Abstract
Osteogenesis imperfecta (OI) comprises a group of heritable connective tissue disorders generally defined by recurrent fractures, low bone mass, short stature and skeletal fragility. Beyond the skeletal complications of OI, many patients also report intolerance to physical activity, fatigue and muscle weakness. Indeed, recent studies have demonstrated that skeletal muscle is also negatively affected by OI, both directly and indirectly. Given the well-established interdependence of bone and skeletal muscle in both physiology and pathophysiology and the observations of skeletal muscle pathology in patients with OI, we investigated the therapeutic potential of simultaneous anabolic targeting of both bone and skeletal muscle using a soluble activin receptor 2B (ACVR2B) in a mouse model of type III OI (oim). Treatment of 12-week-old oim mice with ACVR2B for 4 weeks resulted in significant increases in both bone and muscle that were similar to those observed in healthy, wild-type littermates. This proof of concept study provides encouraging evidence for a holistic approach to treating the deleterious consequences of OI in the musculoskeletal system.
Introduction
Osteogenesis imperfecta (OI) comprises a group of heritable connective tissue disorders generally defined by recurrent fractures, low bone mass, short stature and skeletal fragility. The vast majority of OI cases (∼90%) are the result of dominant mutations in either of the two type I collagen genes, COL1A1 or COL1A2, the most abundant and primary structural proteins in the organic bone matrix.1 Over the past 10 years, a rapidly growing list of recessive gene mutations has emerged, which account for the remaining 5%–10% of OI cases, although—with a few exceptions (e.g., SERPINF1, IFITM5, LRP5, SP7)—most of these genes are intimately involved in the trafficking or complex post-translational processing of type I collagen.2 In the clinic, the wide spectrum of phenotypic variance in OI is classified into five types, based largely on the Sillence classification system that was originally outlined 35 years ago.3 In order of increasing severity, the five phenotypic classifications of OI are type I (classic, non-deforming OI with blue sclerae), type IV (common variable OI with normal sclerae), type V (OI with ossification in interosseous membranes), type III (progressively deforming OI with normal sclerae) and type II (perinatally lethal OI). The majority of the rare, recessive types of OI and newly discovered non-collagen molecular defects, which had previously been assigned their own OI types, are now enfolded as subtypes of type III OI.4
Beyond the skeletal complications of OI, many patients also report intolerance to physical activity, fatigue, and muscle weakness, in some cases so severe that it serves as a presenting symptom for the disease.5 While frequently reported, the impact of OI on skeletal muscle function and anatomy has only received limited investigation. A study of 20 children with type I OI demonstrated decreased resistance to fatigue and lower muscle force in the plantar flexor.6 Another study by Takken and colleagues7 observed decreased isometric muscle force of the shoulder abductors, hip flexors, ankle dorsiflexors, and grip strength in 17 children and adolescents with type I OI, when compared to age-/sex-matched controls. More recently, Veilleux and colleagues8 studied the muscle anatomy and dynamic muscle function of 54 patients with type I OI. They observed that patients with OI had smaller muscle size, lower average peak force and lower specific peak force when compared to age-/sex-matched controls. Interestingly, the deficits in skeletal muscle observed in all of these studies were seen in the least severe form of OI, suggesting that there may be an intrinsic defect in the skeletal muscle of OI patients. Moreover, one might speculate that the deleterious effect of OI on skeletal muscle could be exacerbated in more severe types of the disease by repeated bouts of inactivity with more frequent fractures. Indeed, a recent cross-sectional study of 62 children and adolescents with varying types of OI demonstrated that moderate and severe forms of OI are associated with greater functional impairment, influenced by fracture history, which has a negative impact on ambulation.9
The activin signaling pathway, well known for its activity in regulating skeletal muscle mass through myostatin,10 has recently been demonstrated to affect bone development and remodeling as well.11–15 Systemic blockade of activin receptor signaling using a soluble activin receptor 2B (ACVR2B) has previously been demonstrated to increase muscle mass in mouse models of androgen deficiency,16 muscular dystrophy17 and cancer cachexia.18 ACVR2B administration also increased bone formation rates and bone mineral density in aged mice19 and demonstrated direct effects on osteoblast activity.12 Given the well-established interdependence of bone and skeletal muscle in both physiology and pathophysiology20 and the observations of skeletal muscle pathology in patients with OI, we proposed to investigate the therapeutic potential of simultaneously targeting both bone and skeletal muscle in this study, using a soluble activin receptor in a mouse model of OI. Using the oim mouse, which most closely resembles the severe, deforming type III OI in humans and also exhibits deficits in muscle mass and function,21 we demonstrate that ACVR2B can increase both bone and muscle mass in OI, possibly providing a new therapeutic alternative where so few currently exist.
Materials and methods
Animal studies
Heterozygous oim/+ mice (B6C3Fe a/a-Col1a2oim/J; Jackson Laboratory, Bar Harbor, ME, USA) were bred to produce homozygous oim/oim (oim) mice and wild type littermate controls (wild-type (WT)). As previous studies reported no difference in skeletal muscle phenotype between sexes, only male mice were used in the present study.21 The soluble activin receptor (ACVR2B) is a fusion protein containing the extracellular domain of activin receptor 2B linked to a murine Fc domain. The methods for expression and purification of ACVR2B have been previously described.22 Twelve-week-old WT and oim mice were treated with ACVR2B (10 mg·kg−1, intraperitoneal injection) or vehicle control once per week for 4 weeks prior to euthanasia and tissue harvest (WT, n=5; WT+ACVR2B, n=5; oim, n=11; oim+ACVR2B, n=11). All animal studies were performed in accord with established protocols approved by the Animal Care and Use Committee at the Johns Hopkins University School of Medicine.
Skeletal analysis
Femora were harvested and bone volume was assessed using a desktop microtomographic imaging system (Skyscan 1172; Skyscan, Kontich, Belgium) at the Center for Musculoskeletal Research at Johns Hopkins University. Histological analyses, using a semi-automated method (Osteoplan II, Kontron), were carried out in the Department of Nephrology, Bone and Mineral Metabolism at the University of Kentucky. All analyses of bone structure—both μCT and histomorphometry—were completed in accordance with the recommendations of the American Society for Bone and Mineral Research.23,24
Muscle analysis
Pectoralis, triceps, quadriceps and gastrocnemius muscles were harvested to measure wet weights of various muscle groups. For measurement of muscle weights, individual muscles from both sides of the animal were dissected, and the average weight was used for the value of each muscle weight for that animal.
Statistical analysis
All values are expressed as a mean±standard error of the mean. All statistical analyses were performed using the Microsoft Excel data analysis program for ANOVA or Student’s t-test analysis with an assigned significance level of 0.05 (α).
Results
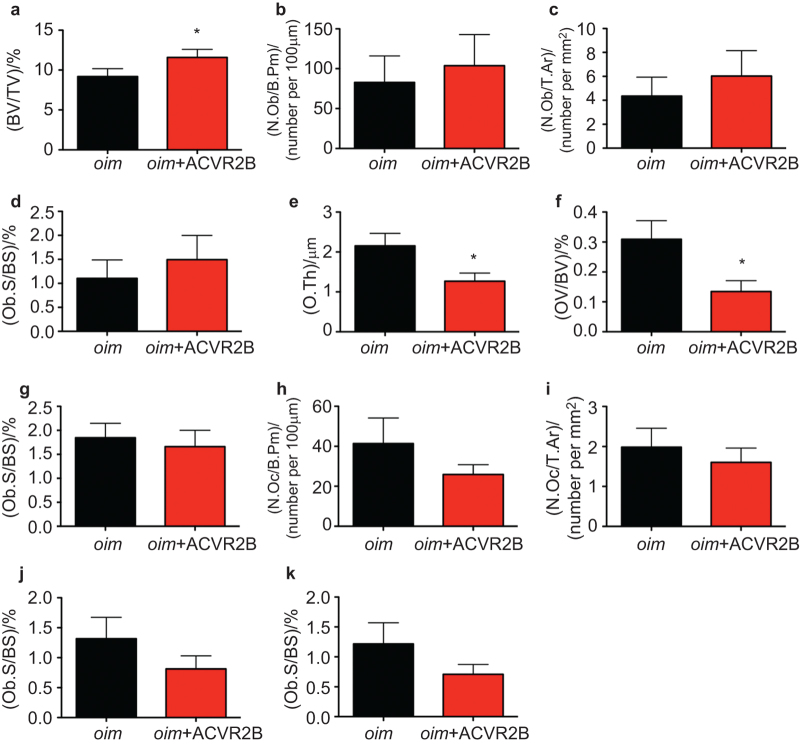
In order to assess the therapeutic efficacy of a dual anabolic (muscle and bone) treatment in OI, 12-week-old WT and oim/oim (oim) mice were treated with a soluble activin receptor 2B (ACVR2B) at 10 mg·kg−1 or vehicle via intraperitoneal injection, once per week, for 4 weeks. μCT analysis of the distal femur revealed a significant increase in trabecular bone volume, trabecular thickness and trabecular number in ACVR2B treated oim mice (Figure 1) similar to increases observed in WT mice receiving ACVR2B (Supplementary Figure S1).
Figure 1.
Administration of ACVR2B increases bone volume in oim mice. μCT analysis of trabecular bone in the distal femur of 16-week-old oim mice following 4 weeks of treatment with ACVR2B (10 mg·kg−1 i.p., 1×/week) or vehicle control. (a) Bone volume fraction; (b) trabecular thickness; (c) trabecular number; (d) trabecular separation.
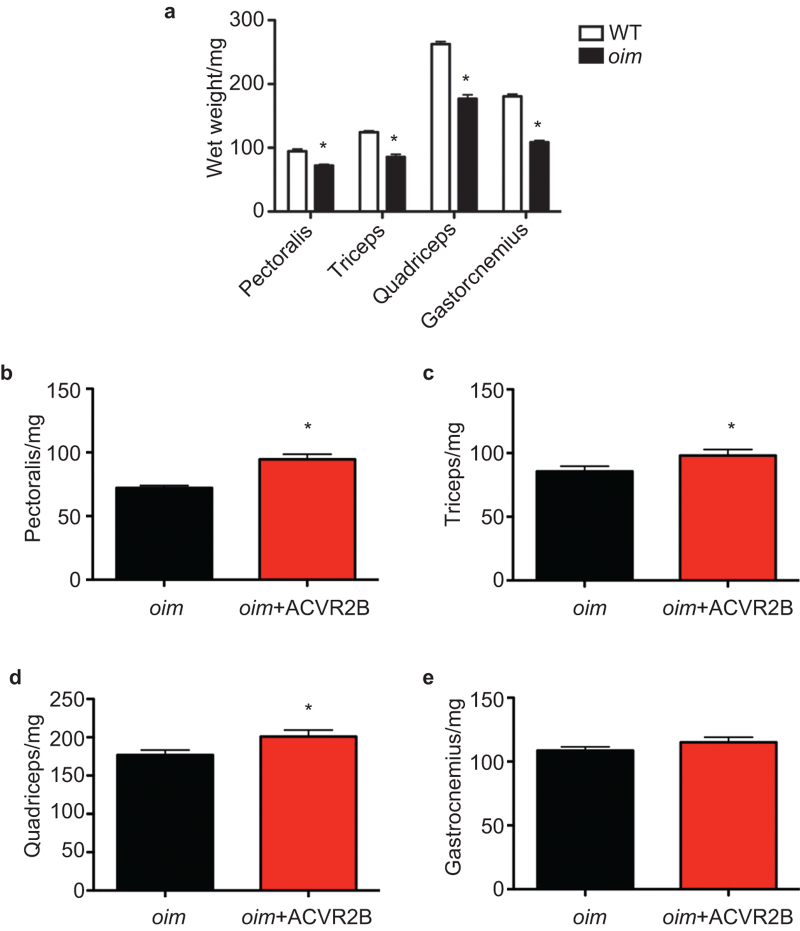
To further analyze the anabolic effect of ACVR2B treatment in the skeleton of the oim mice, histomorphometric analysis was performed in the distal femur. Histomorphometry confirmed the bone volume increase observed in ACVR2B treated oim mice by μCT analysis (Figure 2a). We also observed significantly reduced osteoid volume and thickness in ACVR2B-treated oim mice compared to controls (Figure 2e and 2f), suggesting that the increased bone volume may result from improved osteoblast mineralization, consistent with our previous findings.12 Osteoblast numbers tended to increase in ACVR2B-treated oim mice, although these values did not reach significance, as observed in their WT counterparts treated with ACVR2B (Supplementary Figure S2a–2c), likely due to variability in remodeling as a result of fractures in these severely affected OI mice.
Figure 2.
Administration of ACVR2B reduces osteoid volume while increasing bone volume in oim mice. Histomorphometric analysis of trabecular bone in the distal femur of 16-week-old oim mice following 4 weeks of treatment with ACVR2B (10 mg·kg−1 i.p., 1×/week) or vehicle control. (a) Bone volume; (b) osteoblast number per bone perimeter; (c) osteoblast number per tissue area; (d) osteoblast surface; (e) osteoid thickness; (f) osteoid volume; (g) osteoid surface; (h) osteoclast number per bone perimeter; (i) osteoclast number per tissue area; (j) eroded surface; (k) osteoclast surface.
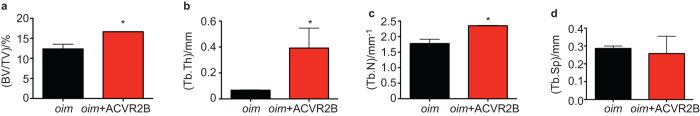
We next examined the effect of ACVR2B administration on skeletal muscle in oim mice. Consistent with previous findings,21 oim mice had significantly lower muscle weights than WT mice across all muscle groups examined (Figure 3a). ACVR2B treatment was able to significantly increase muscle weight in the pectoralis, triceps, and quadriceps of oim mice (Figure 3b–3d), but failed to show a significant effect in the gastrocnemius (Figure 3e). Interestingly, the magnitude of increase in pectoralis weight of ACVR2B treated oim mice (Figure 3a) was similar to that of WT mice treated with ACVR2B (Supplementary Figure S3a), while the anabolic effect of ACVR2B treatment in the limb muscles of oim mice (Figure 3b–3d) was less pronounced than that observed in ACVR2B treated WT mice (Supplementary Figure S3b–3d).
Figure 3.
Administration of ACVR2B improves the reduced muscle mass observed in oim mice. Wet weights of skeletal muscle groups dissected from 16-week-old oim mice following 4 weeks of treatment with ACVR2B (10 mg·kg−1 i.p., 1×/week) or vehicle control. (a) Muscle mass is reduced in oim mice compared to WT in all muscle groups examined. Treatment with ACVR2B increases muscle mass in oim mice in the (b) pectoralis, (c) triceps, (d) quadriceps, but not the (e) gastrocnemius.
Discussion
Osteogenesis imperfecta is a debilitating disease with relatively few clinical interventions. Prior to the introduction of bisphosphonate treatment over 25 years ago,25 orthopaedic surgery and physiotherapy were the sole course of treatment for patients with OI. During this time, patients with OI suffered significantly higher rates of fracture, progressive deformity and immobility. Treatment with bisphosphonates has provided significant improvement in the quality of life of patients with OI, providing reduced bone pain, reduced rates of fracture and subsequent deformity, improved longitudinal growth, better mobility, and an improved sense of well-being in these patients.26 Bisphosphonate treatment, despite all those positives, is not without its drawbacks. Prolonged use of bisphosphonates in children can result in impaired metaphyseal modeling, resulting in widened metaphyses and characteristic radiographic lines of unresorbed calcified cartilage from the growth plate.27 Moreover, the junction between denser, bisphosphonate-treated bone and the less dense bone produced after discontinuation of therapy may be more prone to fracture.28 Finally, the reduction of bone turnover by bisphosphonates can also impair bone repair in patients undergoing corrective osteotomy.29 Thus, despite providing considerable improvement in quality of life for children with OI over surgery and physiotherapy alone, additional therapeutic options are sought.
In the present study, we examined the ability of a soluble activin receptor to improve both bone and muscle mass in a mouse model of type III OI. We believe that such a dual anabolic strategy would be ideal for the setting of OI, where low bone mass and fracture lead to reduced physical activity, which results in muscle atrophy and further reduction in bone mass, further predisposing to fracture, and so on. Indeed, physical activity programs are highly encouraged to prevent contracture and reduce immobility-induced bone loss in patients with OI,30 but in some patients, the risk of fracture—or progression of disease—is too great to accomplish meaningful levels of activity. It is in these patients that such a dual anabolic treatment is most attractive, as one would be able to increase bone and muscle mass to a point that would allow effective physiotherapy, improved mobility, and ultimately, improved quality of life. It is for this reason that we chose to evaluate the efficacy of ACVR2B treatment in a mouse model of the most severe (type III) OI.
Indeed, treating oim mice with ACVR2B was able to significantly increase both bone and muscle mass. Despite starting with a significant deficit in bone mass, the anabolic effect of ACVR2B on the skeleton of oim mice was equal in magnitude to that observed in WT littermates, which is especially encouraging given the severity of disease in these animals. While ACVR2B treatment only partially rescued the deficit in bone mass observed in oim mice, this may be further improved by increasing the duration and/or dose of treatment. Moreover, ACVR2B dramatically increased trabecular thickness in oim mice (Figure 1b). This is in contrast to the mechanism by which bisphosphonates increase bone mass in OI, i.e., the number of abnormally thin trabeculae is increased by inhibition of resorption of the primary trabeculae during the transition to secondary spongiosa with endochondral growth.26 Presumably, the increase of both trabecular number and thickness should result in even greater mechanical benefit than would just the increase in trabecular number seen with bisphosphonate treatment. Unfortunately, we were unable to observe any significant difference in mechanical properties between ACVR2B-treated and vehicle-treated oim mice by three-point-bend testing, as the bones of the oim mice were almost all afflicted with at least one fracture in various states of healing (data not shown). While the precise molecular mechanism(s) by which inhibition of activin receptor signaling exerts anabolic effects in bone has yet to be defined, the efficacy of targeting this pathway to improve bone has been demonstrated in numerous settings 16,31–33. Previous studies have demonstrated that BMP3 signaling through ACVR2B can inhibit osteoblast differentiation and mineralization.34 More recently, however, Bialek and colleagues31 treated Bmp3−/− mice with a soluble ACVR2B and observed further increases in bone volume in these mice, suggesting that additional TGF-β family members are also involved in regulating osteoblast function through the activin receptors.
As in the bone, oim mice also began treatment with ACVR2B with a significant deficit in muscle mass compared to their WT littermates. Interestingly, and by contrast to the effect of ACVR2B on the bone of oim mice, ACVR2B did not increase muscle mass in the oim mice to as great an extent as observed in healthy control animals (Figure 3b–3e vs. Supplementary Figure S3), with the exception of the pectoralis. One possible explanation for this difference may stem from the fact that the other three muscles examined are located in the extremities and have experienced selectively greater disuse atrophy than the pectoralis as a result of the numerous fractures observed in the long bones of the oim mice. Importantly for our proof of concept; however, ACVR2B was still able to improve muscle mass in these muscle groups.
While the effects of OI may be most pronounced and induce the greatest morbidity in patients through the skeletal manifestations of the disease, it is important to consider the entire musculoskeletal system in the approach to treating the disorder. Skeletal muscle is also negatively affected in OI, both by the disease directly, and secondarily, by the eventual loss of mobility due to recurrent fracture and/or surgical treatment. Moreover, improving muscle mass can have a multitude of positive secondary effects on bone via increased mechanical force, paracrine/endocrine signaling, etc. Thus, simultaneously improving both bone and skeletal muscle, as we have demonstrated by targeting the activin signaling pathway with ACVR2B, represents an exciting and promising new approach to treating the deleterious consequences of OI in the musculoskeletal system.
Acknowledgments
Research reported in this publication was supported by NIAMS, of the National Institutes of Health, under award numbers R01AR062074 (to DJD) and R01AR060636 (to S-JL) and the Harry Headley Charitable and Research Foundation, Punta Gorda, FL (to ELG-L). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors declare no conflict of interest.
References
- Cundy T. Recent advances in osteogenesis imperfecta. Calcif Tissue Int 2012; 90: 439–449. [DOI] [PubMed] [Google Scholar]
- Eyre DR, Weis MA. Bone collagen: new clues to its mineralization mechanism from recessive osteogenesis imperfecta. Calcif Tissue Int 2013; 93: 338–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 1979; 16: 101–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sillence DO, Lamande SR. Evolution of the present understanding of the clinical and genetic heterogeneity and molecular and biochemical basis of osteogenesis imperfecta. In: Shapiro J, Byers P, Glorieux F, Sponseller P (ed.), Osteogenesis Imperfecta. New York: Elsevier Academic Press 2014: 5–14. [Google Scholar]
- Boot AM, de Coo RF, Pals G, de Muinck Keizer-Schrama SM. Muscle weakness as presenting symptom of osteogenesis imperfecta. Eur J Pediatr 2006; 165: 392–394. [DOI] [PubMed] [Google Scholar]
- Caudill A, Flanagan A, Hassani S et al. Ankle strength and functional limitations in children and adolescents with type I osteogenesis imperfecta. Pediatr Phys Ther 2010; 22: 288–295. [DOI] [PubMed] [Google Scholar]
- Takken T, Terlingen HC, Helders PJ, Pruijs H, van der Ent CK, Engelbert RH. Cardiopulmonary fitness and muscle strength in patients with osteogenesis imperfecta type I. J Pediatr 2004; 145: 813–818. [DOI] [PubMed] [Google Scholar]
- Veilleux LN, Lemay M, Pouliot-Laforte A, Cheung MS, Glorieux FH, Rauch F. Muscle anatomy and dynamic muscle function in osteogenesis imperfecta type I. J Clin Endocrinol Metab 2014; 99: E356–E362. [DOI] [PubMed] [Google Scholar]
- Brizola E, Staub AL, Felix TM. Muscle strength, joint range of motion, and gait in children and adolescents with osteogenesis imperfecta. Pediatr Phys Ther 2014; 26: 245–252. [DOI] [PubMed] [Google Scholar]
- McPherron AC, Lawler AM, Lee SJ. Regulation of skeletal muscle mass in mice by a new TGF-beta superfamily member. Nature 1997; 387: 83–90. [DOI] [PubMed] [Google Scholar]
- Bowser M, Herberg S, Arounleut P et al. Effects of the activin A-myostatin-follistatin system on aging bone and muscle progenitor cells. Exp Gerontol 2013; 48: 290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digirolamo D, Singhal V, Clemens T, Lee SJ. Systemic administration of soluble 483 activin receptors produces differential anabolic effects in muscle and bone in mice. J Bone Miner Res 2011; 26 (Suppl 1). [Google Scholar]
- Hamrick MW. Increased bone mineral density in the femora of GDF8 knockout mice. Anat Rec A Discov Mol Cell Evol Biol 2003; 272: 388–391. [DOI] [PubMed] [Google Scholar]
- Kellum E, Starr H, Arounleut P et al. Myostatin (GDF-8) deficiency increases fracture callus size, Sox-5 expression, and callus bone volume. Bone 2009; 44: 17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang ZL, He JW, Qin YJ et al. Association between myostatin gene polymorphisms and peak BMD variation in Chinese nuclear families. Osteoporos Int. 2008; 19: 39–47. [DOI] [PubMed] [Google Scholar]
- Koncarevic A, Cornwall-Brady M, Pullen A et al. A soluble activin receptor type IIb prevents the effects of androgen deprivation on body composition and bone health. Endocrinology 2010; 151: 4289–4300. [DOI] [PubMed] [Google Scholar]
- Bogdanovich S, Krag TO, Barton ER et al. Functional improvement of dystrophic muscle by myostatin blockade. Nature 2002; 420: 418–421. [DOI] [PubMed] [Google Scholar]
- Zhou X, Wang JL, Lu J et al. Reversal of cancer cachexia and muscle wasting by ActRIIB antagonism leads to prolonged survival. Cell 2010; 142: 531–543. [DOI] [PubMed] [Google Scholar]
- Chiu CS, Peekhaus N, Weber H et al. Increased muscle force production and bone mineral density in ActRIIB-Fc-treated mature rodents. J Gerontol A Biol Sci Med Sci 2013; 68: 1181–1192. [DOI] [PubMed] [Google Scholar]
- DiGirolamo DJ, Kiel DP, Esser KA. Bone and skeletal muscle: neighbors with close ties. J Bone Miner Res 2013; 28: 1509–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentry BA, Ferreira JA, McCambridge AJ, Brown M, Phillips CL. Skeletal muscle weakness in osteogenesis imperfecta mice. Matrix Biol 2010; 29: 638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Reed LA, Davies MV et al. Regulation of muscle growth by multiple ligands signaling through activin type II receptors. Proc Natl Acad Sci USA 2005; 102: 18117–18122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Muller R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 2010; 25: 1468–1486. [DOI] [PubMed] [Google Scholar]
- Dempster DW, Compston JE, Drezner MK et al. Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 2013; 28: 2–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devogelaer JP, Malghem J, Maldague B, Nagant de Deuxchaisnes C. Radiological manifestations of bisphosphonate treatment with APD in a child suffering from osteogenesis imperfecta. Skeletal Radiol 1987; 16: 360–363. [DOI] [PubMed] [Google Scholar]
- Rauch F, Glorieux FH. Osteogenesis imperfecta. Lancet 2004; 363: 1377–1385. [DOI] [PubMed] [Google Scholar]
- Land C, Rauch F, Glorieux FH. Cyclical intravenous pamidronate treatment affects metaphyseal modeling in growing patients with osteogenesis imperfecta. J Bone Miner Res 2006; 21: 374–379. [DOI] [PubMed] [Google Scholar]
- Rauch F, Cornibert S, Cheung M, Glorieux FH. Long-bone changes after pamidronate discontinuation in children and adolescents with osteogenesis imperfecta. Bone 2007; 40: 821–827. [DOI] [PubMed] [Google Scholar]
- Munns CF, Rauch F, Zeitlin L, Fassier F, Glorieux FH. Delayed osteotomy but not fracture healing in pediatric osteogenesis imperfecta patients receiving pamidronate. J Bone Miner Res 2004; 19: 1779–1786. [DOI] [PubMed] [Google Scholar]
- Zeitlin L, Fassier F, Glorieux FH. Modern approach to children with osteogenesis imperfecta. J Pediatr Orthop B 2003; 12: 77–87. [DOI] [PubMed] [Google Scholar]
- Bialek P, Parkington J, Li X et al. A myostatin and activin decoy receptor enhances bone formation in mice. Bone 2014; 60: 162–171. [DOI] [PubMed] [Google Scholar]
- Fajardo RJ, Manoharan RK, Pearsall RS et al. Treatment with a soluble receptor for activin improves bone mass and structure in the axial and appendicular skeleton of female cynomolgus macaques (Macaca fascicularis). Bone 2010; 46: 64–71. [DOI] [PubMed] [Google Scholar]
- Pearsall RS, Canalis E, Cornwall-Brady M et al. A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci USA 2008; 105: 7082–7087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokabu S, Gamer L, Cox K et al. BMP3 suppresses osteoblast differentiation of bone marrow stromal cells via interaction with Acvr2b. Mol Endocrinol 2012; 26: 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.