Abstract
Background
Resilience has been linked to psychological adaptation to many challenging life events.
Objective
The goal was to examine three coping strategies - expressing positive emotions, positive reframing of the cancer experience, and cultivating a sense of peace and meaning in life - as potential mechanisms by which resilience translates to quality of life among women recently diagnosed with gynecological cancer.
Method
This cross-sectional study utilized baseline data from women diagnosed with gynecological cancer participating in an ongoing randomized clinical trial (N = 281; Mage = 55, 80% Caucasian). Participants completed measures of resilience, positive emotional expression, positive reappraisal, and cultivating a sense of peace and meaning, and quality of life. Univariate and multiple mediation analyses were conducted.
Results
Greater resilience was related to higher quality of life (p < .001). Multiple mediation analyses indicated that the coping strategies, as a set, accounted for 62.6% of the relationship between resilience and quality of life. When considered as a set, cultivating a sense of peace and meaning had the strongest indirect effect (b = .281, se = .073, p < .05).
Conclusion
The findings suggested that resilient women may report higher quality of life during gynecological cancer diagnosis because they are more likely to express positive emotions, reframe the experience positively, and cultivate a sense of peace and meaning in their lives.
Implications for Practice
Interventions promoting a sense of purpose in one’s life and facilitating expression of positive emotions may prove beneficial, particularly for women reporting higher levels of resilience.
Keywords: resilience, quality of life, coping, gynecological cancer
Resilience has become a major focus of research and clinical interventions in psychology over the past two decades 1–4. Resilience is thought to be a key characteristic of individuals that facilitates positive well-being in the face of the myriad negative life events that individuals face in their lives. 2,3 Resilience is a key construct in the broaden and build theory of positive emotions.4 Resilience facilitates positive ways of coping as a method of cultivating positive emotions.4 Resilience has been defined in a number of ways, including the ability to recover strength, spirits, and humor,5 the ability to bounce back and recover from stress, 6 the ability to adapt positively in the face of adversity,2 and the process of identifying or developing resources and strengths to flexibly manage stressors to gain a positive outcome, a sense of mastery, self-transcendence, and self-esteem.7 What these definitions have in common is the view that resilient individuals utilize and develop resources and skills to manage stressors that facilitate positive adaptation. Some researchers conceptualize resilience as a stable personality trait 1 or a set of stable personal characteristics such as perseverance, equanimity, humor, patience, faith, self-efficacy, optimism, and self-reliance.8,9 However, developmental psychologists and other behavioral scientists adopt a dynamic view of resilience.10,11 Dynamic conceptualizations suggest that resilience is a personal resource that develops and changes over one’s lifetime during and after developmental and other life challenges, depending upon how the individual handles these challenges.7,10,12,13 Supporting this dynamic conceptualization of resilience is the fact that resilience may increase over time6 and that resilience can be bolstered by specialized psychological interventions.14,15
According to the broaden and build theory of positive emotion, resilient individuals identify or develop resources and strengths to flexibly manage stressors.4 That is, they use specific cognitive, behavioral, and affective management strategies which match the demands of each situation to develop and/or maintain their resilience and regulate their affective response.11 Although there are a number of coping strategies that may be utilized, the present study focused on three strategies which may be most successful in maintaining quality of life in the face of life threatening illness, which is the stressor examined in the present study: positive emotional expression, positive reappraisal, and cultivating a sense of peace and meaning. Resilient individuals are more likely to express positive affect16 and will attempt to restore and/or maintain positive affect.12 Indeed, prior work has indicated that expression of positive emotions is one way that resilient individuals maintain psychological adjustment to other challenging situations.6,12,17,18 Second, resilient individuals are more likely to use specific cognitive strategies to assimilate a difficult life experience into their existing views. A key way of accomplishing this is to create beliefs about the positive aspects of an event 19 and/or reappraise the event in a less threatening way.20 Resilience has been associated with positive reappraisal in prior studies.21 In turn, positive reappraisal leads to better quality of life.22 Finally, resilient individuals employ cognitive and behavioral strategies to cultivate a sense of spiritual peace and purpose in life. Studies of college undergraduates11 and individuals coping with illnesses21 suggest that cultivating a sense of meaning and purpose is associated with resilience. Indeed, cultivating a sense of peace and meaning has been strongly associated with higher quality of life in a number of studies of individuals coping with serious illness23.
The goal of the present study was to examine resilience in a population of individuals dealing with a life-threatening illness, a new diagnosis of gynecological cancer. Gynecological cancer is typically marked by physical24,25 and psychosocial26 challenges. Women diagnosed with this disease are typically diagnosed when the disease is at an advanced stage and undergo highly ablative gynecological surgery followed by a series of chemotherapy and/or radiation treatments. Ultimately, these treatments are not successful in controlling the disease.27 Fears of recurrence,28 clinically-significant levels of psychological distress,29 and declining quality of life30 are relatively common. Achieving a better understanding of how these patients maintain some semblance quality of life in the face of such a difficult disease is an important area of study. Previous work has linked lower quality of life with younger age,31 lower education,32 and the use of specific coping resources, such as less positive reframing33 and greater disengagement and avoidant coping.34 However, compared with women facing other cancers, such as early stage breast cancer, relatively little is known about resilience as well as other factors contributing to quality of life in this patient population.
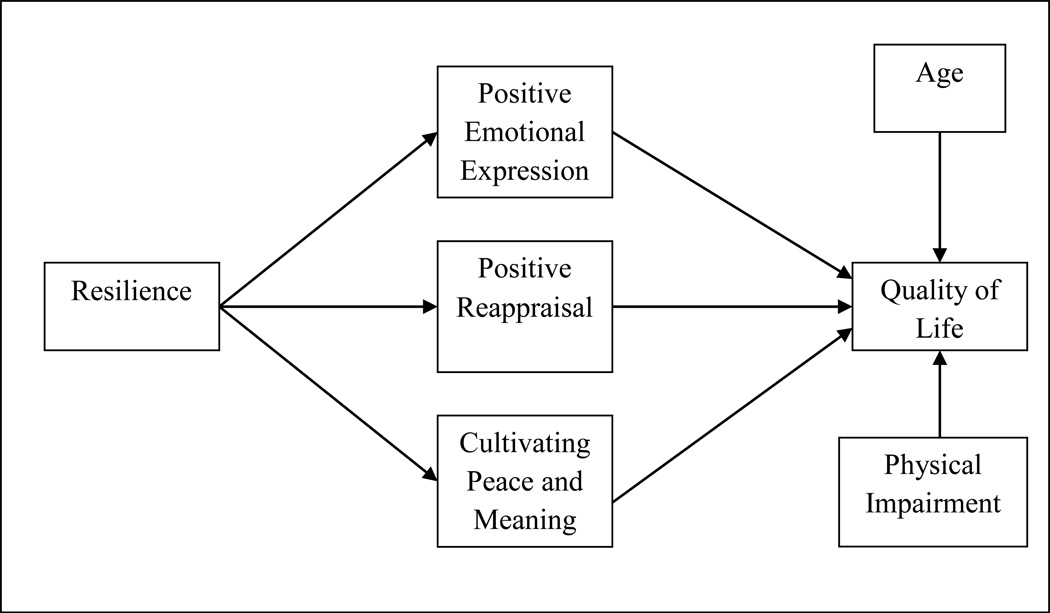
The present study had two aims. The first aim was to characterize resilience in this population because resilience has received little attention among women diagnosed with gynecological cancers. The second aim was to evaluate the associations between resilience and quality of life and to examine specific coping skills that resilient patients choose to maintain quality of life. As noted above, we evaluated three possible coping skills that resilient women may be more likely to utilize when dealing with a new diagnosis of gynecological cancer: more expression of positive emotions, greater use of positive reappraisal, and greater cultivating a sense of peace and meaning in their lives. It was hypothesized that patients endorsing greater resilience would be more likely to express positive emotions, engage in positive reappraisal, and cultivate a greater sense of inner peace and meaning, and that these strategies would be the key ways that resilience contributes to higher quality of life in this patient population. The proposed model is presented in Figure 1.
Figure.
Model of Resilience, Coping, and Quality of Life
Design and Methods
Sample and Setting
This study utilized baseline data from an ongoing randomized clinical trial (RCT) evaluating the efficacy of a two psychosocial interventions and usual care (Manne, unpublished data). The sample consisted of women with primary gynecological (ovarian, endometrial/uterine, cervical, vulvar, or fallopian tube) cancer undergoing medical treatment at seven hospitals in the northeastern United States. Study inclusion criteria for the RCT were: 18 years or older; diagnosed within the past six months at time of initial recruitment; Karnofsky Performance Status of 80 or above or an Eastern Cooperative Oncology Group (ECOG) score of 0 or 1; lived within a two-hour commuting distance from recruitment center; English speaking; and no hearing impairment.
Procedures
Eligible women were identified, sent a letter describing the study, and contacted by the research assistant via person or phone. Participants signed an informed consent document approved by an Institutional Review Board. The survey was mailed to participants’ with a stamped return envelope. Participants were paid $15 for completing the survey.
Of the 1095 eligible patients approached for the clinical trial, 288 (26%) consented and completed questionnaires. Of the 288, seven patients did not complete the resilience measure and could not be included in the present study. Thus, the final sample size was 281 (25.6% of those approached). Of the patients who provided reasons for refusal, the most common reasons were: the patient felt the distance to commute to intervention sessions was too long (15%), the patient would not benefit (10%), the patient felt too overwhelmed to participate (9%), or that the patient felt the study would take too much time (6%). Comparisons between study participants and refusers on the limited available data indicated that participants were younger (t (1056) = 7.2, p < .001, Mparticipants = 55, Mrefusers = 60.3 years) and diagnosed more recently (t (1082) = 5.3, p < .001, Mparticipants = 3.8 months, Mrefusers = 4.5 months). Refusal rates were significantly lower at two sites where nurse practitioners screened patients to identify those eligible (17% and 22%, respectively, compared to an average of 75% across the other five sites).
Measures
Resilience
Resilience was measured by Block and Block’s scale,35 which contains 14 items rated on a 4-point Likert scale (1 = does not apply at all to 4 =applies very strongly). Sample items include “I get over my anger at someone reasonably quickly” and “I quickly get over and recover from being startled.” Scores range from 14–56, with higher scores indicating greater resilience. The scale has been utilized in prior studies of adults.18 The scale has demonstrated internal consistency ranging from .69 to .88. 1,36 In the current study, Cronbach’s alpha was .79.
Positive emotional expression
Positive emotion expression is a 7-item subscale of the Emotional Expressiveness Questionnaire.37 Items are rated on a 5-point Likert scale ranging from 0 (never) to 4 (always). A sample item is “I laugh a lot.” Scores range from 0–28 with higher scores indicating greater positive emotional expression. Internal consistencies in previous work with this population were satisfactory (.76–.80)37. In the current study, Cronbach’s alpha was .76.
Positive reappraisal
The 4-item positive reappraisal subscale of the COPE was utilized.19 Participants rated on a 4-point scale the degree to which they relied upon positive reappraisal as a coping strategy to deal with their cancer. A sample item is “I’ve been trying to learn something from the experience.” This scale has been utilized in prior work with this populaion38. Scores range from 4–16, with higher scores indicating greater use of positive reappraisal. In the current study, Cronbach’s alpha was .84.
Cultivating a sense of peace and meaning
The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp) Peace and Meaning subscale was used.39 It contains eight items assessing the tendency to cultivate meaning, a sense of peace, and purpose in life. Items are rated on a 5-point Likert scale. Sample items include “I am able to reach down deep into myself for comfort” and “I feel a sense of purpose in my life.” The subscale ranges from 0 to 32, with higher scores indicating a greater sense of peace and meaning. The scale has good internal consistency (.81–.88)40 and has been used with cancer patients.40 In the current study, Cronbach’s alpha was .85.
Quality of life
The Functional Assessment of Cancer Therapy – General (FACT-G) 41 was used to assess quality of life (QOL). It is comprised of 27 items assessing well-being in four domains: physical (PWB), functional (FWB), social/family (SFWB), and emotional (EWB). PWB assesses the physical symptoms; FWB assesses the degree to which the person can participate and enjoy normal daily activities; SFWB assesses social support and communication, and EWB measures emotional response to illness. The domains are summed for a total score ranging from 0 to 108, with higher scores indicating greater QOL. The total and domain scores have good internal consistency among cancer patients, (.72–.85), and the instrument is well-validated41. In the current study, Cronbach’s alpha was .90.
Demographic data
Demographic data for the present study were obtained on the baseline survey and included age, race, income, education level, and marital status.
Medical data
Medical chart review captured primary cancer diagnosis, cancer stage, type of treatment, and time from diagnosis at the time the survey was completed.
Functional impairment
Functional impairment was assessed with the 26-item functional status subscale of the Cancer Rehabilitation Evaluation System (CARES).42 Participants rated difficulty during the past month from 0 (not at all) to 4 (very much). Scores range from 0–104 with higher scores indicating greater impairment. In the current study, Cronbach’s alpha was .92.
Statistical Analyses
Data were analyzed utilizing the Statistical Package for Social Sciences (SPSS), version 19. Descriptive statistics were computed for all variables. To determine the relationship between resilience, quality of life, and demographic and medical variables, correlational analyses were conducted for continuous variables and independent sample t-tests and one-way analysis of variance (ANOVA) were conducted for categorical variables. Only demographic and medical variables with statistically significant (p < .05) relationships with either resilience or quality of life were included in subsequent analyses as covariates. There was a small but statistically significant difference in resilience as a function of race, F(4,275) = 2.83, MSE = 39.50, p = .025. We created a dummy variable to contrast Caucasian participants against women of other races. Caucasian participants reported significantly higher resilience (M = 42.98, SD = 6.25) than participants who were not Caucasian (M = 40.49, SD = 6.44); t (279) = 2.67, p = .008. Three other variables were identified as having statistically significant correlations with either resilience or quality of life (older age, less functional impairment, and greater time since diagnosis). These variables were included as covariates in the mediation analyses.
Meditational analyses were conducted to estimate the total, direct, and indirect effects of the predictor (resilience) on the outcome (quality of life). Two approaches were taken for these mediation analyses, both of which used bootstrapping to estimate confidence intervals to test the indirect effects.43 The first approach examined the degree to which each proposed mediator (positive emotion expression, positive reappraisal, and cultivating peace and meaning) alone accounted for variance in the relationship between resilience and quality of life controlling for the four covariates. The second approach used a multiple mediator model47 that tested the extent to which the three proposed mediators as a set accounted for the resilience and quality of life relationship, again controlling for the covariates. The multiple mediator approach provides estimates of the extent to which each individual mediator showed indirect effects when controlling for the presence of the other mediators in the model. The Preacher and Hayes mediation macro47 was used to generate confidence intervals for the overall indirect effect as well as the unique (i.e., partial) indirect effects for each mediator.
Results
Sample Characteristics
Detailed description of demographic and medical data for participants is presented in Table 1. The sample was mostly Caucasian (80%), married (65%), and had attended at least some college (77%). The average age was 55 years (range= 23–78). More than half of the sample was diagnosed with ovarian cancer (58%), and the majority was diagnosed with stage III or IV disease (73.5%). The majority of participants were receiving chemotherapy at the time of survey completion (89%).
Table 1.
Demographic and Medical Data for Study Participants (N=281)
| Variable | n | % | M (SD) | Range |
|---|---|---|---|---|
| Age (years) | 54.8 (10.5) | 23–78 | ||
| Household income ($) | 141,327(251,000) | 1,200–75,000,000 | ||
| Race | ||||
| Caucasian/White | 224 | 80 | ||
| African American/Black | 34 | 12 | ||
| Hispanic/Latino | 10 | 4 | ||
| Asian/Pacific Islander | 6 | 2 | ||
| Other | 7 | 2 | ||
| Education Level | ||||
| < High school | 13 | 5 | ||
| High school graduate | 43 | 15 | ||
| Some college/trade school | 43 | 15 | ||
| College graduate | 88 | 31 | ||
| Graduate school/professional degree | 93 | 33 | ||
| Marital Status | ||||
| Married | 184 | 65.5 | ||
| Not married | 97 | 34.5 | ||
| Primary Cancer | ||||
| Ovarian | 165 | 59 | ||
| Endometrial/Uterine | 65 | 20 | ||
| Fallopian | 25 | 9 | ||
| Cervical | 13 | 5 | ||
| Peritoneal | 6 | 2 | ||
| More than one | 7 | 2 | ||
| Stage | ||||
| I | 45 | 16 | ||
| II | 21 | 7 | ||
| III | 130 | 46 | ||
| IV | 60 | 21 | ||
| Undifferentiated | 7 | 2 | ||
| Functional Impairment | 33.48 (20.19) | 0 – 89.4 | ||
| Months since diagnosis | 4.19 (1.65) | < 1 –9 |
Note. The mean and SD for income was computed excluding the outlying $75,000,000 outlier.
Descriptive Information on Resilience
Average levels of resilience were relatively high (M = 42.5, SD = 6.4, range = 22–56). The mean, standard deviation, and range for this sample were similar to figures reported in prior work with college undergraduates (M =42, SD = 6.41, range = 28–54).9 The average item score was 3.03 (SD = .45) on the 4-point Likert scale, which corresponded to “applies somewhat.” This average item score is very similar to that reported in prior work with female undergraduates (M = 3.04, SD = .36).40 The highest-rated item was “I am generous with my friends” (M = 3.4) and the lowest-rated item was, “I like to take different paths to familiar places.” (M = 2.65). Overall, this older and more ill population reported similar levels of resilience as younger, physically healthy populations.
Preliminary Analyses
The means, standard deviations, and bivariate correlations are presented in Table 2. Greater resilience was significantly associated with higher quality of life, r = .35, p < .001. In terms of disease-related factors, a greater length of time since diagnosis, r = −.15, p = .013 and greater functional impairment, r = −.17, p = .005 were associated with lower resilience. Caucasian women reported higher resilience, r = .16, p = .008. Resilience was not related to age, income, educational level, marital status, stage of cancer, or current medical treatment (chemotherapy, radiation). Older patients reported higher quality of life, r = .21, p = .001, and patients with less functional impairment reported higher quality of life, r = −.70, p < .001. Quality of life was not significantly related to any other demographic or medical variables. Only those variables significantly related to resilience (time since diagnosis, Caucasian/non Caucasian race) or quality of life (age, functional impairment) were included in subsequent analyses.
Table 2.
Descriptive Statistics and Correlations for Study Variables (N = 281)
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Resilience | |||||||||
| 2. Peace and Meaning | .29c | ||||||||
| 3. Positive Reappraisal | .31c | .37c | |||||||
| 4. Pos Emotion expression | .38c | .32c | .29c | ||||||
| 5. Quality of Life | .35c | .61c | .27c | .26c | |||||
| 6. Functional Impairment | −.17b | −.30c | −.09 | −.06 | −.70b | ||||
| 7. Age | .07 | .12a | −.07 | .04 | .18* | −.16 | |||
| 8. Months since Diagnosis | −.15a | .09 | .03 | −.08 | −.04 | .03 | .06 | ||
| 9. Caucasian | .16b | −.14a | −.09 | .02 | .05 | −.09 | .13a | −.17b | |
| M | 42.48 | 22.30 | 11.40 | 16.87 | 75.28 | 33.48 | 54.80 | 4.19 | |
| SD | 6.36 | 6.00 | 3.78 | 4.38 | 15.36 | 20.19 | 10.42 | 1.60 | |
| N | 281 | 279 | 281 | 281 | 280 | 281 | 281 | 281 | 281 |
Note. Caucasian is coded 1 if the participant was Caucasian, −1 otherwise.
p < .05,
p < .01,
p < .001.
Mediation Analyses
The first step of the analysis was to examine the degree to which each mediator alone accounted for the association between resilience and quality of life, controlling for the covariates. Table 3 shows the mediation analyses for each mediator. There was evidence of partial mediation for all three proposed mediators. The indirect for positive emotional expression was b = .177, 95% CI .092 to.309 and the total effect was b = .614, se = .113, p < .001. Positive emotional expression accounted for 29% of the relationship between resilience and quality of life. The indirect effect for positive reappraisal was smaller than that of positive emotional expression, with b = .124, 95% CI .052 to. 223, and a total effect of b = .614, se = .113, p < .001. Positive reappraisal explained 20% of the relationship between resilience and quality of life. Finally, for cultivating a sense of peace and meaning, the total effect was b = .607, se = .114, p < .001, and the indirect effect was b = .304, 95% CI = .161 to .474. Peace and meaning explained 50% of the association between resilience and quality of life.
Table 3.
Mediation Results for Single-Mediator Models Predicting Quality of Life as a Function of Resilience Controlling for Age, Race, Functional Impairment, and Time since Diagnosis
| Mediator Variable | N | Total Effect |
Direct Effect | Indirect Effect | Indirect 95% CI |
|---|---|---|---|---|---|
| Positive Emotional Expression | 211 | .614b | .438b | .177b | .09–.31 |
| Positive Reappraisal | 211 | .614b | .491b | .124a | .05–.22 |
| Cultivating Peace and Meaning | 207 | .607b | .303b | .304a | .16–.47 |
Note. Tabled values are unstandardized regression coefficients. Race was coded as Caucasian = 1, others = −1.
p < .05,
p < .01.
The second step was to examine the multiple mediator model (this model was based on N = 207, due to missing data). The model controlled for four covariates (time since diagnosis, Caucasian/non Caucasian race, age, functional impairment). When all three mediators were included in the model, the total effect of resilience on quality of life was b = .607, se = .114, p < .001. The direct effect was b = .227, se = .105, p = .032, and the total indirect effect was b = .380, se = .088, 95% CI .212 to. 556. As a set, the three proposed mediators accounted for 62.6% of the relationship between resilience and quality of life. Because the three mediators were correlated, their unique indirect effects were substantially smaller than their indirect effects as individual mediators. The mediating effect of cultivating a sense of peace and meaning was similar to the univariate analyses, with a statistically significant indirect effect of b = .281, se = .073, 95% CI .143 to .424. The indirect effect of positive reappraisal was smaller and not statistically significant, with b = .017, se = .032, 95% CI −.043 to .087. The indirect effect of positive emotion expression was smaller but statistically significant, b = .082, se = .040, 95% CI .002 to .165.
Discussion
This study evaluated the association between resilience and quality of life among women newly diagnosed with gynecological cancers. Levels of resilience were similar to those reported among younger undergraduates, and, overall, were relatively high. Patients reporting more resilience experienced a higher quality of life. The study enriches the literature on resilience by identifying possible strategies that resilient women diagnosed with cancer may utilize to maintain their quality of life during the cancer experience. Consistent with the broaden and build theory4 and our hypothesis that resilient patients would use specific positive coping skills which would cultivate positive emotions, resilient women reported using positive emotional expression, positive reappraisal, and cultivating a greater sense of inner peace and meaning in their lives. In addition, our findings were consistent with the hypothesis that these three coping strategies would facilitate better psychological adaptation as they accounted for more than half of the association between resilience and quality of life. When the three strategies were considered together, cultivating a sense of peace and meaning and positive emotional expression were significant mediators, and positive reappraisal was not a significant mediator. In this discussion, we will highlight the theoretical and clinical implications of these findings.
Positive Emotional Expression, Positive Reappraisal and Cultivating Peace and Meaning as Coping Strategies used by Resilient Patients to Maintain Quality of Life
When considered alone, each strategy mediated the association between resilience and quality of life. The fact that positive emotional expression functioned as a mediator is consistent with prior students that have demonstrated that positive emotional expression is a mechanism in maintaining psychological adaptation and consistent with the broaden and build theory of positive emotions 4,6,17,18 Positive emotional expression may help resilient individuals maintain better quality of life in numerous ways, including providing relief from a challenging situation.44 Positive reappraisal functioned as a mediator in the association between resilience and quality of life. There is substantial evidence that cognitive appraisals during a challenging situation impact psychological adaptation to the situation.45 Since resilience is related to greater cognitive flexibility,9 resilient patients may be more likely to engage in efforts to generate positive thoughts during the cancer experience and reframe events as less threatening. Positive appraisals may broaden existing resources and build resilience.4 When considered alone, cultivating peace and meaning in one’s life was the strongest mediator in the association between resilience and quality of life, accounting for half of the association between the two variables. Although many studies utilize slightly different conceptualizations of cultivating peace and meaning (e.g., spirituality, meaning making), there appears to be a consensus in the literature that it is an important coping strategy to facilitate psychological adaptation to life-threatening illness,23 including studies among ovarian cancer patients.23 Our study suggests that it is a coping strategy that is used by resilient patients and facilitates their quality of life.
Considering Positive Emotional Expression, Positive Reappraisal and Cultivating Peace and Meaning Together
Considering the coping strategies together provided a stronger test of the role of each in the ways that resilience contributes to quality of life. When examined together, cultivation of peace and meaning and positive emotional expression remained significant mediators in the association between resilience and quality of life. The fact that cultivating peace and meaning was the strongest mechanism for resilience’s association with quality of life may reflect the unique medical situation for this patient population diagnosed with an incurable cancer. Indeed, cultivating peace and meaning has been shown to be a protective factor among terminally ill cancer patients.46 Psychological interventions that focus on cultivating meaning have shown particular promise among late stage cancer patients,47 suggesting that cultivating a sense of peace and meaning may be a particularly important strategy for patients facing late stage disease.
The broaden and build theory as well as prior research suggests that resilient individuals are more likely to experience and express positive emotions when faced with challenges, and that positive emotion is a mechanism for adaptation to these challenges.4,17,18 Our findings supported the hypothesis that resilient women engaged in more expression of positive emotions and that the expression of positive emotions served as a mediator or mechanism for maintaining a better quality of life for resilient women. Prior studies have not included measures of cultivating peace and meaning when evaluating the association between resilience and positive emotional expression.17,18 Our study suggests that investigators may also wish to consider peace and meaning when evaluating how resilient individuals maintain a positive adaptation to stressors rather than focusing solely on the expression of positive emotions.
Demographic and Medical Correlates of Resilience
Few demographic and medical variables were correlated with resilience, which is consistent with prior research noting no differences in resilience among cancer patients based on age, disease stage, and treatment.48,49 One exception was that women completed the survey a longer period of time from diagnosis reported less resilience, indicating that resilience may possibly decline over time. If this finding is confirmed by longitudinal data, it is consistent with our conceptualization of resilience as a resource that may change over time.13 Longitudinal data are needed to determine whether there are reductions in resilience over the cancer trajectory, as women get sicker and may lose personal resources, and whether expression of positive emotion, positive reappraisal, and/or cultivating peace and meaning protect against this loss of resources. In addition, Caucasian patients reported higher resilience, which has not been shown in other studies. Future research should further investigate why this is the case.
Study Strengths and Limitations
This is the first study to explore possible mechanisms by which resilience may impact quality of life among cancer patients. Given the emphasis on quality of life in this population, a better understanding of the mechanisms underlying quality of life may assist in the development of effective psychological interventions to enhance psychological adaptation.
There are limitations to the study that should be taken into consideration. First, the study was cross-sectional and direction of causation cannot be determined. As has been pointed out by Cohn and colleagues,12 the experience of positive emotions may increase resilience over time. Some investigators evaluate the associations between resilience and coping in a different way by proposing that certain coping strategies contribute to greater resilience.50 Longitudinal research is needed to shed light on the causal ordering. Second, the acceptance rate of 25.6% is relatively low and may have resulted in a biased sample. For example, women who chose to participate in the study tended to be younger and diagnosed more recently than non-participants and thus our sample may have been less representative of the attitudes of older patients who were diagnosed for a longer period of time. Third, women completed the survey at home and returned it by mail. This procedure did not allow participants the opportunity to ask questions about the survey items unless they chose to contact the research staff for assistance. Fourth, the self-report measures used may be influenced by dispositional characteristics, such as optimism or neuroticism, which were not included. Fifth, the majority of the sample was Caucasian, well-educated, middle-class, and diagnosed with advanced stage cancer. Further research is needed with more diverse samples. Finally, the sample consisted of women who agreed to participate in a randomized clinical trial evaluating the efficacy of psychological interventions. There may be certain factors that differentiate patients who chose to participate. For example, women who chose to participate in the study tended to be younger and diagnosed more recently than non-participants. However, analyses including these factors (age and time since diagnosis) as covariates did not substantially change the results. It is possible that women who agreed to participate in the study are more likely to be coping well and/or see the benefit of a psychological intervention. Since a common reason for refusal was ‘feeling too overwhelmed’, we may not have captured some women who are particularly vulnerable to distress. Future research may include more heterogeneous sample of women diagnosed with gynecologic cancer.
Implications
From a conceptual standpoint, this study advances our understanding of how resilient individuals cope with a severe life stressor. Our findings bolster the broaden and build theory of positive emotions and the conceptualization of resilience as a personal resource because resilience was associated with quality of life via greater use of coping strategies whose purpose was to bolster positive thoughts, a positive attitude, and maintain positive affect. Given the negative association between time since diagnosis and resilience, future longitudinal research should evaluate whether resilient individuals ultimately rebound or are worn down by the diagnosis of a life-threatening disease. From a clinical standpoint, promoting a sense of purpose in one’s life and facilitating expression of positive emotions may prove beneficial, particularly for women reporting higher levels of resilience. Existing interventions that focus on these skills have shown promise in cancer populations, such as meaning-based interventions47. Further research may consider examining whether cultivating a sense of peace and meaning might bolster quality of life for less resilient people, or alternatively, could enhance resilience.
Acknowledgements
This work was funded by grant RO1 CA08566 awarded to Sharon L. Manne. The authors thank project managers Tina Gajda, Sara Frederick, and Shira Hichenberg and research study assistants Jaime Betancourt, Kaitlyn Smith, Joanna Crincoli, Katie Darabos, Glynnis McDonnell, Arielle's Schwerd, Kristen Sorice, Caitlin Scally, Sloan Harrison, and Amanda Viner, as well as the study participants, their oncologists, and the clinical teams at Rutgers Cancer Institute of New Jersey, Memorial Sloan Kettering Cancer Center, Fox Chase Cancer Center, Hospital of the University of Pennsylvania, Thomas Jefferson University, Morristown Medical Center, and Cooper University Hospital.
Footnotes
The authors have no funding or conflicts of interest to disclose.
References
- 1.Block J, Kremen AM. IQ and ego-resiliency: conceptual and empirical connections and separateness. J Pers Social Psych. 1996;70(2):349–361. doi: 10.1037//0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- 2.Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Devl. 2000;71(3):543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masten AS. Ordinary magic. Resilience processes in development. Am Psych. 2001;56(3):227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 4.Fredrickson BL. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist. 2001;56(3):218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson GE. The metatheory of resilience and resiliency. J Clin Psych. 2002;58(3):307–321. doi: 10.1002/jclp.10020. [DOI] [PubMed] [Google Scholar]
- 6.Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Social Psych. 2004;86(2):320–333. doi: 10.1037/0022-3514.86.2.320. (2004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haase J. The components of courage in chronically ill adolescents. Adv Nurs Sci. 1987;9:64–80. doi: 10.1097/00012272-198701000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Connor KM, Davidson JR. Development of a new resilience scale: the Connor Davidson Resilience Scale (CD-RISC) Depr Anx. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 9.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Measure. 1993;1(2):165–178. [PubMed] [Google Scholar]
- 10.Masten AS. Resilience in individual development: Successful adaptation despite risk and adversity. In: Wang MC, E Gordon, editors. Educational resilience in inner city America: Challenges and prospects. Hillsdale, NJ: Erlbaum; 1994. pp. 3–25. [Google Scholar]
- 11.Smith BW, Tooley E, Christopher PJ, Kay VS. Resilience as the ability to bounce back from stress: A neglected personal resource. The Journal of Positive Psycholo. 2010;5(3):166–176. [Google Scholar]
- 12.Cohn MA, Fredrickson BL, Brown SL, Mikels JA, Conway AM. Happiness unpacked: positive emotions increase life satisfaction by building resilience. Emotion. 2009;9(3):361–368. doi: 10.1037/a0015952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychological Science. 2000;13(2):172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- 14.Grant AM, Curtayne L, Burton G. Executive coaching enhances goal attainment resilience and workplace well-being: a randomized controlled study. Journal of Positive Psychology. 2009;4(5):396–407. [Google Scholar]
- 15.Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. Journal of American College Health. 2008;56(4):445–453. doi: 10.3200/JACH.56.44.445-454. [DOI] [PubMed] [Google Scholar]
- 16.Tugade MM, Fredrickson BL, Barrett LF. Psychological resilience and positive emotional granularity: examining the benefits of positive emotions on coping and health. Journal of Personality. 2004;72(6):1161–1190. doi: 10.1111/j.1467-6494.2004.00294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th 2001. Journal of Personality and Social Psychology. 2008;84(2):365–376. doi: 10.1037//0022-3514.84.2.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience positive emotions and successful adaptation to stress later in life. Journal of Personality and Social Psychology. 2006;91:730–749. doi: 10.1037/0022-3514.91.4.730. [DOI] [PubMed] [Google Scholar]
- 19.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 20.Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annual Review of Clinical Psychology. 2005;1:255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- 21.Smith BW, Zautra AJ. Vulnerability and resilience in women with arthritis: test of a two-factor model. Journal of Consulting and Clinical Psychology. 2005;76(5):799–810. doi: 10.1037/0022-006X.76.5.799. [DOI] [PubMed] [Google Scholar]
- 22.Manne S, Rini C, Rubin S, Rosenblum N, Bergman C, Edelson M, Rocereto T. Long-term trajectories of psychological adaptation among women diagnosed with gynecological cancers. Psychosomatic Medicine. 2008;70(6):677–687. doi: 10.1097/PSY.0b013e31817b935d. doi: PSY0b013e31817b935d [pii]101097/PSY0b013e31817b935d. [DOI] [PubMed] [Google Scholar]
- 23.Simonelli LE, Fowler J, Maxwell GL, Andersen BL. Physical sequelae and depressive symptoms in gynecologic cancer survivors: meaning in life as a mediator. Annals of Behavioral Medicine. 2008;35(3):275–284. doi: 10.1007/s12160-008-9029-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson NJ, Hacker ED. Fatigue in women receiving intraperitoneal chemotherapy for ovarian cancer: a review of contributing factors. Clinical Journal of Oncology Nursing. 2008;12(3):445–454. doi: 10.1188/08.CJON.445-454. [DOI] [PubMed] [Google Scholar]
- 25.Chun N. A structural equation model on sexual function in women with gynecologic cancer. Journal of Korean Academic Nursing. 2008;38(5):639–648. doi: 10.4040/jkan.2008.38.5.639. [DOI] [PubMed] [Google Scholar]
- 26.Hodgkinson K, Butow P, Fuchs A, Hunt GE, Stenlake A, Hobbs KM, Wain G. Long-term survival from gynecologic cancer: psychosocial outcomes supportive care needs and positive outcomes. Gynecologic Oncology. 2007;104(2):381–389. doi: 10.1016/j.ygyno.2006.08.036. [DOI] [PubMed] [Google Scholar]
- 27.American Cancer Society. Cancer Facts and Figures. 2013 Retrieved from http://wwwcancerorg/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845pdf on January 9 2014.
- 28.Myers S, Manne SL, Kissane D, Ozga M, Kashy D, Rubin S, Heckman C, Rosenblum N, Morgan M, Graff J. Social-cognitive processes associated with fear of recurrence among women newly diagnosed with gynecological cancers. Gynecologic Oncology. 2013;128(1):120–127. doi: 10.1016/j.ygyno.2012.10.014. PMCID: PMC3534914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norton TR, Manne SL, Rubin S, Carlson J, Hernandez E, Edelson MI, Bergman C. Prevalence and predictors of psychological distress among women with ovarian cancer. Journal of Clinical Oncology. 2004;22(5):919–926. doi: 10.1200/JCO.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 30.Wenzel L, Vergote I, Cella D. Quality of life in patients receiving treatment for gynecologic malignancies: special considerations for patient care. International Journal of Gynaecology Obstetrics 83 Supply. 2003;1:211–229. doi: 10.1016/s0020-7292(03)90123-8. [DOI] [PubMed] [Google Scholar]
- 31.Canada AL, Parker PA, de Moor JS, Basen-Engquist K, Ramondetta LM, Cohen L. Active coping mediates the association between religion/spirituality and quality of life in ovarian cancer. Gynecologic Oncology. 2006;101(1):102–107. doi: 10.1016/j.ygyno.2005.09.045. [DOI] [PubMed] [Google Scholar]
- 32.Miller BE, Pittman B, Case D, McQuellon RP. Quality of life after treatment for gynecologic malignancies: a pilot study in an outpatient clinic. Gynecologic Oncology. 2002;87(2):178–184. doi: 10.1006/gyno.2002.6812. [DOI] [PubMed] [Google Scholar]
- 33.Lutgendorf SK, Anderson B, Ullrich P, Johnsen EL, Buller RE, Sood AK, Ritchie J. Quality of life and mood in women with gynecologic cancer: A one year prospective study. Cancer. 2002;94(1):131–140. doi: 10.1002/cncr.10155. [DOI] [PubMed] [Google Scholar]
- 34.Costanzo ES, Lutgendorf SK, Rothrock NE, Anderson B. Coping and quality of life among women extensively treated for gynecologic cancer. Psychooncology. 2006;15(2):132–142. doi: 10.1002/pon.930. [DOI] [PubMed] [Google Scholar]
- 35.Block JH, Block J. The role of ego-control and ego-resiliency in the organization of behavior. In: Collins WA, editor. The Minnesota Symposia on Child Psychology. Hillsdale NJ: Erlbaum; 1980. pp. 39–101. [Google Scholar]
- 36.Letzring TD, Block J, Funder DC. Ego-control and ego-resiliency: Generalization of self-report scales based on personality descriptions from acquaintances clinicians and the self. Journal of Research Personality. 2005;39(4):395–422. [Google Scholar]
- 37.King LA, Emmons RA. Conflict over emotional expression: psychological and physical correlates. Journal of Personality and Social Psychology. 1990;58(5):864–877. doi: 10.1037//0022-3514.58.5.864. [DOI] [PubMed] [Google Scholar]
- 38.Manne SL, Rubin S, Edelson M, Rosenblum N, Bergman C, Hernandez E, Winkel G. Coping and communication-enhancing intervention versus supportive counseling for women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology. 2007;75(4):615–628. doi: 10.1037/0022-006X.75.4.615. doi: 2007-11558-010 [pii] 101037/0022-006X754615. [DOI] [PubMed] [Google Scholar]
- 39.Peterman AH, Fitchett G, Brady MJ, Pharm L, Cella D. Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy-spiritual well-being scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 40.Whitford HS, Olver IN. The multidimensionality of spiritual wellbeing: Peace meaning and faith and their association with quality of life and coping in oncology. Psychooncology. 2012;21:602–601. doi: 10.1002/pon.1937. [DOI] [PubMed] [Google Scholar]
- 41.Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Journal of Clinical Oncology. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 42.Schag C, Heinrich R. CARES: Cancer Rehabilitation Evaluation System. Santa Monica CA: Cares Consultants; 1988. [Google Scholar]
- 43.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavioral Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 44.Lazarus RS, Kanner AD, Folkman S. Emotions: A cognitive phenomenological analysis. In: Plutchik R, Kellerman H, editors. Theories of Emotion. New York: Academic Press; 1980. pp. 189–217. [Google Scholar]
- 45.Benight CC, Cieslak R. Cognitive factors and resilience: how self-efficacy contributes to coping with adversities. In: Southwick SM, Litz BT, Charney D, editors. Resilience mental health:across Challenges the lifespan. United Kingdom: Cambridge University Press; 2011. pp. 45–55. [Google Scholar]
- 46.McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. The Lancet. 2003;361(9369):1603–1607. doi: 10.1016/S0140-6736(03)13310-7. [DOI] [PubMed] [Google Scholar]
- 47.Lee V, Cohen SR, Edgar L, Laizner AM, Gagnon AJ. Meaning-making intervention during breast or colorectal cancer treatment improves self-esteem optimism and self-efficacy. Social Science Medicine. 2006;62(12):3133–3145. doi: 10.1016/j.socscimed.2005.11.041. [DOI] [PubMed] [Google Scholar]
- 48.Ferreira Filho AF, Junior OC, Da Silva DL, de Souza MA, Tavares Cavalcante IM, Wunder AP. Analysis of resilience scores of breast cancer patients undergoing ambulatory chemotherapy treatment. Journal of Clinical Oncology. 2010;28(15) suppl:e19681. abstr. [Google Scholar]
- 49.Junior OC, Ferreira Filho AF, de Souza MA, Wunder AP, Tavares IM, Da Silva DL. Comparison of resilience scores of an ambulatory population of cancer patients older than age 70 or younger than age 50 receiving chemotherapy treatment. Journal of Clinical Oncology. 2010;28(15) suppl:e19657. [Google Scholar]
- 50.Haase J, Kintner EK, Monahan PO, Robb SL. The resilience in illness model part 1. Exploratory evaluation in adolscents and young adults with cancer Cancer Nursing. 2014;37(3):E1–E12. doi: 10.1097/NCC.0b013e31828941bb. [DOI] [PMC free article] [PubMed] [Google Scholar]