Abstract
Attenuated strains of invasive enteric bacteria, such as Salmonella, represent promising gene delivery agents for nucleic acid-based vaccines as they can be administrated orally. In this study, we constructed a novel attenuated strain of Salmonella for the delivery and expression of the hemagglutinin (HA) and neuraminidase (NA) of a highly pathogenic H5N1 influenza virus. We showed that the constructed Salmonella strain exhibited efficient gene transfer activity for HA and NA expression and little cytotoxicity and pathogenicity in mice. Using BALB/c mice as the model, we evaluated the immune responses and protection induced by the constructed Salmonella-based vaccine. Our study showed that the Salmonella-based vaccine induced significant production of anti-HA serum IgG and mucosal IgA, and of anti-HA interferon-γ producing T cells in orally vaccinated mice. Furthermore, mice orally vaccinated with the Salmonella vaccine expressing viral HA and NA proteins were completely protected from lethal challenge of highly pathogenic H5N1 as well as H1N1 influenza viruses while none of the animals treated with the Salmonella vaccine carrying the empty expression vector with no viral antigen expression was protected. These results suggest that the Salmonella-based vaccine elicits strong antigen-specific humoral and cellular immune responses and provides effective immune protection against multiple strains of influenza viruses. Furthermore, our study demonstrates the feasibility of developing novel attenuated Salmonella strains as new oral vaccine vectors against influenza viruses.
Introduction
Influenza infection, which is caused by seasonal and pandemic influenza viruses, can potentially lead to large numbers of deaths in humans, animals, and domestic birds as well as significant financial losses [1]. For example, the World Organization for Animal Health highlighted the outbreaks of highly pathogenic avian influenza (HPAI) H5N1 virus, which is associated with a growing number of human zoonotic infections and has been met with intense public health interest [2, 3]. In 2009, a novel swine-origin H1N1 influenza A virus, which was initially identified in Mexico and spread globally, has continued to circulate in humans and may have the potential to develop into the first influenza pandemic of the twenty-first century [4–6]. To control and prevent potential outbreaks of influenza viruses (e.g. the H5N1 avian influenza virus and the 2009 swine-origin H1N1 virus) in the future, effective vaccines against influenza viruses are urgently needed.
Influenza viruses are members of the Orthomyxoviridae family, which have enveloped, segmented, single-stranded negative sense RNA genome [1]. The hemagglutinin (HA) is the most abundant viral membrane protein in the envelope and is responsible for both binding and fusion with host cells. The neuraminidase (NA), another viral membrane protein found in the virion, is pivotal in the release and spread of progeny virions, following the intracellular viral replication process [1]. It has been reported that influenza virus infections can be primarily and effectively controlled by vaccines that elicit both humoral and cellular immune responses against the viral surface proteins HA and NA [7–9]. Vaccines being used or explored against influenza viruses include conventional inactivated whole viral antigen vaccines, live attenuated reasserted virus vaccines, recombinant protein vaccines, virus-like particle (VLP) vaccines, and DNA vaccines [8, 10, 11]. DNA vaccine, as a novel vaccine candidate, has been shown to induce effective antibody response and long-term cell-mediated immunity in animal models [12–15]. Furthermore, DNA vaccines, when delivered orally, can induce systemic and mucosal immune as well as cellular immune responses to antigens as compared to vaccines delivered via the parenteral routes [9, 16]. These results suggest that orally delivered DNA vaccines may represent promising novel vaccines against influenza virus.
Oral vaccines are cost effective and operate conveniently because they eliminate the use of syringes and needles and thus are an affordable choice for mass vaccination. Attenuated Salmonella strains have successfully been used as an oral carrier system for delivery of nucleic acid-based vaccines [16, 17]. In previous studies, attenuated Salmonella were constructed and transformed with plasmid constructs containing transgenes under the control of an expression promoter [18–20]. In human cells infected by Salmonella, plasmid DNA can be released and transported to the nuclei, leading to the expression of the transgene [18, 21, 22]. The genes of Salmonella pathogenicity island 2 (SPI-2), which encode virulence factors and are required for intracellular survival and replication [23–25], are believed to play important roles in gene transfer ability of Salmonella vector. Inactivation of these genes, including the components of the type III secretion system (T3SS) encoded by SPI-2, led to better lysis of the bacteria and more efficient gene transfer [7, 18, 21, 26].
Salmonella may serve as promising oral vaccine vectors in vivo [19, 27]. Generation of new Salmonella strains with better gene transfer activity and further studies of these strains should facilitate the development of Salmonella as a vaccine vector against infectious pathogens including influenza viruses. In this study, we generated a novel attenuated Salmonella strain, SL368, with a deletion at the spiR gene, which is required for the expression of many SPI-2 genes [28]. Using SL368, we constructed a Salmonella-based vaccine expressing the HA and NA proteins of a human H5N1 influenza virus. We showed that SL368 exhibited efficient gene transfer activity and little virulence, leading to expression of viral antigens in cultured cells and in mice. Using BALB/c mice as the model, we studied the constructed Salmonella-based vaccine in comparison to the current commercial H5N1 and H1N1 influenza vaccines. Our study provides direct evidence that the SL368-based vaccine induces the production of anti-HA serum IgG and mucosal IgA, and of anti-HA interferon-γ producing T cells. Furthermore, mice orally vaccinated with the Salmonella vaccine were completely protected from lethal challenge of both highly pathogenic H5N1 and H1N1 influenza viruses. These results suggest that the Salmonella-based vaccine elicits strong antigen-specific humoral and cellular immune responses and provides effective immune protection against multiple strains of influenza viruses. Furthermore, our study demonstrates the feasibility of developing novel attenuated Salmonella strains as new oral vaccine vectors against influenza viruses.
Materials and Methods
Ethics Statement
This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Research Council (8th Edition). The animal experiment protocol was approved by the Animal Care and Use Committee of the State Key Laboratory of Virology, Wuhan University (Wuhan, China) or the Animal Care and Use Committee of the University of California-Berkeley (Protocol #R240). All efforts were made to minimize suffering of experimental animals.
Virus strains, antibodies and synthetic peptides
Influenza virus A/Puerto Rico/8/34 (H1N1) and a reassortant H5N1 influenza virus (A/Viet Nam/1194R (H5N1)) were used in the study. The reassortant H5N1 virus (kindly provided by Dr. N. Robert (Virology Department, NIBSC, UK)) contains the HA and NA genes of human-isolated influenza virus (A/Viet Nam/1194/2004 (H5N1)) and the internal protein genes of A/Puerto Rico/8/1934 [15]. These viruses were propagated and grown in embryonated chicken eggs, following the procedure described previously [15, 29–31]. The anti-HA and anti-NA antibodies were purchased from GenScript (Piscataway, NJ) and the anti-actin antibody was from Sigma (St Louis, MO). The synthetic peptide IYSTVASSL, which represents amino acid residues 533–541 of the HA protein of the H5N1 influenza virus [32], was purchased from Sangon Biotech (Shanghai, China) and dissolved in water for use in subsequent assays. The commercial H5N1 and H1N1 vaccines, cv-H5N1 and cv-H1N1, which are inactivated vaccines being used for vaccination in humans in China, were purchased from Weike Inc (Harbin, China) and Hualan Inc (Henan, China), respectively.
Construction of recombinant DNA plasmids
Constructs pMD-5HA and pMD-5NA contained the sequences coding for the HA and NA gene of the avian influenza virus A/Viet Nam/1194/2004 (H5N1) strain, respectively [15]. The H5N1 HA gene fragment was amplified from construct pMD-5HA by PCR using the primers 5HA-sense (5’- GGCAAGCTTCTGTCAAAATGGAGAAAAT-3’) and 5HA-antisense (5’- CGCTCGACTTTAACTACAATCTGAACT-3’). The PCR products were digested using Hind III and Xho I and then cloned into eukaryotic expression vector pVAX1 (Invitrogen, Carlsbad, CA, USA) to generate p5HA. Similarly, the H5N1 NA gene fragment was amplified from construct pMD-5NA by PCR using the primers 5NA-sense (5’- GTCAAGCTTACCATGAATCCAAATCAG-3’) and 5NA-antisense (5’- AGCTCGACCTACTTGTCAATGGTGAAT-3’), and then cloned into pVAX1 to generate p5NA.
Construction and growth analysis of Salmonella strains
Salmonella typhimurium clinical strain ST14028s has been described previously [18, 33]. Salmonella strain SL368 was derived from the auxotrophic Salmonella typhimurium aroA strain SL7207 (a gift from Bruce A. D. Stocker, Stanford University, CA)[34] by deleting a part of the SpiR coding sequence with the λ Red recombinase method [35], following the procedures described in detail previously [33, 36]. Growth analysis of bacteria in LB broth was carried out with the experimental protocols as described in detail previously [33, 36].
Expression of viral antigens by Salmonella-mediated delivery in cultured cells
Salmonella carrying different plasmid constructs, Sal-HA-NA and Sal-vector, were generated by transforming strain SL368 with p5HA and p5NA, or pVAX1, respectively. In gene transfer experiments, we infected HeLa cells and differentiated THP (1x106 cells) (pretreated with IFN-γ (150 U/ml) (R&D Systems Inc., Minneapolis, MN) for at least 12 hours) with Salmonella at a multiplicity of infection (MOI) of 10–20 bacteria/cell [18, 21, 33]. The infected cultures were then incubated at 37°C in 5% CO2 for 1 hour. Cells were then washed five times with phosphate-buffered saline (PBS), and then incubated with fresh medium containing 50 μg/ml of gentamicin [18, 21, 33]. Cells were harvested after 72 hours incubation.
To assay the expression of the viral mRNAs, total RNAs were isolated from cells using Trizol (Invitrogen, San Diego, CA) and digested with DNase I to remove the genomic DNA. Northern and Western blot analyses were performed as described in detail previously [18, 21]. In Western blot analyses, we stained electrophoretically separated proteins using antibodies against influenza proteins and actin, and analyzed protein expression with a STORM840 Phosphorimager [18, 21].
Oral immunization of mice
Specific-pathogen-free female BALB/c mice (6 weeks old) were obtained from the Laboratory Animal Centre, Yangzhou University (China) and housed in a specific pathogen free facility. Mice were randomly divided into groups (5–10 mice per group) and were immunization on day 0, 14, and 28. In experiments with Salmonella-based vaccines, mice were first anesthetized with isoflurane and then intragastrically inoculated with 0.1–0.2 mL phosphate-buffered saline (PBS) containing no Salmonella or 1 × 109 cfu Sal-HA-NA or Sal-vector, using a gavage needle [18, 21, 37]. In experiments with the commercial H5N1 and H1N1 vaccines, mice were intramuscularly inoculated with cv-H5N1 (Weike Inc, Harbin, China) and cv-H1N1 (Hualan Inc, Henan, China) respectively, following the manufacturers’ recommendations. We have closely monitored the mice after the treatment. Even though no apparent side effects have been observed in mice vaccinated with the commercial influenza vaccines and SL368 carrying different plasmid constructs, we still took special precautions to ensure that ample food and water as well as sanitary cage conditions were present in order to maximize the animals’ comfort.
Enzyme-linked immunosorbent assay (ELISA)
Sera samples were drawn from mice at indicated time points after immunization and before challenge with the viruses. Blood was spun at 13,000 rpm for 15 min, and the supernatant (serum) was removed and stored at -80°C. The levels of serum IgG and mucosal IgA-specific antibodies against influenza antigens were determined by ELISA with the mouse hemagglutinin HA IgG ELISA Kit and the mouse hemagglutinin HA IgA ELISA Kit (Xiangsheng Inc, Shanghai, China) respectively, following the manufacturers’ recommendations [7, 15]. Briefly, samples of test serum or mucosal nasal wash were added to triplicate wells, then mixed with diluted horseradish-peroxidase (HRP)-labeled anti-mouse IgG or anti-mouse IgA antibody (50 μl/well), and incubated at 37°C for 1 hour. Following several washes, the plates were incubated with 100 μl visualization reagent A and B of the HA IgG and IgA ELISA kits (Xiangsheng Inc, Shanghai, China) for 15 min. The reactions were stopped with 50 μl stop buffer and the absorbance was measured at 450 nm using an ELISA plate reader. The assays were performed in triplicate and the experiments were repeated three times. The values obtained were the average from these experiments.
Hemagglutination inhibition (HI) assay
The serum neutralization activity was measured by HI assays [38]. Briefly, blood samples were collected at 0, 16, 32, 42 day after immunization, and specific receptor-destroying enzyme (RDE)-treated sera were serially diluted (2-fold) in V-bottomed 96-well plates, and then mixed with ~4 HA units of inactive influenza A/Puerto Rico/8/34(H1N1) or A/chicken/China/1204/04(H5N1). After incubating at room temperature for 30 min, 50 μl of 1% chicken erythrocytes was added to each well. The plate was incubated at room temperature for 40 min. The HI titer was defined as the highest serum dilution that showed 100% hemagglutination inhibition. The assays were performed in triplicate and the experiments were repeated three times. The values obtained were the average from these experiments.
IFN-γ ELISPOT assay
The relative numbers of IFN-γ expressing T cells in single cell spleen suspensions were measured using the mouse IFN-γ ELISPOT kit (U-Cytech biosciences, Utrecht, Netherlands) as described previously [15]. Briefly, splenocytes (1×106) were isolated from mice following euthanasia with overdose inhalational CO2, added to each well of pre-coated 96 well plate in triplicate, and stimulated with or without 100 μl/well (5 μg/ml) of HA533–541 epitope peptide (IYSTVASSL) [32] at 37°C for 24 hours. Phytohemagglutinin (PHA, 4 μg/ml, Sigma–Aldrich, St. Louis, MO, USA) was used as a positive control. After incubation, the cells were removed and incubated with 100 μl/well (0.5 μg/ml) of biotinylated detector antibody (anti-mouse IFN-γ) and 50 μl/well of 2% gold particle-labeled anti-biotin antibody (GABA) at 37°C for 1 hour. Finally, the plate was treated with Activator I/II at 37°C for 30 min. The number of spots was counted using a computer-assisted video image analyzer. The results were expressed as spot-forming cells (SFC) per million cells. The assays were performed in triplicate and the experiments were repeated three times. The values obtained were the average from these experiments.
Studies of immunized mice challenged with influenza viruses
For viral challenge experiments, five mice per group were first anesthetized with isoflurane and then infected intranasally with 50 μl PBS (25 μl per nostril) containing a dose of 20 LD50 of lethal influenza virus strain A/Puerto Rico/8/34(H1N1) or A/Viet Nam/1194R (H5N1) two weeks after the final vaccination. The infected mice experienced the typical effects of systemic infection caused by influenza virus. We have taken special precautions and followed standard guidelines outlined in the Guide for the Care and Use of Laboratory Animals to ensure that ample food and water as well as sanitary cage conditions were present in order to maximize the animal’s comfort. Mice were observed daily to monitor body weight for 16 days. Humane (non-lethal) endpoints were used during the survival experiments. Animals were deemed gravely ill and were euthanized by overdose inhalation of carbon dioxide if they lost more than 30% of their weight or exhibited lethargy, ruffled hair coat, or hunched posture. Experiments suggested that inoculation of mice with a virus dose of 20 MLD50 is sufficient for our study as the viruses used are highly pathogenic. All efforts were made to minimize suffering of animals.
For histological analyses, mice were euthanized with overdose inhalational CO2. Lung tissues were collected and fixed with 10% formaldehyde, embedded in paraffin, and cut into 5 μm sections. Sections were stained with hematoxylin and eosin (H&E), and were then examined microscopically.
For determination of viral titers, lungs were isolated from mice at day 3 and 6 after virus inoculation. Lung tissues of equal weight were homogenized in DMEM medium to achieve 10-fold serially diluted suspensions of tissue homogenates and were titrated in 96-well culture plates of Madin-Darbin canine kidney (MDCK) cells. The titers were calculated by use of the Reed-Muench method and were expressed as log10TCID50/g lung tissue. The assays were performed in triplicate and the experiments were repeated three times. The values obtained were the average from these experiments.
Statistical analyses
Statistical analyses of the data were performed using the analysis of variance (ANOVA). A p-value of less than 0.05 was considered significant.
Results
Construction of attenuated Salmonella vaccine
We have previously shown that attenuated Salmonella strains can be used as gene delivery vectors for expression of ribozymes in both human cells and in mice [18, 21, 39]. In this study, we constructed an attenuated Salmonella strain, SL368, as the gene delivery vector for the generation of the influenza vaccines. SL368 was derived from Salmonella typhimurium strain SL7207 [34] and in addition, contained a deletion of a part of the coding sequence of the SpiR protein. SL7207 is an attenuated strain with gene delivery activity [27, 34, 39, 40]. The SpiR protein is a part of the two-component transcription complex regulating the expression of the majority of the SPI-2 encoded genes, which are important for Salmonella intracellular survival and virulence in vivo [28, 41]. To generate Salmonella vaccine expressing influenza virus antigens, SL368 was electroporated with plasmid constructs p5HA and p5NA, which contained the DNA sequences coding for the HA and NA genes of a highly pathogenic influenza A H5N1 virus strain that were under control of a eukaryotic expression promoter, respectively (S1 Table).
Four vaccines were included in our study (S2 Table). Vaccine Sal-HA-NA contained strain SL368 carrying plasmid constructs p5HA and p5NA. Vaccine Sal-vector contained SL368 carrying the empty vector construct pVAX1 without any influenza virus sequences and was used as a negative control. We also included the commercial H1N1 and H5N1 vaccines, cv-H1N1 and cv-H5N1, as the positive controls in our study.
Gene delivery and expression of influenza antigens in cultured cells and in mice mediated by attenuated Salmonella
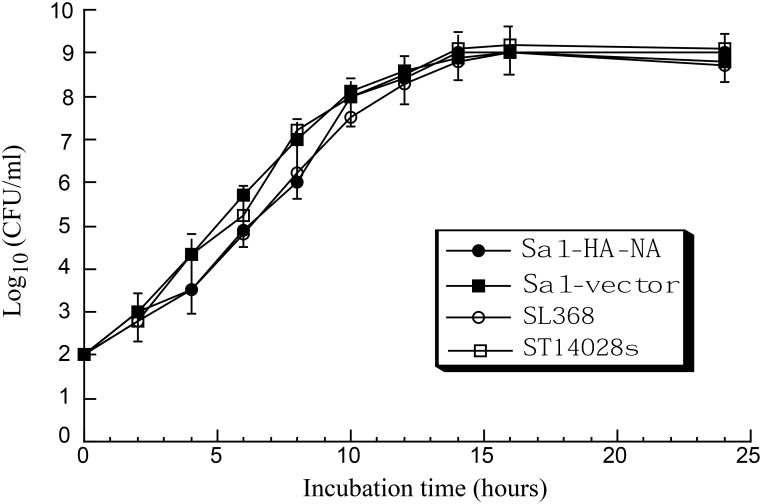
In growth analysis experiments, Salmonella carrying constructs containing expression cassettes for influenza virus genes grew in LB broth as well as bacteria carrying no constructs or carrying the pVAX1 empty vector (Fig 1). These results indicate that the presence of the influenza virus sequence does not result in an impaired viability of the bacterial carrier.
Fig 1. Analysis of growth in LB broth of Salmonella.
Salmonella used in the study include the wild type strain ST14028s, mutant strain SL368, and its derivatives that carry the empty vector construct pVAX1 (Sal-vector), and constructs p5HA and p5NA (Sal-HA-NA). Experimental details can be found in Materials and Methods.
In Northern blot analyses, none of the influenza virus RNA transcripts was detected in Salmonella carrying constructs with viral sequences (data not shown). Furthermore, Western blot analyses using anti-influenza antibodies showed that neither influenza HA nor NA protein was detected in Salmonella grown in LB (data not shown). These results suggested that the viral proteins, which were under the control of a eukaryotic expression cassette, were not expressed when Salmonella grew in culture media outside of human cells.
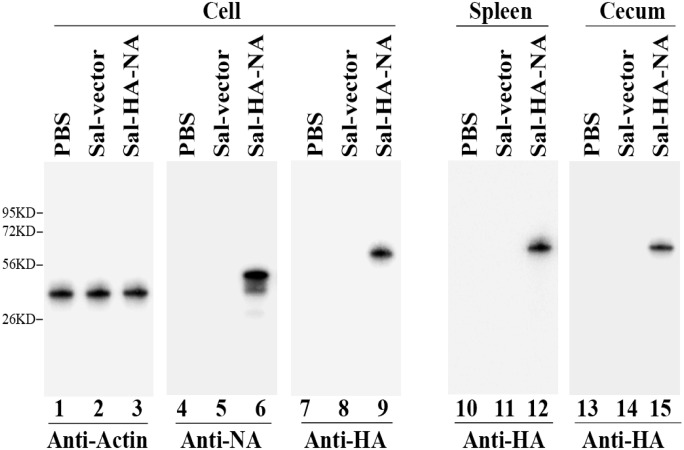
To determine whether Salmonella can efficiently deliver the influenza virus sequences into human cells, HeLa cells and differentiated macrophage THP-1 cells were infected with Salmonella SL368 carrying p5HA, p5NA, and the pVAX1 empty vector, and harvested at 72 hours postinfection. The expression of influenza HA and NA proteins was assayed with antibodies specifically against influenza virus proteins, using actin as the loading control (Fig 2). Western bolt analyses showed that Salmonella Sal-vector, in which SL368 carried the empty vector pVAX1, did not express any influenza antigen (Fig 2, lanes 5 and 8). The HA (~64KD) and NA (~50 KD) proteins were detected in cells infected with Salmonella Sal-HA-NA, in which SL368 carried constructs p5HA and p5NA (lanes 6 and 9). These results indicate that SL368 efficiently carried out gene transfer for delivery of constructs containing DNAs coding for viral antigens and that the HA and NA antigens were efficiently expressed following gene transfer of SL368 in human cells.
Fig 2. Salmonella-mediated delivery for influenza antigen expression in cells and in mice.
Western blot analyses were performed to study the expression of viral HA and NA proteins in differentiated THP-1 cells (lanes 1–9) and viral HA protein in BALB/C mice (lanes 10–15) treated with phosphate-buffered saline (PBS) only (PBS, lanes 1, 4, 7, 10, and 13), SL368 carrying the empty vector construct pVAX1 (Sal-vector, lane 2, 5, 8, 11, and 14) and constructs p5HA and p5NA (Sal-HA-NA, lanes 3, 6, 9, 12, and 15). Cells treated with PBS or Salmonella were harvested at 72 hours post treatment while spleens and cecums were harvested from BALB/C mice that were intragastrically inoculated with PBS or SL368 carrying different constructs at 4 days after inoculation. Protein samples (40 μg) were separated on denaturing gels, transferred to membranes, and stained with antibodies against viral HA (lanes 7–15) and NA (lanes 4–6) or actin (lanes 1–3), which serves as the loading control. Molecular markers are shown on the left.
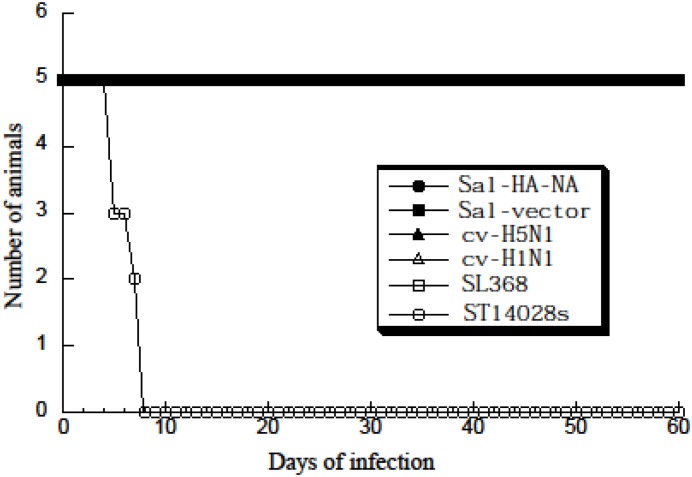
To study Salmonella-mediated gene delivery for the expression of influenza virus antigens in vivo, we intragastrically inoculated BALB/c mice with Salmonella Sal-HA-NA and Sal-vector. Gene delivery mediated by Sal-HA-NA was efficient in vivo as HA and NA proteins were detected in the intestines and spleens of the Salmonella-treated mice (Fig 2, lanes 10–15, data not shown). Furthermore, SL368 carrying no construct, the viral antigen constructs, and the empty vector pVAX1 exhibited much less virulence in vivo than the wild-type strain ST14028s. All mice infected with SL368, Sal-HA-NA, and Sal-vector (1 × 109 cfu/mouse) remained alive even at 60 days postinoculation (Fig 3). In contrast, mice inoculated with a much lower dose of ST14028s (1 × 103 cfu/mouse) died within 7 days (Fig 3). Thus, the constructed SL368-based vaccine appeared to be efficient in gene transfer and exhibited little virulence and pathogenicity in vivo.
Fig 3. Toxicity and virulence of different Salmonella strains in BALB/c mice.
Mice (5 animals per group) were either inoculated intramuscularly with the commercial H5N1 (cv-H5N1) and H1N1 vaccines (cv-H1N1) or intragastrically with PBS, the wild-type strain ST14028 (1 × 103 CFU), and vaccine strain SL368 (1 × 109 CFU) carrying the empty vector construct pVAX1 (Sal-vector) and constructs p5HA and p5NA (Sal-HA-NA). The mortality of the animals was monitored for 60 days. Humane (non-lethal) endpoints were used during the experiments and mice were euthanized with overdose inhalational CO2 to limit suffering, when they exhibited weight loss of more than 30%, lethargy, ruffled hair coat, or hunched posture.
Humoral responses induced by the vaccines
BALB/c mice were randomly divided into groups and vaccinated intragastrically with the constructed Salmonella Sal-HA-NA and Sal-vector at day 0, 14, and 28. Animals were also treated similarly with phosphate-buffered saline (PBS) in the absence of Salmonella and used as the negative controls. To compare the effectiveness of our generated Salmonella-based vaccines, vaccines cv-H5N1 and cv-H1N1, which were currently commercially available for vaccination in China against H5N1 and H1N1 viral infections respectively, were used as positive controls and injected intramuscularly into mice at day 0, 14, and 28. All animals remained alive at day 42 post immunization (i.e. two weeks after the final immunization) (data not shown), consistent with our observations (Fig 3) that SL368 exhibited little virulence/pathogenicity in mice in vivo.
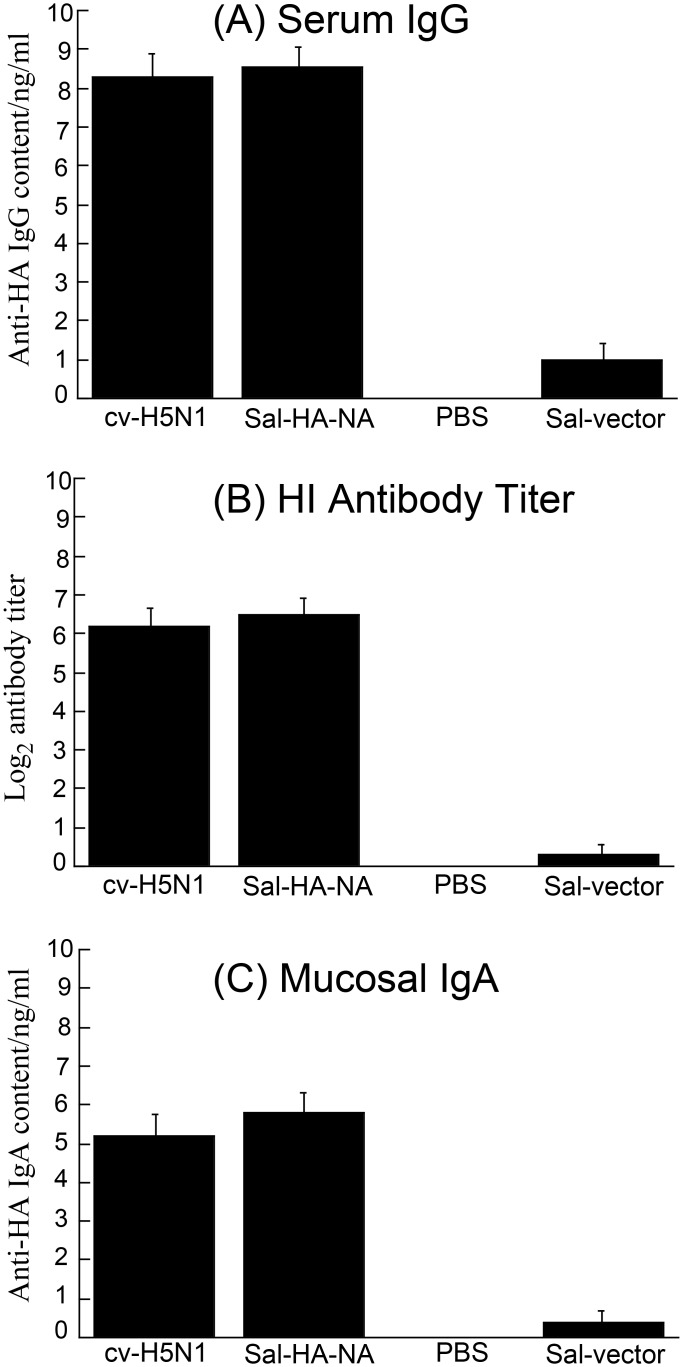
To study the effects of Salmonella vaccines on humoral responses in BALB/c mice, ELISA was carried out to assay the levels of serum antibodies at 0, 16, 32, 42 day after immunization (Fig 4) [42]. At day 42, mice immunized with vaccine Sal-HA-NA, in which SL368 carried constructs p5HA and p5NA, displayed higher (p < 0.01) anti-HA serum IgG levels compared to those immunized with the control vaccine Sal-vector, which carried the empty vector pVAX1 (Fig 4A). Indeed, Sal-HA-NA induced similar anti-HA serum IgG levels as the H5N1 commercial vaccine cv-H5N1 (Fig 4A). The functional activities of the sera from the vaccinated mice were further investigated by determining the antibody titers for hemagglutination inhibition (HI) against influenza virus. Consistent with our results of the serum anti-HA IgG response induced by the vaccines (Fig 4A), mice immunized with Sal-HA-NA also displayed comparable HI antibody titers as those immunized with the commercial H5N1 vaccine, cv-H5N1, and exhibited higher HI antibody titers (p < 0.01) than those with control Sal-vector (Fig 4B).
Fig 4. Antibody titers of anti-HA serum IgG (A), serum hemagglutination inhibition (HI)(B), and anti-HA mucosal IgA (C) detected by ELISA in immunized mice at 42 days after immunization.
Mice were immunized intragastrically at day 0, 14, and 28 with PBS only, the commercial H5N1 vaccine (cv-H5N1), and Salmonella SL368 carrying the empty vector pVAX1 (Sal-vector) and constructs p5HA and p5NA (Sal-HA-NA). Pool serum or mucosal wash samples (n = 5) from mice within a group were assayed and analyzed by two-way ANOVA. *p < 0.01. The assays were performed in triplicate and the experiments were repeated three times. The values obtained were the average from these experiments.
To study the effects of Salmonella vaccines on mucosal antibody responses in BALB/c mice, ELISA was also used to assay the anti-HA IgA levels in the mucosal nasal wash at 0, 16, 32, 42 days after immunization [43]. Mice immunized with vaccine Sal-HA-NA displayed higher anti-HA IgA levels (p < 0.01) compared to those immunized with control Sal-vector (Fig 4C). Indeed, vaccine Sal-HA-NA induced similar levels of mucosal anti-HA IgA as the H5N1 commercial vaccine cv-H5N1 (Fig 4C). These results suggest that the SL368-based vaccine enhances antigen-specific mucosal IgA as well as serum IgG responses.
Antigen specific T cell responses induced by the vaccines
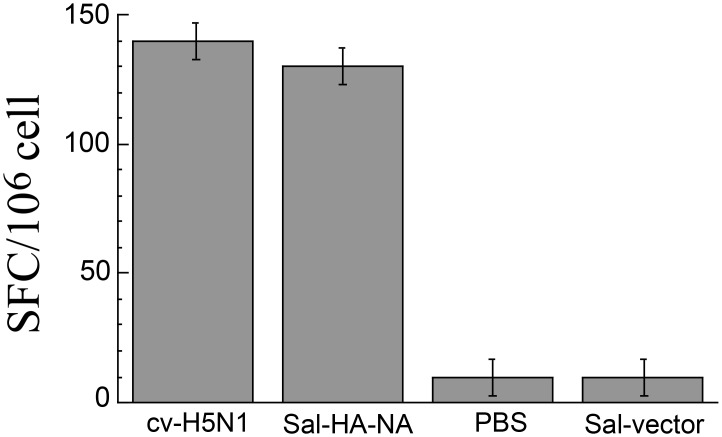
To study the HA-specific T cell responses induced by attenuated Salmonella vaccines, splenocytes (106 cells) were isolated from vaccinated mice 42 days after oral administration, and stimulated with HA533–541 epitope peptide (IYSTVASSL). This peptide, which is common to most of influenza A virus strains, is considered to be an immunodominant MHC class I epitope (Kd restricted) and can induce CD8+ T-cell responses in BALB/C mice [32]. Salmonella Sal-HA-NA induced higher (p < 0.01) anti-HA IFN-γ producing T cell responses than control Sal-vector (Fig 5). Indeed, the level of IFN-γ producing T cell responses induced by Sal-HA-NA was comparable to that by the commercial H5N1 vaccine cv-H5N1 (Fig 5). These results suggest that SL368-based vaccines induce antigen-specific T cell responses.
Fig 5. ELISPOT analysis of IFN-γ production by HA533–541 specific T cells in vaccinated mice at 42 days after immunization.
Mice were immunized intragastrically at day 0, 14, and 28 with PBS, the commercial H5N1 vaccine (cv-H5N1), and Salmonella SL368 carrying the empty vector pVAX1 (Sal-vector) and constructs p5HA and p5NA (Sal-HA-NA). Splenocytes (n = 5) were harvested from immunized mice at 42 days post immunization and stimulated with HA533–541 peptide for 48 hours. The results were expressed as spot-forming cells (SFC) per million cells. The assays were performed in triplicate and the experiments were repeated three times. The values obtained were the average from these experiments. Statistical analysis was performed by two-way ANOVA. *p < 0.01.
Immune protection of mice from virus challenge induced by the vaccines
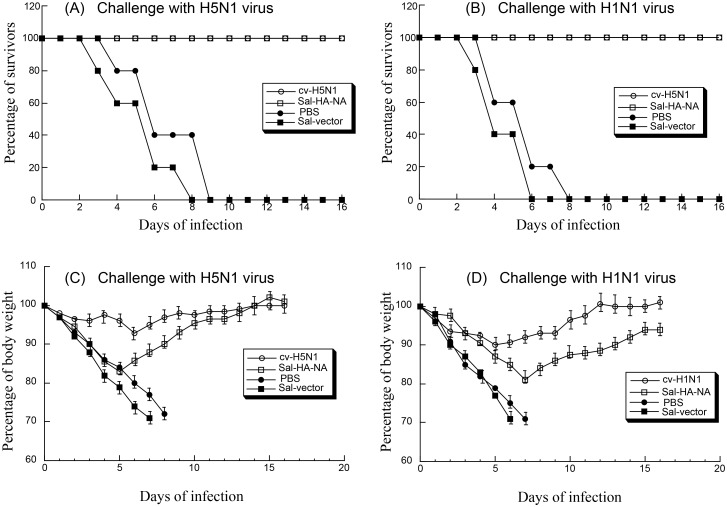
Our observations of strong virus specific humoral and cellular responses suggest that vaccine Sal-HA-NA may provide immune protection to challenge of the H5N1 virus and, possibly, H1N1 virus since the NA proteins of both viruses are similar. To determine if the constructed Salmonella vaccines can induce H5N1 virus-specific and H1N1 virus-specific immune protection, mice were immunized with different vaccines at day 0, 14, and 28, and then isoflurane-anesthetized and intranasally challenged with lethal doses of highly pathogenic H1N1 and H5N1 viruses at day 42 (i.e. two weeks after the final immunization). Animals were closely monitored for weight loss and mortality for 16 days post challenge (Fig 6A–6D). Humane (non-lethal) endpoints were used during the survival experiments and mice were euthanized with overdose inhalational CO2 to limit suffering, when they exhibited weight loss of more than 30%, lethargy, ruffled hair coat, or hunched posture. Our results showed that mice vaccinated with the H5N1 commercial vaccine cv-H5N1 and vaccine Sal-HA-NA exhibited no loss of body weight and showed 100% protection against A/Viet Nam/1194R (H5N1) virus challenge after 16 days post challenge (Fig 6A and 6B). When challenged with A/Puerto Rico/8/34 (H1N1) virus, the mice vaccinated with the H1N1 commercial vaccine cv-H1N1 exhibited no body weight loss and showed 100% protection (Fig 6C and 6D). All mice immunized with Sal-HA-NA survived after challenge with A/Puerto Rico/8/34 (H1N1) virus and regained about 90% body weight by day 16 after challenge (Fig 6C and 6D). Mice administered with control Sal-vector or PBS exhibited significant body weight loss and exhibited no protection against either H5N1 or H1N1 virus challenge (Fig 6). These results suggest that SL368-based vaccine provides immune protection against both H5N1 and H1N1 influenza viruses.
Fig 6. Immune protection of mice from lethal H5N1 (A and C) and H1N1 viral challenge (B and D).
Groups of mice (n = 5) were intragastrically immunized three times at day 0, 14, and 28 with PBS only, the commercial H5N1 (cv-H5N1) and H1N1 vaccines (cv-H1N1), and Salmonella SL368 carrying the empty vector pVAX1 (Sal-vector) and constructs p5HA and p5NA (Sal-HA-NA), and then challenged intranasally with 20 LD50 of lethal H5N1 (A/Viet Nam/1194R) and H1N1 (A/Puerto Rico/8/34) viruses at two weeks after final immunization (i.e. at 42 days post initial immunization). Mice were monitored for survival (A and B) and weight loss (C and D) throughout a 16 day observation period. The results are presented in terms of percent survival and percent of body weight (at the beginning of the trial) respectively. Humane (non-lethal) endpoints were used during the survival experiments and mice were euthanized with overdose inhalational CO2 when they exhibited weight loss of more than 30%, lethargy, ruffled hair coat, or hunched posture.
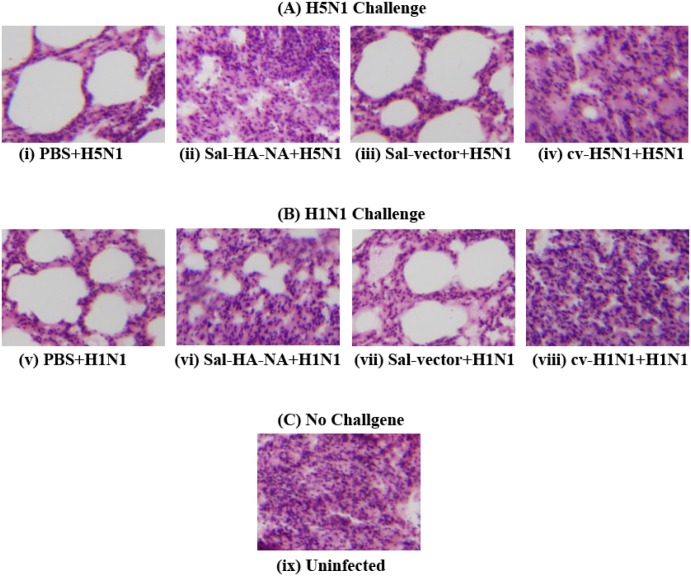
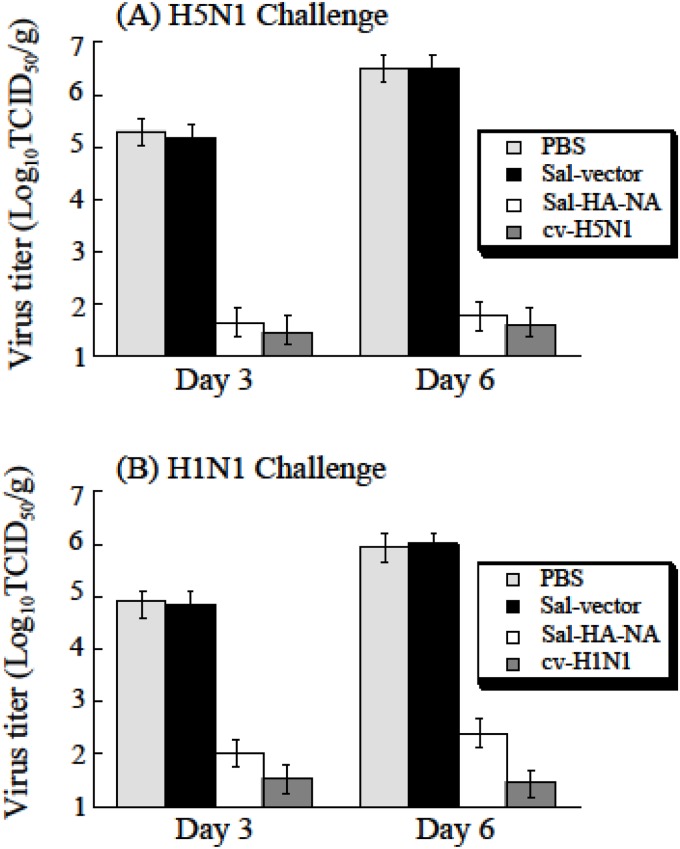
To further study the effect of the Salmonella vaccines on virus-specific immune protection, histological studies were performed with the mice vaccinated and challenged with A/Viet Nam/1194R (H5N1) and A/Puerto Rico/8/34 (H1N1) (Fig 7). At 7 days post-challenge, the lung of the animals were harvested immediately following euthanasia, fixed with 10% formaldehyde, embedded in paraffin and cut into sections. Sections were stained with hematoxylin and eosin, and then examined for histopathologic changes. As expected, no lesion was found in the lungs of uninfected mice (Fig 7C). Mice treated with PBS or control Sal-vector had pulmonary lesions consisting of substantial necrotizing bronchitis and histocytic alveolitis with associated pulmonary edema (Fig 7A(i, iii) and 7B(v, vii)). Mice vaccinated with vaccine Sal-HA-NA, and the H5N1 and H1N1 commercial vaccines (cv-H5N1 and cv-H1N1) lacked lesions in the lung and exhibited minimal bronchitis (Fig 7A(ii, iv) and 7B(vi, viii)). To investigate if immunization with Sal-HA-NA can inhibit local replication of the challenge viruses, lung tissues were harvested from animals at 3 and 6 days post-challenge and the virus titers in these tissues were determined. The titers of H5N1 virus in animals vaccinated with Sal-HA-NA and cv-H5N1 at 6 days post challenge were at least 10,000 fold lower than those in animals administered with PBS or Sal-vector (Fig 8A). Similarly, the titers of H1N1 virus in animals vaccinated with Sal-HA-NA and cv-H1N1 at 6 days post challenge were at least 2,000 fold lower than those in animals administered with PBS or Sal-vector (Fig 8B). These observations are consistent with our immune protection results (Fig 6) and suggest that the SL368-based vaccines can induce effective protection against highly pathogenic H5N1 and H1N1 influenza virus challenge.
Fig 7. Photomicrographs of hematoxylin- and eosin-stained lung sections of mice at 7 days post-challenge.
Mice were intragastrically immunized three times at day 0, 14, and 28 with PBS (i and v), the commercial H5N1 (cv-H5N1) (iv) and H1N1 vaccines (cv-H1N1) (viii), and Salmonella SL368 carrying the empty vector pVAX1 (Sal-vector) (iii and vii) and constructs p5HA and p5NA (Sal-HA-NA) (ii and vi), and then challenged intranasally with 20 LD50 of lethal H5N1 (A/Viet Nam/1194R) and H1N1 (A/Puerto Rico/8/34) viruses at two weeks after final immunization. (A) mice challenged with H5N1 virus; (B) mice challenged with H1N1 virus; (C) uninfected mice with no virus challenge.
Fig 8. Virus titers in the lungs of mice challenged with H5N1 and H1N1 viruses.
Mice were intragastrically immunized three times at day 0, 14, and 28 with PBS, the commercial H5N1 (cv-H5N1) and H1N1 vaccines (cv-H1N1), and Salmonella SL368 carrying the empty vector pVAX1 (Sal-vector) and constructs p5HA and p5NA (Sal-HA-NA), and then challenged intranasally with 20 LD50 of lethal H5N1 (A/Viet Nam/1194R) and H1N1 (A/Puerto Rico/8/34) viruses at two weeks after final immunization. Lung tissues were harvested at 3 and 6 days post challenge and viral titers were determined. The experiments were performed in triplicate and were repeated three times, and the standard deviation is indicated by the error bar. The limit of detection was 1.0 log10TCID50/g.
Discussion
Influenza A viruses continue to pose a public health threat to humans and animals [1]. Consequently, there is an urgent need for effective vaccines against these emerging infectious pathogens [44]. Intranasal influenza virus vaccines, while effective, may not be suitable for persons with asthma and certain chronic airway or pulmonary diseases [45]. Oral vaccines may represent an alternative to be used against influenza virus infection. In addition, oral vaccines are cost effective and operate conveniently because they eliminate the use of syringes and needles and thus are an affordable choice for mass vaccination. In this report, a novel attenuated S. typhimurium strain, SL368, was constructed and used as an oral vaccine vector for expressing HA and NA proteins of H5N1 influenza virus. Using BALB/c mice as the model system, we showed that the Salmonella-based vaccine, Sal-HA-NA, elicited anti-HA-specific humoral and T cell responses and induced immune protection against H5N1 and H1N1 virus challenge in immunized mice. These results provide direct evidence to suggest that attenuated Salmonella (spiR -) strains expressing viral antigens represent promising oral vaccines against influenza virus infection.
Attenuated Salmonella represent unique and promising gene delivery tool for developing vaccine against infectious pathogens. First, as vaccines, the Salmonella-based vectors may be safe and can be administered orally. The currently-used antityphoid fever vaccine is derived from an attenuated Salmonella strain [46, 47]. Second, in the poultry industry, attenuated Salmonella vaccines might have unique potential for anti-influenza application, where inexpensive mass immunization can be achieved through drinking water or spray cabinet administration [48]. Finally, Salmonella-based vectors are highly immunogenic in inducing both innate and adaptive immune responses, due to the bacteria-encoded surface antigens such as lipopolysaccharide (LPS), and therefore can enhance the antigen-specific immune responses induced by the expression of the viral proteins [46, 49].
Attenuated Salmonella strains have been shown to function as oral vaccines against influenza virus infections by expressing different viral antigens [7, 26, 50]. For example, the recent seminal studies carried out by Curtiss and colleagues have shown the utility of attenuated Salmonella strains as oral vaccine candidates against influenza viruses [7, 26]. Anti-influenza vaccines were constructed based on an attenuated Salmonella mutant with the deletion of sifA gene [7]. The sifA gene encodes a secreted effector protein of the Type III secretion system (T3SS) of SPI-2 [51]. The SPI-2 proteins are important for Salmonella intracellular survival and virulence in vivo [23–25]. Salmonella-based vaccines with mutations in the sifA gene have been shown to elicit both humoral and cellular immune responses and induce immune protection against influenza virus infection in mice [7, 26].
In our study, attenuated Salmonella strain SL368 was derived from auxotrophic strain SL7207 [34] and, in addition, contained a deletion of a part of spiR. SpiR is required for the expression of many Salmonella Pathogenicity Island-2 (SPI-2) genes including SifA [28]. Thus, SL368, with a deletion at spiR, is expected to exhibit minimal virulence (Fig 3) and be even less virulent than those mutants with the deletion of a single SPI-2 T3SS factor such as sifA. Moreover, SL368 exhibited excellent gene transfer activity as efficient expression of viral HA and NA proteins was found in cells and in mice treated with the SL368-derived vaccines (Fig 2). Furthermore, the SL368-derived vaccines elicited both HA-specific humoral and T cell immune responses and induced immune protection against influenza virus infection in mice (Figs 4–8). These results suggest that attenuated Salmonella strains with the mutations at spiR represent novel vaccine vectors against influenza virus infection.
The exact mechanism of how Salmonella carry out gene transfer is not currently understood completely. In our delivery system, attenuated Salmonella were constructed and transformed with plasmid constructs containing transgenes (i.e. HA and NA) under the control of a eukaryotic expression promoter [18–20]. In cells (e.g. macrophages) infected by Salmonella, plasmid DNA can be released and transported to the nuclei, leading to the expression of the transgene [18, 21, 22]. As under the eukaryotic expression promoter, the antigens are only expressed and processed for antigen presentation in Salmonella-infected cells (e.g. macrophages and dendritic cells) and are not exposed to the environment of the digestive tract. Once inside the cells, the attenuated Salmonella will be lysed and the plasmid DNA will be released and transported to the nuclei. The antigen expression cassette should be in a plasmid instead of the bacterial genome to facilitate its transport to the nuclei. Additional studies on the process and mechanism of Salmonella-mediated gene delivery would facilitate the generation of Salmonella-based vectors for vaccine development.
One of the ultimate goals for prevention of influenza outbreak is to develop a vaccine that can provide cross-protective immunity against many influenza virus strains. It is interesting to note in our results that vaccine Sal-HA-NA, which expressed the HA and NA proteins of an H5N1 virus, also provided strong protection against an H1N1 virus strain in addition to the H5N1 virus. Our results of the cross-protective immunity by Sal-HA-NA suggest that attenuated Salmonella vector simultaneously carrying expression cassettes for various antigens can function as a vaccine candidate against multiple strains of influenza viruses.
Little is currently known about how our vaccine elicited cross-protective immunity. It is possible that the HA protein expressed in Sal-HA-NA, which is from an H5N1 virus, may elicit cross-protective immune responses against the H1N1 virus, because of potential HA sequence homology between H5N1 and H1N1 viruses [52]. Furthermore, it is also conceivable that the cross-protective immunity against multiple influenza viruses induced by Sal-HA-NA may be due to the expression of the NA protein, which is also from an H5N1 virus and which may share sequence homology with the NA proteins from H1N1 viruses. Previous studies have implicated the roles of NA in cross-protective immunity against influenza viruses [53, 54]. A VLP vaccine expressing the N1 protein was found to elicit cross-protective responses against H5N1 and H1N1 viruses while a DNA vaccine designed to generate anti-human N1 response could induce partial cross immunity against H5N1 virus [53, 54]. It will be interesting to determine if Sal-HA-NA vaccine may also elicit immunity against other influenza A viruses expressing HA and NA antigens such as H3N2 and H7N9 viruses. Further studies on the nature of immune responses elicited by Sal-HA-NA and other Salmonella-based vaccines against these viruses should provide insight into developing novel vaccines against influenza virus infections.
We recognize that the BALB/c mice model used in our study has limitations in the evaluation of the constructed vaccines. The immune responses observed in the mouse model may not truly reflect those in humans when immunized with the vaccines and infected with influenza viruses. Additional studies are needed to study the effect of Salmonella-based influenza vaccines in other animal models as well as in humans. Future studies on these issues, as well as on the construction of new attenuated Salmonella strains with novel mutations for expressing different viral proteins and antigenic regions, should facilitate the development of Salmonella-based vaccines against influenza virus infection.
Supporting Information
(DOCX)
(DOCX)
Acknowledgments
We are grateful to Phong Trang, Yuan-Chuan Chen, Lei Lei, Caifeng Meng, Kuiyou Lu, Wenmin Fu, and Marco Paliza-Carre for critical comments, reagents, and technical assistance.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research has been supported by grants from National Basic Research Program of China (973 Program; No. 2011CB504800 and 2012CB518900), National Natural Science Foundation of China (No. 31100128, 81030031, 31230005, and 812111146), National Mega Project on Major Drug Development (2009ZX09103-678), National Small Business Innovation and Research (SBIR) Program of China, the Technology R & D Program of Jiangsu Province, China (BG20077035 and BG2008662), and NIH (RO1-AI041927, RO1-AI091536, and RO1-DE014842). MR was partially supported by a Chancellor’s Graduate Fellowship and a Hellman Family Graduate Fellowship from University of California at Berkeley. MR and JS were also partially supported by a block grant from the Graduate Division of University of California at Berkeley. Jiangsu Affynigen Biotechnologies, Inc provided support in the form of salaries for authors Zhu Yang and Yu Wang, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Palese P, Shaw ML. Orthomyxoviridae: The Viruses and Their Replication In: Knipe DM, Howley PM, editors. Fields Virology. 2 Philadelphia, Pa.: Lippincott-William & Wilkins; 2007. p. 1648–89. [Google Scholar]
- 2. Jang H, Boltz D, Sturm-Ramirez K, Shepherd KR, Jiao Y, Webster R, et al. From the Cover: Highly pathogenic H5N1 influenza virus can enter the central nervous system and induce neuroinflammation and neurodegeneration. Proceedings of the National Academy of Sciences. 2009;106(33):14063–8. 10.1073/pnas.0900096106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Song MS, Oh TK, Pascua PN, Moon HJ, Lee JH, Baek YH, et al. Investigation of the biological indicator for vaccine efficacy against highly pathogenic avian influenza (HPAI) H5N1 virus challenge in mice and ferrets. Vaccine. 2009;27(24):3145–52. Epub 2009/05/19. 10.1016/j.vaccine.2009.03.061 S0264-410X(09)00486-1 [pii]. . [DOI] [PubMed] [Google Scholar]
- 4. Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, et al. Antigenic and Genetic Characteristics of Swine-Origin 2009 A(H1N1) Influenza Viruses Circulating in Humans. Science. 2009;325(5937):197–201. 10.1126/science . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Smith GJ, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459(7250):1122–5. Epub 2009/06/12. nature08182 [pii] 10.1038/nature08182 . [DOI] [PubMed] [Google Scholar]
- 6. Jagger BW, Memoli MJ, Sheng ZM, Qi L, Hrabal RJ, Allen GL, et al. The PB2-E627K Mutation Attenuates Viruses Containing the 2009 H1N1 Influenza Pandemic Polymerase. mBio. 2010;1(1):e00067–10-e-10. 10.1128/mBio.00067-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ashraf S, Kong W, Wang S, Yang J, Curtiss R. Protective cellular responses elicited by vaccination with influenza nucleoprotein delivered by a live recombinant attenuated Salmonella vaccine. Vaccine. 2011;29(23):3990–4002. 10.1016/j.vaccine.2011.03.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tao P, Luo M, Zhu D, Qu S, Yang Z, Gao M, et al. Virus-like particle vaccine comprised of the HA, NA, and M1 proteins of an avian isolated H5N1 influenza virus induces protective immunity against homologous and heterologous strains in mice. Viral Immunol. 2009;22(4):273–81. Epub 2009/07/15. 10.1089/vim.2009.0017 . [DOI] [PubMed] [Google Scholar]
- 9. Xu K, Ling ZY, Sun L, Xu Y, Bian C, He Y, et al. Broad humoral and cellular immunity elicited by a bivalent DNA vaccine encoding HA and NP genes from an H5N1 virus. Viral Immunol. 2011;24(1):45–56. Epub 2011/02/16. 10.1089/vim.2010.0056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen JR, Ma C, Wong CH. Vaccine design of hemagglutinin glycoprotein against influenza. Trends Biotechnol. 2011;29(9):426–34. Epub 2011/06/07. 10.1016/j.tibtech.2011.04.007 S0167-7799(11)00073-4 [pii]. . [DOI] [PubMed] [Google Scholar]
- 11. Prabhu N, Prabakaran M, Ho HT, Velumani S, Qiang J, Goutama M, et al. Monoclonal antibodies against the fusion peptide of hemagglutinin protect mice from lethal influenza A virus H5N1 infection. J Virol. 2009;83(6):2553–62. Epub 2008/12/26. 10.1128/JVI.02165-08 JVI.02165-08 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Babiuk LA, Pontarollo R, Babiuk S, Loehr B, van Drunen Littel-van den Hurk S. Induction of immune responses by DNA vaccines in large animals. Vaccine. 2003;21(7–8):649–58. Epub 2003/01/18. S0264410X02005741 [pii]. . [DOI] [PubMed] [Google Scholar]
- 13. Ulmer JB, Donnelly JJ, Parker SE, Rhodes GH, Felgner PL, Dwarki VJ, et al. Heterologous protection against influenza by injection of DNA encoding a viral protein. Science. 1993;259(5102):1745–9. Epub 1993/03/19. . [DOI] [PubMed] [Google Scholar]
- 14. Donnelly JJ, Wahren B, Liu MA. DNA vaccines: progress and challenges. J Immunol. 2005;175(2):633–9. Epub 2005/07/09. 175/2/633 [pii]. . [DOI] [PubMed] [Google Scholar]
- 15. Luo M, Qu X, Pan R, Zhu D, Zhang Y, Wu J, et al. The virus-induced signaling adaptor molecule enhances DNA-raised immune protection against H5N1 influenza virus infection in mice. Vaccine. 2011;29(14):2561–7. 10.1016/j.vaccine.2011.01.060 [DOI] [PubMed] [Google Scholar]
- 16. Cardenas L, Clements JD. Oral immunization using live attenuated Salmonella spp. as carriers of foreign antigens. Clin Microbiol Rev. 1992;5(3):328–42. Epub 1992/07/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cheminay C, Hensel M. Rational design of Salmonella recombinant vaccines. Int J Med Microbiol. 2008;298(1–2):87–98. Epub 2007/09/25. S1438-4221(07)00116-6 [pii] 10.1016/j.ijmm.2007.08.006 . [DOI] [PubMed] [Google Scholar]
- 18. Bai Y, Gong H, Li H, Vu GP, Lu S, Liu F. Oral delivery of RNase P ribozymes by Salmonella inhibits viral infection in mice. Proc Natl Acad Sci U S A. 2011;108(8):3222–7. Epub 2011/02/09. 1014975108 [pii] 10.1073/pnas.1014975108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Atkins HS, Morton M, Griffin KF, Stokes MG, Nataro JP, Titball RW. Recombinant Salmonella vaccines for biodefence. Vaccine. 2006;24(15):2710–7. Epub 2006/01/26. S0264-410X(05)01300-9 [pii] 10.1016/j.vaccine.2005.12.046 . [DOI] [PubMed] [Google Scholar]
- 20. Paterson GK, Maskell DJ. Recent advances in the field of Salmonella Typhi vaccines. Hum Vaccin. 2010;6(5):379–84. Epub 2010/06/11. 10755 [pii]. . [DOI] [PubMed] [Google Scholar]
- 21. Jiang X, Gong H, Chen YC, Vu GP, Trang P, Zhang CY, et al. Effective inhibition of cytomegalovirus infection by external guide sequences in mice. Proc Natl Acad Sci U S A. 2012;109(32):13070–5. 10.1073/pnas.1201620109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Loessner H, Endmann A, Rohde M, Curtiss R III, Weiss S. Differential effect of auxotrophies on the release of macromolecules by Salmonella enterica vaccine strains. FEMS Microbiol Lett. 2006;265(1):81–8. Epub 2006/10/13. FML470 [pii] 10.1111/j.1574-6968.2006.00470.x . [DOI] [PubMed] [Google Scholar]
- 23. Abrahams GL, Hensel M. Manipulating cellular transport and immune responses: dynamic interactions between intracellular Salmonella enterica and its host cells. Cell Microbiol. 2006;8(5):728–37. 10.1111/j.1462-5822.2006.00706.x . [DOI] [PubMed] [Google Scholar]
- 24. Galan JE. Salmonella interactions with host cells: type III secretion at work. Annu Rev Cell Dev Biol. 2001;17:53–86. 10.1146/annurev.cellbio.17.1.53 . [DOI] [PubMed] [Google Scholar]
- 25. Waterman SR, Holden DW. Functions and effectors of the Salmonella pathogenicity island 2 type III secretion system. Cell Microbiol. 2003;5(8):501–11. . [DOI] [PubMed] [Google Scholar]
- 26. Kong W, Brovold M, Koeneman BA, Clark-Curtiss J, Curtiss R III. Turning self-destructing Salmonella into a universal DNA vaccine delivery platform. Proc Natl Acad Sci U S A. 2012;109(47):19414–9. 10.1073/pnas.1217554109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Paglia P, Terrazzini N, Schulze K, Guzman CA, Colombo MP. In vivo correction of genetic defects of monocyte/macrophages using attenuated Salmonella as oral vectors for targeted gene delivery. Gene Ther. 2000;7(20):1725–30. Epub 2000/11/18. 10.1038/sj.gt.3301290 . [DOI] [PubMed] [Google Scholar]
- 28. Bijlsma JJ, Groisman EA. The PhoP/PhoQ system controls the intramacrophage type three secretion system of Salmonella enterica. Mol Microbiol. 2005;57(1):85–96. 10.1111/j.1365-2958.2005.04668.x . [DOI] [PubMed] [Google Scholar]
- 29. Gu H, Qi X, Li X, Jiang H, Wang Y, Liu F, et al. Rapid and specific detection of H3 swine influenza virus using reverse transcription loop-mediated isothermal amplification method. J Appl Microbiol. 2010;108(4):1145–54. 10.1111/j.1365-2672.2009.04520.x . [DOI] [PubMed] [Google Scholar]
- 30. Li X, Qi X, Miao L, Wang Y, Liu F, Gu H, et al. Detection and subtyping of influenza A virus based on a short oligonucleotide microarray. Diagn Microbiol Infect Dis. 2009;65(3):261–70. 10.1016/j.diagmicrobio.2009.07.016 . [DOI] [PubMed] [Google Scholar]
- 31. Yang Z, Mao G, Liu Y, Chen YC, Liu C, Luo J, et al. Detection of the pandemic H1N1/2009 influenza A virus by a highly sensitive quantitative real-time reverse-transcription polymerase chain reaction assay. Virol Sin. 2013;28(1):24–35. 10.1007/s12250-013-3290-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Deng Y, Yewdell JW, Eisenlohr LC, Bennink JR. MHC affinity, peptide liberation, T cell repertoire, and immunodominance all contribute to the paucity of MHC class I-restricted peptides recognized by antiviral CTL. J Immunol. 1997;158(4):1507–15. Epub 1997/02/15. . [PubMed] [Google Scholar]
- 33. Gong H, Vu GP, Bai Y, Chan E, Wu R, Yang E, et al. A Salmonella small non-coding RNA facilitates bacterial invasion and intracellular replication by modulating the expression of virulence factors. PLoS Pathog. 2011;7(9):e1002120 10.1371/journal.ppat.1002120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hoiseth SK, Stocker BA. Aromatic-dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature. 1981;291(5812):238–9. . [DOI] [PubMed] [Google Scholar]
- 35. Datsenko KA, Wanner BL. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc Natl Acad Sci U S A. 2000;97(12):6640–5. 10.1073/pnas.120163297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lu S, Killoran PB, Fang FC, Riley LW. The global regulator ArcA controls resistance to reactive nitrogen and oxygen intermediates in Salmonella enterica serovar Enteritidis. Infect Immun. 2002;70(2):451–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lu S, Riley LW. The Global Regulator ArcA Controls Resistance to Reactive Nitrogen and Oxygen Intermediates in Salmonella enterica Serovar Enteritidis. Infection and Immunity. 2002;70(2):451–61. 10.1128/iai.70.2.451-461.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Szretter KJ, Balish AL, Katz JM. Influenza: propagation, quantification, and storage. Curr Protoc Microbiol. 2006;Chapter 15:Unit 15G 1. Epub 2008/09/05. 10.1002/0471729256.mc15g01s3 . [DOI] [PubMed] [Google Scholar]
- 39. Bai Y, Li H, Vu GP, Gong H, Umamoto S, Zhou T, et al. Salmonella-mediated delivery of RNase P-based ribozymes for inhibition of viral gene expression and replication in human cells. Proc Natl Acad Sci U S A. 2010;107(16):7269–74. 10.1073/pnas.0912813107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yang N, Zhu X, Chen L, Li S, Ren D. Oral administration of attenuated S. typhimurium carrying shRNA-expressing vectors as a cancer therapeutic. Cancer Biol Ther. 2008;7(1):145–51. . [DOI] [PubMed] [Google Scholar]
- 41. Walthers D, Carroll RK, Navarre WW, Libby SJ, Fang FC, Kenney LJ. The response regulator SsrB activates expression of diverse Salmonella pathogenicity island 2 promoters and counters silencing by the nucleoid-associated protein H-NS. Mol Microbiol. 2007;65(2):477–93. 10.1111/j.1365-2958.2007.05800.x . [DOI] [PubMed] [Google Scholar]
- 42. Prabakaran M, He F, Meng T, Madhan S, Yunrui T, Jia Q, et al. Neutralizing epitopes of influenza virus hemagglutinin: target for the development of a universal vaccine against H5N1 lineages. J Virol. 2010;84(22):11822–30. Epub 2010/09/17. 10.1128/JVI.00891-10 JVI.00891-10 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Park KS, Lee J, Ahn SS, Byun YH, Seong BL, Baek YH, et al. Mucosal immunity induced by adenovirus-based H5N1 HPAI vaccine confers protection against a lethal H5N2 avian influenza virus challenge. Virology. 2009;395(2):182–9. Epub 2009/10/20. 10.1016/j.virol.2009.09.018 S0042-6822(09)00578-9 [pii]. . [DOI] [PubMed] [Google Scholar]
- 44. Ogra PL, Faden H, Welliver RC. Vaccination strategies for mucosal immune responses. Clin Microbiol Rev. 2001;14(2):430–45. 10.1128/CMR.14.2.430-445.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Prevention CfDCa. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2004;53:1–40. 14724557 [Google Scholar]
- 46. Clairmont C, Lee KC, Pike J, Ittensohn M, Low KB, Pawelek J, et al. Biodistribution and genetic stability of the novel antitumor agent VNP20009, a genetically modified strain of Salmonella typhimurium. J Infect Dis. 2000;181(6):1996–2002. 10.1086/315497 . [DOI] [PubMed] [Google Scholar]
- 47. Levine MM, Herrington D, Murphy JR, Morris JG, Losonsky G, Tall B, et al. Safety, infectivity, immunogenicity, and in vivo stability of two attenuated auxotrophic mutant strains of Salmonella typhi, 541Ty and 543Ty, as live oral vaccines in humans. J Clin Invest. 1987;79(3):888–902. 10.1172/JCI112899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Liljebjelke KA, Petkov DI, Kapczynski DR. Mucosal vaccination with a codon-optimized hemagglutinin gene expressed by attenuated Salmonella elicits a protective immune response in chickens against highly pathogenic avian influenza. Vaccine. 2010;28(27):4430–7. Epub 2010/04/22. 10.1016/j.vaccine.2010.04.009 S0264-410X(10)00502-5 [pii]. . [DOI] [PubMed] [Google Scholar]
- 49. Vassaux G, Nitcheu J, Jezzard S, Lemoine NR. Bacterial gene therapy strategies. J Pathol. 2006;208(2):290–8. 10.1002/path.1865 . [DOI] [PubMed] [Google Scholar]
- 50. Tite JP, Gao XM, Hughes-Jenkins CM, Lipscombe M, O'Callaghan D, Dougan G, et al. Anti-viral immunity induced by recombinant nucleoprotein of influenza A virus. III. Delivery of recombinant nucleoprotein to the immune system using attenuated Salmonella typhimurium as a live carrier. Immunology. 1990;70(4):540–6. [PMC free article] [PubMed] [Google Scholar]
- 51. Brumell JH, Tang P, Zaharik ML, Finlay BB. Disruption of the Salmonella-containing vacuole leads to increased replication of Salmonella enterica serovar typhimurium in the cytosol of epithelial cells. Infect Immun. 2002;70(6):3264–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Xie H, Liu TM, Lu X, Wu Z, Belser JA, Katz JM, et al. A live attenuated H1N1 M1 mutant provides broad cross-protection against influenza A viruses, including highly pathogenic A/Vietnam/1203/2004, in mice. J Infect Dis. 2009;200(12):1874–83. 10.1086/648405 . [DOI] [PubMed] [Google Scholar]
- 53. Sandbulte MR, Jimenez GS, Boon AC, Smith LR, Treanor JJ, Webby RJ. Cross-reactive neuraminidase antibodies afford partial protection against H5N1 in mice and are present in unexposed humans. PLoS Med. 2007;4(2):e59 10.1371/journal.pmed.0040059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wu CY, Yeh YC, Chan JT, Yang YC, Yang JR, Liu MT, et al. A VLP vaccine induces broad-spectrum cross-protective antibody immunity against H5N1 and H1N1 subtypes of influenza A virus. PLoS One. 2012;7(8):e42363 10.1371/journal.pone.0042363 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.