Abstract
The understanding of how cardiac ion channels function in the normal and the diseased heart has greatly increased over the last four decades thanks to the advent of patch-clamp technology and, more recently, the emergence of genetics, as well as cellular and molecular cardiology. However, our knowledge of how these membrane-embedded proteins physically interact with each other within macromolecular complexes remains incomplete. This review focuses on how the main cardiac inward sodium channel (NaV1.5) and the strong inward rectifier potassium channel (Kir2.1) function within macromolecular complexes to control cardiac excitability. It has become increasingly clear that these two important ion channel proteins physically interact with multiple other protein partners and with each other from early stages of protein trafficking and targeting through membrane anchoring, recycling, and degradation. Recent findings include compartmentalized regulation of NaV1.5 channel expression and function through a PDZ (postsynaptic density protein, Drosophila disc large tumor suppressor, and zonula occludens-1 protein) domain-binding motif, and interaction of caveolin-3 with Kir2.1 and ankyrin-G as a molecular platform for NaV1.5 signaling. At the cardiomyocyte membrane, NaV1.5 and Kir2.1 interact through at least two distinct PDZ domain-scaffolding proteins (synapse-associated protein-97 and α1-syntrophin), thus modulating reciprocally their cell-surface expression at two different microdomains. Emerging evidence also shows that inheritable mutations in plakophilin-2, ankyrin-G, dystrophin, syntrophin, synapse-associated protein-97, and caveolin-3, among others, modify functional expression and/or localization in the cardiac cell of NaV1.5, Kir2.1 or both to give rise to arrhythmogenic diseases. Unveiling the mechanistic underpinnings of macromolecular interactions should increase our understanding of inherited and acquired arrhythmogenic cardiac diseases and may lead to advances in therapy.
Keywords: macromolecular complex, NaV1.5, Kir2.1, SAP97, syntrophin
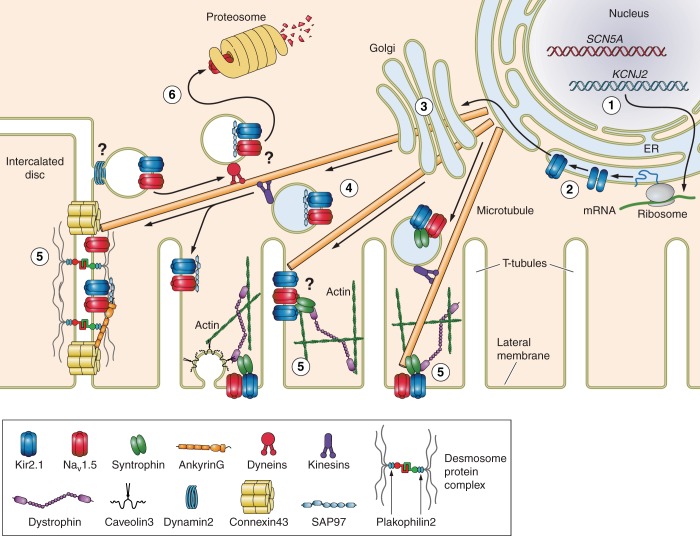
the cardiac action potential (AP) depends on the orchestrated voltage- and time-dependent opening and closing of selective ion channels formed by proteins that embed in the lipid bilayer of the cardiomyocyte membrane (10, 60). Most of our current understanding of how these cardiac ion channels function comes from using reductionist experimental approaches, including one in which a single ion channel or protein is genetically or pharmacologically altered to explore its role in cellular excitability, depolarization, repolarization, and rest. While such approaches have been successful in shedding light on the role played by individual ion channels in shaping the AP, alone they provided an overly simplistic view of the function of such channels within their native multiprotein cellular environment. Like other proteins, the functional lifetime of a cardiac ion channel spans several steps that include, but are not limited to, transcription, translation, oligomerization and glycosylation in the Golgi apparatus, vesicular trafficking, membrane retention, posttranslational modification, turnover, ion channel function, and degradation (Fig. 1) (6). At each step the channel might interact with dozens of other different proteins (26). Furthermore, normal cardiomyocyte function requires certain unique physiological characteristics, such as intracellular compartmentalization of protein assemblies and function, electrical excitation, electromechanical coupling, and cell-to-cell communication, all of which depend on the precise function and localization of ion channels interacting with multiple proteins within each individual cell (6).
Fig. 1.
Steps (1–6) and molecular partners of intracellular trafficking and localization of cardiac inward sodium channel (NaV1.5) and inward rectifier potassium channel (Kir2.1) in the cardiac myocyte. 1, transcription; 2, translation; 3, Golgi-mediated glycosylation; 4, vesicular trafficking; 5, compartmental localization and function; 6, retrograde vesicular trafficking, protein degradation, and recycling. While the processes governing common anterograde and retrograde trafficking of NaV1.5 and Kir2.1 proteins are currently under investigation, evidence suggests interaction at the membrane through synapse-associated protein-97 (SAP97) and/or syntrophin. ER, endoplasmic reticulum.
Na+ and inward rectifier K+ ion channels are of particular interest because the interplay of the ionic currents that flow through them is essential in the control of cellular excitation and AP propagation (80). Evidence is accumulating that from early stages of protein assembly and trafficking, these two channel types physically interact with common partners that may include, but are not limited to, anchoring/adapter proteins, enzymes, and regulatory proteins (Table 1). The increased understanding of how these intermolecular interactions occur has begun to shift the traditional paradigm of a channel-to-channel communication that depends solely on the transmembrane voltage. Importantly, mutations in these adapter/anchoring proteins and enzymes are now starting to be linked to inherited arrhythmogenic syndromes in which ion channels remain structurally intact but have altered function, further highlighting the relevant clinical implications that macromolecular ion channel interplay may have in both normal physiology and cardiac diseases.
Table 1.
Common protein partners of NaV1.5 and Kir2.1
| Protein | Localization | Protein Function | NaV1.5 Interaction | Kir2.1 Interaction | Interaction Sites | References |
|---|---|---|---|---|---|---|
| AnkyrinG | ID | Anchoring, transport | Yes | ? | Domains II and III loop (VPIAXX-ESD) of NaV1.5 | 38, 44, 46, 49–51 |
| AP-1 | Cytosol and TGN | Adaptor, vesicle transport | ? | Yes | Tertiary structure between NH2-terminal and COOH-terminal Kir2.1 domains | 45 |
| Caveolin-3 | LM | Anchoring, caveolae formation | Yes | Yes | ? | 19, 76, 81, 88 |
| Desmoglein-2 | ID | Desmosome structure | Yes | ? | ? | 59 |
| Dystrophin | LM and TT | Cytoskeletal, anchoring | Yes | Yes | COOH-terminus PDZ-binding domain | 27, 39, 54 |
| Filamin-A | Sarcomere | Cytoskeletal, anchoring | ? | Yes | Amino acids 307–326 of COOH-terminus of Kir2.1 | 57, 63 |
| FHF | Cytosol | Growth factor | Yes | ? | COOH-terminus of NaV1.5 | 32, 42, 83 |
| GPD1-L | Cytosol and LM | Enzyme, modulator | Yes | ? | ? | 43, 78, 79 |
| MOG-1 | Cytosol and ID | Intranuclear traffic | Yes | ? | Domain II and III loop of NaV1.5 | 35, 87 |
| Plakophilin-2 | ID | Desmosome structure | Yes | ? | ? | 14, 15, 28, 64, 65 |
| SAP97 | ID and TT | Scaffolding | Yes | Yes | COOH-terminus PDZ-binding domain | 27, 29, 30, 40, 41, 48, 54, 70, 75, 82 |
| Syntrophin | LM | Cytoskeletal, adaptor | Yes | Yes | COOH-terminus PDZ-binding domain | 34, 39, 48, 54, 74, 86 |
AP-1, adaptor protein complex 1; GPD1-L, glycerol-3-phosphate dehydrogenase-like protein; MOG1, multicopy suppressor of gsp-1; SAP97, synapse-associated protein 97; ID, intercalated disc; LM, lateral membrane; TT, T tubule; TGN, trans-Golgi network; FHF, fibroblast growth factor homologous factors.
This brief review article focuses on recent findings on the intermolecular interactions between the main voltage-gated cardiac sodium channel, NaV1.5, and the strong inward rectifier potassium channel, Kir2.1, their protein partners that have been linked to proarrhythmogenic disease, and the potential role that their multiprotein assemblies may have in normal ventricular electrophysiology and arrhythmogenesis.
Sodium Channels in Macromolecular Complexes
The voltage-gated cardiac sodium channel consists of a 260-kDa α-subunit (NaV1.5) coded by the SCN5A gene (12, 31, 61) and two β-subunits that modulate but are not crucial for functional NaV1.5 expression (12, 13). NaV1.5 folds into four homologous domains (I–IV) to form a selective pore that permeates inward sodium current (INa), which is the main depolarizing current involved in excitation (phase 0 of the AP) of atrial, Purkinje, and ventricular cells. Voltage-gated sodium channels are normally closed when the cell is at rest. However, upon depolarization above a threshold of ∼−65 mV, NaV1.5 channels open in an all-or-none fashion, generating a large and fast INa that further depolarizes the cell. Upon depolarization above −40 mV, the channels quickly inactivate, allowing voltage-gated Ca2+ and K+ channels to interact in a voltage-dependent manner and contribute to the AP plateau, excitation-contraction coupling, and repolarization (10, 60). Rapid excitation and all-or-none depolarization generated by INa activation are essential for the rapid conduction of the electrical impulse through the atrial and ventricular myocardium. It is now well established that, given the crucial role of NaV1.5 in cellular excitability, functional defects in NaV1.5 translate into altered AP propagation and conduction, as well as arrhythmia inducibility (2, 16). In addition, in recent years the role of the late INa has become increasingly important in both normal conditions as well as a number of pathologies (3).
Such is the case for mutations in SCN5A, which have been implicated in NaV1.5 loss-of-function (decreased INa) (8, 72, 77) and gain-of-function (increased INa) (84) ion channel diseases. Multiple human SCN5A channel mutations have been reported, and the functional phenotype of each mutation depends on the localization and type of mutation. NaV1.5 gain-of-function mutations are observed, for example, in the long QT syndrome type 3 (LQT3) (52, 84). On the other hand, loss-of-function mutations in SCN5A are predominant in up to 30% of patients with Brugada syndrome (BrS), a genetically transmissible proarrhythmic disease and one of the major causes of sudden death in the young (11, 66, 71). In some cases, BrS associates with inherited SCN5A mutations that impair NaV1.5 trafficking to the cell membrane, resulting in loss of functional expression (7, 72, 77). In other cases, BrS mutations may cause loss of INa through gating defects; e.g., speeding of inactivation and a hyperpolarizing shift in channel availability (58).
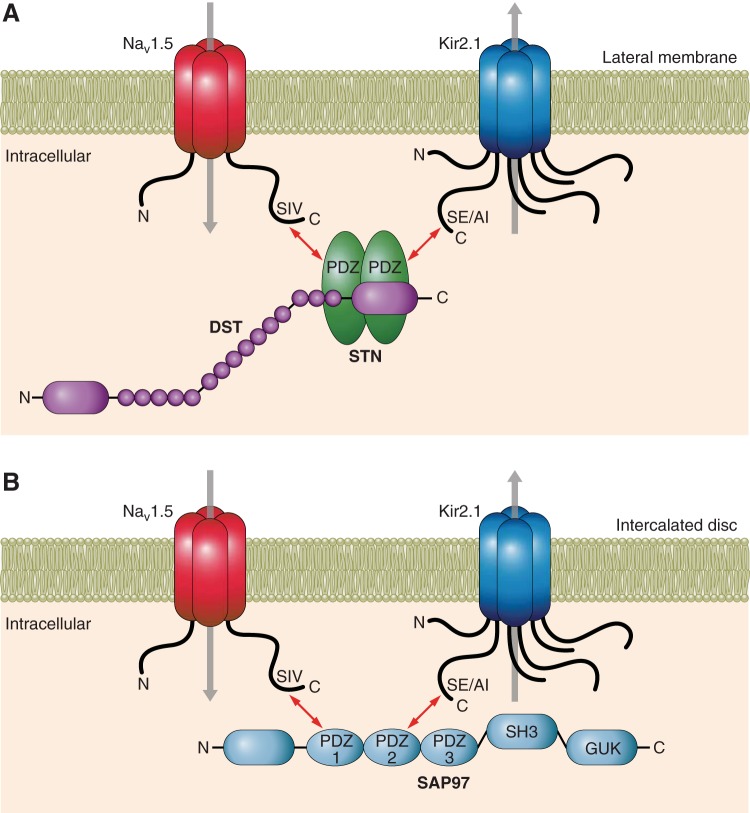
To date. more than 15 different non-ion channel proteins have been reported to interact with NaV1.5 at any time point from biosynthesis to degradation, half of them associated with arrhythmogenic disease. However, the motifs through which NaV1.5 interacts with other proteins have not been fully characterized. While it has been shown that individual NaV1.5 α-subunits interact with each other, it is currently undetermined whether this occurs through their respective NH2-terminal or COOH-terminal domains (17). Voltage-gated Na+-channel COOH-termini are key in the regulation of channel trafficking through their binding partners (62). Also, there is evidence that each channel interacts with anchoring/adapter proteins, enzymes, and protein modulators mainly through its COOH-terminus, which includes a PDZ (postsynaptic density protein, Drosophila disc large tumor suppressor, and zonula occludens-1 protein) domain (S/T)XV-COOH consensus motif (Fig. 2, A and B). NaV1.5 has been shown to interact with syntrophin, synapse-associated protein-97 (SAP97), and PTHP1 proteins through its PDZ-binding domain and a VPIAxxSD motif between loops II and III through which it interacts with ankyrin-G (1).
Fig. 2.
Common protein partners of NaV1.5 and Kir2.1. A: interaction with the syntrophin/dystrophin complex with NaV1.5 and Kir2.1 at the intercalated disc is mediated through PDZ (postsynaptic density protein, Drosophila disc large tumor suppressor, and zonula occludens-1 protein)-binding domains in the COOH-terminus of both channels. B: interaction of NaV1.5 and Kir2.1 with SAP97 at the lateral membrane or T tubule is also mediated through PDZ-binding domains in the COOH-terminus of both channels. NH2-terminus-binding domains have not been described thus far for either channel. DST, dystrophin; STN, syntrophin; SH3, Src homology-3 domain; GUK, guanylate kinase; SIV, serine-isoleucine-valine; SE/AI, serine-glutamic acid/alanine-isoleucine.
Some Proteins Partners of NaV1.5 Associated with Electrophysiological Disease
Plakophilin-2.
Plakophilin-2 (PKP2) is an essential protein component of the cardiac desmosome and is mainly located at the intercalated disc (ID). Mutations in PKP2, the gene that codes for PKP2, have been associated with proarrhythmogenic syndromes such as BrS and arrhythmogenic right ventricular cardiomyopathy (14, 28). The Delmar laboratory has made substantial contributions in this field. They showed that NaV1.5 coimmunoprecipitates with PKP2 and that both proteins clearly colocalize at the ID. Furthermore, in vitro silencing of PKP2 decreased INa in cultured cardiac myocytes and led to slow conduction velocity, rate-dependent activation failure, and arrhythmic behavior in neonatal rat ventricular monolayers (64, 65). Also, reduced levels of PKP2 in PKP2+/− mice correlated with a reduction in INa without changing NaV1.5 mRNA transcript levels or altering NaV1.5 protein localization (15). Finally, in an elegant paper using superresolution microscopy, the same group found different PKP2 mutations in a pool of patients with BrS. They also reported that by decreasing NaV1.5 and increasing separation of microtubules from the cell end (14), BrS-associated PKP2 mutations decreased INa at the ID in both HL-1 and human-induced pluripotent stem cell-derived cardiomyocytes. Importantly, the INa deficit was restored by transfection of wild-type PKP2. While the relevance of PKP2 to cardiac electrophysiology is clear, the molecular determinants of PKP2-NaV1.5 interaction are still unknown and will undoubtedly be the topic of future research efforts.
Desmoglein-2.
Desmoglein-2 is another desmosomal protein that coimmunoprecipitates with NaV1.5 (59). Similar to PKP2, mutations in desmoglein-2 have been linked with arrhythmogenic right ventricular cardiomyopathy. Interestingly, decreased INa and slow conduction velocity (CV) were found in a mouse harboring a N271S mutation in DSG2, the gene that codes for desmoglein-2 (59). While further studies are warranted, this further highlights the importance that desmosomal proteins play in retaining/modulating NaV1.5 at the ID and consequently the potential mechanistic roles in cardiac electrophysiological diseases characterized by impaired CV such as BrS.
Caveolin-3.
The caveolin family of proteins assist in the formation of particular lipid domain or rafts called caveolae. Caveolae are specialized membrane microdomains enriched in cholesterol and sphingolipids that are present in multiple cell types including cardiomyocytes (5). Functionally, caveolin-3 (Cav3) is both an anchoring protein for molecules within caveolae and a regulatory element for protein signaling. Mutations in CAV3, the gene coding Cav3, which is also the main cardiac isoform, have been associated with hypertrophic cardiomyopathy, LQT9, and sudden infant death syndrome (SIDS) (18, 19, 81). Cav3 coimmunoprecipitates with NaV1.5 in both heterologous expression systems and adult mammalian cells, and both proteins colocalize at the lateral membrane (68, 81, 88). Furthermore, coexpressing wild-type NaV1.5 in HEK293 cells with either V14L, T78M, or L79R mutant Cav3 found in SIDS patients increased the persistent inward INa, which could also provide a potential mechanism for increased AP duration leading to LQT9 (19). However, this has not been proven in vivo, and further studies are warranted.
Ankyrin-G.
Ankyrin proteins facilitate the anchoring and transport of other proteins including ion channels to the cell cytoskeleton. Mutations in the two main cardiac isoforms, ANK2, the gene coding for ankyrin-B, and ANK3, which codes for ankyrin-G, have been associated with cardiac proarrhythmogenic syndromes that include LQT4, atrial fibrillation, and BrS (20, 49–51). Currently, only ankyrin-G has been shown to interact with NaV1.5, and this occurs directly via the linker loop VPIAXX-ESD between domains II and III of NaV1.5, an ankyrin-binding motif that was originally described in neurons (38). In the cardiac myocyte, ankyrin-G has been found to primarily localize at the ID and the T tubules (33). Additionally, the NaV1.5 E1053K mutation was found in a patient with BrS and was shown to impair the binding of NaV1.5 to ankyrin-G, which in turn prevented the accumulation of NaV1.5 at the cell surface, without altering protein folding or Golgi-mediated trafficking (44, 50). Interestingly, this effect was only observed in cardiomyocytes, as mutant NaV1.5 E1053K channels were correctly targeted to the membrane in HEK293 cells, further highlighting the importance of using cardiac myocytes for future studies on macromolecular complex interplay. In a recent report, ankyrin-G deficiency in mice resulted in loss of Na+ channels, membrane reorganization of PKP2, and lethal arrhythmias in response to β-adrenergic stimulation. Thus ankyrin-G seems critical for in vivo membrane recruitment and regulation of NaV1.5 at the ID (46).
Dystrophin-associated protein complex.
The dystrophin-associated protein complex (DAPC) includes dystrophin, which is a cytoskeletal protein that plays a major structural role in muscle cells. It links the cytoskeleton to the extracellular matrix by binding its NH2-terminus to actin and its COOH-terminus to the glycoprotein complex at the sarcolemma (24). As illustrated in Fig. 2A, NaV1.5 interacts with dystrophin via syntrophin adapter proteins through its PDZ-binding motif [serine-isoleucine-valine (SIV)] (27, 54). Lack of dystrophin was shown to modulate NaV1.5 in the mdx mouse model of Duchenne muscular dystrophy. In addition to reduced dystrophin, mdx mice have reduced NaV1.5 protein expression, as well as reduced INa and CV, whereas mRNA levels of SCN5A transcript are unchanged (27). Importantly, syntrophin does not localize to the ID. Therefore, syntrophin-dependent NaV1.5 modulation most likely occurs at the lateral membrane (54). To date, two mutations in SNTA1, the gene coding α1-syntrophin, have been associated with LQTS (74, 86). While macromolecular disruption has been proposed as a mechanism of these mutations, further studies are warranted.
Multicopy suppressor of gsp-1.
Multicopy suppressor of gsp-1 (MOG1) is a protein involved in regulating intranuclear protein trafficking. NaV1.5 has been shown to coimmunoprecipitate with MOG1, and both proteins colocalize at the ID. Additionally, the two proteins interact via the intracellular loop between domains II and III of NaV1.5 (87). Furthermore, two mutations in RANGRF, the gene that codes for MOG1, have been recently associated with BrS (35). One of these mutations, E83D, failed to regulate NaV1.5 trafficking to the cell membrane and silencing MOG1 decreased INa by roughly 50% (35).
Glycerol-3-phosphate dehydrogenase-like protein.
Glycerol-3-phosphate dehydrogenase-like protein (GPD1-L) shares more than 80% sequence homology with GPD. While it displays glycerol dehydrogenase activity, it is slower than GPD. Pull-down assays have shown that GPD1-L interacts with NaV1.5 (78). More importantly, mutations in GPD1-L have been associated with BrS and three cases of SIDS (43, 79). The A280V mutation in GPD1-L that was linked with BrS as well as all three SIDS-associated GPD1-L mutations (E83K, I124V, R273C) produced significant reductions in INa in both heterologous expression systems and neonatal mouse myocytes when coexpressed with wild-type NaV1.5 (43, 79). The molecular mechanisms of NaV1.5-GPD1-L have not been elucidated; thus further work is warranted.
Fibroblast growth factor homologous factors.
Fibroblast growth factor homologous factors (FHFs) are nonsecreted intracellular modulators of ion channels that bind to COOH-terminal domain of Na+ channels (42). Knockdown of FHF13 (FGF13), was shown to decrease INa density and channel availability in cardiac myocytes (83). It also reduced wave propagation velocity in myocyte monolayers. In addition, FGF13 knockdown-reduced CaV1.2 current density and substantially altered subcellular targeting of CaV1.2 channels (83). More recently, FGF12 was reported to be the major FHF expressed in the human ventricle and that a single missense mutation in FGF12-B (Q7R-FGF12) reduced binding to the NaV1.5 COOH-terminus, yielding a BrS phenotype. In adult rat cardiac myocytes, Q7R-FGF12, but not wild-type FGF12, reduced INa, channel availability and AP amplitude without affecting Ca2+ channel function (32).
Membrane-associated guanylate kinases protein complexes.
Membrane-associated guanylate kinase (MAGUK) proteins are characterized by their modular domain structure, which contains up to three PDZ domains, an Src homology-3 domain, and a catalytically inactive guanylate kinase-like domain. Such domains allow MAGUK proteins to function as intracellular scaffolding molecules, playing important roles in the assembly of macromolecular signaling complexes and determining the subcellular distribution of different ion channels (25, 36).
Recently, an increasing number of studies have centered on macromolecular complexes that include SAP97, a MAGUK protein that is expressed abundantly in the heart (30, 41, 48, 75). SAP97 is important for the function and localization of a number of ion channels (54). Of interest, a gain-of-function mutation in SAP97 (M861T) was observed in a human patient with BrS (Ackerman M, personal communication, 2015).
In the past few years, studies addressing the role of SAP97 with regard to the function and localization of NaV1.5 channels have led to fascinating results. The interaction of NaV1.5 with SAP97 is very important for the localization of NaV1.5 at the ID, as was first shown in the dystrophin-deficient mdx mouse and confirmed in wild-type adult rat heart (48, 54). Both proteins have been shown to colocalize at both the ID and at the T tubules (48) and to interact through PDZ binding (Fig. 2B) (27). However, in a recent report, NaV1.5 expression at the ID and INa density were shown to be unaffected in knock-in mice lacking the NaV1.5 SIV domain (ΔSIV) (70). Also, the Abriel group (29) has shown that cardiac-specific ablation of SAP97 in a transgenic mouse had no effect on INa, although the authors did observe an increase in SCN5A mRNA expression levels and drastic reduction in potassium currents. These surprising results bring attention to the fact that our current understanding of the role of SAP97 in the regulation of NaV1.5 channel expression and function remains preliminary, and further studies are warranted.
Potassium Channels in Macromolecular Complexes
Evidence accumulated over the last 20 years strongly indicates that K+ channel function depends on complicated, multicomponent protein complexes that help in the assembly and delivery of the right channel subunits to the right place in the cell membrane at the right time. Growing interest on the molecular composition of these complexes and how they influence the function and localization of the different K+ channels is leading to novel insights into how different K+ channel isoforms and accessory proteins within the complexes participate in the control of cardiac excitability and the mechanisms of arrhythmias.
The breadth of the K+ channel field is enormous, and it would take a compendium to do it justice. Therefore, here we will limit the discussion to the inward rectifier potassium (Kir2.x) channels responsible for IK1, which is the strongly rectifying current that controls the resting membrane potential, the depolarization toward threshold and the final phase of AP repolarization (53, 69, 80). Kir2.x ion channel proteins are distinguished by their ability to strongly rectify, that is, to pass K+ current in the inward direction much more readily than outward, a characteristic that is critically important in the modulation of cardiac excitability. The Kir2.x family of proteins includes five isoforms; Kir2.1 (IRK1/KCNJ2), Kir2.2 (IRK2/KCNJ12), Kir2.3 (IRK3/KCNJ4), Kir2.4 (IRK4/KCNJ14), and Kir2.6 (IRK/KCNJ18) (37). IK1 density is substantially larger in the ventricles than the atria, yielding functionally important AP differences; these dissimilarities are due in part to different expression density and subcellular localization of the channels subunits that form IK1 (21). Kir2.1 is the major isoform underlying IK1 in the human ventricular muscle, with Kir2.2 expressing to a lesser extent. In contrast, in atrial cells, IK1 is mainly conducted through Kir2.3 channels (47, 85).
Clinically, KCNJ2 gene mutations leading to loss of function of Kir2.1 have been linked with Andersen-Tawil syndrome (ATS) (23, 55). On ECG, patients with ATS show QT prolongation and predisposition to ventricular tachyarrhythmias such as torsades de pointes. On the other hand, Kir2.1 gain-of-function mutations give rise to the type-3 variant of the short QT syndrome, which results in significant QT shortening and increased risk of sudden cardiac death (56).
Expression, trafficking, localization, and function of Kir2.x channels are all regulated by interactions with other proteins. However, in contrast with other ion channels, the information available on protein-protein interactions involving Kir2.x channels is limited. As illustrated in Fig. 2, Kir2.1, Kir2.2, and Kir2.3 contain a COOH-terminal motif [the last 3 amino acids sequence (SXI), where X is any amino acid] that enables interaction with PDZ domain containing proteins (41). Leonoudakis et al. showed that cardiac Kir2.x channels interact with SAP97, CASK, Veli-4, and Mint1 proteins, all members of the MAGUK family, through a PDZ-binding motif. They also demonstrated that components of the DAPC, including α1-, β1-, and β2-syntrophin, dystrophin and dystrobrevin, interact with Kir2.x channels through the PDZ-binding motif (21, 39–41).
Some Additional Partners of Kir2.x
MAGUK protein complexes.
A model has been proposed in which Kir2.x channels associate with distinct MAGUK proteins (SAP97, CASK, Veli, Mint1), forming different complexes (40). However, the association of Kir2.x channels with CASK, Veli-4, and Mint1 has not been explored in detail, and their role in cardiac cells has not been clarified. On the other hand, it has been shown that SAP97 regulates IK1 by modulating surface expression of Kir2.x channels. Binding to SAP97 is important to anchor Kir2.x channels at the plasma membrane, mainly through their interaction with their PDZ-binding domains (Fig. 2B) (48, 75, 82). In addition, data suggest that SAP97 binding to the Kir2.3 COOH-terminal domain results in conformational modifications in the channel structure with consequent modification of the unitary conductance (82). It has also been shown that SAP97 assembles a signaling complex involved in β1-adrenergic receptor (β1-AR) regulation of IK1. The SAP97-binding site on the COOH-terminus of Kir2.x channels overlaps a putative protein kinase A phosphorylation site (RRXS) at the extreme COOH terminus of Kir2.x channels. If this site is phosphorylated, SAP97 will fail to bind to the Kir2.x channel protein (75). Furthermore, SAP97 with its Src homology-3 and guanylate kinase-like domains (Fig. 2) can interact with A-kinase anchoring protein and help assemble kinases and phosphatases. Taken together, the data suggest that the interaction between the SAP97 and Kir2.x is a dynamic process that can be regulated by the phosphorylation state of the Kir2.x channel. Finally, further data suggest that SAP97 actively participates in the localization of Kir2.1 and Kir2.2 channels at the T tubules and of Kir2.1 and possibly also Kir2.3 at the ID (48, 75, 82). Therefore, the above studies indicate that SAP97 contributes to the function and localization of the Kir2.x channels and that it is central for the assembly of macro-signaling complexes and their distribution within precise cellular subdomains of the cardiac myocyte.
Caveolin-3.
Recently, it was reported that Kir2.1 may associate with Cav3 in human cardiac cells. The interaction seems to play a pathophysiological role in Cav3 mutations related with LQT9, where there is decreased IK1 density, mainly due to reduced cell-surface expression of Kir2.1 channels (76). Even though an important relationship between Cav3 and Kir2.1 has been demonstrated, further studies are needed to elucidate the molecular mechanisms involved in the interaction and to identify other molecular components of the Cav3-Kir2.1 macromolecular complex.
Dystrophin-associated protein complex.
While Kir2.x channels do interact with α1-, β1-, and β2-syntrophin, dystrophin, and dystrobrevin through their respective PDZ-binding motifs (Fig. 2A) (39), the physiological relevance of these interactions in cardiac cells remains poorly understood. For example, cardiomyocytes from the dystrophin-deficient mdx mouse have a small, albeit statistically significant, decrease in Kir2.1 protein without modification in KCNJ2 mRNA (27). On the other hand, a transgenic mouse model that overexpresses Kir2.1 channels also shows significantly increased membrane levels of SAP97, NaV1.5, and syntrophin proteins, without changes in the mRNA levels for their respective genes (DLG1, SCN5A, and SNTA1) (34, 48). Conversely, in the ventricles of heterozygous KCNJ2 knockout (Kir2.1−/+) mice, the relative membrane protein levels of SAP97, NaV1.5, and syntrophin are significantly reduced, whereas the genes coding these proteins are unchanged (34, 48).
Altogether, the foregoing findings suggest that in cardiac cells, the DAPC may be important in the regulation of Kir2.x channel expression/function. It is also possible that DAPC proteins contribute to determining the subcellular localization of Kir2.x channels in cardiomyocytes, similar to what has been demonstrated for NaV1.5 channels. Thus more studies are warranted to further elucidate this potential interaction.
Filamin-A.
Filamins are actin–cross-link proteins. They directly interact with diverse other proteins and are involved in multiple cellular processes including cell-cell and cell-matrix adhesion, mechanoprotection, actin remodeling, and intracellular signaling pathways (89, 90). Filamin-A has been shown to increase the number of functional resident Kir2.1 channels within the membrane in arterial smooth muscle cells by binding to a region located between amino acids 307 and 326 on the Kir2.1 COOH-terminus. Thus filamin-A appears to act as a cytoskeletal-anchoring protein for the Kir2.1 channel within cells, stabilizing its surface expression and potentially recruiting it to signaling complexes within the membrane (63). Altogether, there is growing evidence supporting the significant role of filamin as an interacting partner of membrane channels in cardiac cells (57). Further experiments will be required to pinpoint the role of filamin on the function of Kir2.x channels in cardiomyocytes. Additionally, while filamin has been shown to localize at the Z lines in cardiac cells, more work will be needed to decipher whether pools of Kir2.x channels are localized in this region of the myocytes as a result of their interaction with filamin.
Adaptor protein-1 complex.
Up to this point, we have dealt with proteins that associate with Kir2.x channels at the plasma membrane. However, critical though less well understood are the interactions of Kir2.x with partner proteins encountered during early trafficking. Recently, it was demonstrated that the adaptor protein-1 adaptin complex interacts with Kir2.1 through an unusual Golgi exit signal dictated by a tertiary structure, localized within the confluence of the cytoplasmic NH2 and COOH terminal domains. The signal creates an interaction site that allows properly folded Kir2.1 channels to insert into clathrin-coated vesicles at the trans-Golgi for export to the cell surface (45). This study uncovered a critical regulatory step for controlling cell-surface expression of the Kir2.x channels from the Golgi and highlighted the importance of understanding whether alterations in the Golgi export process can also account for cardiac disorders that may arise from Kir2.1 mistrafficking.
In summary, in addition to normal density and biophysical properties, Kir2.x channels require proper localization at specialized macromolecular membrane subdomains. Clearly, the molecular and structural characteristics of such subdomains are central in the regulation of local Kir2.x channels and a vastly unexplored field in cardiac electrophysiology.
NaV1.5-Kir2.1 Channels in Channelosomes
As illustrated in Fig. 2, in the heart, NaV1.5 and Kir2.1 independently interact with at least two distinct PDZ domain-scaffolding proteins, SAP97 and α1-syntrophin (27, 41, 82). Recent work has demonstrated that SAP97 mediates NaV1.5-Kir2.1 interactions (48). It was shown that Kir2.1 overexpression increased NaV1.5 and excitability. Conversely, Kir2.1 downregulation decreased INa. Moreover, virally mediated transfer of SCN5A in adult rat ventricular myocytes increased Kir2.1 protein at the membrane and also increased IK1 density. Those results suggested that these two channel proteins interact dynamically and reciprocally at the molecular level (48). It also appears that common molecular mechanisms might be involved in the regulation of Kir2.1 and NaV1.5 functional expression, which is mediated at least in part, through SAP97 PDZ binding within a macromolecular complex (27, 39, 48). Figure 1 illustrates potential interacting pathways that might potentially start from early protein biosynthesis or traffic. Common protein partners associated with NaV1.5 and Kir2.1 are listed in Table 1.
A 70 to 80% reduction in INa and IK1 density was recently demonstrated in a zebrafish model of arrhythmogenic cardiomyopathy (ACM) with cardiac myocyte-specific expression of the human 2057del2 mutation in the gene encoding plakoglobin (4). Reduction of INa and IK1 density produced marked changes in the AP morphology: resting membrane potential was significantly depolarized, AP duration was significantly prolonged, and maximum rate of phase 0 rise was markedly reduced. The myocytes expressing 2057del2 plakoglobin showed a marked decrease in the amount of SAP97 signal at the cell surface. Together, these observations suggested that the aberrant SAP97 distribution in mutant plakoglobin expressing myocytes resulted in altered trafficking of NaV1.5 and Kir2.1 channels. ACM is generally associated with mutations in genes that code proteins in the desmosome, a specialized intercellular-junction complex. However, the above study highlights the importance of additional proteins, such as Kir2.1, NaV1.5 and SAP97, as potential mechanistic players in arrhythmias linked to ACM (4).
The in vivo role of SAP97 in the heart was assessed by Gillet et al. (29), using a genetically modified mouse model of cardiomyocyte-specific deletion of SAP97. The mice showed expected functional reductions in potassium currents IK1, Ito, and IKur. However, a surprising finding was that INa was not altered, even though NaV1.5 protein expression was slightly increased, which could reflect some type of compensatory effect. The role of SAP97 in the function and localization of NaV1.5 channels thus remains a topic of further experiments and discussion.
As already discussed, associations of NaV1.5 via its COOH-terminal SIV motif allow at least two coexisting pools of NaV1.5 channels in cardiomyocytes, one targeted to the lateral membrane through association with syntrophin and the other to the ID through SAP97 (54). Recently, a patient with BrS was reported to have a missense substitution that altered the last three amino acids of the COOH terminal (V2016M), highlighting the clinical relevance of the SIV motif in NaV1.5 channels (70). However, in the same study, an unexpected finding was that cardiac-specific deletion of the PDZ SIV motif in mice reduced NaV1.5 expression at the lateral cardiomyocyte membrane but not the ID (70). Two possible alternatives have been put forth to explain these surprising results: either SIV-dependent regulation of NaV1.5 expression is not essential to the ID region or NaV1.5 localization within this region is so crucial that compensatory mechanisms exist to protect NaV1.5 expression and function (70). Another possible scenario is that NaV1.5 channels present other interacting motifs that are still undetermined.
Kir2.x channels also interact with syntrophin through their respective PDZ-binding motifs (39). However, whether NaV1.5 and Kir2.1 form a “channelosome” with syntrophin and whether they are an integral part of the dystrophin proteins complex currently remain undetermined. Even though in the knock-in ΔSIV NaV1.5 mouse, Kir2.1 expression and current density were unaltered (70), it is important to emphasize that a decrease in the level of Kir2.1 channels was found in the dystrophin-deficient mdx mouse in addition to impaired expression and function of NaV1.5 channels (27). Also, in the mouse model that overexpresses Kir2.1, increase of Kir2.1 expression led to significant increase in SAP97, NaV1.5, and syntrophin (34, 48). Moreover, the opposite results were observed in Kir2.1+/− mutant mice in which significant decreases in relative membrane protein levels of SAP97, NaV1.5, and syntrophin were reported in addition to the expected decreased levels of Kir2.1 (34, 48). These results suggest that the dystrophin protein complex might participate in the reciprocal regulation of NaV1.5 and Kir2.1 channels. Additional experiments are warranted to further pinpoint the mechanisms of such participation.
On the other hand, while there is increasing evidence that suggests NaV1.5 and Kir2.1 interact from early targeting and anterograde trafficking steps, this is still not completely understood. Elucidating the role of NaV1.5-Kir2.1 macromolecular complexes in channel function will require knowledge of whether the two channel proteins use common retrograde trafficking pathways, since the balance between anterograde and retrograde trafficking determines steady-state, cell-surface expression of channel proteins. Recent data suggest that by interacting with dynamin-2, which is thought to play a role in retrograde vesicular formation, NaV1.5 and Kir2.1 might share a common mechanism for retrograde trafficking (Fig. 1) (67). However, several other clathrin-dependent or clathrin-independent mechanisms of endocytosis (6) might also be involved. Evidently, further studies are warranted on this exciting area of research. Taken together, the above studies underscore the complex organization that underlies Kir2.1 and NaV1.5 channel function and the different scaffolding proteins with which both channels interact.
Clinical Correlations
The results discussed in the previous sections provide direct experimental evidence that Kir2.1 and NaV1.5 channels share common partner proteins that are important in trafficking and membrane targeting of both channels. The pathophysiological implications of the (im)balance between IK1 and INa are of particular relevance in the context of inherited or acquired arrhythmogenic syndromes in which Kir2.1 and NaV1.5 sarcolemmal protein functional density is modified. Such is the case of ATS and BrS, since both inherited syndromes have been associated with traffic-deficient mutations in Kir2.1 and NaV1.5, respectively.
ATS mutations are widespread along the Kir2.1 protein, and the identified mutated residues may abolish function, affect assembly, and/or disrupt channel trafficking (9, 22, 23, 55, 73). Given the fact that Kir2.1 and NaV1.5 channels share common partner proteins that control trafficking, it is reasonable to surmise that trafficking-deficient mutations in Kir2.1 that give rise to ATS will reduce NaV1.5 expression and that this should contribute to exacerbate the arrhythmogenic phenotype by decreasing INa and cellular excitability and by slowing cardiac conduction. Conversely, given how BrS is associated with reduced INa, it is reasonable to speculate that decreased NaV1.5 cell-surface expression is linked to reduced Kir2.1 and thus IK1. This would depolarize the cell membrane, decrease INa through partial NaV1.5 voltage deactivation, and further impair conduction velocity and increase arrhythmia incidence.
Overall, the molecular interplay between NaV1.5 and Kir2.1 channels with other proteins emerges as a complex and dynamic process in which the channels share common partners and subdomains in the cardiac cell. Additionally, it is likely that the macromolecular interplay among multiple such partners changes dynamically through time and space within each individual cell. Future work should focus on further understanding the role of macromolecular complexes in arrhythmogenic conditions due to alterations that involve not only the defective/altered channels but also proteins that interact with them as part of macromolecular assemblies. In the same context, one may speculate that mutations in undiscovered scaffolding and/or adaptor proteins which interact with cardiac ion channels through macromolecular interplay could also be involved in the pathophysiology of idiopathic arrhythmias. Therefore, unveiling the mechanistic underpinnings of such macromolecular interactions should increase our understanding of inherited and acquired arrhythmogenic diseases and may increase our ability to prevent sudden and premature cardiac death.
GRANTS
This work was supported in part by the National Heart, Lung, and Blood Institute Grant HL122352 and grants from Transatlantic Networks of Excellence Program from the Leducq Foundation, the University of Michigan Health Science Center and University of Peking Health Science Center Joint Institute for Translational and Clinical Research, and the Centro Nacional de Investigaciones Cardiovasculares (Madrid, Spain). B. C. Willis and D. Ponce-Balbuena were supported with American Heart Association Postdoctoral Fellowships 12POST12030292 and 14POST17820005, respectively.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
B.C.W., D.P.-B., and J.J. prepared figures; B.C.W., D.P.-B., and J.J. drafted manuscript; B.C.W., D.P.-B., and J.J. edited and revised manuscript; B.C.W., D.P.-B., and J.J. approved final version of manuscript; J.J. conception and design of research.
REFERENCES
- 1.Abriel H. Cardiac sodium channel Na(v)1.5 and interacting proteins: physiology and pathophysiology. J Mol Cell Cardiol 48: 2–11, 2010. [DOI] [PubMed] [Google Scholar]
- 2.Abriel H. Roles and regulation of the cardiac sodium channel Na v 1.5: recent insights from experimental studies. Cardiovasc Res 76: 381–389, 2007. [DOI] [PubMed] [Google Scholar]
- 3.Antzelevitch C, Nesterenko V, Shryock JC, Rajamani S, Song Y, Belardinelli L. The role of late I Na in development of cardiac arrhythmias. Handb Exp Pharmacol 221: 137–168, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asimaki A, Kapoor S, Plovie E, Karin Arndt A, Adams E, Liu Z, James CA, Judge DP, Calkins H, Churko J, Wu JC, MacRae CA, Kleber AG, Saffitz JE. Identification of a new modulator of the intercalated disc in a zebrafish model of arrhythmogenic cardiomyopathy. Sci Transl Med 6: 240ra274, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balijepalli RC, Kamp TJ. Caveolae, ion channels and cardiac arrhythmias. Prog Biophys Mol Biol 98: 149–160, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balse E, Steele DF, Abriel H, Coulombe A, Fedida D, Hatem SN. Dynamic of ion channel expression at the plasma membrane of cardiomyocytes. Physiol Rev 92: 1317–1358, 2012. [DOI] [PubMed] [Google Scholar]
- 7.Baroudi G, Acharfi S, Larouche C, Chahine M. Expression and intracellular localization of an SCN5A double mutant R1232W/T1620M implicated in Brugada syndrome. Circ Res 90: E11–E16, 2002. [PubMed] [Google Scholar]
- 8.Baroudi G, Pouliot V, Denjoy I, Guicheney P, Shrier A, Chahine M. Novel mechanism for Brugada syndrome: defective surface localization of an SCN5A mutant (R1432G). Circ Res 88: E78–E83, 2001. [DOI] [PubMed] [Google Scholar]
- 9.Bendahhou S, Donaldson MR, Plaster NM, Tristani-Firouzi M, Fu YH, Ptacek LJ. Defective potassium channel Kir2.1 trafficking underlies Andersen-Tawil syndrome. J Biol Chem 278: 51779–51785, 2003. [DOI] [PubMed] [Google Scholar]
- 10.Bers DM. Cardiac excitation-contraction coupling. Nature 415: 198–205, 2002. [DOI] [PubMed] [Google Scholar]
- 11.Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 20: 1391–1396, 1992. [DOI] [PubMed] [Google Scholar]
- 12.Catterall WA. The molecular basis of neuronal excitability. Science 223: 653–661, 1984. [DOI] [PubMed] [Google Scholar]
- 13.Catterall WA. Molecular properties of voltage-sensitive sodium channels. Annu Rev Biochem 55: 953–985, 1986. [DOI] [PubMed] [Google Scholar]
- 14.Cerrone M, Lin X, Zhang M, Agullo-Pascual E, Pfenniger A, Chkourko Gusky H, Novelli V, Kim C, Tirasawadichai T, Judge DP, Rothenberg E, Chen HS, Napolitano C, Priori SG, Delmar M. Missense mutations in plakophilin-2 cause sodium current deficit and associate with a Brugada syndrome phenotype. Circulation 129: 1092–1103, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cerrone M, Noorman M, Lin X, Chkourko H, Liang FX, van der Nagel R, Hund T, Birchmeier W, Mohler P, van Veen TA, van Rijen HV, Delmar M. Sodium current deficit and arrhythmogenesis in a murine model of plakophilin-2 haploinsufficiency. Cardiovasc Res 95: 460–468, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Q, Kirsch GE, Zhang D, Brugada R, Brugada J, Brugada P, Potenza D, Moya A, Borggrefe M, Breithardt G, Ortiz-Lopez R, Wang Z, Antzelevitch C, O'Brien RE, Schulze-Bahr E, Keating MT, Towbin JA, Wang Q. Genetic basis and molecular mechanism for idiopathic ventricular fibrillation. Nature 392: 293–296, 1998. [DOI] [PubMed] [Google Scholar]
- 17.Clatot J, Ziyadeh-Isleem A, Maugenre S, Denjoy I, Liu H, Dilanian G, Hatem SN, Deschenes I, Coulombe A, Guicheney P, Neyroud N. Dominant-negative effect of SCN5A N-terminal mutations through the interaction of Na(v)1.5 alpha-subunits. Cardiovasc Res 96: 53–63, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen AW, Hnasko R, Schubert W, Lisanti MP. Role of caveolae and caveolins in health and disease. Physiol Rev 84: 1341–1379, 2004. [DOI] [PubMed] [Google Scholar]
- 19.Cronk LB, Ye B, Kaku T, Tester DJ, Vatta M, Makielski JC, Ackerman MJ. Novel mechanism for sudden infant death syndrome: persistent late sodium current secondary to mutations in caveolin-3. Heart Rhythm 4: 161–166, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cunha SR, Mohler PJ. Cardiac ankyrins: Essential components for development and maintenance of excitable membrane domains in heart. Cardiovasc Res 71: 22–29, 2006. [DOI] [PubMed] [Google Scholar]
- 21.Dhamoon AS, Pandit SV, Sarmast F, Parisian KR, Guha P, Li Y, Bagwe S, Taffet SM, Anumonwo JM. Unique Kir2.x properties determine regional and species differences in the cardiac inward rectifier K+ current. Circ Res 94: 1332–1339, 2004. [DOI] [PubMed] [Google Scholar]
- 22.Donaldson MR, Jensen JL, Tristani-Firouzi M, Tawil R, Bendahhou S, Suarez WA, Cobo AM, Poza JJ, Behr E, Wagstaff J, Szepetowski P, Pereira S, Mozaffar T, Escolar DM, Fu YH, Ptacek LJ. PIP2 binding residues of Kir2.1 are common targets of mutations causing Andersen syndrome. Neurology 60: 1811–1816, 2003. [DOI] [PubMed] [Google Scholar]
- 23.Donaldson MR, Yoon G, Fu YH, Ptacek LJ. Andersen-Tawil syndrome: a model of clinical variability, pleiotropy, and genetic heterogeneity. Ann Med 36, Suppl 1: 92–97, 2004. [DOI] [PubMed] [Google Scholar]
- 24.Ehmsen J, Poon E, Davies K. The dystrophin-associated protein complex. J Cell Sci 115: 2801–2803, 2002. [DOI] [PubMed] [Google Scholar]
- 25.El-Haou S, Balse E, Neyroud N, Dilanian G, Gavillet B, Abriel H, Coulombe A, Jeromin A, Hatem SN. Kv4 potassium channels form a tripartite complex with the anchoring protein SAP97 and CaMKII in cardiac myocytes. Circ Res 104: 758–769, 2009. [DOI] [PubMed] [Google Scholar]
- 26.Ellgaard L, Helenius A. Quality control in the endoplasmic reticulum. Nat Rev Mol Cell Biol 4: 181–191, 2003. [DOI] [PubMed] [Google Scholar]
- 27.Gavillet B, Rougier JS, Domenighetti AA, Behar R, Boixel C, Ruchat P, Lehr HA, Pedrazzini T, Abriel H. Cardiac sodium channel Nav1.5 is regulated by a multiprotein complex composed of syntrophins and dystrophin. Circ Res 99: 407–414, 2006. [DOI] [PubMed] [Google Scholar]
- 28.Gerull B, Heuser A, Wichter T, Paul M, Basson CT, McDermott DA, Lerman BB, Markowitz SM, Ellinor PT, MacRae CA, Peters S, Grossmann KS, Drenckhahn J, Michely B, Sasse-Klaassen S, Birchmeier W, Dietz R, Breithardt G, Schulze-Bahr E, Thierfelder L. Mutations in the desmosomal protein plakophilin-2 are common in arrhythmogenic right ventricular cardiomyopathy. Nat Genet 36: 1162–1164, 2004. [DOI] [PubMed] [Google Scholar]
- 29.Gillet L, Rougier JS, Shy D, Sonntag S, Mougenot N, Essers M, Shmerling D, Balse E, Hatem SN, Abriel H. Cardiac-specific ablation of synapse-associated protein SAP97 in mice decreases potassium currents but not sodium current. Heart Rhythm 12: 181–192, 2015. [DOI] [PubMed] [Google Scholar]
- 30.Godreau D, Vranckx R, Maguy A, Rucker-Martin C, Goyenvalle C, Abdelshafy S, Tessier S, Couetil JP, Hatem SN. Expression, regulation and role of the MAGUK protein SAP-97 in human atrial myocardium. Cardiovasc Res 56: 433–442, 2002. [DOI] [PubMed] [Google Scholar]
- 31.Goldin AL, Barchi RL, Caldwell JH, Hofmann F, Howe JR, Hunter JC, Kallen RG, Mandel G, Meisler MH, Netter YB, Noda M, Tamkun MM, Waxman SG, Wood JN, Catterall WA. Nomenclature of voltage-gated sodium channels. Neuron 28: 365–368, 2000. [DOI] [PubMed] [Google Scholar]
- 32.Hennessey JA, Marcou CA, Wang C, Wei EQ, Tester DJ, Torchio M, Dagradi F, Crotti L, Schwartz PJ, Ackerman MJ, Pitt GS. FGF12 is a candidate Brugada syndrome locus. Heart Rhythm 10: 1886–1894, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hund TJ, Koval OM, Li J, Wright PJ, Qian L, Snyder JS, Gudmundsson H, Kline CF, Davidson NP, Cardona N, Rasband MN, Anderson ME, Mohler PJ. A beta(IV)-spectrin/CaMKII signaling complex is essential for membrane excitability in mice. J Clin Invest 120: 3508–3519, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jalife J, Milstein ML. Reciprocity of cardiac sodium and potassium channels in the control of excitability and arrhythmias. In: Cardiac Electrophysiology: From Cell to Bedside, edited by Zipes DP and Jalife J. Philadelphia, PA: Elsevier, 2014. [Google Scholar]
- 35.Kattygnarath D, Maugenre S, Neyroud N, Balse E, Ichai C, Denjoy I, Dilanian G, Martins RP, Fressart V, Berthet M, Schott JJ, Leenhardt A, Probst V, Le Marec H, Hainque B, Coulombe A, Hatem SN, Guicheney P. MOG1: a new susceptibility gene for Brugada syndrome. Circ Cardiovasc Genet 4: 261–268, 2011. [DOI] [PubMed] [Google Scholar]
- 36.Kim E, Niethammer M, Rothschild A, Jan YN, Sheng M. Clustering of Shaker-type K+ channels by interaction with a family of membrane-associated guanylate kinases. Nature 378: 85–88, 1995. [DOI] [PubMed] [Google Scholar]
- 37.Kubo Y, Adelman JP, Clapham DE, Jan LY, Karschin A, Kurachi Y, Lazdunski M, Nichols CG, Seino S, Vandenberg CA. International Union of Pharmacology. LIV. Nomenclature and molecular relationships of inwardly rectifying potassium channels. Pharmacol Rev 57: 509–526, 2005. [DOI] [PubMed] [Google Scholar]
- 38.Lemaillet G, Walker B, Lambert S. Identification of a conserved ankyrin-binding motif in the family of sodium channel alpha subunits. J Biol Chem 278: 27333–27339, 2003. [DOI] [PubMed] [Google Scholar]
- 39.Leonoudakis D, Conti LR, Anderson S, Radeke CM, McGuire LM, Adams ME, Froehner SC, Yates JR 3rd, Vandenberg CA. Protein trafficking and anchoring complexes revealed by proteomic analysis of inward rectifier potassium channel (Kir2.x)-associated proteins. J Biol Chem 279: 22331–22346, 2004. [DOI] [PubMed] [Google Scholar]
- 40.Leonoudakis D, Conti LR, Radeke CM, McGuire LM, Vandenberg CA. A multiprotein trafficking complex composed of SAP97, CASK, Veli, and Mint1 is associated with inward rectifier Kir2 potassium channels. J Biol Chem 279: 19051–19063, 2004. [DOI] [PubMed] [Google Scholar]
- 41.Leonoudakis D, Mailliard W, Wingerd K, Clegg D, Vandenberg C. Inward rectifier potassium channel Kir2.2 is associated with synapse-associated protein SAP97. J Cell Sci 114: 987–998, 2001. [DOI] [PubMed] [Google Scholar]
- 42.Liu CJ, Dib-Hajj SD, Renganathan M, Cummins TR, Waxman SG. Modulation of the cardiac sodium channel Nav1.5 by fibroblast growth factor homologous factor 1B. J Biol Chem 278: 1029–1036, 2003. [DOI] [PubMed] [Google Scholar]
- 43.London B, Michalec M, Mehdi H, Zhu X, Kerchner L, Sanyal S, Viswanathan PC, Pfahnl AE, Shang LL, Madhusudanan M, Baty CJ, Lagana S, Aleong R, Gutmann R, Ackerman MJ, McNamara DM, Weiss R, Dudley SC Jr. Mutation in glycerol-3-phosphate dehydrogenase 1 like gene (GPD1-L) decreases cardiac Na+ current and causes inherited arrhythmias. Circulation 116: 2260–2268, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lowe JS, Palygin O, Bhasin N, Hund TJ, Boyden PA, Shibata E, Anderson ME, Mohler PJ. Voltage-gated Nav channel targeting in the heart requires an ankyrin-G dependent cellular pathway. J Cell Biol 180: 173–186, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma D, Taneja TK, Hagen BM, Kim BY, Ortega B, Lederer WJ, Welling PA. Golgi export of the Kir2.1 channel is driven by a trafficking signal located within its tertiary structure. Cell 145: 1102–1115, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Makara MA, Curran J, Little SC, Musa H, Polina I, Smith SA, Wright PJ, Unudurthi SD, Snyder J, Bennett V, Hund TJ, Mohler PJ. Ankyrin-G coordinates intercalated disc signaling platform to regulate cardiac excitability in vivo. Circ Res 115: 929–938, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Melnyk P, Zhang L, Shrier A, Nattel S. Differential distribution of Kir2.1 and Kir23 subunits in canine atrium and ventricle. Am J Physiol Heart Circ Physiol 283: H1123–H1133, 2002. [DOI] [PubMed] [Google Scholar]
- 48.Milstein ML, Musa H, Balbuena DP, Anumonwo JM, Auerbach DS, Furspan PB, Hou L, Hu B, Schumacher SM, Vaidyanathan R, Martens JR, Jalife J. Dynamic reciprocity of sodium and potassium channel expression in a macromolecular complex controls cardiac excitability and arrhythmia. Proc Natl Acad Sci USA 109: E2134–E2143, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mohler PJ, Le Scouarnec S, Denjoy I, Lowe JS, Guicheney P, Caron L, Driskell IM, Schott JJ, Norris K, Leenhardt A, Kim RB, Escande D, Roden DM. Defining the cellular phenotype of “ankyrin-B syndrome” variants: human ANK2 variants associated with clinical phenotypes display a spectrum of activities in cardiomyocytes. Circulation 115: 432–441, 2007. [DOI] [PubMed] [Google Scholar]
- 50.Mohler PJ, Rivolta I, Napolitano C, LeMaillet G, Lambert S, Priori SG, Bennett V. Nav1.5 E1053K mutation causing Brugada syndrome blocks binding to ankyrin-G and expression of Nav1.5 on the surface of cardiomyocytes. Proc Natl Acad Sci USA 101: 17533–17538, 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mohler PJ, Schott JJ, Gramolini AO, Dilly KW, Guatimosim S, duBell WH, Song LS, Haurogne K, Kyndt F, Ali ME, Rogers TB, Lederer WJ, Escande D, Le Marec H, Bennett V. Ankyrin-B mutation causes type 4 long-QT cardiac arrhythmia and sudden cardiac death. Nature 421: 634–639, 2003. [DOI] [PubMed] [Google Scholar]
- 52.Motoike HK, Liu H, Glaaser IW, Yang AS, Tateyama M, Kass RS. The Na+ channel inactivation gate is a molecular complex: a novel role of the COOH-terminal domain. J Gen Physiol 123: 155–165, 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nichols CG, Makhina EN, Pearson WL, Sha Q, Lopatin AN. Inward rectification and implications for cardiac excitability. Circ Res 78: 1–7, 1996. [DOI] [PubMed] [Google Scholar]
- 54.Petitprez S, Zmoos AF, Ogrodnik J, Balse E, Raad N, El-Haou S, Albesa M, Bittihn P, Luther S, Lehnart SE, Hatem SN, Coulombe A, Abriel H. SAP97 and dystrophin macromolecular complexes determine two pools of cardiac sodium channels Nav1.5 in cardiomyocytes. Circ Res 108: 294–304, 2011. [DOI] [PubMed] [Google Scholar]
- 55.Plaster NM, Tawil R, Tristani-Firouzi M, Canun S, Bendahhou S, Tsunoda A, Donaldson MR, Iannaccone ST, Brunt E, Barohn R, Clark J, Deymeer F, George AL Jr, Fish FA, Hahn A, Nitu A, Ozdemir C, Serdaroglu P, Subramony SH, Wolfe G, Fu YH, Ptacek LJ. Mutations in Kir21 cause the developmental and episodic electrical phenotypes of Andersen's syndrome. Cell 105: 511–519, 2001. [DOI] [PubMed] [Google Scholar]
- 56.Priori SG, Pandit SV, Rivolta I, Berenfeld O, Ronchetti E, Dhamoon A, Napolitano C, Anumonwo J, di Barletta MR, Gudapakkam S, Bosi G, Stramba-Badiale M, Jalife J. A novel form of short QT syndrome (SQT3) is caused by a mutation in the KCNJ2 gene. Circ Res 96: 800–807, 2005. [DOI] [PubMed] [Google Scholar]
- 57.Rafizadeh S, Zhang Z, Woltz RL, Kim HJ, Myers RE, Lu L, Tuteja D, Singapuri A, Bigdeli AA, Harchache SB, Knowlton AA, Yarov-Yarovoy V, Yamoah EN, Chiamvimonvat N. Functional interaction with filamin A and intracellular Ca2+ enhance the surface membrane expression of a small-conductance Ca2+-activated K+ (SK2) channel. Proc Natl Acad Sci USA 111: 9989–9994, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rivolta I, Abriel H, Tateyama M, Liu H, Memmi M, Vardas P, Napolitano C, Priori SG, Kass RS. Inherited Brugada and long QT-3 syndrome mutations of a single residue of the cardiac sodium channel confer distinct channel and clinical phenotypes. J Biol Chem 276: 30623–30630, 2001. [DOI] [PubMed] [Google Scholar]
- 59.Rizzo S, Lodder EM, Verkerk AO, Wolswinkel R, Beekman L, Pilichou K, Basso C, Remme CA, Thiene G, Bezzina CR. Intercalated disc abnormalities, reduced Na+ current density, and conduction slowing in desmoglein-2 mutant mice prior to cardiomyopathic changes. Cardiovasc Res 95: 409–418, 2012. [DOI] [PubMed] [Google Scholar]
- 60.Roden DM, Balser JR, George AL Jr, Anderson ME. Cardiac ion channels. Annu Rev Physiol 64: 431–475, 2002. [DOI] [PubMed] [Google Scholar]
- 61.Rogart RB, Cribbs LL, Muglia LK, Kephart DD, Kaiser MW. Molecular cloning of a putative tetrodotoxin-resistant rat heart Na+ channel isoform. Proc Natl Acad Sci USA 86: 8170–8174, 1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rusconi R, Scalmani P, Cassulini RR, Giunti G, Gambardella A, Franceschetti S, Annesi G, Wanke E, Mantegazza M. Modulatory proteins can rescue a trafficking defective epileptogenic Nav1.1 Na+ channel mutant. J Neurosci 27: 11037–11046, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sampson LJ, Leyland ML, Dart C. Direct interaction between the actin-binding protein filamin-A and the inwardly rectifying potassium channel, Kir2.1. J Biol Chem 278: 41988–41997, 2003. [DOI] [PubMed] [Google Scholar]
- 64.Sato PY, Coombs W, Lin X, Nekrasova O, Green KJ, Isom LL, Taffet SM, Delmar M. Interactions between ankyrin-G, Plakophilin-2, and Connexin43 at the cardiac intercalated disc. Circ Res 109: 193–201, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sato PY, Musa H, Coombs W, Guerrero-Serna G, Patino GA, Taffet SM, Isom LL, Delmar M. Loss of plakophilin-2 expression leads to decreased sodium current and slower conduction velocity in cultured cardiac myocytes. Circ Res 105: 523–526, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schulze-Bahr E, Eckardt L, Breithardt G, Seidl K, Wichter T, Wolpert C, Borggrefe M, Haverkamp W. Sodium channel gene (SCN5A) mutations in 44 index patients with Brugada syndrome: different incidences in familial and sporadic disease. Hum Mutat 21: 651–652, 2003. [DOI] [PubMed] [Google Scholar]
- 67.Shi D, Xie D, Zhang H, Zhao H, Huang J, Li C, Liu Y, Lv F, The E, Yuan T, Wang S, Chen J, Pan L, Yu Z, Liang D, Zhu W, Zhang Y, Li L, Peng L, Li J, Chen YH. Reduction in dynamin-2 is implicated in ischaemic cardiac arrhythmias. J Cell Mol Med 18: 1992–1999, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shibata EF, Brown TL, Washburn ZW, Bai J, Revak TJ, Butters CA. Autonomic regulation of voltage-gated cardiac ion channels. J Cardiovasc Electrophysiol 17, Suppl 1: S34–S42, 2006. [DOI] [PubMed] [Google Scholar]
- 69.Shimoni Y, Clark RB, Giles WR. Role of an inwardly rectifying potassium current in rabbit ventricular action potential. J Physiol 448: 709–727, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shy D, Gillet L, Ogrodnik J, Albesa M, Verkerk AO, Wolswinkel R, Rougier JS, Barc J, Essers MC, Syam N, Marsman RF, van Mil AM, Rotman S, Redon R, Bezzina CR, Remme CA, Abriel H. PDZ domain-binding motif regulates cardiomyocyte compartment-specific NaV1.5 channel expression and function. Circulation 130: 147–160, 2014. [DOI] [PubMed] [Google Scholar]
- 71.Smits JP, Eckardt L, Probst V, Bezzina CR, Schott JJ, Remme CA, Haverkamp W, Breithardt G, Escande D, Schulze-Bahr E, LeMarec H, Wilde AA. Genotype-phenotype relationship in Brugada syndrome: electrocardiographic features differentiate SCN5A-related patients from non-SCN5A-related patients. J Am Coll Cardiol 40: 350–356, 2002. [DOI] [PubMed] [Google Scholar]
- 72.Tan BH, Pundi KN, Van Norstrand DW, Valdivia CR, Tester DJ, Medeiros-Domingo A, Makielski JC, Ackerman MJ. Sudden infant death syndrome-associated mutations in the sodium channel beta subunits. Heart Rhythm 7: 771–778, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tristani-Firouzi M, Jensen JL, Donaldson MR, Sansone V, Meola G, Hahn A, Bendahhou S, Kwiecinski H, Fidzianska A, Plaster N, Fu YH, Ptacek LJ, Tawil R. Functional and clinical characterization of KCNJ2 mutations associated with LQT7 (Andersen syndrome). J Clin Invest 110: 381–388, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ueda K, Valdivia C, Medeiros-Domingo A, Tester DJ, Vatta M, Farrugia G, Ackerman MJ, Makielski JC. Syntrophin mutation associated with long QT syndrome through activation of the nNOS-SCN5A macromolecular complex. Proc Natl Acad Sci USA 105: 9355–9360, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vaidyanathan R, Taffet SM, Vikstrom KL, Anumonwo JM. Regulation of cardiac inward rectifier potassium current (IK1) by synapse-associated protein-97. J Biol Chem 285: 28000–28009, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vaidyanathan R, Vega AL, Song C, Zhou Q, Tan BH, Berger S, Makielski JC, Eckhardt LL. The interaction of caveolin 3 protein with the potassium inward rectifier channel Kir2.1: physiology and pathology related to long qt syndrome 9 (LQT9). J Biol Chem 288: 17472–17480, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Valdivia CR, Tester DJ, Rok BA, Porter CB, Munger TM, Jahangir A, Makielski JC, Ackerman MJ. A trafficking defective, Brugada syndrome-causing SCN5A mutation rescued by drugs. Cardiovasc Res 62: 53–62, 2004. [DOI] [PubMed] [Google Scholar]
- 78.Valdivia CR, Ueda K, Ackerman MJ, Makielski JC. GPD1L links redox state to cardiac excitability by PKC-dependent phosphorylation of the sodium channel SCN5A. Am J Physiol Heart Circ Physiol 297: H1446–H1452, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Van Norstrand DW, Valdivia CR, Tester DJ, Ueda K, London B, Makielski JC, Ackerman MJ. Molecular and functional characterization of novel glycerol-3-phosphate dehydrogenase 1 like gene (GPD1-L) mutations in sudden infant death syndrome. Circulation 116: 2253–2259, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vaquero M, Calvo D, Jalife J. Cardiac fibrillation: from ion channels to rotors in the human heart. Heart Rhythm 5: 872–879, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vatta M, Ackerman MJ, Ye B, Makielski JC, Ughanze EE, Taylor EW, Tester DJ, Balijepalli RC, Foell JD, Li Z, Kamp TJ, Towbin JA. Mutant caveolin-3 induces persistent late sodium current and is associated with long-QT syndrome. Circulation 114: 2104–2112, 2006. [DOI] [PubMed] [Google Scholar]
- 82.Vikstrom KL, Vaidyanathan R, Levinsohn S, O'Connell RP, Qian Y, Crye M, Mills JH, Anumonwo JM. SAP97 regulates Kir2.3 channels by multiple mechanisms. Am J Physiol Heart Circ Physiol 297: H1387–H1397, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang C, Hennessey JA, Kirkton RD, Graham V, Puranam RS, Rosenberg PB, Bursac N, Pitt GS. Fibroblast growth factor homologous factor 13 regulates Na+ channels and conduction velocity in murine hearts. Circ Res 109: 775–782, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang Q, Shen J, Splawski I, Atkinson D, Li Z, Robinson JL, Moss AJ, Towbin JA, Keating MT. SCN5A mutations associated with an inherited cardiac arrhythmia, long QT syndrome. Cell 80: 805–811, 1995. [DOI] [PubMed] [Google Scholar]
- 85.Wang Z, Yue L, White M, Pelletier G, Nattel S. Differential distribution of inward rectifier potassium channel transcripts in human atrium versus ventricle. Circulation 98: 2422–2428, 1998. [DOI] [PubMed] [Google Scholar]
- 86.Wu G, Ai T, Kim JJ, Mohapatra B, Xi Y, Li Z, Abbasi S, Purevjav E, Samani K, Ackerman MJ, Qi M, Moss AJ, Shimizu W, Towbin JA, Cheng J, Vatta M. alpha-1-syntrophin mutation and the long-QT syndrome: a disease of sodium channel disruption. Circ Arrhythm Electrophysiol 1: 193–201, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wu L, Yong SL, Fan C, Ni Y, Yoo S, Zhang T, Zhang X, Obejero-Paz CA, Rho HJ, Ke T, Szafranski P, Jones SW, Chen Q, Wang QK. Identification of a new co-factor, MOG1, required for the full function of cardiac sodium channel Nav 1.5. J Biol Chem 283: 6968–6978, 2008. [DOI] [PubMed] [Google Scholar]
- 88.Yarbrough TL, Lu T, Lee HC, Shibata EF. Localization of cardiac sodium channels in caveolin-rich membrane domains: regulation of sodium current amplitude. Circ Res 90: 443–449, 2002. [DOI] [PubMed] [Google Scholar]
- 89.Zhou AX, Hartwig JH, Akyurek LM. Filamins in cell signaling, transcription and organ development. Trends Cell Biol 20: 113–123, 2010. [DOI] [PubMed] [Google Scholar]
- 90.Zhou X, Boren J, Akyurek LM. Filamins in cardiovascular development. Trends Cardiovasc Med 17: 222–229, 2007. [DOI] [PubMed] [Google Scholar]