Abstract
Objective
To determine the incidence of falls and to investigate the consequences of falls in adults with rheumatoid arthritis (RA).
Methods
A total of 559 community-dwelling adults with RA, ages 18–88 years (mean age 62 years, 69% women), participated in this prospective cohort study. After a detailed clinical assessment, patients were followed for 1 year, using monthly falls calendars and followup telephone calls. Followup took place in the participant's usual place of residence in the Northwest of England. Outcome measures included fall occurrence, reason for fall, type and severity of injuries, fractures, fall location, lie-times, use of health services, and functional ability.
Results
A total of 535 participants followed for 1 year had a total of 598 falls. Of these participants, 36.4% (95% confidence interval 32%–41%) reported falling during the 1-year followup period, with an incidence rate of 1,313 per 1,000 person-years at risk or 1.11 falls per person. Age and sex were not associated with falls. More than one-third of the falls were reportedly caused by hips, knees, or ankle joints “giving way.” More than half of all the falls resulted in moderate injuries, including head injuries (n = 27) and fractures (n = 26). Treatment by general practitioners or other health professionals was required for 15.0% of falls, and emergency services were required for 8.8% of falls.
Conclusion
These results indicate that adults with RA are at high risk of falls and fall-related injuries, fractures, and head injuries. Strategies to prevent falls in adults with RA must be prioritized to reduce falls, fall-related injuries, and fractures.
Introduction
Falls in adults and older people are a global public health challenge and are associated with substantial health, social, and economic costs. Falls are not just restricted to older persons, but can have severe consequences for other at-risk groups, such as people with arthritis. Rheumatoid arthritis (RA) affects approximately 0.8% of the UK population and 1% worldwide (1). Previous small-scale research suggests that people with RA may be at greater risk of falls and osteoporotic fractures due to altered gait, poor mobility and balance, muscle weakness, bone fragility, pain, and fatigue (2–6). To date, clinic-based studies have examined the 1-year prevalence of falls in adults with RA by asking patients if they had fallen over the previous 12 months (4, 7, 8). These studies report similar results, with 31–35% of people with RA reporting falls. A small prospective study of 84 women with RA reported an incidence of falls of 50% in a 12-month period (2). However, these results cannot be generalized due to the age range (ages 50–82 years) and exclusion of men. Another small prospective study of 25 men and 59 women reported an incidence of 42% (9), but did not use a definition of a fall, which may lead to different interpretations of falls by participants and researchers (10). To date, there are no prospective data reporting fall incidence in younger subjects.
Many epidemiologic studies and fall prevention trials have been conducted in older community-dwelling adults (11). In comparison, there is scant epidemiologic research relating to the occurrence and consequences of falls in adults with RA. The aim of this study was to determine the 1-year incidence of falls in adult men and women with RA and to characterize the mechanisms and outcomes related to falls that occurred.
Significance & Innovations
Adults with rheumatoid arthritis (RA) are at high risk of falls and fall-related injuries, fractures, and head injuries.
Strategies to prevent falls in adults with RA must be prioritized to reduce fall-related injuries and fractures.
Patients who have a history of falls are more likely to fall again.
Patients and Methods
Patient recruitment
Participants were recruited from 4 rheumatology outpatient clinics in 3 National Health Service Hospital Trusts and 1 Primary Care Trust in Northwest England. Patients were included if they had RA based on the 2010 American College of Rheumatology/European League Against Rheumatism classification criteria for RA (12) and were age >18 years. Participants were excluded from the study if they were without the mental or physical capacity to give informed consent.
Three patients with RA were involved in the planning of the study and assisted with data collection decisions, such as the language used in the questionnaire and information sheets. Patients gave written informed consent before taking part. Ethical approval was gained from the National Research Ethics Committee and the University of Manchester Committee on Ethics of Research on Human Beings.
Baseline assessments
Measurements taken at the baseline clinical assessment included demographic data (age, sex, ethnicity, socioeconomic status); the RA Disease Activity Score in 28 joints (DAS28), including number of swollen and tender joints; the Stanford Arthritis Center Health Assessment Questionnaire (HAQ); a 12-month history of falling; fear of falling questionnaire (Short Falls Efficacy Scale-International) (13); and falls risk using the Assessment of Falls Risk Tool (14). Fall history was recorded at the baseline assessment by asking, “During the past year, how often have you had any fall, including a slip or trip in which you lost your balance and landed on the floor, ground, or lower level?” The response set to this question consisted of never, once, or twice or more. Data on medication, pain, fatigue, vision, comorbidities, and history of surgery, fractures, and joint replacements were also recorded. The results and further details on these measurements are reported elsewhere.
Followup
Falls and injuries were recorded during the followup period using the Prevention of Falls Network Europe fall definition of “an unexpected event in which participants come to rest on the ground, floor, or other lower level” (15). Falls and injuries were monitored using monthly, prepaid preaddressed calendar postcards that were completed daily by participants. An example of the information and style of the calendar postcards is shown in Figure 1. Those reporting a fall were followed up by telephone to gather information about the fall and any injuries, using methods by Campbell et al to subclassify falls according to severity by using both injury outcomes (e.g., fractures, bruising, cuts, and sprains) and health care utilization (e.g., hospital admission, medical assistance, and physiotherapy) (16), as recommended by Schwenk et al (17). This information included date of fall, participant description of how the fall occurred, consequences and injuries (injuries coded by researcher as 0 = no injury, 1 = moderate injury, and 2 = severe injury), and length of time (minutes) before being able to get up or when help arrived (lie-time). The participant's functional status after the fall was assessed with the use of 3 questions as follows: 1) as a result of this fall, did you have any difficulty walking around your home? 2) as a result of this fall, did you have any difficulty walking around outside or away from your home? and 3) as a result of this fall, did you have any difficulty doing things around your home like cooking or cleaning? The response set consisted of could not do before the fall, could not do because of the fall, able to do but had more difficulty than before the fall, and could do after the fall without difficulty. Participants who failed to complete the calendars were followed up by telephone.
Figure 1.
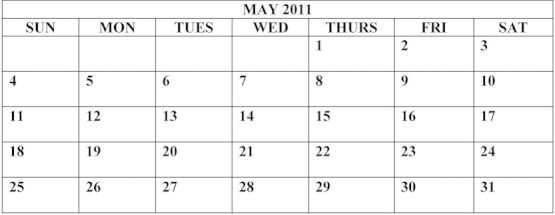
Example of a calendar postcard. Participants were instructed to 1) at the end of the day, please place the letter “N” in the box if you did not fall, or the letter “F” in the box if you did fall, and 2) at the end of each month, please detach the calendar for that month and post it. No stamp is necessary.
Sample
Based on an estimated frequency of falls over a 12-month period of 30%, it was estimated that a sample of 550 people with RA (495 people after an assumed 10% dropout rate) was needed to achieve an exact 95% confidence interval (95% CI) (18) for the fall frequency of (95% CI 26%–35%), as given by StatsDirect, version 2.6.5 (19).
Data analysis
Fall data were summarized as recommended by Prevention of Falls Network Europe (15), using number of falls, number of nonfallers/single fallers/multiple fallers, and the fall rate per person-year. CIs were reported for the incidence rate of falls and for the sex- and age-specific fall rates. To explore the differences between those who did not fall in the 1-year followup period but did fall in the previous year, the absolute risk differences between the groups were calculated. Injuries were classified according to the International Classification of Diseases, Tenth Revision, classification system (20). Injury data were summarized as type of injury, fracture rate per person-year, number of fractures, number of persons sustaining fractures, and number of persons sustaining multiple injury events (15). Statistical analysis was performed using SPSS, version 16 (21).
Results
A total of 845 letters were sent to participants prior to their clinic appointment. Of the 656 patients who attended the clinics and were assessed for eligibility, 31 were excluded and 66 refused to take part. There was a high recruitment rate (85%) for participants, and 535 of 559 (96%) participants took part in the 1-year followup. Sixty percent of participants completed all of the 12 calendar returns within the 1-year followup period. Twenty-four participants did not complete the followup; reasons included death (n = 7), felt too unwell (n = 14), or wished to discontinue as sending the postcards was too onerous (n = 3) (Figure 2).
Figure 2.
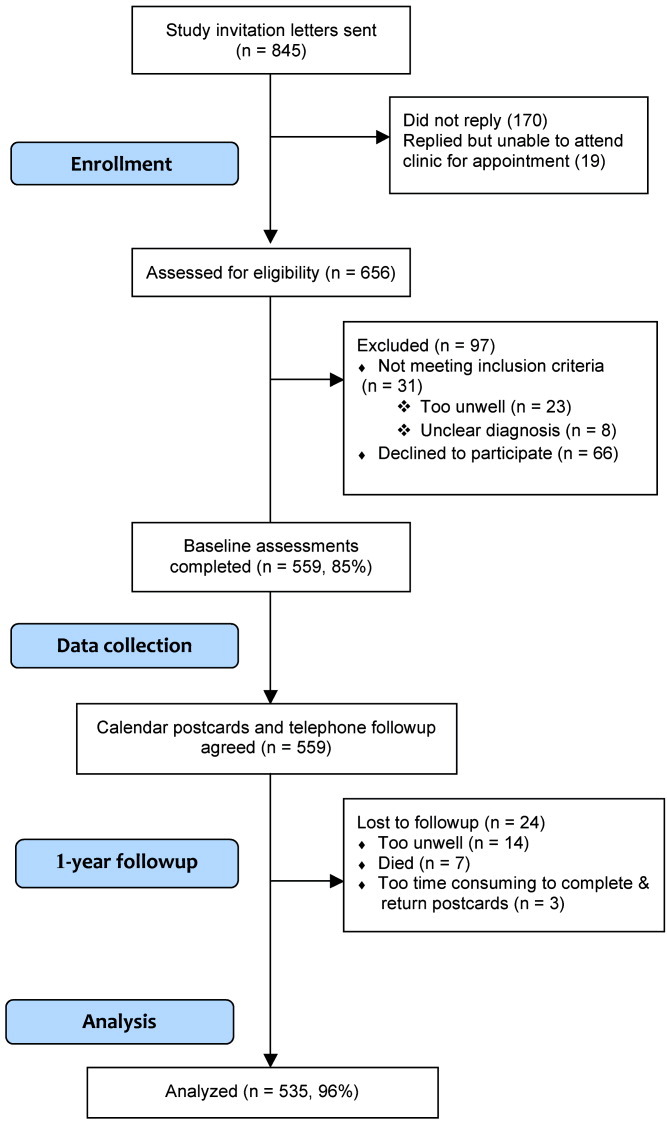
Flow diagram of the research process.
Table 1 presents the demographic and descriptive characteristics of the sample. More women (n = 386, 69%) were recruited to the study than men. The mean ± SD age of men was 62.4 ± 11.0 years, and the mean ± SD age of women was 61.9 ± 13.5 years. The majority of participants were married or living with a partner (n = 378, 69.7%) and were of British white ethnicity and born in the UK (n = 544, 97.3%). More than half of the participants were retired (n = 327, 58.5%), and 15% (n = 82) were unable to work due to their disabilities. Twenty-four percent (n = 134) of the participants continued to be employed.
Table 1.
Demographics and characteristics of baseline and followup nonfaller and faller participants*
| Characteristics | Total (n = 559) | Nonfallers (n = 340) | Fallers (n = 195) |
|---|---|---|---|
| Male | 173 (30.9) | 105 (30.9) | 57 (29.3) |
| Female | 386 (69.1) | 235 (69.1) | 138 (70.8) |
| Mean ± SD DAS28 score (0–10) | 4.1 ± 1.6 | 3.9 ± 1.62 | 4.3 ± 1.2 |
| Mean ± SD HAQ score (1–4) | 2.4 ± 0.9 | 2.3 ± 0.8 | 2.6 ± 0.8 |
| Ethnic origin | |||
| African/Caribbean | 3 (0.5) | 1 (0.3) | 2 (1.0) |
| British white/Irish white/other white background | 544 (97.3) | 330 (97.1) | 191 (97.9) |
| Asian/British Indian/British Pakistani | 8 (1.4) | 5 (1.5) | 2 (1.0) |
| Mixed ethnicity | 2 (0.4) | 2 (0.6) | 0 (0) |
| Other ethnicity | 2 (0.4) | 2 (0.6) | 0 (0) |
| Employment status | |||
| Employed | 134 (24.0) | 89 (26.2) | 38 (19.5) |
| Retired | 327 (58.5) | 197 (57.9) | 118 (60.5) |
| Full-time student/volunteer work/unemployed | 3 (0.5) | 1 (0.3) | 2 (1.0) |
| At home/housework/caring for family | 13 (2.3) | 9 (2.6) | 4 (2.1) |
| Unemployed due to sickness/disability | 82 (14.7) | 44 (12.9) | 33 (16.9) |
| Marital status | |||
| Single, never married | 49 (9.0) | 36 (10.6) | 11 (5.7) |
| Married/living with partner | 378 (69.7) | 229 (67.4) | 138 (71.9) |
| Divorced/separated | 43 (7.9) | 22 (6.5) | 25 (13.0) |
| Widowed | 72 (13.3)† | 40 (6.5) | 18 (9.2) |
| Socioeconomic classification | |||
| Higher managerial/professional occupations | 13 (2.3) | 8 (2.5) | 3 (1.6) |
| Lower managerial/professional occupations | 87 (15.6) | 53 (16.4) | 30 (16.4) |
| Intermediate | 85 (15.2) | 58 (18.0) | 24 (13.1) |
| Small employers/own-account workers | 120 (21.5) | 69 (21.4) | 47 (25.7) |
| Lower supervisory and technical | 166 (29.7) | 94 (29.1) | 66 (36.1) |
| Semiroutine/routine | 57 (10.8) | 41 (12.7) | 12 (6.6) |
| Never worked/long-term unemployed | 1 (0.2)‡ | 0 (0) | 1 (0.5) |
Values are the number (percentage) unless indicated otherwise. DAS28 = Disease Activity Score in 28 joints; HAQ = Health Assessment Questionnaire.
N = 17 for not recorded.
N = 30 for not recorded.
At baseline, the mean DAS28 score (4.1, mode 3.9), the mean ± SD visual analog scale (VAS) fatigue score (4.7 ± 2.8), the mean ± SD VAS pain score (3.9 ± 2.7), and the mean ± SD HAQ score (2.4 ± 0.9) of the participants were all within the moderate range. The mean ± SD numbers of swollen and tender joints (0–28) were 4.7 ± 6.3 and 5.3 ± 6.9, respectively. Cardiovascular drugs were taken by 46.5% of participants (n = 260), while 18.8% of participants (n = 105) were classified as taking psychotropic type medicines and 77.1% of participants (n = 431) were recorded as taking ≥4 types of medicines per day. Thirty-eight participants reported a history of stroke or Parkinson's disease (6.8%), and a small proportion reported their eyesight as either registered blind, very poor, or poor (n = 46, 8.2%), with the majority of participants reporting their vision as fair (n = 145, 25.9%), good (n = 313, 56.0%), or excellent (n = 55, 9.8%). Nearly one-quarter of participants (n = 117, 20.9%) were reportedly taking steroids at the baseline assessment, and almost half of the participants (n = 228, 40.6%) reported a history of fracture(s). Further baseline descriptive results and factors associated with falls and predictive and explanatory risk models (using binary multivariate logistic regression analyses) are reported elsewhere.
Incidence of falls
From the initial sample of 559 participants, 535 (95.7%) completed 1 year of followup. A total of 598 falls were reported in 5,467 months of observation, with a crude incidence rate of 1,313 falls per 1,000 person-years at risk or 1.11 falls per person. More than one-third of the participants experienced ≥1 fall(s) (36.4%, 95% CI 32%–41%). Ninety-four people fell once, and 101 people fell twice or more (Figure 3).
Figure 3.
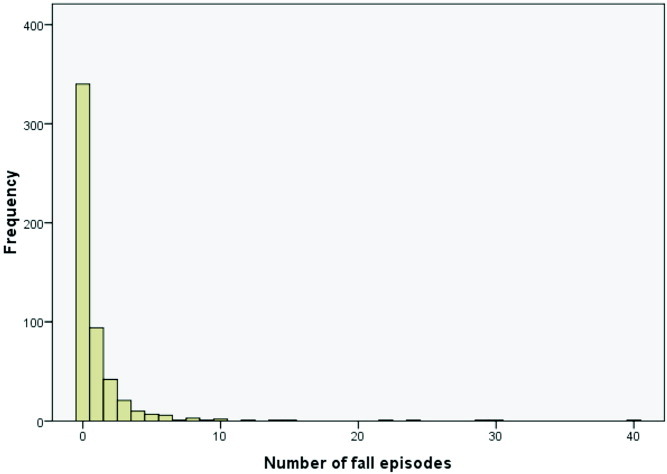
Histogram of number of falls in 1-year followup.
Age- and sex-specific incidence rates in 12 months
Table 2 presents the age-specific incidence rates in 12 months for the participants. A small number of younger participants (n = 7) fell frequently, which gave the 18–34 years age group a high incidence rate of falls. However, due to the small number in this group, CIs are wide. There was also an increase in the incidence rate of falls in the 65–74 years age group, but this drops again in the ≥75 years age group.
Table 2.
Age- and sex-specific fall incidence rates in 1 year*
| Patients | Fallers | Fall events | Person-years at risk | Incidence rate of falls per 1,000 person-years | 95% CI | |
|---|---|---|---|---|---|---|
| Age, years | ||||||
| 18–34 | 19 | 7 | 34 | 13.7 | 2,481.6 | 1,718.7–3,468.0 |
| 35–44 | 35 | 10 | 34 | 28.3 | 1,201.4 | 832.0–1,678.9 |
| 45–54 | 87 | 31 | 67 | 69 | 971.0 | 752.5–1,233.2 |
| 55–64 | 165 | 62 | 251 | 150 | 1,673.3 | 1,472.7–1,893.7 |
| 65–74 | 155 | 56 | 149 | 49.8 | 2,991.9 | 2,530.9–3,512.8 |
| ≥75 | 74 | 29 | 63 | 61.5 | 1,024.4 | 787.2–1,310.6 |
| All ages | 535 | 195 | 598 | 455.9 | 1,312.6 | 1,208.7–1,420.0 |
| Sex | ||||||
| Male | 162† | 57 | 240 | 136.6 | 1,756.9 | 1,541.7–1,993.9 |
| Female | 373‡ | 138 | 358 | 318.9 | 1,122.6 | 1,009.3–1,245.1 |
Values are the number unless indicated otherwise. 95% CI = 95% confidence interval.
Thirty-five percent fallers per year.
Thirty-seven percent fallers per year.
There were no significant differences in the percentage of men (35%) and women (37%) who fell at least once during the 1-year followup period, but the sex-specific incidence rates (Table 2) show that male fallers fell proportionally more than the female fallers and had a statistically significant higher incidence rate of falls per 1,000 person-years (P < 0.0001).
The absolute risk of falling during the study for participants without a 1-year history of falls was 23%, while for participants who did have a 1-year history of falls the absolute risk of falling during the study was 53%. Participants with a 12-month history of a fall were more likely to fall again in the following year (χ2 [1df] = 51.1, P < 0.0001).
Self-reported fall event descriptions and locations
The self-reported fall descriptions were recorded and later categorized into types of falls and reasons for falls. Seventeen participants could not remember the full details of their fall(s).
The commonly reported types of falls were hips, knees, or ankles “giving way” (n = 187, 31.0%), with the knee joints most frequently affected or slips/trips forward on a level (n = 101, 17.7%) or uneven surface (n = 96, 16.8%). Falls due to loss of balance were also a problem for 9.8% of participants (n = 56), as were slips or trips going upstairs (n = 25, 4.4%) or downstairs (n = 21, 3.7%). Smaller proportions of falls were described as falling sideways, slips/trips backwards on level or rough surfaces, and falls getting out of bed or the bath.
Table 3 summarizes the self-reported underlying reasons for the fall(s) described by participants. Sixty-three percent (n = 356) of the participants affected by falls blamed their RA for the underlying cause of the fall (described as joint pain, muscle weakness, joints giving way, or a flare of the condition). Tripping over hazards was the next most commonly described fall (n = 105, 18.7%), and the majority of the tripping over hazard falls resulted in moderate or serious injuries (n = 61, 58.1%). Sixty-five percent (n = 363) of the falls took place inside the participants' houses on a level surface, such as in the kitchen or going up or down stairs, while 31.5% (n = 177) of participants fell outside their home or outside going up or down steps.
Table 3.
Self-reported reasons for fall in 1-year followup*
| Reason | Falls, no. (%) | 95% CI |
|---|---|---|
| RA | 356 (63.3) | 55.5–63.4 |
| Tripped over hazard | 105 (18.7) | 14.7–20.8 |
| Dizziness | 21 (3.7) | 2.3–5.3 |
| Slipped on ice | 17 (3.0) | 1.9–4.7 |
| Feeling generally unwell | 14 (2.5) | 1.4–3.8 |
| Recent surgery | 9 (1.6) | 0.8–2.9 |
| Momentary lapse of concentration | 8 (1.4) | 0.7–2.6 |
| Epilepsy | 7 (1.2) | 0.6–2.4 |
| Rushing | 7 (1.2) | 0.6–2.4 |
| Difficulty with visibility at night | 6 (1.1) | 0.5–2.2 |
| Fatigue | 5 (0.9) | 0.3–2.0 |
| TIA/stroke | 5 (0.9) | 0.3–2.0 |
| Fainted | 1 (0.2) | 0.0–0.95 |
| Hypotension | 1 (0.2) | 0.0–0.95 |
| Total | 562 (100.0) | |
| Missing | 36 | |
| Total including missing | 598 |
95% CI = 95% confidence interval; RA = rheumatoid arthritis; TIA = transient ischemic attack.
In order to enable the estimated lie-time to be calculated, the participants were asked to recall the amount of time they spent on the floor or lower level following the fall. Most lie-times were short, with 89.3% (n = 448) of participants able to stand up again in <10 minutes following a fall. The median lie-time was 2 minutes (mean 7 minutes, range 0–480 minutes). Six participants had lie-times >60 minutes, where they required further assistance from medical personnel due to the severity of the fall.
Injuries and consequences of falls
More than half of the falls (n = 291, 51.5%) resulted in bruising, stiffness, and exacerbated joint pains, sprains, and bangs to the head (not hospitalized) and were recorded as moderate injuries. Severe injuries included fractures and injuries requiring further assessment and treatment in the hospital (n = 43, 7.6%). Lower body injuries were most common (n = 139, 24.6%) and included hip, thigh, knee, lower leg, ankle, and foot injuries (Table 4). Shoulder, upper arm, elbow, and forearms (n = 66, 11.6%) were also frequently reported, but wrist and hand injuries were less common (n = 8, 1.4%). The number of head injuries (minor bumps to more severe concussions) was high (n = 27, 5.1%) compared to Fessel and Nevitt, who reported 16 (2.8%) fall-related head injuries in their cross-sectional fear of falling and RA study (8). Injuries involving multiple body regions (n = 81, 14.3%) were also high. There were 26 fractures in total as a result of falls (n = 20, 4%), which resulted in a fracture rate of 57.1 fractures per 1,000 person-years at risk. Lower extremity fractures were most common (knee, ankle, and toe fractures, n = 7), while 6 participants reported lower arm/wrist and hand fractures. Four participants reported fractured pelvis/hip, 2 participants reported rib fractures, and 2 participants reported vertebrae fractures. Of these, 14 were single fractures, 3 falls resulted in 2 fractures, and 2 falls resulted in 3 fractures (bilateral hip fractures and a fractured pelvis for one participant, and 3 fractured toes in another participant).
Table 4.
Type of fall-related injury in 1-year followup according to the International Classification of Diseases, Tenth Revision*
| Type of injury | Participants, no. (%) | 95% CI |
|---|---|---|
| No injury | 232 (41.0) | 34.9–42.7 |
| Head | 15 (2.7) | 1.5–4.1 |
| Thorax | 6 (1.1) | 0.5–2.1 |
| Abdomen, lower back, lumbar spine, and pelvis | 18 (3.2) | 1.9–4.7 |
| Shoulder and upper arm | 37 (6.5) | 4.5–8.4 |
| Elbow and forearm | 29 (5.1) | 3.4–6.9 |
| Wrist and hand | 8 (1.4) | 0.7–2.6 |
| Hip and thigh | 32 (5.5) | 3.8–7.5 |
| Knee and lower leg | 28 (4.9) | 3.3–6.7 |
| Ankle and foot | 79 (14.0) | 10.7–16.2 |
| Injuries involving multiple body regions (including head) | 81 (14.3) | 11.0–16.5 |
| Total | 565 (100.0) | |
| Missing | 33 | |
| Total including missing | 598 |
95% CI = 95% confidence interval.
More than half of the falls that participants related to their RA resulted in moderate injuries (n = 182, 51.1%), and 7.0% (n = 25) resulted in serious injuries (e.g., fractures or hospitalization). Significantly more outdoor falls resulted in moderate or severe injury (n = 124, 70.1%) in comparison to indoor falls (n = 210, 54.6%; P < 0.01).
As a consequence of a fall, 31.9% of participants (n = 183) experienced more difficulty in being able to walk around their home, while 8.2% of the falls resulted in the participants being unable to walk independently around their home (n = 47). Nearly 40% of the falls resulted in participants having difficulty or being unable to walk outside or away from their home (n = 217). Thirteen percent of participants could not walk outside before the fall occurred. Of the falls, 36.5% led to participants being unable or having difficulties in being able to continue with activities around the home, such as cooking and cleaning (n = 209).
Use of health services
Fifteen percent of falls (n = 86) resulted in visits to the general practictioner or required physiotherapy or nursing assistance for treatment or rehabilitation. Furthermore, emergency services such as an ambulance or visit to the accident and emergency department were necessary for treatment of 8.8% (n = 50) of the falls, and 2.4% (n = 14) of the falls resulted in hospital admissions. Hospital stays ranged from 5–140 days (median 6 days).
Discussion
In the largest prospective study of falls in RA patients to date, we have demonstrated that adults of all ages with RA fall frequently. In our study, the crude incidence rate of falls in adults with RA was high at 1,313 per 1,000 person-years at risk or 1.11 falls per person. This is similar to the fall rates in community-dwelling older adults ages ≥70 years and reported as 1.2 falls per person-year (22). During the 12-month followup, 36.4% (95% CI 32%–41%) of participants reported ≥1 fall(s).
Increasing age was not associated with increased falls. Hayashibara et al (2) and Smulders et al (9) also report that age was not associated with falls in their small prospective studies. This is different from studies of falls in community-dwelling older people, where age is considered to be one of the most important risk factors for falls (10, 23, 24). Older people in general have decreased activity leading to muscle weakness, poor balance, and other fall risk factors. These factors occur in all age groups with RA. Both younger and older people with RA appear to have muscle weakness and this may lead to the similar fall rates.
No relationship was found between frequency of falls and sex in adults in this study and by Smulders et al (9), which is also different from studies of community-dwelling people, where women are more likely to fall than men (10, 25). Reasons for fall sex differences in the general population are attributed to biologic differences in muscle mass between men and women and more women living alone, along with higher levels of polypharmacy among women (26). A general decline in muscle mass and similarities in polypharmacy between men and women with RA may result in the similar fall rates between the groups. The incidence of falls was higher in men than women because men who fell were more likely to fall more than once during the study period, possibly reflecting differences in activities and risk-taking behavior.
More than one-third of the falls reported by the participants were caused by their hips, knees, or ankles giving way, and this type of fall is common in the RA population. Although the mechanisms of this type of fall are not fully understood, and there is a lack of literature in this area, these falls may occur due to joint instability caused by weakness in the quadriceps and in the muscles used to stabilize the lower extremity joints alongside joint degeneration and reduced proprioception. Exercises to improve muscle strength and proprioception may assist in preventing these types of falls; however, further research is needed to investigate this.
More than half (51.5%) of all the falls resulted in moderate injuries, which is greater than fall injuries reported by community-dwelling older people (26). Falls mainly occurred in the participants' homes (68.5%), and it is likely that this is where the participants spent most of their time, particularly as more than half were retired from work. However, more moderate and severe injuries were caused by falls occurring outdoors. This may be due to the more vigorous types of activities undertaken outdoors. The severity of the injuries was similar among all the age ranges of participants. Lower-body injuries were the most common. The number of head injuries was high compared to other cross-sectional studies that reported a 12-month history of fall-related head injuries (8), possibly due to hand joint involvement causing difficulties in breaking the impact of falls. Injuries involving multiple body regions were also high.
Consultation and/or treatment by general practitioners or other health professionals were required for 15.0% of the falls, and emergency services were required after 8.8% of the falls (ambulance or visit to accident and emergency department). It is estimated that between 10–15% of all emergency department visits are made as a result of falls (26). The functional ability of participants was decreased after more than one-third of the falls, which could affect levels of independence and requirements from caregivers.
There are few health services available for patients with RA at risk of falls, other than mainstream physiotherapy and occupational therapy. A report by the King's Fund identified an “unacceptably wide variation” in the levels and quality of access to specialists available to the 450,000 people with RA in the UK (27). Yet RA appears as a condition in the widely used World Health Organization's Fracture Risk Assessment Tool (28), and RA has been highlighted as a key risk factor for osteoporotic fractures due to low bone mass (6, 29). Indeed, the higher than expected fracture risk in this study may be due to an interaction between falls and low bone mass. Currently, there does not appear to be specialist service provision to which to refer RA patients at risk of falls and fractures. Although falls prevention services have grown rapidly since their recommendation in the National Service Framework for Older People (30) and the consequent National Institute for Health and Clinical Excellence Guidelines (31), they have remained a service for older people who fall, not for those of all ages with RA (7). Future policy documents related to long-term care and falls prevention should include references to the issues affecting adults with RA in terms of falls risk, fear of falling, and the debilitating characteristics of the disease.
The high incidence of falls in adults with RA confirms that patients need to be screened for potentially modifiable risk factors for falls, and treatments need to be targeted at each of the risk factors. There have been many randomized intervention trials that have aimed to reduce falls in the community-dwelling older population (11), and useful interventions should be considered from these trials to prevent falls in adults with RA. These include referral to appropriate services to deliver tailored exercise programs (targeting strength, balance, endurance, and flexibility), reviewing and adjusting medication (particularly, the gradual withdrawal of medicines used for sleep disorders, anxiety, and depression), and home safety assessments for those at high risk of falls. This study also shows that those who have a history of falls are more likely to fall again, and so taking a simple fall history may highlight those at high risk and in need of intervention.
The strengths of this study are its prospective design, high response rate, and low attrition rate. The 12-month followup allowed for any seasonal variations in the number of falls. The study has a number of limitations. Attempts were made to attend a variety of clinics so that people with varying levels of severity of RA were recruited from the 4 outpatient clinics. However, it is likely that people with more severe RA may be included in the sample due to the recruitment from the clinics. Also, people who have previously fallen may have been more inclined to participate in the study, and this could cause a degree of selection bias.
In conclusion, falls are common and an important cause of injury and fracture in adults of all ages with RA. Head injuries and fractures appear to be particularly high in this group of patients. Due to the lack of patients reporting falls and minor injuries to clinicians, it is important that falls are assessed regularly in medical consultations.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Stanmore had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Stanmore, Oldham, Skelton, O'Neill, Campbell, Todd.
Acquisition of data. Stanmore.
Analysis and interpretation of data. Stanmore, Oldham, Skelton, O'Neill, Pilling, Campbell, Todd.
Acknowledgments
Special thanks to all the participants involved in the research, particularly the 3 patients who assisted with the piloting of the questionnaires, as well as the nursing staff who cooperated with the data collection phase of the study. Thanks also to the research nurses at the Wellcome Trust Clinical Research Facility, particularly Mr. C. Kilkelly and the administration assistance provided by Ms K. Entwistle. We would also like to gratefully acknowledge the expertise and support of Professor I. Bruce, Dr. A. Hassell, Dr. S. Ryan, Mr. P. New, Dr. M. Campbell, and Associate Professor M. Clare Robertson.
References
- 1.Silman AJ, Pearson JE. Epidemiology and genetics of rheumatoid arthritis. Arthritis Res. 2002;4(Suppl):S265–72. doi: 10.1186/ar578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hayashibara M, Hagino H, Katagiri H, Okano T, Okada J, Teshima R. Incidence and risk factors of falling in ambulatory patients with rheumatoid arthritis: a prospective 1-year study. Osteoporos Int. 2010;21:1825–33. doi: 10.1007/s00198-009-1150-4. [DOI] [PubMed] [Google Scholar]
- 3.Oswald AE, Pye SR, O'Neill TW, Bunn D, Gaffney K, Marshall T. Prevalence and associated factors for falls in women with established inflammatory polyarthritis. J Rheumatol. 2006;33:690–4. [PubMed] [Google Scholar]
- 4.Armstrong C, Swarbrick CM, Pye SR, O'Neill TW. Occurrence and risk factors for falls in rheumatoid arthritis. Ann Rheum Dis. 2005;64:1602–4. doi: 10.1136/ard.2004.031195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brand CA, Lowe A, Morton C. Prevalence, outcome and risk for falling in 155 ambulatory patients with rheumatic disease. APLAR J Rheum. 2005;8:99–105. [Google Scholar]
- 6.Huusko TM, Korpela M, Karppi P, Avikainen V, Kautianen H, Sulkava R. Threefold increased risk of hip fractures with rheumatoid arthritis in Central Finland. Ann Rheum Dis. 2001;60:521–2. doi: 10.1136/ard.60.5.521. [abstract] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jamison M, Neuberger GB, Miller PA. Correlates of falls and fear of falling among adults with rheumatoid arthritis. Arthritis Rheum. 2003;49:673–80. doi: 10.1002/art.11383. [DOI] [PubMed] [Google Scholar]
- 8.Fessel KD, Nevitt MC. Correlates of fear of falling and activity limitation among persons with rheumatoid arthritis. Arthritis Care Res. 1997;10:222–8. doi: 10.1002/art.1790100403. [DOI] [PubMed] [Google Scholar]
- 9.Smulders E, Schreven C, Weerdesteyn V, van den Hoogen FH, Laan R, Van Lankveld W. Fall incidence and fall risk factors in people with rheumatoid arthritis. Ann Rheum Dis. 2009;68:1795–6. doi: 10.1136/ard.2009.109009. [abstract] [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. WHO global report on falls prevention in older age. Geneva: World Health Organization; 2007. [Google Scholar]
- 11.Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;2:CD007146. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO., III 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62:2569–81. doi: 10.1002/art.27584. [DOI] [PubMed] [Google Scholar]
- 13.Kempen GI, Yardley L, van Haastregt JC, Zijlstra GA, Beyer N, Hauer K. The Short FES-I: a shortened version of the Falls Efficacy Scale-International to assess fear of falling. Age Ageing. 2008;37:44–50. doi: 10.1093/ageing/afm157. [DOI] [PubMed] [Google Scholar]
- 14.Nandy S, Parsons S, Cryer C, Underwood M, Rashbrook E, Carter Y Falls Prevention Pilot Steering Group. Development and preliminary examination of the predictive validity of the falls risk assessment tool (FRAT) for use in primary care. J Pub Health. 2004;26:138–43. doi: 10.1093/pubmed/fdh132. et al, on behalf of the. [DOI] [PubMed] [Google Scholar]
- 15.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc. 2005;53:1618–22. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 16.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–9. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwenk M, Lauenroth A, Stock C, Moreno RR, Oster P, McHugh G. Definitions and methods of measuring and reporting on injurious falls in randomized controlled fall prevention trials: a systematic review. BMC Med Res Methodol. 2012;12:50. doi: 10.1186/1471-2288-12-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clopper C, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404–13. [Google Scholar]
- 19.StatsDirect Ltd. StatsDirect statistical software. 2008. URL: http://www.statsdirect.com.
- 20.World Health Organization (WHO) 1992. International Classification of Diseases, 10th Revision. Geneva: World Health Organization;
- 21.SPSS Inc. SPSS 16.0 for Windows, release 16.0.2. Chicago: SPSS; 2008. [Google Scholar]
- 22.Blake A, Morgan K, Bendall MJ, Dallosso H, Ebrahim SB, Arie TH. Falls by elderly people at home: prevalence and associated factors. Age Ageing. 1988;17:365–72. doi: 10.1093/ageing/17.6.365. [DOI] [PubMed] [Google Scholar]
- 23.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 24.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–5. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ebrahim S, Kalache A. Epidemiology in old age. London: Blackwell BMJ Books; 1996. [Google Scholar]
- 26.Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57:740–4. doi: 10.1136/jech.57.9.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steward K, Land M. Perceptions of patients and professionals on rheumatoid arthritis care: a consultancy report by The King's Fund for the Rheumatology Futures Group. London: The King's Fund; 2009. [Google Scholar]
- 28.Kanis JA, McCloskey EV, Johansson H, Oden A, Borgstrom F, Strom O. Development and use of FRAX in osteoporosis. Osteoporo Int. 2010;21(Suppl):S407–13. doi: 10.1007/s00198-010-1253-y. [DOI] [PubMed] [Google Scholar]
- 29.Cooper C, Coupland C, Mitchell M. Rheumatoid arthritis, corticosteroid therapy and hip fracture. Ann Rheum Dis. 1995;54:49–52. doi: 10.1136/ard.54.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Department of Health. The National Service framework for older people. London: Department of Health; 2001. [Google Scholar]
- 31.National Institute for Health and Clinical Excellence (NICE) Falls: the assessment and prevention of falls in older people: clinical guideline 21. London: NICE; 2004. [Google Scholar]


