Abstract
Introduction
Young injection drug users (IDU, under age 30) often inject with other IDU, creating an environment for risk of blood-borne disease transmission through sharing of needles and drug preparation equipment. Epidemiologic studies rely on self reported injection behavior data for measures of transmission risk, therefore we sought to quantify the degree of concordance of reported injecting risk behaviors between injecting dyads.
Methods
From May, 2006 through 2013 we enrolled 72 injecting dyads in San Francisco, California, who were hepatitis C virus (HCV) RNA discordant. Each partnership was followed prospectively for up to six months. Monthly interviews from each partner were date-matched and responses to relationship characteristics and risk behavior questions were compared. Concordance of reporting was estimated with the concordance correlation coefficient for longitudinal data (CCC) and the prevalence adjusted bias adjusted kappa (PABAK).
Results
Participants had a median age of 26 (IQR: 23, 28) years and median years injecting of 7.0 (IQR: 3.0,10.6). Thirty-eight percent of the injecting dyads were also sexual partners. Concordance levels were highest for partnership characteristics, such as length of acquaintance, number of days cohabitating, and sexual intercourse in the past month (CCC = 0.95; 0.82, and 0.90, respectively). Shared injection risk behaviors such as injecting with the HCV+ partner’s previously used syringe and using contaminated injection preparation equipment had slight to fair agreement (CCC = 0.22; 0.23; PABAK = 0.43,0.36, respectively).
Conclusions
Concordance levels ranged from low to high. Potential sources of measurement error for low agreement items include recall and social-desirability biases and question interpretation.
Keywords: Epidemiology, Drug users, Agreement, Young adult, Hepatitis C, Dyad
1. Introduction
Drug use among young injection drug users (IDU) is a highly social activity (Koester et al., 2005; Stimson et al, 1998). Young IDU frequently inject with other IDU and have risk behaviors that put them at high risk for blood-borne disease transmission, such as sharing injecting equipment (Hahn et al, 2010, 2002). Self-reported data are frequently used to assess the behavioral risks associated with parenteral disease transmission, however, these data are subject to reporting biases, such as social desirability bias due to the sensitive nature of the subject matter (Latkin et al, 1993). Self-reported drug consumption can be validated with biomarkers derived from biological specimens, such as urine, hair, and nails, each which have varying time frames and test characteristics. Self-reported condom use can be validated with prostate-specific antigen testing within a limited time frame (Macaluso et al, 1999). However, validating self-reported injection risk-behaviors, such as sharing injecting equipment is not currently feasible (Catania et al., 1990; Darke, 1998). In circumstances where no biomarkers exist, collateral validation is an alternative method of examining the validity of self-reported behaviors.
Collateral interviews, in which close contacts are asked about the behaviors of the study subjects, have been used extensively, with varied results, to examine concordance of HIV and sexually transmitted infection (STI) risk reporting in heterosexual couples (Hageman et al, 2009; Harvey et al., 2004; Helleringer et al, 2011; Stoner et al., 2003; Witte et al, 2007; Yamazaki et al., 2010). For example, Helleringer et al. (2011) found low concordance in sexual partnership concurrency reporting when examining partnership histories in a sexual network mapping study in Malawi. Witte et al. (2007) found relatively high levels of agreement for awareness of partner’s HIV status and injection drug use history, but low concordance on concurrent sexual behavior. In Stoner et al. (2003) agreement was highest for perceived partner age, race/ethnicity, and duration of sexual partnership; but low for knowledge of partner’s work in commercial sex, number of other sex partners, and for perceived quality of communication within the partnership. We are aware of only a small number of studies that have examined the concordance of reporting of injection behaviors within injecting dyads (Bell et al., 2000; Darke, 1998,1992; Goldstein et al., 1995). Using collateral interviews of sexual partners of IDUs, Darke et al. (1992) reported moderate to high concordance on injecting and sexual practices. In a study of injecting dyads, Goldstein et al. (1995) found low concordance on injection behavior and higher agreement on sexual behaviors. Another study in sexual and drug using partners found high concordance on sexual and drug use behaviors but lower concordance on frequency and lower agreement as the time intervals between partner interviews increased (Bell et al., 2000). To our knowledge, there are no studies of concordance of injection behavior reporting among young IDU, a key population in an emerging epidemic of HCV.
In order to develop prevention strategies targeted to injecting dyads, we need an accurate assessment of injection and sexual risk behavior occurring within those partnerships. Examining behaviors reported by both members allows the assessment of the relative accuracy of key behavioral data. In the present study, our objectives were (1) to determine the level of agreement between self-reported relationship characteristics and injection and sexual risk behaviors within hepatitis C virus (HCV) discordant injecting partnerships, and (2) to utilize measures of concordance appropriate for comparing low-prevalence behaviors and repeated measures data.
2. Methods
The Partner Study is a sub-study of the UFO Study, a prospective observational cohort study of young IDU at risk for HCV in San Francisco, CA. From May, 2006 to December, 2013 the Partner Study recruited participants from the greater UFO Study. Detailed methods on the recruitment and eligibility of the UFO Study cohort have been published previously (Hahn et al., 2002; Page et al., 2009). The primary objectives of the Partner Study were to evaluate transmission among these partnerships and to document distinct HCV transmission events using phylogenetic methods. The present study examines concordance of self-reported data utilizing data collected for the Partner Study.
Injecting partnerships were recruited as follows: participants in the UFO Study who, during their UFO study interview, reported injecting at least weekly with a person of HCV discordant or unknown serostatus were invited to return with up to 3 their injecting partner(s) within 4 weeks to screen for Partner Study eligibility. Eligible partnerships were either injection-only or injection and sexual partnerships. Both members of the dyad were required to be present at the time of screening, where each was screened separately about their injecting activity with their partner. Interviewers administered a series of rotating questions asking each partner to provide basic demographic and injecting behavior information about themselves and their partner, as well as information about the partnership, based on methods used in a study of drug using couples (McMahon et al., 2003) to validate the partnership. Those that reported injecting together five or more times in the same physical space in the past month then had blood drawn to test for HCV and were asked to return a week later for results. Anti-HCV was detected using a third generation EIA(EIA-3; Abbott Laboratories) and HCV RNA testing was performed using a transcription mediated amplification (TMA) technique (dHCV TMA assay component of the Procleix HIV-1/HCV assay, Gen-Probe Inc., San Diego, CA). Injecting partnerships that were HCV RNA discordant were subsequently invited to enroll in the Partner Study. HCV results were disclosed separately and privately for each individual, and those of their partners were not discussed. Upon successful enrollment, participants completed an interviewer-administered structured interview and were asked to return monthly for six months for follow-up interviews. Re-enrollment for another 6 months occurred if the partnership was still actively injecting together and HCV RNA discordant. Participants were allowed to enroll with maximum of 3 partners at any one time. While both members of the partnership were required to complete the initial partner interview on the same day, they were not required to do so on their follow-up visits. Informed consent was obtained from all participants and study procedures were approved by the Institutional Review Board of the University of California, San Francisco.
For this analysis, interviews were matched with a corresponding partner interview on the same day or closest date within a 3 week period. Matched interviews occurring more than 7 days apart were excluded from the analysis. Responses to risk behavior questions on the matched interviews were compared. In the interview, we asked about partnership characteristics and prior month injecting and sexual risk behaviors within the partnerships. The participants reported the duration of acquaintance and duration injecting together at the baseline interview. At baseline and at each monthly interview participants were asked whether they had cohabitated with the partner for at least 1 night and the number of days cohabitating. Injecting behaviors in the prior month were elicited for each member of the dyad and included the number of days the participant had injected with the partner, injecting with the partner’s previously used needle, preparing drugs with one’s partnerin the same cooker, backloading (dividing dissolved drug by using one syringe to squirt drug solution into the back of other syringes). We also asked whether injection partners did a rinse (injected the residue from the other partner’s cotton or cooker), and whether the participant was injected by the partner. Injection behaviors measured on a Likert scale were examined first as continuous and then dichotomized into “Always/usually” vs. “Sometimes/Rarely/Never”. Participants were asked whether they engaged in vaginal or anal sex with the injection partner in the prior month and the frequency of condom use with that partner. Condom use frequency was dichotomized into always vs. not always used.
We examined injection risk to the HCV negative participants, as reported by both partners. For example, the HCV negative partner’s response to “How many times did you inject with a needle that ‘partner’ had already used?” was compared to the HCV positive partner’s response to “How many times did ‘partner’ inject with a needle that you had already used?” and vice versa. We called this a directional risk comparison. We also compared the reporting of engaging in vaginal or anal sex in the past month and the frequency of condom use within injection partnerships that were also sexual partnerships.
We assessed concordance at baseline and follow-up visits within the first 6 months. Differences in concordance by frequency of injecting together and partnership type were compared. Agreement between partners was assessed through the percent agreement, the concordance correlation coefficient for repeated measures (CCC; Carrasco et al., 2013) and the prevalence and bias adjusted kappa statistic (PABAK; Byrt et al., 1993; Cunningham, 2009). Both the percent agreement and PABAK were limited to categorical variables. The CCC is a measure of the strength of agreement computed from an appropriate specification of the intra-class correlation coefficient from a variance components linear mixed model. For categorical measures it can be comparable to a repeated measures version of kappa (King et al., 2007). PABAK is a measure of agreement that assumes a 50% prevalence of the condition and absence of any bias. By adjusting the prevalence to 50%, PABAK is preferable to the kappa statistic (K) in situations where prevalence of the condition is not distributed equally (Chen et al., 2009; Cicchetti and Feinstein, 1990; Feinstein and Cicchetti, 1990). We chose to report the PABAK because many of our dichotomous outcomes of interest had considerably less than 50% prevalence, and the CCC because it handles repeated measures and can measure concordance for both continuous and dichotomous outcomes.
We employed bootstrapping methods to examine the correlation induced by individuals enrolled in multiple partnerships. Statistical analyses were performed using Stata 11.2 (College Station, TX, USA) and SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
3. Results
From May, 2006 to December, 2013,120 potential partnerships were identified from the UFO cohort and screened for eligibility. Of those, 72 (60%) were eligible for and enrolled into the Partner Study. Among those that were not eligible, 27% were excluded due to HCV seroconcordance, and 13% were excluded because they did not inject together at least 5 times in the past 30 days. The 72 partnerships consisted of 92 unique individuals and contributed 402 interviews (201 time-linked pairs). Of the 201 pairs of interviews included in the analysis, 69% were conducted on the same day, and 31% between 1 and 7 days apart. Forty-one pairs of interviews were excluded from the analysis because the interviews were administered more than 7 days apart.
Participants had a median age of 26, (Interquartile Range (IQR): 23, 28) and median years injecting of 7.0, (IQR: 3.0, 10.6). Over two-thirds (67%) were members of 1 partnership, 17% were members of 2 partnerships, 10% were members of 3 partnerships, and 5% were a member of either 4, 5, or 6 partnerships.
At enrollment, injection partners reported knowing each other for a median of 12 months, (IQR: 5–24) and injecting together for 6 months (IQR: 2–12). Thirty-eight percent of the injecting partnerships were also sexual partnerships while 62% were solely injecting partnerships. Sixty-three percent were female-male and 32% were male-male partnerships. HCV RNA negative partners were a median of 3 years younger than their HCV positive counterpart. Partnerships contributed a median of 3 data points to the analysis (IQR: 1–6). Of the 72 partnerships enrolled at baseline, only 13 (18%) remained in the study and were active injecting partners at 6 months (Fig. 1).
Fig. 1.
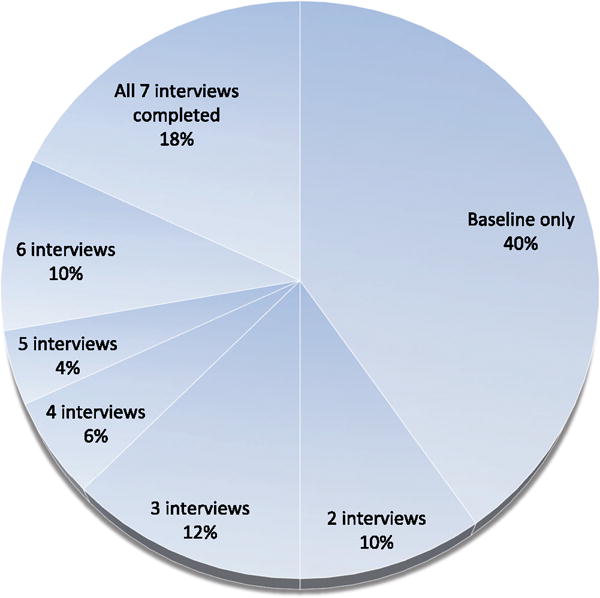
Number of repeated measures obtained from each partnership over 6 months as a proportion of total partnerships (N = 72 partnerships).
At baseline, partnerships reported injecting together frequently, the HCV negative partner reporting a median of 15 (IQR: 4, 28.5) days per month. Fifteen percent of HCV negative partners reported receptive needle sharing and 28% used a contaminated cooker with their partner. Nearly half pooled money with their partner to buy drugs (47%) and 56% used a syringe backloaded by their partner. Over one-third (38%) had sexual intercourse with their partner and among those, almost all (92%) reported unprotected sex. Corresponding reports from the HCV positive partner are found in Table 1.
Table 1.
Partnership characteristics and injection and sex behaviors in the past month within partnerships at baseline interview (n = 72).
| Partnership characteristic | HCV− partner n (%)/median (IQR) | HCV+ partner n (%)/median (IQR) |
|---|---|---|
| Number of months has known partner | 12 (5–24) | 12 (5.5–36) |
| Number of months injected with partner | 6 (2–12) | 6 (2–18) |
| Live with partner | 56 (77.8) | 51 (72.9) |
| Number of days cohabitation (if live togethera) | 15 (4–28.5) | 15 (5–28) |
| Stable housing (if live togethera) | 11 (20.0) | 10 (19.2) |
| Number of days injected together | 15 (8–23) | 14 (7–30) |
| Number of times injected together per day | 2 (1.5–3) | 2 (2–3.5) |
| Number of other people partner injects with | 3 (2–5) | 3 (1–9) |
| Always pool money to buy drugs | 34 (47.2) | 36 (50.7) |
| Used a contaminated cooker | 19 (27.5) | 26 (38.2) |
| Used a syringe backloaded by partner | 40 (56.3) | 46 (64.8) |
| Injected partner’s rinse | 28 (38.9) | 36 (51.4) |
| Injected partner (always or usually) | 5 (6.9) | 14 (20.0) |
| Was injected by partner (always or usually) | 11 (15.3) | 3 (4.2) |
| Injected with a needle partner already used | 10 (14.5) | 21 (30.4) |
| Partner injected with a needle you already used | 18 (26.1) | 11 (16.9) |
| Vaginal or anal sex with partner | 27 (37.5) | 28 (39.4) |
N for living together = 56 for HCV− partners and 51 for HCV+ partners.
In Table 2, we report the concordance correlation coefficient (CCC) and prevalence bias adjusted kappa (PABAK) for all matched interviews within the first six months of enrollment. We found almost perfect concordance for both the duration of acquaintanceship (CCC = 0.95) and number of months partners injected together (CCC = 0.97).
Table 2.
Concordance of reported partnership characteristics, injection behaviors, and sexual and condom use behaviors within injection partnerships in the past month (linked-pairs analysis, n = 402).
| N | Percentage agreementb | Concordance correlation coefficient | 95% CI | PABAKa | |
|---|---|---|---|---|---|
| Relationship characteristic | |||||
| Number of months has known partner | 402 | 0.95 | 0.74–0.99 | ||
| Number of months injected with partner | 402 | 0.97 | 0.32–1.00 | ||
| Live with partner | 398 | 81.7 | 0.54 | 0.41–0.66 | 0.63 |
| Number of days cohabitation (if live with) | 287 | 0.82 | 0.74–0.87 | ||
| Stable housing (if live with) | 288 | 88.0 | 0.63 | 0.49–0.75 | 0.76 |
| Injection behavior (bi-directional) | |||||
| Number of days injected together | 399 | 0.64 | 0.53–0.73 | ||
| Number of times injected together per day | 398 | 0.11 | 0.01–0.21 | ||
| How often pooled money to buy drugs | 401 | 70.0 | 0.37 | 0.22–0.51 | 0.40 |
| How often shared injecting equipment | 399 | 67.7 | 0.35 | 0.18–0.49 | 0.35 |
| Injection behavior (risk direction HCV+ to HCV− partner) | |||||
| Used a contaminated cooker | 387 | 67.9 | 0.23 | 0.06–0.39 | 0.36 |
| Used a syringe backloaded by partner | 397 | 66.7 | 0.22 | 0.07–0.35 | 0.33 |
| Injected partner’s rinse | 388 | 65.0 | 0.41 | 0.26–0.54 | 0.30 |
| Was injected by partner | 399 | 97.0 | 0.73 | 0.63–0.80 | 0.94 |
| Injected with a needle partner already used (y/n) | 385 | 71.7 | 0.22 | 0.04–0.38 | 0.43 |
| Number of times injected with a needle partner already used | 385 | 0.25 | 0.03–0.45 | ||
| Sexual and condom use behavior | |||||
| Had sex with partner | 399 | 96.4 | 0.90 | 0.86–0.93 | 0.93 |
| Frequency of condom use | 179 | 94.1 | 0.63 | 0.40–0.79 | 0.88 |
PABAK: Prevalence and bias adjusted kappa.
Percentage agreement and PABAK were only calculated for categorical variables.
We found moderate concordance for number of days injecting together in the past month (CCC = 0.64) but poor concordance on average number of times injected together on a typical day (CCC = 0.11). Concordance on how often pooled money to buy drugs and how often shared injecting equipment, were both relatively low (CCC = 0.37, PABAK = 0.40; CCC = 0.35, PABAK = 0.35) respectively.
In examining concordance of injection risk behaviors in the direction of HCV+ to the HCV− partner we found low concordance on most measures including using a contaminated cooker (CCC = 0.23; PABAK = 0.36), using a syringe backloaded by the partner (CCC = 0.22; PABAK = 0.33), and receptive syringe sharing (CCC = 0.22; PABAK= 0.43). Concordance was moderate to substantial for whether or not the HCV− partner was injected by the HCV+ partner (CCC = 0.73; PABAK = 0.94).
Concordance for reported sexual risk behaviors was higher than for injecting risk. We found excellent concordance for any sexual intercourse in the past month (CCC = 0.90; PABAK = 0.93) and agreement was moderate to substantial for frequency of condom use (CCC = 0.63; PABAK = 0.88).
We found higher concordance of injection risk behaviors among partners who had injected together at least 20 days in the past month (Table 3). Compared to partners who injected together less than 20 days in the past month, those who injected together at least 20 days had significantly higher concordance for average number of times injected together per day, how often pooled money to buy drugs, how often shared injecting equipment, and receptive syringe sharing. We found no difference in concordance levels by partnership type.
Table 3.
Concordance of reported partnership characteristics, injection behaviors, and sexual and condom use behaviors within injection partnerships in the past month stratified by partnership type and injection frequency (linked-pairs analysis, n = 402).
| Frequency of Injecting together in the past month
|
||||||
|---|---|---|---|---|---|---|
| <20 days
|
20 or more days
|
|||||
| Concordance correlation coefficient | 95% CI | PABAKa | Concordance correlation coefficient | 95% CI | PABAKa | |
| Relationship characteristic | ||||||
| Live with partner | 0.46 | 0.26–0.62 | 0.52 | 0.80 | 0.64–0.89 | 0.76 |
| Number of days cohabitation (if live with) | 0.75 | 0.54–0.87 | 0.73 | 0.54–0.85 | ||
| Stable housing (if live with) | 0.52 | 0.18–0.74 | 0.41 | 0.66 | 0.48–0.79 | 0.93 |
| Injection behavior (bi-directional) | ||||||
| Number of days injected together | 0.18 | −0.08 to 0.41 | 0.74 | 0.44 | 0.20–0.62 | 0.77 |
| Number of times injected together per day | 0.06 | −0.20 to 0.31 | 0.96 | 0.94–0.98 | ||
| How often pooled money to buy drugs | 0.24 | 0.05–0.40 | 0.11 | 0.70 | 0.50–0.83 | 0.62 |
| How often shared injecting equipment | 0.25 | 0.01–0.47 | 0.25 | 0.65 | 0.46–0.78 | 0.47 |
| Injection behavior (risk direction HCV+ to HCV− partner) | ||||||
| Used a contaminated cooker | 0.33 | 0.10–0.53 | 0.41 | 0.43 | 0.15–0.65 | 0.30 |
| Used a syringe backloaded by partner | 0.11 | −0.09 to 0.31 | 0.33 | 0.40 | 0.15–0.60 | 0.33 |
| Injected partner’s rinse | 0.18 | −0.07 to 0.41 | 0.09 | 0.51 | 0.25–0.70 | 0.53 |
| Was injected by partner | 0.64 | 0.46–0.77 | 0.92 | 0.68 | 0.48–0.81 | 0.96 |
| Injected with a needle partner already used (y/n) | 0.00 | 0.00–0.00 | 0.42 | 0.42 | 0.15–0.64 | 0.45 |
| Number of times injected with a needle partner already used | 0.05 | −0.09 to 0.19 | 0.26 | −0.06 to 0.53 | ||
| Sexual and condom use behavior | ||||||
| Had sex with partner | 0.88 | 0.81–0.92 | 0.90 | 0.90 | 0.83–0.94 | 0.90 |
| Frequency of condom use | 0.50 | −0.02 to 0.80 | 0.92 | 0.77 | 0.59–0.87 | 0.86 |
| Partnership type
|
||||||
|---|---|---|---|---|---|---|
| Injection only
|
Injection and sex
|
|||||
| Concordance correlation coefficient | 95% CI | PABAKa | Concordance correlation coefficient | 95% CI | PABAKa | |
| Relationship characteristic | ||||||
| Live with partner | 0.00 | −0.35 to 0.35 | 0.41 | 0.35 | 0.15–0.53 | 0.93 |
| Number of days cohabitation (if live with) | 0.83 | 0.73–0.90 | 0.66 | 0.22–0.88 | ||
| Stable housing (if live with) | 0.68 | 0.50–0.80 | 0.69 | 0.75 | 0.55–0.87 | 0.75 |
| Injection behavior (bi-directional) | ||||||
| Number of days injected together | 0.66 | 0.48–0.79 | 0.52 | 0.34–0.66 | ||
| Number of times injected together per day | 0.05 | −0.05 to 0.14 | 0.07 | −0.03 to 0.18 | ||
| How often pooled money to buy drugs | 0.25 | −0.05 to 0.51 | 0.33 | 0.32 | 0.12–0.49 | 0.50 |
| How often shared injecting equipment | 0.43 | 0.19–0.62 | 0.58 | 0.32 | 0.13–0.53 | 0.40 |
| Injection behavior (risk direction HCV+ to HCV− partner) | ||||||
| Used a contaminated cooker | 0.23 | −0.02 to 0.46 | 0.39 | 0.16 | −0.07 to 0.37 | 0.31 |
| Used a syringe backloaded by partner | 0.37 | 0.12–0.57 | 0.30 | 0.12 | −0.07 to 0.30 | 0.38 |
| Injected partner’s rinse | 0.42 | 0.18–0.61 | 0.14 | 0.32 | 0.09–0.51 | 0.47 |
| Was injected by partner | 0.77 | 0.61–0.87 | 0.98 | 0.66 | 0.51–0.78 | 0.89 |
| Injected with a needle partner already used (y/n) | 0.33 | 0.08–0.55 | 0.49 | 0.02 | −0.22 to 0.26 | 0.37 |
| Number of times injected with a needle partner already used | 0.59 | 0.28–0.79 | 0.11 | −0.15 to 0.36 | ||
PABAK: Prevalence and bias adjusted kappa. PABAK was only calculated for categorical variables.
Bootstrapping analyses indicated the correlation due to individuals enrolled in multiple partnerships did not influence our concordance estimates, as the results were qualitatively the same.
4. Discussion
In our study of reporting concordance in the injecting partnerships of young IDU, agreement was highest for duration of acquaintance and injection relationship, sexual intercourse and number of days of cohabitation; and lowest for shared injection risk behaviors such as receptive syringe sharing and sharing of contaminated drug preparation equipment. Levels of agreement varied considerably, ranging from fair to almost perfect. Qualitatively, the PABAK and the CCC were close but for several outcomes, the PABAK was higher due to the adjustments made to handle unevenly distributed outcomes. Agreement was higher for injecting partnerships who injected together more days in the past month. The results suggest that young IDU in injecting partnerships, while agreeing on the general relationship context (duration of acquaintance, cohabitation and sexual activity) have a greater degree of difference in terms of the ‘content’; specifically concurrent injecting behaviors.
The concordance of risk behavior reporting in the past month during the first 6 months of follow up was consistent with prior studies of risk behavior concordance among drug users. Among dyads recruited as part of a drug and sexual network study in New York City, NY, (Bell et al., 2000) concordance was higher for partnership characteristics such as partnership type and partnership closeness. Lower concordance was found for frequency of drug use and sexual behaviors occurring within the partnership. In another study of injection dyads in New York City, NY concordance of reports on injection behavior were low (slight on the K index) while sexual behavior was higher (fair to almost perfect agreement; Goldstein et al., 1995). Contrasting with concordance levels found in our study, in a study of opiate users in Sydney, (Darke et al., 1992) concordance of injection behaviors was higher than we found (moderate on the K index), whereas sexual behavior concordance was consistent with our findings, with substantial agreement on the K index.
In prior studies of concordance that were not restricted to IDUs, our findings are consistent with higher concordance on partnership characteristics and lower concordance on specific behaviors. In studies of heterosexual couples in the United States, concordance was moderate to substantial for relationship characteristics (Harvey et al., 2004; Stoner et al., 2003). Concordance on sexual behaviors was mixed, ranging from slight in Stoner et al. and moderate in Harvey et al. And in one other study on heterosexual couples in New York City, concordance on drug and alcohol use during sex was poor to fair (Witte et al., 2007).
Several factors may contribute to low concordance. Imprecise time interval matching has been suggested as a factor in discordant responses (Bell et al., 2000). In that study, in sexual and drug injection partners lower concordance was found for 30-day and 6-month recall when interviews were conducted at intervals greater than 5 days apart. In our study, we sought to minimize this potential effect by limiting the reporting period to 30 days and restricting the analysis to pairs of interviews conducted seven or fewer days apart. Another source of disagreement may be differing interpretation of questions about injection behaviors, such that one partner’s perception of risk behavior may differ from the other. For example, survey questions about sharing contaminated injection equipment are actually two-part questions (1) did the equipment sharing occur and if so (2) was there anytime the other partner’s dirty needle was used in the cooker before the respondent used it. Precision may be improved by separating two-part questions into separate parts. Additionally, concordance of injection frequency differed greatly for two aspects of frequency: (1) number of days injected together in the past month (CCC = 0.64) and (2) average number of times per day (CCC = 0.11). This suggests that a more exacting question, such as, number of days in past month, will elicit a more precise answer. The respondent is not required to perform a mental calculation to yield an ‘average’ number of times. Precision of responses to these types of questions could be improved by asking about a specific episode such as the last injection episode, i.e., “How many times did you inject the last day you injected together?” Moreover, studies examining reliability of recall for sexual and drug use behaviors support the use of shorter recall periods for measures requiring enumeration of episodes or reporting on more specific behaviors (Jaccard et al, 2004; Martin et al., 1998; McFarlane and St Lawrence, 1999; Napper et al., 2010). Our finding of higher concordance among partnerships who injected together at least 20 days in the past month suggests that concordant reporting increases when the behaviors of interest occur more frequently and perhaps more recently.
A unique aspect of this study was the ability to explore reporting concordance within HCV discordant partnerships, as differences in risk behavior disclosure could be attributed to knowledge of one’s own HCV status and/or knowledge of their partner’s HCV status. Although this study did not evaluate participants’ knowledge or perception of their partner’s status, it has been reported that participants who know their own HCV status are more likely to know their partner’s HCV status (Kim and Page, 2013; Smith et al, 2013).
This study was subject to several limitations. The sample size was modest, thus limiting our ability to detect differences. In addition, our results may not be generalizable to the larger population of injection partnerships as our eligibility requirements excluded injection partners who did not inject together at least five times in the past month and excluded partnerships that were HCV concordant. Finally, as has been previously reported in multiple studies, self-reported risk may be underreported in accordance with the level of stigma associated with the risk behavior (Mirzazadeh et al., 2014; Zenilman et al., 1995). Our finding of low concordance on measures of injection risk behavior could be a result of the sensitive nature of the information being elicited. Respondents may be unwilling to disclose sensitive information to interviewers about injection practices that are associated with transmission risk. If the underreporting is differential by one versus the other partner, it will impact concordance. To minimize the potential reporting bias, interviewers were trained to administer questions in a neutral tone and not to react to responses during the interview, leaving risk reduction counseling to occur after the completion of the behavioral interview.
Given the high risk of HCV among injectors, HCV’s parenteral mode of transmission, and the fact that young IDUs often inject with others, dyadic level data provides an opportunity to go beyond traditional individual-level self-reported data, and examine risk contextually. Assessing the relative accuracy of self-reported risk in the relationship context provides a more ‘dimensional’ view or picture of transmission risk. Such information could be key for the formulation of prevention messages and risk reduction strategies that might be delivered within a social context. For example, interventions to help injectors negotiate safe needle and equipment use within partnerships could have more impact than traditional individualized risk-reduction strategies. This information also provides the research and therapeutic community with much needed measures of reliability regarding data collected on partner-related risk behaviors. In conclusion, our findings underscore the challenge of obtaining accurate reports of risk when eliciting data on sensitive, stigmatized, or complex behaviors and draw attention to the importance of quality measures to assess such behaviors. Given the challenges inherent in observational research we recommend allowing adequate time to pre-test measures for comprehension, examining potential reporting biases on sensitive questions by comparing interviewer-administered to self-administered instruments, and where available, validating reporting of partnership-specific risk behaviors using phylogenetic methods to document transmission events.
Acknowledgments
The authors would like to thank the UFO Study Field Staff for their time and dedication in conducting the study.
Role of funding source: Funding for this study was provided by Institutes of Health grants (R01 DA016017 andK24 AA022586); the NIH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Contributors
Authorship credit is as follows: Jennifer Evans made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data and drafted the article; Judith Hahn made substantial contributions to conception and design and critically reviewed and revised the article; Meghan Morris, Michelle Yu, and Kimberly Page contributed to interpretation of the data and critically reviewed the article. All authors approved the final version of the manuscript.
Conflict of interest
No conflict declared.
References
- Bell DC, Montoya ID, Atkinson JS. Partner concordance in reports of joint risk behaviors. J Acquir Immune Defic Syndr. 2000;25:173–181. doi: 10.1097/00042560-200010010-00012. [DOI] [PubMed] [Google Scholar]
- Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol. 1993;46:423–429. doi: 10.1016/0895-4356(93)90018-v. [DOI] [PubMed] [Google Scholar]
- Carrasco JL, Phillips BR, Puig-Martinez J, King TS, Chinchilli VM. Estimation of the concordance correlation coefficient for repeated measures using SAS and R. Comput. Methods Programs Biomed. 2013;109:293–304. doi: 10.1016/j.cmpb.2012.09.002. [DOI] [PubMed] [Google Scholar]
- Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108:339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- Chen G, Faris P, Hemmelgarn B, Walker RL, Quan H. Measuring agreement of administrative data with chart data using prevalence unadjusted and adjusted kappa. BMC Med Res Methodol. 2009;9:5. doi: 10.1186/1471-2288-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti DV, Feinstein AR. High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. 1990;43:551–558. doi: 10.1016/0895-4356(90)90159-m. [DOI] [PubMed] [Google Scholar]
- Cunningham M. More Than Just the Kappa Coefficient: A Program to Fully Characterize Inter-Rater Reliability between Two Raters Proceedings of the SAS® Global Forum 2009 Conference; Rockville, MD: SAS Institute Inc; 2009. [Google Scholar]
- Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. discussion 267–258. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W, Wodak A, Heather N, Ward J. Development and validation of a multi-dimensional instrument for assessing outcome of treatment among opiate users: the Opiate Treatment Index. Br J Addict. 1992;87:733–742. doi: 10.1111/j.1360-0443.1992.tb02719.x. [DOI] [PubMed] [Google Scholar]
- Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43:543–549. doi: 10.1016/0895-4356(90)90158-l. [DOI] [PubMed] [Google Scholar]
- Goldstein MF, Friedman SR, Neaigus A, Jose B, Ildefonso G, Curtis R. Self-reports of HIV risk behavior by injecting drug users: are they reliable? Addiction. 1995;90:1097–1104. doi: 10.1046/j.1360-0443.1995.90810978.x. [DOI] [PubMed] [Google Scholar]
- Hageman KM, Karita E, Kayitenkore K, Bayingana R, van der Straten A, Stephenson R, Conkling M, Tichacek A, Mwananyanda L, Kilembe W, Haworth A, Chomba E, Allen SA. What the better half is thinking: a comparison of men’s and women’s responses and agreement between spouses regarding reported sexual and reproductive behaviors in Rwanda. Psychol Res Behav Manag. 2009;2:47–58. doi: 10.2147/prbm.s4910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, Evans JL, Davidson PJ, Lum PJ, Page K. Hepatitis C virus risk behaviors within the partnerships of young injecting drug users. Addiction. 2010;105:1254–1264. doi: 10.1111/j.1360-0443.2010.02949.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, Page-Shafer K, Lum PJ, Bourgois P, Stein E, Evans JL, Busch MP, Tobler LH, Phelps B, Moss AR. Hepatitis C virus seroconversion among young injection drug users: relationships and risks. J Infect Dis. 2002;186:1558–1564. doi: 10.1086/345554. [DOI] [PubMed] [Google Scholar]
- Harvey SM, Bird ST, Henderson JT, Beckman LJ, Huszti HC. He said, she said: concordance between sexual partners. Sex Transm Dis. 2004;31:185–191. doi: 10.1097/01.olq.0000114943.03419.c4. [DOI] [PubMed] [Google Scholar]
- Helleringer S, Kohler HP, Kalilani-Phiri L, Mkandawire J, Armbruster B. The reliability of sexual partnership histories: implications for the measurement of partnership concurrency during surveys. AIDS. 2011;25:503–511. doi: 10.1097/QAD.0b013e3283434485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaccard J, McDonald R, Wan CK, Guilamo-Ramos V, Dittus P, Quinlan S. Recalling sexual partners: the accuracy of self-reports. J Health Psychol. 2004;9:699–712. doi: 10.1177/1359105304045354. [DOI] [PubMed] [Google Scholar]
- Kim AY, Page K. Hepatitis C virus serosorting in people who inject drugs: sorting out the details. J Infect Dis. 2013;208:1929–1931. doi: 10.1093/infdis/jit526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King TS, Chinchilli VM, Wang KL, Carrasco JL. A class of repeated measures concordance correlation coefficients. J Biopharm Stat. 2007;17:653–672. doi: 10.1080/10543400701329455. [DOI] [PubMed] [Google Scholar]
- Koester S, Glanz J, Baron A. Drug sharing among heroin networks: implications for HIV and hepatitis B and C prevention. AIDS Behav. 2005;9:27–39. doi: 10.1007/s10461-005-1679-y. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Vlahov D, Anthony JC. Socially desirable responding and self-reported HIV infection risk behaviors among intravenous drug users. Addiction. 1993;88:517–526. doi: 10.1111/j.1360-0443.1993.tb02058.x. [DOI] [PubMed] [Google Scholar]
- Macaluso M, Lawson L, Akers R, Valappil T, Hammond K, Blackwell R, Hortin G. Prostate-specific antigen in vaginal fluid as a biologic marker of condom failure. Contraception. 1999;59:195–201. doi: 10.1016/s0010-7824(99)00013-x. [DOI] [PubMed] [Google Scholar]
- Martin GW, Pearlman S, Li S. The test-retest reliability of the frequency of multiple drug use in young drug users entering treatment. J Subst Abuse. 1998;10:275–290. doi: 10.1016/s0899-3289(99)00004-8. [DOI] [PubMed] [Google Scholar]
- McFarlane M, St Lawrence JS. Adolescents’ recall of sexual behavior: consistency of self-report and effect of variations in recall duration. J Adolesc Health. 1999;25:199–206. doi: 10.1016/s1054-139x(98)00156-6. [DOI] [PubMed] [Google Scholar]
- McMahon JM, Tortu S, Torres L, Pouget ER, Hamid R. Recruitment of heterosexual couples in public health research: a study protocol. BMC Med Res Methodol. 2003;3:24. doi: 10.1186/1471-2288-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirzazadeh A, Nedjat S, Navadeh S, Haghdoost A, Mansournia MA, McFarland W, Mohammad K. HIV and related risk behaviors among female sex workers in Iran: bias-adjusted estimates from the 2010 National Bio-Behavoral Survey. AIDS Behav. 2014;18(Suppl 1):19–24. doi: 10.1007/s10461-013-0548-3. [DOI] [PubMed] [Google Scholar]
- Napper LE, Fisher DG, Reynolds GL, Johnson ME. HIV risk behavior self-report reliability at different recall periods. AIDS Behav. 2010;14:152–161. doi: 10.1007/s10461-009-9575-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page K, Hahn JA, Evans J, Shiboski S, Lum P, Delwart E, Tobler L, Andrews W, Avanesyan L, Cooper S, Busch MP. Acute hepatitis C virus infection in young adult injection drug users: a prospective study of incident infection, resolution, and reinfection. J Infect Dis. 2009;200:1216–1226. doi: 10.1086/605947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BD, Jewett A, Burt RD, Zibbell JE, Yartel AK, DiNenno E. To share or not to share? Serosorting by hepatitis C status in the sharing of drug injection equipment among NHBS-IDU2 participants. J Infect Dis. 2013;208:1934–1942. doi: 10.1093/infdis/jit520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimson GV, Des Jarlais D, Ball AL, World Health Organization . Drug Injecting and HIV Infection: Global Dimensions and Local Responses. UCL Press; London/Bristol, PA: 1998. [Google Scholar]
- Stoner BP, Whittington WL, Aral SO, Hughes JP, Handsfield HH, Holmes KK. Avoiding risky sex partners: perception of partners’ risks v partners’ self reported risks. Sex Transm Infect. 2003;79:197–201. doi: 10.1136/sti.79.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte SS, El-Bassel N, Gilbert L, Wu E, Chang M. Predictors of discordant reports of sexual and HIV/sexually transmitted infection risk behaviors among heterosexual couples. Sex Transm Dis. 2007;34:302–308. doi: 10.1097/01.olq.0000240288.90846.6a. [DOI] [PubMed] [Google Scholar]
- Yamazaki M, Strobino D, Ellen J. Concordance in perceived partner types and unprotected sex among couples of adolescents and young adults: analysis of reciprocally nominated heterosexual dyads. Sex Transm Infect. 2010;86:141–147. doi: 10.1136/sti.2009.037754. [DOI] [PubMed] [Google Scholar]
- Zenilman JM, Weisman CS, Rompalo AM, Ellish N, Upchurch DM, Hook EW, 3rd, Celentano D. Condom use to prevent incident STDs: the validity of self-reported condom use. Sex Transm Dis. 1995;22:15–21. doi: 10.1097/00007435-199501000-00003. [DOI] [PubMed] [Google Scholar]


