Abstract
To investigate women’s attachment style in relation to risk for pregnancy-specific distress and perinatal depression. During the 2nd trimester, 186 women were evaluated for Axis I psychiatric disorders. In the 3rd trimester they self-reported: attachment style, pregnancy experience, current life stress, and symptoms of depression and anxiety. At 4 months post partum, a sub-sample of them (n=56) repeated the self-report questionnaires. Wariness of attachments (high on fear dimension) was associated with greater ‘hassles’ compared to ‘uplifts’ in the assessment of pregnancy (r=0.31, p≤0.001) while attachment security was negatively related to this ratio (r=−0.31, p≤0.001). Healthy women, versus women with a psychiatric diagnosis, scored higher on security (t=(150) −3.47, p≤0.001) and lower on attachment fear (t=(150) −2.32, p≤0.05). Using multiple regression models, there was a significant main effect of fearful attachment style on prenatal depressive symptoms (ß=1.7, p≤0.05), and of fearful and secure attachment styles for postpartum depression (ß=−2.88, p≤0.05, ß=−3.78, p≤0.05, respectively), even in the context of other known risk factors (in the two models, F(8, 106)=29.33, p≤0.0001, F(3, 33)=10.85, p≤0.0001, respectively). A hierarchical regression showed that attachment security uniquely contributed to the risk for postpartum depression, beyond depression during pregnancy (R2 change from 0.25 to 0.35). An approach to perinatal psychiatric disorders that includes psychological factors such as attachment could improve screening, and provide pregnant women with specifically-tailored psychosocial interventions focused on modifying attachment schemas.
Keywords: Perinatal depression, Postpartum depression, Attachment style
Introduction
Depression is relatively common during the perinatal period (Gavin et al. 2005; Ross and McLean 2006). Approximately 8.5–11% of women experience either a major or minor depression during pregnancy (Gaynes et al. 2005). Nearly 20% of women have a minor or major depression in the first 3 months following delivery (Gavin et al. 2005). This morbidity in the mother is associated with children’s development of emotion regulation difficulties, conduct problems, and other signs of risk for future psychopathology (Newport et al. 2002; Cooper et al. 1999; Downey and Coyne 1990; Lyons-Ruth et al. 2000; Sinclair and Murray 1998; Murray et al. 1996; Field 1995, 1998; Hart et al. 2003; Weissman et al. 1984; Rosenbaum et al. 1988; Warren et al. 2003). Moreover, women’s psychiatric symptoms appear to affect children even before birth. Stress, anxiety, and depression during pregnancy are associated with alterations in fetal and infant neurobehavioral development that have long-term implications for the child’s future health (Field et al. 2004; O’Connor et al. 2002, 2005; Monk et al. 2000, 2004; Sandman et al. 1999; Van den Bergh and Marcoen 2004; Werner et al. 2007; Bergman et al. 2007).
This significant perinatal psychiatric morbidity for mother, and infant, necessitates improved intervention. In particular, treatment during pregnancy can be ameliorative as well as preventative since both prenatal depression and anxiety predict postpartum depression (Austin et al. 2006; Heron et al. 2004; O’Hara and Gorman 2004; Beck 2001). Although many studies indicate that one of the most reliable forms of psychiatric intervention, pharmacology, is safe for the fetus (Alwan et al. 2007; Louik et al. 2007; Way 2007), others suggest that it is associated with potential risks to healthy infant development (i.e., persistent pulmonary hypertension (Chambers et al. 2006), cardiac anomalies (Berard et al. 2007; Rooney et al. 2006), earlier birth (Oberlander et al. 2006; Suri et al. 2007), and diminished newborn pain sensitivity, which may be a marker for other effects on brain development (Oberlander et al. 2002, 2005).
Improving care for perinatal mood disorders also depends on more effective risk prediction. Risk factors for depression during pregnancy include premenstrual mood changes (Sugawara et al. 1997) a history of affective illness, marital dissatisfaction, poor social support, recent stressful events, lower education, younger age, and unwanted pregnancy (Gotlib et al. 1989; O’Hara 1986). Risk factors for postpartum depression include: previous depression, anxiety and depressive symptoms during pregnancy, stressful recent life events, lack of social support, and low self esteem (Blackmore et al. 2006; Da Costa et al. 2000; O’Hara et al. 1991). However, both specificity and sensitivity for predicting postpartum depression are poor in the current screening protocols, possibly because personality structure is largely excluded (Austin and Lumley 2003). A more fully characterized, biopsychosocial conceptualization of perinatal psychiatric disorders could improve the methods of screening and intervention for this period, and ultimately provide women with specifically-tailored psychological adjunctives and/or alternatives to pharmacological care.
Studies primarily from social psychology use a personality construct known as ‘attachment style’ to predict risk for depression (Bifulco et al. 2002b; Gerlsma and Luteijn 2000). Based on Bowlby’s (1988) work, as well as that of cognitive and interpersonal theorists (Beck et al. 1979; Brown and Harris 1978), this approach suggests that people who have an insecure attachment style, characterized by either worry about the emotional availability and support of others or by distrust or fear of closeness, attend selectively to aspects of interpersonal interactions which support their views. These cognitive schemas of relationships—which function largely outside of awareness—can engender feelings of loss and isolation and therefore predispose people to depression. Insecure schemas also influence behavior as people act in response to their distorted perceptions, inadvertently alienating others and undermining relationships, which solidifies their negative schemas and further contributes to depression.
New research applying attachment theory to perinatal psychiatric symptoms indicates that pregnant women with insecure attachment styles are at greater risk for postpartum depression (Feeney et al. 2003; McMahon et al. 2005; Simpson et al. 2003). In this research, the transition to parenthood is conceptualized as a general life stressor that activates the attachment system. When insecure schemas are predominant, this ‘world view’ and associated behavior contribute to pregnant women feeling depressed, as well as anxious, throughout the perinatal period. (Bifulco et al. 2004; Feeney et al. 2003; Meredith and Noller 2003; Simpson et al. 2003).
In our model, pregnancy is distinct from a general life stressor. Pregnancy is a life event intrinsically related to the attachment domains in women’s lives. As such, pregnancy recruits attention and orients cognitions to attachment concerns as they relate to one’s partner, family of origin, and future child. Influenced by Fraiberg’s (1995) “Ghosts in the Nursery” and contemporary social psychologists’ theories of a social-cognitive model of transference (Andersen and Chen 2002), we view the anticipation of a future child as activating self-other attachment representations, which cause shifts in affect, behavior, and motivation based on the characteristics of these representations. When a woman’s dominant attachment schema is insecure, even a healthy pregnancy may be experienced as primarily stressful because the activation of representations about relationships is associated with interpersonal dissatisfaction, low self-esteem, and negative mood. Conversely, the cognitions and behavior associated with secure attachment are emotionally protective such that the everyday challenges of a healthy pregnancy likely do not contribute to mood disturbance.
Our aims in this paper are to add to the emerging literature linking an aspect of personality—dominant attachment style—with susceptibility to perinatal depression. We seek to extend the investigation to show that attachment schemas also are related to women’s assessment of the pregnancy experience, and thereby emphasize the centrality of attachment style for overall perinatal mental health. Specifically, we hypothesize that women’s attachment styles influence, and thus are highly correlated with, their feelings about pregnancy (as largely ‘uplifting’ (i.e., associated with positive emotion) or stressful, i.e., full of ‘hassles’). We further hypothesize that attachment style will be associated with perinatal depression independent of other possible risk factors such as life stress, anxiety, a history of depression, and low socioeconomic status.
Materials and methods
Participants
Through posted announcements and signs in obstetricians’ offices, 186 pregnant women with singleton fetuses were recruited at the Columbia University Medical Center (CUMC) between 2001 and 2006 for a psychophysiology study examining women’s perinatal moods and fetal and infant neurobehavior (other results from this study have been reported elsewhere (Kaplan et al. 2007; Monk et al. 2004; Werner et al. 2007)). Women were excluded from the study if there were any maternal or fetal complications including hypertension, diabetes mellitus, a fetal structural anomaly on ultrasound, or if the women smoked. Women’s mean age was 26 (range=18–40) years. Sixty-four percent of the sample was Latina, 17% Caucasian, 13% African American and 6% others. Eighty-eight percent of women in the study had received at least a high school degree. At birth, babies’ average weight was 3,366 g (SD=495 g; range=1,815–4,335 g) and no baby was born prior to 37 weeks.1,2 Seventy–two percent of the women were living with the baby’s father and 55% were nulliparous. Because this sample was drawn from an urban hospital and included doctors and support staff as well as patients, 25% earned less than $15,000 annually and/or received public assistance while 9% earned between $100,000 and $250,000 and the top 3% earned over $250,000.
Due to marked subject attrition, only 56 subjects provided useable data during pregnancy and the follow up visit at 4 months postpartum. Subjects lost to follow up had a significantly higher Center for Epidemiological Studies-Depression Scale (CES-D) score at the 3rd trimester session (M=15.64±9.68) compared to those who returned (M=10.85±7.31; t=−3.21, p≤0.01)3. However, comparing the full sample to the subset who also returned for the 4 month follow up session there were no differences on the following demographics: maternal age, ethnicity, number of children, living with baby’s father, education, and income. This study was approved by the New York State Psychiatric Institute Institutional Review Board. Informed consent was obtained from each subject.
Antenatal psychiatric and pregnancy experience assessments
During the second trimester, subjects came to the laboratory at CUMC and underwent a psychiatric interview with a licensed psychologist using the Axis I module of the Structured Clinical Interview for DSM-IV (SCID; First et al. 1997) and also provided demographic information. Based on the assessment, women were either rated as free of any Axis I diagnoses or assigned one, and given a clinical referral, if necessary. Although it was not an exclusionary criterion, none of the women in the study took psychotropic medication during pregnancy.
In the 3rd trimester, study participants made a second trip to the laboratory for a psychophysiology session, reported elsewhere (Monk et al. 2004). Women completed five questionnaires assessing (1) current feelings of depression (CES-D; Radloff 1977), (2) reactions to the experience of pregnancy (Pregnancy Experience Scale (PES); DiPietro et al. 2004), (3) their general orientation to close (attachment) relationships (Relationship Scales Questionnaire (RSQ); Griffin and Bartholomew 1994a), (4) state anxiety (State and Trait Anxiety Inventory (STAI); Spielberger 1983) and (5) current life stress (the Perceived Stress Scale (PSS); Cohen et al. 1983).
4-month postpartum assessment
At 4 months postpartum, women and their infants returned to the laboratory and participated in an interactive session, reported elsewhere (Kaplan et al. 2007; Werner et al. 2007). During this session women again completed the CES-D, the state module of the STAI, and the PSS.
CES-D
The CES-D is a 20-item questionnaire with a possible score range from 0–60. A score of 16 or more is considered an indication of depression. The validation and use of the CES-D in community samples has been well established (Radloff 1977; Roberts 1980; Boyd et al. 1982; Weissman et al. 1978).
PES
The PES contains 41 questions and measures women’s appraisal of exposures to daily, ongoing ‘hassles’ and ‘uplifts’ specific to pregnancy (i.e., “thinking about the baby’s appearance,” “thoughts about whether the baby is normal,” “baby’s sex”). Respondents indicate on a scale of 0 (not at all) to 4 (a great deal) the degree to which the item has made them feel “unhappy, negative or upset” (scored under ‘hassle’) or “happy, positive, or uplifted” (scored under ‘uplift’). Scoring for this analysis was based on intensity values for hassles and uplifts (i.e., the sum of scores divided by the total number of questions) for hassles and uplifts, respectively, as well as on a composite score of the ratio of the frequency of hassles to the frequency of uplifts such that a higher score reflects more negative feelings. Convergent and discriminant validity of the scale has been established by comparison with other self-report data on depression and anxiety. The frequency and intensity scores on the PES have been found to be stable over the course of pregnancy, and internal scale reliability is high (Cronbach’s alpha 0.91 to 0.95; DiPietro et al. 2004).
RSQ
Based on a prototypic approach to the measurement of attachment styles (Griffin and Bartholomew 1994b), the RSQ contains 30 short statements (i.e., “I worry that I will be hurt if I allow myself to become too close to others,” “I find that others are reluctant to get as close as I would like”) that a subject rates on a five-point scale from “not at all like me” to “very like me”. Subjects are told to answer the questions about themselves in relation to their general orientation to close relationships. The scale yields scores for four attachment prototypes—secure, fearful, preoccupied and dismissing—which are derived by computing the mean of the items representing each prototype. These four attachment prototypes are conceptualized as measuring a dimension of the self in relationships as well as a dimension of the other. A ‘fearful’ style is marked by wishes for closeness in the context of a distrust and avoidance of dependency to protect against anticipated rejection related to low self worth; ‘Preoccupied’ style refers to doubt about one’s needs for emotional contact being met while there is an anxious urgency to obtain validation from others; ‘dismissive’ denotes a style oriented to rejection of the importance of interpersonal closeness and satisfaction in self-reliance. These three are characterized as insecure attachment prototypes. In contrast, the secure prototype refers to an ease with emotional closeness, interdependency, as well as with self-sufficiency. Three of the RSQ patterns—secure, preoccupied, and dismissing—are asserted to be conceptually similar to the same-named patterns generated by the Adult Attachment Interview (George et al. 1985; Griffin and Bartholomew 1994b); in addition, the secure, preoccupied, and fearful prototypes are thought to be similar to Hazen and Shaver’s (1987) secure, anxious–ambivalent, and avoidant categories, respectively (Griffin and Bartholomew 1994b). Alphas (averaged over partners with an unspecified sample) for the four scales have been found to range from 0.41 for secure to 0.70 for the dismissing scale. Though some of these alphas are low, the authors suggest that this is not a result of few items making up a prototype score, nor problems with the scales psychometrics. Instead, low internal consistency in the RSQ can reflect the fact that two orthogonal dimensions (self in relationship dimension and other in relationship dimension) are being combined (Griffin and Bartholomew 1994b). The RSQ shows fair convergent validity (ranging from 0.22 to 0.50) with interview attachment ratings and fair discriminant validity from major personality factors (Griffin and Bartholomew 1994b; though see (Kurdek 2002) for a full discussion of the RSQ’s psychometric properties in relation to other personality factors).
STAI
The state module of the STAI consists of 20 questions that measure the current experience of anxiety. Anxiety scores range from 20–80, with higher scores reflecting higher levels of anxiety. This measure has been extensively used and its validity and reliability are well established (Spielberger 1983).
PSS
The PSS is a 14-item instrument designed to measure the degree to which subjects’ appraise situations in their lives as stressful. Specifically, respondents rate the frequency of specific stressful experiences over the past month on a five-point scale from “never” to “very often”, i.e. “in the last month how often have you found that you could not cope with all the things that you had to do?” The scale has adequate reliability (alphas of 0.84, 0.85, 0.86 for three different samples (Cohen et al. 1983)) and has been found to prospectively predict psychological symptoms, physical symptoms, and health behavior even after psychopathology was factored out (Cohen 1986).
Approach to data analysis
We used Pearson Correlation Coefficients to examine associations between women’s attachment ratings and (1) feelings about their pregnancy and (2) their self-report depression scores. We used t-tests to examine the difference between women’s psychiatric diagnosis (‘H’ for healthy control or ‘DX’ for carrying a diagnosis) in relation to their ratings on the attachment assessment. To determine if attachment ratings predicted depression even in the context of other possible risk variables, some of which have been previously identified in perinatal depression research, we used Pearson Correlation Coefficients to learn which demographic and mood variables are related to perinatal depression in this sample and should be included in multiple regression models predicting prenatal and postnatal depression. Covariates were entered into the model if the univariate correlation was significant at p≤0.05. We used t-tests or analyses of variance (ANOVAs) to determine if there were differences in living with the baby’s father, having had a past depression, and ethnicity related to pre and postpartum depression and thus, if these variables also should be included in multiple regressions. Because the pregnancy rating of the intensity of hassles was more strongly correlated with CES-D scores than the intensity of uplifts (r=0.48 versus r=−0.28), we only included the hassles rating in the models. For the multiple regression analyses, we included only the fear and secure dimensions as they differentiated DX from H women. Finally, to determine if attachment ratings uniquely contribute to the prediction of postpartum depression beyond depression during pregnancy, we conducted a hierarchical regression.
Results
Psychiatric assessment
Based on the 2nd trimester SCID assessment, 78 women met diagnostic criteria for a current DSM-IV mood and/or anxiety disorder, comprising the patient (DX) group. The distribution of specific diagnoses was as follows: An anxiety disorder (n=44), major unipolar depression or dysthymia (n=11), or both (n=23). One-hundred and eight women free of Axis I pathology constituted the healthy control group (H). Descriptive statistics for women’s perinatal mood, attachment, and pregnancy ratings are listed in Table 1.4
Table 1.
Women’s mood, attachment, and pregnancy ratings
| DX |
Control |
All |
||||
|---|---|---|---|---|---|---|
| N | Mean±SD | N | Mean±SD | N | Mean±SD | |
| CES-D 3rd trimester | 61 | 19.41±9.54 | 92 | 10.22±6.79 | 153 | 13.89±9.16 |
| CES-D 4 months postpartum | 17 | 15.41±9.87 | 45 | 7.60±6.16 | 62 | 9.74±8.08 |
| State anxiety 3rd trimester | 60 | 38.23±8.85 | 94 | 30.36±8.39 | 154 | 33.43±9.37 |
| State anxiety 4 months postpartum | 20 | 33.40±10.95 | 45 | 27.80±7.90 | 65 | 29.52±9.23 |
| Perceived life stress 3rd trimester | 61 | 27.70±5.75 | 95 | 20.07±7.17 | 156 | 23.06±7.61 |
| Perceived life stress 4 months postpartum | 20 | 26.40±6.16 | 43 | 18.79±7.39 | 63 | 21.21±7.83 |
| Attachment style secure | 58 | 3.12±0.58 | 94 | 3.45±0.55 | 152 | 3.33±0.58 |
| Attachment style fearful | 58 | 2.57±0.91 | 94 | 2.24±0.81 | 152 | 2.37±0.86 |
| Attachment style preoccupied | 58 | 2.67±0.67 | 94 | 2.55±0.61 | 152 | 2.60±0.63 |
| Attachment style dismissive | 58 | 3.22±0.70 | 94 | 3.10±0.70 | 152 | 3.14±0.70 |
| Pregnancy experience uplifts frequency | 55 | 29.29±6.00 | 94 | 30.49±5.81 | 149 | 30.05±5.89 |
| Pregnancy experience hassles frequency | 53 | 18.75±8.50 | 94 | 16.27±8.64 | 147 | 17.16±8.64 |
| Pregnancy experience uplifts intensity | 55 | 1.60±0.47 | 94 | 1.75±0.48 | 149 | 1.69±0.48 |
| Pregnancy experience hassles intensity | 53 | 0.82±0.43 | 94 | 0.67±0.38 | 147 | 0.73±0.40 |
Due to subject attrition and errors in data collection, we have data from fewer subjects in session 2 (3rd trimester) compared to session 1 (2nd trimester); this is true for the postpartum session as well.
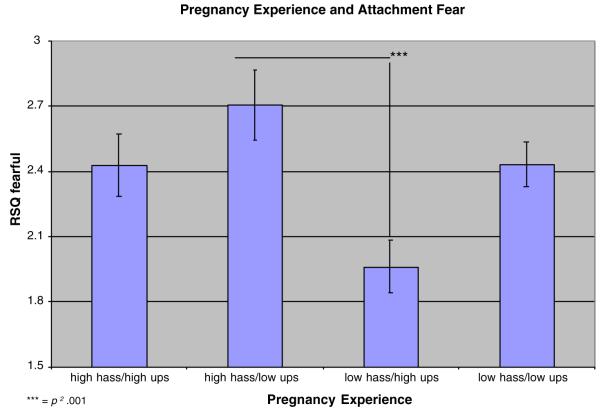
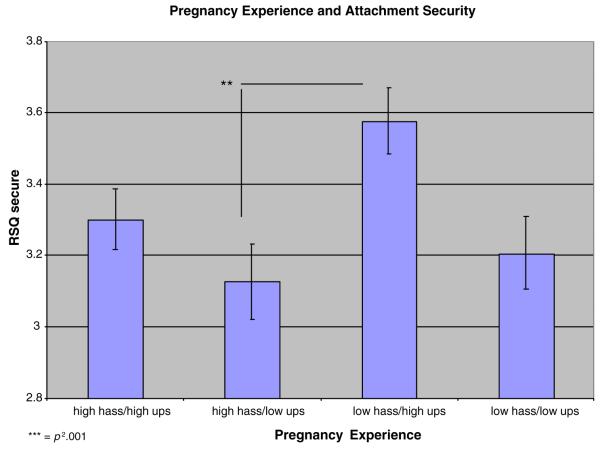
Associations between women’s attachment styles and pregnancy ratings
Women’s endorsement of a secure attachment prototype was negatively related to their intensity rating of hassles on the PES (r=−0.22, p=0.01) while their level of attachment fear was positively related to the hassles rating (r=0.24, p≤0.01). In contrast, their endorsement of a secure attachment style was positively related to the intensity of their uplifts regarding pregnancy (r=0.29, p≤0.001) and the fearful dimension of attachment was negatively related to uplifts (r=−0.25, p≤0.01). Attachment security and fear also were related to a composite score of the frequency of hassles to the frequency of uplifts (r=−0.31, p≤0.0001; r=0.31, p≤0.0001, respectively). Neither of the relationship prototypes of preoccupied or dismissive was associated with either pregnancy rating. Finally, using median splits on the PES data, we created four groups: (1) high intensity hassles/high intensity uplifts; (2) high intensity hassles/low intensity uplifts; (3) low intensity hassles/high intensity uplifts; (4) low intensity hassles/low intensity uplifts. On RSQ attachment fear and security ratings, there were significant differences between these PES groups (F (3, 135)=5.33; p≤0.001, F (3, 135)=4.37; p≤0.01, respectively; see Figs. 1 and 2). Post-hoc Tukey Studentized Range tests indicated that lower scores on attachment fear were found in the low hassles/high uplifts group versus the high hassles/low uplifts group (p≤0.01) and that women who had higher security scores tended to be in the low hassles/high uplifts group compared to the high hassles/low uplifts group (p≤0.01).
Fig. 1.
Women who rate their pregnancy experience as high on hassles, low on uplifts score higher on attachment fear compared to women who view their pregnancy as low as hassles, high on uplifts
Fig. 2.
Women who rate their pregnancy experience as low on hassles, high on uplifts, score higher on attachment security compared to those who describe their pregnancy as high on hassles, low on uplifts
Pregnant women’s attachment style and concurrent mood disturbance
Women’s security in attachment was negatively correlated with depressive symptoms during pregnancy (as assessed by the CES-D; r=−0.42, p≤0.0001) while their endorsement of attachment fear was positively associated with the CES-D scores (r=0.51, p≤0.0001). The attachment prototypes of preoccupation and dismissive also were positively associated with depressive symptoms (r=0.27, p≤0.001 and r=0.23, p≤0.001, respectively).
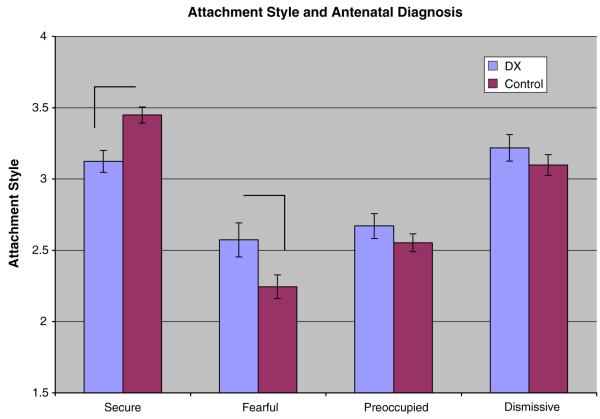
Pregnant women with a DSM-IV psychiatric diagnosis (DX group) versus those without (H) differed in their endorsements of attachment styles: Healthy control women scored higher on the security scale (t (150)=−3.47, p≤0.001) and lower on the fear dimension (t (150)=−2.32, p≤0.05); the groups did not differ on the other two attachment dimensions (see Fig. 3).
Fig. 3.
Pregnant women differ by psychiatric status in levels of attachment fear and security
To determine if ratings on the fear and secure attachment styles predict depression during pregnancy in the context of other mood and demographic factors, we used a multiple regression analysis. We first considered factors to include in the model based on results from a correlation matrix (see Table 2) and other analyses for dichotomous variables. Specifically, an ANOVA indicated that there was no significant difference in depressive symptoms during pregnancy between different ethnic groups (F (3, 144)=1.58, p=0.20) and t-tests showed no difference in symptoms between women who had and did not have a past depression (t (151)=−1.73, p≤0.08); however, women who were not living with their baby’s father scored higher on the CES-D (t (151)=2.01, p≤0.05). In the multivariate regression model (F (8, 106)=29.33, p≤0.0001; see Table 3; that included the covariates living with baby’s father, education, income, PSS, PES, STAI), the association between a fearful attachment style and depressive symptoms during pregnancy remained significant (ß=1.7, p≤0.01) as did higher life stress (ß=0.58, p≤0.0001) and a higher rating of pregnancy-specific distress (ß=4.00, p≤0.01). None of the other factors was significant.
Table 2.
Correlation matrix of demographic, mood, and attachment variables with depressive symptoms during pregnancy
| Depressive symptoms during pregnancy (CES-D) |
|
|---|---|
| Women’s age | −0.09 |
| Number of children | 0.10 |
| Education | −0.27* |
| Income | −0.23** |
| Life stress 3rd trimester | 0.74* |
| State anxiety 3rd trimester | 0.55* |
| Pregnancy experience hassles intensity | 0.48* |
p<0.01;
p<0.001
Table 3.
Multivariate regression: predictors of depressive symptoms during pregnancy (CES-D)
| Parameter | Estimatea | Standard error |
t value (df=106) |
Pr>∣t∣ |
|---|---|---|---|---|
| Intercept | −0. 75 | 4.82 | −0.16 | 0.88 |
| Not living with baby’s father |
0.11 | 1.19 | 0.09 | 0.93 |
| Living with baby’s father |
0.00 | |||
| Education | −0.27 | 0.20 | −1.36 | 0.188 |
| Income | −0.19 | 0.44 | −0.43 | 0.67 |
| Life stress 3rd trimester |
0.58 | 0.09 | 6.31 | ≤0.0001 |
| State anxiety 3rd trimester |
0.10 | 0.07 | 1.42 | 0.16 |
| Pregnancy experience hassles intensity |
3.95 | 1.44 | 2.74 | ≤0.001 |
| Attachment style fearful |
1.65 | 0.65 | 2.55 | ≤0.01 |
| Attachment style secure |
−1.38 | 0.92 | −1.50 | 0.14 |
Estimate non-standardized
Pregnant women’s attachment style and postpartum depressive symptoms
As described above, we constructed a correlation matrix (see Table 4) to determine which other risk factors for postpartum depression should be included in a multiple regression model along with ratings on attachment styles. In addition, t-tests indicated that there was no significant difference in depressive symptoms postpartum between women who had and did not have a past depression (t (60)=1.00, p=0.32) and those living and not living with the baby’s father (t (60)=0.16, p=0.87). An ANOVA indicated that there was no significant difference in depressive symptoms postpartum between different ethnic groups (F (3, 58)=1.89, p=0.14). In this multivariate regression model (F (3, 33)=10.85, p≤0.0001; see Table 5) that included women’s age, education, PSS scores at 4 months, STAI scores at 4 months, and PES ratings, the associations between fearful and secure attachment styles and postpartum depression remained significant (ß=−2.88, p≤0.05; and (ß=−3.78, p≤0.05, respectively). Life stress at 4 months postpartum, education, and depression during pregnancy also were significant factors (ß=0.31, p≤0.05, ß=−0.69, p≤0.05, ß=0.32, p≤0.05, respectively). None of the other factors was significant. Finally, to determine if attachment style assessed during pregnancy makes a unique contribution to risk for postpartum depression, and is not primarily a marker of depressed mood during pregnancy, we conducted a hierarchical regression with these variables (F (3, 46)=11.78, p≤0.001; see Table 6). As can be seen from the table, scoring high on the secure attachment prototype significantly contributed to the overall variance beyond what was accounted for by CESD scores during pregnancy (R2 change from 0.25 to 0.35), though this was not true for ratings on the attachment fear scale (R2 change from 0.25 to 0.30).
Table 4.
Correlation matrix of demographic, mood, and attachment variables with depressive symptoms postpartum
| Depressive symptoms 4 months postpartum (CES-D) |
|
|---|---|
| Women’s age | −0.26* |
| Number of children | −0.09 |
| Education | −0.31* |
| Income | −0.02 |
| Life stress 4 months postpartum | 0.69** |
| State anxiety 4 months postpartum | 0.64** |
| Pregnancy experience hassles intensity | 0.32* |
p<0.05;
p<0.001
Table 5.
Multivariate regression: predictors of depressive symptoms postpartum (CES-D)
| Parameter | Estimatea | Standard error |
t value (df=33) |
Pr>∣t∣ |
|---|---|---|---|---|
| Intercept | 14.58 | 7.77 | 1.88 | 0.07 |
| Depression during pregnancy |
0.32 | 0.16 | 2.03 | ≤0.05 |
| Women’s age | 0.23 | 0.18 | 1.29 | 0.20 |
| Education | −0.69 | 0.33 | −2.06 | ≤0.05 |
| Life stress 4 months postpartum |
0.31 | 0.13 | 2.29 | ≤0.05 |
| State anxiety 4 months postpartum |
0.25 | 0.14 | 1.81 | 0.08 |
| Pregnancy experience hassles intensity |
0.47 | 2.84 | 0.16 | 0.87 |
| Attachment style fearful | −2.88 | 1.18 | −2.44 | ≤0.05 |
| Attachment style secure | −3.78 | 1.70 | −2.22 | ≤0.05 |
Estimate non-standardized
Table 6.
Hierarchical regression: attachment styles as predictors of depressive symptoms postpartum (CES-D)
| Variable | Estimatea | Standard error |
F value |
df | Pr>F |
|---|---|---|---|---|---|
| Intercept | 32.03 | 7.98 | |||
| Depression during pregnancy |
0.49 | 0.15 | 16.19 | 1.48 | ≤0.001 |
| Attachment style fear |
−3.43 | 1.30 | 2.99 | 1.47 | =0.09 |
| Attachment style secure |
−6.33 | 1.89 | 11.19 | 1.46 | ≤0.01 |
Estimate non-standardized
Discussion
In this study, pregnant women’s attachment styles were associated with their appraisal of their pregnancy experience, as well as with their concurrent and postpartum mood. Pregnant women who were more fearful and less secure with respect to relationships reported greater pregnancy distress. This relationship style marked by fear with respect to relationships also was an independent predictor of greater depression during pregnancy, even in the context of other positive predictors such as current life stress and pregnancy-specific distress. When we tested other possible risk factors for depressed prenatal mood, such as past depression, anxiety, income, non co-habitation with a partner (as an index of social support), number of children, and education, none were associated with women’s depression during pregnancy as seen in univariate and/or multivariate models. Moreover, characteristics of attachment style assessed during pregnancy also were strong predictors of postpartum depression. Specifically, less security and less fear regarding relationships, along with depression during pregnancy, lower education, and higher life stress, were related to increased risk for postpartum depression. A hierarchical regression analysis indicated that ratings on attachment security taken during pregnancy make a unique contribution in accounting for postpartum depression, beyond the contribution from depression during pregnancy. Finally, consistent with the results, pregnant women with a frank psychiatric mood disorder, versus healthy subjects, described themselves as more fearful and less secure about relationships.
The findings lend support to our hypothesis that pregnancy is stressful primarily when women’s attachment styles are characterized by less security and more fear. Having lower security and more fear with respect to relationships was associated with judging one’s pregnancy as higher on hassles (negative affective experience) and lower on uplifts (positive affective experience). This pregnancy-specific distress was associated with depressive symptoms during pregnancy, but not postpartum. It may be, as we theorize, that pregnancy activates attachment schemas. When a woman’s dominant schemas concern fear about closeness and a lack of a sense of security in relationships, she experiences her pregnancy, and the intimate bonds associated with it, as largely stress-provoking. Perhaps it is the woman’s attachment style that undergirds her experience of pregnancy, as well as influences her risk for perinatal mood disturbance. In a related study, Hart and McMahon (2006) found that greater anxiety during pregnancy was associated with more negative attitudes about motherhood and negative cognitions towards the fetus. However, whereas these authors emphasize anxiety as having a negative impact on aspects of the pregnancy experience, we are highlighting the influence of attachment schemas on the experience of pregnancy and overall perinatal mood.
Our results are in line with other reports showing associations between attachment style and perinatal mood disorder (Bifulco et al. 2004; Feeney et al. 2003; Meredith and Noller 2003; Simpson et al. 2003), indicating that pregnant women with insecure attachments may experience negative attachment-related cognitions and engage in associated interpersonal behavior that leaves them feeling isolated and depressed. Specifically, in our study, pregnant women scoring high on attachment fear, who self-identified as “finding it difficult to depend on other people”, “worried they would be hurt if they allow themselves to become close to others”, “can’t trust others” and are “uncomfortable being close to others,” were more likely to be depressed during pregnancy.
With respect to postpartum mood, common risk factors emerged as predictors of depression, such as depression during pregnancy, lower education, and greater life stress. Even in the context of these risk factors, scores on the fear and secure attachment prototypes also contributed to predicting depression. Specifically, some of these data indicated that fear in relation to attachment is inversely associated with risk for depression postpartum, while less attachment security was associated with greater risk. That is, during the 3rd trimester, pregnant women who scored low on both fear and secure prototypes (i.e., “finding it easy to get emotionally close to others” and on being “comfortable having other people depend on me) were more likely to be depressed postpartum. Thus, the direction of the association between attachment fear and depression changed for the prediction of depression during pregnancy versus postpartum, and security becomes a significant factor, which may reflect the reduced sample size postpartum, lack of power, possible unreliability of the secure rating, and therefore unreliability of the results. In a simplified hierarchical regression, greater attachment fear did not contribute to predicting postpartum depression beyond the contributions from depression during pregnancy. Importantly, in this hierarchical model, low ratings on attachment security made a unique contribution to understanding risk for postpartum depression, suggesting that attachment security is not merely a marker for prenatal depression but provides specific information relevant to women’s postpartum mood.
If, on the other hand, the counter-intuitive finding regarding high scores on the attachment fear prototype and reduced risk for postpartum depression were to be replicated, there is a plausible interpretation. Having an orientation to attachment that emphasizes fear, particularly wariness about being emotionally hurt, could function differently during the prenatal versus postpartum period. During pregnancy, women often encounter increased social interest in them and their baby-to-be. For those who fear closeness, these experiences may sadden them by underscoring their difficulty with social interactions and interdependence. However, in the period after birth, women often find themselves more alone than anticipated, and those who do not have an attachment style dominated by fear may be more vulnerable to depression secondary to greater social isolation—the same reason those with greater fear may be protected during this postnatal period (Beck 1996; O’Hara et al. 1983). It could also be that during pregnancy, women who self-describe as fearful of relationships may be distressed anticipating the intimacy of mothering; post birth they may be relieved to learn that they can modulate the closeness to suit their interpersonal style.
These interpretations are somewhat similar to those of Bifulco et al. (2004), who found some specificity with respect to attachment styles and risk for perinatal depressions. Using an extensive interview that is then rated by trained coders, Bifulco and colleagues found that an ‘avoidant’ style of attachment was associated with depression during pregnancy. This finding could be viewed as consistent with our results regarding the fear dimension in relation to depression during pregnancy in that the avoidant category referred to women who were assessed as ‘angry dismissive’ as well as ‘withdrawn’. In the same paper, what the authors termed ‘anxious’ attachment, which referred to women who were either ‘enmeshed’ and/or ‘fearful’ with respect to attachments, was associated with depression postpartum, which would seem to conflict with our findings. However, because enmeshed and fearful styles were treated as a collapsed variable, comparison across studies for these variables is less clear. We did not find significant associations between two of the attachment prototypes, preoccupied and dismissive, with diagnosed mood disorders, and the relationships with depressed symptoms were much lower for these two attachment prototypes than for the other two. Possibly the anticipation of a dependent child partially satisfies the attachment needs of women whose dominant attachment schema is preoccupied, that is, concerned with wanting more closeness than those around her, and thus is unrelated to risk for depression. Alternatively, having a dismissive style may mark a ‘deactivation’ of attachment schemas and not be relevant to the risks for depression that stem, in part, from attachment concerns. Given the overlapping attachment constructs, and multiple methods for assessment, it is clear that more research is needed to clarify which specific dimensions of relationship templates are most salient for understanding risk for perinatal mood disorders.
Although we hypothesized that attachment style would be an independent predictor of perinatal mood disorder, we did not anticipate that consideration of this variable would result in other known risk factors, such as past affective illness, low social support (as indexed by living with a partner) and current anxiety, no longer showing predictive power. Perhaps this is a function of collinearity between attachment style and these other variables, which, could however indicate that a rigorous assessment of attachment style compared to these other factors could be a stronger, more reliable, and more parsimonious, predictor of risk for depression during pregnancy and the postpartum period.
These data suggest that an assessment of pregnant women’s personality, particularly attachment style, likely would contribute to the prediction of postpartum depression, as well as mood disturbance during pregnancy. Other reports describe the possible predictive value of considering personality variables in relation to perinatal depression (Austin and Lumley 2003), and some indicate that an assessment of the pregnant women’s relationship with her mother could be useful (Cooper et al. 1996; Boyce et al. 1991; Matthey et al. 2000)—a factor that would certainly be captured by an assessment of attachment style as these relationship templates have been shown to be largely shaped by one’s primary attachments (Fonagy et al. 1993; Sroufe 2005), and to be readily activated in adulthood by appropriate contemporary triggers (Andersen and Chen 2002). Recent data further support this conceptualization in that they show that insecure attachment mediates an association between non-optimal maternal care in childhood and persistent postpartum depression (McMahon et al. 2005).
A primary weakness in this study is the high attrition rate for the 4-month postpartum session. We attribute this to inadequate contact with participants during the first months after birth, insufficient subject incentive for the 4-month session, as well as the prevalence of depressive symptoms during pregnancy in those who did not return for this portion of the study. Another weakness is the lack of a direct measure of social support, which is significantly associated with risk for depression (O’Hara 1986). We also did not have a system to check reliability in our SCID assessments. Nearly 42% of our sample met criteria for an anxiety disorder and/or depression during pregnancy, approximately double typical rates (Gavin et al. 2005). Although ours was a sample of convenience, there likely was a self-selection bias in that women in distress volunteered in higher numbers as they indirectly were seeking greater support and oversight. Thus, the results of this study may not generalize to a more typical population. Finally, we primarily relied on brief self-report measures of depressive symptoms and attachment styles, and did not characterize women’s attachment fear in relation to their attachment security. A more thorough assessment of women’s attachment style may help in further identifying who is at risk for pregnancy distress as well as perinatal mood disorders.
Conclusion
Increasingly, we use diathesis–stress models to understand psychiatric symptoms, with genetic predisposition(Caspi et al. 2003), biological factors such as hormone profiles (Kammerer et al. 2006), and personality characteristics such as attachment styles acting as diatheses (Bifulco et al. 2002a, b). During pregnancy, when attachment concerns may be activated, relationship templates dominated by fear or a lack of security may act as a diathesis, leading to pregnancy distress, and making women vulnerable to perinatal depression. Assessing attachment during pregnancy could contribute to better screening for risk for perinatal mood disturbance, and, ultimately, to the development of a fuller conceptual model of perinatal mood dysregulation, which also could help advance specially-tailored psychosocial interventions focused on the modification of insecure attachment schemas.
Acknowledgements
This research was supported by the March of Dimes, the National Alliance for Research on Schizophrenia and Depression, the Sackler Institute, and by a Career Development Award MH01928 to Catherine Monk. We would like to thank the many women who participated in this research, as well as Liz Werner, Lynn M. Evans, Ph.D., and Anuja Kriplani for their contributions in the collection and management of these data. We also extend thanks to Michael Myers, Ph.D. for commenting on an earlier draft of this manuscript.
Footnotes
Thirty-seven subjects are missing data on birth weight and gestational age. However, because this study is not specifically concerned with infant outcome, we did not exclude subjects missing these data. We ran all analyses only with subjects with gestational age (none of whom were born prior to 37 weeks). In no instance did the results differ from analyses with all subjects.
Five babies weighed <2,500 g at birth. Eighteen hundred and fifteen grams (1,815 g) was the lowest weight.
The prediction of postpartum depressive symptoms based on women who were less depressed during pregnancy biases the data against our hypothesis. We lose power and, given that prior research indicates that depression during pregnancy predicts postpartum depression, likely constrict our range in the outcome variable.
The distribution of CES-D scores during pregnancy and at 4 months postpartum were skewed somewhat to the right. Using the square root transformation, both distributions were normal. We conducted regression analyses using the square root transformation and found similar results.
Contributor Information
Catherine Monk, Behavioral Medicine Program, Department of Psychiatry, College of Physicians and Surgeons, Columbia University Medical Center, 1150 St. Nicholas Avenue, Suite 1-121, New York, NY 10032, USA; Department of Obstetrics and Gynecology, College of Physicians and Surgeons, Columbia University Medical Center, New York, NY, USA.
Kristin L. Leight, Columbia Department of Psychiatry, New York State Psychiatric Institute, 1051 Riverside Drive, Box 106, New York, NY 10032, USA
Yixin Fang, Department of Mathematics and Statistics, Georgia State University, Atlanta, GA, USA.
References
- Alwan S, Reefhuis J, Rasmussen SA, Olney RS, Friedman JM. Use of selective serotonin-reuptake inhibitors in pregnancy and the risk of birth defects. N Engl J Med. 2007;356:2684–2692. doi: 10.1056/NEJMoa066584. [DOI] [PubMed] [Google Scholar]
- Andersen SM, Chen S. The relational self: an interpersonal social-cognitive theory. Psychol Rev. 2002;109:619–645. doi: 10.1037/0033-295x.109.4.619. [DOI] [PubMed] [Google Scholar]
- Austin MP, Lumley J. Antenatal screening for postnatal depression: a systematic review. Acta Psychiatr Scand. 2003;107:10–17. doi: 10.1034/j.1600-0447.2003.02024.x. [DOI] [PubMed] [Google Scholar]
- Austin MP, Tully L, Parker G. Examining the relationship between antenatal anxiety and postnatal depression. J Affect Disord. 2006;101(1–3):169–174. doi: 10.1016/j.jad.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Beck CT. A meta-analysis of predictors of postpartum depression. Nurs Res. 1996;45:297–303. doi: 10.1097/00006199-199609000-00008. [DOI] [PubMed] [Google Scholar]
- Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50:275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emeny G. Cognitive therapy of depression. Guilford; New York: 1979. [Google Scholar]
- Berard A, Ramos E, Rey E, Blais L, St-Andre M, Oraichi D. First trimester exposure to paroxetine and risk of cardiac malformations in infants: the importance of dosage. Birth Defects Res B Dev Reprod Toxicol. 2007;80:18–27. doi: 10.1002/bdrb.20099. [DOI] [PubMed] [Google Scholar]
- Bergman K, Sarkar P, O’Connor TG, Modi N, Glover V. Maternal stress during pregnancy predicts cognitive ability and fearfulness in infancy. J Am Acad Child Adolesc Psychiatry. 2007;46:1454–1463. doi: 10.1097/chi.0b013e31814a62f6. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Moran PM, Ball C, Bernazzani O. Adult attachment style. I: its relationship to clinical depression. Soc Psychiatry Psychiatr Epidemiol. 2002a;37:50–59. doi: 10.1007/s127-002-8215-0. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Moran PM, Ball C, Lillie A. Adult attachment style. II: its relationship to psychosocial depressive-vulnerability. Soc Psychiatry Psychiatr Epidemiol. 2002b;37:60–67. doi: 10.1007/s127-002-8216-x. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Figueiredo B, Guedeney N, Gorman LL, Hayes S, Muzik M, Glatigny-Dallay E, Valoriani V, Kammerer MH, Henshaw CA. Maternal attachment style and depression associated with childbirth: preliminary results from a European and US cross-cultural study. Br J Psychiatry Suppl. 2004;46:s31–s37. doi: 10.1192/bjp.184.46.s31. [DOI] [PubMed] [Google Scholar]
- Blackmore ER, Carroll J, Reid A, Biringer A, Glazier RH, Midmer D, Permaul JA, Stewart DE. The use of the Antenatal Psychosocial Health Assessment (ALPHA) tool in the detection of psychosocial risk factors for postpartum depression: a randomized controlled trial. J Obstet Gynaecol Can. 2006;28:873–878. doi: 10.1016/S1701-2163(16)32268-X. [DOI] [PubMed] [Google Scholar]
- Bowlby J. A secure base: parent–child attachment and healthy human development. Routledge; London: 1988. [Google Scholar]
- Boyce P, Hickie I, Parker G. Parents, partners or personality? Risk factors for post-natal depression. J Affect Disord. 1991;21:245–255. doi: 10.1016/0165-0327(91)90004-c. [DOI] [PubMed] [Google Scholar]
- Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample. Understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. 1982;39:1195–1200. doi: 10.1001/archpsyc.1982.04290100059010. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO. Social origins of depression: a study of psychiatric disorder in women. Tavistock; London: 1978. [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Chambers CD, Hernandez-Diaz S, Van Marter LJ, Werler MM, Louik C, Jones KL, Mitchell AA. Selective serotonin-reuptake inhibitors and risk of persistent pulmonary hypertension of the newborn. N Engl J Med. 2006;354:579–587. doi: 10.1056/NEJMoa052744. [DOI] [PubMed] [Google Scholar]
- Cohen S. Contrasting the hassles scale and the perceived stress scale: who’s really measuring appraised stress? Am Psychol. 1986;41:716–718. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Cooper PJ, Murray L, Hooper R, West A. The development and validation of a predictive index for postpartum depression. Psychol Med. 1996;26:627–634. doi: 10.1017/s0033291700035698. [DOI] [PubMed] [Google Scholar]
- Cooper PJ, Tomlinson M, Swartz L, Woolgar M, Murray L, Molteno C. Post-partum depression and the mother–infant relationship in a South African peri-urban settlement. Br J Psychiatry. 1999;175:554–558. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- Da Costa D, Larouche J, Dritsa M, Brender W. Psychosocial correlates of prepartum and postpartum depressed mood. J Affect Disord. 2000;59:31–40. doi: 10.1016/s0165-0327(99)00128-7. [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Ghera MM, Costigan K, Hawkins M. Measuring the ups and downs of pregnancy stress. J Psychosom Obstet Gynaecol. 2004;25:189–201. doi: 10.1080/01674820400017830. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: an integrative review. Psychol Bull. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Feeney J, Alexander R, Noller P, Hohaus L. Attachment insecurity, depression, and the transition to parenthood. Pers Relatsh. 2003;10:475–493. [Google Scholar]
- Field T. Infants of depressed mothers. Infant Behav Dev. 1995;18:1–13. doi: 10.1016/j.infbeh.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Field T. Maternal depression effects on infants and early interventions. Prev Med. 1998;27:200–203. doi: 10.1006/pmed.1998.0293. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Dieter J, Hernandez-Reif M, Schanberg S, Kuhn C, Yando R, Bendell D. Prenatal depression effects on the fetus and the newborn. Infant Behav Dev. 2004;27:216–229. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Biometrics Research Department. NYSPI; New York: 1997. Structured clinical interview for DSM-IV axis I disorders—non-patient edition. [Google Scholar]
- Fonagy P, Steele M, Moran G, Steele H, Higgitt A. Measuring the ghost in the nursery: an empirical study of the relation between parents’ mental representations of childhood experiences and their infants’ security of attachment. J Am Psychol Assoc. 1993;41:957–989. doi: 10.1177/000306519304100403. [DOI] [PubMed] [Google Scholar]
- Fraiberg S. Assessment and therapy of disturbances in infancy. Aronson; Northvale: 1995. Ghosts in the nursery: a psychoanalytic approach to the problems of impaired mother–infant relationships; pp. 164–221. [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC. Evidence Report/Technology Assessment (Summ) Agency for Healthcare Research and Quality; Rockville: 2005. Perinatal depression: prevalence, screening accuracy, and screening outcomes; pp. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George C, Kaplan N, Main M. An adult attachment interview. University of California at Berkeley; Berkeley: 1985. [Google Scholar]
- Gerlsma C, Luteijn F. Attachment style in the context of clinical and health psychology: a proposal for the assessment of valence, incongruence, and accessibility of attachment representations in various working models. Br J Med Psychol. 2000;73(Pt 1):15–34. doi: 10.1348/000711200160273. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Whiffen VE, Mount JH, Milne K, Cordy NI. Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57:269–274. doi: 10.1037//0022-006x.57.2.269. [DOI] [PubMed] [Google Scholar]
- Griffin D, Bartholomew K. Models of self and other: fundamental dimensions underlying measures of adult attachment. J Pers Soc Psychol. 1994a;67:430–445. [Google Scholar]
- Griffin D, Bartholomew K. The metaphysics of measurement: the case of adult attachment. In: Bartholomew K, Perlman D, editors. Advances in personal relationships. Jessica Kingsley; London: 1994b. pp. 17–52. [Google Scholar]
- Hart R, McMahon CA. Mood state and psychological adjustment to pregnancy. Arch Womens Ment Health. 2006;9:329–337. doi: 10.1007/s00737-006-0141-0. [DOI] [PubMed] [Google Scholar]
- Hart S, Jones NA, Field T. Atypical expressions of jealousy in infants of intrusive- and withdrawn-depressed mothers. Child Psychiatry Hum Dev. 2003;33:193–207. doi: 10.1023/a:1021452529762. [DOI] [PubMed] [Google Scholar]
- Hazan C, Shaver P. Romantic love conceptualized as an attachment process. J Pers Soc Psychol. 1987;52:511–524. doi: 10.1037//0022-3514.52.3.511. [DOI] [PubMed] [Google Scholar]
- Heron J, O’Connor TG, Evans J, Golding J, Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80:65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Kammerer M, Taylor A, Glover V. The HPA axis and perinatal depression: a hypothesis. Arch Womens Ment Health. 2006;9:187–196. doi: 10.1007/s00737-006-0131-2. [DOI] [PubMed] [Google Scholar]
- Kaplan LA, Evans L, Monk C. Effects of mothers’ prenatal psychiatric status and postnatal caregiving on infant biobehavioral regulation: can prenatal programming be modified. Early Hum Dev. 2007;84(4):249–256. doi: 10.1016/j.earlhumdev.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurdek LA. On being insecure about the assessment of attachment styles. J Soc Pers Relatsh. 2002;19:811–834. [Google Scholar]
- Louik C, Lin AE, Werler MM, Hernandez-Diaz S, Mitchell AA. First-trimester use of selective serotonin-reuptake inhibitors and the risk of birth defects. N Engl J Med. 2007;356:2675–2683. doi: 10.1056/NEJMoa067407. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Wolfe R, Lyubchik A. Depression and the parenting of young children: making the case for early preventive mental health services. Harv Rev Psychiatry. 2000;8:148–153. [PubMed] [Google Scholar]
- Matthey S, Barnett B, Ungerer J, Waters B. Paternal and maternal depressed mood during the transition to parenthood. J Affect Disord. 2000;60:75–85. doi: 10.1016/s0165-0327(99)00159-7. [DOI] [PubMed] [Google Scholar]
- McMahon C, Barnett B, Kowalenko N, Tennant C. Psychological factors associated with persistent postnatal depression: past and current relationships, defence styles and the mediating role of insecure attachment style. J Affect Disord. 2005;84:15–24. doi: 10.1016/j.jad.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Meredith P, Noller P. Attachment and infant difficultness in postnatal depression. J Fam Issues. 2003;24:668–686. [Google Scholar]
- Monk C, Fifer WP, Sloan RP, Myers MM, Trien L, Hurtado A. Maternal stress responses and anxiety during pregnancy: effects on fetal heart rate. Dev Psychobiol. 2000;36:67–77. [PubMed] [Google Scholar]
- Monk C, Myers MM, Sloan RP, Werner L, Jeon J, Tager F, Fifer WP. Fetal heart rate reactivity differs by women’s psychiatric status: an early marker for developmental risk? J Am Acad Child Adolesc Psych. 2004;43:283–290. doi: 10.1097/00004583-200403000-00009. [DOI] [PubMed] [Google Scholar]
- Murray L, Fiori-Cowley A, Hooper R, Cooper PJ. The impact of postnatal depression and associated adversity on early mother infant interactions and later infant outcomes. Child Dev. 1996;67:2512–2526. [PubMed] [Google Scholar]
- Newport DJ, Wilcox MM, Stowe ZN. Maternal depression: a child’s first adverse life event. Semin Clin Neuropsychiatry. 2002;7:113–119. doi: 10.1053/scnp.2002.31789. [DOI] [PubMed] [Google Scholar]
- Oberlander TF, Grunau RE, Fitzgerald C, Ellwood A-L, Misri S, Rurak D, Riggs KW. Prolonged prenatal psychotropic medication exposure alters neonatal acute pain response. Pediatr Res. 2002;51:443–453. doi: 10.1203/00006450-200204000-00008. [DOI] [PubMed] [Google Scholar]
- Oberlander TF, Grunau RE, Fitzgerald C, Papsdorf M, Rurak D, Riggs W. Pain reactivity in 2-month-old infants after prenatal and postnatal serotonin reuptake inhibitor medication exposure. Pediatrics. 2005;115:411–425. doi: 10.1542/peds.2004-0420. [DOI] [PubMed] [Google Scholar]
- Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C. Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Arch Gen Psychiatry. 2006;63:898–906. doi: 10.1001/archpsyc.63.8.898. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children’s behavioral/emotional problems at 4 years: report from the Avon longitudinal study of parents and children. Br J Psychiatry. 2002;180:502–508. doi: 10.1192/bjp.180.6.502. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Ben-Shlomo Y, Heron J, Golding J, Adams D, Glover V. Prenatal anxiety predicts individual differences in cortisol in pre-adolescent children. Biol Psychiatry. 2005;58:211–217. doi: 10.1016/j.biopsych.2005.03.032. [DOI] [PubMed] [Google Scholar]
- O’Hara MW. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry. 1986;43:569–573. doi: 10.1001/archpsyc.1986.01800060063008. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Gorman LL. Can postpartum depression be predicted? Prim Psychiatry. 2004;11:42–47. [Google Scholar]
- O’Hara MW, Rehm LP, Campbell SB. Postpartum depression. A role for social network and life stress variables. J Nerv Ment Dis. 1983;171:336–341. [PubMed] [Google Scholar]
- O’Hara MW, Schlechte JA, Lewis DA, Varner MW. Controlled prospective study of postpartum mood disorders: psychological, environmental, and hormonal variables. Journal of Abnormal Psychology. 1991;100:63–73. doi: 10.1037//0021-843x.100.1.63. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Roberts RE. Reliability of the CES-D Scale in different ethnic contexts. Psychiatry Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- Rooney E, Gaudette M, Pergament E. Neonatal complications associated with late pregnancy use of selective serotonin reuptake inhibitors. ITIS Newsletter. 2006 Apr;13(no. 2) 2006. [Google Scholar]
- Rosenbaum JF, Biederman J, Gersten M, Hirshfeld DR, Meminger SR, Herman JB, Kagan J, Reznick JS, Snidman N. Behavioral inhibition in children of parents with panic disorder and agoraphobia. A controlled study. Arch Gen Psychiatry. 1988;45:463–470. doi: 10.1001/archpsyc.1988.01800290083010. [DOI] [PubMed] [Google Scholar]
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: a systematic review. J Clin Psychiatry. 2006;67:1285–1298. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- Sandman CA, Wadhwa P, Glynn L, Chicz-Demet A, Porto M, Garite TJ. Corticotrophin-releasing hormone and fetal responses in human pregnancy. Ann N Y Acad Sci. 1999;897:66–75. doi: 10.1111/j.1749-6632.1999.tb07879.x. [DOI] [PubMed] [Google Scholar]
- Simpson JA, Rholes WS, Campbell L, Tran S, Wilson CL. Adult attachment, the transition to parenthood, and depressive symptoms. J Pers Soc Psychol. 2003;84:1172–1187. doi: 10.1037/0022-3514.84.6.1172. [DOI] [PubMed] [Google Scholar]
- Sinclair D, Murray L. Effects of postnatal depression on children’s adjustment to school. Teacher’s reports. Br J Psychiatry. 1998;172:58–63. doi: 10.1192/bjp.172.1.58. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. Consulting Psychologists. Palo Alto: 1983. Manual for the state—trait anxiety inventory. [Google Scholar]
- Sroufe LA. Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum Dev. 2005;7:349–367. doi: 10.1080/14616730500365928. [DOI] [PubMed] [Google Scholar]
- Sugawara M, Toda MA, Shima S, Mukai T, Sakakura K, Kitamura T. Premenstrual mood changes and maternal mental health in pregnancy and the postpartum period. J Clin Psychol. 1997;53:225–232. doi: 10.1002/(sici)1097-4679(199704)53:3<225::aid-jclp5>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Suri R, Altshuler L, Hellemann G, Burt VK, Aquino A, Mintz J. Effects of antenatal depression and antidepressant treatment on gestational age at birth and risk of preterm birth. Am J Psychiatry. 2007;164:1206–1213. doi: 10.1176/appi.ajp.2007.06071172. [DOI] [PubMed] [Google Scholar]
- Van den Bergh BR, Marcoen A. High antenatal maternal anxiety is related to ADHD symptoms, externalizing problems and anxiety in 8–9 year olds. Child Dev. 2004;75:1085–1097. doi: 10.1111/j.1467-8624.2004.00727.x. [DOI] [PubMed] [Google Scholar]
- Warren SL, Gunnar MR, Kagan J, Anders TF, Simmens SJ, Rones M, Wease S, Aron E, Dahl RE, Sroufe LA. Maternal panic disorder: infant temperament, neurophysiology, and parenting behaviors. J Am Acad Child Adolesc Psychiatry. 2003;42:814–825. doi: 10.1097/01.CHI.0000046872.56865.02. [DOI] [PubMed] [Google Scholar]
- Way CM. Safety of newer antidepressants in pregnancy. Pharmacotherapy. 2007;27:546–552. doi: 10.1592/phco.27.4.546. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. J Nerv Ment Dis. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Gammon GD, Merikangas KR, Leckman JF, Kidd KK. Psychopathology in the children (ages 6–18) of depressed and normal parents. J Am Acad Child Psychiatry. 1984;23:78–84. doi: 10.1097/00004583-198401000-00011. [DOI] [PubMed] [Google Scholar]
- Werner A, Myers MM, Fifer WP, Cheng B, Fang Y, Allen R, Monk C. Prenatal predictors of infant temperament. Dev Psycho-biol. 2007;49:474–484. doi: 10.1002/dev.20232. [DOI] [PubMed] [Google Scholar]