Abstract
Objective
To evaluate if the peak knee flexor moment provides unique and meaningful information about peak medial compartment loading above and beyond what is obtained from the peak knee adduction moment.
Methods
Standard video-based motion capture and EMG recordings were collected for 10 ACL reconstructed subjects walking at a self-selected speed. Knee joint moments were obtained using inverse dynamics and medial contact force was computed using an EMG-driven musculoskeletal model. Linear regression with the peak adductor moment entered first was implemented to isolate the unique contribution of the peak flexor moment to peak medial loading.
Results
Peak moments and medial contact force occurred during weight acceptance at approximately 23% of stance. The peak adduction moment (pKAM) was a significant predictor of peak medial loading (p = 0.004) accounting for approximately 63% of the variance. The peak knee flexor moment (pKFM) was also a significant predictor (p = 0.009) accounting for an additional 22% of the variance. When entered together pKAM and pKFM accounted for more than 85% of the variance in peak medial compartment loading.
Conclusion
The combined use of the peak knee flexor and adductor moments provides a significantly more accurate estimate of peak medial joint loading than the peak adduction moment alone. More accurate inferences of joint contact force will assist clinicians and researchers investigating relationships between joint loading and the onset and progression of knee OA.
Keywords: Contact Force, Modeling, Gait, Electromyography
Introduction
The knee is the most commonly affected joint in people with osteoarthritis (OA) [1]. Altered loading is thought to contribute to the onset and progression of knee OA [2-5] and therefore knowledge of the magnitude, timing and distribution of forces between the medial and lateral compartments is of interest to clinicians and researchers. In recent years it has become possible to measure joint contact forces in vivo in a select few individuals who have undergone total knee arthroplasty with an instrumented prosthesis [6, 7]. These data allow researchers to quantify joint loading during activities of daily living and have shown that gait modifications can alter tibio-femoral contact force magnitudes. While these data have increased our knowledge of knee forces in the middle age and older adult after TKA, joint loading in younger and more active people, and persons with pathology are of interest. For example, there is a high incidence of secondary knee OA following anterior cruciate ligament (ACL) injury[8, 9] and for this group of patients it would be helpful to know if altered loading is associated with onset and progression of the disease.
In general it is not possible to measure joint forces in vivo and consequently indirect or surrogate measures are used to evaluate loading and how it changes with time or responds to an intervention. The most common surrogate measure is the external knee adduction moment (KAM). The general view is the larger the KAM the greater the medial compartment contact force, and vice-versa [10, 11]. KAM has been shown to be related to disease severity [5] and progression [12] in those with medial knee OA and varus mal-alignment, and for these reasons it has been the focus of many studies investigating mechanisms of and treatment for the disease [13].
The relationship between KAM and medial joint loading is influenced by an individual's gait and the manner in which they activate their muscles. Consider the following instrumented knee cases studies reporting the following: (i) a positive linear relationship between KAM and medial contact force [14]; (ii) a decrease in KAM does not guarantee a decrease in medial contact force [15]; (iii) and the 2012 Grand Challenge1 in which peak KAM decreased when walking with a medial thrust gait but medial contact force increased. Collectively these studies show the relationship between KAM and contact force is anything but straightforward.
The net external knee flexor moment (KFM) is reflective of all agonist and antagonistic muscle forces crossing the knee. Peak medial contact force occurs at approximately 25% of stance as the quadriceps contract eccentrically and muscle force contributions from the hamstrings and gastrocnemii are relatively small [16]. Since KFM is dominated by the quadriceps during this time, and muscle forces are the primary contributors to knee joint loading [17, 18], this led us to question if peak KFM (pKFM) would provide unique and meaningful information above and beyond peak KAM (pKAM) when inferring peak medial contact force. To address this non-invasively requires a model to predict medial contact force. The EMG-driven model implemented by Manal and Buchanan[19] in the 2012 Grand Challenge to predict in vivo knee forces was used to predict knee contact force for a group of ACL reconstructed subjects walking at a self-selected speed. The relative contribution of pKAM and pKFM to the model predicted peak medial contact force was then evaluated using blockwise linear regression. We hypothesized that pKFM would be a significant predictor of medial joint loading after accounting for variance attributed to pKAM.
Methods
Ten subjects (5 male, 5 female) were tested approximately 6 months after ACL reconstruction. These subjects were part of a larger on-going study investigating gait mechanics and clinical outcomes after surgery (ClinicalTrials.gov identifier: NCT01773317). Each subject was evaluated by a licensed Physical Therapist to ensure joint effusion, range of motion, strength deficits, pain and obvious gait deviations were resolved prior to testing. Exclusion criteria included: a full-thickness chondral defect ≥ 1 cm2, symptomatic meniscus tear or concomitant grade III rupture to other knee ligaments.
Subject characteristics are listed in Table 1. The purpose of the study, experimental procedures and potential risks were explained to each subject and written informed consent was obtained prior to participation. The study was approved by the Institutional Review Board of the University of Delaware.
Table 1. Subject Characteristics (n=10) and descriptive statistics for natural cadence walking.
| Characteristic | Mean (SD) or Sex (male / female) |
|---|---|
| Age (years) | 30.1 (7.9) |
| Height (m) | 1.75 (0.08) |
| Weight (N) | 866 (155) |
| Time from Surgery (weeks) | 26.4 (3.0) |
| Graft Type | |
| Allograft (male / female) | 5 (3 / 2) |
| Autograft (male / female) | 5 (3 / 2) |
| Walking Speed (m/s) | 1.54 (0.10) |
| Quadriceps Index (Inv / Uninv) | 0.98 (0.05) |
| Peak KAM (% BW * Ht) | 2.66 (0.85) |
| Peak KFM (% BW * Ht) | 4.44 (1.48) |
| Peak MC (BW) | 2.30 (0.40) |
Five natural cadence walking trials per subject were collected using an 8-camera Vicon motion capture system (Oxford Metrics Ltd., London, UK) and a Bertec force platform (Bertec Corportation, Worthington, OH). Shod walking speed was maintained at +/- 5% of an individual's preferred speed determined prior to testing using photo-electric timing gates (Brower Timing Systems, Draper, Utah). Retro-reflective markers positioned over bony landmarks were used to define anatomical coordinate systems that were subsequently tracked from markers affixed to thermoplastic shells secured to the pelvis, thigh, shank and foot of each leg. The specific marker set has been described elsewhere[20]. Marker data were sampled at 120 Hz and filtered with a bi-directional 4th order Butterworth filter with a cut-off frequency of 6 Hz. Ground reaction force data were sample at 1080 Hz. Visual3D (C-Motion, Germantown, MD) was used to calculate stance phase kinematics and joint moments derived from inverse dynamics. Joint moments were normalized to body weight and height (m) and expressed as %BW*Ht. A vertical ground reaction force threshold of 20 N was used to identify foot contact and lift-off.
Surface EMG (MA-300 Motion System Labs, Baton Rouge, LA) was sampled at 1080 Hz for the major muscles crossing the knee including: rectus femoris (RF), vastus medialis and lateralis (VM & VL), biceps femoris longus (BFL), semitendinosus (ST) and the medial and lateral gastrocnemii (MG & LG). EMG data were high pass filtered (30 Hz), rectified and then low-pass filtered at 6 Hz creating a linear envelope. The enveloped signals for the VM and VL were averaged and used to approximate the signal for the vastus intermedius (VI). Signals for the semimembranosus (SM) and biceps femoris short head (BFS) were set equal to the ST and BFL respectively. The enveloped signals were then normalized to maximum values determined from separate isometric trials to elicit maximal EMG signal magnitude. Subjects performed 2 flexion and extension maximum voluntary isometric contractions (MVIC) while seated in a Biodex dynamometer (Shirley NY). The knee was positioned in 60 degrees of flexion and the hip was flexed at approximately 90 degrees. In addition, the gastrocnemius was tested with the subject seated, knee extended and the ankle in a neutral position. Two MVIC plantar flexion trials were recorded. All MVIC trials were processed as previously described with the peak enveloped value for each muscle considered the maximum EMG and used for normalization.
Normalized EMG and joint kinematics were input to an EMG-driven musculoskeletal model of the knee to predict individual muscle forces. The EMG-driven model has been described in detail elsewhere[21] and therefore will not be presented here. Medial joint contact force was calculated from the EMG-driven model-predicted muscle forces and a frontal plane moment balancing algorithm summarized in Manal and Buchanan [19]. Briefly, the external knee adduction moment must be balanced internally by an equal and opposite moment created by muscle and joint contact forces acting on the medial and lateral compartments. It is convenient to sum the moments about the lateral condyle eliminating the unknown lateral contact force since it does not create a moment about the lateral condyle. Muscle forces are obtained from the EMG-driven model leaving medial contact force as the only unknown. This process is repeated at each time-step resulting in a time-varying medial contact force profile. The external knee adduction moment expressed about the lateral condyle is not identical to pKAM which is calculated about the center of the knee joint. This distinction is important as pKAM and pKFM are used in the regression analysis to predict medial contact force. The EMG-driven model has been shown to have good reliability [22] and accuracy [19] in predicting medial contact force during gait. Intra-class correlation coefficients (ICC(3;k)) of 0.869, 0.946 and 0.808 for peak medial contact force, pKAM and pKFM respectively demonstrate test-retest reliability for these measures [22].
Medial contact force, pKAM and pKFM for three walking trials per subject were ensemble-averaged with all data normalized to 101 data points. Linear regression was used to predict peak medial loading from pKAM and pKFM. Peak KAM was entered first to isolate the unique contribution of pKFM. A constant Y-intercept was retained as zero contact force during stance is not possible. The coefficient of determination, R2, was used to evaluate goodness of fit and statistical significance for each predictor was set an alpha level of p=0.05 for all analyses. The Wilk-Shapiro test of normality confirmed peak medial contact force (p=0.443), pKAM (p=0.261) and pKFM (p=0.621) were all normally distributed. Statistical procedures were performed using IBM SPSS Statistics 22.
Results
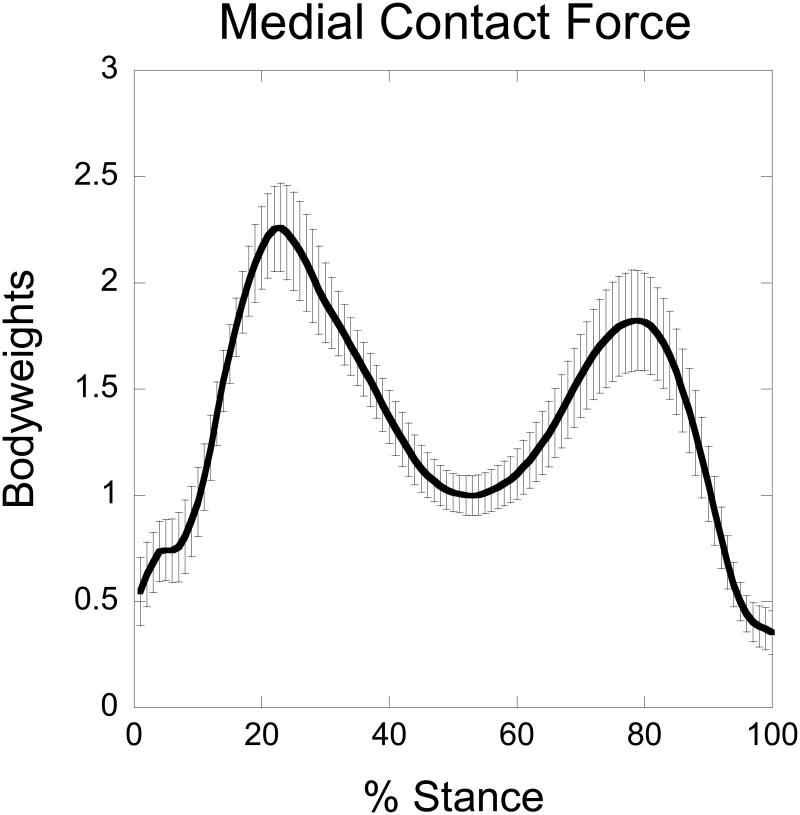
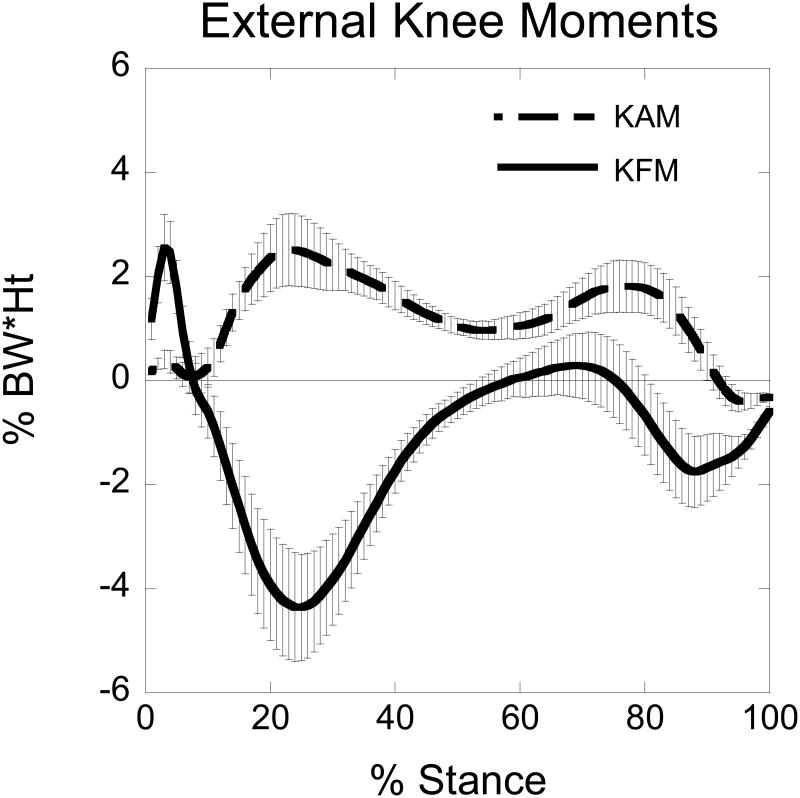
The EMG-driven model prediction of medial contact force had an average peak magnitude of 2.3 BWs occurring at 23% of stance. The second peak was smaller (1.8 BWs) and the overall shape had the expected double hump pattern (Figure 1). Both KAM and KFM exhibited patterns typical of normal walking (Figure 2). Peak KAM and pKFM reached peak values at approximately the same time (23% & 25% of stance respectively), and this coincided with the timing of peak medial contact force (23% stance).
Figure 1.
Ensemble averaged medial compartment contact force for 10 subjects walking at a self-selected speed (gray band = 95% confidence interval).
Figure 2.
Ensemble averaged external knee adduction (KAM) and flexor (KFM) moments for 10 subjects walking at a self-selected speed. The gray bars represent 95% confidence intervals. An increasing positive value for KAM indicates an increasing external knee adduction moment. A larger negative value for KFM indicates a larger external knee flexion moment. Note the timing of peak KAM and KFM was almost identical.
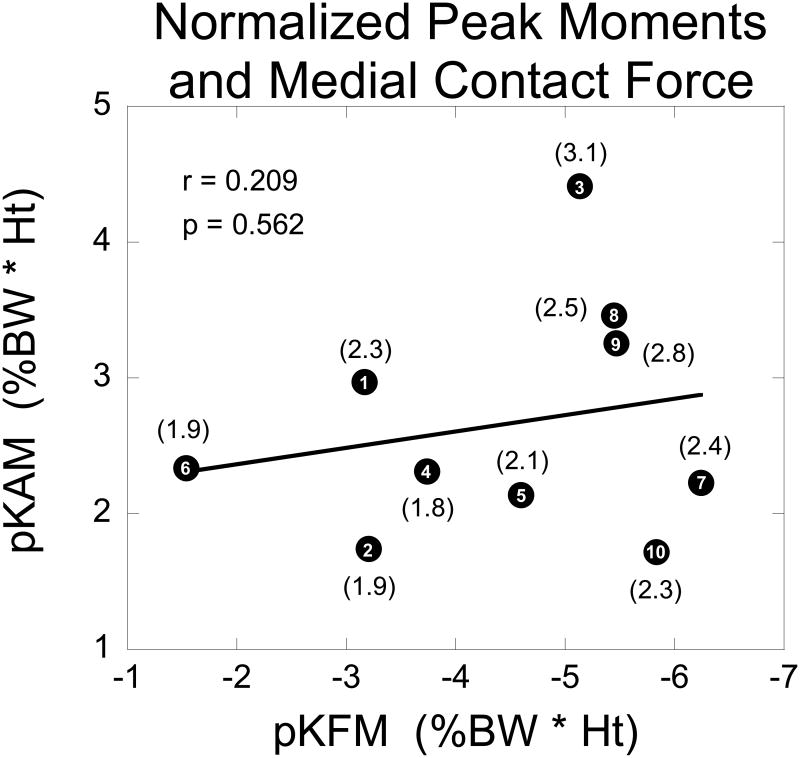
Peak KAM was itself a significant predictor of peak medial loading (p = 0.004) accounting for approximately 63% of the variance as indicated by the adjusted R2 (Table 2). There was a strong positive relationship (unstandardized beta = 0.386) between pKAM and peak loading indicating that as pKAM increased so did peak medial contact force and vice-versa. The primary finding of interest supporting our hypothesis was that pKFM was also a significant predictor of peak loading (p = 0.009) (Table 2). Peak KFM was significant after accounting for the variance attributed to pKAM. The overall model fit with pKAM and pKFM entered together improved significantly (p = 0.009) with an adjusted R2 of 0.851 (Table 2). Unstandardized betas for pKAM and pKFM were 0.340 and -0.127 respectively indicating pKAM was the stronger of the two predictors. The negative beta associated with pKFM reflects our negative sign convention for an increasing knee flexor moment (see Figure 2). We also looked at the pKAM by pKFM interaction and found that it was not significant and thus it was not included in the final regression model. Additionally, pKAM and pKFM were not correlated (r = -0.209, p = 0.562) as seen in Figure 3.
Table 2. Regression results for pKAM as a sole predictor of peak MC (Model: Const. & pKAM), and when pKFM was entered as a second predictor after accounting for variance attributed to pKAM (Model: Const., pKAM & pKFM).
| Model | Beta Coefficients | t | Sig. | R | Adj. R2 | Sig. F Change | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Unstandardized | Std. Error | ||||||
|
| |||||||
| Const. | 1.275 | 0.264 | 4.829 | 0.001 | 0.821 | 0.633 | 0.004 |
| pKAM | 0.386 | 0.095 | 4.066 | 0.004 | |||
|
| |||||||
| Const. | 0.834 | 0.209 | 3.988 | 0.005 | 0.940 | 0.851 | 0.009 |
| pKAM | 0.340 | 0.062 | 5.485 | 0.001 | |||
| pKFM | -0.127 | 0.036 | -3.556 | 0.009 | |||
Figure 3.
Scatter plot of subjects' normalized pKAM and pKFM. There was a weak and nonsignificant correlation between pKAM and pKFM. The number contained within each data point is the subject ID while values reported in parentheses are the EMG-driven model predicted medial compartment contact forces.
Discussion
The purpose of this study was to evaluate if pKFM provides unique and meaningful information above and beyond pKAM when evaluating medial knee joint loading. The regression analysis with pKAM entered first revealed several interesting findings. Firstly, pKAM by itself was a significant predictor of peak medial loading (p < 0.004) accounting for 63% of the variance in peak medial contact force. This finding supports the idea the larger the pKAM the greater the medial contact force and vice-versa. Additionally, these data provide an indication of the strength of the association between pKAM and peak medial contact force which cannot be assessed when pKAM is used as a surrogate measure of loading since there is no quantitative expression of the contact force.
The second noteworthy finding and the motivation for this study was that pKFM was a significant predictor of peak loading (p < 0.009) after accounting for the variance attributed to pKAM. The adjusted R2 increased from 0.633 for pKAM alone to 0.851 when pKAM and pKFM were both included in the regression model (Table 2). The unstandardized beta for pKAM was larger than pKFM indicating it was the stronger of the 2 predictors. Also important was that pKAM and pKFM were not correlated (r = -0.209, p = 0.562), supporting the idea that both joint moments provide unique information about medial joint contact force. Although it may seem obvious pKFM would be associated with medial loading, clinical studies often focus uniquely on pKAM with little consideration given to KFM. For example, Butler and colleagues speculated that joint loading for ACL-reconstructed subjects increased with time from surgery based on their observation that pKAM increased [23]. While this interpretation is plausible, without considering how the flexor moment changed (they did not report knee flexor moment) it is difficult to conclude with any degree of certainty whether medial loading truly increased for their group of subjects.
Recently, Creaby and colleagues reported peak KAM and KAM impulse were both associated with cartilage defects in persons with mild to moderate knee OA[24], but only KAM impulse at baseline was associated with cartilage volume loss over a 12 month period[25]. This finding implies cumulative load is more strongly associated with OA progression than peak loading. Whether pKAM is the best indicator of peak loading is questionable, and based on our results future studies may wish to consider the combined use of pKAM and pKFM as a more accurate representation of peak loading.
The use of surrogate measures to infer loading is not meant to be predictive of actual contact force magnitude, but rather it is used to evaluate if loading has likely changed due to an intervention or if loading differs between groups. Considering that pKAM itself was a significant predictor of peak medial loading one may question whether considering pKFM is necessary if the goal is simply to evaluate relative loading. We believe the answer is yes as seen in the 2012 Grand Challenge data to predict in vivo knee loads. The subject had reduced pKAM walking with a medial thrust gait, but medial contact force increased from 1.80 BWs to 2.57 BWs. Walking with a medial thrust gait required much larger KFM and the net effect was greater medial loading despite a significant reduction in pKAM.
Including pKFM as a second predictor can strengthen and also complicate inferences about loading depending on the relative magnitude of pKAM and pKFM. For example, if pKAM and pKFM both increase or decrease in the same direction it is likely that medial loading will also change in the that direction. Less straightforward is when pKAM and pKFM change in opposite directions. For example, if a decrease in pKAM is offset by a similar increase in pKFM (or vice-versa) one might expect that medial loading will decrease since pKAM is a more heavily weighted predictor (see unstandardized coefficients in Table 2). For our group of subjects the regression coefficient for pKAM was approximately 2.5 times greater than pKFM and thus for a similar change in moment the effect on peak medial loading would be about 2.5 times greater for pKAM. The significance of this is that any potential reduction in medial loading associated with a decrease in pKAM can be offset by a large increase in pKFM. A similar pattern was reported by Simic and colleagues for subjects walking with toes-pointed-in compared to natural gait. Peak KAM was smaller with toes pointed-in, but this caused pKFM to increase. The change in pKFM was approximately twice the change in pKAM making it difficult to infer how medial contact force may have changed during toed-in gait.
Although much can be learned from group averaged data it is ultimately how an individual responds to treatment that is of interest in a clinical setting. Inspecting individual subject data we see that those with large pKAM and pKFM had the greatest medial contact force while subjects with the least loading had relatively small pKAM and pKFM (Figure 3). For these subjects correctly grouping them as high or low loaders based on the magnitude of pKAM and pKFM is straightforward. Other data are not as obvious. For example, consider subjects 2 and 6 with peak loading of 1.9 BWs. Based on pKAM alone one might have concluded that subject 6 had the larger contact force. A different interpretation arises when pKAM and pKFM are considered together, and for these two subjects, the interplay between KAM and KFM resulted in identical peak contact force. A similar and more striking example can be seen for subjects 1 and 10 both of whom had a peak contact force of 2.3 BWs. Both of these examples illustrate how KFM and KAM both influence medial contact force and therefore they both should be considered when inferring medial joint loading indirectly from knee joint moments.
There are several limitations of this work that warrant discussion. Firstly, we did not measure joint contact force directly but rather estimated medial loading using a previously validated musculoskeletal model. Although the patient specific EMG-driven model has been shown to have good accuracy, the values reported in this study are model-based predictions that cannot be validated. Additionally, the regression coefficients we report were based on a limited sample size of 10 subjects, all of whom were approximately 6 months post-ACL reconstruction. It was never our intent to provide a generalizable predictive regression equation for use by others. Whether the moment based regression coefficients are appropriate for other subjects is uncertain and should be viewed cautiously. What can be generalized from our data however is the idea that pKFM provides unique and meaningful information above and beyond pKAM. A practical implication of this is that when pKAM and pKFM increase or decrease in the same direction one can be confident that medial loading will change in a similar direction. Whether this holds for other tasks should not be assumed and requires additional investigation.
It is often assumed the larger the pKAM the greater the medial contact force and vice-versa. In recent years it has become clear this interpretation is too simplistic. In this paper we demonstrate using experimental data and modeling results that pKAM and pKFM are both significant predictors of peak medial loading, and depending on the relative magnitude of these moments there are likely varying degrees of confidence with which one can make inferences about medial joint loading. The take-home message of this study is that both pKAM and pKFM should be considered when evaluating joint loading indirectly from external knee moments. The combined use of pKAM and pKFM is easy to incorporate and provides a more accurate indication of peak medial contact force than pKAM alone. More accurate inferences of joint contact force will assist clinicians and researchers investigating relationships between joint loading and the onset and progression of knee OA.
Acknowledgments
This work was supported by the National Institutes of Health (P30-GM103333, R01-AR046386, R01-AR048212).
Footnotes
The Grand Challenge competition to predict In Vivo knee loads provides researchers comprehensive data sets enabling validation of musculoskeletal model estimates of muscle and joint contact forces. Data are obtained from individuals implanted with instrumented knee prostheses and the data are publically available from https://simtk.org/home/kneeloads. The model implemented by Manal and Buchanan and used in the present study placed first in the 2012 Grand Challenge competition.
Author Contributions: Kurt Manal made substantial contributions to study conception, design and data analysis. KM drafted the article and is the corresponding author.
Emily Gardinier contributed significantly to the data acquisition and analysis. EG revised the article prior to submission and approved the final version.
Thomas S Buchanan made substantial contributions to study design and interpretation of results. TSB revised the article prior to submission and approved the final version
Lynn Snyder-Mackler made substantial contributions to study design and interpretation of results. LSM revised the article prior to submission and approved the final version
Conflicts of Interest: There are no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Oliveria SA, et al. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis and rheumatism. 1995;38(8):1134–41. doi: 10.1002/art.1780380817. [DOI] [PubMed] [Google Scholar]
- 2.Felson DT. Osteoarthritis as a disease of mechanics. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2013;21(1):10–5. doi: 10.1016/j.joca.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baliunas AJ, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10(7):573–9. doi: 10.1053/joca.2002.0797. [DOI] [PubMed] [Google Scholar]
- 4.Andriacchi TP, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18(5):514–8. doi: 10.1097/01.bor.0000240365.16842.4e. [DOI] [PubMed] [Google Scholar]
- 5.Sharma L, et al. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41(7):1233–40. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 6.D'Lima DD, et al. Tibial forces measured in vivo after total knee arthroplasty. J Arthroplasty. 2006;21(2):255–62. doi: 10.1016/j.arth.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Bergmann GBA, Graichen F, Dymke J, Rohlmann A, Trepczynski A, Heller MO, Kutzner I. Standardized Loads Acting in Knee Implants. PLoS ONE. 2014;9(1) doi: 10.1371/journal.pone.0086035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barenius B, et al. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–57. doi: 10.1177/0363546514526139. [DOI] [PubMed] [Google Scholar]
- 9.Lohmander LS, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–52. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 10.Erhart-Hledik JC, et al. Effect of variable-stiffness walking shoes on knee adduction moment, pain, and function in subjects with medial compartment knee osteoarthritis after 1 year. J Orthop Res. 2012;30(4):514–21. doi: 10.1002/jor.21563. [DOI] [PubMed] [Google Scholar]
- 11.Shakoor N, Block JA. Walking barefoot decreases loading on the lower extremity joints in knee osteoarthritis. Arthritis Rheum. 2006;54(9):2923–7. doi: 10.1002/art.22123. [DOI] [PubMed] [Google Scholar]
- 12.Miyazaki T, et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61(7):617–22. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simic M, et al. Gait modification strategies for altering medial knee joint load: a systematic review. Arthritis Care Res (Hoboken) 2011;63(3):405–26. doi: 10.1002/acr.20380. [DOI] [PubMed] [Google Scholar]
- 14.Zhao D, et al. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J Orthop Res. 2007;25(6):789–97. doi: 10.1002/jor.20379. [DOI] [PubMed] [Google Scholar]
- 15.Walter JP, et al. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J Orthop Res. 2010;28(10):1348–54. doi: 10.1002/jor.21142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim HJ, et al. Evaluation of predicted knee-joint muscle forces during gait using an instrumented knee implant. J Orthop Res. 2009;27(10):1326–31. doi: 10.1002/jor.20876. [DOI] [PubMed] [Google Scholar]
- 17.Herzog W, Longino D. The role of muscles in joint degeneration and osteoarthritis. J Biomech. 2007;40 Suppl 1:S54–63. doi: 10.1016/j.jbiomech.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Sasaki K, Neptune RR. Individual muscle contributions to the axial knee joint contact force during normal walking. J Biomech. 2010;43(14):2780–4. doi: 10.1016/j.jbiomech.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manal K, Buchanan TS. An electromyogram-driven musculoskeletal model of the knee to predict in vivo joint contact forces during normal and novel gait patterns. J Biomech Eng. 2013;135(2):021014. doi: 10.1115/1.4023457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gardinier ES, et al. Gait and neuromuscular asymmetries after acute anterior cruciate ligament rupture. Med Sci Sports Exerc. 2012;44(8):1490–6. doi: 10.1249/MSS.0b013e31824d2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buchanan TS, et al. Neuromusculoskeletal modeling: estimation of muscle forces and joint moments and movements from measurements of neural command. J Appl Biomech. 2004;20(4):367–95. doi: 10.1123/jab.20.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gardinier ES, et al. Minimum detectable change for knee joint contact force estimates using an EMG-driven model. Gait Posture. 2013;38(4):1051–3. doi: 10.1016/j.gaitpost.2013.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Butler RJ, et al. Gait mechanics after ACL reconstruction: implications for the early onset of knee osteoarthritis. Br J Sports Med. 2009;43(5):366–70. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 24.Creaby MW, et al. Dynamic knee loading is related to cartilage defects and tibial plateau bone area in medial knee osteoarthritis. Osteoarthritis Cartilage. 2010;18(11):1380–5. doi: 10.1016/j.joca.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 25.Bennell KL, et al. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis. 2011;70(10):1770–4. doi: 10.1136/ard.2010.147082. [DOI] [PubMed] [Google Scholar]