Abstract
BACKGROUND
Differences among hospitals in the use of inpatient consultation may contribute to variation in outcomes and costs for hospitalized patients, but basic epidemiologic data on consultations nationally are lacking.
OBJECTIVE
The purpose of the study was to identify physician, hospital, and geographic factors that explain variation in rates of inpatient consultation.
DESIGN
This was a retrospective observational study.
SETTING AND PARTICIPANTS
This work included 3,118,080 admissions of Medicare patients to 4,501 U.S. hospitals in 2009 and 2010.
MAIN MEASURES
The primary outcome measured was number of consultations conducted during the hospitalization, summarized at the hospital level as the number of consultations per 1,000 Medicare admissions, or “consultation density.”
KEY RESULTS
Consultations occurred 2.6 times per admission on average. Among non-critical access hospitals, use of consultation varied 3.6-fold across quintiles of hospitals (933 versus 3,390 consultations per 1,000 admissions, lowest versus highest quintiles, p < 0.001). Sicker patients received greater intensity of consultation (rate ratio [RR] 1.18, 95 % CI 1.17–1.18 for patients admitted to ICU; and RR 1.19, 95 % CI 1.18–1.20 for patients who died). However, even after controlling for patient-level factors, hospital characteristics also predicted differences in rates of consultation. For example, hospital size (large versus small, RR 1.31, 95 % CI 1.25–1.37), rural location (rural versus urban, RR 0.78, CI 95 % 0.76–0.80), ownership status (public versus not-for-profit, RR 0.94, 95 % CI 0.91–0.97), and geographic quadrant (Northeast versus West, RR 1.17, 95 % CI 1.12–1.21) all influenced the intensity of consultation use.
CONCLUSIONS
Hospitals exhibit marked variation in the number of consultations per admission in ways not fully explained by patient characteristics. Hospital “consultation density” may constitute an important focus for monitoring resource use for hospitals or health systems.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-015-3216-7) contains supplementary material, which is available to authorized users.
KEY WORDS: consultation, hospital care, variation, medicare
INTRODUCTION
Surprisingly little research has focused on understanding the clinical epidemiology of one of the most common physician practices in the care of hospitalized patients: inpatient consultation. The attending physician consults additional physicians for the care of a hospitalized patient to seek procedural assistance or clinical expertise in a specific field that ensures the patient receives needed clinical interventions or insights. The vast majority of consultations are likely beneficial to patient care.1,2 The involvement of additional medical perspectives, however, may also carry risks to the patient. For example, each new physician could recommend additional diagnostic and therapeutic interventions, contribute to a longer length of stay, offer conflicting recommendations, or lead to excessive specialist involvement after discharge.2 As a result, it is possible that some consultations could actually worsen care, leading to both inferior patient outcomes and higher costs.
Consequently, the use of inpatient consultation may represent a source of variation in hospital care, which in turn may contribute to national variation in hospital and post-acute care costs and outcomes, as physician practice patterns determine a substantial portion of health care expenditures.3 Little is known, however, about the basic clinical epidemiology of inpatient consultation. Therefore, we used a large, nationally representative sample of admissions of Medicare beneficiaries in order to quantify the extent of variation in the practice of inpatient consultation. We hypothesized that inpatient consultation would vary in ways not fully explained by patient characteristics and health needs, and that physician, hospital, and geographic factors would play key roles in explaining variation in this common medical practice.
METHODS
Study Population
We studied acute care hospital admissions occurring in the 50 states and Washington, D.C. in 2009 and 2010 among a random 20 % sample of traditional fee-for-service Medicare beneficiaries aged 66 years or older at the time of admission, who had been continuously enrolled in Medicare Parts A and B for at least one full year, excluding patients with end-stage renal disease and those enrolled in Medicare Advantage health plans at any point during the year. We identified all acute care hospitalizations in the inpatient file and then identified all inpatient physician evaluation and management services and procedures billed in the Carrier file between the dates of admission and discharge, which captured 95 % or more of inpatient services provided by physicians. Transfers, defined as sequential hospitalizations where the discharge date of the first matched the admission date of the second for the same patient, were considered independent, occurring in less than 2 % of hospitalizations.
Study Variables
Defining Consultation Density
Our primary outcome of interest was the number of consultations conducted during the hospitalization, which we summarized at the hospital level as the number of consultations per 1,000 Medicare admissions, or “consultation density.” We used the specialty field in the Carrier file to identify the most common specialty code for which each physician billed, and the National Provider Identification (NPI) file to identify the specialties of attending and operating physicians in the inpatient file for whom a specialty was not listed. Services delivered by anesthesiologists, emergency medicine physicians, diagnostic radiologists, and pathologists were excluded from the consultation count. To account for cross-coverage and handoffs among physicians from the same specialty, we defined the number of consultations per admission conservatively as the number of unique specialties billing during the admission, minus one to account for the attending or operating physician.
Patient Characteristics
Demographic information, including beneficiary age, race, and sex, was obtained from the Medicare Master Beneficiary Summary File. We measured clinical comorbidities in the 365 days prior to admission using the Elixhauser comorbidity score4,5 and estimated the severity of the current admission using the cost weight of the diagnosis-related group (DRG), as well as length of stay, whether each admission included an intensive care unit stay, and inpatient mortality. We also examined the number of hospitalizations within the previous 365 days, as we hypothesized that the likelihood of a consultation may increase on subsequent admissions if a particular subspecialty had been involved in a patient’s care during a prior inpatient stay. We also ascertained the assigned diagnosis-related group (DRG) of the admission in order to perform subgroup analyses.
Hospital Characteristics
Hospital characteristics, which were obtained from the 2009 and 2010 American Hospital Association surveys, included critical access status, ownership (for-profit, not-for-profit, and public, defined as government-owned but non-federal), number of beds (categorized as fewer than 100, between 100 and 249, and 250 or more beds), and teaching status (major teaching [Council of Teaching Hospitals members], minor teaching [any hospital with residents or medical students], and non-teaching). Indian Health Service hospitals and Veterans Affairs hospitals were excluded. Hospitals were further characterized as rural or urban (defined using the Rural Health Research Center definitions for dichotomizing ZIP codes into rural or urban regions6), by quadrant of the country (Northeast, South, Midwest, and West), and by state. The average Elixhauser score for each hospital was used to aid in adjusting for variations in overall hospital patient mix. In an effort to capture the tendency of the hospital to admit patients to the ICU, which also may vary significantly by hospital,7 the percentage of patients admitted to the ICU at each hospital was measured as well.
Statistical Analysis
We restricted our analyses to hospitals with at least ten admissions in the 2010 sample.8 To minimize the impact of outlier hospitals, we first classified hospitals into quintiles by consultation density, defined as mean number of consultations per 1,000 admissions for each hospital. We then compared patient (age, gender, race, Medicaid dual eligibility, number of discharges in past year, Elixhauser score in the past year, length of stay, ICU stay, in-hospital death, and DRG cost weight), hospital (number of beds, ownership, teaching status, availability of medical/surgical ICU, availability of cardiac ICU, and average number of ICU admissions per 100 admissions per year), and geographic characteristics (urban versus rural location, region) of hospitals by quintile using chi-squared tests for categorical variables and t tests for continuous variables. Critical access hospitals (CAHs), which are small, isolated rural hospitals that receive cost-based reimbursement from Medicare, were analyzed descriptively on their own but together with other acute care hospitals in multivariate models. We used a multivariate Poisson marginal regression model with a log link that clustered by hospital to account for hospital and geographic characteristics. To understand the between-hospital variation in use of consultation, we then accounted for the hierarchical nature of the data using a three-level hierarchical mixed effects log-link model with Poisson distribution, with random intercepts for hospital within state, with the Medicare admission as the unit of analysis.
To ensure that the results were not driven by patients with a specific diagnosis, sensitivity analyses were conducted after restricting to admissions comprising the most common DRGs, and separate subgroup analyses were performed for all admissions for pneumonia, congestive heart failure, or acute myocardial infarction.
Our study was approved by the institutional review board at the Beth Israel Deaconess Medical Center. The requirements of informed consent and authorization for disclosure of protected health information were waived.
RESULTS
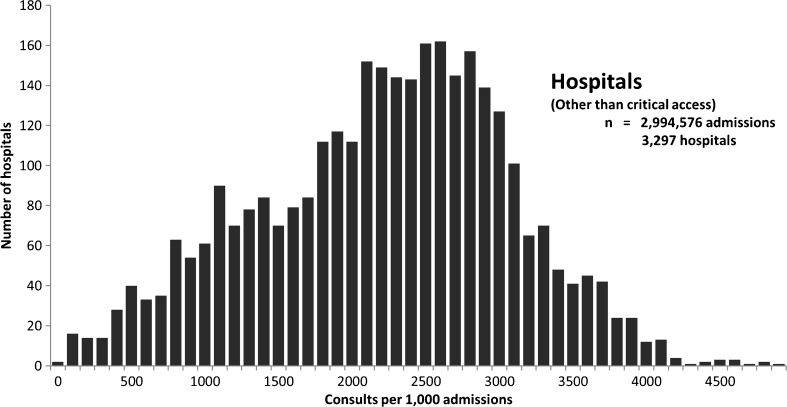
We studied a total of 3,118,080 hospital admissions between January 1, 2009, and December 31, 2010, to 4,501 hospitals nationally. These included 2,994,576 admissions to 3,297 non-critical access hospitals (non-CAHs) and 123,504 admissions to 1,204 critical access hospitals (CAHs). Approximately 90 % of admissions had at least one consultation. On average, among non-CAHs, there were 2,586 consultations per 1,000 admissions (range: first quintile, 933 consultations per 1,000 admissions; fifth quintile, 3,390 consultations per 1,000 admissions; Fig. 1). Consultation rates among CAHs were lower (mean = 631, range: first quintile, 169 consultations per 1,000 admissions; fifth quintile, 1,295 consultations per 1,000 admissions; eFig. 1).
Fig. 1.
Distribution of consult density (consults per 1,000 admissions) across all non-critical access hospitals
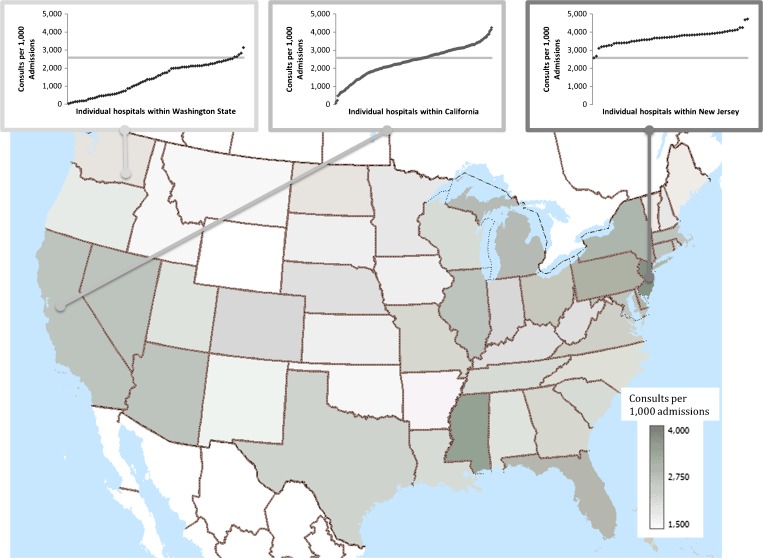
The use of consultation varied markedly among hospitals. When hospitals other than CAHs were divided into quintiles by consultation density, the number of consultations per admission for hospitals in the highest quintile was 3.6-fold that of their counterparts in the lowest quintile (p < 0.001) (Table 1, with univariate comparisons of CAHs available in eTable 1). There was also a greater than twofold difference in the number of consultations by state, from 1,532 consultations per 1,000 admissions in Wyoming to 3,751 consultations per 1,000 admissions in New Jersey (Fig. 2); substantial variation was evident within states as well.
Table 1.
Hospital characteristics by hospital consultation quintile among non-critical access hospitals
| Lowest quintile consultation density (n = 660 hospitals) | Q2 through Q4 consultation density (n = 1,978 hospitals) | Highest quintile consultation density (n = 659 hospitals) | Test of difference, high versus low quintile | |||
|---|---|---|---|---|---|---|
| Consultations per 1,000 admissions | 933 | 2,275 | 3,390 | <0.0001 | ||
| Average consults per admission | 1.19 | 2.31 | 3.03 | |||
| Patient | Demographic characteristics | Age (mean, SD) | 80 (8) | 79 (8) | 79 (8) | <0.0001 |
| Female (%) | 61 | 58 | 58 | <0.0001 | ||
| White (%) | 90 | 89 | 83 | <0.0001 | ||
| Hispanic (%) | 1 | 1 | 2 | <0.0001 | ||
| Black (%) | 6 | 8 | 11 | <0.0001 | ||
| Medicaid dual-eligible (%) | 36 | 24 | 25 | <0.0001 | ||
| Number discharges in prior year (mean) | 0.4 (0.9) | 0.4 (0.8) | 0.4 (0.9) | <0.0001 | ||
| Elixhauser score in prior year (mean) | 6.7 (8.4) | 6.6 (8.5) | 7.1 (8.9) | <0.0001 | ||
| Admission characteristics | Length of stay (mean, SD) | 5.1 (3.3) | 5.8 (4.8) | 6.6 (5.7) | <0.0001 | |
| ICU stay (%) | 20 | 27 | 31 | <0.0001 | ||
| Inpatient mortality (%) | 3.8 | 3.9 | 4.1 | <0.0001 | ||
| DRG cost weight (mean, SD) | 1.2 (0.7) | 1.6 (1.4) | 1.7 (1.6) | <0.0001 | ||
| Region | Northeast | 5.6 | 13.6 | 31.0 | <0.0001 | |
| Midwest | 17.4 | 19.3 | 15.3 | <0.0001 | ||
| South | 61.5 | 44.2 | 36.3 | <0.0001 | ||
| West | 15.5 | 22.9 | 17.5 | <0.0001 | ||
| Urban (%) | 18.8 | 74.0 | 95.1 | <0.0001 | ||
| Hospital | Size | <100 beds | 78.5 | 25.5 | 6.7 | <0.0001 |
| 100-249 beds | 19.4 | 44.1 | 34.6 | <0.0001 | ||
| 250 beds | 2.1 | 30.3 | 58.7 | <0.0001 | ||
| Ownership | Government, non-federal | 32.7 | 12.4 | 9.0 | <0.0001 | |
| Other characteristics | Not-for-profit | 40.6 | 65.7 | 69.7 | <0.0001 | |
| For-profit | 26.7 | 21.9 | 21.4 | <0.0001 | ||
| Major teaching hospital (%) | 0.5 | 7.4 | 18.5 | <0.0001 | ||
| Minor teaching hospital (%) | 10.8 | 30.2 | 34.2 | <0.0001 | ||
| With medical or surgical ICU (%) | 57.4 | 81.1 | 85.1 | <0.0001 | ||
| With cardiac ICU (%) | 7.1 | 34.2 | 52.4 | <0.0001 | ||
| Mean ICU admissions per 100 admissions per year | 0.5 | 1.1 | 1.5 | <0.0001 | ||
| Physician | % with generalist attending | 75.9 | 63.0 | 62.8 | <0.0001 | |
| % with medicine specialist attending | 8.3 | 15.1 | 20.7 | <0.0001 | ||
| % with surgical specialist attending | 13.1 | 20.0 | 14.7 | <0.0001 | ||
Fig. 2.
Consultation density (consultations per admission) by state across the United States. Inset graphs demonstrate within-state variation for (a) a low-use state, Washington state, (b) a middle-use state, California, and (c) a high-use state, New Jersey. The median consultation density across all U.S. hospitals is indicated as a gray line on the three inset graphs.
There was no meaningful difference in age, race, or gender between patients served by non-CAHs in the highest quintile and those in the lowest quintile (Table 1). However, hospitals with the highest number of consultations cared for patients with slightly more identified comorbidities (Elixhauser comorbidity scores, 7.1 versus 6.7, p < 0.0001), longer lengths of stay (6.6 days versus 5.1 days, p < 0.0001), more frequent ICU stays (31.5 % versus 20.1 %, p < 0.0001), higher DRG cost weights (1.7 versus 1.2, p < 0.0001), and higher average mortality (4.1 % versus 3.8 %, p < 0.0001). Compared with hospitals in the lowest quintile of consultation use, a greater proportion of hospitals in the highest quintile were large hospitals, located in the Northeast or South, members of the Council of Teaching Hospitals, and with not-for-profit ownership.
Predictors of Hospital Consultation Density
In multivariate marginal models that accounted for clustering of admissions by hospital, multiple patient-level, hospital-level, and regional-level characteristics continued to predict greater use of consultation. Patient severity of illness, as determined by DRG cost weight (greater than or equal to 3.0 versus less than or equal to 1.0, rate ratio [RR] 1.48, 95 % CI 1.47–1.50, p < 0.001), ICU admission (RR 1.18, 95 % CI 1.17–1.18, p < 0.0001), and inpatient mortality (RR 1.19, 95 % CI 1.18–1.12, p < 0.0001) remained significant independent predictors of increased consultation, whereas pre-existing patient comorbidities did not meaningfully predict consultation use. Patients with prior hospital admission in the past year experienced fewer consultations (more than three admissions versus no prior admissions, RR 0.94, 95 % CI 0.93–0.95, p < 0.0001).
Even after controlling for patient comorbidities and discharge diagnosis, patients admitted to larger hospitals experienced more consultations (≥250 beds versus <100 beds, RR 1.31, 95 % CI 1.25–1.37, p < 0.0001). When compared with not-for-profit hospitals, admission to non-federal public hospitals was associated with a decreased likelihood of consultation (RR 0.94, 95 % CI 0.91–0.97, p < 0.0001), while there was no difference when compared with for-profit hospitals. Consultation was most frequent in the Northeast (e.g., Northeast versus West, RR 1.17, 95 % CI 1.12–1.21, p < 0.0001) and least common in the West (Table 2). Even after these adjustments, there was substantial unexplained variation in consultation density among states, and to a greater degree among hospitals within states (covariance of state: 0.04, standard error 0.008; covariance of hospital within state: 0.12, standard error 0.003).
Table 2.
Predictors of inpatient consultation among all admissions. These effect estimates adjust for patient-level factors and cluster patients within hospitals in a marginal model. The measure of effect is presented as the rate ratio of an additional consultation as compared with the reference group of each variable.
| Variable | Category | Rate ratio | Lower 95 % CI | Upper 95 % CI | Test of difference | |
|---|---|---|---|---|---|---|
| Patient characteristics | Age (Ref = 66–70 years) | 71–75 | 1.01 | 1.01 | 1.01 | <0.0001 |
| 76–80 | 1.01 | 1.01 | 1.02 | <0.0001 | ||
| 81–85 | 1.01 | 1.01 | 1.02 | <0.0001 | ||
| 86–90 | 0.99 | 0.99 | 1.00 | 0.011 | ||
| 91–95 | 0.95 | 0.94 | 0.95 | <0.0001 | ||
| >95 | 0.89 | 0.88 | 0.91 | <0.0001 | ||
| Sex (Ref = Male) | Female | 0.98 | 0.98 | 0.98 | <0.0001 | |
| Race (Ref = White) | Black | 1.03 | 1.02 | 1.04 | <0.0001 | |
| Hispanic | 1.04 | 1.01 | 1.07 | 0.002 | ||
| Asian | 1.08 | 1.06 | 1.11 | <0.0001 | ||
| Other | 1.00 | 0.98 | 1.02 | 1.0 | ||
| Medicaid dual-eligible | Yes | 0.96 | 0.96 | 0.97 | <0.0001 | |
| Number of hospital discharges in the prior year (Ref = 0) | 1 | 0.98 | 0.98 | 0.98 | <0.0001 | |
| 2–3 | 0.96 | 0.96 | 0.97 | <0.0001 | ||
| >3 | 0.94 | 0.93 | 0.95 | <0.0001 | ||
| Elixhauser score in the prior year (Ref = less than 0) | 0–10 | 0.99 | 0.98 | 0.99 | <0.0001 | |
| 10–20 | 0.98 | 0.98 | 0.99 | <0.0001 | ||
| >20 | 1.00 | 1.00 | 1.01 | 0.16 | ||
| Died during this hospitalization | Yes | 1.19 | 1.18 | 1.20 | <0.0001 | |
| Cost weight of the DRG (Ref = less than 1) | 1–2 | 1.13 | 1.13 | 1.14 | <0.0001 | |
| 2–3 | 1.28 | 1.27 | 1.29 | <0.0001 | ||
| >3 | 1.48 | 1.47 | 1.50 | <0.0001 | ||
| Admitted to the ICU | Yes | 1.18 | 1.17 | 1.18 | <0.0001 | |
| Length of stay (Ref = 1 day) | 2–3 days | 0.97 | 0.94 | 1.00 | 0.06 | |
| 4–7 days | 1.34 | 1.30 | 1.39 | <0.0001 | ||
| >7 days | 1.99 | 1.92 | 2.06 | <0.0001 | ||
| Physician characteristics | Specialty of admission (Ref = Medicine, generalist) | Medicine, specialist | 1.03 | 1.01 | 1.05 | <0.0001 |
| Surgery, specialist | 1.05 | 1.04 | 1.07 | <0.0001 | ||
| Other | 0.98 | 0.95 | 1.00 | 0.03 | ||
| Hospital characteristics | Average ICU use by hospital (% of total admissions admitted to ICU) (Ref = <10 %) | 10–20 % | 1.02 | 0.98 | 1.06 | 0.47 |
| 20–30 % | 1.01 | 0.97 | 1.05 | 0.93 | ||
| >30 % | 1.02 | 0.99 | 1.06 | 0.36 | ||
| Teaching status (Ref = non-teaching | Major teaching | 0.98 | 0.95 | 1.01 | 0.31 | |
| Minor teaching | 1.00 | 0.98 | 1.03 | 0.91 | ||
| Type of ownership (Ref = Not-for-profit) | For-profit | 0.99 | 0.97 | 1.02 | 0.82 | |
| Government, non-federal | 0.94 | 0.91 | 0.97 | <0.0001 | ||
| Size (Ref = <100 beds) | >250 beds | 1.31 | 1.25 | 1.37 | <0.0001 | |
| 100–250 beds | 1.25 | 1.20 | 1.30 | <0.0001 | ||
| Region (Ref = West) | Midwest | 1.01 | 0.98 | 1.04 | 0.89 | |
| Northeast | 1.17 | 1.12 | 1.21 | <0.0001 | ||
| South | 1.00 | 0.97 | 1.03 | 0.99 | ||
| Rural versus urban (Ref = Urban) | Rural | 0.78 | 0.76 | 0.80 | <0.0001 | |
| Critical access hospital (Ref = no) | Yes | 0.53 | 0.50 | 0.55 | <0.0001 | |
| Average Elixhauser weight score by hospital (Ref = <5) | 5–5.9 | 1.03 | 0.98 | 1.08 | 0.33 | |
| 6–6.9 | 1.07 | 1.03 | 1.12 | 0.0001 | ||
| >7 | 1.12 | 1.08 | 1.18 | <0.0001 | ||
Sensitivity Analyses
In sensitivity analyses of marginal models and in separate models restricted to admissions for the ten most common DRGs and for congestive heart failure, pneumonia, and acute myocardial infarction, the patient-, hospital-, and regional-level findings all were essentially unchanged (Table 2; full model described in eTables 3, 4, and 5).
DISCUSSION
Our results demonstrate that consultation is a commonplace practice in inpatient care in the United States, occurring an average 2.6 times per hospital admission in the Medicare population. We find striking variability in “consultation density,” or the rate at which inpatient consultation takes place at each hospital, not fully explained by patient characteristics or disease severity. Our results provide substantial new insight into the epidemiology of inpatient consultation nationally.
To date, research on inpatient consultation has largely focused on qualitative work, single-site studies, and post-surgical populations to elucidate patient-level factors related to consultation.2,9,22 In particular, Chen et al. identified variability in the use of medical consultants following specific surgical procedures,22 whereas we studied inpatient consultation more generally across the full spectrum of inpatient conditions seen in the Medicare population. While our study confirms earlier findings that sicker and more complex patients receive more consultations, we also demonstrate that patient comorbidities and prior hospitalizations contribute little to explaining the use of consultation use during acute hospitalization. This finding may reflect the possibility that consultations were unrelated to patients’ underlying conditions or previous reasons for hospitalization, or may be explained by other non-clinical factors.
Our study details many factors other than patient characteristics that play a role in the likelihood of receiving consultation. Hospital size, ownership, rural location, and quadrant of the country were all important predictors of the use of consultation, even after adjustment for patient characteristics. Despite their teaching mission, major teaching hospitals used consultation less frequently than other types of hospitals. These findings suggest that the use of consultation may be related to factors other than the clinical condition of the patient. Future research may consider other potential non-clinical explanations for such variation in consultation, such as the malpractice climate, clinical experience of the attending physician, and financial incentives, both for Medicare patients and for those of other private payers.
We do not attempt to identify the appropriate number of consults per admission, a value that we anticipate would vary by hospital and patient clinical need and would depend on the expertise available in any given hospital on a given day. Nonetheless, the degree of variation we see is substantial, and could be generated by both overuse and underuse of consultation. Further investigation is needed to quantify appropriate use of this hospital resource.
Other studies have described national variation in elective procedures,23 services such as hospice,24 and spending on physician services.25 The magnitude of the variability in inpatient consultation density—a greater than 3.6-fold difference between highest and lowest quintiles of hospitals—exceeds the variability seen in total costs per Medicare beneficiary,26 and suggests that variation in consultation use might contribute to national variation in patient outcomes and costs among U.S. hospitals. Further, hypothetically comparing two hospitals in the same state with similar observed characteristics and patient mix, one with moderately low consultation density (1 SD below average) and one moderately high (1 SD above average), their rate ratio is 1.99, larger than any of the effects we found for other observable characteristics. These findings also suggest an urgent need for research into the quality and effectiveness of inpatient consultation, since we estimate that more than 20 million inpatient consultations occur every year in the Medicare population alone—more than 55,000 inpatient consultations per day.
How significant is consultation to the hospital and downstream costs of inpatient care? If we estimate total cost to Medicare based on the physician’s fee, and assume one visit by the consultant, the total cost to Medicare would vary from $1.7 billion if the encounters are of low complexity (Current Procedural Terminology code 99,221, national payment amount of $99.35 for 2013) to $2.7 billion if the encounters are of high complexity (Current Procedural Terminology code 99,223, national payment amount of $198.01 for 2013).27 These figures may underestimate the total cost, as most inpatient consultations consist of more than a single visit and usually generate substantial downstream laboratory, radiological, procedural, and post-hospital costs.
The amount of non-patient-driven variation in consultation that we found suggests both overuse and underuse of consultation. Clearly, some consultations are helpful, but do more consultations always benefit the patient? Some consultations may entail not only a diminishing benefit to patients, but also potential harm. Large numbers of consultations may be accompanied both by increased resource utilization and multiple and potentially conflicting recommendations of several consulting services.2 Given the evidence of variation in consultation practices, further investigation should assess the clinical consequences of these practices and the circumstances under which consultation is beneficial, wasteful, or harmful.
Our study has several important strengths. To our knowledge, this work represents the first study of inpatient consultation in a large, nationally representative sample of U.S. hospital admissions. Second, our multilevel models included factors at the patient, hospital, and regional levels, and accounted for clustering of observations. Third, our findings were consistent across subgroups and diagnoses. Finally, our approach to identifying consulting specialties was agnostic to the specific billing code used, thus minimizing the effect of regional variation in billing practices on our results.
Our study also has several limitations. First, we were not able to study outcomes associated with consultations. Nonetheless, we believe the findings are an important contribution, as so little is known about the frequency of and variability in consultation nationally. The findings suggest that variables not directly related to the clinical condition of individual patients can explain much of the difference in consultation density that we observed. Thus, improving the use of inpatient consultation might represent an important opportunity to improve the value of inpatient care. Second, we only examined the Medicare population, and our results might not generalize to other payers and age groups. Third, we used administrative data, which lacks the nuances of clinical data. Fourth, it is possible that unmeasured confounders might explain some of our results. We took several steps to minimize this potential impact through robust comorbidity adjustment, by including ICU admission, individual admission-level case mix, and inpatient mortality in our models, and through performing stratified subgroup analyses on individual DRGs. We also structured our model to account for the clustering of hospitals within states.28,29 Finally, because we counted the number of consulting specialties, our results likely represent a lower bound, as multiple consultations may occur within a specialty (e.g., consulting both an interventional cardiologist and an electrophysiologist), but we had no way to accurately distinguish between cross-coverage within a new specialty and additional consultations. Further, we did not use evaluation and management codes for consultation, as these expired in 2009 and were used inconsistently in different regions and specialties, reflecting variation in billing practices rather than variation in consultation use.
CONCLUSIONS
We found that inpatient consultation affects the majority of Medicare admissions in the United States, that there is as much as a 3.6-fold difference across non-critical access hospitals in the number of consultations used, and that this variation is not entirely explained by patient characteristics. These findings suggest that variation in consultation use may contribute to national variation in costs among U.S. hospitals. As all participants in the health care marketplace seek to control costs and increase value, closer examination of inpatient processes may yield additional opportunities to maximize the value of care, with inpatient consultation emerging as a prime target.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOCX 70.3 KB)
Acknowledgments
Competing Interest
There are no conflicts of interests or competing interests declared by any of the authors.
Disclaimer
The findings and views expressed herein are solely those of the authors and are not meant to reflect the views or policies of the federal government. The authors assume responsibility for the accuracy and completeness of the information contained in this article.
References
- 1.Howell MD. 2009; Pages https://www.rmf.harvard.edu/Clinician-Resources/Article/2012/Insight-Are-You-Complicating-Your-Consults on September 15 2013.
- 2.Stevens JP, Johansson AC, Schonberg MA, Howell MD. Elements of a High-Quality Inpatient Consultation in the Intensive Care Unit. A Qualitative Study. Annals of the American Thoracic Society. 2013;10(3):220–227. doi: 10.1513/AnnalsATS.201212-120OC. [DOI] [PubMed] [Google Scholar]
- 3.Sirovich B, Gallagher PM, Wennberg DE, Fisher ES. Discretionary decision making by primary care physicians and the cost of U.S. Health care. Health affairs. 2008;27(3):813–823. doi: 10.1377/hlthaff.27.3.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baldwin LM, Klabunde CN, Green P, Barlow W, Wright G. In search of the perfect comorbidity measure for use with administrative claims data: does it exist? Medical care. 2006;44(8):745–753. doi: 10.1097/01.mlr.0000223475.70440.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 6.University of Washington;Pageshttp://depts.washington.edu/uwruca/ruca-download.php on September 15 2013.
- 7.Gershengorn HB, Iwashyna TJ, Cooke CR, Scales DC, Kahn JM, Wunsch H. Variation in use of intensive care for adults with diabetic ketoacidosis*. Critical Care Medicine. 2012;40(7):2009–2015. doi: 10.1097/CCM.0b013e31824e9eae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kochanek KD, Xu J, Murphy SL, Minino AM, Kung HC. 2011;Pages. Accessed at National Center for Health Stastics at http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_03.pdf on September 15 2013.
- 9.Conley J, Jordan M, Ghali WA. Audit of the consultation process on general internal medicine services. Qual Saf Health Care. 2009;18(1):59–62. doi: 10.1136/qshc.2007.025486. [DOI] [PubMed] [Google Scholar]
- 10.Huynh T, Jacobs DG, Dix S, Sing RF, Miles WS, Thomason MH. Utility of neurosurgical consultation for mild traumatic brain injury. Am Surg. 2006;72(12):1162–1165. [PubMed] [Google Scholar]
- 11.Katz RI, Cimino L, Vitkun SA. Preoperative medical consultations: impact on perioperative management and surgical outcome. Can J Anaesth. 2005;52(7):697–702. doi: 10.1007/BF03016556. [DOI] [PubMed] [Google Scholar]
- 12.Lee T, Pappius EM, Goldman L. Impact of inter-physician communication on the effectiveness of medical consultations. Am J Med. 1983;74(1):106–112. doi: 10.1016/0002-9343(83)91126-9. [DOI] [PubMed] [Google Scholar]
- 13.Mehta RL, McDonald B, Gabbai F, Pahl M, Farkas A, Pascual MT, et al. Nephrology consultation in acute renal failure: does timing matter? Am J Med. 2002;113(6):456–461. doi: 10.1016/S0002-9343(02)01230-5. [DOI] [PubMed] [Google Scholar]
- 14.Puig J, Supervia A, Marquez MA, Flores J, Cano JF, Gutierrez J. Diabetes team consultation: impact on length of stay of diabetic patients admitted to a short-stay unit. Diabetes Res Clin Pract. 2007;78(2):211–216. doi: 10.1016/j.diabres.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 15.Reuben DB, Borok GM, Wolde-Tsadik G, Ershoff DH, Fishman LK, Ambrosini VL, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. N Engl J Med. 1995;332(20):1345–1350. doi: 10.1056/NEJM199505183322007. [DOI] [PubMed] [Google Scholar]
- 16.Salerno SM, Hurst FP, Halvorson S, Mercado DL. Principles of effective consultation: an update for the 21st-century consultant. Arch Intern Med. 2007;167(3):271–275. doi: 10.1001/archinte.167.3.271. [DOI] [PubMed] [Google Scholar]
- 17.Weed HG. Outcomes of Preoperative Medical Consultation [Editor’s Correspondence] Archives of Internal Medicine. 2011;171(4):367–368. doi: 10.1001/archinternmed.2011.6. [DOI] [PubMed] [Google Scholar]
- 18.Streeten EA, Mohamed A, Gandhi A, Orwig D, Sack P, Sterling R, et al. The inpatient consultation approach to osteoporosis treatment in patients with a fracture. Is automatic consultation needed? J Bone Joint Surg Am. 2006;88(9):1968–1974. doi: 10.2106/JBJS.E.01072. [DOI] [PubMed] [Google Scholar]
- 19.Wijeysundera DN, Beattie WS, Austin PC, Hux JE, Laupacis A. Is There Value in a Preoperative Medical Consultation?–Reply [Editor’s Correspondence] Archives of Internal Medicine. 2011;171(4):368–369. [Google Scholar]
- 20.Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753–1755. doi: 10.1001/archinte.1983.00350090131022. [DOI] [PubMed] [Google Scholar]
- 21.Winograd CH, Gerety MB, Lai NA. A negative trial of inpatient geriatric consultation. Lessons learned and recommendations for future research. Arch Intern Med. 1993;153(17):2017–2023. [PubMed] [Google Scholar]
- 22.Chen LM, Wilk AS, Thumma JR, Birkmeyer JD, Banerjee M. Use of medical consultants for hospitalized surgical patients: an observational cohort study. JAMA Intern Med. 2014;174(9):1470–1477. doi: 10.1001/jamainternmed.2014.3376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE. Variation profiles of common surgical procedures. Surgery. 1998;124(5):917–923. doi: 10.1016/S0039-6060(98)70017-0. [DOI] [PubMed] [Google Scholar]
- 24.Virnig BA, Kind S, McBean M, Fisher E. Geographic variation in hospice use prior to death. Journal of the American Geriatrics Society. 2000;48(9):1117–1125. doi: 10.1111/j.1532-5415.2000.tb04789.x. [DOI] [PubMed] [Google Scholar]
- 25.Welch WP, Miller ME, Welch HG, Fisher ES, Wennberg JE. Geographic variation in expenditures for physicians’ services in the United States. The New England journal of medicine. 1993;328(9):621–627. doi: 10.1056/NEJM199303043280906. [DOI] [PubMed] [Google Scholar]
- 26.Skinner JS, Gottlieb DJ, Carmichael D. 2011;Pages. Accessed at Dartmouth Institute for Health Policy and Clinical Practice at http://www.dartmouthatlas.org/downloads/reports/PA_Spending_Report_0611.pdf on July 9 2014. [PubMed]
- 27.Center for Medicare and Medicaid Services 2013;Pageshttp://www.cms.gov/apps/physician-fee-schedule/ on January 2 2014.
- 28.Stefan MS, Pekow PS, Nsa W, Priya A, Miller LE, Bratzler DW, et al. Hospital performance measures and 30-day readmission rates. Journal of General Internal Medicine. 2013;28(3):377–385. doi: 10.1007/s11606-012-2229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindenauer PK, Bernheim SM, Grady JN, Lin Z, Wang Y, Merrill AR, et al. The performance of US hospitals as reflected in risk-standardized 30-day mortality and readmission rates for medicare beneficiaries with pneumonia. Journal of hospital medicine : an official publication of the Society of Hospital Medicine. 2010;5(6):E12–E18. doi: 10.1002/jhm.822. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 70.3 KB)