |||
| <20 | 0.022 | < .01 | 0.013 |
| 20–29 | 0.279 | 0.281 | 0.280 |
| 30–39 | 0.221 | 0.186 | 0.207 |
| 40–49 | 0.184 | 0.190 | 0.186 |
| 50–59 | 0.136 | 0.149 | 0.141 |
| 60–69 | 0.077 | 0.110 | 0.090 |
| 70+ | 0.081 | 0.084 | 0.082 |
| Marital status | |||
| Married/living together | 0.770 | 0.870 | 0.811 |
| Separated | 0.019 | 0.008 | 0.015 |
| Divorced | 0.079 | 0.028 | 0.058 |
| Widowed | 0.120 | 0.018 | 0.078 |
| Never married | 0.012 | 0.076 | 0.038 |
| Children ever born | 5.66 | 5.96 | 5.79 |
| (3.36) | (4.59) | (3.91) | |
| Schooling attainment | |||
| No formal schooling | 0.273 | 0.125 | 0.212 |
| Primary schooling | 0.631 | 0.641 | 0.635 |
| Secondary or higher | 0.096 | 0.233 | 0.153 |
| Wealth indicator:house has metal roof | 0.213 | 0.207 | 0.211 |
| Region of residence | |||
| Central (Mchinji) | 0.317 | 0.339 | 0.326 |
| South (Balaka) | 0.351 | 0.323 | 0.339 |
| North (Rumphi) | 0.332 | 0.338 | 0.335 |
| Religion | |||
| Christian | 0.687 | 0.687 | 0.687 |
| Muslim | 0.262 | 0.248 | 0.256 |
| Other/none | 0.051 | 0.065 | 0.057 |
| Subjective health | |||
| Poor | 0.022 | 0.013 | 0.018 |
| Fair | 0.055 | 0.038 | 0.048 |
| Good | 0.237 | 0.181 | 0.214 |
| Very good | 0.437 | 0.404 | 0.424 |
| Excellent | 0.249 | 0.365 | 0.297 |
| Subjective likelihood of being infected with HIV | |||
| No likelihood | 0.570 | 0.656 | 0.605 |
| Low | 0.300 | 0.269 | 0.287 |
| Medium | 0.091 | 0.055 | 0.076 |
| High | 0.040 | 0.020 | 0.032 |
| At least one MLSFH HIV test result | 0.796 | 0.809 | 0.801 |
| HIV-positivea | 0.064 | 0.040 | 0.054 |
aHIV+ = at least one MLSFH HTC had a HIV-positive test result.
Comparisons of the 2010 MLSFH study population with the rural samples of the Malawi DHS and IHS3 surveys reveal that the MLSFH study population continues to closely match the characteristics of nationally-representative cross-sectional surveys (Appendix A4, available as Supplementary data at IJE online). As expected given the high mobility of the rural population, attrition in the MLSFH is substantial (Figure 2) and is predicted by several observable characteristics (such as age, gender, HIV status). Refusal to participate in the MLSFH, conditional on successfully contacting a respondent, is relatively rare (less than 5%), and temporary/permanent migration out of the MLSFH study regions are the primary causes of loss to follow-up. Despite these high levels of attrition, our analyses indicate that attrition does not necessarily bias the coefficients of estimated multivariate relationships that control for key socioeconomic characteristics (Appendix A5, available as Supplementary data at IJE online).
For about 40% of respondents who were interviewed by the MLSFH at least once, four or more rounds of MLSFH data are available (Table 2). Among 2010 MLSFH participants, more than 40% have data available from five or more MLSFH rounds, and more than 80% have data from three or more MLSFH rounds. Due to the specific selection criteria used for the 2012 MLSFH data collection for mature adults, all 2012 MLSFH participants have at least three rounds of available MLSFH data; for about two-thirds, data are available from five or more rounds, and for 40% of the 2012 participants, data are available from seven MLSFH rounds covering the period 1998–2012.
Table 2.
Number of MLSFH survey rounds available for MLSFH respondents
| Number of available MLSFH surveys | Among MLSFH respondents: |
|||||
|---|---|---|---|---|---|---|
| With at least one | MLSFH 6 (2010) | MLSFH 7 (2012) | ||||
| MLSFH interview |
participants |
participants |
||||
| % | Cum % | % | Cum % | % | Cum % | |
| 7 | 8.0 | 8.0 | 13.4 | 13.4 | 40.1 | 40.1 |
| 6 | 10.7 | 18.7 | 18.0 | 31.3 | 18.6 | 58.7 |
| 5 | 7.9 | 26.6 | 9.4 | 40.7 | 6.8 | 65.5 |
| 4 | 12.9 | 39.5 | 16.0 | 56.7 | 4.3 | 69.8 |
| 3 | 19.9 | 59.4 | 23.4 | 80.1 | 30.2 | 100.0 |
| 2 | 17.2 | 76.6 | 10.7 | 90.8 | – | – |
| 1 | 23.4 | 100.0 | 9.2 | 100.0 | – | – |
| Total | 6369 | 3798 | 1266 | |||
Cum, cumulative.
How often have they been followed up?
Major MLSFH rounds were collected in 1998 (MLSFH 1), 2001 (MLSFH 2), 2004 (MLSFH 3), 2006 (MLSFH 4), 2008 (MLSFH 5), 2010 (MLSFH 6) and 2012 (MLSFH 7) (Figure 2 and Tables 2 and 3). The MLSFH 7 in 2012 interviewed only mature adults (aged 45 and older), whereas all the earlier MLSFH rounds included the full MLSFH sample (Figure 2). In addition to the major MLSFH rounds 1–7, a subset of MLSFH respondents participated in 2006–07 in the collection of ‘sexual diaries’ (Table 3 and Appendix A6.6, available as Supplementary data at IJE online).1 A migration follow-up that tried to trace all ever-interviewed MLSFH respondents not interviewed during MLSFH 4 (2006) due to migration and/or temporary absence was conducted in 2007 and updated in 2013 (Table 3 and Appendix A2.2, available as Supplementary data at IJE online).2 In addition, in 2009 the MLSFH collected blood plasma-based biomarkers of cardiovascular and related health risks for a subset of MLSFH respondents in Balaka (Table 3 and Appendix A6.7, available as Supplementary data at IJE online).3,4
Table 3.
MLSFH survey content and other study components, by year
| MLSFH round | Measurements |
|---|---|
| All MLSFH rounds | Survey data: Demographic and socioeconomic characteristics of respondents, social and economic context, linkages with spouse data, vital status and migration/absence at time of MLSFH survey. Geocoded respondent residences since 2004; regional market and rainfall data |
| MLSFH 1 (1998) | Survey data: Childbearing and fertility desires; attitudes about and use of family planning methods; conversational networks about family planning and HIV/AIDS (see Appendix A6.1); gender attitudes and female autonomy; HIV/AIDS-related knowledge and risk perceptions; sexual behaviours and HIV risk reduction strategies |
| MLSFH 2 (2001) | Survey data: Mostly identical to MLSFH 1 (1998), plus social participation, marriage and sexual partnership histories (see Appendix A6.4). |
| MLSFH 3 (2004) | Survey data: Similar to MLSFH 2 (2001), plus: household rosters with data on household membership and health/schooling/morbidity and marital status of household members; measures of religious activities/affiliations; social capital and basic data on transfer and exchange networks; time use; household expenditures on health and schooling; AIDS-related stigma. No longer included: fertility histories and childbearing desires; detailed data about use of and attitudes to family planning methods |
| Biomarkers: Testing and counselling for HIV, gonorrhoea, chlamydia and trichomonas infections (see Appendix A3.1) | |
| Other: Randomized experimental design offering financial incentives for learning HIV status (see Appendix A3.1) | |
| MLSFH 4 (2006) | Survey data: Similar to MLSFH 3, plus: SF-12 self-reported health questionnaire; probabilistic expectations about health and HIV-risks (see Appendix A6.3); subjective discount rate; HIV testing history; audio-CASI interview for sensitive behaviours; intergenerational transfers and transfers with community members (see Appendix A6.2); mortality of household/family members. No longer included were conversational networks about family planning and religion |
| Biomarkers: Testing and counselling for HIV (see Appendix A3.2) | |
| Other: Initiation of MLSFH Incentive Study, a randomized experiment offering financial incentives for maintaining HIV-negative status (see Appendix A6.6) | |
| MLSFH Incentive Study 2006–07 | Survey data: Four rounds of sexual diaries providing detailed day-to-day data on sexual behaviours during a 9-day period prior to the interview (see Appendix A6.6) |
| Biomarkers: Testing and counselling for HIV in 2007 (after 3rd round of sexual diary collection) | |
| MLSFH 4 migration follow-up (2007) | Migration follow-up: with all ever-interviewed MLSFH respondents not interviewed during MLSFH 4 (2006) due to migration and/or temporary absence (see Appendix A2.2) |
| Survey data: Similar to MLSFH 4, plus detailed questions about migration history and migration reasons | |
| Biomarkers: Testing and counselling for HIV (see Appendix A3.3) | |
| MLSFH 5 (2008) | Survey data: Human capital, including schooling, self-reported SF-12 questionnaire module on physical and mental health, subjective well-being; household production and consumption, including standard of living, household assets, time use, health expenditure; social capital, including intergenerational/intrafamilial transfers and help relationships, transfer relationships with community members, participation in community associations; expectations, risk perceptions and attitudes, including probabilistic expectations about HIV risks and survival (see Appendix A6.3 and AIDS-related attitudes and knowledge; biographic information, including marriage and partnership histories (see Appendix A6.4), extra- and pre-marital relationships, partner characteristics. No longer included: conversational networks about AIDS |
| Biomarkers: Testing and counselling for HIV (see Appendix A3.3) | |
| MLSFH Biomarker Study (2009) | Focused on selected subset of MLSFH respondents residing in Balaka (N = 982) and collected biomarkers of inflammation, cardiovascular risks, metabolic processes and organ function (see Appendix A6.7) |
| Survey data: Health; illnesses and pain experienced by respondent, and household members; illnesses experienced by family members; water source; diet/nutrition | |
| Biomarkers: Biomarkers for wide-range CRP, total cholesterol, LDL, HDL, total protein, urea, albumin, blood urea nitrogen, creatinine, random blood glucose and HbA1c, collected using the LabAnywhere (previously Demecal) System (LabAnywhere, Haarlem, The Netherlands)5 | |
| Other: Height, weight and body mass index (BMI) | |
| MLSFH 6 (2010) | Survey data: Same as MLSFH 5 (2008). |
| MLSFH 7 (2012) | Follow-up survey focused on MLSFH mature adults aged 45 and older focused on mental heath, cognition and well-being (see Appendix A6.8) |
| Survey data: Similar to MLSFH 6 (2010), plus measures of depression and anxiety, measures of spatial/temporal orientation and language, measures of memory/recall and executive functioning, alcohol consumption | |
| Biomarkers: Testing and counselling for HIV (see Appendix A3.3) | |
| Other: Grip strength (both hands), height, weight and BMI | |
| MLSFH qualitative and related contextual data | Qualitative interviews on sexual attitudes and behaviours; qualitative data on HTC, HIV risks and investments in children; ethnographic studies of public conversations about AIDS in informal settings; detailed village characteristics and local infrastructure data; GPS data for all respondents; condom prices and local market prices of key crops and commodities |
What has been measured?
Across all rounds the MLSFH measured and documented the health, social, economic and demographic context of the MLSFH study population (Table 3). Whereas the specific MLSFH focus topics evolved over time, the seven rounds of MLSFH data provide longitudinal data on aspects such as: household structure and family change (household/family rosters, marriage and partnership histories), human capital (health, schooling, nutritional status), social capital (social networks, intrafamilial/intergenerational and community transfers, social participation), sexual behaviours (sexual relations and networks, HIV/AIDS risk behaviours and prevention strategies), subjective expectations and well-being [12-item Short-Form health survey (SF12) module, subjective well-being and mental health, HIV risk perceptions, mortality and HIV infection risks], household production and consumption (standard of living, household assets and income, expenditures on health and schooling, time use, migration) and mortality and migration of MLSFH participants and family members (verbal autopsies, migrant tracking). The MLSFH has also conducted repeated HIV testing and counselling (HTC) at respondents’ homes (see Appendix A3), and it has collected anthropometric data (height, weight and BMI) in 2008 and 2012 (Appendix A6.7 and A6.8, available as Supplementary data at IJE online). Selected biomarker-based indicators of health [C-reactive protein (CRP), high-density and low-density lipoprotein cholesterol (HDL, LDL) and others] were collected in 2009 for a subset of MLSFH respondents residing in Balaka (Appendix A6.7, available as Supplementary data at IJE online). The MLSFH also implemented randomized experimental designs related to HIV prevention. In 2004, the MLSFH HTC was combined with an experimental design that offered randomized financial incentives for individuals to learn their HIV status (see Appendix A3.1, available as Supplementary data at IJE online) and, during 2006–07, the MLSFH offered randomized conditional cash transfer to a subset of MLSFH respondents to encourage maintaining their HIV status for approximately year (see Appendix A6.6, available as Supplementary data at IJE online).1,6
What has the MLSFH found? Key findings and publications
A publication list for the MLSFH is available at http://malawi.pop.upenn.edu/mlsfh-publications/. Key findings across important topical areas follow.
Social interaction and social networks
MLSFH studies have shown that social networks exerted systematic and strong influences on risk perceptions (Figure 3) and the probability of spousal communication about HIV/AIDS risks. Social networks also amplified programme efforts aimed at increasing individuals’ information about HIV/AIDS and their assessments of their own risks as well as the risk they face from their spouses,7–10 and they were important in terms of providing mutual insurance and resources.11–14
Figure 3.
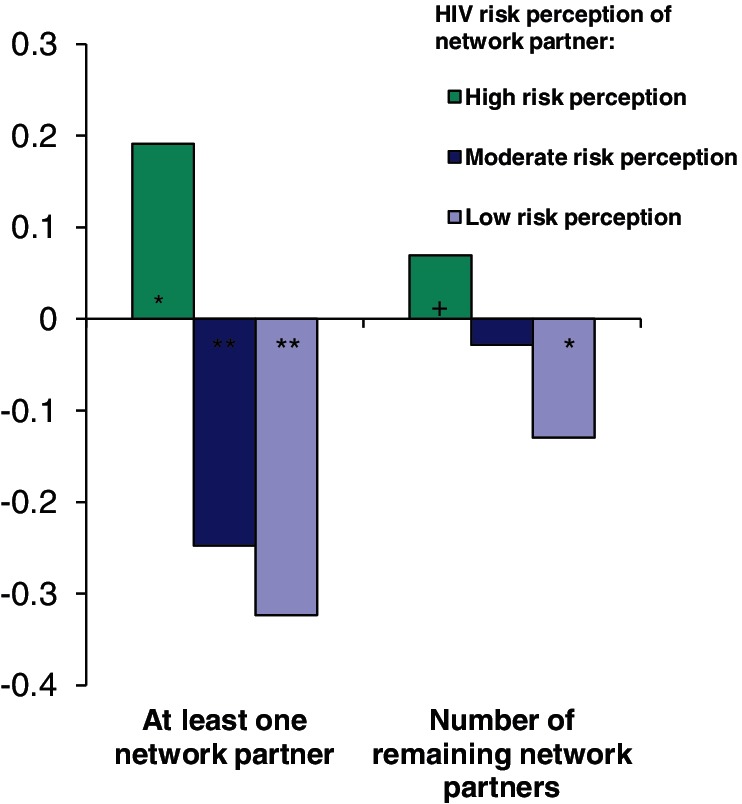
Effect of social network partners’ HIV/AIDS risk perceptions of MLSFH respondent’s own HIV/AIDS risk perceptions. The MLSFH survey measured perceived HIV/AIDS risk using the question ‘How worried are you that you might catch AIDS?’, with three response categories ranging from ‘not worried at all’ (coded as 1) to ‘worried a lot’ (coded as 3). The respondent was asked a corresponding question about his/her social network partners’ HIV/AIDS risk perceptions (for up to four social network partners). The graph shows the effect of the network partners’ risk perception (by number of network partners in each subjective risk category) on the respondent’s own risk perception, estimated based on longitudinal MLSFH 1–2 data using an instrumental-variable fixed-effect regression technique that controls for unobserved respondent characteristics and the potential selective reporting of network partners by respondents. The graph shows that social interactions with network partners who have high HIV risk perceptions increase the respondent’s own risk perceptions about HIV/AIDS, and this effect is particularly pronounced for the first member in a respondent’s network with high risk perceptions. Network partners with moderate or low HIV risk perceptions tend to reduce respondent’s own worries about HIV/AIDS. P-values: +P ≤ 0.10; *P ≤ 0.05; **P ≤ 0.01. Source: based on estimation results in Kohler et al.7
Subjective expectations about HIV infection and related health risks
For the period before 2006, when testing and treatment were not widely available in rural Malawi, the MLSFH has shown that the heuristics used by rural Malawians to assess their HIV risks often resulted in overestimates of their own likelihood of current HIV infection, as well as that of their spouses.15–17 Independently of HIV status, these high perceived risks of being infected with HIV had a strong negative effect on mental health and subjective well-being in rural Malawi.18 Higher subjective HIV infection risks were also significantly associated with the behaviours that were perceived as being most risky in terms of HIV infection.8,19 Using probabilistic expectations to measure subjective risk assessments, the MLSFH has also shown that rural Malawians have relatively accurate risk perceptions about a newborn child dying within its first year of life, and related frequent life outcomes/events. However, mortality expectations that measured the respondents’ own risk of death over a 1-, 5- or 10-year horizon were substantially overestimated compared with life table estimates.20–22
HIV testing and counselling (HTC)
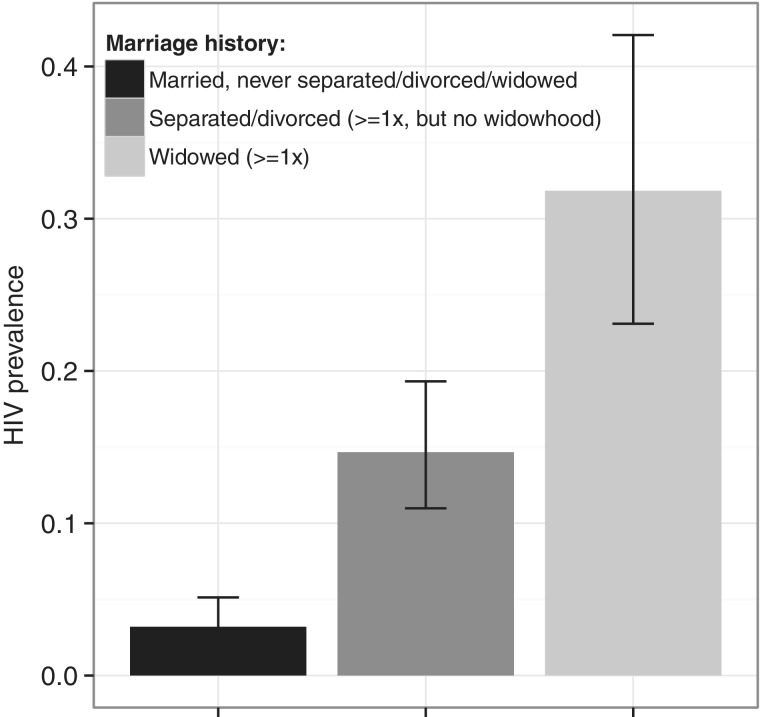
The MLSFH first implemented home-based HIV testing and counselling (HTC) in 2004, being the first large-scale survey to do so in Malawi, and over 90% of respondents in 2004 accepted the HIV test.23–25 MLSFH HTCs were repeated in 2006, 2008 and 2012. Adult HIV prevalence in the MLSFH in 2004–06 was around 7%.23,26 Among 2008 MLSFH respondents aged 15–49, 5.8% (women: 7.0%; men: 3.7%) were HIV-positive. HIV prevalence varies strongly with age, peaking for women around age 35 and for men around 50 (Appendix A3, available as Supplementary data at IJE online), which is similar to the pattern of HIV prevalence observed in the 2010 Malawi DHS,27 and it is substantially higher among female respondents who have experienced a marital separation/divorce or entered widowhood (Figure 4).
Figure 4.
HIV prevalence for women aged 35 with different marital histories. Marital histories are measured as: (i) women who are married and have never experienced a separation, divorce or widowhood (predicted HIV prevalence = 3.2%, 95% CI: 2.0%–5.1%); (ii) women who have experienced at least one marital separation or divorce, but not widowhood (predicted HIV prevalence = 14.7%, 95% CI: 11.0%–19.3%); and (iii) women who have entered widowhood at least once (predicted HIV prevalence = 31.8%, 95% CI: 23.1%–42.1%). Predicted HIV status at age 35 is obtained from a logistic regression of HIV status on age and marital history using 947 ever-married women aged 25–45 who were interviewed in the 2008 (MLSFH 5) (57.4% were married and had never experienced a separation, divorce or widowhood; 31.9% had experienced at least one marital separation or divorce, but not widowhood; and 10.7% had entered widowhood at least once). Marital histories up to 2008 were constructed using data from the 2006, 2008 and 2010 MLSFH and were cleaned for consistency (Appendix A6.4). Only respondents with recorded marital histories and at least one valid MLSFH HIV test during 2006–08 are included. Respondents with at least one HIV-positive MLSFH HIV test during 2006–08 are considered HIV-positive and all others are considered HIV-negative at the 2008 MLSFH round (MLSFH 5). Source: own calculations based on reconstructed marriage histories provided by Chae28
MLSFH studies have shown that sexually active HIV-positive individuals who learned their results during 2004 MLSFH HTC were three times more likely to purchase condoms 2 months later than sexually active HIV-positive individuals who did not learn their results.6 In addition, disclosure of HIV status by respondents to their spouses and other community members was found to be relatively common among rural Malawians (HIV-negative individuals also disclosed their HIV status, more frequently than HIV-positive individuals).29 Studying the medium-term consequences of learning HIV status during the 2004 MLSFH HTC on subsequent HIV/AIDS-related expectations and sexual behaviours also revealed that MLSFH respondents who received an HIV-negative test result in 2004 reported—somewhat paradoxically—higher and less accurate subjective expectations about being HIV-positive after 2 years.21 Learning the HIV status in 2004 did not seem to affect chances of divorce for either HIV-negative or HIV-positive MLSFH respondents after 2004, whereas it reduced the number of sexual partners among HIV-positive respondents, reduced fertility and increased condom use with spouses for both HIV-negative and HIV-positive respondents.21,30–35
Sexual behaviours, HIV risks and HIV prevention strategies
The MLSFH provided essential insights into the strategies of prevention that women and men in rural Malawi were using to reduce their HIV infection risks.8,36–39 For many within marriage, the extremes of complete fidelity or consistent condom use were not considered possible or acceptable, and there was considerable struggle to find strategies that were personally and socially acceptable. The emerging compromise strategy that has been documented using qualitative and quantitative MLSFH data was to avoid extramarital sex ‘as much as possible’; when it was not possible, select a partner who was likely to be ‘safe’; when that was not possible, use a condom.8,40,41 For married individuals, a primary strategy was to try to persuade the spouse to be faithful.8,42 For both women and men, divorce was also increasingly seen as an appropriate response to the threat that a spouse ‘will bring AIDS into the family’.8,43,44
Conditional cash transfers (CCTs) implemented as part of the MLSFH significantly increased the demand for learning one’s HIV status and the respondents’ participation in counselling subsequent to HIV tests.6 However, a MLSFH conditional cash transfer programme that offered financial incentives to men and women to maintain their HIV status for approximately 1 year found no effects of the offered incentives on HIV status or on reported sexual behaviour.1
Health and mortality
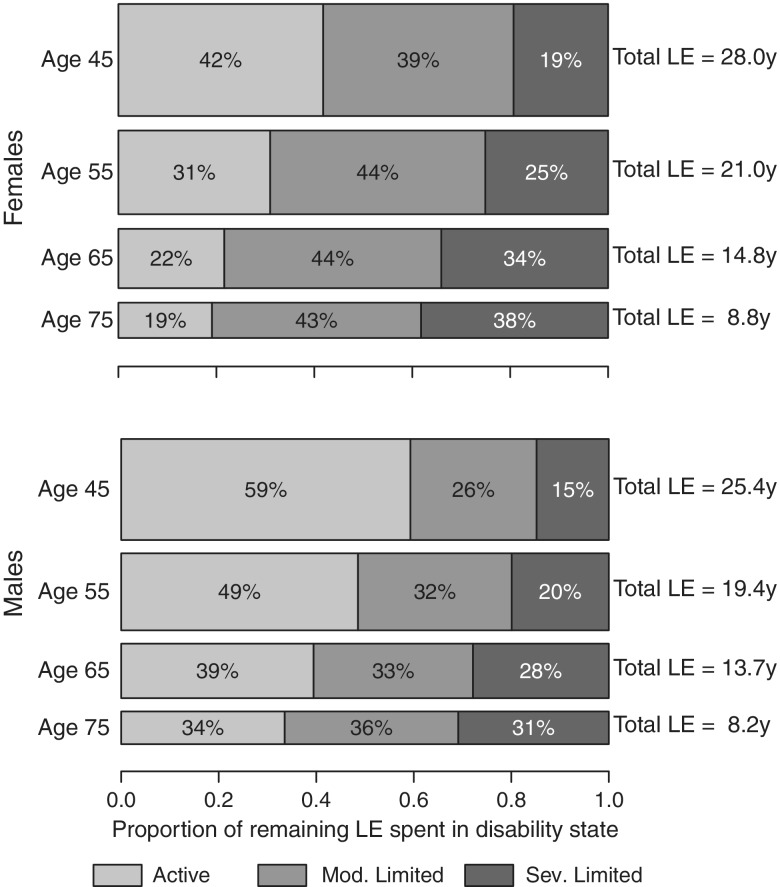
Mortality levels among MLSFH respondents have been shown to be similar to those of the Malawi general population, including differences by gender, region and HIV status.45–48 Analyses of the MLSFH biomarkers (total cholesterol, LDL, HDL, ratio of total cholesterol to HDL, albumin, creatinine and wr-CRP) found that only small proportions of MLSFH respondents had biomarker values in the critical range as defined by developed country standards. The biomarkers exhibited also only very modest associations with measures of socioeconomic status (SES), indicating that commonly found associations between SES and biomarker-based risk factors for age-related diseases among prime-aged and elderly individuals may not necessarily hold in contexts such as rural Malawi where individuals have been exposed to frequent infectious diseases and undernutrition.3,4 Although these biomarker-based analyses did not indicate widespread chronic conditions in the MLSFH study population, MLSFH data on self-reported functional limitations showed that disabilities among mature adults were common, and that the physical health may have been an important limiting factor for individuals’ social and economic activities. For example, in 2010, close to one-third of respondents aged 45–64 indicated that they had moderate functional limitations, and 8.5% reported being severely limited in their physical activities, and both physical limitations were substantially more common among individuals aged 65+.45 Moreover, the MLSFH suggested that 45-year-old women in Malawi can expect to spend 58% of their remaining 28 years of life with functional limitations, wheras 45-year-old men can expect to live 41% of their remaining 25.4 years subject to such limitations (Figure 5).
Figure 5.
Distribution of remaining life expectancy (LE) by disability state. The figure shows the proportions of remaining life an average individual will spend in healthy, moderately limited and severely limited life at ages 45, 55, 65 and 75, for females (top panel) and males (bottom panel). The height and area of each bar is proportional to the overall remaining life expectancy of the synthetic cohorts with initial ages of 45, 55, 65 and 75 years, and the differently shaded areas represent the distribution of the remaining life expectancy across the three disability states: healthy, moderately limited and severely limited. The bars do not necessarily reflect the ordering of these life-years by disability states as individuals in our analysis can recover and relapse between disability states, so not all years of limitation are spent at the end of life. Analyses are based on MLSFH respondents from 2006, 2008 and 2010, using longitudinal data to estimate age-patterns of functional limitations and the transitions-over-time between different disability states using a discrete-time hazard model. Based on these transition rates, multi-state life tables (MSLTs) are estimated using microsimulation approaches to estimate the above LEs by disability state. Source: Payne et al.45 Mod, moderately; sev, severely; y, year
What are the main strengths and weaknesses?
The MLSFH cohort was selected to represent the rural population of Malawi, where the majority of Malawians live in conditions that are similar to those in the rural areas of other countries in high HIV prevalence. In addition, main strengths of the MLSFH data include the relatively large sample size, generally high data quality, the longitudinal design covering more than a decade of health conditions and socioeconomic changes, and the broad focus of the MLSFH that provides information about health (including biomarkers for HIV), social networks, social and economic contexts, sexual behaviours, marriage and marital transitions and household structures and dynamics. Some weaknesses of the MLSFH are noteworthy. First, the MLSFH does not have a nationally representative sample design; this is in part related to the considerable costs such a study design would entail. As a result, urban contexts—where about 15% of the Malawi population live—are not reflected in the MLSFH, and the rural MLSFH study population is from only three study sites (Balaka, Mchinji and Rumphi). Nevertheless, despite this limitation, the MLSFH reflects the considerable heterogeneity of social and demographic contexts across rural Malawi, and comparison of the MLSFH study with the rural samples of nationally representative studies have shown few substantively relevant differences in the composition of MLSFH and national representative study populations (Appendix A4, available as Supplementary data at IJE online). A second important concern in the MLSFH pertains to attrition. As is expected, the MLSFH study population is subject to considerable attrition as a result of migration, temporary absences and mortality (Figure 2). Attrition was sometimes reversed as attriters at one wave were reinterviewed again at subsequent MLSFH waves. The MLSFH made some efforts to follow migrants who left the MLSFH study villages,2 but this migration follow-up was not comprehensive and did not cover the most recent waves. The data collection for an update of this migration follow-up was completed in 2013, and data cleaning is currently ongoing. Our analyses of attrition indicated that even though respondent characteristics often differ significantly between those who were lost to follow-up and those who were re-interviewed, and attrition was often predicted by key respondent characteristics, the coefficient estimates for standard family background variables in regressions and probit equations for the majority of the outcome variables were not affected significantly by attrition (see Appendix A5, available as Supplementary data at IJE online, and related attrition analyses31,49,50). Thus, the attrition levels observed in the MLSFH may not necessarily represent a general problem for obtaining consistent estimates of the coefficients of interest for most of these outcomes.
Can I get hold of the data? Where can I find out more?
Public use versions of the MLSFH data without identifying individual or village information are made publicly available with some delay after data collection. MLSFH data up to 2010 (MLSFH 6) can currently be requested on the project website at: http://www.malawi.pop.upenn.edu/, and these data are also processed for inclusion at the Inter-university Consortium for Political and Social Research (ICPSR) at the University of Michigan. Researchers interested in using MLSFH data that have not (yet) been made available as part of the MLSFH public use data files can submit a two-page proposal (including an analysis plan and IRB plan) to the MLSFH principal investigator (mailto:hpkohler@pop.upenn.edu). If deemed scientifically sound and not overlapping with ongoing MLSFH research projects, researchers will then be asked to sign a Data Use Agreement to be able to access and utilize the MLSFH data that are not part of the public use data sets. All analyses of the restricted MLSFH data are conducted in collaboration with members of the MLSFH study team.
Supplementary Data
Supplementary data are available at IJE online.
Funding
The first wave of the MLSFH was funded by the Rockefeller Foundation. Subsequent funding has been provided by the NICHD (grants R01 HD053781, R01 HD/MH041713, R01 HD37276, R01 HD044228, R21 HD050652, R03 HD058976, R21 HD071471), and has been supported by pilot grants from the Population Studies Center (PSC), Population Aging Research Center (PARC), the Boettner Center for Pensions and Retirement Security, the Institute on Aging and the Center for AIDS Research (CFAR), all at the University of Pennsylvania, supported by among other sources NIH grants NICHD R24 HD044964, NIA P30 AG12836, NIAID AI 045008. The project also received funding from the University of Pennsylvania Research Foundation. We are also grateful for pilot funding received through the Penn Center for AIDS Research (CFAR), supported by NIAID AI 045008, and the Penn Institute on Aging. NICHD R01HD053781 is the only grant that provided direct support for the writing of this manuscript.
Supplementary Material
Acknowledgements
We are grateful for research assistance provided by Sophia Chae, Theresa Fedor and Collin Payne for the analyses in this paper.
In addition to the authors of this paper, members of the MLSFH Study Team who have made important contribution to the design and/or implementation of the MLSFH during 1998–2012 include: Jimi Adams, Thomas Anderson, Nicole Angotti, Afua Appiah-Yeboah, Simona Bignami-Van Assche, Crystal Biruk, Jennifer Browning, Kevin Burke, Ben Capistrant, Ruben Castro, Sophia Chae, Davie Chagunda, Li-Wei Chao, Kondwani Chavula, Edgar Chihana, Raphael Chikadza, Abdullah Chilungu, Twaina Chilungu, Agnes Chimbiri, Rachael Chimbwete, Wyson Chimesya, Angela Chimwaza, Brian Chin, Jesman Chintsanya, Davie Chitenje, Shelley Clark, Elisabetta De Cao, Adeline Delavande, Kim Deslandes, Kim Dionne, Henry Doctor, Theresa Fedor, David Frankenfield, Emily Freeman, Margaret Frye, Patrick Gerland, Monica Grant, Sylvester Guuru, Mike Harhay, Stéphane Helleringer, Ning Hsieh, Heide Jackson, Humphreys Kabota, Liney Kachama, Amy Kaler, Jonathan Kandodo, Doreen Kanyika, Nancy Luke, Sydney Lungu, Denview Malagasi, Christopher Manyamba, Aaron Mapondera, Winford Masanjala, Chiyembekezo Mbewe, Tara McKay, Andy Mguntha, Esnat Mkandawire, Mathero Mkhalamba, Placid Mpeketula, Grace Msefula, Patrick Msukwa, Macgivens Msumba, James Mwera, Tyler Myroniuk, Blessings M’bwerazino, Flora Nankhuni, Ken Ndala, Oleosi Ntshebe, Julius Nyambo, Gift Nyasulu, Francis Obare Onyango, Collin Payne, Joel Phiri, Michelle Poulin, Mark Regnerus, George Reniers, Julio Romero Prieto, Anat Rosenthal, Gifton Saizi, Raül Santaeulàlia-Llopis, Enid Schatz, Chikondi Singano, Kristen Smith, Beth Soldo, Erica Soler-Hampejsek, Sarah Spell, Frank Taulo, Linda Tawfik, Evance Tchale Rebbeca Tesfai, Jenny Trinitapoli, Ina Warriner, Alexander Weinreb, Anika Wilson, Sara Yeatman, Eliya Zulu.
Conflict of interest: None declared.
References
- 1.Kohler HP, Thornton R. Conditional cash transfers and HIV/AIDS prevention: unconditionally promising? World Bank Econ Rev 2012;26:165–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anglewicz P. Migration, marital dissolution, and HIV infection in Malawi. Demography 2012;49:239–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kohler IV, Soldo BJ, Anglewicz P, Chilima B, Kohler HP. Association of blood lipids, creatinine, albumin and CRP with socioeconomic status in Malawi. Popul Health Metrics 2013;11:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohler IV, Anglewicz P, Kohler HP, Mcabe J, Chilima B, Soldo BJ. Evaluating health and disease in sub-Saharan Africa: minimally invasive collection of plasma in the Malawi Longitudinal Study of Families and Health. Genus 2012;68:1–27. [PMC free article] [PubMed] [Google Scholar]
- 5.Gootjes J, Tel RM, Bergkamp FJM, Gorgels JPMC. Laboratory evaluation of a novel capillary blood sampling device for measuring eight clinical chemistry parameters and HbA1c. Clin Chim Acta 2009;401:152–57. [DOI] [PubMed] [Google Scholar]
- 6.Thornton RL. The demand for learning HIV status and the impact on sexual behavior: evidence from a field experiment. Am Econ Rev 2008;98:1829–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kohler HP, Behrman JR, Watkins SC. Social networks and HIV/AIDS risk perceptions. Demography 2007;44:1–33. [DOI] [PubMed] [Google Scholar]
- 8.Watkins SC. Navigating the AIDS epidemic in rural Malawi. Popul Dev Rev 2004;30:673–705. [Google Scholar]
- 9.Kohler HP, Helleringer S, Behrman JR, Watkins SC. The social and the sexual: networks in contemporary demographic research. In: Kreager P, Capelli C, Ulijaszek S, Winney B. (eds). Population in the Human Sciences: Concepts, Models, Evidence. Oxford, UK: Oxford University Press, 2014. [Google Scholar]
- 10.Behrman JR, Kohler HP, Watkins SC. Lessons from empirical network analyses on matters of life and death in East Africa. In: Kleindorfer PR, Wind Y. (eds). The Network Challenge: Strategy, Profit, and Risk in an Interlinked World . Upper Saddle River, NJ: Wharton School Publishing; 2009. [Google Scholar]
- 11.Kohler IV, Kohler HP, Anglewicz P, Behrman JR. Intergenerational transfers in the era of HIV/AIDS: evidence from rural Malawi. Demogr Res 2012;27:775–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mtika MM, Doctor HV. Matriliny, patriliny, and wealth flow variations in Malawi. Afr Sociol Rev 2004;6:71–97. [Google Scholar]
- 13.Weinreb AA. Lateral and vertical intergenerational exchange in rural Malawi. J Cross-Cult Gerontol 2002;12:1–38. [DOI] [PubMed] [Google Scholar]
- 14.Potter GE, Handcock MS. A description of within-family resource exchange networks in a Malawian village . Demogr Res 2010;23:117–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anglewicz P, Kohler HP. Overestimating HIV infection: the construction and accuracy of subjective probabilities of HIV infection in rural Malawi . Demogr Res 2009;20:65–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anglewicz P, Bignami-Van Assche S, Clark S, Mkandawire J. HIV risk among currently married couples in rural Malawi: what do spouses know about each other? AIDS Behav 2010;14:103–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bignami-Van Assche S, Chao LW, Anglewicz P, Chilongozi D, Bula A. The validity of self-reported likelihood of HIV infection among the general population in rural Malawi. Sex Transm Infect 2007;83:35–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsieh N. Perceived risk of HIV Infection and mental well-being in rural Malawi. Demogr Res 2013;28:373–408. [Google Scholar]
- 19.Smith KP, Watkins SC. Perceptions of risk and strategies for prevention: responses to HIV/AIDS in rural Malawi. Soc Sci Med 2005;60:649–60. [DOI] [PubMed] [Google Scholar]
- 20.Delavande A, Kohler HP. Subjective expectations in the context of HIV/AIDS in Malawi. Demograp Res 2009;20:817–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delavande A, Kohler HP. The impact of HIV testing on subjective expectations and risky behavior in Malawi. Demography 2012;49:1011–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delavande A, Giné X, McKenzie D. Eliciting probabilistic expectations with visual aids in developing countries: how sensitive are answers to variations in elicitation design? J App Econometrics 2011;26:479–97. [Google Scholar]
- 23.Obare F, Fleming P, Anglewicz P, et al. Acceptance of repeat population-based voluntary counseling and testing for HIV in rural Malawi. Sex Transm Infect 2009;85:139–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Angotti N, Bula A, Gaydosh L, Zeev Kimchi E, Thornton RL, Yeatman SE. Increasing the acceptability of HIV counseling and testing with three C’s: convenience, Confidentiality and Credibility. Soc Sci Med 2009;68:2263–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Angotti N. Working outside of the box: how HIV counselors in Sub-Saharan Africa adapt Western HIV testing norms. Soc Sci Med 2010;71:986–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Obare F. Response to population-based voluntary counseling and testing for HIV in rural Malawi. PhD thesis Graduate Group in Demography, University of Pennsylvania, 2007. [Google Scholar]
- 27.Malawi Demographic Health Survey. Malawi Demographic and Health Survey 2010 (Final Report) . Zomba, Malawi, and Calverton, MD: National Statistical Office and ICF Macro, 2011. [Google Scholar]
- 28.Chae S. Essays on family structure and marriage in sub-Saharan Africa. PhD thesis, Graduate Group in Demography, University of Pennsylvania, 2013. [Google Scholar]
- 29.Anglewicz P, Chitsanya J. Disclosure of HIV status between spouses in Malawi. AIDS Care 2011;23:998–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thornton RL. HIV testing, subjective beliefs and economic behavior. J DevEcon 2012;99:300–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fedor TM, Kohler HP, Behrman JR. The impact of learning HIV status on marital stability and sexual behavior within marriage in Malawi. Population Studies Center, University of Pennsylvania, 2013. [Google Scholar]
- 32.Yeatman S. HIV infection and fertility preferences in rural Malawi. Stud Fam Plann 2009;40:261–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yeatman SE. The impact of HIV status and perceived status on fertility desires in rural Malawi. AIDS Behav 2009;13:S12–S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Paula A, Shapira G, Todd P. How beliefs about HIV status affect risky behaviors: evidence from Malawi. J Appl Econ In press. Earlier version of this paper is available as PIER Working Paper No. 11-005. URL: http://ssrn.com/paper=1766000 (14 February 2014, date last accessed). [Google Scholar]
- 35.Shapira G. How Subjective Beliefs About HIV Infection Affect Life-Cycle Fertility: Evidence From Rural Malawi. 2013. World Bank Policy Research Working Paper #6343. http://elibrary.worldbank.org/content/workingpaper/10.1596/1813-9450-6343 (24 February 2014, date last accessed). [Google Scholar]
- 36.Tawfik L, Watkins SC. Sex in Geneva, sex in Malawi. Soc Sci Med 2007;64:1090–101. [DOI] [PubMed] [Google Scholar]
- 37.Poulin MJ. The sexual and social relations of youth in rural Malawi: strategies for AIDS prevention. PhD thesis Department of Sociology, Boston University, 2006. [Google Scholar]
- 38.Tavory I, Swidler A. Condom semiotics: meaning and condom use in rural Malawi. Am Sociol Rev 2009;74:171–89. [Google Scholar]
- 39.Behrman JR, Kohler HP. Sexual transmission of HIV. In: Lomborg B. (ed). Rethink HIV: Smarter Ways to Invest in Ending HIV in Sub-Saharan Africa . Cambridge, MA: Cambridge University Press; 2012. [Google Scholar]
- 40.Chimbiri A. The condom is an intruder in marriage: evidence from rural Malawi. Soc Sci Med 2007;64:1102–15. [DOI] [PubMed] [Google Scholar]
- 41.Clark S, Poulin M, Kohler HP. Marital aspirations, sexual behaviors, and HIV/AIDS in rural Malawi. J Marriage Fam 2009;71:396–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zulu EM, Chepngeno G. Spousal communication about the risk of contracting HIV/AIDS in rural Malawi. Demogr Res 2003;1:247–77. [Google Scholar]
- 43.Kaler A. AIDS-talk in everyday life: HIV/AIDS in men’s informal conversations in southern Malawi. Soc Sci Med 2004;59:285–97. [DOI] [PubMed] [Google Scholar]
- 44.Reniers G. Divorce and remarriage in rural Malawi. Demogr Res 2003;1:175–206. [Google Scholar]
- 45.Payne C, Mkandawire J, Kohler HP. Disability transitions and health expectancies among adults 45 years and older mature in Malawi: a cohort modeling approach. PLoS Med 2013;10:e1001435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Doctor HV. Adult mortality in rural Malawi. S AfrJDemogr 2004;9:49–66. [Google Scholar]
- 47.Chin B. Essays on health, mortality, and intergenerational transfers in rural Malawi. PhD thesis. Graduate Group in Demography, University of Pennsylvania, 2011. [Google Scholar]
- 48.Gerland P, Kaphuka J, Mandere G, Misiri H, Fleming P. Adult mortality estimations from cohort and census/survey data: a comparison of direct and indirect methods in rural Malawi. 2007. http://uaps2007.princeton.edu/abstracts/70706 (24 February 2014, date last accessed). [Google Scholar]
- 49.Alderman H, Behrman JR, Kohler HP, Maluccio J, Watkins SC. Attrition in longitudinal household survey data: some tests for three developing country samples. Demogr Res 2001;5:79–123. [Google Scholar]
- 50.Anglewicz P, Adams J, Obare F, Kohler HP, Watkins S. The Malawi Diffusion and Ideational Change Project 2004–06: data collection, data quality and analyses of attrition. Demogr Res 2009;20:503–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.