Abstract
Background
Evidence-based interventions to reduce hospital readmissions may not generalize to resource-constrained safety-net hospitals.
Objective
To determine if an intervention by patient navigators (PNs), hospital-based Community Health Workers, reduces readmissions among high risk, low socioeconomic status patients.
Design
Randomized controlled trial.
Participants
General medicine inpatients having at least one of the following readmission risk factors: (1) age ≥60 years, (2) any in-network inpatient admission within the past 6 months, (3) length of stay ≥3 days, (4) admission diagnosis of heart failure, or (5) chronic obstructive pulmonary disease. The analytic sample included 585 intervention patients and 925 controls.
Interventions
PNs provided coaching and assistance in navigating the transition from hospital to home through hospital visits and weekly telephone outreach, supporting patients for 30 days post-discharge with discharge preparation, medication management, scheduling of follow-up appointments, communication with primary care, and symptom management.
Main Measures
The primary outcome was in-network 30-day hospital readmissions. Secondary outcomes included rates of outpatient follow-up. We evaluated outcomes for the entire cohort and stratified by patient age >60 years (425 intervention/584 controls) and ≤60 years (160 intervention/341 controls).
Key Results
Overall, 30-day readmission rates did not differ between intervention and control patients. However, the two age groups demonstrated marked differences. Intervention patients >60 years showed a statistically significant adjusted absolute 4.1 % decrease [95 % CI: −8.0 %, -0.2 %] in readmission with an increase in 30-day outpatient follow-up. Intervention patients ≤60 years showed a statistically significant adjusted absolute 11.8 % increase [95 % CI: 4.4 %, 19.0 %] in readmission with no change in 30-day outpatient follow-up.
Conclusions
A patient navigator intervention among high risk, safety-net patients decreased readmission among older patients while increasing readmissions among younger patients. Care transition strategies should be evaluated among diverse populations, and younger high risk patients may require novel strategies.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-015-3185-x) contains supplementary material, which is available to authorized users.
KEY WORDS: care transitions, continuity of care, health care delivery, patient safety, underserved populations
INTRODUCTION
Hospital readmission rates have been publicly reported since 2009 by the Centers for Medicare and Medicaid Services (CMS). In 2012, CMS instituted a payment penalty for hospitals with higher than expected readmission rates, focusing national attention on improving care transitions and reducing hospital readmissions.1 This policy poses challenges for safety-net hospitals serving predominantly patients of low socioeconomic status (SES) who contend with social and financial hardships in addition to established causes of readmission.2 They are more likely to be non-English speakers,3 have lower health literacy, which can impair self-management;4–6 higher rates of mental health and substance abuse disorders;7 greater exposure to social stressors;6 and are more likely to experience hospital readmission.8–10
Several care transitions programs11–16 have demonstrated success in decreasing hospital readmissions. These programs have primarily targeted elderly Medicare populations or patients with high risk diagnoses, such as heart failure. However, key groups of challenging patients, some of whom are disproportionately served at safety-net hospitals, were excluded or underrepresented in these studies,17,18 including non-elderly patients, non-English speakers, patients with dementia, those who leave against medical advice (AMA), and the homeless.
Furthermore, these programs used relatively expensive licensed personnel, such as nurse practitioners, pharmacists, or social workers. Safety-net hospitals typically have limited resources for new initiatives and professional staff. Less costly community health workers (CHWs)19, 20 have increased medical follow-up with primary care and specialists,21–23 improved adherence to medical regimens,24,25 and provided meaningful social support.22 These competencies may enhance post-discharge transitional care and reduce rehospitalizations.
We implemented an intervention led by hospital-based CHWs, or patient navigators (PNs), designed to reduce readmissions among high risk patients in a safety-net medical system. We assess the effects of this intervention in two distinct patient populations—those over and under age 60—groups whose distinctive distribution of medical and psychiatric comorbidities26–28 and different networks of social support29,30 shape their post-discharge needs and potentially their response to the PN intervention.
METHODS
Study Setting and Participants
We conducted a randomized, controlled trial among hospitalized patients within Cambridge Health Alliance (CHA), an academic public safety-net system with an ethnically diverse and traditionally underserved patient population. CHA is an integrated health care provider comprising two hospitals, three Emergency Departments (EDs), and ten community health centers. CHA serves 100,000 patients, one-third of whom have a language-of-care other than English. Patients were recruited between October 2011 and April 2013. Enrollment was initially at Cambridge Hospital; in September 2012, the protocol was modified to include Whidden Hospital, expanding the pool of eligible patients.
We randomized patients to the intervention or control group during their first admission in the study period that met the criteria for study entry, namely; having a primary care provider (PCP) within CHA; observation or inpatient admission on CHA’s general medicine service; community dweller; and discharged to a community setting (i.e., home, assisted living, shelter, or street). Additionally, eligible patients had at least one of five risk factors associated with elevated readmission rates documented in previous studies31–35 and in CHA historical data: (1) age >60 years; (2) admission to CHA’s general medicine, surgery, or psychiatry service within the past 6 months; (3) length of stay (LOS) ≥3 days; and (4) admission diagnosis of heart failure or (5) chronic obstructive pulmonary disease. Notably, our eligible population included non-English speakers, patients who left AMA, were homeless, or had a diagnosis of dementia.
The Institutional Review Boards of the CHA and Harvard Pilgrim Health Care approved the study as low risk and waived the requirement for informed consent, as patient navigators had been similarly utilized for several years in various settings within CHA.
Randomization
Eligible patients were identified daily using the hospital electronic medical record (EMR). PNs determined how many intervention patients to enroll each day, aiming to maintain a panel of 30–35 patients per full-time PN. A computer algorithm randomly assigned the PN-selected number of eligible patients to the intervention group and remaining eligibles to the controls. After randomization, patients were excluded if they died in-house or transferred to an ineligible service (e.g., psychiatry or surgery), an outside acute care hospital, a skilled nursing facility (SNF), long term care, or jail.
Control Group
Control patients received usual inpatient and outpatient care. Patient treatment and discharge plans are discussed daily at multidisciplinary rounds. Each patient is assigned a case manager who organizes post-discharge care including visiting nurses, home care, durable medical supplies, or referral to substance abuse programs or homeless shelters. At discharge, a floor nurse reviews written discharge instructions with the patient, including an updated medication list, scheduled appointments, and patient education. After discharge, a nurse from their primary care site attempts to telephone patients within 2 business days to assess patients’ medication adherence, confirm scheduled appointments, availability of transportation, and identify issues requiring immediate attention.
Intervention Group
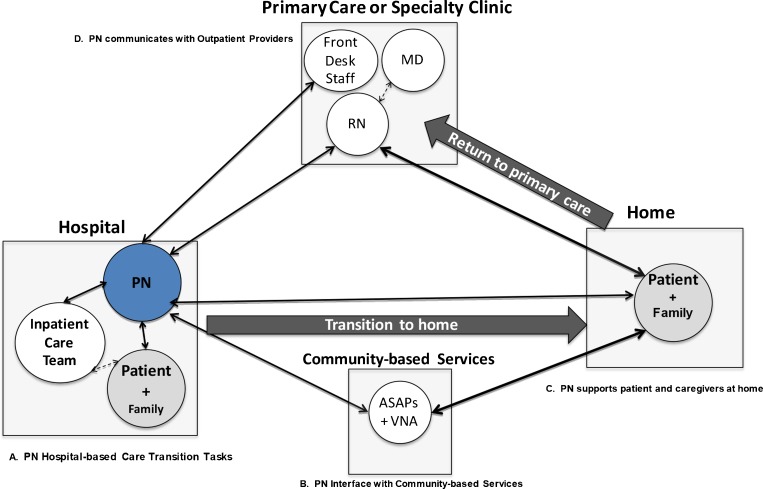
The PN intervention, piloted in 2010,36 is designed to assist patients with the logistics of navigating a complicated system to optimize post-discharge care (Fig. 1). PNs received extensive training and ongoing supervision (see Supplemental Appendix A, available online). Two of the three PNs were native Portuguese-speakers; telephone interpreters were used for other languages. Patients were assigned to PNs based on panel size and language concordance between the PN and patient; otherwise assignments alternated between PNs.
Figure 1.
Patient navigator roles and responsibilities: the interaction of the hospital-based patient navigators with patients, family, and other care team members during the hospital stay, transition to home, and return to primary care.
The intervention used scripts to promote standardization, lasted for 30 days post-discharge, and included hospital visits and weekly post-discharge outreach calls. The intervention protocol was fulfilled by one hospital visit and three completed calls. The PNs coached patients to independently direct their medical care, but actively coordinated care for patients less capable of self-management. PNs wrote a brief EMR note summarizing each completed call, which was sent to the patient’s primary care nursing staff. If unable to reach patients after three attempts, a voicemail was left with PN contact details and pending appointment information. The PNs coded the content of all outreach using a customized database.
The PNs had a broad range of tasks and responsibilities. Prior to discharge, the PNs conducted introductory visit(s) with the patient and caregivers to establish rapport, describe the PN program, and assess post-discharge needs; assisted patient in communicating with inpatient providers to address post-discharge concerns; verified patient’s post-discharge contact information and confirmed convenient times for outreach; highlighted the importance of obtaining new medications, having timely outpatient follow-up, and reporting concerning symptoms; and alerted PCP offices of a patient’s discharge.
After discharge, through weekly telephone contacts, the PNs confirmed appointments and rescheduled as needed; addressed barriers to obtaining or taking medications; identified concerning symptoms and facilitated communication with PCP offices; assisted with transportation; reassessed patients’ home care needs and made connections to community services; assisted with health insurance issues; supported patient self-management; and helped patients navigate the health care system.
Study Data and Outcome Measures
Data on patient demographics, health insurance, comorbidities, hospital readmissions, ED visits, and primary care appointments were abstracted from the EMR. Charlson comorbidity scores were calculated from diagnoses associated with the initial, qualifying hospitalization. Measures of intervention fidelity included the number of PN hospital visits, attempted and completed calls. The prespecified primary outcome measure was in-network all-cause hospital readmission (observation or full admission) to any service (including medicine, surgery, or psychiatry) within 30 days post-discharge. Planned readmissions were not excluded. Secondary outcomes were attending a primary care appointment within 7 days and any outpatient or ED visit within 30 days of discharge.
Statistical Analysis
We aimed to enroll 2,600 patients to provide 80 % power to detect absolute changes of 0.033 to 0.043 in the proportion of 30-day readmissions for baseline readmission rates ranging from 0.15 to 0.25 for PN patients compared to controls. The trial ended when the PN’s completed their prespecified period of effort, having enrolled 1,510 patients. In setting a target of 2,600 patients, we had not fully anticipated the large number of repeat admissions, which limited the number of eligible index discharges. Additionally, the intervention was more time-consuming than expected, limiting enrollment in the PN arm.
We first examined differences in demographic and clinical descriptors between PN and control patients, and between patients over and under age 60, using chi-square or t-tests, as appropriate. We next compared measures of intervention fidelity between patients over and under age 60 using chi-square tests. We used logistic regression to examine the association between PN/control study assignment and our outcomes of interest, adjusting for gender, language preference, race/ethnicity, insurance, Charlson score, psychiatric and substance abuse diagnoses, our identified readmission risk factors, and assigned hospital.
We performed an intention-to-treat analysis, modeling outcomes in the overall study cohort, and in patients over and under age 60. Our original analytic plan called for subgroup analyses according to Medicare enrollment status; however, we revised this plan early in the trial. The trial inclusion criteria allowed patients over age 60 to qualify based solely on age without other risk factors, while patients under 60 had to have at least one risk factor other than age. Consequently, the two groups exhibited very different risk profiles, affecting potential response to the PN intervention.
RESULTS
Participant Characteristics
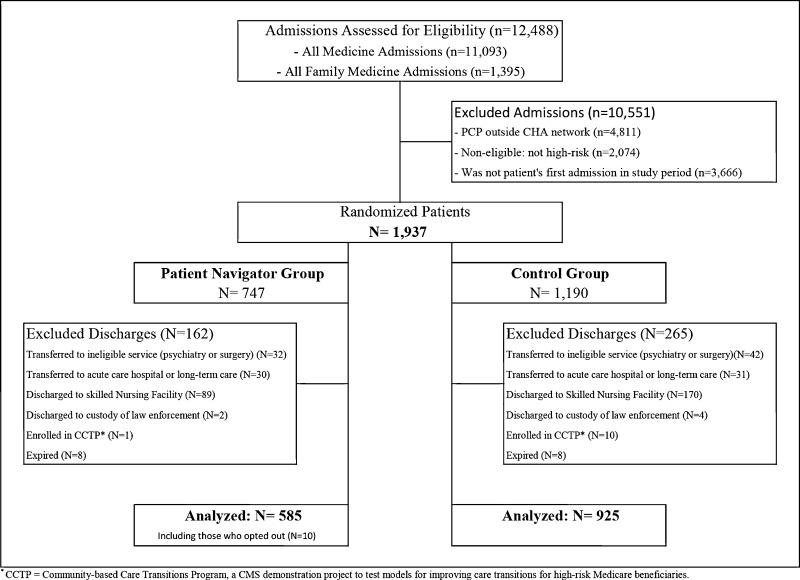
Of 12,488 first admissions to the general medicine service during the study period, 1,937 met the eligibility criteria of which 747 were randomized to the PN intervention and 1,190 to controls. After exclusions, the analytic sample included 585 intervention patients and 925 controls. Ten patients opting out of the intervention were analyzed in the PN group and were similar to PN enrollees in all characteristics except for a shorter LOS (1.8 days) (Fig. 2).
Figure 2.
Patient participation flow.
The study population, consistent with its low SES, was highly diverse in race and language, almost exclusively publicly insured, with a high burden of psychiatric illness and substance abuse (Table 1). Older patients were more medically complex with higher Charlson comorbidity scores, while younger patients had significantly more mental illness, substance abuse, and higher rates of previous hospitalizations and LOS >3 days.
Table 1.
Baseline Characteristics of the Study Sample by Intervention Group and Age Group
| PN | Ctrl | 60 years old+ | ≤60 years old | |||
|---|---|---|---|---|---|---|
| (N = 585) | (N = 925) | (N = 1009) | (N = 501) | |||
| p-value | p-value | |||||
| Age at discharge, mean (SD) | 66.4 (15.5) | 63.7 (16.7) | 0.001 | 74 (9.3) | 46.1 (10.3) | <0.001 |
| Female, n (%) | 323 (55.2) | 548 (59.2) | 0.123 | 611 (60.6) | 260 (51.9) | 0.001 |
| Language, n (%) | 0.064 | <0.001 | ||||
| English | 363 (62.1) | 583 (63.0) | 563 (55.8) | 383 (76.4) | ||
| Portuguese | 97 (16.6) | 113 (12.2) | 163 (16.2) | 47 (9.4) | ||
| Spanish | 43 (7.4) | 88 (9.5) | 86 (8.5) | 45 (9.0) | ||
| Other | 82 (14.0) | 141 (15.2) | 197 (19.5) | 26 (5.2) | ||
| Race, n (%) | 0.800 | <0.001 | ||||
| White | 337 (57.6) | 532 (57.5) | 585 (58.0) | 284 (56.7) | ||
| Black | 94 (16.1) | 144 (15.6) | 177 (17.5) | 61 (12.2) | ||
| Hispanic | 86 (14.7) | 151 (16.3) | 123 (12.2) | 114 (22.8) | ||
| Other | 68 (11.6) | 98 (10.6) | 124 (12.3) | 42 (8.4) | ||
| Health insurance type, n (%) | 0.623 | <0.001 | ||||
| Medicare | 174 (29.7) | 245 (26.5) | 407 (40.3) | 12 (2.4) | ||
| Medicaid | 165 (28.2) | 276 (29.8) | 199 (19.7) | 242 (48.3) | ||
| Duals Medicare and Medicaid | 135 (23.1) | 208 (22.5) | 237 (23.5) | 106 (21.2) | ||
| Health Safety Net* | 70 (12.0) | 123 (13.3) | 118 (11.7) | 75 (15.0) | ||
| Commercial/other | 41 (7.0) | 73 (7.9) | 48 (4.8) | 66 (13.2) | ||
| Weighted Charlson score, mean (SD) | 1.3 (1.6) | 1.1 (1.5) | 0.004 | 1.3 (1.5) | 0.9 (1.5) | <0.001 |
| Chronic behavioral health issues | ||||||
| Substance abuse or psychiatric diagnosis, n (%) | 272 (46.5) | 494 (53.4) | 0.009 | 421 (41.7) | 345 (68.9) | <0.001 |
| Psychiatric diagnosis†, n (%) | 222 (37.9) | 397 (42.9) | 0.056 | 348 (34.5) | 271 (54.1) | <0.001 |
| Substance abuse‡, n (%) | 126 (21.5) | 272 (29.4) | <0.001 | 159 (15.8) | 239 (47.7) | <0.001 |
| Dementia | 65(11.1) | 109(11.8) | 0.690 | 107(10.6) | 67(13.4) | 0.113 |
| Qualifying risks of readmission | ||||||
| 60 years old+, n (%) | 425 (72.6) | 584 (63.1) | <0.001 | |||
| Index admission, LOS ≥3 days, n (%) | 261 (44.6) | 467 (50.5) | 0.026 | 395 (39.1) | 333 (66.5) | <0.001 |
| Admission at CHA in past 6 months, n (%) | 167 (28.5) | 257 (27.8) | 0.748 | 149 (14.8) | 275 (54.9) | <0.001 |
| COPD§, n (%) | 50 (8.5) | 63 (6.8) | 0.212 | 71 (7.0) | 42 (8.4) | 0.349 |
| Heart failure§, n (%) | 40 (6.8) | 38 (4.1) | 0.020 | 65 (6.4) | 13 (2.6) | 0.001 |
| Outpatient visit(s) in previous month, n (%) | 360 (61.5) | 570 (61.6) | 0.974 | 611 (60.6) | 319 (63.7) | 0.241 |
| Length of stay, mean (SD) | 3 (2.4) | 3.5 (3.8) | 0.003 | 2.8 (3.0) | 4.3 (3.8) | <0.001 |
| Discharge against medical advice, n(%) | 12(2.1) | 16(1.7) | 0.652 | 9(0.9) | 19(3.8) | <0.001 |
*Health Safety Net is a Massachusetts state program for uninsured patients
†Based on ICD-9 discharge codes: 290–302.9 and 306–319
‡Based on ICD-9 discharge codes: 303–305.93
§Based on primary Emergency Department admission diagnosis
Randomization elicited comparable intervention and control groups, with exceptions noted in Table 1. In the over 60 population, intervention patients had higher Charlson comorbidity scores (1.63 vs. 1.45; p = 0.005), while controls had more behavioral health issues (44.7 % vs. 37.6 %; p = 0.025) (results not shown). Among those under 60, intervention patients had a higher percentage of admissions in the past 6 months (65.6 % vs. 49.9 %; p < 0.001) (results not shown).
Fidelity of Implementation
The PNs met with virtually all patients while hospitalized and were resolute in attempting to contact patients after discharge. The PNs were more successful contacting older compared to younger patients post-discharge and thus more likely to deliver a complete intervention (Table 2).
Table 2.
Fidelity of Patient Navigator Intervention Implementation and Description of Issues Addressed, Stratified by Age Group
| 60 years old+ | ≤60 years old | ||
|---|---|---|---|
| (N = 425) | (N = 160) | ||
| n (%) | n (%) | p-value | |
| Fidelity of implementation | |||
| Hospital visits during index hospitalization | 0.051 | ||
| PN did not visit patient | 13 (3.1) | 9 (5.6) | |
| PN visited patient once | 194 (45.6) | 57 (35.6) | |
| PN visited patient more than once | 218 (51.3) | 94 (58.8) | |
| Attempted outreach calls w/in 30 days of index discharge* | 0.004 | ||
| PN did not attempt to call patient | 37 (8.7) | 4 (2.5) | |
| PN attempted to call patient 1–2 times | 30 (7.1) | 21 (13.1) | |
| PN attempted to call patient 3+ times | 358 (84.2) | 135 (84.4) | |
| Successful outreach calls w/in 30 days of index discharge* | 0.007 | ||
| PN did not speak to patient/caregiver | 46 (10.8) | 27 (16.9) | |
| PN successfully contacted patient/caregiver 1–2 times | 120 (28.2) | 58 (36.3) | |
| PN successfully contacted patient/caregiver 3+ times | 259 (60.9) | 75 (46.9) | |
| Full implementation† | 257 (60.5) | 74 (46.3) | 0.002 |
| Issues addressed | |||
| Medical needs or problems | |||
| PN reviewed medical issues in discharge plan | 285 (67.1) | 85 (53.1) | 0.002 |
| PN identified medical issues | 211 (49.6) | 66 (41.3) | 0.070 |
| PN identified medication issues | 201 (47.3) | 58 (36.3) | 0.017 |
| PN identified a medical emergency | 6 (1.4) | 4 (2.5) | 0.365 |
| Follow-up appointments | |||
| PN contacted patient about an appointment reminder | 337 (79.3) | 126 (78.8) | 0.885 |
| PN helped patient with scheduling an appointment | 159 (37.4) | 64 (40) | 0.566 |
| Other | |||
| Arranging transportation | 152 (35.8) | 44 (27.5) | 0.059 |
| Home services | 38 (8.9) | 6 (3.8) | 0.034 |
| Medical insurance | 13 (3.1) | 6 (3.8) | 0.674 |
*Or before readmission if readmitted within 30 days
†Defined as patient received 1+ hospital visit by PN and 3+ successful outreach calls from PN
As planned, the PNs assisted patients primarily with medical and medication issues, appointments, and transportation. Older patients received more assistance with medical issues, medications, and transportation.
Outcomes
Results from unadjusted analyses were consistent with the adjusted analyses, and in most cases, had similar patterns of statistical significance (Table 3). We observed no difference in 30-day readmission rates between intervention and control patients for the entire study population (full model results in Supplemental Appendix B, available online). However, the two age subgroups had markedly different, statistically significant responses to the PN intervention. The older group experienced an adjusted absolute 4.1 % decrease [95 % CI: −8.0 %, -0.2 %] in readmission; conversely, the younger PN group experienced an adjusted absolute 11.8 % increase [95 % CI: 4.4 %, 19.0 %] in readmission. Of note, psychiatric readmissions (12.2 % of younger and 2.0 % of older patients) occurred evenly between intervention and control patients; removing these did not change results.
Table 3.
Adjusted and Unadjusted Trial Results for All Patients and Stratified by Age Group
| Difference in rate of outcome | ||||
|---|---|---|---|---|
| (PN-Ctrl) | ||||
| Unadjusted | Adjusted* | |||
| All (N = 1,510) | PN (n = 585) | Ctrl (n = 925) | ||
| Readmission w/in 30 days of index discharge (%) | 14.2 | 13.1 | 1.1 [−2.5, 4.7] | 0.4 [−3.1, 3.8] |
| PCP visit w/in 7 days of index discharge (%) | 27.9 | 22.6 | 5.3 [0.8, 9.8] | 5.1 [0.6, 9.6] |
| Outpatient visit w/in 30 days of index discharge (%) | 83.3 | 78.5 | 4.8 [0.7, 8.8] | 4.9 [0.9, 8.9] |
| ED visit w/in 30 days of index discharge (%)† | 13.5 | 11.6 | 1.9 [−1.5, 5.4] | 2.6 [−0.9, 6.0] |
| 60 years old+ (N = 1009) | PN (n = 425) | Ctrl (n = 584) | ||
| Readmission w/in 30 days of index discharge (%) | 10.1 | 13.5 | −3.4 [−7.4, 0.6] | −4.1 [−8.0, −0.2] |
| PCP visit w/in 7 days of index discharge (%) | 29.9 | 25.2 | 4.7 [−0.9, 10.0] | 4.9 [−0.7, 10.0] |
| Outpatient visit w/in 30 days of index discharge (%) | 85.2 | 79.1 | 6.1 [1.3, 11.0] | 6.7 [2.0, 11.0] |
| ED visit w/in 30 days of index discharge (%)† | 9.4 | 8.1 | 1.4 [−2.2, 4.9] | 1.1 [−2.4, 4.7] |
| ≤60 years old (N = 501) | PN (n = 160) | Ctrl (n = 341) | ||
| Readmission w/in 30 days of index discharge (%) | 25.0 | 12.3 | 12.7 [5.1, 20.0] | 11.8 [4.4, 19.0] |
| PCP visit w/in 7 days of index discharge (%) | 22.5 | 18.2 | 4.3 [−3.3, 12.0] | 4.6 [−3.1, 12.0] |
| Outpatient visit w/in 30 days of index discharge (%) | 78.1 | 77.4 | 0.7 [−7.1, 8.5] | 3.8 [−3.7, 11.0] |
| ED visit w/in 30 days of index discharge (%)† | 24.4 | 17.6 | 6.8 [−1.0, 15.0] | 6.2 [−1.6, 14.0] |
Bold indicates p < 0.05
*Adjusted for gender, language, race/ethnicity (black, Hispanic, other compared to white), health insurance (Medicaid or dual status, Health Safety Net, commercial compared to Medicare), readmission risk factors, comorbidities, chronic behavioral health issues, and index hospital (Whidden compared to Cambridge Hospital)
†ED visits with discharge to home
For older intervention patients, rates of primary care follow-up at 7 days trended higher and outpatient visits within 30 days were significantly higher compared to controls. No significant differences were seen in the younger population. Rates of ED visits within 30 days did not differ between groups, regardless of age.
DISCUSSION
This randomized controlled trial evaluated a PN intervention using low-cost CHWs to improve care transitions for general medicine inpatients discharged to home. While previous studies evaluated general medical populations in safety-net hospitals,14,37 ours is the first to target patients at high risk for readmission in this setting. The PN intervention did not reduce hospital readmissions among the full cohort of patients; however, we found dramatically different responses related to patient age.
Among patients older than 60, the PN intervention significantly decreased 30-day readmissions compared to controls. The PNs implemented the key components of a well-functioning care transitions program. They made hospital visits to 97 % of older patients, allowing an individualized understanding of patients’ transitional needs. More than 60 % of older patients received three or more outreach calls, allowing PNs to assist patients with medication management, symptom control, outpatient follow-up, and self-care. The PNs were empathic and caring, forming relationships that could motivate patients to engage more fully in their health care.38 Intervention patients trended toward higher rates of 7-day primary care follow-up and had significantly more outpatient appointments within 30 days, visits that could play an important role in preventing readmission.39,40
The reduction in readmissions among those over 60 is similar to other effective post-discharge programs.11,15 However, ours is the first study to successfully employ CHWs in reducing readmissions in an older population. While not medically licensed, the PNs were trained to recognize when medical assistance was necessary and could readily engage primary care nursing; they also provided logistical assistance and motivational support. Achieving comparable readmission reductions at lower cost may heighten interest in this strategy, particularly at financially constrained safety-net institutions.
Among patients under age 60, PNs visited nearly 95 % in-hospital and 83 % received at least one post-discharge call. However, it was more challenging to engage younger patients over the 30-day period, as 25 % fewer received the complete intervention compared with older patients. There were only small nonsignificant increases in outpatient follow-up among younger PN patients, which may reflect weaker ties to primary care or other access barriers. Yet the startling 11.8 % adjusted increase in the readmission rate among PN patients compared to controls was unforeseen, especially in the context of readmission reductions among older patients.
These findings are not unprecedented. Several care transition programs have reported increased readmissions of up to 96 %: high-risk inpatients on a psychiatric-substance abuse unit assigned to a peer mentorship intervention;41medically complex Veterans Affairs patients who received intensive primary care support;42 younger general medicine patients assigned to nurse case managers coordinating outpatient care;43 and patients with heart failure assigned to a comprehensive treatment program.44 Explanations for these paradoxical findings included: increased receptiveness to inpatient treatment for long-standing psychiatric disorders;41 improved provider-patient communication facilitating detection and treatment of undiagnosed medical problems;42 patients better enabled to self-identify concerning symptoms and seek medical care;42 personnel added to the care team increased complexity, impairing patients’ ability to self-care;45 and patients using the hospital as respite from housing or social problems.7 Furthermore, other studies have demonstrated that increased outpatient contact (e.g., PN outreach) may be associated with more readmissions, particularly among younger low SES patients,46,47 suggesting that such patients may need more finely targeted, and possibly more intensive, outpatient care.
Additionally, younger, low SES patients have exhibited high utilization of hospital-based care,48,49 possibly reflecting an underlying belief that hospital-based care is easier to access and of higher quality.50 Because PNs were hospital-based, their supportive work may have unintentionally encouraged younger patients to return to the hospital for medical care. Finally, the higher rate of previous admissions among younger PN-assigned patients might indicate that this group was predisposed to higher readmission rates. Future qualitative studies may elucidate our paradoxical findings, as it is challenging to identify the most likely explanation from our study data.
The markedly different responses to the PN intervention highlight the need to evaluate care transition strategies in different settings and with different populations. Even well-validated programs, such as the Care Transitions Intervention®, have performed differently or required modifications to succeed in new venues.51
Our study has several limitations. First, without access to claims data, we assess utilization only within CHA’s network; we do not observe out-of-network readmissions, estimated to comprise 20 % of all readmissions.52 We expected that non-network readmissions would occur equally between intervention and control patients; however, even a small imbalance in unobserved out-of-network rehospitalizations might render our estimated reductions in readmissions among older patients nonsignificant. On the other hand, a positive experience with a PN might have led some intervention patients to selectively choose a CHA hospital for readmission; in this case, our readmission reductions with the older population may actually be underestimated.
Second, because discharge coordinators often knew which patients were assigned post-discharge PN support, they may have had increased comfort discharging PN patients home (vs. SNF) compared with controls who lacked extra support. Indeed, among older patients, a significantly higher percentage of controls vs. PN-patients (19.5 % vs. 15.1 %, data not shown) was discharged to SNFs and consequently excluded from analysis. Thus, the older PN group may have had sicker patients discharged to home, making readmission more likely. If correct, decreased readmissions among older patients may again be underestimated.
Third, we evaluated 30-day post-discharge utilization, the most frequently used time frame for assessing transitional care. However, 30 days is a short period to effect change, especially for patients with complex behavioral health issues. Future studies should evaluate longer term effects of CHW-based care transition interventions.
Fourth, our analysis considered one qualifying admission per patient. This widely used approach minimizes the impact of high utilizers, but may better represent an intervention’s effectiveness across different populations. Nonetheless, strategies to address high utilizers need further attention.
Finally, our study took place in two small hospitals within a safety-net system. Further validation of this approach is needed before generalizing it to other settings.
CONCLUSION
A patient navigator intervention using CHWs to reduce barriers to post-discharge care among high risk patients in a safety-net setting differentially impacted older and younger patients. Older patients received more outpatient care after hospitalization and experienced less inpatient care, whereas younger patients experienced much higher rates of readmission.
Our study raises provocative questions about the younger publicly insured population. Did their readmissions address unmet medical needs? Could these readmissions have been prevented with more intensive community-based care? Were our results shaped by previously excluded populations, such as non-English speakers, those leaving AMA, or the homeless? Future studies that address these questions may help to optimize transitional care of vulnerable patients across all age groups.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 22 kb)
Acknowledgments
Funders
This study was funded by the Agency for Healthcare Research and Quality (1R01HS020628-01A1). A pilot study was funded by Partners Community Healthcare, Inc., and the Department of Population Medicine at Harvard Medical School.
Prior Presentations
Study findings were presented at the 2013 Annual Meeting of the American Public Health Association, November 2013, Boston, MA, and at the Cambridge Health Alliance Academic Poster Session, April 2014, Cambridge, MA.
Conflict of Interest
The authors of this manuscript have no conflict of interest to report.
Footnotes
NIH Trial Registration
ClinicalTrials.gov identifier: NCT01619098
References
- 1.Readmissions Reduction Program. Centers for Medicare and Medicaid Services Available at: http://cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 2.American Hospital Association. Examining the drivers of readmissions and reducing unnecessary readmissions for better patient care. Trendwatch. 2011.
- 3.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non-safety-net hospitals. J Urban Health Bull N Y Acad Med. 1999;76(3):351–70. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20(2):175–84. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kripalani S, Jacobson TA, Mugalla IC, Cawthon CR, Niesner KJ, Vaccarino V. Health literacy and the quality of physician-patient communication during hospitalization. J Hosp Med Off Publ Soc Hosp Med. 2010;5(5):269–75. doi: 10.1002/jhm.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell SE, Sadikova E, Jack BW, Paasche-Orlow MK. Health literacy and 30-day postdischarge hospital utilization. J Health Commun. 2012;17(Suppl 3):325–38. doi: 10.1080/10810730.2012.715233. [DOI] [PubMed] [Google Scholar]
- 7.Kangovi S, Grande D, Meehan P, Mitra N, Shannon R, Long JA. Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med Off Publ Soc Hosp Med. 2012;7(9):709–12. doi: 10.1002/jhm.1966. [DOI] [PubMed] [Google Scholar]
- 8.Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48(4):495–504. doi: 10.1093/geront/48.4.495. [DOI] [PubMed] [Google Scholar]
- 9.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA J Am Med Assoc. 2011;305(7):675–81. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol. 2001;87(12):1367–71. doi: 10.1016/S0002-9149(01)01554-5. [DOI] [PubMed] [Google Scholar]
- 11.Coleman EA, Parry C, Chalmers S, Min S-J. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–8. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 12.Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med Off Publ Soc Hosp Med. 2009;4(4):211–8. doi: 10.1002/jhm.427. [DOI] [PubMed] [Google Scholar]
- 13.Evans RL, Hendricks RD. Evaluating hospital discharge planning: a randomized clinical trial. Med Care. 1993;31(4):358–70. doi: 10.1097/00005650-199304000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–87. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA J Am Med Assoc. 1999;281(7):613–20. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 16.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–84. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 17.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–8. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 18.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA J Am Med Assoc. 2009;301(6):603–18. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 19.Kangovi S, Long JA, Emanuel E. Community health workers combat readmission. Arch Intern Med. 2012;172(22):1756–7. doi: 10.1001/2013.jamainternmed.82. [DOI] [PubMed] [Google Scholar]
- 20.Singh P, Chokshi DA. Community health workers–a local solution to a global problem. N Engl J Med. 2013;369(10):894–6. doi: 10.1056/NEJMp1305636. [DOI] [PubMed] [Google Scholar]
- 21.Krieger J, Collier C, Song L, Martin D. Linking community-based blood pressure measurement to clinical care: a randomized controlled trial of outreach and tracking by community health workers. Am J Public Health. 1999;89(6):856–61. doi: 10.2105/AJPH.89.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenthal EL, Brownstein JN, Rush CH, et al. Community health workers: part of the solution. Health Aff Proj Hope. 2010;29(7):1338–42. doi: 10.1377/hlthaff.2010.0081. [DOI] [PubMed] [Google Scholar]
- 23.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–7. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roth AM, Holmes AM, Stump TE, et al. Can lay health workers promote better medical self-management by persons living with HIV? An evaluation of the Positive Choices program. Patient Educ Couns. 2012;89(1):184–90. doi: 10.1016/j.pec.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 25.Pilote L, Tulsky JP, Zolopa AR, Hahn JA, Schecter GF, Moss AR. Tuberculosis prophylaxis in the homeless. A trial to improve adherence to referral. Arch Intern Med. 1996;156(2):161–5. doi: 10.1001/archinte.1996.00440020063008. [DOI] [PubMed] [Google Scholar]
- 26.Crane SJ, Tung EE, Hanson GJ, Cha S, Chaudhry R, Takahashi PY. Use of an electronic administrative database to identify older community dwelling adults at high-risk for hospitalization or emergency department visits: the elders risk assessment index. BMC Health Serv Res. 2010;10:338. doi: 10.1186/1472-6963-10-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA J Am Med Assoc. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 28.Regenstein M, Andres E. Reducing hospital readmissions among medicaid patients: a review of the literature. Qual Manag Health Care. 2014;23(1):20–42. doi: 10.1097/QMH.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 29.Grafft CA, McDonald FS, Ruud KL, Liesinger JT, Johnson MG, Naessens JM. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Intern Med. 2010;170(11):955–60. doi: 10.1001/archinternmed.2010.105. [DOI] [PubMed] [Google Scholar]
- 30.Older Americans Act and Aging Network. Available at: http://www.aoa.gov/AoARoot/AoA_Programs/OAA/introduction.aspx. Accessed March 12, 2014.
- 31.Smith DM, Giobbie-Hurder A, Weinberger M, et al. Predicting non-elective hospital readmissions: a multi-site study. Department of Veterans Affairs Cooperative Study Group on Primary Care and Readmissions. J Clin Epidemiol. 2000;53(11):1113–8. doi: 10.1016/S0895-4356(00)00236-5. [DOI] [PubMed] [Google Scholar]
- 32.Billings J, Dixon J, Mijanovich T, Wennberg D. Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients. BMJ. 2006;333(7563):327. doi: 10.1136/bmj.38870.657917.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 34.Amarasingham R, Moore BJ, Tabak YP, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48(11):981–8. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 35.Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211–9. doi: 10.1007/s11606-009-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burns ME, Galbraith AA, Ross-Degnan D, Balaban RB. Feasibility and evaluation of a pilot community health worker intervention to reduce hospital readmissions. Int J Qual Health Care J Int Soc Qual Health Care ISQua. 2014 doi: 10.1093/intqhc/mzu046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Int Med. 2014 doi: 10.1001/jamainternmed.2013.14327. [DOI] [PubMed] [Google Scholar]
- 38.Mautner DB, Pang H, Brenner JC, et al. Generating hypotheses about care needs of high utilizers: lessons from patient interviews. Popul Health Manag. 2013;16(Suppl 1):S26–33. doi: 10.1089/pop.2013.0033. [DOI] [PubMed] [Google Scholar]
- 39.Koekkoek D, Bayley KB, Brown A, Rustvold DL. Hospitalists assess the causes of early hospital readmissions. J Hosp Med Off Publ Soc Hosp Med. 2011;6(7):383–8. doi: 10.1002/jhm.909. [DOI] [PubMed] [Google Scholar]
- 40.Balla U, Malnick S, Schattner A. Early readmissions to the department of medicine as a screening tool for monitoring quality of care problems. Medicine (Baltimore) 2008;87(5):294–300. doi: 10.1097/MD.0b013e3181886f93. [DOI] [PubMed] [Google Scholar]
- 41.Tracy K, Burton M, Nich C, Rounsaville B. Utilizing peer mentorship to engage high recidivism substance-abusing patients in treatment. Am J Drug Alcohol Abuse. 2011;37(6):525–31. doi: 10.3109/00952990.2011.600385. [DOI] [PubMed] [Google Scholar]
- 42.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 43.Einstadter D, Cebul RD, Franta PR. Effect of a nurse case manager on postdischarge follow-up. J Gen Intern Med. 1996;11(11):684–8. doi: 10.1007/BF02600160. [DOI] [PubMed] [Google Scholar]
- 44.Mudge A, Denaro C, Scott I, Bennett C, Hickey A, Jones MA. The paradox of readmission: effect of a quality improvement program in hospitalized patients with heart failure. J Hosp Med Off Publ Soc Hosp Med. 2010;5(3):148–53. doi: 10.1002/jhm.563. [DOI] [PubMed] [Google Scholar]
- 45.Holland R, Lenaghan E, Harvey I, et al. Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ. 2005;330(7486):293. doi: 10.1136/bmj.38338.674583.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gill JM, Mainous AG, 3rd, Nsereko M. Does having an outpatient visit after hospital discharge reduce the likelihood of readmission? Del Med J. 2003;75(8):291–8. [PubMed] [Google Scholar]
- 47.Huff ED. Outpatient utilization patterns and quality outcomes after first acute episode of mental health hospitalization. Is some better than none, and is more service associated with better outcomes? Eval Health Prof. 2000;23(4):441–56. doi: 10.1177/01632780022034714. [DOI] [PubMed] [Google Scholar]
- 48.Weissman JS, Stern RS, Epstein AM. The impact of patient socioeconomic status and other social factors on readmission: a prospective study in four Massachusetts hospitals. Inq J Med Care Organ Provis Finan. 1994;31(2):163–72. [PubMed] [Google Scholar]
- 49.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA J Am Med Assoc. 2010;304(6):664–70. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff Proj Hope. 2013;32(7):1196–203. doi: 10.1377/hlthaff.2012.0825. [DOI] [PubMed] [Google Scholar]
- 51.Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011;171(14):1232–7. doi: 10.1001/archinternmed.2011.278. [DOI] [PubMed] [Google Scholar]
- 52.Kind AJH, Bartels C, Mell MW, Mullahy J, Smith M. For-profit hospital status and rehospitalizations at different hospitals: an analysis of Medicare data. Ann Intern Med. 2010;153(11):718–27. doi: 10.7326/0003-4819-153-11-201012070-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 22 kb)