Abstract
Objective: To address the effect of intrinsic factors on craniofacial growth by analyzing the craniofacial morphology of unoperated isolated cleft palate in Chinese adult. Materials and Methods: This study included 37 nonsyndromic isolated cleft palate and 39 age and gender matched non-clefts. Twenty-six cephalometric measurements were employed to evaluate the facial morphology. Independent samples T test and Mann-Whitney U were used for comparison. Significant difference was defined at 95% level. Results: Data from this study showed patients with unoperated isolated cleft palate have a reduced maxillary sagittal length (ANS-PMP, A-PMP, P<0.05), a smaller ANB angle (ANB, P<0.05) and a retrusive ANS point (S-N-ANS, P<0.05; Ba-N-ANS, P<0.05). Measurements descripted position of maxilla (S-Ptm, P>0.05), depth of bony pharynx (Ba-PMP, P>0.05), anterior and posterior maxillary height (N-ANS, P>0.05; R-PMP, P>0.05) and mandible morphology (including linear measurements and angle measurements) did not show any significant difference between case and control groups. Conclusions: Patients with isolated cleft palate were characterized by maxillary retrusion. Mandible morphology and cranial basal morphology in isolated cleft palate showed no significant difference with nonclefts. Patients with isolated cleft palate are more vulnerable to cross bite than nonclefts. Intrinsic deficiencies did detrimental effect on maxilla sagittal length, but did no detrimental effect on maxilla position, mandible size and position.
Keywords: isolated cleft palate, unoperated, craniofacial morphology, maxillary growth, cephalometry
Introduction
The reasons affected facial morphology including three main factors: intrinsic developmental deficiencies, functional distortions affecting the position and growth, and iatrogenic factors (1,2).
Some investigations indicated that facial morphology in infants, children, adolescents, and adults with isolated cleft palate (ICP) were all different compared with non-clefts (3–12). Facial growth deficiency goes worse with age (6,12), but facial morphology is still acceptable because of modulation of mandible position (6). Iatrogenic factors are not the main reason resulted in maxillary retrusion, but intrinsic deficiencies are (3,13). However, another researches showed that the facial morphology is similarly normal when compared with nonclefts (14–20). Different findings may result from the heterogeneity of the samples (18,21), small sample size (22,23), the various range of age (18), different cleft types of samples (15,24,25) and factors related to the control group.
Craniofacial morphology is of genetic and racial characteristic. In previous studies about unoperated isolated cleft palate, both patients with soft cleft palate only and patients with hard and soft cleft palate were included. The two types of cleft are so different: vomer is well connected with palate plane in soft cleft palate, but vomer is not in hard and soft cleft palate.
The aim of this research is to address the effect of intrinsic factors on craniofacial growth by analyzing the craniofacial morphology of unoperated isolated cleft palate in Chinese adult.
Materials and Methods
Patients included were selected from patients with Han nationality, who examined at the West China Hospital of Stomatology, the People's Republic of China, during 2005 and 2009. All the samples had non-syndromic ICP and the cleft from uvula to incisive foramen. All the samples had not received any craniofacial surgeries and orthodontic treatments, and did not have family history and craniofacial trauma. Besides, all the samples were elder than 16-year-old. This study protocol was appraised and approved by the Research Subject Review Board and Ethical Scientific Board of Sichuan University. Informed consent was obtained from all patients or their parents.
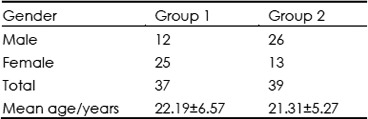
Case group was named as group 1. Control group was constituted with age and gender matched non-cleft adults. The control group was named as group 2. Sample distribution of this study was shown in Table 1.
Table 1. Sample distribution.
All the radiographs were taken by the same professional radiologist using the same equipment. All the cephalometric radiographs were obtained in centric occlusion with the patients positioned in a standardized upright posture with a transporionic axis and Frankfort plane parallel with the floor (26,27).
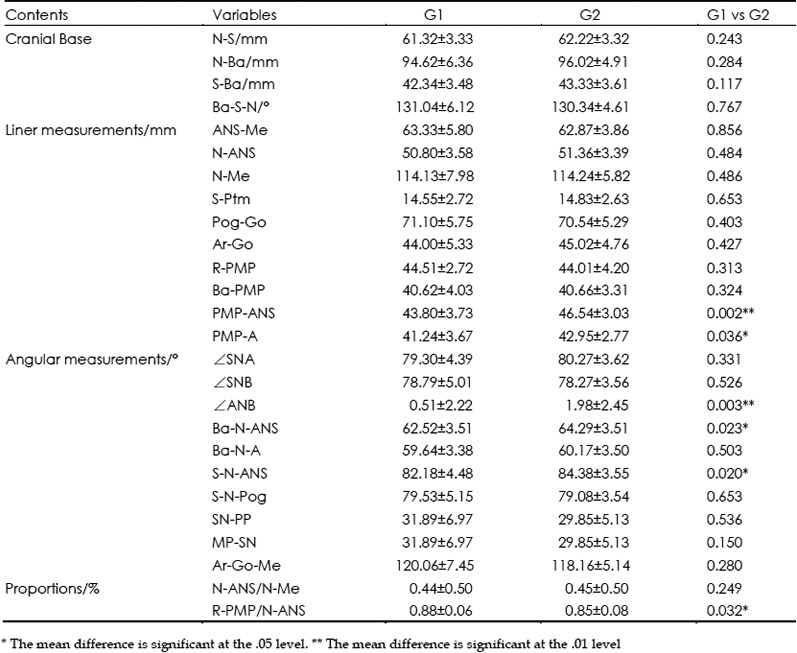
The constructed landmarks used in this study were traced according to Ross (1). Anatomic landmarks used were shown in Table 2 and Figure 1. Planes analyzed were listed in Figure 1. Measurements utilized, including 13 linear measurements, 11 angular measurements and 2 ratio measurements, were shown in Table 3. PNS was not included in measurements, because it was not clear enough in cleft patients to be included for evaluation (28). All the measurements were traced and measured by the same researcher using Winceph7.0 cephalometric software (Rise Corporation, Sendai, Japan). Tracing was performed twice, with two weeks interval. Intra-investigator reliability was assessed within 30 subjects selected randomly, and intra-class correlation coefficients (ICC) were above 0.9 for all the measurements, suggesting satisfactory level. Mean values were used for analysis.
Table 2. Landmarks tracing on the cephalometric radiographs.
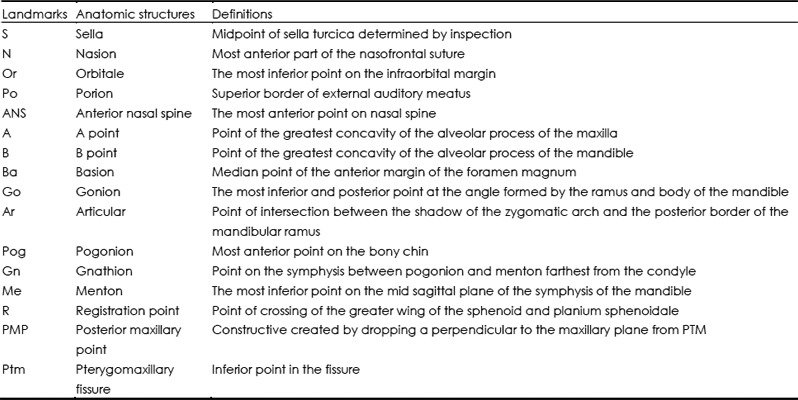
Figure 1.
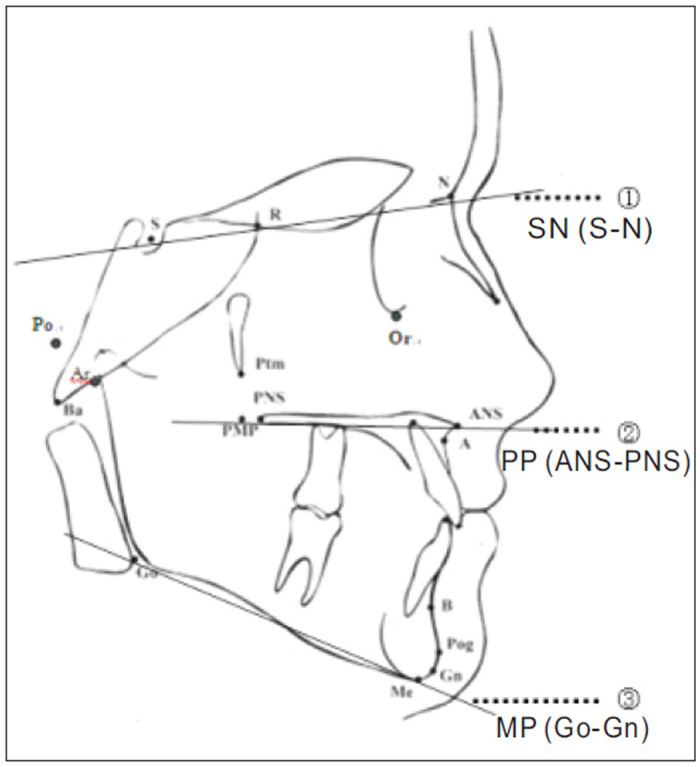
Landmarks and planes traced on the lateral cephalometric radiographs. 1SN (S-N): Anterior basal plane; 2PP (ANS-PNS): Palatal plane; 3MP (Go-Gn): Mandibular plane.
Table 3. Statistical descriptions of all the measurements and results of statistics between two groups.
Statistical analyses
Statistical analyses were performed using SPSS 13.0 software package. The nature of data distribution was tested with the one-sample Kolmogorov-Smirnov test. Independent samples T test and Mann-Whitney U were employed to determine the difference between case and control group. Significant difference was defined at 95% level.
Results
There was no significant difference when comparing gender ratio between case and control groups. So data in each group were put together to analysis.
Data in this study showed patients with unoperated ICP lead a reduced maxillary sagittal length (ANS-PMP, A-PMP, P<0.05), a smaller ANB angle (ANB, P<0.05), a retrusive ANS point (S-N-ANS, P<0.05; Ba-N-ANS, P<0.05) and a smaller ratio of posterior facial height to anterior facial height (R-PMP/N-ANS) (Figure 2). Measurements descripted position of maxilla (S-Ptm, P>0.05), depth of bony pharynx (Ba-PMP, P>0.05), anterior and posterior maxillary height (N-ANS, P>0.05; R-PMP, P>0.05), and mandible morphology (including linear measurements and angle measurements) showed no significant difference between case and control group. The statistic results were shown in Table 3.
Figure 2.
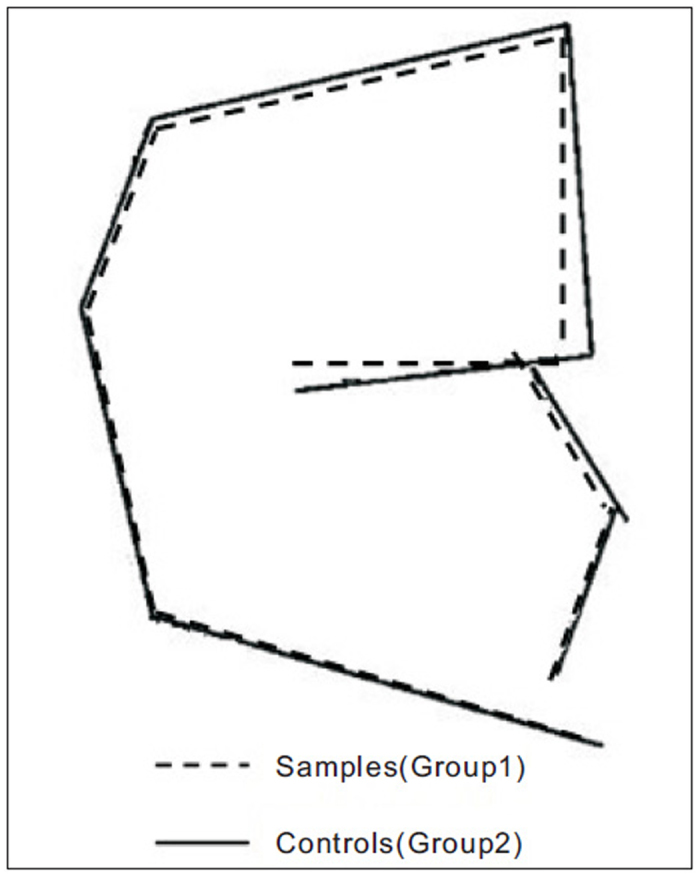
Craniofacial skeleton features in unoperated ICP. The broke line is for group 1 and the solid line for group2. Diagrams are orientated along the S-Ba line and recorded at S.
Discussion
Isolated cleft palate was thought to be different with other types of cleft in embryology, growth pattern, and features of craniofacial morphology (29). The best way to learn the effect of intrinsic factor is by studying adult unoperated patients with cleft (2). So only patients elder than 16-year-old were brought into this study.
Patients with isolated cleft palate have always been considered to have better facial growth, but the fact is not like this (2,18). Patients with unoperated ICP in this study lead a decreased maxilla length and fairly normal maxilla position. The consistent depth of the bony pharynx and retrusive ANS point indicated that the maxillary retrusion can be attributed to maxillary length rather than to maxillary position. Growth potential deficiency of the maxilla in clefts resulted in retrusive maxilla (5,30). Chen et al (12) compared 16 unoperated ICP with mixed dentition and 25 with permanent dentition with non-clefts respectively, concluded that unoperated ICP with mixed dentition have a short maxilla in sagittal dimension, and patients with permanent dentition have a short and retropositioned maxilla. Many scholars got the similar conclusion (6,9,16,31). Yoshida et al (11) analysed 21 ICP patients and concluded that short hard palate and retropositioned maxilla existed in ICP patients with permanent dentition. Dahl (16) and Bishara (7) considered maxilla was retropositioned in unoperated isolated cleft lip and palate. Diah et al (2) drew the conclusion that unoperated ICP had smaller SNA angle and palatal surface area, shorter arch depth and length, smaller palatal vault volume by analyzing plaster cast of 10 patients with isolated cleft palate elder than 16 years.
The normal maxilla increases in length by a forward movement of the entire bone and a concomitant apposition of bone to the posterior tuberosity (29). The anterior surface of the basal maxilla shows resorption (32), although there is some dento-alveolar apposition which contributes to over-all length (29). The maxilla drifts forward as a result of a number of factors including the facial sutures (33), the nasal septum (34) and the soft tissue functional matrix (35). Maxillary translocation takes place in a sliding fashion along the length of the junction of the vomer with the maxilla (36). The vomer moves downward and forward because of bony appositional growth at its superior and posterior surfaces (37). When the cleft existed from uvula to incisive foramen, the vomer almost isolated from maxilla, and then the normal sliding of the vomer along maxillary was destroyed, the balanced reconciliation of maxillary forward growth, nasal septum growth and vomer forward growth are lost (38). Maxilla growth deficiency should be attributed to intrinsic factors (7,16,24,39). The role of nasal septum plays in forward development of the upper face has been suggested by Scott (40), and expanded later by Latham and Delaire (41,42).
In this study, no significant difference existed between ICP and nonclefts about mandible length and growth direction. Some scholars got the similar conclusion that mandible morphology in ICP had no significant difference compared with nonclefts, no matter what age they were (43,44). While the others got the opposite opinion, they thought ICP got a short (Go-Gn) (6,16) and clockwised mandible (6,11,16). Smahel (45) concluded that both body and ramus of mandible were shorter than nonclefts. Da Silva Filho et al (46) and Hermann et al (31) hold the similar viewpoint. Shibasaki and Ross (47) considered the only significant intrinsic abnormality was in the maxillary complex with the possibility of a slight mandibular deficiency. Dahl (16) and Bishara (7) considered mandible is retropositioned in unoperated isolated cleft lip and palate.
Researches about adults with ICP have shown that differences existed in both size and shape of cranial base when compared with nonclefts (16). Length of cranial base (S-Ba, S-N) was smaller and angle of cranial base (Ba-S-N) was blunter than nonclefts. Deviation above was resulted from functional factors (48). However, in our study, data showed there was no significant difference in both size and shape of cranial base between ICP and nonclefts. Ross (4) got the similar results by analyzing 103 ICP individuals and nonclefts from 4-year-old to adulthood, and just realized that significant differences were existed in linear measurements (4,16).
Conclusions
Patients with isolated cleft palate were characterized by maxillary retrusion. Mandible morphology and cranial basal morphology in isolated cleft palate showed no significant difference with nonclefts. Patients with isolated cleft palate are more vulnerable to cross bite than nonclefts. Intrinsic deficiencies did detrimental effect on maxilla sagittal length, but did no detrimental effect on maxilla position, mandible size and position.
References
- Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Part 1: treatment affecting growth. Cleft Palate J. 1987;24:5–23. [PubMed] [Google Scholar]
- Diah E, Lo LJ, Huang CS, Sudjatmiko G, Susanto I, Chen YR. Maxillary growth of adult patients with unoperated cleft: answers to the debates. J Plastic Reconstr Aesthet Surg. 2007;60:407–413. [DOI] [PubMed] [Google Scholar]
- Bishara SE, Krause JC, Olin WH, Weston D, Ness JV, Felling C. Facial and dental relationships of individuals with unoperated clefts of the lip and/or palate. Cleft Palate J. 1976;13:238–252. [PubMed] [Google Scholar]
- Ross RB. Cranial base in children with lip and palate clefts. Cleft Palate J. 1965;2:157–166. [PubMed] [Google Scholar]
- Ross RB, Coupe TB. Craniofacial morphology in six pairs of monozygotic twins discordant for cleft lip and palate. J Can Dent Assoc. 1965;31:149–157. [PubMed] [Google Scholar]
- Shibasaki Y, Ross RB. Facial growth in children with isolated cleft palate. Cleft Palate J. 1969;6:290–302. [PubMed] [Google Scholar]
- Bishara SE. Cephalometric evaluation of facial growth in operated and nonoperated individuals with isolated clefts of the palate. Cleft Palate J. 1973;10:239–246. [PubMed] [Google Scholar]
- Smahel Z. Variations in craniofacial morphology with severity of isolated cleft palate. Cleft Palate J. 1984;21:140–158. [PubMed] [Google Scholar]
- Smahel Z, Brousilová M, Müllerová Z. Craniofacial morphology in isolated cleft palate prior to palatoplasty. Cleft Palate J. 1987;24:200–208. [PubMed] [Google Scholar]
- Athanasiou AE, Moyers RE, Mazaheri M, Toutountzakis N. Frontal cephalometric evaluation of transverse dentofacial morphology and growth of children with isolated cleft palate. J Craniomaxillofac Surg. 1991;19:249–253. [DOI] [PubMed] [Google Scholar]
- Yoshida H, Nakamura A, Michi K, Wang GM, Liu K, Qiu WL. Cephalometric analysis of maxillofacial morphology in unoperated cleft palate patients. Cleft Palate J. 1992;29:419–424. [DOI] [PubMed] [Google Scholar]
- Chen ZQ, Qian YF, Wang GM, Shen G. Sagittal Maxillary Growth in Patients with Unoperated Isolated Cleft Palate. Cleft Palate J. 2009;46:664–667. [DOI] [PubMed] [Google Scholar]
- Berkowitz S. Cleft lip and palate: perspectives in management. San Diego, CA: Singular Publishing Group, Inc, 1996:13–28. [Google Scholar]
- Ortiz-Monasterio F, Rebeil AS, Valderrama M, Cruz R. Cephalometric measurement on adult patients with non-operated cleft palate. Plast Reconstr Surg Transplant Bull. 1959;24:53–61. [DOI] [PubMed] [Google Scholar]
- Ortiz-Monasterio F, Serrano A, Barrera G, Rodriguez-Hoffman H, Vinageras E. A study of untreated adult cleft palate patients. Plast Reconstr Surg. 1966;38:36–41. [DOI] [PubMed] [Google Scholar]
- Dahl E. Craniofacial morphology in congenital clefts of the lip and palate. An x-ray cephalometric study of young adult males. Acta Odontol Scand. 1970;28:107–116. [PubMed] [Google Scholar]
- Boo-Chai K. The unoperated adult bilateral cleft of the lip and palate. Br J Plast Surg. 1971;24:250–257. [DOI] [PubMed] [Google Scholar]
- Mars M, Houston WJ. A preliminary study of facial growth and morphology in unoperated male unilateral cleft lip and palate subjects over 13 years of age. Cleft Palate J. 1990;27:7–10. [DOI] [PubMed] [Google Scholar]
- Rees TD. Unoperated bilateral cleft lip and palate in a young adult: a thirty year follow-up. Br J Plast Surg. 1991;44:378–383. [DOI] [PubMed] [Google Scholar]
- Capelozza Júnior L, Taniguchi SM, da Silva Júnior OG. Craniofacial morphology of adult unoperated complete unilateral cleft lip and palate patients. Cleft Palate J. 1993;30:376–381. [DOI] [PubMed] [Google Scholar]
- Shetye PR. Facial growth of adults with unoperated clefts. Clin Plast Surg. 2004;31:361–371. [DOI] [PubMed] [Google Scholar]
- Bishara SE, De Arrendondo RS, Vales HP, Jakobsen JR. Dento-facial relationships in persons with unoperated clefts: comparisons between three cleft types. Am J Orthod. 1985;87:481–507. [DOI] [PubMed] [Google Scholar]
- Bishara SE, Jakobsen JR, Krause JC, Sosa-Martinez R. Cephalometric comparisons of individuals from India and Mexico with unoperated cleft lip and palate. Cleft Palate J. 1986;23:116–125. [PubMed] [Google Scholar]
- Isiekwe MC, Sowemimo GO. Cephalometric findings in a normal Nigerian population sample and adult Nigerians with unrepaired clefts. Cleft Palate J. 1984;21:323–328. [PubMed] [Google Scholar]
- Ross RB. Treatment variables affecting growth in unilateral cleft lip and palate. Part 5: timing of palate repair. Cleft Palate J. 1987;24:54–63. [PubMed] [Google Scholar]
- Grummons DC, Kappeyne van de Coppello MA. A frontal asymmetry analysis. J Clin Orthod. 1987;21:448–465. [PubMed] [Google Scholar]
- Nollet PJ, Katsaros C, Huyskens RW, Borstlap WA, Bronkhorst EM, Kuijpers-Jaqtman AM. Cephalometric evaluation of long-term craniofacial development in unilateral cleft lip and palate patients treated with delayed hard palate closure. Int J Oral Maxillofac Surg. 2008;37:123–130. [DOI] [PubMed] [Google Scholar]
- Yamanishi T, Nishio J, Sako M, Kohara H, Hirano Y, Yamanishi Y, Adachi T, Miya S, Mukai T. Early two-stage double opposing Z-plasty or one-stage push-back palatoplasty? Comparisons in maxillary development and speech outcome at 4 years of age. Ann Plast Surg. 2011;66:148–153. [DOI] [PubMed] [Google Scholar]
- Ross RB. The clinical implications of facial growth in cleft lip and palate. Cleft Palate J. 1970;7:37–47. [PubMed] [Google Scholar]
- Coupe TB, Subtelny JD. Cleft palate deficiency or displacement of tissue. Plastic Reconstr Surg. 1960;26:600–612. [PubMed] [Google Scholar]
- Hermann NV, Kreiborg S, Darvann TA, Jensen BL, Dahl E, Bolund S. Craniofacial morphology and growth comparisons in children with Robin Sequence, Isolated cleft palate and unilateral complete cleft lip and palate. Cleft Palate J. 2003;40:373–396. [DOI] [PubMed] [Google Scholar]
- Enlow DH, Bang S. Growth and remodeling of the human maxilla. Am J Orthod. 1965;51:446–464. [DOI] [PubMed] [Google Scholar]
- Sicher H, DuBrul EL. Oral Anatomy (8th edition). St. Louis: IshiyakuEuro America, Inc, 1988:65–86. [Google Scholar]
- Scott JH. Growth at facial sutures. Am J Orthod. 1956;42:381–387. [Google Scholar]
- Moss ML. The functional matrix hypothesis revisited. 4. The epigenetic antithesis and the resolving synthesis. Am J Orthod Dentofacial Orthop. 1997;112:410–417. [DOI] [PubMed] [Google Scholar]
- Friede H. The vomero-premaxillary suture—a neglected growth site in mid-facial development of unilateral cleft lip and palate patients. Cleft Palate J. 1978;15:398–404. [PubMed] [Google Scholar]
- Melsen B. Histological analysis of the postnatal development of the nasal septum. Angle Orthod. 1977;47:83–96. [DOI] [PubMed] [Google Scholar]
- Delaire J, Precious D. Avoidance of the use of vomerine mucosa in primary surgical management of velopalatine clefts. Oral Surg Oral Med Oral Pathol. 1985;60:589–597. [DOI] [PubMed] [Google Scholar]
- Hagerty RF, Hill MJ. Facial growth and dentition in the unoperated cleft palate. J Dent Res. 1963;42:412–421. [Google Scholar]
- Scott JH. The analysis of facial growth from fetal life to adulthood. Angle Orthod. 1963:33:110–113. [Google Scholar]
- Latham RA, Scott JH. A newly postulated factor in the early growth of the human middle face and the theory of multiple assurances. Arch Oral Biol. 1970;15:1097–1100. [DOI] [PubMed] [Google Scholar]
- Delaire J, Precious D. Interaction of the development of the nasal septum, nasal pyramid and the face. Int J Pediatr Otorhino-laryngol. 1987;12:311–326. [DOI] [PubMed] [Google Scholar]
- Mestre JC, De Jesus J, Subtelny JD. Unoperated oral clefts at maturation. Angle Orthod. 1960;30:78–85. [Google Scholar]
- Lu DW, Shi B, Wang HJ, Zheng Q. The comparative study of craniofacial structural characteristic of individuals with different types of cleft palate. Ann Plast Surg. 2007;59:382–387. [DOI] [PubMed] [Google Scholar]
- Smahel Z. Variation in craniofacial morphology with severity of isolated cleft palate. Cleft Palate J. 1984;21:140–158. [PubMed] [Google Scholar]
- Da Silva Filho OG, Normando AD, CapelozzaFilho L. Mandibular growth in patients with cleft lip and/or cleft palate—the influence of cleft type. Am J Orthod Dentofacial Orthop. 1993;104:269–275. [DOI] [PubMed] [Google Scholar]
- Shibasaki Y, Ross RB. Facial growth in children with isolated cleft palate. Cleft Palate J. 1969;6:290–302. [PubMed] [Google Scholar]
- Sandham A, Foong K. The effect of cleft deformity, surgical repair and altered function in unilateral cleft lip and palate. In: Proceedings of the 8th International Congress on Cleft Palate and Related Craniofacial Anomalies. Singapore: Stamford Press; 1997:673–678. [Google Scholar]


