Introduction
Each year, about one third of the elderly over 65 fall 1, 2, and fall-related injuries increase with age 3. Falls lead to functional decline, hospitalization, institutionalization, higher health care costs, and decreased quality of life 4–6; and rank as the sixth leading cause of death in older people 1. Similarly, elderly are a special group with respect to rising incidence rates of cancer 7. Cancer survivors are living longer but are continuing to encounter physical, psychosocial, and economic impacts until the end of life. The likelihood that an elderly cancer survivor experiences falls may be influenced by their cancer history 8–10. Disparities in the occurrence of falls among cancer survivors are beginning to emerge in the literature 11–15, and there is a need to understand whether the diagnosis of cancer increases the burden of falls. The purpose of this study was to examine community dwelling elderly to identify if individuals with a history of cancer fall at a higher rate than those without a cancer diagnosis; and if falls were influenced by individual characteristics, symptoms, or functional status.
Conceptual Framework
The conceptual framework for this study was a synthesis of the Life-Course Model of Aging 16 and the Health Related Quality of Life model 17. Early-life intrinsic biologic factors and mid-life medical care influence late-life health and disablement 16. Factors contributing to late-life outcomes are extrinsic variations, social capital, financial capital, human capital, health behaviors, and health status. Emotional and psychological factors are causal at every level in the model and are bidirectional. Figure 1 delineates a mechanism for the study of falls in the elderly with cancer. The conceptual framework was used to derive the hypothesis. The primary null hypothesis used in this study was that no correlation between characteristics, symptoms, functional status, cancer diagnosis and the health outcome of falls exists.
Figure 1.
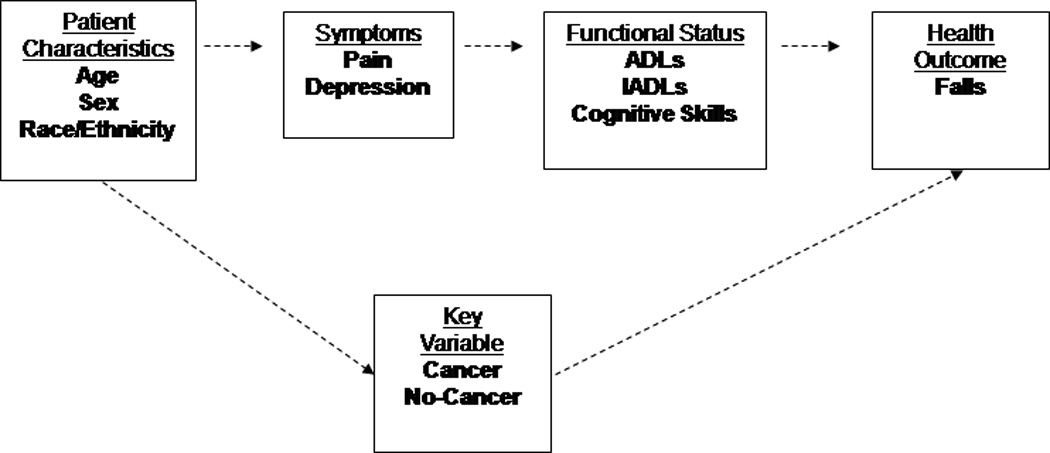
Framework for the Study of Cancer on Falls in Community Dwelling Elderly
Review of Literature
A major risk factor for falling is aging 18, and the risk of being seriously injured in a fall increases with age. Annually, 1 in 3 Americans, or 33% of older adults 65 and older, fall, and 40% of those 80 and older fall 19, 20. Additionally, elderly individuals often have comorbidities and disabilities which increase the occurrence of falls 21, 22.
Compounded with the general effects of aging, people are diagnosed with cancer at an older age and cancer survivors are living longer 23. Evidence has shown that cancer-related fatigue 24, 25 and pain 26, 27 influences functional status in elderly survivors increasing the risk of falls 28. Some evidence suggests that people with cancer fall more often than others 8–10 and that certain types of cancer 29, 30 or metastatic disease 30 may be associated with higher rates of falling. Three studies conducted in palliative care settings demonstrating the incidence rate of falls to be significantly higher 8,10,31. Both the rate of falls and risk of falling may be significantly higher for cancer survivors 8, 9.
Studying the incidence and impact of falls is significant because 20% of the population in the United States are 65 years and older 32. In 2006, health care utilization for older adults resulting from fall injuries included more than 1.8 million treated in emergency departments and more than 421,000 hospitalized 1. According to the Center for Disease Control, direct medical costs related to falls totaled $179 million for fatal falls and $19 billion for nonfatal falls 33. The known estimate of elderly cancer survivors is more than 6,000,000 34. Fifty-six percent of all new cancer diagnoses are among people 65 or older 21.
There are a host of risk factors related to falls in the elderly supported by evidence in the literature 35. Besides known risk factors in aging, people with cancer have added multiple risk factors for falls that include; neurotoxicity 36, fatigue 24, depression 9, postural hypotension 37, hypoesthesia 37, delirium 8, impaired cognitive function 9, 38, pain 25, gait and balance problems 39, loss of bone density 37, weight loss 40, reduced muscle strength 37, and Vitamin D deficiency 41.
Innovations in medical technology have led to earlier diagnoses and improved treatment of cancer 33, and consequently, people are living longer and developing chronic conditions. As the elderly population grows, cancer survivorship and the impact of falls and fall injuries will be felt on families and pervade our economic, health care, and social systems.
Little is known about whether the diagnosis of cancer increases the burden of falls in cancer survivors. The purpose of this study was to examine community dwelling elderly to identify if individuals with a history of cancer fall at a higher rate than those without a cancer diagnosis; and if falls were influenced by individual characteristics, symptoms, or functional status.
Methods
This retrospective, cross-sectional study carried out secondary analysis of the MDS. The purpose of the study was to examine the occurrence of falls in low income community dwelling settings, with or without a history of cancer diagnosis. The study was approved by the Internal Review Board of the sponsoring university. The sample included low income and community-dwelling patients 65 years of age and older classified who were enrolled in the Home and Community Based Service (HCBS) program during 2007. The median age of enrollees in the HSCB program was 72; with multiple comorbidities: 75% with arthritis, 69% with hypertension, 67% with heart disease, 39% with diabetes, and 15% with cancer. Eligibility for admittance to the HCBS includes financial eligibility below 300% of the Federal Poverty Level and a required level of care similar to that a nursing facility level of care requirements (assistance with activities of daily living [ADL] and instrumental activities of daily living [IADL] needs) 42. In addition, those persons who were members of Health Maintenance Organizations were excluded.
Instrument and Measures
This secondary analysis focused on patient level data from the Minimum Data Set (MDS). The MDS is a person-centered assessment with uniform standards for the collection of minimum essential nursing data, enabling clinicians to assess multiple domains 42. The MDS in the HCBS program was modified in 1993 from the nursing home version, to inform and guide comprehensive care and service planning for community-dwelling elderly 42. The information on the MDS contains a combination of self-report by the patient and clinical validation by a Registered Nurse, which is collected in person, in the patient’s home upon entry into the HCBS program, and then every 180 days thereafter 42. The MDS validity and reliability is reported in an international trial, with independent dual assessment of 241 patients using 780 assessments, with a Kappa of .74 43.
The MDS data used in this study was obtained from one assessment closest to the date of December 31st, 2007. Variables in this study included: number of falls, age, gender, race/ethnicity; the diagnosis of cancer, ADLs, IADLs, cognitive skills, vision, incontinence, pain and depression. On the MDS, a fall is defined as an unexpected event in which the participant comes to rest on the ground, floor, or lower level. Falls are measured in ordinal frequency from 0 to 9 over the past 6-months, and for this study a faller was defined as a person who had at least one fall. Age is measured as a continuous variable, gender is dichotomous, and race/ethnicity is coded per census criteria. The remainder of the variables were ordinal: ADLs for bathing as independent, supervised, assisted, or total dependence; IADLs for activity difficulty level as none, some, or great; cognitive for daily decision making as independent, modified, impaired, or impaired; vision ability to see as adequate or levels of impairment; urinary continence as usually, occasionally, frequently or incontinent; depression or feelings of sadness as none, weekly, or daily; and pain as none, less than daily, or daily.
Statistical Analysis
Descriptive statistics were used to examine subject characteristics. Association between each categorical variable and falls was tested by using a univariate logistic regression model. A multivariate regression model was developed to determine significant interactions between the variables and falls. Multivariate regression is commonly used to fit mathematical models to data by tuning the free parameters of the model to provide a good fit 44. In this model, falls was the dependent variable. The independent variables were the following: age, gender, race/ethnicity; the diagnosis of cancer, ADLs, IADLs, cognitive skills, vision, incontinence, pain and depression. Statistical calculations were conducted by using SPSS software.
Results
7448 participants were enrolled in the HCBS program in 2007. The mean age was 80.92 years old, with 76.4% females, 74.3% white and 22% African American. Table 1 shows the demographic characteristics. A total of 2125 (28.5%) had experienced a fall, with 1123 (53%) had one fall and 1002 (47%) had more than one fall. A total of 967 (13.0%) had cancer; and of those with cancer, 263 (27.2%) had a fall.
Table 1.
Characteristics of Nonfallers and Fallers in Community Dwelling Elderly in the HCBS Program
| Characteristic |
Nonfallers n %* |
Fallers n %* |
Total n %* |
|---|---|---|---|
| Age Groups | |||
| 65–69 | 649 (12.2) | 261 (12.8) | 910 (12.2) |
| 70–74 | 818 (15.4) | 319 (15.6) | 1137 (15.3) |
| 75–79 | 960 (18.0) | 354 (17.4) | 1341 (17.6) |
| 80–84 | 1144 (21.5) | 438 (21.5) | 1582 (21.2) |
| 85–89 | 940 (7.7) | 356 (17.5) | 1296 (17.4) |
| 90–94 | 545 (10.2) | 207 (10.2) | 752 (10.1) |
| ≥95 | 267 (5.0) | 104 (5.1) | 371 (5.0) |
| Gender | |||
| Female | 4087 (71.8) | 1533 (28.2) | 5620 (76.4) |
| Male | 1236 (70.3) | 506 (29.7) | 1742 (23.6) |
| Race or ethnicity | |||
| White | 3799 (71.4) | 1670 (81.9) | 5469 (74.3) |
| African American | 1318 (24.8) | 300 (14.7) | 118 (22.0) |
| American Indian | 11 (.2) | 5 (.2) | 16 (0.2) |
| Asian and Pacific Islander | 28 (.5) | 5 (.2) | 33 (0.4) |
| Unknown | 101 (1.9) | 35 (1.7) | 136 (1.8) |
| Hispanic | 66 (1.2) | 24 (1.2) | 88 (1.2) |
| Cancer | |||
| No diagnosis of Cancer | 4588 (71.8) | 1762 (27.6) | 6350 (86.3) |
| Cancer not subject to treatment | 419 (74.8) | 138 (24.7) | 557 (7.9) |
| Cancer subject to treatment | 285 (68.9) | 125 (30.3) | 410 (5.8) |
| ADL (bathing assistance) | |||
| Independent | 887 (16.7) | 264 (12.9) | 1151 (19.0) |
| Supervision | 433 (8.1) | 137 (6.7) | 570 (7.9) |
| Assistance Transfer Only | 212 (4.0) | 90 (4.4) | 302 (4.3) |
| Assistance part of Bathing | 2650 (49.8) | 1229 (60.3) | 3879 (50.3) |
| Total Dependence | 1107 (20.8) | 301 (14.5) | 1408 (18.5) |
| IADL (how difficult it is to do an activity independently) | |||
| No Difficulty | 74 (1.4) | 20 (1.0) | 94 (1.3) |
| Some Difficulty | 924 (17.4) | 317 (15.5) | 1241 (17.0) |
| Great Difficulty | 4515 (81.1) | 1690 (82.9) | 6028 (81.7) |
| Cognitive skills (daily decision making) | |||
| Independent | 2069 (38.7) | 659 (32.3) | 2728 (36.9) |
| Modified Independence | 1628 (30.6) | 710 (34.8) | 2338 (32.6) |
| Moderately Impaired | 1199 (22.5) | 516 (25.3) | 1707 (23.2) |
| Severely Impaired | 401 (7.5) | 137 (6.7) | 538 (7.3) |
| Vision | |||
| Adequate | 3127 (58.7) | 1141 (56.0) | 4268 (57.9) |
| Impaired | 1547 (29.1) | 615 (30.2) | 2162 (29.7) |
| Moderately Impaired | 344 (6.5) | 148 (7.3) | 492 (6.7) |
| Highly Impaired | 176 (3.3) | 89 (4.4) | 265 (3.7) |
| Severely Impaired | 109 (2.0) | 38 (1.9) | 147 (2.0) |
| Incontinence | |||
| Continent | 2096 (39.4) | 698 (34.2) | 2794 (37.7) |
| Usually Continent | 825 (15.5) | 331 (16.2) | 1156 (15.8) |
| Occasionally Incontinent | 762 (14.3) | 341 (16.7) | 1103 (14.9) |
| Frequently Incontinent | 976 (18.3) | 474 (23.2) | 1450 (19.9) |
| Incontinent | 621 (11.7) | 177 (8.7) | 798 (10.7) |
| Depression | |||
| Not Exhibited in Last 30 days | 4130 (77.6) | 1377 (67.5) | 5507 (74.9) |
| Exhibited up to 5 days/Wk | 959 (18.0) | 514 (25.2) | 1473 (20.4) |
| Exhibited daily/Almost Daily | 182 (3.4) | 121 (5.9) | 303 (4.7) |
| Pain | |||
| No Pain | 1453 (27.3) | 455 (22.3) | 1908 (25.7) |
| Pain Less Than Daily | 1341 (25.2) | 421 (20.6) | 1762 (24.7) |
| Pain Daily | 2474 (46.5) | 1138 (55.8) | 3612 (49.6) |
A small number of values are missing and n % does not always equal 100
First, separate bivariate logistic regression models were used to examine the cross-sectional relationship between age, gender, race, cancer, ADLs, IADLs, cognitive status, vision, incontinence, depression, pain and falls respectively. Chi-square tests revealed the following results: race (p < .0001), ADL (p=.032), IADL (p=.021), cognitive skill status (p=.002), impaired vision (p=.030), incontinence (p=.023), depression (p=.000), and pain (p=.000) were significant predictors of one or more falls during 2007; while age (p=.677), gender (p=.149), and cancer (p=.732) were not significant. Pain was the only indicator that was inversely associated with falls in these models, with the more pain experienced, the more falls.
To better understand how specific features of each variable explain falls in the HCBS sample, significant factors in the final model will be discussed in relation to association with falls (see Table 1 and Table 3). All odd ratios (ORs) were expressed per 95% of the distribution of the parameter. For female versus male (reference group) (OR 1.20, 95% confidence interval [CI] 1.06–1.37, p = 0.005) indicating male gender was associated with fewer falls. For African American versus unknown race (reference group) (OR 0.61, CI 0.37–1.00, p = 0.040) indicating the African American was associated with fewer falls. For ADLs: supervision with transfer versus total dependence (reference group) (OR .97, CI 0.44–2.13, p = 0.018); for assistance with transfer for bathing versus total dependence (reference group) (OR 1.49, CI 0.67–3.34, p = 0.018); and some assistance with bathing versus total dependence (reference group) (OR 0.91, CI 0.42–1.97, p < 0.000) assistance with ADLs for bathing was associated with more falls. For continence versus incontinence (reference group) (OR 0.95, CI 0.77–1.17, p < 0.000); and frequently incontinent versus incontinence (reference group) (OR 1.34, CI 1.08–1.66, p = 0.001) indicating incontinence was associated with more falls. For no depression experienced versus depression daily (reference group) (OR .58, CI 0.46–0.75, p < .000) indicating depression was associated with more falls. Finally, for some pain versus pain daily (reference group) (OR 0.75, CI 0.65–0.86, p = .0111) indicating pain is associated with falls. In summary, these findings suggest that in the community dwelling elderly in this sample, males, who are white, dependent in ADLs, incontinent, depressed, and have daily pain, are more likely to fall.
Table 3.
Multivariate Logistic Regression Analysis of Odds Ratio Estimates in Final Model Predicting Falls
| Effect | Point Estimate |
95% Wald Confidence Limits |
|
|---|---|---|---|
| Gender: Male vs* Female | 1.203 | 1.059 | 1.367 |
| Age | 0.998 | 0.991 | 1.004 |
| Race | |||
| White vs Unknown | 1.091 | 0.675 | 1.763 |
| African American vs Unknown | 0.612 | 0.373 | 1.004 |
| American Indian v vs Unknown | 1.012 | 0.282 | 3.631 |
| Asian Pacific vs Unknown | 0.510 | 0.174 | 1.492 |
| Hispanic vs Unknown | 0.983 | 0.530 | 1.824 |
| ADL | |||
| Independent vs Total Dependence | 0.942 | 0.434 | 2.044 |
| Supervision vs Total Dependence | 0.971 | 0.442 | 2.134 |
| Transfer vs Total Dependence | 1.494 | 0.669 | 3.339 |
| Assist Bathing vs Total Dependence | 0.905 | 0.417 | 1.967 |
| Incontinence | |||
| Continent vs incontinent | 0.946 | 0.768 | 1.165 |
| Usually Continent vs Incontinent | 1.123 | 0.895 | 1.411 |
| Occasionally Continent vs Incontinent | 1.264 | 1.008 | 1.585 |
| Frequently Incontinent vs Incontinent | 1.340 | 1.082 | 1.660 |
| Depression | |||
| No depression vs depressed | 0.583 | 0.456 | 0.747 |
| Some depression vs depressed | 0.828 | 0.638 | 1.076 |
| Pain | |||
| No pain vs pain frequently | 0.785 | 0.687 | 0.897 |
| No pain vs pain daily | 0.748 | 0.653 | 0.856 |
vs means versus
A multivariate regression model with Maximum Likelihood Estimates with a Wald Chi-square was then used to examine interactions among the variables in order to construct the final model for this study. MLE is a method fitting mathematical models to data by freeing parameters of the model to provide a good fit 44. In separate MLE models, adjusting for the same covariates mentioned above (see Table 2 and 3) significant factors in the final model in this study on falls included: race, gender, ADLs, incontinence, depression, and pain. Factors that did not influence falls in the final model included: cancer, age, IADLs, and vision. In summary, the findings were somewhat different than findings in the literature and will be discussed in the following.
Table 2.
Multivariate Logistic Regression Analysis of Maximum Likelihood Estimates in Final Model Predicting Falls
| Parameter | DF* | Estimate | Standard Error |
Wald Chi-Square |
|---|---|---|---|---|
| Intercept | 1 | −0.9991 | 0.1626 | 37.7521 |
| Age | 1 | −0.0025 | 0.0034 | 0.5347 |
| Gender | 1 | 0.0924 | 0.0326 | 8.0522 |
| Race: White | 1 | 0.2674 | 0.1428 | 3.5067 |
| Race: African American | 1 | −0.3104 | 0.1509 | 4.2345 |
| Race: American Indian | 1 | 0.1926 | 0.5134 | 0.1408 |
| Race: Asian/Pacific | 1 | −0.4932 | 0.4248 | 1.3480 |
| Race: Hispanic | 1 | 0.1633 | 0.2158 | 0.5727 |
| ADL: Independent | 1 | −0.1567 | 0.0937 | 2.7967 |
| ADL: Supervision | 1 | −0.1260 | 0.1102 | 1.3065 |
| ADL: Supervision transfer | 1 | 0.3051 | 0.1290 | 5.5979 |
| ADL: Assistance Bathing | 1 | 0.2703 | 0.0783 | 11.9115 |
| ADL: Total Dependence | 1 | −0.1961 | 0.0950 | 4.2626 |
| Continent | 1 | −0.1732 | 0.0483 | 12.8467 |
| Usually Continent | 1 | −0.0011 | 0.0605 | 0.0004 |
| Frequently Incontinent | 1 | 0.1166 | 0.0604 | 3.7264 |
| Incontinent | 1 | 0.1753 | 0.0541 | 10.4958 |
| Depression: none | 1 | −0.2964 | 0.0499 | 35.2299 |
| Depression: exhibited | 1 | 0.0540 | 0.0561 | 0.9270 |
| No Pain | 1 | −0.0644 | 0.0439 | 2.1464 |
| Pain | 1 | −0.1130 | 0.0445 | 6.4528 |
DF=degrees of freedom
Discussion
This study was performed with the intention to better understand whether cancer influences falls in the community dwelling elderly. Additionally, this study was a first step in developing a conceptual framework specific to disability, disablement, and falls in community dwelling elderly with cancer.
Contrary to findings in other studies where patients may not volunteer or may forget to offer information concerning falls 45, the MDS seemed to be an effective instrument to measure a fall, incorporating questions that prompted recall of a fall in this sample. Furthermore, this study demonstrated that assessing falls using the MDS can offer information about Relative Risks in the community dwelling elderly.
The elderly in the HCBS program fall at a rate of occurrence of 28.5%, a high rate. The population was vulnerable (mean age 80.92 and 76.4% female), and diverse (25.7% non-white). This is an unusually high percentage of non-whites in a study sample, which historically has ranged from three to 10%, in randomized clinical trials 46. Additionally, the population examined had relatively compromised functional status (84.6% needing ADL assistance and 98.7% needing IADL assistance).
Little research has been conducted concerning falls in people with cancer; therefore comparing the results of this study to established norms is difficult. In two studies in the inpatient palliative care setting,18% 8 and 10% 10 of the cancer patients had a fall. These findings may be a result of limited amount of time out of bed, which is different when compared to the activity level of most community dwelling elderly. In a study of independent, high-functioning community dwelling elderly in an outpatient cancer program, 23% fell 9. While these rates are similar to the findings in this study, the samples had distinctly different levels of functioning (high-functioning compared to low-functioning). This pattern in distinctly different populations supports the notion that fall screening should take place in all populations, not just the obviously disabled.
Although the fall prediction model needs refinement and testing; cancer, IADLs, vision, and age were not found to be significant in the final model in this study. These findings are not consistent with geriatric medicine and nursing literature, and will each be discussed in the following paragraphs.
A limited amount of literature has suggested that individuals with a history of cancer are more likely to fall 8, 9, 30; this was not found in the present sample. This study identified a cancer diagnosis based on information on the MDS. The cancer diagnosis was categorized in three manners. The first was no cancer. The second was cancer with treatment which includes chemotherapy or radiation, or both. Finally, the third was cancer without treatment (more than likely treatment was finished or the patient was transferred to hospice care). No information on cancer was available on date of diagnosis, type, stage, or specific treatment, all of which are known to influence the functional status of cancer survivors. Additionally, fewer falls for cancer patients in this sample may be explained by the inclusion of younger ambulatory survivors or older terminal bedridden patients who are known to fall less. Furthermore, Medicaid recipients who have cancer yet are not diagnosed may have caused an underestimation of the fall rate in cancer survivors. This confirms the need for future research to examine in more detail how cancer date of diagnosis, type, stage, or specific treatment may be associated with falls in elderly cancer survivors.
Age was not predictive of falls in the present sample. This finding is consistent with the literature in geriatric medicine and nursing. Chronological age is not a known limiting factor for disability and disablement 47. IADL was not predictive of falls in the present sample, although the literature consistently supports IADLs as a significant predictor of fall risk and falls 37. In this sample, 98% of the study participants had a need for assistance with IADLs, which led to saturation of the model, as no comparison was available for those who did not need IADL assistance. Therefore, further study is needed with a sample that varies around the dimension of IADLs. Vision was also not predictive of falls in the present sample, although the literature supports poor vision as a predictor of fall risk 48. However, vision problems are often related to other problems such as poor gait and balance, when an elderly individual gets up at night to use the bathroom, and a fall occurs, and further study is needed to clarify the cause of the fall.
Limitations
As stated previously, a limitation of this study included the ability to determine whether a specific cancer diagnosis, such as lung, breast, prostate, or colon cancer placed individuals at a higher risk for falls. In addition, the effect of cancer stage, recurrence, or if treatment phase placed individuals at fall risk could not be determined. A final limitation of this study was the ability to determine comorbidities that may have placed individuals at a higher risk for falls. These limitations should be considered in future nursing research.
An examination of the burden of falls in the elderly with cancer could lead to research on delineation of barriers to promoting fall-prevention strategies that could be implemented to improve the delivery and financing of care for this population. Competing clinical demands exist, and the multi-factoral nature of falls requires coordination, and a multifaceted approach that does not adhere to the traditional disease model that drives most medical care 49. Nursing is in a position to focus on this problem.
Conclusion
Falls in the community dwelling elderly with cancer, has significant potential for physical and psychological consequences. Nurses, particularly those delivering HCBS services, must be attuned to the prevalence and risk of falls occurring. Many of the health problems that increase the chance of falling are known and are treatable. Nursing can play a vital role in conducting fall screening and risk assessment to identify those at risk for falls, directing educational efforts to patients in need of fall precaution teaching.
Findings from this study will be used to shape future studies. Ultimately, findings from the study of this topic will be used to provide useful approaches for nursing practice to assess those who are at risk. Additionally, findings will be used to allocate valuable nursing time towards those patients who “need” more intense management of preventive measures. Finally, findings will be used to design effective models of care that will assist elderly cancer survivors to live in the community.
Footnotes
Acknowledgements, credits or disclaimers: NONE
Sources of funding: NONE
Disclosures: NONE
Contributor Information
Sandra Spoelstra, Michigan State University College of Nursing.
Barbara Given, Michigan State University College of Nursing.
Alexander von Eye, Michigan State University Department of Psychology.
Charles Given, Michigan State University College of Human Medicine.
References
- 1.Center for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) National Center for Injury Prevention and Control, Center for Disease Control and Prevention; [Google Scholar]
- 2.Davison J, Marrinan S. Falls. Reviews in Clinical Gerontology. 2007;17(2):93–107. [Google Scholar]
- 3.Lim LS, Chutka DS. Preventive medicine beyond 65. Geriatrics & Gerontology International. 2006;6(2):73–81. [Google Scholar]
- 4.van Helden S, van Geel ACM, Geusens PP, Kessels A, Kruseman ACN, Brink PRG. Bone and fall-related fracture risks in women and men with a recent clinical fracture. Journal of Bone & Joint Surgery. 2008;90A(2):241–248. doi: 10.2106/JBJS.G.00150. [DOI] [PubMed] [Google Scholar]
- 5.Tinetti ME, Allore H, Araujo KLB, Seeman T. Modifiable impairments predict progressive disability among older persons. Journal of Aging & Health. 2005;17(2):239–256. doi: 10.1177/0898264305275176. [DOI] [PubMed] [Google Scholar]
- 6.Chen JS, Simpson JM, March LM, et al. Risk factors for fracture following a fall among older people in residential care facilities in Australia. Journal of the American Geriatric Society. 2008;56(11):1–7. doi: 10.1111/j.1532-5415.2008.01954.x. [DOI] [PubMed] [Google Scholar]
- 7.Hodgson NA. Epidemiological trends of cancer in older adults: Implications for gerontological nursing practice and research. Journal of Gerontological Nursing. 2002;101(4):34–23. [Google Scholar]
- 8.Pautex S, Herrmann FR, Zulian GB. Factors associated with falls in patients with cancer hospitalized for palliative care. Journal of Palliative Medicine. 2008;11(6):878–884. doi: 10.1089/jpm.2007.0241. [DOI] [PubMed] [Google Scholar]
- 9.Overcash J. Journal club. Prediction of falls in older adults with cancer: a preliminary study. Oncology Nursing Forum. 2007;34(2):341–346. doi: 10.1188/07.ONF.341-346. [DOI] [PubMed] [Google Scholar]
- 10.Pearse H, Nicholson L, Bennett M. Falls in hospices: a cancer network observational study of fall rates and risk factors. Palliative Medicine. 2004;18(5):478–481. doi: 10.1191/0269216304pm903oa. [DOI] [PubMed] [Google Scholar]
- 11.Sweeney C, Schmitz KH, Lazovich D, Virnig BA, Wallace RB, Folsom AR. Functional Limitations in Elderly Female Cancer Survivors. Journal of the National Cancer Institute. 2006;98(8):521–529. doi: 10.1093/jnci/djj130. April 19, 2006. [DOI] [PubMed] [Google Scholar]
- 12.Yabroff KR, McNeel TS, Waldron WR, et al. Health limitations and quality of life associated with cancer and other chronic diseases by phase of care. Medical Care. 2007;45(7):629–637. doi: 10.1097/MLR.0b013e318045576a. [DOI] [PubMed] [Google Scholar]
- 13.Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: Age, health, and disability. Journals of Gerontology Series A: Biological Sciences & Medical Sciences. 2003;58A(1):82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- 14.Keating NL, Narredam M, Landrum MB, Huskamp HA, Meara E. Physical and mental health status of older long-term cancer survivors. Journal of the American Geriatrics Society. 2005;53(12):2145–2152. doi: 10.1111/j.1532-5415.2005.00507.x. [DOI] [PubMed] [Google Scholar]
- 15.Koroukian S, Murray P, Madigan E. Comorbidity, disability, and geriatric syndromes in elderly cancer patients receiving home health care. Journal of Clinical Oncology. 2006;24(15):2304–2310. doi: 10.1200/JCO.2005.03.1567. [DOI] [PubMed] [Google Scholar]
- 16.Freedman VA, Martin LG, Schoeni RF, Cornman JC. Declines in late-life disability: the role of early- and mid-life factors. Social Science & Medicine. 2008;66(7):1588–1602. doi: 10.1016/j.socscimed.2007.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferrans C, Zerwic J, Wilbur J, Larson J. Conceptual model of health-related quality of life. Journal of Nursing Scholarship. 2005;37(4):223–337. doi: 10.1111/j.1547-5069.2005.00058.x. [DOI] [PubMed] [Google Scholar]
- 18.Fauth E, Zarit SH, Malmberg B, Johansson B. Physical, cognitive, and psychosocial variables from the disablement process model predict patterns of independence and the transition into disability for the oldest old. The Gerontologist. 2007;47(5):613–624. doi: 10.1093/geront/47.5.613. [DOI] [PubMed] [Google Scholar]
- 19.Tinetti ME, Baker DI, McAvay G. A multifactoral intervention to reduce the risk of falling among elderly people living in the community. New England Journal of Medicine. 1994;331:821–827. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- 20.Tinetti ME, Speeckley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 21.US Department of Health and Human Services. United States Cancer Statistics: 1999–2002 incidence and mortality web-based report. Centers for Disease Control and Prevention and National Cancer Institute; 2005. Available at www.cdc.gov/cancer/npcr/uscs/. [Google Scholar]
- 22.Guilley E, Ghisletta P, Armi F, et al. Dynamics of frailty and ADL dependence in a five-year longitudinal study of octogenarians. Research on Aging. 2008;30(3):299–317. [Google Scholar]
- 23.Rowland JH, Yancik R. Cancer survivorship: the interface of aging, comorbidity, and quality care. Journal of the National Cancer Institute. 2006;98(8):504–505. doi: 10.1093/jnci/djj154. [DOI] [PubMed] [Google Scholar]
- 24.Luctkar-Flude MF, Groll DL, Tranmer JE, Woodend K. Fatigue and physical activity in older adults with cancer: a systematic review of the literature. Cancer Nursing. 2007;30(5):E35–E45. doi: 10.1097/01.NCC.0000290815.99323.75. [DOI] [PubMed] [Google Scholar]
- 25.Deimling GT, Bowman KF, Wagner LJ. The effects of cancer-related pain and fatigue on functioning of older adult, long-term cancer survivors. Cancer Nursing. 2007;30(6):421–433. doi: 10.1097/01.NCC.0000300168.88089.2b. [DOI] [PubMed] [Google Scholar]
- 26.Gulluoglu BM, Cingi A, Cakir T, Gercek A, Barlas A, Eti Z. Factors related to post-treatment chronic pain in breast cancer survivors: the interference of pain with life functions. International Journal of Fertility & Womens Medicine. 2006;51(2):75–82. [PubMed] [Google Scholar]
- 27.Holen JC, Lydersen S, Klepstad P, Loge JH, Kaasa S. The Brief Pain Inventory: pain's interference with functions is different in cancer pain compared with noncancer chronic pain. Clinical Journal of Pain. 2008;24(3):219–225. doi: 10.1097/AJP.0b013e31815ec22a. [DOI] [PubMed] [Google Scholar]
- 28.Deimling GT, Sterns S, Bowman KF, Kahana B. Functioning and activity participation restrictions among older adult, long-term cancer survivors. Cancer Investigation. 2007;25(2):106–116. doi: 10.1080/07357900701224813. [DOI] [PubMed] [Google Scholar]
- 29.Waltman N, Ott C, Twiss J, Gross G, Lindsey A, Berg K. Predicting likelihood of multiple falls in postmenopausal breast cancer survivors (BCSs) with low bone mineral density. Oncology Nursing Forum. 2007;34(1):181–181. [Google Scholar]
- 30.Pearce T, Ryan S. Cancer and falls risk assessment. Australian Nursing Journal. 2008;15(8):37–37. [Google Scholar]
- 31.Flood KL, Carroll MB, Le CV, Ball L, Esker DA, Carr DB. Geriatric syndromes in elderly patients admitted to an oncology-acute care for elders unit. Journal of Clinical Oncology. 2006;24(15):2298–2303. doi: 10.1200/JCO.2005.02.8514. [DOI] [PubMed] [Google Scholar]
- 32.Johnson RW, Wiener JM. A profile of frail older Americans and their caregivers. Robert Wood Johnson Foundation; 2006. [Google Scholar]
- 33.Center for Disease Control. Fall Injury episodes among noninstitutionalized older adults: United States, 2001–2003, no. 292. Atlanta: Vital and Health Statistics; 2007. Sep 21, [Google Scholar]
- 34.National Cancer Institute. National Cancer Institute SEER Cancer Statistics Review, 1975–2004. 2007. [Google Scholar]
- 35.Gates S, Fisher JD, Cooke MW, et al. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: Systematic review and meta-analysis. BMJ. 2008;336:130–133. doi: 10.1136/bmj.39412.525243.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Visovsky C. The Effects of Neuromuscular Alterations in Elders with Cancer. Seminars in Oncology Nursing. 2006;22(1):36–42. doi: 10.1016/j.soncn.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 37.Bennett JA, Winters KM, Nail L. Falls and characteristics of fallers among older breast cancer survivors. Disability & Rehabilitation. 2007;29(20–21):1651–1651. [Google Scholar]
- 38.Holley S. A look at the problem of falls among people with cancer. Clinical Journal of Oncology Nursing. 2002;6(4):193. doi: 10.1188/02.CJON.193-197. [DOI] [PubMed] [Google Scholar]
- 39.O'Connell BO, Baker L, Gaskin CJ, Hawkins MT. Risk items associated with patient falls in oncology and medical settings. Journal of Nursing Care Quality. 2007;22(2):130–137. doi: 10.1097/01.NCQ.0000263102.06311.a9. [DOI] [PubMed] [Google Scholar]
- 40.Limburg CE. Screening, prevention, detection, and treatment of cancer therapy-induced bone loss in patients with breast cancer. Oncology Nursing Forum. 2007;34(1):55–61. doi: 10.1188/07.ONF.55-36. [DOI] [PubMed] [Google Scholar]
- 41.Overcash J. Vitamin D in older patients with cancer. Clinical Journal of Oncology Nursing. 2008;12(4):655–659. doi: 10.1188/08.CJON.655-662. [DOI] [PubMed] [Google Scholar]
- 42.CMS. Medicaid State Waiver Program Demonstration Projects - General Information. Health and Human Services; [ http://www.cms.hhs.gov/MedicaidStWaivProgDemoPGI/. [Google Scholar]
- 43.Morris JN, Fries B, Steel K, et al. Comprehensive clinical assessment in community setting: Applicability of the MDS-HC. Journal of the American Geriatrics Society. 1997;45(8):1–13. doi: 10.1111/j.1532-5415.1997.tb02975.x. [DOI] [PubMed] [Google Scholar]
- 44.Hulley SB, Cummings SR, Brower WS, Grady DG, Newman TB. Designing Clinical Research. 3rd ed. Philadelphia, Pennsylvania: Wolters Kluwer Health, Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 45.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies in community dwelling older people: Effect of recall interval. Journal of American Geriatric Society. 2005;53:2190–2194. doi: 10.1111/j.1532-5415.2005.00509.x. [DOI] [PubMed] [Google Scholar]
- 46.Institute of Medicine. Unequal Treatment. Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: 2003. [Google Scholar]
- 47.Arking R. The biology of aging: Observations and principles. 3rd ed. New York: Oxford University Press; 2006. [Google Scholar]
- 48.Szabo SM, Jannsen PA, Khan K, Potter MJ, Lord SR. Older women with age-related macular degeneration have a greater risk of falls: A physiological profile assessment study. Journal of the American Geriatrics Society. 2008;56(5):800–807. doi: 10.1111/j.1532-5415.2008.01666.x. [DOI] [PubMed] [Google Scholar]
- 49.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. Journal of the American Geriatrics Society. 2007;55(5):780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


