Abstract
Objective
To assess the evidence regarding the adoption and efficacy of worksite health promotion programs (WHPPs) in small businesses.
Methods
Peer-reviewed research articles were identified from a database search. Included articles were published before July 2013, described a study that used an experimental or quasiexperimental design and either assessed adoption of WHPPs or conducted interventions in businesses with fewer than 500 employees. A review team scored the study’s rigor using the WHO-adapted GRADEprofiler “quality of evidence” criteria.
Results
Of the 84 retrieved articles, 19 met study inclusion criteria. Of these, only two met criteria for high rigor.
Conclusions
Fewer small businesses adopt WHPPs compared with large businesses. Two high-rigor studies found that employees were healthier postintervention. Higher quality research is needed to better understand why small businesses rarely adopt wellness programs and to demonstrate the value of such programs.
Employed Americans spend on average 54% of their waking time at work.1 Worksite wellness programs provide an opportunity to introduce preventive strategies that improve employee health. Nevertheless, health care in the United States has largely focused on disease treatment in clinical settings, placing less emphasis on health promotion and disease prevention in the workplace. Even when worksite wellness programs are adopted by US businesses, the majority of success has been reported in large, not small, businesses. For example, in 2008, 24% of large US businesses offered all elements of a comprehensive program as defined by HealthyPeople 2020,2 whereas only 4.6% of small worksites offer these components.30
With over half of the US workforce being employed by a small company (<500 employees),4 it is imperative that we understand the barriers to adoption of worksite wellness programs in small businesses. It is also necessary to identify evidence-based interventions that could improve the health of workers in small businesses. Perhaps not surprisingly, much of what we have learned on the subject comes from research studies conducted in large corporations,5–13 and not small businesses.14,15
The purpose of this study was to conduct a systematic review and determine the quality of evidence of the published literature regarding two key questions: (1) What is known concerning the adoption and barriers to adoption of worksite wellness programs in small businesses? (2) Do worksite wellness programs improve worker health in small businesses? On the basis of this systematic review and quality of evidence analysis, there seem to be unique challenges and significant research gaps regarding health promotion in small businesses.
METHODS
Data Sources
A literature search was conducted using the databases PubMed and Web of Science, and included articles up to and including September 2013. The MeSH terms used included health promotion/organization and administration, health promotion, disease management, wellness program, wellness center, small business, small businesses, workplace, and worksite, as well as combinations of these terms.
Inclusion and Exclusion Criteria
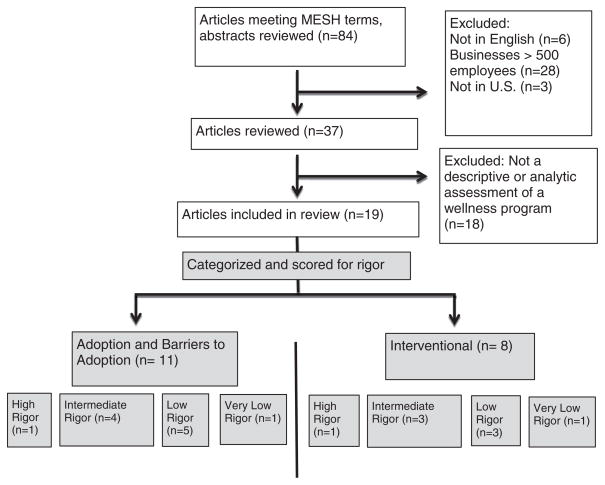
The criteria for study inclusion included the English language, businesses with fewer than 500 employees, and a descriptive or analytic assessment of a wellness program. Only studies conducted in the United States were included in this review. Studies were excluded if they only evaluated programs addressing occupational health and safety. As outlined in Fig. 1, we identified 84 articles meeting the MeSH terms. Nineteen of these references fulfilled the inclusion criteria.
FIGURE 1.
Inclusion criteria.
Assessing Rigor
Key findings were extracted from each article and complied in two tables. We extracted information regarding study design, subjects, business size, and the type of the wellness program.
To evaluate the quality of evidence, the 2002 GRADEprofiler (GRADEpro) rating scale adapted by the World Health Organization was used to score each study.16 This scale consists of four categories (high, intermediate, low, and very low), which take into account study type, sample representativeness, response rate, potential bias, external validity, and other factors. High rigor indicates an extremely strong association and no serious flaws in the study design. Intermediate rigor indicates a strong, consistent association with some flaws in the study design or execution. Low rigor indicates serious flaws in the study design or execution. Very low rigor indicates very serious flaws in the study design and poor execution. Two researchers independently scored the 19 articles. There was concordance on 16 of 19 studies. Consensus was reached on the three scoring discrepancies, both of which had differed by one grade level.
RESULTS
Tables 1 and 2 summarize the 19 studies included in this systematic review, separated into two categories: 11 articles examining adoption and barriers to worksite wellness programs in small businesses (Table 1), and 8 articles evaluating an actual intervention in small businesses (Table 2). Within the first category, we identified only one article with a score of “high” rigor, four as “intermediate,” five as “low,” and one as “very low.” For the interventional category, we scored one article as “high,” three as “intermediate,” three as “low,” and one as “very low.”
TABLE 1.
Studies Assessing Adoption of Wellness Programs
| Rigor Score | Author | Design | Modality | Subject(s) | Number of Employees | Key Findings | Limitations |
|---|---|---|---|---|---|---|---|
| High | Linnan et al3 | Descriptive | Comprehensive wellness program | 1553 businesses | Categories: 50–99, 100–249, 250–749, ≥750 | Business size was negatively correlated with the number of worksite wellness programs. Top barriers to program implementation (regardless of the size): lack of employee interest (63.5%), staff resources (50.1%), funding (48.2%), participation on the part of high-risk employees (48.0%), and management support (37.0%) | Variability of weights in 1 yr, less than ideal confidence intervals for industry comparisons, moderate nonresponse rates (yet nonresponse adjustments made) |
| Intermediate | Hersey et al17 | Descriptive | Obesity prevention | 16 worksites | Categories: 1–300 and 301–5000 | Important features of successful wellness programs included managerial support (8 of 9 businesses), use of health risk assessment (5 of 9 businesses), and creating a culture of health (9 of 9 businesses). Rapid implementation of programs was deemed an important advantage for small businesses | Only the highest-ranked businesses confirmed with on-site visits, data gathered by peers, small sample size |
| Intermediate | Hannon et al20 | Capacity and readiness assessment | Multiple wellness programs | 145 (small), 134 (medium) | Small (100–250), medium (250–4999) | In low-wage industries, capacity to implement WHP was very low; nearly half the sample reported no capacity. Smaller companies report less capacity and offer fewer programs than larger companies. Most respondents agreed a worksite wellness program would be beneficial, but fewer agreed one would be feasible, citing low capacity as one of the primary barriers | Presence of the program was self-reported. Response rate was 33.2%. Possible response bias. Implementation measures dichotomous, employers received equal treatment if the program reached all employees or only some |
| Intermediate | Jung et al40 | Interviews | Multiple wellness programs | 522 chief executive officers in Germany | Small (10–49), medium (50–249), large (≥250) | 40% of small companies had a positive attitude toward health promotion, 56% of medium, and 67% of large employers. This attitude has positive associations with company size, number of hierarchical levels, percentage of academically educated employees, and presence of employee management committee. Companies with a mid-market and upper-market position had a 90% higher odds of a positive health promotion attitude than lower-positioned companies. Study concludes that small companies with lower market positions and employees with lower education should be prioritized in establishing a positive attitude toward health promotion | 21% response rate (nonresponse analysis showed no difference) and limited transferability |
| Intermediate | Wilson et al19 | Descriptive | Descriptive | 2680 businesses | Categories: 15–50 and 51–99 | Worksites with 51–99 employees are twice as likely to offer a health promotion activity than worksites with 15–50employees. Breadth and depth of programs is lesser in worksites with 15–50employees. The programs offered at smaller businesses are focused on job-related hazards, as opposed to lifestyle topics. No significant difference for policies (smoking, alcohol, and drugs) between the two size groups | Not enough diversity in industry type to stratify for smaller businesses, did not examine businesses with fewer than 15 or greater than 100 employees |
| Intermediate | Smogor and Macrina18 | Descriptive | Multiple wellness programs | 204 businesses | <500 | A paper-based questionnaire found 87% did not have wellness programming. Programs most reported were first aid, safety and accident prevention, stress management, drug/alcohol abuse, and emotional health. Most reported reasons for not having a program: cost, perceived lack of employee interest, lack of facilities, and lack of expertise. The “major” reasons for discontinuing health promotion were lack of employee interest and participation, in addition to scheduling difficulties | Outcomes self-reported, some conclusions drawn from nonrigorous evidence |
| Low | Escoffery et al41 | Qualitative: semistructured interviews | Obesity prevention | 33 employees (over 50 yrs)0 | <50 | Qualitative themes reported: lack of a wellness program, no vending machines or cafeterias at work, not enough time to eating healthy, and lack of conversations with coworkers about health. Reported barriers to exercise included sedentary nature of work, or schedule that does not permit physical activity | Self-reported responses not validated, sample not representative, small sample size |
| Low | Divine27 | Descriptive, including the focus group | Multiple wellness programs | 187 business managers | <200 | The focus group reported humanitarian argument as more influential than financial motive: “letting employees know the company cares” and “improving employees’ quality of life” were two notable objectives. Interest in wellness programs about perceived effectiveness rather than meeting business’s needs | Low response rate |
| Low | Dubuy et al39 | Intervention evaluation (nonrandomized) | Bike-to-work program | 12 businesses (7 adopted programs) in Belgium | Small <100, medium <800 | Company size and sector had no statistical difference on adoption of the program comparing adopting and nonadopting businesses. Among employees, there was 65% awareness of the program. Those aware reported significantly more commuter cycling and a more positive view of cycling than unaware employees. The most reported barrier to participation was distance to work (20%) | Nonrandomized, no control group. Intervention implemented by the biased biking advocacy group. Initial participation fee, changed midway through study. Low response rate (23%), self-reported |
| Low | Kuehl et al42 | Study on adoption | Wellness and injury prevention | 12 fire departments | 40–140 | Adoption most dependent on the presence of both a willing fire chief and a firefighter to champion the wellness program. Organizational factors: finances, previous or existing wellness programs, and resistance to change, had little to no effect on adoption. Size did not significantly correlate with adoption | Nonrandomized, industry-specific, geographically limited, small sample size, self-reported |
| Low | Thompson26 | Descriptive | Multiple wellness programs | 64 businesses | <50 | Worksite size was a strong indicator of the number of wellness programs offered. Small companies on average offered fewer programs than large companies. Top reasons for implementing included: 83% improve health and decrease health problems, 70% decrease health care costs, 70% improve employee morale, and 53% improve productivity. Top barriers included: 38% too costly, 35% employees do not show an interest | Low response rate, only one industry |
| Low | McMahan et al 31 | Descriptive | Health promotion | 2000 businesses | <500 | 84% of businesses had at least one health promotion activity. Among those offered, the most common were safety related (67%), emergency training (52%), and hazardous materials training (48%). Only 51% offered a program involving fitness, nutrition of smoking cessation. Company size was a strong predictor of the number of health promotion activities offered. Small companies were less likely to offer every type of health activity. Businesses with 2–14 employees reported higher participation rates than businesses with 15–19 or 100–500 employees | Low response rate, limited geographic sampling |
| Very low | Yum43 | Descriptive | Multiple wellness programs | 2958 businesses in Korea | <300 | 41% of businesses expressed that periodical consultation and education were beneficial. The highest satisfaction was with consultation and education, in addition to the occupational disease screening service. The conclusion indicates that industrial workers prefer medical care services rather than health promotion (such as smoking cessation programs) | Inadequate explanation of research process, no assessment of nonresponse population, self-report of satisfaction |
| Very low | Tampson44 | Observational/descriptive case study | Multiple wellness programs | One business: 140 employees (204 white-collar and 179 manufacturing) | <500 | There was higher overall participation among office employees than among manufacturing employees. Overall, 50% of the company’s employees participated at least once. Over 2 yrs, the number of workouts declined, yet there was no trend in the number of participants | No control group, intervention not randomized, low external validity because of only one business |
TABLE 2.
Studies Assessing Interventions of Wellness Programs
| Rigor Score | Author | Design | Modality | Subject(s) | Number of Employees | Key Findings | Limitations |
|---|---|---|---|---|---|---|---|
| High | Sorensen et al21 | RCT | Cancer prevention: healthful eating, physical activity, tobacco control, and occupational health | 24 multiethnic manufacturing businesses | 50–150 | The intervention group scored higher on all outcomes (physical activity, produce consumption, red meat consumption and vitamin use) compared with control worksites. For fruit and vegetable consumption, the intervention was more effective among women, nonmanagers, and all other ethnic groups more so than whites. For red meat consumption, the intervention was more effective for women and less educated employees | Businesses not nationally representative, outcomes self-reported yet validated, statistic power to detect subgroup differences |
| Intermediate | Merrill et al24 | Case study | Physical, emotional, and mental health | One business | <500 | Employees improved on almost all categories of the well-being indices over 3 yrs: physical, emotional, and mental health, in addition to health behaviors, access to safe drinking water, affordable produce, and a safe exercise space. Greatest improvements were among those with a high-risk baseline, and older employees | No control group, selection bias |
| Intermediate | Merrill25 | Case-cohort descriptive study | Physical health, mental health, healthy behavior, and access to health services | One intervention company and 1276 control employees | <500 | Four well-being indices improved significantly in the intervention group. Nevertheless, there was no significant difference of self-perceived access to basic needs. There was a positive association between income and scores on the well-being indices. Perceived physical health was greater for men than for women, yet perceived healthy behaviors were opposite | Nonrandomized intervention group, selection bias |
| Intermediate | Merrill26 | Intervention evaluation | Exercise, sleep, stress, and diet programs | Five businesses | <500 | Exercise, diet, sleep, health perception, and life satisfaction had significant improvements. Smallest companies (<50 employees) had greater fruit consumption, nights of restful sleep, smoking cessation, and job satisfaction. Participation was lower among those with poor health and men. Job satisfaction decreased significantly. There was a positive association between health perception and health behaviors | Nonrandomized (selection bias), no control group, behavior and health outcome data self-reported |
| Low | Devine et al45 | Process evaluation | Walking and eating | Five businesses | <500 | There was a positive association between site-specific intervention reach, dose, and employee achievement of health goals (walking and eating habits). The two sites with fewer than 25 employees had greater reach. High reach was also associated with younger, more educated, and mixed job-type employees. In the three sites with the lowest implementation scores, competing priorities for leaders’ time was noted as a barrier | Nonrandomized, small sample size, potential positive response bias, self-reported and recall bias |
| Low | Allen et al46 | Intervention evaluation | Heart disease prevention: screening, education, and physical activity | 29 intervention employees and 31 control employees | 172 | After 1 yr, the intervention group scored better on health outcomes compared with the comparison group. For cost effectiveness, there was a $10.2 per percentage point reduction in LDL cholesterol and a $454.2 per percentage point reduction in heart disease risk | Nonrandomized, selection bias, not true RCT, controls received some exposure to intervention, only one business |
| Low | Erfurt and Holtyn29 | Analytic | Screenings, referral, education, and counseling | Three businesses | 5–296 | After the program, the employees showed improvements in blood pressure, cholesterol, cigarette smoking, weight control, and oxygen uptake | Only three worksites compared with much variability, no control group, low response rate |
| Very low | Taylor et al | Analytic: pre-/postassessment | Physical activity | 14 employees | <15 | After the program, a reduction in HDL cholesterol and weight was shown among employees | No control group, strong wellness culture before intervention, no correction for multiple comparisons |
RCT, randomized controlled trial
Study types varied, including descriptive, randomized controlled trials, case studies, and qualitative, yet all articles assessed a wellness program. The programs assessed were diverse, yet all fell under the wellness umbrella, including studies of physical fitness, smoking cessation, cancer risk reduction, cardiovascular disease education, violence prevention, and mental health promotion.
Specific strengths and limitations of the 19 studies are reported in Tables 1 and 2. Notably, many of the studies lacked a control group design, making it difficult to determine a causal relationship between wellness programming and health outcomes. Studies ranked with high and intermediate rigor are discussed below, within the two categories: adoption and interventions.
Studies on Adoption of Wellness Programs and Barriers to Adoption
Linnan and colleagues3 performed a study among businesses nationwide to monitor the progress of the HealthyPeople 2010 goal of 75% of businesses attaining worksite wellness programs. The goals posed in 2010 have been retained within the HealthyPeople 2020 goals, with a minor modification.2 A large sample of nationally representative businesses—stratified by size and industry type—was surveyed by telephone regarding their adoption of the five components of a comprehensive wellness program: health education, supportive social and physical environments, integration of programs into organization structure, linkages with existing programs, and screening programs.2 Results indicated that small businesses were less likely to offer all five components. In addition to few worksites meeting the comprehensive criteria, smaller worksites offered fewer individual programs: screening services, counseling opportunities, and disease management programs. Larger companies were more likely to have environments supporting physical activity, including shower facilities, on-site fitness facilities, and walking trails. The study concludes that despite shortcomings in adoption of worksite wellness by businesses of all sizes, larger worksites do more health promotion. Linnan and colleagues also reported on perceived barriers, irrespective of the employer size: lack of employee interest (63.5%), lack of staff resources (50.1%), funding (48.2%), low participation on the part of high-risk employees (48.0%), and lack of management support (37.0%). With its large sample size, high response rate, nonresponse adjustments, and stratification by industry, this study demonstrated strong external validity and was scored as having high rigor.
Hersey and colleagues17 developed the novel measure SWAT (Swift Worksite Assessment and Translation) to examine obesity prevention in small- and medium-sized worksites. The researchers conducted site visits and administered surveys to assess the wellness programs at each worksite. An expert panel reviewed reports written about each worksite, and determined three necessary components for a successful program: individual, environmental, and occupational elements. Specifically, the panel recommended managerial support, a culture of health, and organizational policy changes. Several incentive-driven programs were offered to spouses, as a potentially important way to integrate a home/work balance. On the basis of GRADEpro criteria, this study was not highly rigorous, having performed site-visit validation for only selected businesses. It was also limited by small sample size.
Smogor and colleagues18 conducted a survey among small businesses, defined as fewer than 500 employees. The investigators assessed types of programming offered and perceived barriers among 204 businesses, of which 87% had no wellness programming. Among those that did offer programs, the areas most reported were first aid, safety and accident prevention, stress management, drug/alcohol abuse, and emotional health. Most organizations reported reasons for not having wellness programs as cost, perceived lack of employee interest, lack of facilities, and lack of expertise. According to the authors, small businesses lack awareness about the benefits of a wellness program. The reported reasons for discontinuing health promotion were lack of employee interest and participation, in addition to scheduling difficulties. This study design validated the questionnaire and stratified businesses by size and industry, yet it received an intermediate score because it was descriptive and responses were not validated by on-site visits.
Wilson and colleagues19 surveyed 2680 worksites nationally to assess the presence of worksite wellness programs. The researchers found that smaller worksites offer fewer programs than do larger worksites. The programs offered at smaller businesses were more focused on job-related hazards, as opposed to health behavior and lifestyle topics. Wilson and colleagues found that large worksites are twice as likely to offer a health promotion activity compared with small businesses. Yet, they found little difference by workplace size for institutional health policies such as tobacco or alcohol use. This study was ranked intermediate because of a large sample size and stratification by size, yet there was not enough diversity by industry to stratify for businesses smaller than 15 employees.
Hannon and colleagues assessed both the capacity and the readiness of 145 small worksites in addition to 134 medium-sized companies.20 They found that the capacity of small employers to implement worksite health promotion was very low. The average capacity score (measure assessing capacity to implement a program) was 0.6 (0 to 3 range) and 1.08 for medium-sized employers. Compared with medium-sized workplaces, smaller companies offered fewer programs. Hannon and colleagues also asked for qualitative feedback and found that most respondents agreed that a worksite wellness program would be beneficial (rated 3.78 of 5 on the beneficial scale), but few agreed adopting and running one would be feasible. Because of the study’s reliance on unconfirmed, self-reported data, a 33.2% response rate with potential for response bias, this article was rated as intermediate.
Studies on Interventions in Small Businesses
The “Healthy Directions–Small Business” worksite wellness program is a social-contextual model that focuses on multiple levels of influence, inclusion of employees’ families, and integrates occupational and health promotion.21 The focus of this specific intervention was cancer prevention, which included topics such as healthful eating, physical activity, and tobacco control. A crucial step was the creation of an employee advisory board, composed of workers and managers, to assess interest, design programs, and meet with an external program advisor for guidance. A randomized, controlled trial was conducted among 24 multiethnic manufacturing businesses in Massachusetts, of which half received the “Healthy Directions” program, and half served as a control group. The program was designed and implemented with the multiethnic population in mind, being conscious of low literacy and cultural backgrounds. Each intervention worksite had the same program components, yet they were tailored to the specific employee community (ie, testimonials of workers from that site and photographs of specific employees using stairs). Other interventional studies in this systematic review include two articles published about the same program: a process evaluation by Hunt et al22 and a randomized, controlled trial by Sorensen et al,21 examining health outcomes.
The process evaluation study examined factors promoting and inhibiting worker participation, and assessed the feasibility of implementation.22 The evaluation was both quantitative (measuring participation rates) and qualitative (attaining employee and manager feedback). At the intervention sites, there was an average of a 47% participation rate. Hunt et al compared those worksites with the maximum and minimum participation rates to infer successful or detrimental strategies of the best and worst programs. On the basis of these comparisons, Hunt et al suggested that managerial support and participation were notable characteristics of the well-attended programs. In addition, a culture of worksite-wide gatherings before the introduction of the wellness intervention may have played a role in increasing participation. Other successful strategies included interactive displays and demonstrations available throughout the day to accommodate schedules, and cohesive worker–manager relationships. The qualitative evidence does not indicate causality; however, we scored the study as high rigor because of the study design and external validation.
Sorensen et al21 published the second article regarding the program, which assesses the health outcomes of the intervention. Employees were surveyed before and after the intervention, examining the following health behaviors: physical activity use, fruit and vegetable consumption, red meat consumption, and vitamin use. In addition, the following demographic covariates were examined: sex, ethnicity, education, and job status (manager or nonmanager). After the intervention, those assigned to the intervention scored higher on all relevant health behaviors, as compared with control worksites. For fruit and vegetable consumption, the intervention seemed to be more effective among the following groups: women, nonmanagers, and all other ethnic groups more so than whites. In terms of red meat consumption, women and less educated employees showed a greater reduction when compared with other subgroups within the intervention. These results indicate that education or ethnicity may be predictive of a lower baseline measure, and therefore indicate a greater opportunity to improve. Sorensen et al conclude that small businesses that have more blue-collar workers have a potential for greater behavior change. Because of a rigorous study design, assessment of nonparticipating worksites and external validity, this study was given a high-rigor score.
In a study scored as intermediate, Merrill and colleagues24 evaluated an intervention within a 479-employee business in Nebraska. The wellness program incorporated physical health, mental health, healthy behavior, and access to health services. The employees with the intervention improved their scores on all four well-being indices compared with control workers in the same geographic area. Nevertheless, there was no significant difference of self-perceived access to basic needs. Merrill and colleagues report a correlation between income and scores on the well-being indices. Also, men in the study perceived greater physical health than women, yet women perceived more healthy behaviors than did the male participants. The baseline well-being scores tended to increase with income, which indicates that managers and CEOs started with higher scores, and had less room for health improvement. This study was not scored with high rigor because the measures were only given once to each group, the intervention was not randomized, and control participants were not exclusively from small businesses.
Another study by Merrill and colleagues assessed the efficacy of a wellness program in a 440-employee business, over a 3-year period.25 The program focused on physical, emotional, and mental health, and used several well-being indices to measure health outcomes, in addition to health behaviors, access to safe drinking water, affordable produce, and a safe exercise space. Employees improved on almost all categories of the well-being indices over 3 years. The greatest improvements in behavior change were observed among employees with a high-risk baseline, and among older employees. Although this study was longitudinal, it only assessed a program in a single business, and there was no control group or randomization of the intervention; therefore, it received an intermediate score.
A third article, published in 2013, by Merrill,26 examined an intervention consisting of six incentivized behavior change campaigns with five small companies. The researchers measured exercise, diet, sleep, health perception, and life satisfaction pre- and postintervention, observing statistically significant improvements in company averages for all categories. Unexpectedly, the smallest companies (fewer than 50 employees) had greater fruit consumption, nights of restful sleep, smoking cessation, and job satisfaction. Merrill and colleagues found that participation was lower among men and among those with poor health. This finding provides impetus to focus recruitment efforts among these hard-to-reach populations. This article was rated as intermediate because the intervention was nonrandomized and lacked a control group.
DISCUSSION
Several studies included in this review provide useful insights into factors that influence the adoption or effectiveness of wellness programs in small businesses. Nevertheless, it is difficult to draw broad conclusions because limited high-quality evidence exists. The interventional studies examined in this review lack consistency. Few meet current standards for overall rigor. We identified two high-rigor studies. Although they examined different dimensions of worksite wellness programs and different worksite settings (eg, industry and geographical region), we can conclude that employees were healthier postintervention compared with the control group. The interventional literature in this review explored a variety of health outcomes, and the low number of rigorous studies limits our ability to formulate evidence-based specific recommendations for small businesses, without extrapolating from studies of large corporations.
The evidence-based strategies used in large worksites are being adopted by small employers and may prove beneficial. Nevertheless, we were unable to identify any studies that specifically address the hypothesis that large business solutions are generalizable to small business. Caution should be taken in posing recommendations to small businesses because there is simply not enough published evidence to verify the transferability, especially when considering the many unique challenges faced by small businesses.
Unique Barriers and Opportunities for Small Businesses
Table 3 summarizes barriers faced by small businesses that may hinder the implementation or sustainability of a worksite wellness program. Although we found a paucity of rigorous evidence on the barriers to adoption of wellness programs, it is worth enumerating some of the qualitative and limited quantitative evidence to evaluate and inform recommendations for small businesses and to guide further research. There have been several studies that have surveyed businesses, inquiring about perceived barriers; some of which did not score highly using the GRADEpro scale.26,28 Linnan and colleges conducted a rigorous survey of perceived barriers, with high external validity. This study likely reflects the obstacles faced by businesses, though it does not examine the nuanced barriers specifically for smaller worksites.
TABLE 3.
Unique Barriers and Opportunities for Small Businesses
| Barriers | Opportunities |
|---|---|
| Direct cost3 | Less bureaucracy, easier implementation |
| Indirect cost (time, staff, and facility)32 | Employee suggestions incorporated more easily |
| Lack of employee interest3 | Greater personal accountability |
| Lack of management support3 | Potential for teamwork/bonding |
| Lack of expertise | Higher participation rates31 (note: study scored as low rigor) |
| Uncertain ROI because of less employer-based health insurance33 | |
| Rural setting with less access, or fewer health promotion providers32 | |
| Manager fear of “paternalistic” image29 | |
| Difficult to evaluate (expertise, cost to outsource) | |
| Protecting employee privacy, avoid stigmatizing individuals |
ROI, return on investment.
Direct cost of a program is likely a major hindrance for small businesses; there are fewer resources to invest in a program that may or may not pay off. There is also the indirect cost of wellness programs, including time and staff. Many small businesses cannot afford to hire a staff person dedicated to wellness, and yet this is a crucial component; one study found that businesses with this dedicated staff person are ten times more likely to offer a wellness program.14
Small businesses may lack the facility space or expertise to carry out a program independently.32 Hiring a third party to run the program may be too costly for a small operation to consider. Small businesses in rural settings may have more difficulty because of a lack of such providers.32
Large companies may invest in wellness programs because of the return on investment in the form of lower health insurance premiums. Yet employer-based coverage has declined in recent years at a faster rate for employees of small businesses, particularly very small businesses.33 There may be less incentive to implement wellness programs when employers may not benefit from the changes in insurance premiums.
Protecting employee privacy is also an issue in small settings, as is avoiding stigmatizing high-risk populations and discriminatory job dismissal.
Businesses need to evaluate their wellness programs—or hire a third party to do so—to ensure efficacy and sustainability, yet this process may also require expertise and time that the company lacks, or may require additional financial resources to outsource the evaluation.
A possible additional barrier, not included in Table 3, is that managers may be wary of seeming paternalistic in smaller, more intimate business communities.29 By analogy, this avoidance of perceived “meddling” might account for why 15.1% more businesses with 100 or more employees conduct drug screenings as compared with businesses with 15 to 99 employees.19 Employers may want to deflect responsibility to the employees to become healthier, or many genuinely think their employees do not need wellness programs.
The broad selection of the effective “menu” approach proposed by Erfurt and Holtyn30 may be challenging for small businesses to implement. With a small population, it is hard to justify targeted interventions that may reach the small number of individuals in a small business.
On the positive side, there are a number of reasons why small businesses may prove to be in a good position to adopt successful worksite wellness programs, as summarized in Table 3. The decision-making process may be less bureaucratic in a small setting, allowing for an easier implementation process. Also, because there are fewer employees, a larger percentage of preferences may be accommodated. The sense of individual contribution could encourage employees to be more invested in the program.31 In a larger workplace, the program would most likely come from management, with less perceived input from employees. In a more intimate workplace community, there may me more personal accountability, which could impact follow-through and sustainability of the program. Within a small group of colleagues, there is a potential for teamwork development and group bonding because of collective wellness involvement. There is some indication that when small businesses do institute wellness programs, they can be successful. Participation rates in wellness programs have been studied and found to be higher in small businesses.32 Although that study lacked rigor because of a low sample size and lack of external validity, if this finding is confirmed by future studies, it would lend impetus to efforts to help small businesses overcome barriers to adoption.
Limitations
We acknowledge several limitations in this systematic literature review. We may have missed relevant articles because of insufficient MeSH terms. There may be studies examining the current topic that do not explicitly mention a small business definition in the abstract. The term “worksite wellness” may not be used explicitly in abstracts concerning this topic. To mitigate this limitation, we conducted separate searches for specific topics such as cancer prevention or mental health. Those searches did not yield additional small business research studies. Another limitation is the GRADE-pro scoring system that we used to rate the quality of evidence. This scoring system has specific criteria for assessing rigor, although there is some ambiguity. We do not think this significantly impacted our conclusions, because this ambiguity mainly affects the ability to distinguish between the “low” and “very low” categories, and the level of agreement between our two independent graders was high. There is also inherent subjectivity in assessing the quality of evidence, which is an additional limitation.
Research Gaps
Businesses of any size may be motivated to implement a program because of the desire for a healthier workforce, increased job satisfaction, reduced absenteeism, reduced costs, or other rationales. Nevertheless, more research is needed to measure what factors motivate employers and employees in small business settings. One primary area of concern is cost, which could be offset by changes in health insurance premiums because of healthier employees. Health insurance is particularly salient because of its rising cost. In 1991, employers covered 14% of national health expenditures, which increased to 33% in 2005.35,36 Partially because of this increasing expense, more and more businesses are implementing wellness programs. Yet, small businesses still incorporate far fewer programs than do larger corporations.3
There are several gaps in the research that warrant further investigation. The location of a business—whether it is rural or urban—may be an important characteristic when considering worksite wellness. Businesses in rural settings may not have the level of access to facilities, vendors, or education personnel that are available to workplaces in cities. Recommendations in many of the publications that we reviewed address all worksites without consideration of a business’s geographic location, potentially overlooking important regional differences. More research is also needed to examine low-wage and underserved worker populations. Merrill and colleagues found that recruitment was lower among hard-to-reach employees, leading the authors to recommend the use of more tailored recruitment strategies among these populations.26 Many worksite wellness interventions may lack cultural relevance for certain audiences, challenging small businesses to find resources that work for these populations. Also, warranting more research, are the factors that influence the participation rates in worksite wellness programs, and that examine the characteristics of those employees who participate and those who do not. Evidence that smaller worksites show higher participation rates than larger businesses, warrants confirmation and should take into account various incentive and disincentive strategies. This area is important to understand because it will inform how transferable the evidence for large worksite wellness is to smaller settings. An additional research gap is how worksite wellness impacts workers’ compensation in small businesses. Examining this outcome is important because both direct cost and lost time can be very important for smaller worksites. Further research is also needed to examine how worksite health promotion carries over from work to home and impacts family members of the employee. We speculate that in a smaller, more cohesive environment, employers may have a better opportunity to promote good health that improves health for family members as well. Understanding the work–life transferability may have widespread implications, such as confirming a method of improving the nation’s health.
Nishikido and colleagues15 reviewed some of the Japanese literature on worksite wellness for small- and medium-sized businesses and developed an “action checklist” to help employers implement an extensive wellness program. The checklist of recommendations developed by Nishikido et al is similar to the HealthyPeople 2020 comprehensive worksite wellness program,2 with two additions: an emphasis on mental health promotion and use of available services/information. Although the checklist was designed specifically for Japanese businesses, it stresses topics that may be applicable to US businesses in which these factors are overlooked and provides directions for future research. Evidence-based resources specifically for small businesses are lacking; however, a few valuable websites were identified.37,38
Lastly, researchers need to examine how to disseminate worksite wellness to small employers. Simply touting the evidence from studies of large businesses may not be sufficient to drive the implementation of a program; employers may be more receptive to advice from fellow business owners. Even if high-quality evidence supports wellness programs, it may be rendered useless if employers are not sold based on the delivery.
There are many facets of health promotion in small businesses that need further study. The field would greatly benefit from a large, longitudinal randomly controlled trial examining the efficacy of a comprehensive wellness program. Studies examining small business health promotion have largely addressed single interventions and not assessed comprehensive wellness programs. Future studies should include more multidimensional interventions. That being said, such studies are challenging because if they find an effect, it becomes complicated to assess which components of the intervention produced the effect. Researchers examining worksite wellness for all business sizes will continue to face this challenge. When randomly controlled trials are conducted, it would be important to stratify by business size, geographic location, and industry. More research could also determine the effects of national policy on small business wellness programming. Finally, there is a large push from the National Institute of Occupational Safety and Health for organizations to integrate health promotion and health protection. Historically, these two fields have resided in separate silos. An emerging body of evidence supports efforts to integrate these two approaches to promote the total health of workers; however, little is known at this time regarding the merits of this approach when applied to small businesses.
In the United States, the Patient Protection and Affordable Care Act39 of 2010 provides technical assistance for small businesses to offer worksite wellness programs and suggests a series of incentives, or “rewards,” for participation. This federal law and its language in support of small business health promotion reinforces the urgent need for more high-quality research that specifically addresses adoption, implementation, efficacy, and sustainability of worksite wellness within small business settings.
CONCLUSIONS
In conclusion, limited high-quality evidence exists regarding the prevalence, characteristics, or effectiveness of wellness programs in the small business setting. Several studies, though, provide useful insights into factors that influence the adoption or effectiveness of wellness programs in small businesses. On the basis of the adoption and barriers to adoption literature, we conclude that small businesses offer fewer programs than do larger businesses for a number of reasons that may be unique challenges for small organizations. Future interventional research studies should address how addressing such barriers can improve participation at the organizational level.
Acknowledgments
All authors were funded through a grant from the Centers for Disease Control, National Institute for Occupational Safety and Health, awarded to our institution, the University of Colorado. Ms McCoy is a former employee and all other authors are current employees at the University of Colorado Denver.
Footnotes
The authors declare no conflicts of interest.
References
- 1.The U.S. Bureau of Labor Statistics. [Accessed December 23, 2013];American time use survey. 2010 Available at http://www.bls.gov/news.release/archives/atus06222011.pdf.
- 2.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC: [Accessed August 22, 2012]. Available at http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf. [Google Scholar]
- 3.Linnan L, Bowling M, Childress J, et al. Results of the 2004 national worksite health promotion survey. Am J Public Health. 2008;98:1503–1509. doi: 10.2105/AJPH.2006.100313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The U.S. Bureau of Labor Statistics. [Accessed August 22, 2012];Business employment dynamics survey. 2011 Available at http://www.bls.gov/schedule/archives/cewbd_nr.htm#2011.
- 5.Chapman LS. Meta-evaluation of worksite health promotion economic return studies. Am J Health Promot. 2003;17:1–10. doi: 10.4278/0890-1171-19.4.TAHP-1. [DOI] [PubMed] [Google Scholar]
- 6.Chapman LS. American journal of health promotion, meta-evaluation of worksite health promotion economic return studies: 2005 update. Am J Health Promot. 2005;19:1–11. doi: 10.4278/0890-1171-19.4.TAHP-1. [DOI] [PubMed] [Google Scholar]
- 7.Goetzel RZ, Ozminkowski RJ. The health and cost benefits of work site health-promotion programs. Annu Rev Public Health. 2008;29:303–323. doi: 10.1146/annurev.publhealth.29.020907.090930. [DOI] [PubMed] [Google Scholar]
- 8.Hallett R. Smoking intervention in the workplace: review and recommendations. Prev Med. 1986;15:213–231. doi: 10.1016/0091-7435(86)90042-3. [DOI] [PubMed] [Google Scholar]
- 9.Hilliard TM, Boulton ML. Public health workforce research in review: a 25-year retrospective. Am J Prev Med. 2012;42:17–28. doi: 10.1016/j.amepre.2012.01.031. [DOI] [PubMed] [Google Scholar]
- 10.Hughes MC, Yette EM, Hannon PA, Harris JR, Tran NM, Reid TR. Promoting tobacco cessation via the workplace: opportunities for improvement. Tob Control. 2011;20:305–308. doi: 10.1136/tc.2010.041038. [DOI] [PubMed] [Google Scholar]
- 11.Osilla KC, Van Busum K, Schnyer C, Larkin JW, Eibner C, Mattke S. Systematic review of the impact of worksite wellness programs. Am J Manag Care. 2012;18:68–81. [PubMed] [Google Scholar]
- 12.Parks KM, Steelman LA. Organizational wellness programs: a meta-analysis. J Occup Health Psychol. 2008;13:58–68. doi: 10.1037/1076-8998.13.1.58. [DOI] [PubMed] [Google Scholar]
- 13.Soler RE, Leeks KD, Razi S, et al. A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. Am J Prev Med. 2010;38:237–262. doi: 10.1016/j.amepre.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 14.Linnan LA, Birken BE. Small businesses, worksite wellness, and public health: a time for action. N C Med J. 2006;67:433–437. [PubMed] [Google Scholar]
- 15.Nishikido N, Yuasa A, Motoki C, et al. Development of multi-dimensional action checklist for promoting new approaches in participatory occupational safety and health in small and medium-sized enterprises. Ind Health. 2006;44:35–41. doi: 10.2486/indhealth.44.35. [DOI] [PubMed] [Google Scholar]
- 16.Guidelines for WHO Global programme on evidence for health policy. 2003:18. [Google Scholar]
- 17.Hersey J, Williams-Piehota P, Sparling PB, et al. Promising practices in promotion of healthy weight at small and medium-sized US worksites. Prev Chronic Dis. 2008;5:1–11. [PMC free article] [PubMed] [Google Scholar]
- 18.Smogor J, Macrina DM. Problems in worksite health promotion: the perspective of small business (continuing education credit) AAOHN J. 1987;35:224–228. [PubMed] [Google Scholar]
- 19.Wilson MG, DeJoy DM, Jorgensen CM, et al. Health promotion programs in small worksites: results of a national survey. Am J Health Promot. 1999;13:358–365. doi: 10.4278/0890-1171-13.6.358. [DOI] [PubMed] [Google Scholar]
- 20.Hannon PA, Garson G, Harris JR, Hammerback K, Spoher CJ, Clegg-thorp C. Workplace health promotion implementation, readiness, and capacity among midsize employers in low-wage industries. Am College Occup Environ Med. 2012;54:1337–1343. doi: 10.1097/JOM.0b013e3182717cf2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sorensen G, Barbeau E, Stoddard AM, et al. Promoting behavior change among working-class, multiethnic workers: results of the healthy directions—small business study. Am J Public Health. 2005;95:1389–1395. doi: 10.2105/AJPH.2004.038745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hunt MK, Barbeau EM, Lederman R, et al. Process evaluation results from the Healthy Directions-Small Business study. Health Educ Behav. 2007;34:90–107. doi: 10.1177/1090198105277971. [DOI] [PubMed] [Google Scholar]
- 23.Merrill RM, Aldana SG, Pope JE, et al. Evaluation of a best-practice worksite wellness program in a small-employer setting using selected well-being indices. J Occup Environ Med. 2011;53:448–454. doi: 10.1097/JOM.0b013e3182143ed0. [DOI] [PubMed] [Google Scholar]
- 24.Merrill RM, Aldana SG, Vyhlidal TP, Howe G, Anderson DR, Whitmer RW. The impact of worksite wellness in a small business setting. J Occup Environ Med. 2011;53:127–131. doi: 10.1097/JOM.0b013e318209e18b. [DOI] [PubMed] [Google Scholar]
- 25.Merrill RM. A small business worksite wellness model for improving health behaviors. J Occup Environ Med. 2013;55:895–900. doi: 10.1097/JOM.0b013e31826eef83. [DOI] [PubMed] [Google Scholar]
- 26.Thompson SE. Worksite wellness programs on the USA-Mexico border. Calif J Health Promot. 2003;1:102–108. [Google Scholar]
- 27.Divine RL. Determinants of small business interest in offering a wellness program to their employees. Health Mark Q. 2005;22:43–58. doi: 10.1300/j026v22n03_04. [DOI] [PubMed] [Google Scholar]
- 28.Eakin JM. Leaving it up to the workers: sociological perspective on the management of health and safety in small workplaces. Int J Health Serv. 1992;22:689–704. doi: 10.2190/DNV0-57VV-FJ7K-8KU5. [DOI] [PubMed] [Google Scholar]
- 29.Erfurt JC, Holtyn K. Health promotion in small business: what works and what doesn’t work. J Occup Med. 1991;33:66–73. doi: 10.1097/00043764-199101000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Harden A, Peersman G, Oliver S, Mauthner M, Oakley A. A systematic review of the effectiveness of health promotion interventions in the workplace. Occup Med (Lond) 1999;49:540–548. doi: 10.1093/occmed/49.8.540. [DOI] [PubMed] [Google Scholar]
- 31.McMahan S, Wells M, Stokols D, et al. Assessing Health Promotion Programming in Small Business. Am J Health Stud. 2001;17:120–128. [Google Scholar]
- 32.Goetzel RZ, Liss-Levinson RC, Goodman N, et al. Development of a community-wide cardiovascular risk reduction assessment tool for small rural employers in upstate New York. Prev Chronic Dis. 2009;6:1–7. [PMC free article] [PubMed] [Google Scholar]
- 33.Jost TS. Employers and the exchanges under the small business health options program: examining the potential and the pitfalls. Health Aff (Millwood) 2012;31:267–274. doi: 10.1377/hlthaff.2011.1011. [DOI] [PubMed] [Google Scholar]
- 34.Stokols D, Pelletier KR, Fielding JE. Integration of medical care and worksite health promotion. JAMA. 1995;273:1136–1142. [PubMed] [Google Scholar]
- 35.Thompson SE, Smith BA, Bybee RE. Factors influencing participation in Worksite Wellness Programs among minority and underserved populations. Fam Community Health. 2005;28:267–273. doi: 10.1097/00003727-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Wellness Council of America. [Accessed January 30, 2014];Wellness for small business. Available at http://welcoa.org/wellworkplace/index.php?category=22.
- 37.Centers for Disease Control and Prevention. [Accessed January 30, 2014];Workplace safety & health topics, small business. Available at http://www.cdc.gov/niosh/topics/smbus.
- 38.Patient Protection and Affordable Care Act, P. L. (March 23, 2010). Technical Assistance for Employer-based Wellness Programs. Sec. 4303.
- 39.Dubuy V, de Cocker K, De Bourdeaudhuij I, et al. Evaluation of a workplace intervention to promote commuter cycling: a RE-AIM analysis. BMC Public Health. 2013;13:587–598. doi: 10.1186/1471-2458-13-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jung J, Nitzsche A, Ansmann L, et al. Organizational factors and the attitude toward health promotion in German ICT companies. Health Promot Int. 2011;27:382–393. doi: 10.1093/heapro/dar049. [DOI] [PubMed] [Google Scholar]
- 41.Escoffery C, Kegler MC, Alcantara I, Wilson M, Glanz K. A qualitative examination of the role of small, rural worksites in obesity prevention. Prev Chronic Dis. 2011;8:A75. [PMC free article] [PubMed] [Google Scholar]
- 42.Kuehl H, Mabry L, Elliot DL, Kuehl KS, Favorite KC. Factors in adoption of a fire department wellness program: champ-and-chief model. J Occup Environ Med. 2013;55:424–429. doi: 10.1097/JOM.0b013e31827dba3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yum Y. Realization of Workers’ Health Promotion Services under the umbrella of the National Health Promotion System of Korea. J of Occup Health. 2000;42:156–162. [Google Scholar]
- 44.Tampson P. A facility based wellness program adapted to serve a small white and blue collar population. Am J Health Promotion. 1988:39–46. doi: 10.4278/0890-1171-2.3.39. [DOI] [PubMed] [Google Scholar]
- 45.Devine CM, Maley M, Farrell TJ, Warren B, Sadigov S, Carroll J. Process evaluation of an environmental walking and healthy eating pilot in small rural worksites. Eval Program Plann. 2012;35:88–96. doi: 10.1016/j.evalprogplan.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 46.Allen JC, Lewis JB, Tagliaferro AR. Cost-effectiveness of health risk reduction after lifestyle education in the small workplace. Prev Chronic Dis. 2012;9:E96. doi: 10.5888/pcd9.110169. [DOI] [PMC free article] [PubMed] [Google Scholar]