Abstract
Purpose
Oropharyngeal carcinoma (OPC) positive for human papillomavirus type 16 (HPV16) has a significantly better prognosis than OPC unrelated to HPV. Within HPV16-positive OPC, biomarkers of prognosis are urgently needed to individualize care. We hypothesized that serum antibodies specific to HPV16, the major HPV type causing OPC, have biological relevance and are potential biomarkers for improved prognosis among patients with HPV16-positive OPC.
Methods
IgG antibodies to the HPV16 antigens E1, E4-E7, L1, L2, and the N-terminal and C-terminal fragments of E2 (NE2, CE2) were quantified using a custom programmable enzyme-linked immunosorbent assay. Sera were obtained at diagnosis from 209 OPC patients (96 HPV16-positive). The ratios of median fluorescent intensity (MFI) for each antigen to MFI for control GST protein were determined. Kaplan-Meier survival curves and Cox proportional hazards regression were used to determine survival differences between groups. ROC curves were used to determine the best combination of E antibodies to predict disease recurrence.
Results
E1, NE2, and E6 antibody positivity were all strongly associated with improved overall and progression-free survival in the entire cohort and in patients with known HPV16-positive tumors (P<.05). For both overall and progression-free survival among HPV-positive patients, hazard ratios were 0.2 for NE2, 0.3 for E1, and 0.3 for E6 antibody positivity.
Conclusion
We identified 3 HPV16-specific antibodies that are associated with improved overall and progression-free survival in patients with HPV-related OPC. These results suggest that differential serologic responses in patients may reflect differential biological processes within the host and tumor and may have prognostic value.
INTRODUCTION
The incidence of HPV-positive oropharyngeal squamous cell carcinoma (OPC) is expected to increase substantially over the next several decades due to the lack of a screening paradigm and despite the availability of a prophylactic vaccine (1). Serum antibodies to HPV proteins, in particular the early (E) proteins E6 and E7, have been detected in several HPV-related cancers and have been found to be reliable indicators of an HPV-positive tumor, including oropharyngeal tumors (2–11). Although patients with HPV-positive OPC are typically diagnosed with late-stage disease, numerous case-control and prospective studies have shown that patients with HPV-positive tumors have better response to treatment and better survival than patients with HPV-negative tumors (12–17). Furthermore, Kreimer et al recently reported a 68% reduced risk of death among patients with OPC who were positive for E6 antibodies versus those who were negative for E6 antibodies after adjustment for smoking (10).
To investigate whether there are differential immune responses to HPV16 proteins with biological and prognostic relevance, we used a novel protein array to investigate the association between serum antibodies to the entire HPV16 proteome and overall and progression-free survival among patients with OPC treated at our institution.
Methods
Study participants
Patients with newly diagnosed, histopathologically confirmed, and previously untreated OPC who presented to The University of Texas MD Anderson Cancer Center and participated in a large prospective epidemiological study of head and neck cancer between January 2006 and September 2008 were invited to participate in this separate protocol (presented herein) of serial monitoring of serum markers of disease prognosis. All patients gave written informed consent and provided demographic and exposure data as well as a blood sample for biological testing. Samples were collected at initial workup, six weeks following the end of treatment, and at 6-month intervals up to 36 months for a total possible number of 8 samples. Samples were collected using a standardized protocol and stored at −80°C until use. The study was approved by the MD Anderson Institutional Review Board.
Laboratory methods
Determination of tumor HPV16 DNA status
Diagnostic in-house paraffin-embedded tumor tissue was obtained following histopathologic confirmation of the diagnosis. A tissue DNA extraction kit (Qiagen Inc., Valencia, CA) was used to extract DNA, and a PCR-based type-specific assay was used to test tumor tissue for the presence of HPV16 E6 or E7 regions. β-actin served as the DNA quality control and positive and negative controls were included in each run. Samples were run in triplicate with 100% concordance between samples.
Magnetic programmable bead ELISA
Bead array ELISAs were performed at Arizona State University essentially as described (11, 18, 19), with the following modifications (20). The in vitro translation products were captured on magnetic microspheres (BioRad, Hercules, CA), pooled, and blocked with HeteroBlock (Omega Biologicals, Bozeman, MT) diluted to 2 µg/mL into SeaBlock (Thermo Scientific, Rockford, IL). Sera were diluted 1:80 and incubated with the pooled beads and bound IgG was detected using median fluorescent intensity (MFI).. To control for nonspecific and GST-specific antibodies, the ratio of MFI for individual HPV16-specific antibodies to MFI for the control GST antigen was measured. To establish cut-off values for seropositivity, an MFI ratio > (the average +3 standard deviations) of 78 healthy control samples was designated positive. The cut-off values were as follows: E1, 1.4; CE2, 2.4; NE2, 1.5; E4, 2.7; E5, 1.5; E6, 1.7; E7, 2.2; L1, 1.4; and L2, 1.4. Control sera were obtained from Oregon Health and Science University (Portland, OR) from subjects participating in a head and neck cancer screening event who had no history or evidence on clinical examination of head and neck cancer (20). The control cohort consisted of 47 females and 31 males with a mean age of 51.4 years (SD, 13.5 years). The intra-assay coefficient of variation was determined to be 1.04–8.34% and the intra-assay coefficient of variation was 1.39–7.06%. The lower limit of detection of the assay varied based on the serum sample tested, but is shown in representative format in Supplemental Figure 1. Laboratory researchers were blinded to clinical outcome.
Statistical analysis
Stata 12.0 (StataCorp, College Station, TX) was used for all statistical analyses. A P value of <.05 was considered significant, and all tests were 2-sided. Standard descriptive statistical methods were used to describe demographic and clinical characteristics.
Overall survival was defined as time from first appointment to death from any cause. Progression-free survival was defined as time from first appointment to clinical detection of recurrent cancer (local, regional, or distant) or death from any cause. Participants alive and recurrence-free (for progression-free survival) at last follow-up or lost to follow-up were considered censored. Kaplan–Meier curves were created to compare survival between groups, and the log-rank statistic was used to test the hypothesis of a difference in survival between groups. Cox proportional hazards models were used to calculate hazard ratios (HRs) and 95% CIs to assess whether presence of specific HPV16 antibodies was associated with overall and progression-free survival. Akaike information criterion was used to select variables for inclusion in the multivariable models. Overall and progression-free survival within each group of patients were assessed separately and the models with minimum AIC were used as the final models. Additionally, smoking is a known predictor for survival and was included in the models. A binary logistic regression model was used to compute the area under the receiver operating characteristic curve (ROC) to compare the performance of all combinations of E antibodies for predicting disease recurrence. The probability cut-off value for the predictions was 0.5.
Results
A total of 209 patients were included in the final analysis. Of these, 114 had tumor HPV16 status available for subgroup analyses; 96 of these patients had HPV16-positive tumors. The median follow-up time for patients who survived was 62.7 months (range, 3.9–96.9 months). The median follow-up time for patients with HPV16-positive tumors who survived was 68.9 months (range, 4.1–92.5 months). There was no difference with respect to survival between patients who had tumor HPV16 status available and those who did not (P=.577).
Demographic and clinical characteristics
The demographic, exposure, and clinical characteristics of the patients are summarized in Table 1. Ninety percent of patients were positive for at least 1 E antibody, while 16% were positive for at least 1 L antibody. Of the 114 patients with tumor HPV16 DNA status available, 96 (84%) had HPV16-positive tumors. The characteristics of the patients by tumor HPV16 status are shown in Table 1.
Table 1.
Demographic, exposure, and clinical characteristics of 209 patients with OPCa
| Characteristic | All Patients (n = 209) |
Tumor HPV statusc (n=114) |
||
|---|---|---|---|---|
| HPV+ Patients (n = 96) |
HPV- Patients (n=18) |
P | ||
| Age, mean (SD), years | 55.8 (9.2) | 54.8 (8.4) | 56.7 (8.1) | |
| Age, median, years | 55 | 54 | 54 | |
| Sex | .429d | |||
| Male | 184 (88.0) | 86 (89.6) | 15 (83.3) | |
| Female | 25 (12.0) | 10 (10.4) | 3 (16.7) | |
| Race | .657d | |||
| White | 192 (91.9) | 88 (91.7) | 16 (88.9) | |
| Other | 17 (8.1) | 8 (8.3) | 2 (11.1) | |
| Smoking | .708d | |||
| Never | 103 (49.3) | 45 (46.9) | 10 (55.6) | |
| Former | 71 (34.0) | 32 (33.3) | 4 (22.2) | |
| Current | 35 (16.8) | 19 (19.8) | 4 (22.2) | |
| Pack-years of smoking | .508 | |||
| ≤10 | 130 (62.5) | 56 (58.3) | 12 (66.7) | |
| >10 | 78 (37.5) | 40 (41.7) | 6 (33.3) | |
| Missing | 1 | 0 | 0 | |
| Alcohol use | .237d | |||
| Never | 60 (28.7) | 23 (24.0) | 5 (27.8) | |
| Former | 52 (24.9) | 29 (30.2) | 2 (11.1) | |
| Current | 97 (46.4) | 44 (45.8) | 11 (61.1) | |
| Subsite | .039d | |||
| Tonsil | 99 (47.4) | 43 (44.8) | 14 (77.8) | |
| Base of tongue | 105 (50.2) | 49 (51.0) | 4 (22.2) | |
| Other oropharynx | 5 (2.4) | 4 (4.2) | 0 | |
| Stage | .095d | |||
| I-II | 17 (8.1) | 8 (8.3) | 4 (22.2) | |
| III-IV | 192 (91.9) | 88 (91.7) | 14 (77.8) | |
| T category | .233d | |||
| 0–2 | 156 (74.6) | 70 (72.9) | 16 (88.9) | |
| 3–4 | 53 (25.4) | 26 (27.1) | 2 (11.1) | |
| N category | .047 | |||
| 0–2a | 57 (27.3) | 30 (31.3) | 10 (55.6) | |
| 2b-3 | 152 (72.7) | 66 (68.8) | 8 (44.4) | |
| Grade | .392 | |||
| Well-moderately differentiated | 61 (33.7) | 31 (36.1) | 8 (47.1) | |
| Moderately-poor to poorly differentiated | 120 (66.3) | 55 (64.0) | 9 (52.9) | |
| Missing | 28 | 10 | 1 | |
| Treatmentb | .525 | |||
| Radiation | 59 (28.2) | 30 (31.3) | 7 (38.9) | |
| Radiation+chemotherapy | 150 (71.8) | 66 (68.8) | 11 (61.1) | |
| HPV antibody status | ||||
| E1+ | 150 (71.8) | 69 (71.9) | 12 (66.7) | .655 |
| NE2+ | 173 (82.8) | 83 (86.5) | 11 (61.1) | .009 |
| CE2+ | 101 (48.3) | 53 (55.2) | 6 (33.3) | .088 |
| E4+ | 46 (22.0) | 20 (20.8) | 4 (22.2) | 1.0d |
| E5+ | 7 (3.4) | 3 (3.1) | 1 (5.6) | .502d |
| E6+ | 161 (77.0) | 76 (79.2) | 8 (44.4) | .002 |
| E7+ | 132 (63.2) | 63 (65.6) | 9 (50.0) | .207 |
| Any E+ | 188 (90.0) | 86 (89.6) | 13 (72.2) | .046 |
| L1+ | 19 (9.1) | 14 (14.6) | 3 (16.7) | .731d |
| L2+ | 23 (11.0) | 14 (14.6) | 1 (5.6) | .459d |
| Any L+ | 33 (15.8) | 20 (20.8) | 4 (22.2) | 1.0d |
Values in table are number of patients (percentage) unless otherwise specified.
Radiation is radiation only and radiation+chemotherapy is radiation plus chemotherapy with or without surgery.
The Radiation group includes 1 patient who had surgery only.
Tumor status determined by PCR.
Fisher’s exact test
Survival according to antibody status
Progression-free survival was better among patients positive for any E antibodies (Figure 1A), but no survival advantage was noted among patients positive for any L antibodies (Figure 1B) (P<.001 and P=.657, respectively). Therefore, we excluded L antibody status in subsequent analyses.
Figure 1.
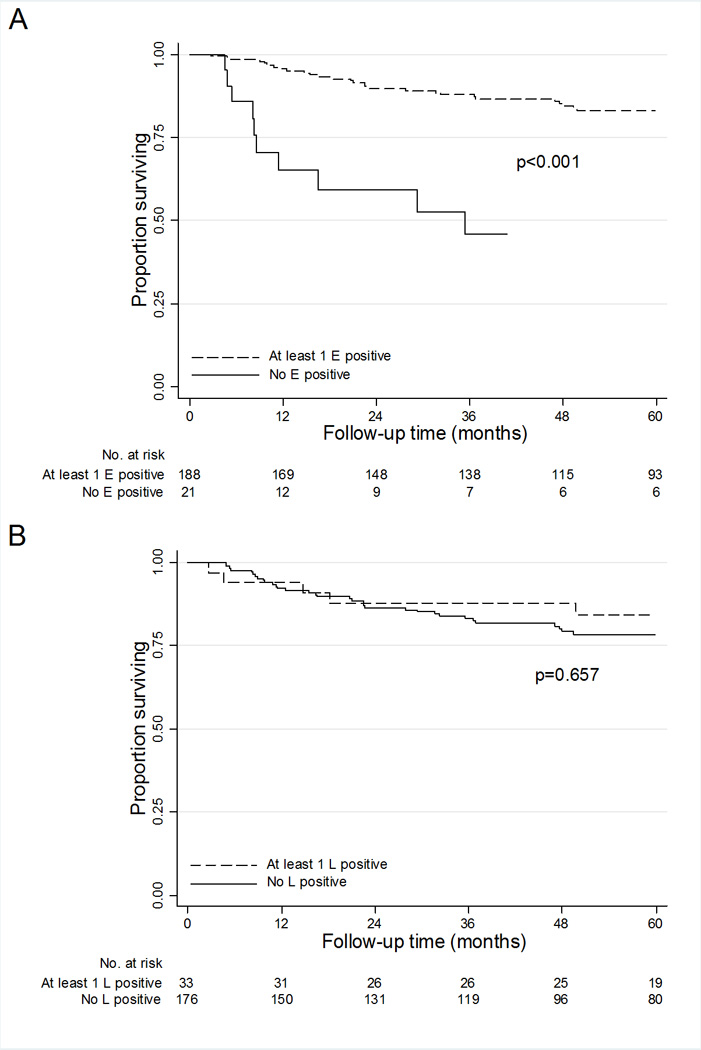
Progression-free survival of 209 patients with OPC. A) Patients positive for at least 1 E antibody versus patients negative for all E antibodies (P<.001). B) Patients positive for at least 1 L antibody versus patients negative for all L antibodies (P=.657).
Patients positive for any E antibodies had better overall and progression-free survival than patients negative for all E antibodies: 5-year overall survival estimates were 87.4% and 42.2%, respectively, and 5-year progression-free survival estimates were 82.9% and 46.1%, respectively (P<.001 for both). In multivariable Cox proportional hazards regression, patients positive for any E antibodies had an 80% lower risk of death (HR, 0.2; 95% CI, 0.1–0.4) and progression (HR, 0.2; 95% CI, 0.1–0.5) (Table 2). NE2 positivity, E1 positivity, and E6 positivity reduced the risk of death by up to 80% and the risk of progression by up to 70% (Table 2). Because smoking is a strong predictor of survival and patients with HPV-positive tumors are more likely to be never-smokers or light smokers, we also evaluated a subset of patients with a smoking history of 10 or fewer pack years. Among these patients (n=130), positivity for any E antibodies was also associated with a significantly reduced risk of death (HR, 0.1; 95% CI, 0–0.7) and progression (HR, 0.1; 95% CI, 0–1.0) (Table 2). In never-smokers and light smokers, we did not observe the strong associations with individual antibodies that we observed for the entire cohort; nevertheless, the trend for improved survival among antibody -positive patients was observed in this subset.
Table 2.
Cox proportional hazards regression for association of pretreatment antibody status with overall and progression-free survival among 209 patients with OPC, 130 patients with ≤10 pack-years of smoking, and 96 patients with tumor HPV-positive OPC.
| All patients N=209 |
Patients with ≤10 pack years N=130 |
Tumor HPV-positive patients N=96 |
||||
|---|---|---|---|---|---|---|
| Crude HR (95% CI) |
Adjusted HR (95% CI) |
Crude HR (95% CI) |
Adjusted HR (95% CI) |
Crude HR (95% CI) |
Adjusted HR (95% CI) |
|
| Overall survivala | ||||||
| E1+ vs. E1 − | 0.3 (0.1–0.5) | 0.3 (0.2–0.5) | 0.5 (0.2–1.3) | 0.5 (0.2–1.4) | 0.2 (0.1–0.6) | 0.3 (0.1–0.7) |
| NE2+ vs. NE2− | 0.2 (0.1–0.3) | 0.2 (0.1–0.4) | 0.3 (0.1–1.2) | 0.5 (0.1–1.8) | 0.1 (0.1–0.3) | 0.2 (0.1–0.6) |
| CE2+ vs. CE2− | 0.4 (0.2–0.8) | 0.5 (0.2–1.0) | 0.8 (0.3–2.1) | 0.8 (0.3–2.1) | 0.5 (0.2–1.4) | 0.6 (0.2–1.6) |
| E4+ vs. E4− | 0.5 (0.2–1.2) | 0.4 (0.2–1.0) | 0.2 (0–1.4) | 0.2 (0–1.6) | 0.2 (0–1.6) | 0.3 (0–2.2) |
| E5+ vs. E5− | NC | NC | NC | NC | NC | NC |
| E6+ vs. E6− | 0.2 (0.1–0.4) | 0.3 (0.2–0.6) | 0.3 (0.1–0.8) | 0.5 (0.2–1.3) | 0.3 (0.1–0.7) | 0.3 (0.1–0.9) |
| E7+ vs. E7− | 0.5 (0.3–1.0) | 0.7 (0.3–1.3) | 1.3 (0.4–3.9) | 1.2 (0.4–3.8) | 0.6 (0.2–1.5) | 0.9 (0.3–2.6) |
| Any E+ vs. all − | 0.2 (0.1–0.3) | 0.2 (0.1–0.4) | 0.1 (0–0.8) | 0.1 (0–0.7) | 0.1 (0.1–0.4) | 0.3 (0.1–0.9) |
| Progression-free survivalb | ||||||
| E1+ vs. E1 − | 0.3 (0.2–0.6) | 0.4 (0.2–0.7) | 0.7 (0.3–1.8) | 0.7 (0.3–1.9) | 0.3 (0.10–0.7) | 0.3 (0.1–0.7) |
| NE2+ vs. NE2− | 0.2 (0.1–0.4) | 0.3 (0.1–0.5) | 0.5 (0.1–1.6) | 0.5 (0.1–1.8) | 0.1 (0.05–0.3) | 0.2 (0.1–0.6) |
| CE2+ vs. CE2− | 0.5 (0.3–0.9) | 0.5 (0.3–1.0) | 1.0 (0.4–2.4) | 1.1 (0.4–2.6) | 0.5 (0.19–1.3) | 0.5 (0.2–1.4) |
| E4+ vs. E4− | 0.5 (0.2–1.2) | 0.4 (0.2–1.0) | 0.3 (0.1–1.4) | 0.3 (0.1–1.4) | 0.4 (0.09–1.8) | 0.5 (0.1–2.3) |
| E5+ vs. E5− | NC | NC | NC | NC | NC | NC |
| E6+ vs. E6− | 0.3 (0.2–0.5) | 0.4 (0.2–0.7) | 0.4 (0.2–1.0) | 0.5 (0.2–1.5) | 0.3 (0.11–0.7) | 0.3 (0.1–0.9) |
| E7+ vs. E7− | 0.6 (0.3–1.0) | 0.6 (0.4–1.2) | 1.3 (0.5–3.7) | 1.8 (0.6–5.4) | 0.5 (0.19–1.2) | 0.7 (0.3–1.9) |
| Any E+ vs. all- | 0.2 (0.1–0.4) | 0.2 (0.1–0.5) | 0.2 (0–1.3) | 0.1 (0–1.0) | 0.1 (0.05–0.4) | 0.3 (0.1–0.8) |
All patients: adjusted for age, smoking, and treatment; Patients with ≤10 pack-years: adjusted for age and treatment; HPV-positive patients: Adjusted for age, smoking, and T category.
All patients: adjusted for age, smoking, and treatment; Patients with ≤10 pack-years: adjusted for age, N category, and treatment; HPV-positive patients: Adjusted for age, smoking, and T category.
NC: not calculable due to zero cells.
Figure 2A shows progression-free survival by E antibody status, and Figure 2B shows progression-free survival by tumor HPV16 DNA status. Although E antibody positivity and HPV16 tumor positivity were associated with significantly better progression-free survival, E antibody status appeared to be a stronger predictor (P<.001 by E antibody status and P=.016 by HPV16; Figure 2A and 2B, respectively). This result was consistent for overall survival as well (P<.001 by E antibody status and P=.031 by HPV16; data not shown). After multivariable adjustment, both patients positive for E antibodies and those with HPV16-positive tumors had an 80% decreased risk of death (95% CI, 0.1–0.5 and 0.1–0.7, respectively). Likewise, E antibody status and HPV16 status were both strongly associated with progression-free survival (E antibody: HR, 0.2; 95% CI, 0.1–0.5, and HPV16: HR, 0.2; 95% CI, 0.1–0.7). Treating E1, NE2, and E6 as continuous variables in the multivariable analysis resulted in significant associations with both overall and progression-free survival (only E6 was not significant for progression-free survival; data not shown).
Figure 2.
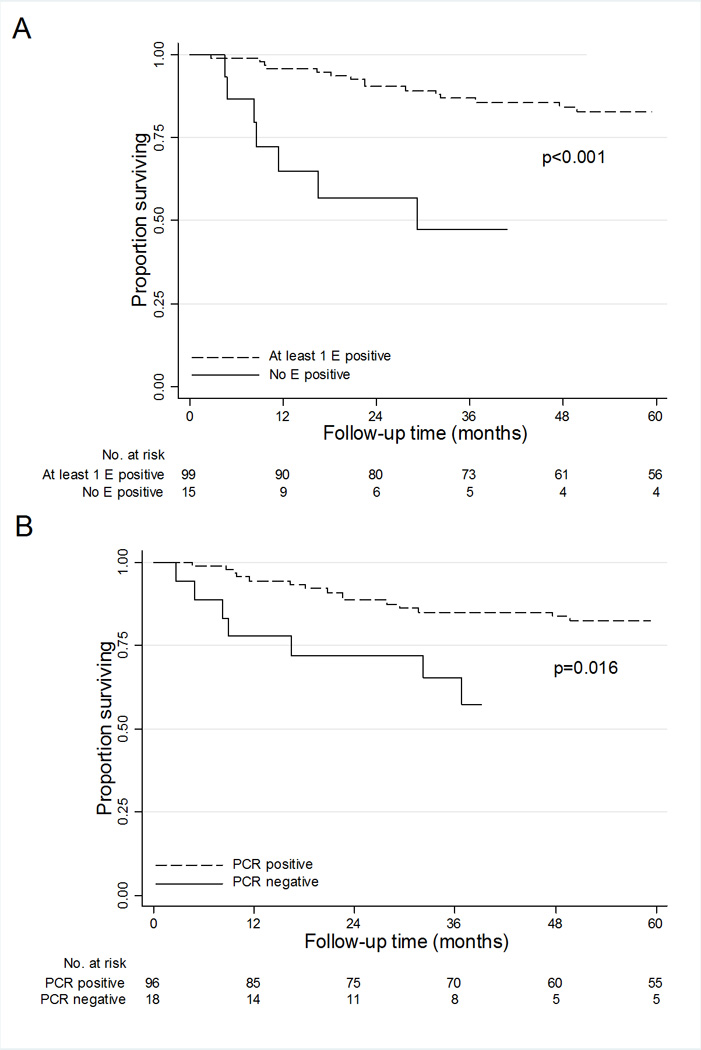
Progression-free survival among 114 patients with OPC with tumor HPV DNA status available. A) Patients positive for at least 1 E antibody versus patients negative for all E antibodies (P<.001). B) Patients with HPV16-positive tumors by PCR versus patients with HPV16-negative tumors by PCR (P=.016).
Among patients with HPV16-negative tumors, E antibody positivity had no demonstrable predictive value for either overall or progression-free survival, although due to the small number of patients this result should be interpreted with caution (data not shown). However, when the analysis was restricted to patients with HPV16-positive tumors (by PCR), patients serologically positive for E antibodies remained at a survival advantage compared with patients who were serologically negative for E antibodies (HR, 0.3; 95% CI, 0.1–0.9 for overall survival and HR, 0.3; 95% CI, 0.1–0.8 for progression-free survival; Table 2 and Figure 3). In particular, antibodies to NE2, E1, and E6 remained strong predictors of overall and progression-free survival. Treating E1, NE2, and E6 as continuous variables in the multivariable analysis resulted in significant or borderline significant (P<.10) associations (data not shown).
Figure 3.
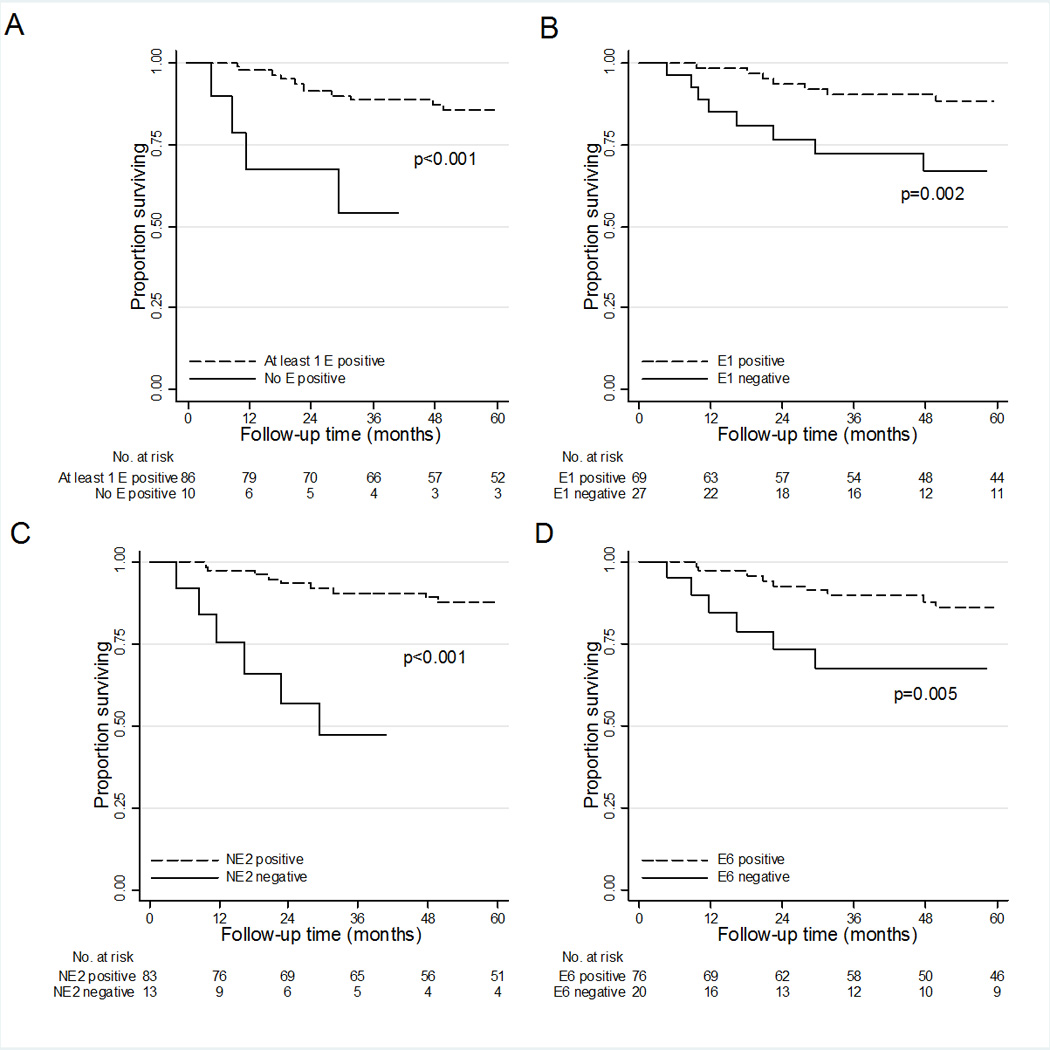
Progression-free survival among 96 patients with HPV16-positive OPC. A) Patients positive for at least 1 E antibody versus patients negative for all E antibodies (P<.001). B) Patients positive for E1 antibody versus patients negative for E1 antibody (P=.002). C) Patients positive for NE2 antibody versus patients negative for NE2 antibody (P<.001). D) Patients positive for E6 antibody versus patients negative for E6 antibody (P=.005).
We used ROC curves to determine the best combination of E antibodies for predicting disease recurrence for all 209 patients. The combination of NE2, E4, E6, and E7 showed the highest accuracy; the optimal operating point was 71.4% at a specificity of 70.2% (AUC=0.71). Adding E1, CE2, and E5 did not improve this. Additionally, the accuracy for NE2 and E6 alone was good relative to the combined antibodies (AUC=0.69 and AUC=0.61; data not shown).
Figure 4 shows the median antibody levels of E1, NE2, and E6 over time for patients with HPV-positive OPC according to recurrence status. A subset of 23 patients chosen at random who did not recur had higher median antibody levels than the 8 patients who did recur, although due to the small sample size we were not able to detect statistically significant differences between the groups.
Figure 4.
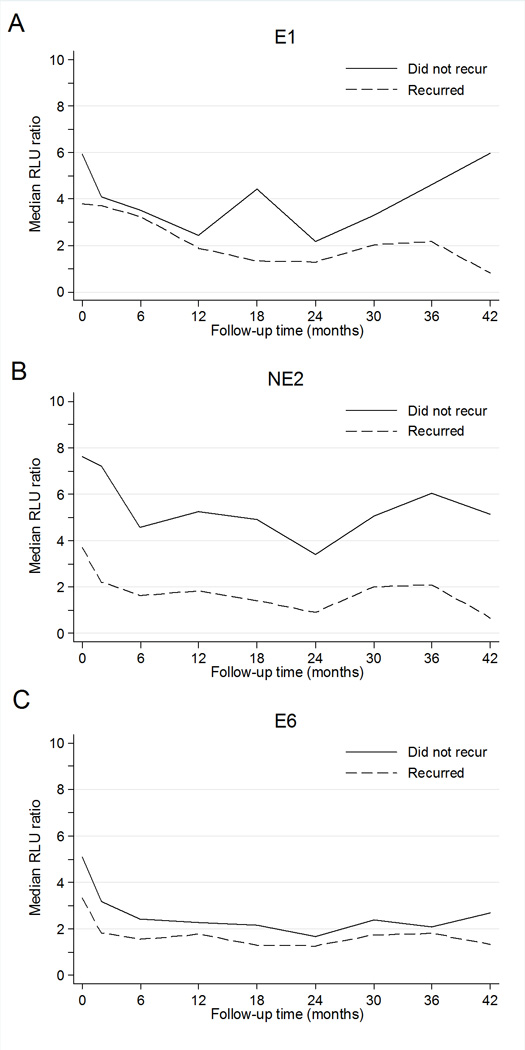
Median antibody levels over time for patients with HPV-positive OPC by disease recurrence status for A) E1 antibodies, B) NE2 antibodies, and C) E6 antibodies. All 8 patients with HPV-positive tumors who recurred and a random subset of 23 patients with HPV-positive tumors but without recurrence at last follow-up were tested at initial workup, 6 months post-treatment, and at 6 month intervals up to 36 months post-treatment.
Discussion
We used a novel protein array serologic assay to determine the prognostic significance of HPV16 antibodies for predicting survival among patients with OPC and HPV-positive OPC. We found that positivity for HPV16 antibodies was strongly associated with both overall and progression-free survival. This association was limited to E antibodies, in particular antibodies to the early proteins NE2, E1, and E6; positivity for antibodies to coat protein L were not predictive for survival. This preliminary evidence suggests that serologic response to antigens involved in HPV-mediated carcinogenesis, but not serologic response to antigens important to the infectious process (L proteins), may differentially predict cancer outcomes. Our findings support the hypothesis that cancer outcomes are in part dictated by the immune response and that E antibodies may be biomarkers of carcinogenic changes and prognosis.
We previously showed that a small subset of patients with HPV16-positive tumors who were negative for E6 and E7 antibodies were positive for E1 and NE2 antibodies, which illustrates the need for including multiple markers in HPV16 serologic studies and for diagnosis (19). More recently, we showed a dramatically increased risk for OPC among individuals who were positive for E antibodies in a study that included 256 cases and 250 controls (manuscript submitted). We found that those positive for any E antibody had 244 times the OPC risk of those negative for all E antibodies. Furthermore, patients with tumors positive for HPV16 DNA were 4 times as likely to be positive for any E antibody as were patients with tumors negative for HPV16 DNA, and this association was particularly strong among patients with HPV16-positive tumors who were never-smokers or light smokers.
Although HPV16 capsid proteins, L1 and L2, have been used to establish the causal association between HPV16 and OPC and are present several years before the development of an HPV16-positive cancer (3, 8, 21, 22), we did not find that antibodies to capsid proteins were associated with survival among patients with OPC. This is not surprising biologically given that capsid antibodies are not expressed following tumor development and are lost on HPV DNA integration into host DNA. Capsid antibodies thus are not expected to be useful as a diagnostic tool or as predictors of cancer outcome.
The immunobiology that might explain differences or absences in antibody responses to one or another specific antigen is not understood. Serologic immune responses to HPV16-positive tumors may correlate with high viral load. For example, in the Costa Rica HPV16 vaccine trial, high viral load was predictive of HPV16 seropositivity among 646 young, HPV16-infected women (23). It has also been reported that viral load is a reliable indicator of an HPV16-driven tumor and subsequent risk of death (24, 25). Mellin et al found in a small number of subjects that viral load had a wide distribution among patients with tonsillar cancer and that it was positively correlated with survival (25). This may reflect changes during carcinogenesis with decreased dependence on HPV early antigens as the tumors progress genetically. HPV16-positive tumors that fail to elicit or lose a serologic response may no longer be completely driven by HPV-based mechanisms.
This study has several limitations. First, since a large proportion of patients whose tumors were negative for HPV16 DNA were positive for at least 1 E antibody (13/18, 72.2%) and, conversely, a subset of patients whose tumors were positive for HPV16 DNA were negative for all E antibodies (10/96, 10.4%), these patients may have been misclassified. If we had evaluated HPV16 status using other methods in addition to PCR, such as p16 expression or in situ hybridization, we might have found more HPV16-positive cases among patients serologically positive for E antibodies but with tumors negative for HPV16 DNA by PCR. Additionally, although HPV16 is the predominant type found in OPC tumor tissue, the HPV16-negative cases could have been positive for another HPV type. We were unable to further analyze this subset of HPV16-negative, antibody-positive patients due to the small sample size and lack of availability of additional tumor tissue for analysis. Second, while the study included 209 patients with follow-up, we had HPV16 status for only 114, which limited our sample size for analysis to 96 patients with HPV16-positive tumors. Furthermore, most patients were positive for at least 1 HPV16 antibody, limiting our ability to isolate effects of individual antibodies. These limitations may have reduced the power to detect differences in survival between individual antibody-positive and antibody-negative subgroups. We are currently expanding the study to increase the sample size as well as using p16 expression and in situ hybridization to determine tumor HPV status. Given the high accuracy of these assays, along with increased study power, we will be able to explore more fully the association between tumor HPV DNA and antibody status.
Our results show that HPV16 antibody status, in particular E antibody status, is a strong predictor of survival among patients with HPV-positive OPC. Specific antibody status has the potential to be a useful prognostic indicator that may identify subsets of patients diagnosed with HPV16-positive tumors who may benefit from altered monitoring and/or treatments. Additionally, the suggestion that immune response to HPV16 antigens is important to cancer outcomes suggests the potential of augmenting immune responses to improve treatment of patients with HPV-driven OPC. Using serology to identify HPV16-positive tumors may be useful as tumor tissue is not always available and serology is less invasive and therefore more acceptable to patients. Furthermore, combining multiple biomarkers may improve the validity of a prognostic test. In light of this, larger prospective studies are needed to confirm our findings.
Supplementary Material
Statement of translational relevance.
Patients with HPV16-positive oropharyngeal carcinoma (OPC) have significantly better survival than do patients with HPV16-negative OPC. Furthermore, differences in survival exist within HPV16-positive OPC. The goal of this study was determine the usefulness of serum antibodies to HPV16 DNA antigens as predictors of survival for patients with OPC. We found that E1, NE2, and E6 antibody positivity were all strongly associated with improved overall and progression-free survival in the entire cohort and in patients with known HPV16-positive tumors (P<.05). Serum antibodies to HPV16 DNA antigens, in particular to the early proteins E1, NE2, and E6, have prognostic significance for patients with HPV16-positive OPC.
Acknowledgements
We thank Alison Goulder for technical assistance and Stephanie Deming for manuscript editing.
Financial support: This research was supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant, CA016672, National Institutes of Health grant R03 Grant CA128110-01A1 (to E.M.S.), an institutional research grant from The University of Texas MD Anderson Cancer Center (to E.M.S.), Arizona State University institutional funds (to K.S.A.), and National Cancer Institute Early Detection Research Network grant U01 CA117374 (to K.S.A.). Dr. Anderson received travel support from Luminex Corporation in 2011 and serves on the scientific advisory board and receives consultant fees from ProvistaDx. This research was accomplished within the Oropharynx Program at The University of Texas MD Anderson Cancer Center and funded in part through the Stiefel Oropharyngeal Research Fund.
References
- 1.Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29:4294–4301. doi: 10.1200/JCO.2011.36.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reuschenbach M, Waterboer T, Wallin KL, Einenkel J, Dillner J, Hamsikova E, et al. Characterization of humoral immune responses against p16, p53, HPV16 E6 and HPV16 E7 in patients with HPV-associated cancers. Int J Cancer. 2008;123:2626–2631. doi: 10.1002/ijc.23837. [DOI] [PubMed] [Google Scholar]
- 3.Herrero R, Castellsague X, Pawlita M, Lissowska J, Kee F, Balaram P, et al. Human papillomavirus and oral cancer: The International Agency for Research on Cancer multicenter study. J Natl Cancer Inst. 2003;95:1772–1783. doi: 10.1093/jnci/djg107. [DOI] [PubMed] [Google Scholar]
- 4.Zumbach K, Hoffmann M, Kahn T, Bosch F, Gottschlich S, Gorogh T, et al. Antibodies against oncoproteins E6 and E7 of human papillomavirus types 16 and 18 in patients with head-and-neck squamous-cell carcinoma. Int J Cancer. 2000;85:815–818. doi: 10.1002/(sici)1097-0215(20000315)85:6<815::aid-ijc14>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 5.Meschede W, Zumbach K, Braspenning J, Scheffner M, Benitez-Bribiesca L, Luande J, et al. Antibodies against early proteins of human papillomaviruses as diagnostic markers for invasive cervical cancer. J Clin Microbiol. 1998;36:475–480. doi: 10.1128/jcm.36.2.475-480.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosales R, Lopez-Contreras M, Cortes RR. Antibodies against human papillomavirus (HPV) type 16 and 18 E2, E6 and E7 proteins in sera: Correlation with presence of papillomavirus DNA. J Med Virol. 2001;65:736–744. doi: 10.1002/jmv.2098. [DOI] [PubMed] [Google Scholar]
- 7.Ravaggi A, Romani C, Pasinetti B, Tassi RA, Bignotti E, Bandiera E, et al. Correlation between serological immune response analyzed by a new ELISA for HPV-16/18 E7 oncoprotein and clinical characteristics of cervical cancer patients. Arch Virol. 2006;151:1899–1916. doi: 10.1007/s00705-006-0787-y. [DOI] [PubMed] [Google Scholar]
- 8.Mork J, Lie AK, Glattre E, Hallmans G, Jellum E, Koskela P, et al. Human papillomavirus infection as a risk factor for squamous-cell carcinoma of the head and neck. N Engl J Med. 344:1125–1131. doi: 10.1056/NEJM200104123441503. 200. [DOI] [PubMed] [Google Scholar]
- 9.Anantharaman D, Gheit T, Waterboer T, Abedi-Ardekani B, Carreira C, McKay-Chopin S, et al. Human papillomavirus infections and upper aero-digestive tract cancers: The ARCAGE study. J Natl Cancer Inst. 2013;105:536–545. doi: 10.1093/jnci/djt053. [DOI] [PubMed] [Google Scholar]
- 10.Kreimer AR, Johansson M, Waterboer T, Kaaks R, Chang-Claude J, Drogen D, et al. Evaluation of human papillomavirus antibodies and risk of subsequent head and neck cancer. J Clin Oncol. 2013;31:2708–2715. doi: 10.1200/JCO.2012.47.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson KS. Multiplexed detection of antibodies using programmable bead arrays. Methods Mol Biol. 2011;723:227–238. doi: 10.1007/978-1-61779-043-0_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, Pinto H, et al. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst. 2008;100:261–269. doi: 10.1093/jnci/djn011. [DOI] [PubMed] [Google Scholar]
- 13.Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehta V, Yu GP, Schantz SP. Population-based analysis of oral and oropharyngeal carcinoma: Changing trends of histopathologic differentiation, survival and patient demographics. Laryngoscope. 2010;120:2203–2212. doi: 10.1002/lary.21129. [DOI] [PubMed] [Google Scholar]
- 15.Rischin D, Young RJ, Fisher R, Fox SB, Le QT, Peters LJ, et al. Prognostic significance of p16INK4A and human papillomavirus in patients with oropharyngeal cancer treated on TROG 02.02 phase III trial. J Clin Oncol. 2010;28:4142–4148. doi: 10.1200/JCO.2010.29.2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Posner MR, Lorch JH, Goloubeva O, Tan M, Schumaker LM, Sarlis NJ, et al. Survival and human papillomavirus in oropharynx cancer in TAX 324: A subset analysis from an international phase III trial. Ann Oncol. 2011;22:1071–1077. doi: 10.1093/annonc/mdr006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fakhry C, Zhang Q, Nguyen-Tan PF, Rosenthal D, El-Naggar A, Garden AS, et al. Human papillomavirus and overall survival after progression of oropharyngeal squamous cell carcinoma. J Clin Oncol. 2014;32:3365–3373. doi: 10.1200/JCO.2014.55.1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong J, Sibani S, Lokko NN, LaBaer J, Anderson KS. Rapid detection of antibodies in sera using multiplexed self-assembling bead arrays. J Immunol Methods. 2009;350:171–182. doi: 10.1016/j.jim.2009.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson KS, Wong J, D'Souza G, Riemer AB, Lorch J, Haddad R, et al. Serum antibodies to the HPV16 proteome as biomarkers for head and neck cancer. Br J Cancer. 2011;104:1896–1905. doi: 10.1038/bjc.2011.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D'Souza G, Gross ND, Pai SI, Haddad R, Anderson KS, Rajan S, et al. Oral human papillomavirus (HPV) infection in HPV-positive patients with oropharyngeal cancer and their partners. J Clin Oncol. 2014;32:2408–2415. doi: 10.1200/JCO.2014.55.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dillner J. The serological response to papillomaviruses. Semin Cancer Biol. 9:423–430. doi: 10.1006/scbi.1999.0146. 199. [DOI] [PubMed] [Google Scholar]
- 22.Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92:709–720. doi: 10.1093/jnci/92.9.709. [DOI] [PubMed] [Google Scholar]
- 23.Porras C, Bennett C, Safaeian M, Coseo S, Rodriguez AC, Gonzalez P, et al. Determinants of seropositivity among HPV-16/18 DNA positive young women. BMC Infect Dis. 2010;10:238. doi: 10.1186/1471-2334-10-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holzinger D, Schmitt M, Dyckhoff G, Benner A, Pawlita M, Bosch FX. Viral RNA patterns and high viral load reliably define oropharynx carcinomas with active HPV16 involvement. Cancer Res. 2012;72:4993–5003. doi: 10.1158/0008-5472.CAN-11-3934. [DOI] [PubMed] [Google Scholar]
- 25.Mellin H, Dahlgren L, Munck-Wikland E, Lindholm J, Rabbani H, Kalantari M, et al. Human papillomavirus type 16 is episomal and a high viral load may be correlated to better prognosis in tonsillar cancer. Int J Cancer. 2002;102:152–158. doi: 10.1002/ijc.10669. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


