Abstract
Study Design Case report.
Objective The purpose of the present case report was to present a patient with a history of ankylosing spondylitis who sustained a dislocation of C6 on C7 and died soon after his presentation in the emergency room (ER).
Methods An 88-year-old man was brought to the ER due to a neck injury secondary to a fall. Imaging of the cervical spine revealed anterior dislocation of C6 on C7 and the characteristic “bamboo” spine of ankylosing spondylitis.
Results The patient died within 30 minutes due to respiratory insufficiency.
Conclusion Isolated cervical spine injuries in patients with ankylosing spondylitis can be fatal. A high degree of clinical suspicion, thorough imaging with computed tomography, and meticulous handling are required in this patient population.
Keywords: cervical spine, dislocation, ankylosing spondylitis, respiratory insufficiency
Introduction
Isolated cervical spine trauma is rare in elderly people. These injuries are usually combined with other injuries (e.g., brain and thoracic injuries) as a result of motor vehicle accidents or falls. The clinical and/or radiographic findings vary after a cervical spine injury depending on many factors, such as the severity of the injury, the presence of spinal cord injury, the age of the patient, the time of arrival in the emergency room (ER), and the presence of comorbidities.
Cervical spine injuries in patients with ankylosing spondylitis are associated with greater mortality and morbidity regardless of the treatment used. The purpose of this report is to present a rare case of an 88-year-old man with ankylosing spondylitis who sustained a dislocation of C6 on C7 and died minutes after his presentation in the ER.
The study was approved by the University Hospital of Ioannina ethics committee.
Case Report
An 88-year-old man was brought to the ER due to a neck injury secondary to a fall. The patient was transferred without a neck collar to the hospital by his relatives in a car. Upon his arrival in the ER, he was conscious with muscle strength of 2 of 5 in the upper extremities and 2 of 5 in the lower extremities, according to the Medical Research Council muscle grading scale. No Achilles and no patella reflexes could be obtained, and the Babinski sign was positive bilaterally. In the upper extremities, the triceps reflex was present and symmetric but not the biceps bilaterally. Sensitivity was absent below the level of the nipples.
The patient was on warfarin due to chronic atrial fibrillation and his international normalized ratio was 5. Immediately after the arrival of the patient in the ER, he was started on intravenous steroids. Imaging of the cervical spine revealed anterior dislocation of C6 on C7 and the characteristic “bamboo” spine of ankylosing spondylitis (Figs. 1 and 2). The patient died within 30 minutes due to respiratory insufficiency.
Fig. 1.
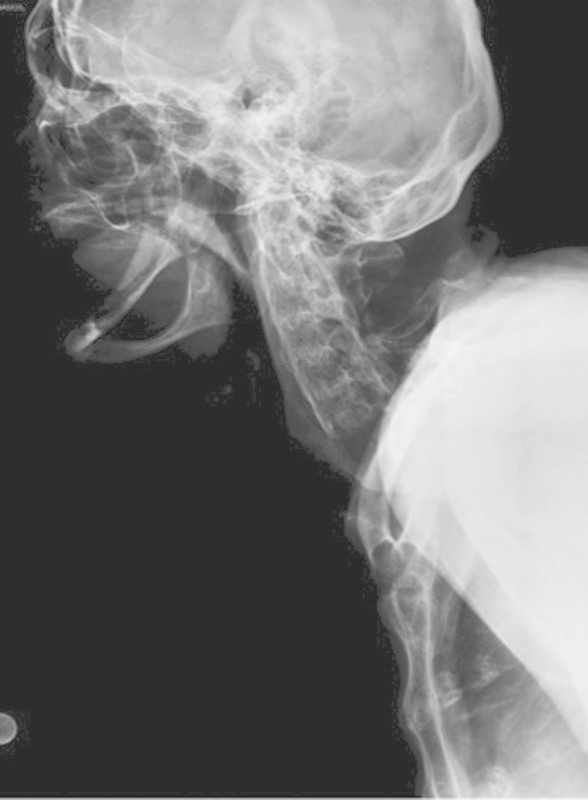
Lateral film of the cervical spine showing the dislocation of C6 on C7.
Fig. 2.

Sagittal view of the cervical spine on computed tomography (CT) scan showing the anterior dislocation of C6 on C7. The ankylotic vertebras C7, T1, and T2 are clearly shown on CT.
Discussion
Isolated cervical spine injury in elderly people is a rare condition. The data from the literature is limited because of the combination of cervical spine trauma with other injuries as a result of major accidents. Older patients with comorbidities tend to have increased injury severity status compared with younger patients with cervical spine trauma, regardless of the fact that younger patients are more commonly involved in higher-energy injuries than the elderly.1 2 3 4 5 6 7
Ankylosing spondylitis involves chronic inflammation, which leads to disorders mainly in the spine and the sacroiliac joints.8 One of the main findings of the disease in the spine is the ossification of the soft tissues, mainly the ligaments and the disks. This abnormal ossification leads to biomechanical alterations in patients with ankylosing spondylitis, and these patients tend to suffer from spinal fractures even with low-energy injuries.9 10 11 After trauma in these patients, a fixed kyphotic disorder is commonly observed; the most common injury in the spinal column is observed around the C5 and C7 segments, with neurologic deficits for the patients.12 13
Immobilization of the injured patient with ankylotic spondylitis must be done with great care. Neurologic deterioration can have a rapid onset or can develop gradually in the first few hours. Etgen and Rieder reported on a patient with ankylotic spine who presented with a C4 fracture without any neurologic deficits after a minor fall.14 During regular X-ray positioning, he developed severe bradycardia and had to be resuscitated. The early manifestation of neurogenic shock with bradycardia and hypotension is unusual in cervical cord injury, as <20% of patients display classical neurogenic shock upon arrival in the ER. The authors suggest that the bone fragments compressing the spinal column triggered the early bradyarrhythmia.
Spinal cord injury on the level of the cervical spine is not only associated with motor and sensory deficits but also goes hand in hand with respiratory disorders.15 The deficits in the respiratory system after trauma in the spinal cord have been well reported and reviewed by Mansel and Norman,16 who emphasize the different innervations of the inspiratory (higher cervical spinal cord C4 and above) and expiratory (innervations below C5) muscles. From electromyographic findings, it is suggested that a great part of the active expiration in patients with cervical spinal cord trauma is provided by the clavicular portion of the pectoralis major muscle. In another study, Roth et al reported that in patients with trauma in cervical and high thoracic spinal cord, a decrease in the strength of the muscles of the chest is documented with simultaneous increase in the muscle tone for these patients.17 These factors are implicated in the diminished function of the respiratory system observed in patients with cervical and high thoracic spinal cord injuries.
Conclusion
Isolated cervical spine injuries in patients with ankylosing spondylitis can be fatal. A high degree of clinical suspicion, thorough imaging with computed tomography, and meticulous handling are required in this patient population.
Footnotes
Disclosures Ioannis D. Gelalis, none Marios G. Lykissas, none Apostolos A. Dimou, none Dionysios K. Giannoulis, none Alexandros E. Beris, none
Editorial Perspective
To report on unfavorable outcomes, such as complications and especially death of a patient, requires uncommon courage on the part of the authors. Credit goes to the authors and the invited commentator Dr. Bransford, who brought this important and increasingly common patho-entity to our attention in a straightforward and unambiguous fashion. As pointed out in the poignant commentary, the constellation of an ankylosed spine and spine fracture(s) is challenging to diagnose and even more daunting to treat, especially if the patient has had a significant baseline deformity such as a significant kyphosis. Anyone charged with treatment of these conditions is also tasked to take into account and manage the multitude of comorbidities these patients usually present with and the high morbidity and mortality these patient face regardless of treatment. Based on the numbers presented in the commentary of Dr. Bransford, it appears reasonable to calculate morbidity and mortality rates for these patients in a different category from other spine trauma. With the changing age demographics of our planet in clear sight, it is safe to assume that we can expect a steady rise of similar cases over many years to come.
EBSJ would like to highlight two other points: absence of a reduction protocol and respiratory implications of cervical spinal cord injuries.
The discussion about the value of timing of closed reduction for a cervical spine dislocation relative to getting magnetic resonance imaging for patients with and without spinal cord injury has been going on for over 20 years, with a general practice consensus slowly emerging in the more recent years. All of these closed reduction algorithms can pretty much considered ill-advised for patients with ankylosing disorders and especially with concurrent deformity. As mentioned in the commentary, a straight recumbent positioning of a neurologically intact patient with kyphotically ankylosed cervicothoracic spine is likely to induce displacement of any fracture in a frozen spinal column. Positioning in a semiupright position of comfort in an awake patient supported by cushions and pillows seems much more appropriate for this circumstance. For patients with a complete spinal cord injury, it remains desirable to try to get neuroimaging if possible followed by rapid surgical realignment and stabilization. However, the severity of spinal deformities afflicting many of patients with ankylosing spine frequently makes any form of advanced neuroimaging difficult if not outright impossible. Finally, a patient with an incomplete and likely ascending spinal cord injury, such as was described in this case, creates an almost prohibitive added layer of difficulty. All other mentioned challenges aside, early surgical intervention for a true surgical emergency, such as this case theoretically constitutes, becomes seriously challenging in the face of frequent poorly controlled comorbidities, such as described in this case with anticoagulation. The AOSpine community with its global Spine Trauma Knowledge Forum seeks to address these issues of offering improved and validated ways of classifying and weighting the magnitude of such cervical spine injuries with its upcoming Cervical Spine Injury Scoring System. In the absence of immediate solutions to the growing challenge of serious spine injuries in patients with ankylosing disorders, we have an opportunity to raise awareness of the susceptibility of patients with these disorders to sustain unstable serious spine injuries from frequently trivial mechanisms. Awareness needs to be raised in medical specialties such as emergency medicine, radiologists, and emergency responders, as these pathologies will present more commonly in the future.
We will never completely know what the exact cause of death of the patient described in this case report was. Was it a primary respiratory insufficiency due to a differential air-exchange problem as hypothesized by the authors, or was it an ascending epidural hematoma as outlined by Dr. Bransford? Without additional information, we will likely never fully know. This discussion, however, underscores the importance of trying to secure a rapid safe airway in a patient with an unstable kyphotically ankylosed spine. For the reasons stated by the authors and the commentator, patients with ankylosing spines are very much at risk for respiratory decompensation. Expedient decision making and decisive interventions directed at effective decompression, stabilization, and mobilization of the affected patient remains the treatment algorithm offering the best chances for survival and recovery of the patient.
EBSJ hopes that this case report and the ensuing discussions will spur further commentary and investigations by its readers around the world.
References
- 1.Spivak J M, Weiss M A, Cotler J M, Call M. Cervical spine injuries in patients 65 and older. Spine (Phila Pa 1976) 1994;19(20):2302–2306. doi: 10.1097/00007632-199410150-00009. [DOI] [PubMed] [Google Scholar]
- 2.Bergeron E, Clement J, Lavoie A. et al. A simple fall in the elderly: not so simple. J Trauma. 2006;60(2):268–273. doi: 10.1097/01.ta.0000197651.00482.c5. [DOI] [PubMed] [Google Scholar]
- 3.Grossman M D, Miller D, Scaff D W, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J Trauma. 2002;52(2):242–246. doi: 10.1097/00005373-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Hannan E L, Waller C H, Farrell L S, Rosati C. Elderly trauma inpatients in New York state: 1994–1998. J Trauma. 2004;56(6):1297–1304. doi: 10.1097/01.ta.0000075350.66739.53. [DOI] [PubMed] [Google Scholar]
- 5.Inaba K, Goecke M, Sharkey P, Brenneman F. Long-term outcomes after injury in the elderly. J Trauma. 2003;54(3):486–491. doi: 10.1097/01.TA.0000051588.05542.D6. [DOI] [PubMed] [Google Scholar]
- 6.McGwin G Jr, MacLennan P A, Fife J B, Davis G G, Rue L W III. Preexisting conditions and mortality in older trauma patients. J Trauma. 2004;56(6):1291–1296. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 7.Tornetta P III, Mostafavi H, Riina J. et al. Morbidity and mortality in elderly trauma patients. J Trauma. 1999;46(4):702–706. doi: 10.1097/00005373-199904000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Apley A G, Solomon L. Oxford, UK: Butterworth Heinemann; 1995. Apley's System of Orthopaedics and Fractures. 7th ed; pp. 54–72. [Google Scholar]
- 9.Hitchon P W From A M Brenton M D Glaser J A Torner J C Fractures of the thoracolumbar spine complicating ankylosing spondylitis J Neurosurg 200297(2, Suppl):218–222. [DOI] [PubMed] [Google Scholar]
- 10.Gartman J J Jr Bullitt E Baker M L Axis fracture in ankylosing spondylitis: case report Neurosurgery 1991294590–593., discussion 593–594 [DOI] [PubMed] [Google Scholar]
- 11.Wade W, Saltzstein R, Maiman D. Spinal fractures complicating ankylosing spondylitis. Arch Phys Med Rehabil. 1989;70(5):398–401. [PubMed] [Google Scholar]
- 12.Young J S, Cheshire J E, Pierce J A, Vivian J M. Cervical ankylosis with acute spinal cord injury. Paraplegia. 1977;15(2):133–146. doi: 10.1038/sc.1977.19. [DOI] [PubMed] [Google Scholar]
- 13.Surin V V. Fractures of the cervical spine in patients with ankylosing spondylitis. Acta Orthop Scand. 1980;51(1):79–84. doi: 10.3109/17453678008990772. [DOI] [PubMed] [Google Scholar]
- 14.Etgen T, Rieder G. Fatality from minor cervical trauma in ankylosing spondylitis. BMJ Case Rep. 2009;2009(8):1400. doi: 10.1136/bcr.12.2008.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hassid V J, Schinco M A, Tepas J J. et al. Definitive establishment of airway control is critical for optimal outcome in lower cervical spinal cord injury. J Trauma. 2008;65(6):1328–1332. doi: 10.1097/TA.0b013e31818d07e4. [DOI] [PubMed] [Google Scholar]
- 16.Mansel J K, Norman J R. Respiratory complications and management of spinal cord injuries. Chest. 1990;97(6):1446–1452. doi: 10.1378/chest.97.6.1446. [DOI] [PubMed] [Google Scholar]
- 17.Roth E J, Lu A, Primack S. et al. Ventilatory function in cervical and high thoracic spinal cord injury. Relationship to level of injury and tone. Am J Phys Med Rehabil. 1997;76(4):262–267. doi: 10.1097/00002060-199707000-00002. [DOI] [PubMed] [Google Scholar]


