Abstract
Syphilis has existed for millenni, but its epidemiology was only recently linked to men who have sex with men (MSM) after the introduction of penicillin in the 1940s; the syphilis epidemic became concentrated within the MSM community in subsequent decades. The HIV/AIDS epidemic in the 1980s led to a surge of new syphilis cases and revealed the potentiation between HIV and syphilis, as evidenced by a shift in the natural history of neurosyphilis. In response, MSM revolutionised their sexual behaviour by implementing community-driven seroadaptive strategies to stem HIV transmission. The Centers for Disease Control in the US called for the elimination of syphilis in the late 1990s since the rates had fallen sharply but this effort was overtaken by a resurgence of global outbreaks among MSM in the 2000s, many of which were linked to methamphetamine use and sexual networking websites. Syphilis remains highly prevalent today, especially among MSM and individuals infected with HIV, and it continues to present a significant public health conundrum. Innovative syphilis prevention strategies are warranted. MSM engaging in high-risk behaviour such as condomless anal receptive intercourse, sex with multiple partners or recreational drug use should be routinely screened for syphilis infection; they should also be counselled about the limits of seroadaptive behaviours and HIV pre-exposure prophylaxis as they relate to syphilis transmission.
Introduction
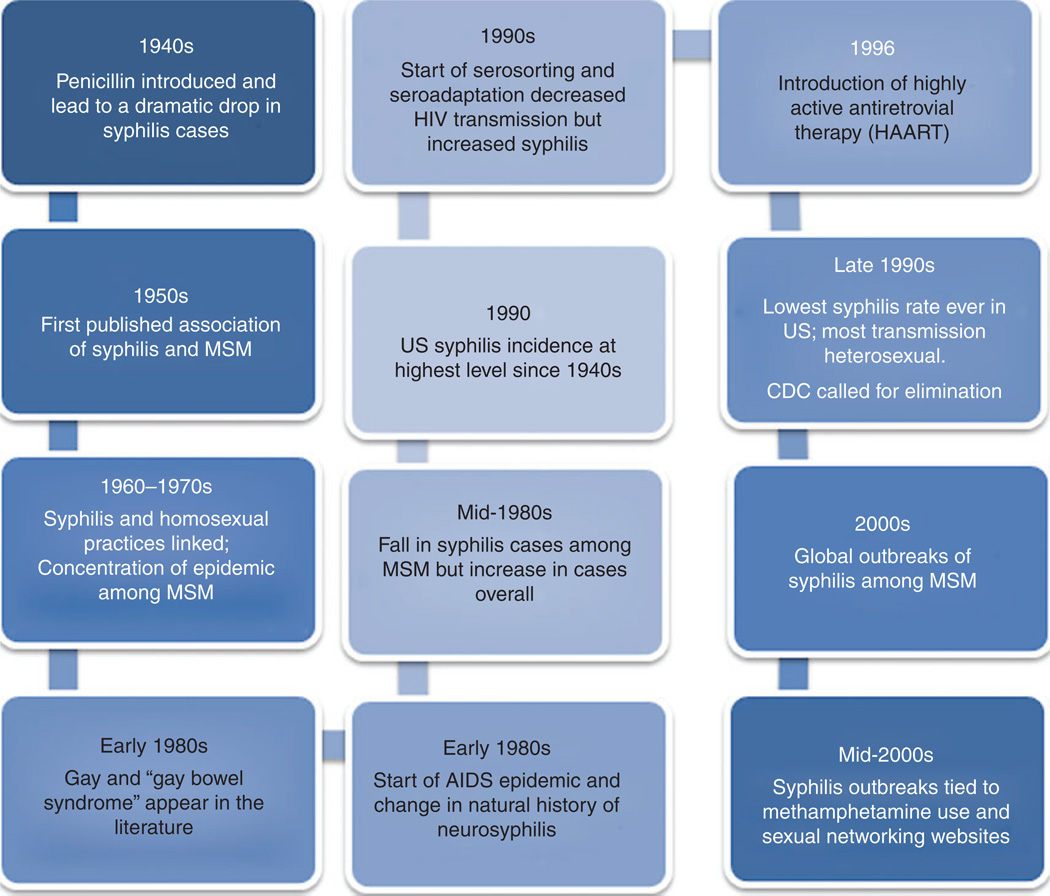
Although syphilis has existed in humans for millennia,1 it was described in more recent scientific literature in the early 19th century, with case reports about successful treatment approaches that did not include mercury.2 The introduction of penicillin in the 1940s3 decreased the long-term perception of syphilis as a principal public health scourge.4 The later development of benzathine penicillin G led to a drastic decrease in syphilis incidence in the US and other industrialised countries, from 76 per 100 000 population in 1945 to 4 per 100 000 population in 1955–57.5 The first association of syphilis with the ‘esoteric male’ and, presumably, other men who have sex with men (MSM) occurred in the 1950s.6 By the end of the decade, an analysis in New York City7 and a survey of West Coast metropolitan cases linked homosexuality and venereal diseases.8 At that time, ‘homosexual acts’ were ‘prohibited by law and punishable as felonic’ with 15 years for ‘oral copulation’ and ‘life imprisonment for sodomy’ in California.8 It was acknowledged more widely that syphilis was spread via homosexual relations in the early 1960s8,9 when two clinics in London reported that the majority of men with early syphilis ‘admitted’ homosexual exposure.10
Syphilis and homosexuality (Fig. 1)
Fig. 1.
Timeline of key events in the syphilis epidemic from 1940 to the present. MSM, men who have sex with men; CDC, Centers for Disease Control and Prevention.
Once it was recognised that syphilis and homosexual practices were strongly associated in the 1970s, public health efforts to characterise and address the syphilis epidemic among homosexuals were undertaken.11–14 As the epidemic became concentrated among MSM, some even questioned whether the long-term practice of premarital syphilis screening remained important.15 Rates of syphilis tripled during the 1960s and 1970s as the male-to-female ratio of infections also increased.5 During the 1970s, the percentage of men diagnosed with syphilis who reported at least one male sexual partner increased from 38% to 70%,16 although it is hard to be sure whether this increase primarily represented a change in behaviour or more accurate reporting as societal acceptance of alternative sexual preferences became better tolerated.
Due to its high transmission efficiency, syphilis infections occurred in diverse MSM subgroups reporting a wide spectrum of sexual behaviours. Relative to HIV, syphilis is much easier to transmit, even via certain sexual behaviours, such as insertive or receptive oral sex, that were not associated with HIV transmission (as compared with receptive anal intercourse).17 As the incidence of syphilis among the MSM community snowballed, it became increasingly difficult to halt new infections; removing syphilis from the MSM community once it had arrived provided a great challenge because of its efficient transmissibility among MSM and high community prevalence.
By the late 1970s, screening efforts of high-risk individuals had moved beyond traditional medical clinics and extended into high-risk venues, such as bathhouses, and other places where men had sex with men.18 The term ‘gay’ started appearing in the medical literature in the early 1980s,19 reflecting increased understanding, if not acceptance, of alternative modes of sexual expression. Syphilis was found to be one of several causes of anorectal infections among homosexual men around the same time,20,21 earning its place among one of the aetiologies of the ‘gay bowel syndrome’ a non-specific term that pulled together clinical and pathological findings occurring with increasing frequency among homosexual men22–24 in the early 1980s.
According to the Centers for Disease Control and Prevention, the incidence of syphilis increased in the US from 9.4 cases per 100 000 population in 1977 (a relative low) to 14.6 per 100 000 in 1982, primarily due to MSM.25 The rate subsequently decreased to 14.1 per 100 000 in 1983, which has been attributed to response to the AIDS epidemic, including increased condom use and a decrease in the proportion of men who named other men as sexual partners.25
Syphilis, HIV and changes in sexual behaviour
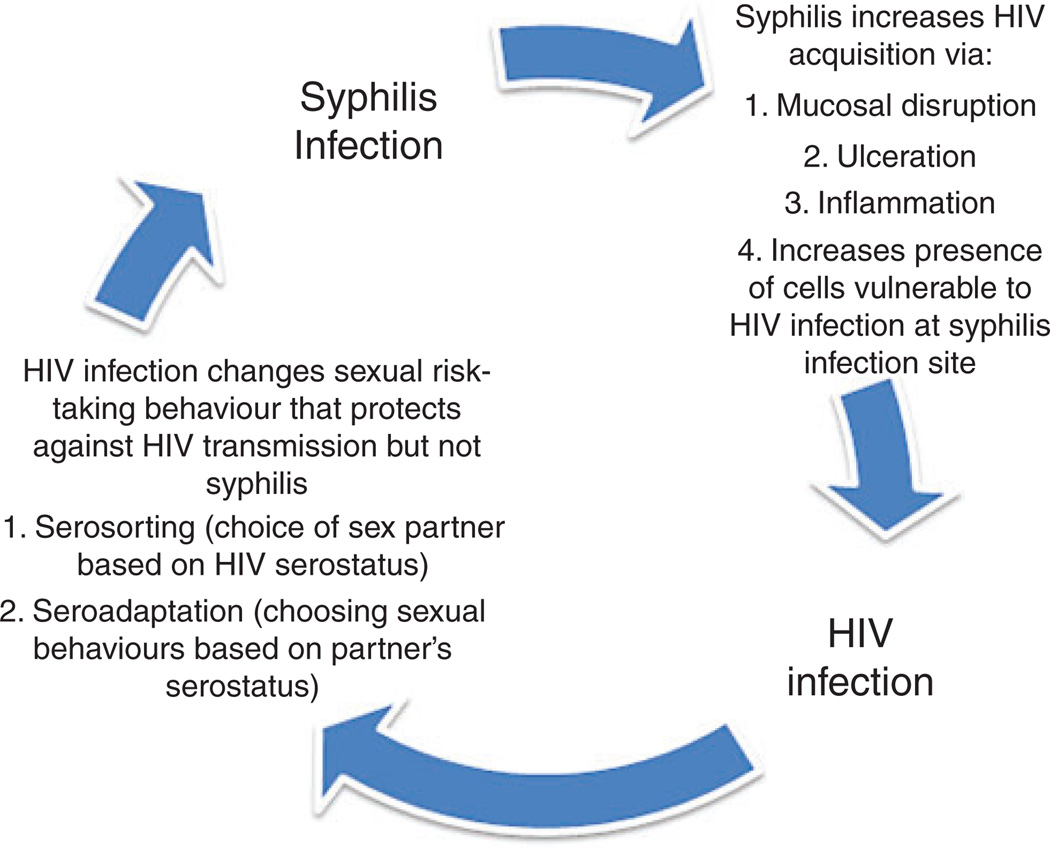
The HIV/AIDS epidemic has increased attention to syphilis as a public health problem, since co-infection can increase susceptibility to HIV and augment transmission efficiency, and untreated co-infection could lead to a severe infection with catastrophic neurological impacts.26 Prior to the advent of the AIDS epidemic in MSM, the incidence of neurosyphilis – a consequence of untreated syphilis that had previously occurred in ~7% of untreated cases27 – had decreased because of early penicillin treatment.28 The decline in cases of neurosyphilis had been attributed to early antibiotic administration either ‘intentionally or inadvertently’ and to the ‘low propensity of the disease to progress to neurosyphilis.’28 However, the HIV epidemic changed the natural history of neurosyphilis, resulting in earlier expression of neurological disease, suggesting an interaction between HIV and syphilis (Fig. 2). The immunodeficient state caused by HIV infection before the advent of highly active antiretroviral therapy reduced the natural immunological response to syphilis.28,29 This synergistic interaction led to diagnostic and therapeutic changes in clinical practice, including increased use of lumbar punctures in syphilis–HIV co-infected asymptomatic patients, regardless of the duration of syphilis or the presence of neurological symptoms, as well as increased HIV testing among those presenting with syphilis.28 Thus some of the reports of increasing prevalence of syphilis–HIV co-infection may be due to ascertainment biases.
Fig. 2.
Inter-relationships of syphilis infection and HIV infection.
With the rise of the AIDS epidemic, the importance of screening for HIV among individuals presenting to sexually transmissible infection (STI) clinics became paramount. It was observed that HIV seropositivity was associated with a history of syphilis and that this association was independent of the number and type of reported sexual partners, raising the possibility that disruption in the skin or mucosa, secondary to an asymptomatic gumma, could have been important in the transmission of HIV.30,31 By 1987, the incidence of primary and secondary syphilis had peaked at 14.6 cases per 100 000 population, reflecting a 25% increase from 1986, with the greatest increases seen in racial and ethnic minority populations.32 Interestingly, among MSM, the incidence of syphilis continued to decline and this was thought to be due to changes in sexual behaviour related to HIV prevention campaigns,33 which were hoped to control the spread of HIV.32,34 One study of homosexual men in Amsterdam tested for HIV for the first time in the mid-1980s demonstrated a fall in HIV incidence over time, even though the men had not received prior counselling on HIV prevention.35
The fall and subsequent rise in syphilis among MSM
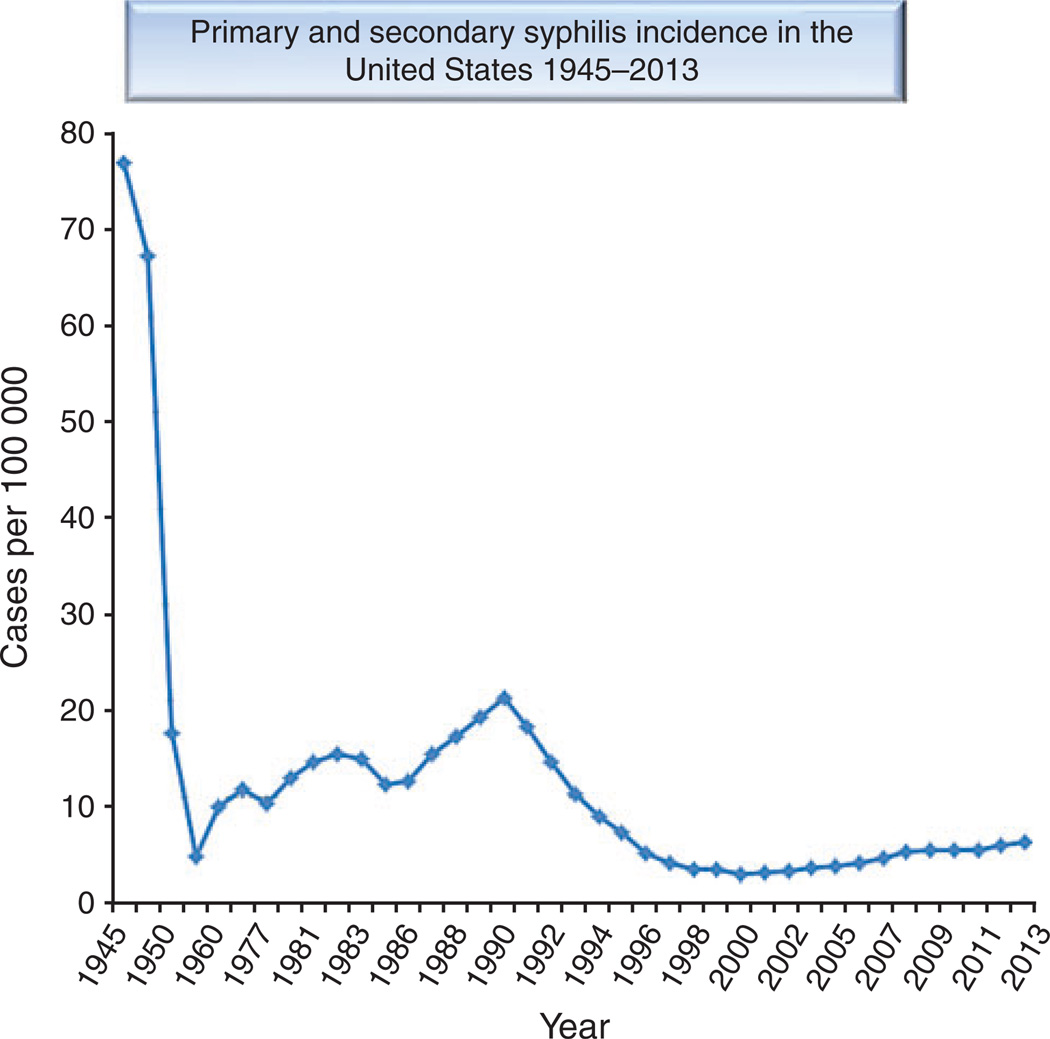
The slope of the decline of syphilis cases seen in the early to mid-1980s rebounded at the end of the decade because of resurgence in high-risk MSM sexual behaviour.36,37 Overall, between 1981 and 1989, the incidence of primary and secondary syphilis in the US increased 34% from 13.7 to 18.4 cases per 100 000 population (Fig. 3). The epidemic among White men, however, decreased dramatically (a 69% drop between 1982 and 1989) and was attributed to the fall of cases within the White MSM community.38,39 A similar decrease occurred early on among Black MSM but this trend reversed in 1986 at the same time that the incidence among White MSM continued to fall.40 What led to stark differences in the incidence of syphilis between White and Black MSM remains unclear, but reporting bias (Blacks may be more likely to be seen in public clinic with better reporting practices), disparities in healthcare access or use, or variations in sexual practices have been proposed as possible explanations.40 In 1990, the annual incidence of primary and secondary syphilis reached its highest level in the US since the 1940s. The surge in syphilis cases was seen in certain other regions as well, such as in Russia and former Soviet states.41,42 However, it should be noted that some of the individuals who were part of the new syphilis epidemic were heterosexual men and women, whose risk may have been primarily due to the use of crack cocaine or transactional sex, either by the individuals or by their partners. 43
Fig. 3.
Primary and secondary syphilis incidence in the United States, 1945–2013.
Norms regarding safer sexual behaviour changed among many MSM in the 1990s as part of a shift in community perceptions regarding the severity of the HIV/AIDS epidemic,44 resulting in an increase in anal sex and a decrease in condom usage.45 Seroadaptive practices such as serosorting (selection of sexual partners based on reported HIV serostatus) or seropositioning (focussing on specific practices with partners based on serostatus perceptions) could decrease HIV transmission, even while increasing STIs including syphilis, since HIV-infected MSM selecting only other HIV-infected partners for condomless anal sex, or engaging in only insertive or receptive oral sex, could transmit syphilis without transmitting HIV.46 In England and Wales, syphilis incidence fell to a low in the mid-1990s but then started to rise.47 In 1997, US syphilis incidence was at its lowest rate: 3.2 cases per 100 000 population48 and most of the transmissions in the US occurred in urban heterosexual Blacks, particularly in the South.49 This trend continued through 1999, when the number and rate of primary and secondary syphilis were at the lowest reported level in the US.50 The US Centers for Disease Control and Prevention called for a syphilis elimination campaign.51
Despite progress in the elimination of syphilis among heterosexuals in the US, MSM remained difficult to reach in the next decade.52 A large syphilis outbreak occurred among MSM in southern California in 2000, where the proportion of all reported syphilis cases occurring in MSM increased from 26% to 51% within 1 year. Behavioural risks included anonymous sex, frequenting bathhouses, meeting partners on the Internet, intimate contact with sex workers, condomless sex and using crystal methamphetamine53 (which decreases inhibitions, increases sexual pleasure and increases the likelihood of engaging in condomless sex).54,55 Use of geosocial networking phone apps such as Grindr to meet sexual partners has been associated with a greater odds of testing positive for some STIs.56 A report of the reintroduction of syphilis among MSM in King County, Washington, suggested that anonymous sex among MSM with many partners was the primary driver.45
Similar syphilis outbreaks among MSM occurred in the 2000s in other major US cities, including Los Angeles, Chicago, Seattle and New York, with similar reports from England, Wales, and Italy,57–60 particularly in MSM with HIV co-infection.59 The rates of syphilis have subsequently increased each year since 2001 (Fig. 3), with MSM accounting for an increasing proportion of new cases, whereas syphilis rates among women have declined globally. Whereas heterosexual transmission was responsible for most of the cases in the 1990s, by early 2003, the majority of new cases in the US were occurring among MSM,43 especially among Black and Latino MSM, who had an 8-fold and 2.4-fold increase, respectively, in syphilis rates compared with White MSM during the same period.61 In the same report, two-thirds of recently acquired syphilis infections in the US affected MSM, with the largest change in new infections occurring among young Black and Latino MSM aged 15–19 years. This trend has persisted, with syphilis rates increasing among men of all ages and ethnicities in the US, with an accelerated increase among MSM,62 especially Black MSM.63 These concerning trends have also been seen globally.64
The resurgence of syphilis and other STIs among MSM in recent years have spawned concern about a resurgence of HIV among MSM.62,65–74 This was attributed to ‘an abandonment of safer sex practices among some gay and bisexual men’75, with concerns about an emerging syndemic (i.e. synergistic epidemics of HIV, STIs, substance use, etc.).76 More recently, incarcerated MSM and those with repeated syphilis infections have been the foci of enhanced HIV screening and prevention efforts.77,78 MSM with new syphilis infections are more likely to report methamphetamine use and use of the Internet to meet sex partners on sexual networking websites,56 suggesting that these individuals may benefit from routine HIV and STI testing, as well as culturally tailored counselling.79 Given the increased HIV and syphilis prevalence of users of social networking sites, these virtual venues may provide an invaluable tool to notify partners of syphilis or HIV exposures.80
Modern-day challenges and strategies
The epidemiology of syphilis has shifted over time, consistent with improvements in diagnostics and the introduction of penicillin, HIV infection and the evolution of sexual behaviour; however, syphilis continues to present a significant public health infectious diseases conundrum. Today, syphilis is highly prevalent among MSM and individuals infected with HIV, and the prevalence of infection is on the rise. Many infections remain occult and asymptomatic; hence the need to improve screening programs among populations at highest risk. Creative testing strategies such as Internet outreach,81 opt-out testing,82 or increasing the frequency of screening rather than increasing the proportion screened83 offer some promise to increase the rates of early diagnosis.82,84 MSM engaging in condomless anal receptive intercourse, particularly if they have sex with multiple partners, use drugs such as crystal methamphetamine, erectile dysfunction drugs for recreational use85 or intravenous drugs, should be routinely screened for syphilis infection (i.e. every 3–6months).86 Individuals diagnosed with syphilis infection should be counselled about the limits of serosorting and other seroadaptive behaviours as they pertain to syphilis transmission (e.g. oral sex is not safer sex for syphilis). HIV-uninfected MSM with syphilis should be educated about newer HIV prevention modalities, such as oral pre-exposure prophylaxis, as a diagnosis of syphilis is strongly associated HIV acquisition.87 However, since pre-exposure prophylaxis will not protect against syphilis, MSM using it should be regularly evaluated for syphilis and other treatable STIs. The significant prevalence of syphilis among MSM can be decreased through culturally tailored prevention counselling, education about pre-exposure prophylaxis and repetitive screening for those who continue to engage in behaviours known to transmit syphilis and HIV.
Footnotes
Conflicts of interest
None declared.
References
- 1.Idsoe O, Guthe T. The rise and fall of the treponematoses. I. Ecological aspects and international trends. in venereal syphilis. Br J Vener Dis. 1967;43:227–243. doi: 10.1136/sti.43.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rose T. Observations on the treatment of syphilis, with an account of several cases of that disease in which a cure was effected without the use of mercury. Med Chir Trans. 1817;8:347–424. doi: 10.1177/095952871700800116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahoney JF, Arnold RC, Sterner BL, Harris A, Zwally MR. Penicillin treatment of early syphilis: II. JAMA. 1984;251:2005–2010. doi: 10.1001/jama.251.15.2005. [DOI] [PubMed] [Google Scholar]
- 4.Parran T. Shadow on the land. New York: Reynal and Hitchcock; 1937. [Google Scholar]
- 5.Holmes KK. Azithromycin versus penicillin G benzathine for early syphilis. N Engl J Med. 2005;353:1291–1293. doi: 10.1056/NEJMe058161. [DOI] [PubMed] [Google Scholar]
- 6.Goodman H. The esoteric male as a focus for spread of venereal diseases. Acta Derm Venereol. 1957;37:483–488. [PubMed] [Google Scholar]
- 7.Goodman H. The male homosexual and venereal diseases; the homosexual male is a victim and transfer agent of venereal disease particularly syphilis in New York City; analyses of statistics of Annual Report of Magistrates, Courts, 1957, imply dangers of unwitting infection. Acta Derm Venereol. 1958;38:274–282. [PubMed] [Google Scholar]
- 8.Tarr JD, Lugar RR. Early infectious syphilis. Male homosexual relations as a mode of spread. Calif Med. 1960;93:35–37. [PMC free article] [PubMed] [Google Scholar]
- 9.Trice ER, Gayle S, Jr, Clark FA., Jr The transmission of early infectious syphilis through homosexual practices. Va Med Mon. 1960;87:132–134. [PubMed] [Google Scholar]
- 10.Jefferiss FJ. Homosexually-acquired venereal disease. Br J Vener Dis. 1966;42:46–47. doi: 10.1136/sti.42.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fluker JL. A 10-year study of homosexually transmitted infection. Br J Vener Dis. 1976;52:155–160. doi: 10.1136/sti.52.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thin RN, Smith DM. Some characteristics of homosexual men. Br J Vener Dis. 1976;52:161–164. doi: 10.1136/sti.52.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dans PE. The establishment of a university-based veneral disease clinic I: description of the clinic and its population. J Am Vener Dis Assoc. 1974;1:70–78. [PubMed] [Google Scholar]
- 14.Henderson RH. Improving sexually transmitted disease health services for gays: a national prospective. Sex Transm Dis. 1977;4:58–62. doi: 10.1097/00007435-197704000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Felman YM. Should premarital syphilis serologies continue to be mandated by law? JAMA. 1978;240:459–460. [PubMed] [Google Scholar]
- 16.Fichtner RR, Aral SO, Blount JH, Zaidi AA, Reynolds GH, Darrow WW. Syphilis in the United States: 1967–1979. Sex Transm Dis. 1983;10:77–80. doi: 10.1097/00007435-198304000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Peterman TA, Furness BW. The resurgence of syphilis among men who have sex with men. Curr Opin Infect Dis. 2007;20:54–59. doi: 10.1097/QCO.0b013e32801158cc. [DOI] [PubMed] [Google Scholar]
- 18.Judson FN, Miller KG, Schaffnit TR. Screening for gonorrhea and syphilis in the gay baths - Denver, Colorado. Am J Public Health. 1977;67:740–742. doi: 10.2105/ajph.67.8.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Darrow WW, Barrett D, Jay K, Young A. The gay report on sexually transmitted diseases. Am J Public Health. 1981;71:1004–1011. doi: 10.2105/ajph.71.9.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quinn TC, Corey L, Chaffee RG, Schuffler MD, Brancato FP, Holmes KK. The etiology of anorectal infections in homosexual men. Am J Med. 1981;71:395–406. doi: 10.1016/0002-9343(81)90167-4. [DOI] [PubMed] [Google Scholar]
- 21.Nazemi MM, Musher DM, Schell RF, Milo S. Syphilitic proctitis in a homosexual. JAMA. 1975;231:389. [PubMed] [Google Scholar]
- 22.Kazal HL, Sohn N, Carrasco JI, Robilotti JG, Delaney WE. The gay bowel syndrome: clinico-pathologic correlation in 260 cases. Ann Clin Lab Sci. 1976;6:184–192. [PubMed] [Google Scholar]
- 23.Heller M. The gay bowel syndrome: a common problem of homosexual patients in the emergency department. Ann Emerg Med. 1980;9:487–493. doi: 10.1016/s0196-0644(80)80310-6. [DOI] [PubMed] [Google Scholar]
- 24.Kang JY, Stiel D, Doe WF. Gay bowel syndrome: syphilis association. Med J Aust. 1980;2:523. doi: 10.5694/j.1326-5377.1980.tb100741.x. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) Atlanta: CDC; 1998. Syphilis – United States, 1983. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/00000381.htm [verified 6 November 2014]. [Google Scholar]
- 26.Gordon SM, Eaton ME, George R, Larsen S, Lukehart SA, Kuypers J, et al. The response of symptomatic neurosyphilis to high-dose intravenous penicillin G in patients with human immunodeficiency virus infection. N Engl J Med. 1994;331:1469–1473. doi: 10.1056/NEJM199412013312201. [DOI] [PubMed] [Google Scholar]
- 27.Clark EG, Danbolt N. The Oslo study of the natural history of untreated syphilis; an epidemiologic investigation based on a restudy of the Boeck–Bruusgaard material; a review and appraisal. J Chronic Dis. 1955;2:311–344. doi: 10.1016/0021-9681(55)90139-9. [DOI] [PubMed] [Google Scholar]
- 28.Johns DR, Tierney M, Felsenstein D. Alteration in the natural history of neurosyphilis by concurrent infection with the human immunodeficiency virus. N Engl J Med. 1987;316:1569–1572. doi: 10.1056/NEJM198706183162503. [DOI] [PubMed] [Google Scholar]
- 29.Pavis CS, Folds JD, Baseman JB. Cell-mediated immunity during syphilis. Br J Vener Dis. 1978;54:144–150. doi: 10.1136/sti.54.3.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quinn TC, Glasser D, Cannon RO, Matuszak DL, Dunning RW, Kline RL, et al. Human immunodeficiency virus infection among patients attending clinics for sexually transmitted diseases. N Engl J Med. 1988;318:197–203. doi: 10.1056/NEJM198801283180401. [DOI] [PubMed] [Google Scholar]
- 31.Stamm WE, Handsfield HH, Rompalo AM, Ashley RL, Roberts PL, Corey L. The association between genital ulcer disease and acquisition of HIV infection in homosexual men. JAMA. 1988;260:1429–1433. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Syphilis and congenital syphilis – United States, 1985–1988. MMWR Morb Mortal Wkly Rep. 1988;37:486–489. [PubMed] [Google Scholar]
- 33.Nicoll A, Hughes G, Donnelly M, Livingstone S, De Angelis D, Fenton K, et al. Assessing the impact of national anti-HIV sexual health campaigns: trends in the transmission of HIV and other sexually transmitted infections in England. Sex Transm Infect. 2001;77:242–247. doi: 10.1136/sti.77.4.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Continuing increase in infectious syphilis–United States. MMWR Morb Mortal Wkly Rep. 1988;37:35–38. [PubMed] [Google Scholar]
- 35.Evans BA, McLean KA, Dawson SG, Teece SA, Bond RA, MacRae KD, et al. Trends in sexual behaviour and risk factors for HIV infection among homosexual men, 1984–7. BMJ. 1989;298:215–218. doi: 10.1136/bmj.298.6668.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van den Hoek JA, van Griensven GJ, Coutinho RA. Indications for increase in unsafe sexual behavior in homosexual men in Amsterdam. Ned Tijdschr Geneeskd. 1990;134:1229–1230. [In Dutch] [PubMed] [Google Scholar]
- 37.Handsfield HH, Schwebke J. Trends in sexually transmitted diseases in homosexually active men in King County, Washington, 1980–1990. Sex Transm Dis. 1990;17:211–215. doi: 10.1097/00007435-199010000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Increases in primary and secondary syphilis–United States. MMWR Morb Mortal Wkly Rep. 1987;36:393–397. [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Continuing increase in infectious syphilis – United States. Arch Dermatol. 1988;124:509–510. doi: 10.1001/archderm.124.4.509. [DOI] [PubMed] [Google Scholar]
- 40.Rolfs RT, Nakashima AK. Epidemiology of primary and secondary syphilis in the United States, 1981 through 1989. JAMA. 1990;264:1432–1437. [PubMed] [Google Scholar]
- 41.Tichonova L, Borisenko K, Ward H, Meheus A, Gromyko A, Renton A. Epidemics of syphilis in the Russian Federation: trends, origins, and priorities for control. Lancet. 1997;350:210–213. doi: 10.1016/S0140-6736(97)01382-2. [DOI] [PubMed] [Google Scholar]
- 42.Linglöf T. Rapid increase of syphilis and gonorrhea in parts of the former USSR. Sex Transm Dis. 1995;22:160–161. doi: 10.1097/00007435-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Heffelfinger JD, Swint EB, Berman SM, Weinstock HS. Trends in primary and secondary syphilis among men who have sex with men in the United States. Am J Public Health. 2007;97:1076–1083. doi: 10.2105/AJPH.2005.070417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crepaz N, Hart TA, Marks G. Highly active antiretroviral therapy and sexual risk behavior: a meta-analytic review. JAMA. 2004;292:224–236. doi: 10.1001/jama.292.2.224. [DOI] [PubMed] [Google Scholar]
- 45.Williams LA, Klausner JD, Whittington WL, Handsfield HH, Celum C, Holmes KK. Elimination and reintroduction of primary and secondary syphilis. Am J Public Health. 1999;89:1093–1097. doi: 10.2105/ajph.89.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Truong HM, Kellogg T, Klausner JD, Katz MH, Dilley J, Knapper K, et al. Increases in sexually transmitted infections and sexual risk behaviour without a concurrent increase in HIV incidence among men who have sex with men in San Francisco: a suggestion of HIV serosorting. Sex Transm Infect. 2006;82:461–466. doi: 10.1136/sti.2006.019950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nicoll A, Hamers FF. Are trends in HIV, gonorrhoea, and syphilis worsening in western Europe? BMJ. 2002;324:1324–1327. doi: 10.1136/bmj.324.7349.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.St. Louis ME, Wasserheit JN. Elimination of syphilis in the United States. Science. 1998;281:353–354. doi: 10.1126/science.281.5375.353. [DOI] [PubMed] [Google Scholar]
- 49.Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men – Southern California, 2000. MMWR Morb Mortal Wkly Rep. 2001;50:117–120. [PubMed] [Google Scholar]
- 50.Centers for Disease Control and Prevention. Primary and secondary syphilis – United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50:113–117. [PubMed] [Google Scholar]
- 51.Syphilis elimination seen as good HIV prevention. Aids Alert. 1998;13:63–66. [PubMed] [Google Scholar]
- 52.Darrow WW, Biersteker S. Short-term impact evaluation of a social marketing campaign to prevent syphilis among men who have sex with men. Am J Public Health. 2008;98:337–343. doi: 10.2105/AJPH.2006.109413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men – southern California, 2000. JAMA. 2001;285:1285–1287. [PubMed] [Google Scholar]
- 54.Crosby GM, Stall RD, Paul JP, Barrett DC, Midanik LT. Condom use among gay/bisexual male substance abusers using the timeline follow-back method. Addict Behav. 1996;21:249–257. doi: 10.1016/0306-4603(96)00055-x. [DOI] [PubMed] [Google Scholar]
- 55.Chesney MA, Barrett DC, Stall R. Histories of substance use and risk behavior: precursors to HIV seroconversion in homosexual men. Am J Public Health. 1998;88:113–116. doi: 10.2105/ajph.88.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Beymer MR, Weiss RE, Bolan RK, Rudy ET, Bourque LB, Rodriguez JP, et al. Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles county. Sex Transm Infect. 2014;90:567–572. doi: 10.1136/sextrans-2013-051494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Poulton M, Dean GL, Williams DI, Carter P, Iversen A, Fisher M. Surfing with spirochaetes: an ongoing syphilis outbreak in Brighton. Sex Transm Infect. 2001;77:319–321. doi: 10.1136/sti.77.5.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lacey HB, Higgins SP, Graham D. An outbreak of early syphilis: cases from North Manchester General Hospital. Sex Transm Infect. 2001;77:311–313. doi: 10.1136/sti.77.5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Centers for Disease Control and Prevention. Primary and secondary syphilis among men who have sex with men – New York City, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:853–856. [PubMed] [Google Scholar]
- 60.Giuliani M, Palamara G, Latini A, Maini A, Di Carlo A. Evidence of an outbreak of syphilis among men who have sex with men in Rome. Arch Dermatol. 2005;141:100–101. doi: 10.1001/archderm.141.1.100. [DOI] [PubMed] [Google Scholar]
- 61.Su JR, Beltrami JF, Zaidi AA, Weinstock HS. Primary and secondary syphilis among black and Hispanic men who have sex with men: case report data from 27 states. Ann Intern Med. 2011;155:145–151. doi: 10.7326/0003-4819-155-3-201108020-00004. [DOI] [PubMed] [Google Scholar]
- 62.Patton ME, Su JR, Nelson R, Weinstock H. Primary and secondary syphilis – United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63:402–406. [PMC free article] [PubMed] [Google Scholar]
- 63.Mayer KH, Wang L, Koblin B, Mannheimer S, Magnus M, Del Rio C, et al. Concomitant socioeconomic, behavioral, and biological factors associated with the disproportionate HIV infection burden among Black men who have sex with men in 6 U.S. cities. PLoS ONE. 2014;9:e87298. doi: 10.1371/journal.pone.0087298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jin F, Prestage GP, Kippax SC, Pell CM, Donovan BJ, Kaldor JM, et al. Epidemic syphilis among homosexually active men in Sydney. Med J Aust. 2005;183:179–183. doi: 10.5694/j.1326-5377.2005.tb06989.x. [DOI] [PubMed] [Google Scholar]
- 65.Wolitski RJ, Valdiserri RO, Denning PH, Levine WC. Are we headed for a resurgence of the HIV epidemic among men who have sex with men? Am J Public Health. 2001;91:883–888. doi: 10.2105/ajph.91.6.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Doherty L, Fenton KA, Jones J, Paine TC, Higgins SP, Williams D, et al. Syphilis: old problem, new strategy. BMJ. 2002;325:153–156. doi: 10.1136/bmj.325.7356.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cox JH, Elliott E, Sivaprakasam V, Chima-Okereke C. Audit of the management of the syphilis outbreak in Herefordshire 2011–2013. Int J STD AIDS. 2014 doi: 10.1177/0956462414538771. [DOI] [PubMed] [Google Scholar]
- 68.Hakre S, Arteaga GB, Nunez AE, Arambu N, Aumakhan B, Liu M, et al. Prevalence of HIV, syphilis, and other sexually transmitted infections among MSM from three cities in Panama. J Urban Health. 2014;91:793–808. doi: 10.1007/s11524-014-9885-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jin F, Prestage GP, Zablotska I, Rawstorne P, Kippax SC, Donovan B, et al. High rates of sexually transmitted infections in HIV positive homosexual men: data from two community based cohorts. Sex Transm Infect. 2007;83:397–399. doi: 10.1136/sti.2007.025684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Centers for Disease Control and Prevention. Notes from the field: repeat syphilis infection and HIV coinfection among men who have sex with men – Baltimore, Maryland, 2010–2011. MMWR Morb Mortal Wkly Rep. 2013;62:649–650. [PMC free article] [PubMed] [Google Scholar]
- 71.Centers for Disease Control and Prevention. HIV and syphilis infection among men who have sex with men – Bangkok, Thailand, 2005–2011. MMWR Morb Mortal Wkly Rep. 2013;62:518–520. [PMC free article] [PubMed] [Google Scholar]
- 72.Sánchez C, Plaza Z, Vispo E, de Mendoza C, Barreiro P, Fernandez-Montero JV, et al. Scaling up epidemics of acute hepatitis C and syphilis in HIV-infected men who have sex with men in Spain. Liver Int. 2013;33:1357–1362. doi: 10.1111/liv.12212. [DOI] [PubMed] [Google Scholar]
- 73.Jakopanec I, Grjibovski AM, Nilsen O, Blystad H, Aavitsland P. Trends in HIV infection surveillance data among men who have sex with men in Norway, 1995–2011. BMC Public Health. 2013;13:144. doi: 10.1186/1471-2458-13-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Brosh-Nissimov T, Mor Z, Avramovich E, Katchman E, Avidor B, Mor O, et al. Syphilis outbreak among men who have sex with men, Tel Aviv, Israel, 2008–2009. Isr Med Assoc J. 2012;14:152–156. [PubMed] [Google Scholar]
- 75.Stephenson J. Syphilis outbreak sparks concerns. JAMA. 2003;289:974. doi: 10.1001/jama.289.8.974. [DOI] [PubMed] [Google Scholar]
- 76.O’Leary D. The syndemic of AIDS and STDS among MSM. Linacre Q. 2014;81:12–37. doi: 10.1179/2050854913Y.0000000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cohen SE, Chew NgRA, Katz KA, Bernstein KT, Samuel MC, Kerndt PR, et al. Repeat syphilis among men who have sex with men in California, 2002–2006: implications for syphilis elimination efforts. Am J Public Health. 2012;102:e1–e8. doi: 10.2105/AJPH.2011.300383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen JL, Callahan DB, Kerndt PR. Syphilis control among incarcerated men who have sex with men: public health response to an outbreak. Am J Public Health. 2002;92:1473–1474. doi: 10.2105/ajph.92.9.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chew NgRA, Samuel MC, Lo T, Bernstein KT, Aynalem G, Klausner JD, et al. Sex, drugs (methamphetamines), and the Internet: increasing syphilis among men who have sex with men in California, 2004–2008. Am J Public Health. 2013;103:1450–1456. doi: 10.2105/AJPH.2012.300808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hunter P, Oyervides O, Grande KM, Prater D, Vann V, Reitl I, et al. Facebook-augmented partner notification in a cluster of syphilis cases in Milwaukee. Public Health Rep. 2014;129:43–49. doi: 10.1177/00333549141291S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zou H, Wu Z, Yu J, Li M, Ablimit M, Li F, et al. Internet-facilitated, voluntary counseling and testing (VCT) clinic-based HIV testing among men who have sex with men in China. PLoS ONE. 2013;8:e51919. doi: 10.1371/journal.pone.0051919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Guy R, El-Hayek C, Fairley CK, Wand H, Carr A, McNulty A, et al. Opt-out and opt-in testing increases syphilis screening of HIV-positive men who have sex with men in Australia. PLoS ONE. 2013;8:e71436. doi: 10.1371/journal.pone.0071436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tuite AR, Fisman DN, Mishra S. Screen more or screen more often? Using mathematical models to inform syphilis control strategies. BMC Public Health. 2013;13:606. doi: 10.1186/1471-2458-13-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Callander D, Baker D, Chen M, Guy R. Including syphilis testing as part of standard HIV management checks and improved syphilis screening in primary care. Sex Transm Dis. 2013;40:338–340. doi: 10.1097/OLQ.0b013e31828052c5. [DOI] [PubMed] [Google Scholar]
- 85.Pantalone DW, Bimbi DS, Parsons JT. Motivations for the recreational use of erectile enhancing medications in urban gay and bisexual men. Sex Transm Infect. 2008;84:458–462. doi: 10.1136/sti.2008.031476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mansergh G, Flores S, Koblin B, Hudson S, McKirnan D, Colfax GN. Alcohol and drug use in the context of anal sex and other factors associated with sexually transmitted infections: results from a multicity study of high-risk men who have sex with men in the USA. Sex Transm Infect. 2008;84:509–511. doi: 10.1136/sti.2008.031807. [DOI] [PubMed] [Google Scholar]
- 87.Solomon MM, Mayer KH, Glidden DV, Liu AY, McMahan VM, Guanira JV, et al. Syphilis predicts HIV incidence among men and transgender women who have sex with men in a preexposure prophylaxis trial. Clin Infect Dis. 2014;59:1020–1026. doi: 10.1093/cid/ciu450. [DOI] [PMC free article] [PubMed] [Google Scholar]