Abstract
Objective
To determine the impact of varying ADHD diagnostic criteria, including new DSM-5 criteria, on prevalence estimates.
Method
Parent and teacher reports identified ADHD high and low screen children from elementary schools in two states that produced a diverse overall sample. The parent interview stage included the Diagnostic Interview Schedule for Children – IV (DISC-IV), and up to four additional follow-up interviews. Weighted prevalence estimates, accounting for complex sampling, quantified the impact of varying ADHD criteria using baseline and the final follow-up interview data.
Results
At baseline 1060 caregivers were interviewed; 656 had at least one follow-up interview. Teachers and parents reported six or more ADHD symptoms for 20.5% (95% CI: 18.1%–23.2%) and 29.8% (CI: 24.5%–35.6%) of children respectively, with criteria for impairment and onset by age seven (DSM-IV) reducing these proportions to 16.3% (CI: 14.7%–18.0%) and 17.5% (CI: 13.3%–22.8%); requiring at least four teacher-reported symptoms reduced the parent-reported prevalence to 8.9% (CI: 7.4%–10.6%). Revising age of onset to 12 years per DSM-5 increased this estimate to 11.3% (CI: 9.5%–13.3%), with a similar increase seen at follow-up: 8.2% with age seven onset (CI: 5.9%–11.2%) versus 13.0% (CI: 7.6%–21.4%) with onset by age 12. Reducing the number of symptoms required for those aged 17 and older increased the estimate to 13.1% (CI: 7.7%–21.5%).
Conclusion
These findings quantify the impact on prevalence estimates of varying case definition criteria for ADHD. Further research of impairment ratings and data from multiple informants is required to better inform clinicians conducting diagnostic assessments. DSM-5 changes in age of onset and number of symptoms required for older adolescents appear to increase prevalence estimates, although the full impact is uncertain due to the age of our sample.
Keywords: ADHD, diagnostic criteria, DSM-5, impairment, age of onset
I. Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) is described as the most common neurodevelopmental disorder of childhood;1,2 however, prevalence estimates vary, given their sensitivity to factors such as the period of study,3 country or region of the country,3–6 and research methods,7,8 though a recent meta-analysis has disputed the variability for studies using standardized procedures over time.9 In the U.S., rates are higher in the South and Midwest;3 however, even where prevalence estimates vary across regions, trends may be similar. Different study settings result in varying estimates, with clinic-based studies differing from community-based studies in both prevalence and case mix. The direction of differences depends on the denominator used for clinical studies, but clinic-based studies tend to reflect more severe cases with greater comorbidity.10–13 Additionally, studies using different methods and case definitions, such as those that utilize administrative data and parent surveys, report different point estimates, yet similar upward trends in the prevalence of ADHD;14,15 however, once sample selection parameters are made comparable, estimates may become similar.16
ADHD terminology and criteria have undergone substantial revision over time starting with Hyperkinetic Reaction of Childhood in the Diagnostic and Statistical Manual of Mental Disorders (DSM) 2nd edition, then Attention Deficit Disorder with or without hyperactivity in DSM-III.17 In DSM-III-R, subtypes were removed and the diagnosis was ADHD, without further specification.18 Three subtypes were created in DSM-IV (inattentive, hyperactive/impulsive, and combined), reframed as presentation specifiers in DSM-5.1,19,20
Alongside changing terminology, diagnostic criteria have changed over DSM’s four revisions with direct impact on diagnosis and estimates of prevalence. The most marked changes occurred with the more clearly described disorder of inattentiveness with or without hyperactivity in DSM-III,17 followed by delineated subtypes in DSM-IV.19 The impact of modifications to the ADHD criteria in DSM-51 has yet to be realized; particularly with regard to age of onset and criteria for older adolescents and adults, though a recent study examined the change in age of onset in a cross-sectional national sample and concluded increased case finding with comparable clinical significance validated the change.21 Due to the variability in prevalence across study types and settings noted above, investigations of the impact of case definition on prevalence estimates is important.
In DSM-IV and DSM-5, ADHD diagnosis requires meeting symptom count criteria and exhibiting impaired functioning in at least two settings. DSM-IV stated there must be “some impairment” related to the symptoms in two or more settings and that there must be “clear evidence of clinically significant impairment”. DSM-IV noted that clinicians should obtain information from multiples sources. DSM-5 requires that several symptoms22 be present before age 12, that they be evident in more than one setting, and that they impair functioning. DSM-5 asserts that reliably ascertaining symptoms and impairment in multiple settings would be difficult without multiple informants, but both editions stop short of explicitly requiring multiple informants. The challenges of collecting data from multiple informants include the difficulty of obtaining information from teachers, while respecting privacy concerns, regulations, and time constraints, as well as the difficulty of resolving disagreement between informants,23,24 raising concerns about the value of investing resources in obtaining data from other informants. Depending on how information is combined, diagnostic rates and prevalence estimates could increase or be attenuated. Barkley25(p. 91) pointed out that DSM-IV criteria “confound settings with sources of information”, and that impairment is the important clinical issue to be ascertained, rather than agreement among informants.
Further, standard research instruments do not couch impairment classification in the terms used in DSM-IV criteria, namely, “clinically significant impairment”, instead using terms such as “moderate” and “severe”, as in DSM-5. Translating the level of impairment reported in research data to comparable thresholds for DSM classification has been a challenge. Just as there is no standard for assessing the level of impairment for research diagnostic classification, neither is there a standard metric for clinicians to use in determining level of impairment, especially with the deletion of the Global Assessment of Functioning from DSM-5, which previously served as a common measure of functional impairment.
Another major change in DSM-5 was the increase in the age of onset criterion, which was raised from age seven to 12. The age of onset requirement has been questioned for some time, especially because the inattentive symptoms may be delayed in presentation or more difficult to identify, particularly among females.10,26–28 Understanding the impact of the change in the age of onset criterion is critical for understanding trends in reported ADHD prevalence over the next generation of studies.21
DSM-5 also provides more guidance on diagnosis of ADHD among teens and adults 17 years of age and older, including reducing the number of symptoms required from six to five for that group. If prevalence estimates in adults change, the challenge will be to disentangle (a) age effects (i.e., adolescents newly meeting or no longer meeting criteria as a result of development or treatment) from (b) period effects (i.e., the expanded guidance for adult diagnosis in DSM-5) and from (c) cohort effects (i.e., children and adolescents from later cohorts with higher prevalence rates aging into adulthood).
These issues of variability in prevalence estimates are important because they impact research methodology and clinical practice with regard to diagnosis and treatment. Further, continued wide variability in research reports and in clinical diagnosis can undermine public confidence in reports of ADHD research, delaying their impact or reducing their utility for informing policy and programs.
In light of the foregoing, the objective of this paper is to quantify the impact of varying case definition criteria on prevalence estimates, with focus on symptom and impairment criteria, reliance on two informants for multiple settings, and age of onset. Our primary hypothesis is that each successive additional requirement will result in a clinically meaningful decrease in the proportion classified as having probable ADHD. A secondary objective is to estimate the impact on prevalence estimates of the DSM-5 criterion regarding age of onset for impairing symptoms and reduced number of required symptoms for those aged 17 and older. Our secondary hypothesis is that higher age of onset and lower symptom count for older adolescents and adults will result in more participants meeting diagnostic criteria, thus increasing the prevalence of diagnosed ADHD. We examined these issues using data from the longitudinal Project to Learn about ADHD in Youth.29
II. Methods
Population
The Project to Learn about ADHD in Youth (PLAY) is a community-based epidemiological study to characterize the prevalence and impact of ADHD in school-aged children. Methods and demographic characteristics of the districts and screened sample by site have been previously described.29 Briefly, study participants were selected from public elementary schools in school districts in South Carolina and Oklahoma using a stratified, two-stage sampling design to maximize case-finding and recruit comparable ratios of boys to girls within high and low screen groups. The first stage involved parent and teacher screening in mainstream classrooms (SC N=4,606; OK N=12,626). Parents were asked if their child had ever been diagnosed with ADHD/ADD and if their child was on medication for ADHD/ADD. For each child, teachers completed the Vanderbilt ADHD Diagnostic Teacher Rating Scale (VADTRS)30 in all six school districts and the Strengths and Difficulties Questionnaires (SDQ)31 in four districts. Teachers were also asked two questions about diagnosis and treatment for each child, comparable to those asked of parents. Screening excluded students in self-contained special education classrooms and included kindergarten through 5th grade, with a small number of pre-K students (n=21 in SC and n=37 in OK).
Students with positive responses to the diagnosis and treatment questions from either parent or teacher or whose teachers endorsed at least six inattentive or six hyperactive/impulsive descriptors on the VADTRS and were rated as having at least some impairment on the SDQ or VADTRS were classified as high screen. SDQ data were used where present to determine teacher-reported impairment. For the two OK districts that did not administer the SDQ, VADTRS performance items were used due to good agreement of impairment classification between the SDQ and the VADTRS (based on 86.5% of the sample who had both: κ=0.68). A low screen group was randomly selected from remaining screened students, with proportions by gender equal to proportions in the high screen group. These students constituted the pool eligible for in-depth interviews.
For most children the participating interviewee was the child’s mother (94% in SC, 86% in OK). Data from child interviews were not considered for this report. Interviews included selected modules from the Diagnostic Interview Schedule for Children, version IV (DISC-IV).32 DISC-IV computer algorithms for probable diagnosis were supplemented by additional criteria in initial estimates of ADHD prevalence.29 The case definition required at least two moderate or one severe rating of impairment across six domains. In addition, to meet our ADHD case definition, low screen students had to exhibit at least four teacher-reported symptoms of hyperactivity/impulsivity or inattention as confirmation symptoms were present and problematic in the school setting. Studies at both sites were approved by their respective Institutional Review Boards.
Participants with baseline interviews were eligible for up to four follow-up interview waves in SC and up to two waves in OK beginning approximately four years after the baseline interview wave. Follow-up interviews included the parent and child DISC-IV and parent Vanderbilt ADHD Diagnostic Rating Scale and SDQ, as well as additional assessments. Among respondents 78% in SC (n=373) and 49% in OK (n=283) completed at least one follow-up interview. The median time between baseline interview and last follow-up interview was 6.2 years in SC (interquartile range: 5.6–6.6) and 4.2 years in OK (3.1–5.0). The last follow-up interview for each child is used in these analyses in order to examine the impact of changes to DSM criteria in an older cohort of children (OK median age=13: range 7–18; SC median age=15: range 7–19; overall median age=14).
Weights were developed at each wave that reflected initial participation in the screening, stratified sampling, and non-response over time.29 Analyses were conducted in SAS 9.2 (SAS Institute, Inc., Cary, NC) and SAS-callable SUDAAN 11.0 (RTI International, Research Triangle Park, NC) to account for the sampling design and weighting. The weighted population reflected the composition of the school districts with respect to race, gender, distribution across schools, and screening status at the time of the baseline interview. For a longitudinal analysis of symptom persistence and factors associated with elevated symptom counts, see Holbrook et al.33
Variations in Case Definition
The project case definition was based on the DISC algorithms, with additional requirements reflecting our interpretation of DSM-IV criteria. Those criteria were formulated a priori and previously reported.29 For this report, data from initial teacher and parent screens concerning diagnosis and treatment, teacher report of symptoms and impairment, and parent DISC-IV interviews were used to evaluate the impact on ADHD prevalence estimates of different case definition criteria that might be employed in clinical practice or research studies. The evaluation of varying diagnostic criteria relies primarily on baseline data to which different case definition criteria were applied in succession to explore the impact of each additional criterion. Teacher evaluations were not available for follow-up assessments.
Symptom count criteria
In the first step, to parallel research studies that rely only on teacher-reported symptom counts, estimates reflect rates of (a) teacher report of six or more symptoms, as well as estimates based on (b) the report of at least some impairment due to symptoms, then (c) the effect of requiring both a minimum symptom count and at least some impairment.
Report of diagnosis or treatment
The second step parallels surveys that rely solely on reported diagnosis and treatment, and reflects parent and teacher reports of ADHD diagnosis or treatment, separately and combined.
DSM-based estimates
The third step is patterned after DSM-IV criteria and successively reports proportions in the following order, each conditioned on meeting the prior criterion: (a) six or more parent-reported DISC-IV symptoms, (b) problem onset before age seven, (c) at least two moderate or one severe rating of impairment, and, finally, (d) a second informant (teacher) report of at least four symptoms.
At each stage results are reported as unweighted numbers with weighted percentages and 95% confidence intervals for proportions representing the school population, and unweighted percentages for within-sample comparisons.
Applying DSM-5 Criteria
Age of onset and symptom count data from each participant’s last follow-up interview were used to estimate changes in prevalence due to DSM-5’s revised criteria. Consistent with DSM-5 specification of symptoms as ‘Mild’, ‘Moderate’, or ‘Severe’, we used DISC-IV parent-reported severity of impairment associated with symptoms to determine the impact of requiring at least two moderate or at least one severe rating of impairment across six domains.
III. Results
Case Definition Parameters
Teacher screeners and baseline parent interviews were obtained for 481 children in South Carolina and 579 children in Oklahoma. Demographic characteristics are shown in Table 1. Because relative changes in estimates when applying different case definition criteria resulted in similar patterns in both sites, combined results are presented here. The SC sample had a higher proportion of Black students and the OK sample had more Hispanic and American Indian students, though both samples were racially diverse. The most significant difference between the two samples was in the proportion of students from families at less than 200% of the 2004 federal poverty line (<200% FPL: 67.8% in OK versus 29.5% in SC).
Table 1.
Frequencies and weighted percentages of Project to Learn about Attention Deficit/Hyperactivity Disorder (ADHD) in Youth sample demographics
| BASELINE | EACH PARTICIPANT'S FINAL FOLLOW-UP |
||||
|---|---|---|---|---|---|
| Frequency | Percent (95% CI) | Frequency | Percent (95% CI) | ||
| Total | 1060 | 100.00% | 656 | 100.00% | |
| Sex | |||||
| Male | 737 | 51.5% (47.8–55.1%) | 440 | 47.9% (41.7–54.2%) | |
| Female | 323 | 48.5% (44.9–52.2%) | 216 | 52.1% (45.8–58.3%) | |
| Age (years) | |||||
| 4–7 | 285 | 28.8% (23.5–34.8%) | 3 | 1.4% (0.2–8.0%) | |
| 8–10 | 477 | 46.1% (39.9–52.4%) | 44 | 12.8% (7.4–21.5%) | |
| 11–13 | 293 | 24.7% (19.9–30.2%) | 205 | 35.8% (28.3–44.2%) | |
| 14–16 | 5 | 0.5% (0.1–1.7%) | 295 | 36.2% (29.7–43.2%) | |
| 17–19 | 0 | 0.0% | 109 | 13.8% (8.8–21.0%) | |
| Race | |||||
| White | 623 | 51.6% (45.6–57.5%) | 393 | 52.8% (44.6–60.9%) | |
| Black | 263 | 28.6% (23.5–34.3%) | 191 | 37.2% (29.7–45.4%) | |
| Other | 174 | 19.8% (15.5–25.0%) | 72 | 10.0% (6.5–14.9%) | |
| Ethnicity | |||||
| Hispanic | 74 | 10.5% (7.2–15.1%) | 28 | 3.6% (1.6–7.8%) | |
| Not Hispanic | 986 | 89.5% (85.0–92.8%) | 628 | 96.4% (92.2–98.4%) | |
| Poverty status: 2004 Federal Poverty Level (FPL) | |||||
| <200% FPL | 590 | 54.5% (48.0–60.8%) | 440 | 47.9% (41.7–54.2%) | |
| ≥200% FPL | 470 | 45.5% (39.2–52.0%) | 216 | 52.1% (45.8–58.3%) | |
| Past year parent-reported ADHD medication use | |||||
| Among those meeting criteria | |||||
| SC | 57/99 | 57.2% (46.9–66.9) | 41/68 | 50.6% (36.3–64.8) | |
| OK | 33/116 | 21.4% (13.7–31.7) | 42/82 | 24.4% (9.4–50.1) | |
| Pooled | 90/215 | 39.5% (31.1–48.6) | 83/150 | 32.3% (16.6–53.5) | |
| Among those not meeting criteria | |||||
| SC | 84/382 | 10.3% (7.6–13.8) | 62/305 | 12.2% (8.6–17.0) | |
| OK | 114/463 | 9.2% (6.8–12.3) | 39/201 | 7.0% (4.2–11.3) | |
| Pooled | 198/845 | 9.6% (7.3–11.9) | 101/506 | 9.4% (7.0–12.5) | |
| Entire sample | |||||
| SC | 141/481 | 14.4% (11.6–17.7) | 103/373 | 15.6% (12.0–20.1) | |
| OK | 147/579 | 9.8% (7.5–12.7) | 81/283 | 9.8% (6.8–13.9) | |
| Pooled | 288/1060 | 11.2% (9.3–13.4) | 184/656 | 12.4% (9.9–15.4) | |
CI: Confidence Interval; SC: South Carolina; OK: Oklahoma
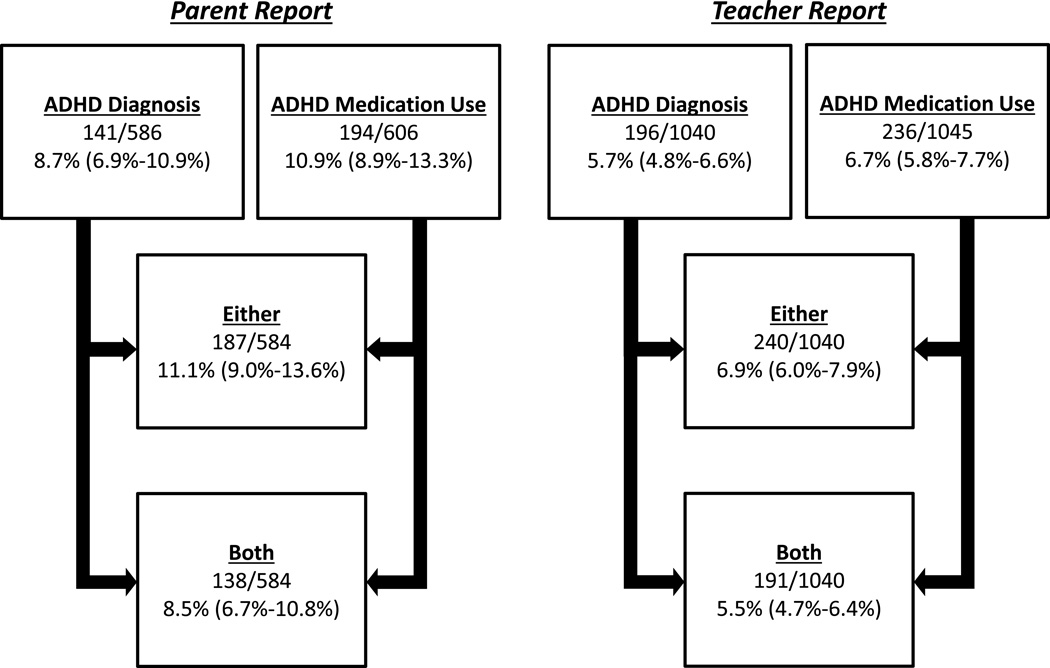
For the screener questions on ADHD diagnosis and medication history, there were 584 parent reports (11 parent-only) and 1040 teacher reports (467 teacher-only). Teacher-reported proportions were lower than parent-reported results (Figure 1). Of the subset of children for whom both parent and teacher screening data are available (n=573), agreement between parent and teacher report of either a diagnosis or medication use was good to excellent (SC: κ=0.88, 95% CI =0.84–0.92; OK: κ=0.67, 95% CI=0.58–0.70); combined κ=0.78, 95% CI=0.69–0.87), with 7.7% of children having either diagnosis or medication usage reported by both parent and teacher, and 11.6% of children having diagnosis or medication usage reported by at least one informant. Of those with parent-reported diagnosis, 67.5% were reported by teachers as having a diagnosis. When parents reported medication, 78.5% of teachers also reported medication; 91.3% of parents reported a diagnosis when the teacher also reported a diagnosis; and 90.2% of parents reported medication when the teacher reported medication.
Figure 1.
Number and unweighted percent (95% CI) of the screened Project to Learn about Attention Deficit/Hyperactivity Disorder (ADHD) in Youth sample with a parent- or teacher-reported ADHD diagnosis or medication use
Note: Denominators reported above show the number of parents and teachers who responded to whether a child had been diagnosed or used medication. Likely explanations for more teacher-reported data include that they received incentives, they were directly requested to complete them by school administrators, and they were able to complete classroom-sized batches of instruments.
Teachers reported 20.5% of children had at least six ADHD inattentive or hyperactive/impulsive symptoms, and 33.6% of children had at least some impairment based on the SDQ or VADTRS. When symptom count and impairment criteria were combined, the proportion of children who met both criteria dropped to 16.3%.
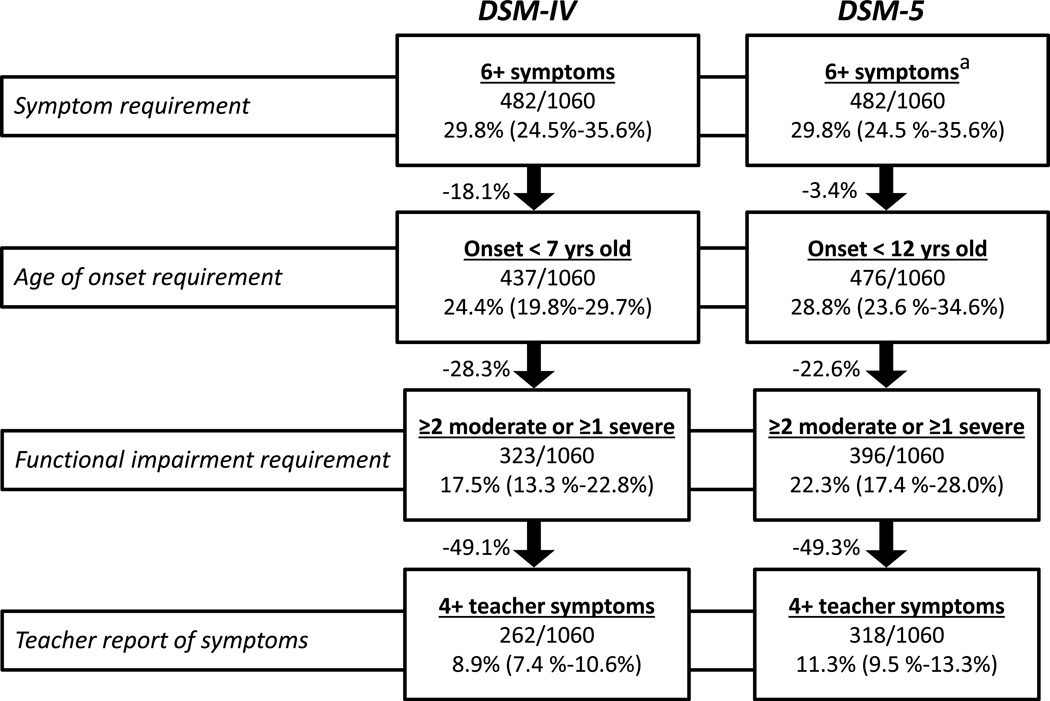
Baseline parent interview data reflected that 29.8% of children had at least six ADHD symptoms (Figure 2), 81.9% of whom had symptom onset by age seven years. Varying impairment criteria resulted in prevalence estimates ranging from 11.5% to 17.5%. Only three children had a severe rating in one domain with no other moderate or severe ratings, thus requiring at least two moderate ratings captures 99.1% (320 out of 323) of those meeting the impairment component of our study case definition and 98.8% (249 out of 252) of those with at least one severe rating.
Figure 2.
Depreciation in the number and percent (95% CI) of the baseline Project to Learn about Attention Deficit/Hyperactivity Disorder (ADHD) in Youth sample who met each level of ADHD diagnostic criteria.
* No participants at baseline were 17 years or older, so required symptom count remains 6+.
Finally, we added the requirement of teacher report of at least four symptoms in those children meeting DISC-based parent-reported criteria but who were low screen. With that additional requirement, the prevalence estimates decrease by approximately half, from 17.5% to 8.9% in the pathway corresponding to our case definition, quantifying the impact of the inclusion of information from multiple informants.
DSM-5-Based Case Definition Comparison
While 45 of 482 sample children with six or more DSM-IV ADHD symptoms did not meet the age of onset criterion of seven years, all but six of the children meeting symptom count criteria met the new age of onset criterion of 12 years (Figure 2). Adding the impairment criterion resulted in a greater reduction in the prevalence estimate when using the earlier age of onset: 28.3% reduction versus 22.6% for the later age of onset. Alternatively, 323 of 437 with earlier symptom onset met the impairment criterion, while 396 of the 476 with onset by age 12 years met that additional requirement. When adding in the requirement of at least four teacher-reported symptoms, the weighted prevalence estimates were 8.9% based on DSM-IV versus 11.3% of school-aged children based on DSM-5 (Figure 2).
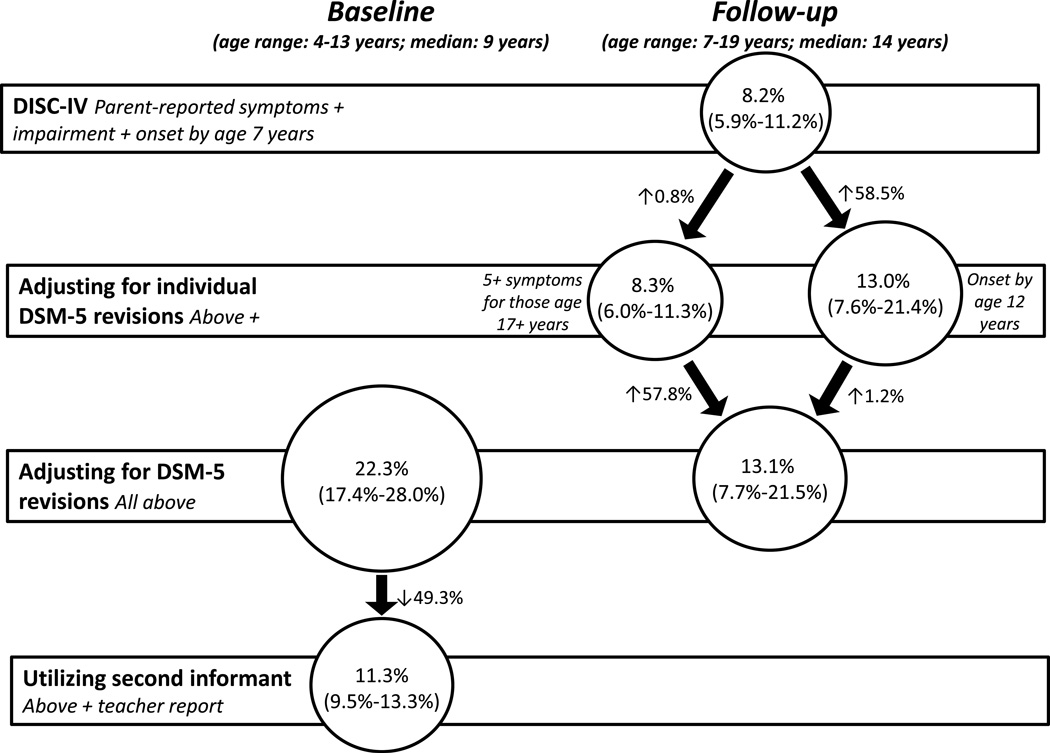
Of the 1,060 participants at baseline, 656 had at least one follow-up interview. Demographic characteristics of participants at their final PLAY follow-up assessment (age range: 7–19) are in Table 1, and characteristics of the case group under differing criteria in Table 2; the effects of modifying diagnostic criteria on prevalence estimates are shown in Figure 3. At follow-up the SC sample was slightly older than in OK because of additional follow-up interviews. In the final assessment sample 8.2% (n=128 of 656) met DISC-IV case criteria (95% CI: 5.9, 11.2) with 54.7% classified with the inattentive subtype. When the age of onset criterion is modified for symptom onset to have occurred before age 12 years rather than age seven, the prevalence of ADHD increases to 13.0% (95% CI: 7.6, 21.4), adding 20 cases, with 58.1% (16 additional) as inattentive subtype. The remaining four new cases were all combined subtype.
Table 2.
Project to Learn about Attention Deficit/Hyperactivity Disorder (ADHD) in Youth follow-up data: Demographics and sample characteristics (unweighted) of ADHD cases under various diagnostic criteria reflecting DSM-IV and DSM-5
| DSM-IV criteria | DSM-IV criteria + relaxing age of onset to <12 years + requiring only 5+ symptoms for 17+ year olds |
|||
|---|---|---|---|---|
| Total % (n) |
Additional cases %(n) |
Total % (n) |
||
| Total | 100.0% (128) | 100.0% (22) | 100.0% (150) | |
| Sex | ||||
| Male | 71.1% (91) | 77.3% (17) | 72.0% (108) | |
| Female | 28.9% (37) | 22.7% (5) | 28.0% (42) | |
| Race | ||||
| White | 68.0% (87) | 59.1% (13) | 66.7% (100) | |
| Black | 14.8% (19) | 36.4% (8) | 18.0% (27) | |
| Other | 17.2% (22) | 4.5% (1) | 15.3% (23) | |
| Ethnicity | ||||
| Hispanic | 7.8% (10) | 0.0% (0) | 6.7% (10) | |
| Not Hispanic | 92.2% (118) | 100.0% (22) | 93.3% (140) | |
| Subtype | ||||
| IA | 54.7% (70) | 81.8% (18) | 58.0% (87) | |
| HI | 7.8% (10) | 0.0% (0) | 6.7% (10) | |
| Combined | 37.5% (48) | 18.2% (4) | 35.3% (53) | |
| Ever met criteria for a condition other than ADHD | ||||
| Yes | 66.4% (85) | 63.6% (14) | 66.0% (99) | |
| No | 33.6% (43) | 36.4% (8) | 34.0% (51) | |
| Ever took ADHD medication treatment | ||||
| Yes | 74.2% (95) | 68.2% (15) | 73.3% (110) | |
| No | 25.8% (33) | 31.8% (7) | 26.7% (40) | |
| SDQ Total Difficulties score | ||||
| Abnormal | 53.6% (67) | 55.0% (11) | 53.8% (78) | |
| Borderline | 20.0% (25) | 15.0% (3) | 19.3% (28) | |
| Normal | 26.4% (33) | 30.0% (6) | 26.9% (39) | |
| Missing | -- (3) | -- (2) | -- (5) | |
This table only includes additional cases, though there was some shifting between subtypes of cases from baseline to last follow-up interview. After requiring only 5+ symptoms for those who were 17+ yrs old, one ADHD-IA case became an ADHD-combined case.
IA=Inattentive; HI=Hyperactive/impulsive
SDQ=Strengths and Difficulties Questionnaire
Figure 3.
Change in Attention Deficit/Hyperactivity Disorder prevalence (95% CI) after incorporating DSM-5 changes and inclusion of teacher report.
The final major change to the DSM-5 criteria allows for a decrease from six to five in the number of symptoms needed to qualify for diagnosis among young adults. There were 109 participants aged 17 years or older in the last interview (n= 656), 23 (21.1%) who were considered cases, yielding a weighted prevalence among those aged 17 and older of 8.1% (95% CI: 4.1, 15.6). The required symptom count reduction resulted in only two additional cases (both inattentive subtype), producing a weighted prevalence in older participants of 8.7% (95% CI: 4.4, 16.3) and a slight increase in overall prevalence of ADHD cases from 13.0% to 13.1% (95% CI 7.7, 21.5) in the full follow-up cohort.
IV. Discussion
In spite of widely varying published estimates of the prevalence of ADHD, there has been very little research on the qualitative and quantitative impact of varying case definitions and criteria on prevalence estimates. Relying on data from a community-based cohort, we have examined the extent to which applying successively more rigorous criteria impact the resulting proportions of the study sample who meet a specific case definition. We have also examined the potential impact of new DSM-5 criteria on prevalence estimates.
Consistent with DSM, requiring at least some impairment decreases the estimated prevalence by 28.3% compared to reliance on symptom count alone. Even for research studies that rely only on teacher questionnaires that assess symptoms, requiring the full count of symptoms and a measure of impairment are important as an initial basis for classifying probable diagnosis or for obtaining reasonable estimates of prevalence.
In our DISC-IV parent interview data, the prevalence of suspected ADHD with onset by age seven dropped by about one-half when at least one severe rating of impairment was required versus our original definition of one severe or two moderate ratings. This highlights the importance of clarity in the definition of impairment and the need for guidance for both clinical diagnosis and research classification. It also demonstrates that the definition of impairment, especially regarding the level of severity required, has a large impact on the classification of disorder. Degree of impairment is also the most salient clinical finding, as it has been shown that the presence of impairment, rather than symptoms, may drive who seeks treatment.34 Further research on the measurement of impairment severity is crucial for both diagnosis and treatment of ADHD.
Because many survey-based estimates rely on parent reports of diagnosis and medication treatment, we examined the agreement between teacher and parent reports and the impact of combining rules for diagnosis or treatment and for informants. There was moderate to strong agreement between parents and teachers on diagnosis and medication for ADHD, with parent-reported rates higher than those based on teacher report, though the difference between parents and teachers was greater for reported diagnosis (36%) than for medication use (19%). Teachers may be more aware of medication treatment than of diagnoses, due to the marked change in behavior that is achieved with medication treatment, even with the emergence of extended release formulations that may be administered exclusively at home. Our findings are consistent with this interpretation: teachers reported medication 78.5% of the time when parents reported medication, but reported a diagnosis only two-thirds of the time when parents reported diagnosis.
It should also be noted that parents are able to respond to whether the child has ever been diagnosed but teachers may be able to respond only for the period they have the child in class. As expected, when teachers reported diagnosis or medication, parents also reported over 90% of the time. That is, teacher reports appear to have good specificity, but less sensitivity, especially for ‘ever diagnosed’ classifications.
The results also demonstrate the importance of multiple informants in determining the presence of symptoms and impairment in multiple settings. Adding the requirement of at least four teacher-reported symptoms to the DISC-IV case definition with full parent-reported symptoms and impairment reduced the prevalence estimate in our data by half. Our data support the conclusions of others that the use of a second informant is important to appropriate diagnosis and to valid estimates of prevalence.22,35
It should be noted, however, that DSM-5 is not explicit about the extent to which symptoms must be present in different settings. Though the multiple informant issue is distinct from the multiple settings issue, they are related in that additional informants provide information about the subject in other settings or relationships. These concerns are further complicated for older adolescents and adults, who may be the only informant at diagnosis. Attempts to feign symptoms in order to obtain special accommodations or prescriptions for stimulant medication have been documented36,37 and further reinforce the need for additional confirmatory reports from other informants. Thus, a clinical decision, rather than reliance on checklists from informants, may be most important, with multiple informants enriching the information available to the clinician for making diagnostic and treatment decisions. This is a significant issue, particularly with primary care evaluations, where the time for assessment is limited in most practices.
We were able to assess the potential impact of the changes in diagnostic criteria in DSM-5 regarding age of onset and number of symptoms required for those aged 17 and older. Comparable to a recent U.S. study,21 but in contrast to estimates from a British birth cohort,38 older age of onset had a substantial impact, increasing the proportion with probable ADHD by 18% compared to estimates based only on symptomatology and by 27% after application of the impairment and second informant criteria. Given the baseline age of this elementary school sample, it was expected that the expanded age of onset criterion was not going to rule out many of the children, because most of them were younger than 12 at baseline. However at follow-up, when only 13.4% of the participants were under age 12, the extended age of onset added 20 cases resulting in an increase in prevalence from 8.2% to 13.1%. It seems clear that the change in the age of onset criterion is likely to result in a substantial increase in ADHD diagnosis, the extent of which is also a function of how rigorously the DSM-IV criterion had been applied in practice in the past.
In our sample the reduction in symptom count from six to five for those aged 17 and older resulted in the addition of only two cases, both with inattentive type, in the final interview follow-up sample in which 16.6% (n=109) were 17 years of age or older. Of those with five or more inattentive symptoms, 183 of 208 (88%) had at least six symptoms, and of those with five or more hyperactive-impulsive symptoms, 70 of 94 (74.5%) had at least six symptoms. This difference is consistent with our previous findings of greater persistence of inattentive versus hyperactive symptoms through adolescence.33 It does not appear that this relaxation of criteria for those 17 and older will have major impact for older adolescents, though we cannot draw any conclusions about the impact on adult populations with a broader age range.
This study exhibits some of the limitations common to community-based epidemiologic studies. Though the evaluations were conducted using validated systematic structured interviews (DISC-IV), with standardized algorithms and rigorous training of interviewers, there is potential for response bias, including social desirability and selective recall, especially in recalling age of onset for symptoms. The interviewed sample when weighted is diverse in race, ethnicity, and socioeconomic status and representative of the school districts from which it was drawn, but is not representative of the US population as a whole. Response rates were typical of contemporary epidemiologic studies – of those who participated at baseline, 62% had at least one follow-up interview – so there is a possibility of bias due to attrition. Finally, we did not have access to physician or other provider records to verify treatment and diagnosis, and relied only on parent and teacher reports of diagnosis, treatment, symptoms, impairment, and age of onset, though we believe parents to be the optimal informant for age of onset.
These findings quantify the impact of various DSM-based case definition criteria on research-based prevalence estimates, but also have implications for clinical practice because they indicate the influence of various criteria on the probability of valid classification. Changes in diagnosis may impact patterns of comorbidity in research studies as well as in clinical settings where treatment decisions may be affected. Further, the new criteria are especially likely to impact perceptions of developmental trajectories and considerations of the appropriateness of ADHD diagnosis in older adolescents and adults.
Assessment of impairment is a critical component of research and clinical diagnosis, and is most useful for diagnosis, treatment, and research when it includes both specification of the level of severity and consideration of multiple domains. Similarly, our findings document the sensitivity of prevalence estimates to both symptoms and impairment across settings, further supporting the importance of including reports from multiple informants. The level of impairment remains a matter of clinical judgment, rather than simple reliance on checklists from informants. Although time for assessment and access to additional informants in clinical settings is often limited, the determination of the extent and level of impairment is important, even if derived from a single informant.
We were also able to assess the probable impact of new DSM-5 criteria: the likely increase in prevalence from raising the required age of onset, and a possible smaller increase in prevalence among older adolescents and young adults due to the reduction in symptom count required. These findings will contribute to evaluating trends in ADHD diagnosis by assisting clinicians and researchers in differentiating changes due to new criteria from secular changes due to trends in prevalence already documented. Because of the age of our participants, we are less clear about how the new criteria will impact diagnosis and estimates of prevalence among adults older than those in our sample.
Finally, even though multi-axial assessment is no longer part of DSM-5, it remains clinically important to consider environmental factors that may exacerbate symptoms and impairment in late-onset cases. We hope to use our longitudinal data to shed light on this little-studied phenomenon.
Acknowledgments
Funding: This manuscript was supported by the Centers for Disease Control and Prevention through cooperative agreements U50/CCU622315-02 and U84/CCU422516-02 and contracts 200-2006-18912 and 200-2006-18949.
Dr. McKeown reports research support from CDC and consulting with Greenville (SC) Health System.
Dr. Cuffe reports the following sources of research support: CDC, Nexstim Corporation, Otsuka Pharmaceutical Co. Ltd.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Financial Conflicts of Interests
Dr. Holbrook reports no biomedical financial interests or potential conflicts of interest.
Ms. Danielson reports no biomedical financial interests or potential conflicts of interest.
Dr. Wolraich reports no biomedical financial interests or potential conflicts of interest.
Dr. Visser reports no biomedical financial interests or potential conflicts of interest.
Contributor Information
Robert E. McKeown, University of South Carolina, Arnold School of Public Health
Joseph R. Holbrook, Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities
Melissa L. Danielson, Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities
Steven P. Cuffe, University of Florida College of Medicine - Jacksonville
Mark L. Wolraich, University of Oklahoma Health Sciences Center, OU Child Study Center
Susanna N. Visser, Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Perou R, Bitsko RH, Blumberg SJ, et al. Mental health surveillance among children--United States, 2005–2011. Morb Mortal Wkly Rep Surveill Summ. 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- 3.Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34–46.e32. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Yagon M, Cavendish W, Cornoldi C, et al. The proposed changes for DSM-5 for SLD and ADHD: International perspectives - Australia, Germany, Greece, India, Israel, Italy, Spain, Taiwan, United Kingdom, and United States. J Learn Disabil. 2013;46(1):58–72. doi: 10.1177/0022219412464353. [DOI] [PubMed] [Google Scholar]
- 5.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007 Jun;164(6):942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 6.Visser SN, Blumberg SJ, Danielson ML, Bitsko RH, Kogan MD. State-based and demographic variation in parent-reported medication rates for attention-deficit/hyperactivity disorder, 2007–2008. Prev Chronic Dis. 2013 Jan;10:E09. doi: 10.5888/pcd9.120073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hinshaw SP, Scheffler RM, Fulton BD, et al. International variation in treatment procedures for ADHD: Social context and recent trends. Psychiatr Serv. 2011 May 1;62(5):459–464. doi: 10.1176/ps.62.5.pss6205_0459. 2011. [DOI] [PubMed] [Google Scholar]
- 8.Thome J, Reddy DP. The current status of research into Attention Deficit Hyperactivity Disorder: Proceedings of the 2nd International Congress on ADHD: From Childhood to Adult Disease. Atten Defic Hyperact Disord. 2009 Dec;1(2):165–174. doi: 10.1007/s12402-009-0016-0. [DOI] [PubMed] [Google Scholar]
- 9.Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014 Apr;43(2):434–442. doi: 10.1093/ije/dyt261. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cuffe SP, McKeown RE, Jackson KL, Addy CL, Abramson R, Garrison CZ. Prevalence of attention-deficit/hyperactivity disorder in a community sample of older adolescents. J Am Acad Child Adolesc Psychiatry. 2001 Sep;40(9):1037–1044. doi: 10.1097/00004583-200109000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Eaton WW, Martins SS, Nestadt G, Bienvenu OJ, Clarke D, Alexandre P. The burden of mental disorders. Epidemiol Rev. 2008;30:1–14. doi: 10.1093/epirev/mxn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldberg D. Epidemiology of mental disorders in primary care settings. Epidemiol Rev. 1995;17:182–190. doi: 10.1093/oxfordjournals.epirev.a036174. [DOI] [PubMed] [Google Scholar]
- 13.Susser E, Schwartz S, Morabia A, Bromet EJ, editors. Psychiatric Epidemiology: Searching for the Causes of Mental Disorders. New York, NY: Oxford University Press; 2006. [Google Scholar]
- 14.Visser SN, Danielson ML, Bitsko RH, et al. Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children — United States, 2003 and 2007. Morb Mortal Wkly Rep. 2010;59(44):1439–1443. [PubMed] [Google Scholar]
- 15.Getahun D, Jacobsen SJ, Fassett MJ, Chen W, Demissie K, Rhoads GG. Recent trends in childhood attention-deficit/hyperactivity disorder. JAMA Pediatr. 2013;167(3):282–288. doi: 10.1001/2013.jamapediatrics.401. [DOI] [PubMed] [Google Scholar]
- 16.Visser SN, Danielson ML, Bitsko RH, Perou R, Blumberg SJ. Convergent validity of parent-reported ADHD diagnosis: A cross-study comparison. JAMA Pediatr. 2013:1–2. doi: 10.1001/jamapediatrics.2013.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd - Revised ed. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- 19.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th text revision ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 21.Vande Voort JL, He J-P, Jameson ND, Merikangas KR. Impact of the DSM-5 attention-deficit/hyperactivity disorder (ADHD) age of onset criterion in the U.S. adolescent population. J Am Acad Child Adolesc Psychiatry. 2014 doi: 10.1016/j.jaac.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sibley MH, Waxmonsky JG, Robb JA, Pelham WE. Implications of changes for the field: ADHD. J Learn Disabil. 2013;46(1):34–42. doi: 10.1177/0022219412464350. [DOI] [PubMed] [Google Scholar]
- 23.De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol Bull. 2005 Jul;131(4):483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- 24.Wolraich ML, Lambert EW, Bickman L, Simmons T, Doffing MA, Worley KA. Assessing the impact of parent and teacher agreement on diagnosing ADHD. J Dev Behav Pediatr. 2004;25:41–47. doi: 10.1097/00004703-200402000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Barkley RA. Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. New York: The Guilford Press; 2006. [Google Scholar]
- 26.Biederman J, Mick E, Faraone S, et al. Influence of gender on attention-deficit/hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry. 2002;159:36–42. doi: 10.1176/appi.ajp.159.1.36. [DOI] [PubMed] [Google Scholar]
- 27.Grizenko N, Paci M, Joober R. Is the inattentive subtype of ADHD different from the combined/hyperactivity subtype? J Atten Disord. 2010;13:649–657. doi: 10.1177/1087054709347200. [DOI] [PubMed] [Google Scholar]
- 28.Oner O, Oner P, Cop E, Munir KM. Characteristics of DSM-IV attention deficit hyperactivity disorder combined and predominantly inattentive subtypes in a Turkish clinical sample. Child Psychiatry Hum Dev. 2012;43(4):523–532. doi: 10.1007/s10578-012-0281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolraich M, McKeown R, Visser S, et al. The Prevalence of ADHD: Its Diagnosis and Treatment in Four School Districts Across Two States. J Atten Disord. 2014;18(7):563–575. doi: 10.1177/1087054712453169. [DOI] [PubMed] [Google Scholar]
- 30.Wolraich ML, Lambert EW, Doffing MA, Bickman L, Simmons T, Worley KA. Psychometric properties of the Vanderbilt ADHD Diagnostic Parent Rating Scale. J Pediatr Psychol. 2003;28(8):559–567. doi: 10.1093/jpepsy/jsg046. [DOI] [PubMed] [Google Scholar]
- 31.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001 Nov;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Shaffer D, Fisher P, Lucas C, Dulcan M, Schwab-Stone M. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliablity of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 33.Holbrook J, Cuffe S, Cai B, et al. Persistence of Parent-Reported ADHD Symptoms From Childhood Through Adolescence in a Community Sample. J Atten Disord. doi: 10.1177/1087054714539997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Angold A, Costello EJ, Farmer EM, Burns BJ, A E. Impaired but undiagnosed. J Am Acad Child Adolesc Psychiatry. 1999;38(2):129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Tannock R. Rethinking ADHD and LD in DSM-5: Proposed changes in diagnostic criteria. J Learn Disabil. 2013;46(1):5–25. doi: 10.1177/0022219412464341. [DOI] [PubMed] [Google Scholar]
- 36.Barrett SP, Darredeau C, Bordy LE, Pihl RO. Characteristics of methylphenidate misuse in a university student sample. Can J Psychiatry. 2005;50:457–461. doi: 10.1177/070674370505000805. [DOI] [PubMed] [Google Scholar]
- 37.Lakhan SE, Kirchgessner A. Prescription stimulants in individuals with and without attention deficit hyperactivity disorder: misuse, cognitive impact, and adverse effects. Brain Behav. 2012;2(5):661–677. doi: 10.1002/brb3.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Polanczyk G, Caspi A, Houts R, Kollins SH, Rohde LA, Moffitt TE. Implications of Extending the ADHD Age-of-Onset Criterion to Age 12: Results from a Prospectively Studied Birth Cohort. J Am Acad Child Adolesc Psychiatry. 2010;49(3):210–216. [PubMed] [Google Scholar]