Abstract
Measured human dosimetry of the 68Ga-labeled synthetic somatostatin analog 68Ga-DOTATATE has not been reported in the peer-reviewed literature. 68Ga-DOTATATE is an investigational PET/CT imaging agent that binds with high affinity to somatostatin receptor subtype 2, found on many human cancers, most classically neuroendocrine tumors but also others. Reporting of measured dosimetry of 68Ga-DOTATATE could be useful for investigations for diagnosis, staging, and restaging of somatostatin receptor–expressing tumors.
Methods
We performed measured dosimetry with 68Ga-DOTATATE PET/CT scanning in 6 volunteer human subjects as part of an Institutional Review Board–approved biodistribution investigation of the use of this radiopharmaceutical for possible future use in the diagnosis of indeterminate lung nodules or lung cancer. Five subjects were imaged at 3 time points, and 1 subject was imaged at 2 time points. Dosimetry was then measured for the whole body and for specific organs.
Results
There were no observed adverse events to the radiopharmaceutical in the immediate or delayed time frames, with a follow-up of 1 y. One patient had stage IV non–small cell lung cancer and remains alive but with disease progressing on treatment. For the other 5 patients, it was ultimately proven that they had benign nodules. The measured dosimetry shows that the critical organ with 68Ga-DOTATATE is the spleen, followed by the uroepithelium of the bladder, the kidneys, and the liver, in that order. Organ-specific and whole-body dosimetries for 68Ga-DOTATATE were similar to but often slightly greater than those for 68Ga-DOTATOC or 68Ga-DOTANOC but less than those for 111In-diethylenetriaminepentaacetic acid-octreotide.
Conclusion
No toxicity was observed in our 6 patients, and no adverse events occurred. The measured human dosimetry of 68Ga-DOTATATE is similar to that of other 68Ga-labeled somatostatin receptor analogs.
Keywords: 68Ga-DOTATATE, dosimetry, neuroendocrine tumors
For more than a decade, PET emitter–labeled high-affinity somatostatin receptor analogs have been used for imaging, predominately outside the United States. The improved spatial and contrast resolution of PET imaging results in improvements in the quality of information used by care-givers, leading to better patient care decisions for those with somatostatin receptor–expressing tumors. These synthetic somatostatin analogs can also be labeled with β-emitting radionuclides, resulting in directed radiotherapy (peptide receptor radionuclide therapy [PRRT]) to these tumors, with several trials demonstrating improved outcomes in patients who are not candidates for attempted surgical cure and who demonstrate poor response to conventional medical treatments (1,2).
Several somatostatin analog peptides have been used for PET-based imaging of somatostatin receptor–expressing tumors. These are typically DOTA-conjugated peptides allowing chelation with PET-emitting metal ions (such as 68Ga or 64Cu (3)) for diagnosing, staging, and assessing treatment response or allowing chelation with 177Lu (4), 90Y (5), or a combination of each (6) for PRRT. The imaging-based radiopharmaceuticals have been used to estimate tumor dosimetry before the administration of PRRT, an important function because significant radiation-induced toxicity can occur with the unsealed radiotherapeutic compounds (7). Diagnostic scans permitting a rough estimate of uptake in the tumor and normal vital organs (8) are especially important for patients receiving multiple PRRTs because of the resulting transient and sometimes permanent deterioration of renal and hematopoietic function that can result (9,10). Diagnostic scans also allow the detection of patients with tumors that have become poorly differentiated or anaplastic, with loss of somatostatin receptor expression, thereby identifying patients who are unlikely to benefit from PRRT. The use of 68Ga-DOTATATE PET/CT scans after PRRT is also predictive of response, with a decrease in uptake in the tumor-to-spleen ratio after PRRT, compared with baseline, identifying patients with prolonged time to progression. This decrease in the tumor-to-spleen uptake ratio also correlated with improvement in clinical symptoms, compared with patients with no change or increase in the tumor-to-spleen uptake ratio (11).
A variety of synthetic somatostatin analog peptides, including DOTATOC, DOTATATE, and DOTANOC, have been described in numerous published articles. Detailed measured human dosimetry has been reported in the peer-reviewed literature for 68Ga-DOTATOC (12) and 68Ga-DOTANOC (13) but not for 68Ga-DOTATATE. Accordingly, we report our results for the imaging of 6 subjects with 68Ga-DOTATATE using multiple time points.
MATERIALS AND METHODS
This dosimetry investigation was performed as part of a Veterans Affairs Tennessee Valley Healthcare System (VATVHS) institutional review board (IRB)–approved investigation using 68Ga-DOTATATE. Informed consent was obtained from all subjects as part of a Veterans Affairs–funded Merit Review investigation and under the oversight of the VATVHS Radioactive Drug Research Committee. The 68Ga-DOTATATE imaging was for biodistribution only and was not used for diagnosis. Inclusion and exclusion criteria were the same as for overall investigation, plus these subjects had to be able and willing to undergo the additional emission imaging needed for dosimetry data collection. An additional requirement for the dosimetry protocol included the ability to remain motionless on the scanner table while one or two additional emission datasets were acquired. Toxicity monitoring included preinjection and post-scan vital signs (heart rate, blood pressure, body temperature, and respiratory rate), pulse oximetry on room air, and 12-lead electrocardiography.
The purpose of the investigation was to establish the biodistribution of 68Ga-DOTATATE in patients either with indeterminate lung nodules or with newly diagnosed lung cancer in areas with high false-positive rates on 18F-FDG scanning that were due to endemic fungal disease. Inclusion criteria of this study protocol for early detection of malignant lung nodules or lung cancer required adults who were 30 y or older (younger patients are unlikely to have lung cancer) with the ability to provide informed consent and with a newly diagnosed, indeterminate lung nodule or a newly diagnosed, untreated lung cancer. Though both male and female subjects were eligible for enrollment, the study group for the dosimetry analysis was composed entirely of men because of the predominately male sex in the older VA population. Although the subjects were exclusively men, we calculated the dosimetry using a reference adult model, which contains both male and female organs. Subjects with a history of any prior treatment for a systemic malignancy, comorbidities suggesting a life span of 2 y or less if untreated, a known active infection, or a body weight in excess of 135 kg (300 pounds) were excluded because these factors could influence image quality; body weight, however, would not significantly affect dosimetry because yellow adipose tissue has low somatostatin receptor expression levels.
Radiopharmaceutical Preparation
Because 68Ga has a 68-min half-life, production of 68Ga-DOTATATE requires the use of an onsite 68Ge/68Ga generator (model IGG100; Eckert & Ziegler Isotope Products). At this time, there is no good manufacturing practice (GMP)–certified generator; thus, radiopharmaceutical preparation was not performed with GMP standards. The generator was eluted within 24 h before use to minimize the buildup of 68Zn (the decay product of 68Ga) on the generator column. The 68Ge/68Ga generator was fractionally eluted with 0.1N HCl in 3 fractions. The middle fraction, containing approximately 75% of the activity available from the generator, was used for the dose preparation. An individual vial containing 100 μg of lyophilized GMP-prepared DOTATATE obtained commercially (ABX Advanced Biochemical Compounds GmbH) was dissolved with 1 mL of 0.1 M acetate buffer (pH 5.5). The DOTATATE solution (0.5 mL; 50 μg) was added to the appropriate elution fraction in a sterile vial and heated for 10 min at 100°C. The vial was removed from heat, and after 5 min of cooling 3–5 mL of sterile water for injection (U.S. Pharmacopeial Convention) were added to the vial. This solution was removed with a sterile syringe and needle and filtered using a sterile 0.22-μm membrane filter into the final collection vial. Samples were then aseptically removed for quality control testing. The non–decay-corrected radiochemical yield averaged 64%.
Radiochemical purity was confirmed using a miniature, reversed-phase liquid chromatography system with a prepared C-18 Sep-Pak cartridge (Waters Corp.). The sample was initially eluted with 10 mL of 0.001N HCl, followed by an elution of 10 mL of a 50:50 mixture of ethanol:water. In this system, free 68GaCl is eluted with 0.001N HCl and 68Ga-DOTATATE is eluted in the 50:50 ethanol:water elution mixture, with colloidal 68Ga retained on the column. The average radiochemical purity was 96.8% (range, 95.7%–98.2%). Radiochemical identity was determined for each new lot of precursor using a gradient high-performance liquid chromatography system and an analytic C-18 column with a gradient of acetonitrile and water. The nominal retention time using this system is 13.5 min.
Radionuclidic purity was determined by taking 2 measurements in a dose calibrator using the same geometry at a minimum of 10 min apart and calculating half-life. Bacterial endotoxin testing was performed using the Endosafe-PTS system (Charles River Laboratories International, Inc.). Because no organic solvents are used in the synthesis, testing for residual solvents is not required (14). Provided that the release criteria were met, the finished drug was released for human use (Table 1).
TABLE 1.
68Ga-DOTATATE Release Specifications
| Test | Release criterion |
|---|---|
| Appearance of final product | Clear with no visible impurities |
| Filter test | >45 psi |
| pH | 3.0–5.5 |
| Radiochemical purity | >90% (achieved >95%) |
| Endotoxin level | <17.5 Endotoxin units per mL |
| Radionuclidic purity | Within ±90 s of 68Ga half-life |
After release, tryptic soy broth and fluid thioglycollate media were inoculated, incubated (tryptic soy broth at room temperature and fluid thioglycollate medium at 36°C), and checked for growth during the following 14 d. Reserve samples were periodically tested for radionuclidic purity using a multichannel analyzer 48 or more hours after synthesis. Radionuclidic impurities were found to be less than 0.001% using this method. The nominal injected dose was 185–260 MBq (5–7 mCi) in a volume of 2–7 mL containing 7–45 μg of 68Ga-DOTATATE.
Dosimetry Protocol
Data from 6 subjects were analyzed. To avoid biologic elimination, subjects voided their urinary bladders immediately before injection of the 68Ga-DOTATATE radiopharmaceutical but did not void again until after the entire dosimetry series was completed. The patients were placed on the scanner table (Discovery VCT whole-body PET/CT scanner; GE Healthcare) to allow a vertex to mid thigh low-dose CT scan without contrast (used for anatomic localization and attenuation correction), followed immediately by emission imaging beginning at 0.8 h after injection. Emission imaging was performed from the vertex to mid thighs, with 4 min per bed position in 3-dimensional acquisition mode. We acquired data for 5 subjects at 3 time points, approximately 0.8, 1.5, and 2 h after radiopharmaceutical injection. In subject 6, we acquired data at 2 time points (1.2 and 1.7 h after injection) because this subject was unable to tolerate an additional emission acquisition because of arthritic pain.
Emission images were reconstructed using an ordered-subset expectation maximization algorithm with 28 subsets and 2 iterations and a z-axis filter of 6 mm in full width at half maximum. Final images were stored using a 128 × 128 matrix set with 3.75-mm cubic voxels covering a 70-cm field of view. Emission data were corrected for dead-time, scatter, and decay, and resulting voxels were stored in units of Bq/mL. Attenuation correction was performed with CT using 120 KVp, with automatic adjustment of mAs (range, 30–400) by the scanner to minimize radiation dose to the subjects. Corresponding CT images were reconstructed using a soft-tissue filter in a 512 matrix covering the full 70-cm field of view.
Data Analysis
From the Digital Imaging and Communications in Medicine emission and transmission data, volumes of interest were drawn around regions identified on the scans as pituitary gland, major salivary glands, thyroid, liver, spleen, kidneys, urinary bladder, the central sacrum (for hematopoietic marrow), testicles, and whole body, using the Medical Image Processing, Analysis and Visualization software (National Institutes of Health) (15). The activity in the nonmeasured portions of the lower extremities was estimated by taking the recovered activity of the first time point (estimated to be about 80% because of omission of portions of the extremities), and then dividing the total measured counts in the whole body by 80% to yield a reasonable estimate of the activity in the whole body. The average voxel intensity was multiplied by the volume of interest and related to absolute activity using the measured PET/CT system calibration factor to obtain the dosimetry data as previously reported.
Data were fitted using the SAAM II software (16). Time integrals of activity (17) were entered into the OLINDA/EXM software (18), using the reference adult model. Because the patients did not void after injection, it was assumed that there was no excretion of the activity; any activity not accounted for in the organs was assumed to be uniformly distributed throughout the remainder of the body, being removed only by physical decay. Because patients did void after data acquisition was completed (postscan voiding as increased by encouraging patients to augment fluid intake), the actual bladder exposure will be lower than what is calculated by this protocol. In addition, the results from all patients enrolled in dosimetry analysis were combined so that dosimetry could be reported in relation to the diagnosis and overall disease burden of each patient and to allow the calculation of mean, SD, and range of radiation-absorbed doses to individual organs.
RESULTS
Toxicity Reporting
There were no observed adverse events from the investigational radiopharmaceutical. No physiologic responses were observed. Preinjection and postscan complete blood counts, electrolytes (serum sodium, potassium, chloride, and bicarbonate levels), liver function studies, and renal function studies were also unchanged. The subjects reported no subjective symptoms. Subject 3 had stage IV non–small cell lung cancer; 1 y later, at the time of this report, the patient is still alive, though with disease progressing on treatment. The other 5 patients had benign nodules and remain in their usual state of health, with no long-term observed toxicity. Normal biodistribution is demonstrated in Figure 1.
FIGURE 1.
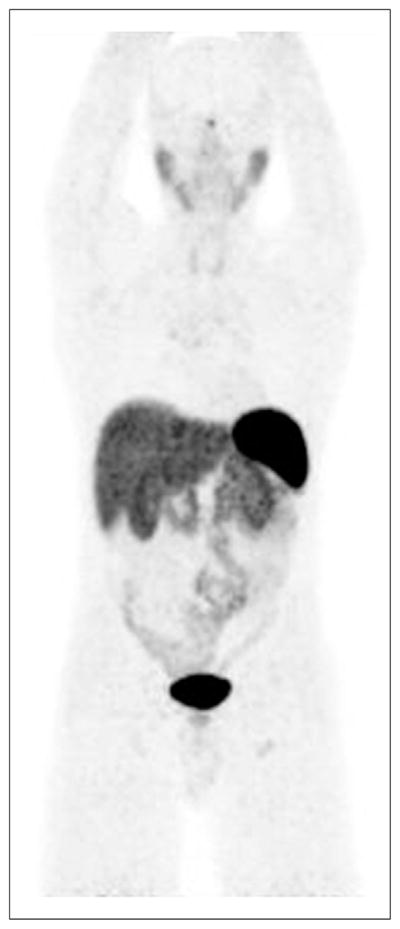
Anterior 3-dimensional maximum-intensity projection demonstrating normal, physiologic biodistribution of 68Ga-DOTATATE.
Dosimetry
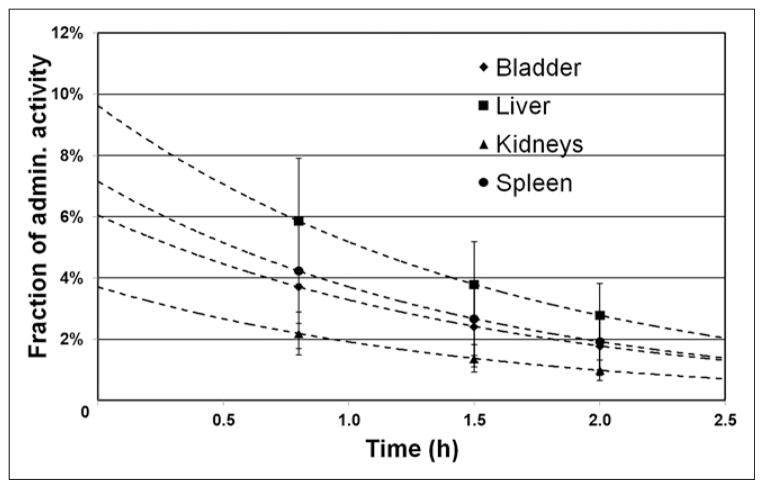
Similar to results reported for 68Ga-DOTATOC and 68Ga-DOTANOC, the critical organ was the spleen, with the next greatest exposure in the urinary bladder uroepithelium, kidneys, and liver, in descending order (Table 2). Comparable results in 4 organs and in effective dose (ED) are shown for 68Ga-DOTATATE, 68Ga-DOTATOC, 68Ga-DOTANOC, 111In-diethylenetriaminepentaacetic acid (DTPA)-octreotide, and 18F-FDG in Table 3. The individual results of the 6 patients are reported in Table 4. Although all subjects were men, doses are given for both male and female organs, using the standardized dosimetry phantoms, and the ED was calculated using the usual rules for choice of male or female gonads. Time–activity curves of the spleen, urinary bladder, kidneys, and liver are shown in Figure 2.
TABLE 2.
Estimated Organ-Specific Dose and ED
| Target organ | Estimated radiation dose (mSv/MBq) | ||
|---|---|---|---|
| Average | SD | Percentage coefficient of variation | |
| Adrenals | 1.46E−02 | 5.18E−04 | 3.55E+00 |
| Brain | 9.86E−03 | 5.46E−04 | 5.54E+00 |
| Breasts | 9.96E−03 | 4.26E−04 | 4.28E+00 |
| Gallbladder wall | 1.49E−02 | 6.77E−04 | 4.54E+00 |
| Lower large intestine wall | 1.29E−02 | 8.43E−04 | 6.52E+00 |
| Small intestine | 1.38E−02 | 2.60E−03 | 1.88E+01 |
| Stomach wall | 1.38E−02 | 6.47E−04 | 4.68E+00 |
| Upper large intestine wall | 1.29E−02 | 4.23E−04 | 3.29E+00 |
| Heart wall | 1.23E−02 | 3.93E−04 | 3.21E+00 |
| Kidneys | 9.21E−02 | 2.84E−02 | 3.08E+01 |
| Liver | 4.50E−02 | 1.52E−02 | 3.38E+01 |
| Lungs | 1.15E−02 | 3.52E−04 | 3.06E+00 |
| Muscle | 1.13E−02 | 4.47E−04 | 3.96E+00 |
| Ovaries | 1.31E−02 | 8.32E−04 | 6.35E+00 |
| Pancreas | 1.67E−02 | 1.37E−03 | 8.20E+00 |
| Pituitary gland | 4.16E−02 | 3.20E−02 | 7.70E+01 |
| Hematopoietic cells | 9.61E−03 | 3.47E−04 | 3.61E+00 |
| Bone-forming cells | 1.55E−02 | 7.39E−04 | 4.76E+00 |
| Salivary glands | 1.17E−02 | 7.82E−03 | 6.68E+01 |
| Skin | 9.66E−03 | 4.24E−04 | 4.39E+00 |
| Spleen | 2.82E−01 | 1.21E−01 | 4.28E+01 |
| Testes | 1.12E−02 | 6.78E−04 | 6.06E+00 |
| Thymus | 1.09E−02 | 4.93E−04 | 4.51E+00 |
| Thyroid | 1.87E−02 | 1.05E−02 | 5.65E+01 |
| Urinary bladder wall | 1.25E−01 | 6.18E−02 | 4.96E+01 |
| Uterus (estimated)* | 1.47E−02 | 1.56E−03 | 1.06E+01 |
| Total body | 1.34E−02 | 2.83E−04 | 2.11E+00 |
| ED | 2.57E−02 | 2.85E−03 | 1.11E+01 |
Uterus dosimetry is estimated because all subjects were men.
TABLE 3.
Selected Organ Dose and ED for Discussed Radiopharmaceuticals
| Organ | 68Ga-DOTATATE* | 68Ga-DOTATOC (12) | 68Ga-DOTANOC (13) | 111In-DTPA-octreotide (19) | 18F-FDG (20) |
|---|---|---|---|---|---|
| Kidneys (mSv/MBq) | 9.21E−02 | 2.2E−01 | 8.97E−02 | 4.5E−01 | 1.7E−02 |
| Liver (mSv/MBq) | 4.50E−02 | 7.4E−02 | 3.38E−02 | 7.0E−02 | 2.1E−02 |
| Spleen (mSv/MBq) | 2.82E−01 | 2.4E−01 | 7.25E−02 | 3.2E−01 | 1.1E−02 |
| Urinary bladder wall (mSv/MBq) | 1.25E−01 | 7.0E−02 | 8.36E−02 | 1.8E−01 | 1.3E−01 |
| ED (mSv/MBq) | 2.57E−02 | 2.3E−02 | 1.67E−02 | 8.0E−02 | 1.9E−02 |
| Typical IA | |||||
| MBq | 185 | 185 | 185 | 74 | 370 |
| mCi | 5 | 5 | 5 | 2 | 10 |
| Estimated ED per scan (mSv) | 4.8 | 4.3 | 3.1 | 5.9 | 7.0 |
Radiation dose to uroepithelium is higher than would be experienced in patients allowed to void after injection. There are technical differences between these reported series. Additionally, subjects in these series are not same.
IA = injected activity for adult scan.
TABLE 4.
Detailed Measured ED and Organ-Specific Dosimetry
| Target organ | Estimated radiation dose (mSv/MBq) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Subject | Average | SD | Percentage coefficient of variation | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | ||||
| Adrenals | 1.48E−02 | 1.41E−02 | 1.49E−02 | 1.42E−02 | 1.54E−02 | 1.42E−02 | 1.46E−02 | 5.18E−04 | 3.55E+00 |
| Brain | 1.07E−02 | 9.98E−03 | 9.14E−03 | 1.01E−02 | 9.83E−03 | 9.42E−03 | 9.86E−03 | 5.46E−04 | 5.54E+00 |
| Breasts | 1.06E−02 | 9.96E−03 | 9.42E−03 | 1.01E−02 | 1.01E−02 | 9.55E−03 | 9.96E−03 | 4.26E−04 | 4.28E+00 |
| Gallbladder wall | 1.42E−02 | 1.47E−02 | 1.53E−02 | 1.51E−02 | 1.60E−02 | 1.43E−02 | 1.49E−02 | 6.77E−04 | 4.54E+00 |
| Lower large intestine wall | 1.37E−02 | 1.37E−02 | 1.20E−02 | 1.34E−02 | 1.18E−02 | 1.30E−02 | 1.29E−02 | 8.43E−04 | 6.52E+00 |
| Small intestine | 1.91E−02 | 1.32E−02 | 1.23E−02 | 1.31E−02 | 1.27E−02 | 1.26E−02 | 1.38E−02 | 2.60E−03 | 1.88E+01 |
| Stomach wall | 1.41E−02 | 1.29E−02 | 1.40E−02 | 1.34E−02 | 1.48E−02 | 1.38E−02 | 1.38E−02 | 6.47E−04 | 4.68E+00 |
| Upper large intestine wall | 1.35E−02 | 1.30E−02 | 1.23E−02 | 1.30E−02 | 1.28E−02 | 1.25E−02 | 1.29E−02 | 4.23E−04 | 3.29E+00 |
| Heart wall | 1.27E−02 | 1.21E−02 | 1.19E−02 | 1.24E−02 | 1.27E−02 | 1.18E−02 | 1.23E−02 | 3.93E−04 | 3.21E+00 |
| Kidneys | 1.39E−01 | 1.02E−01 | 1.03E−01 | 6.38E−02 | 6.85E−02 | 7.61E−02 | 9.21E−02 | 2.84E−02 | 3.08E+01 |
| Liver | 1.93E−02 | 4.03E−02 | 5.84E−02 | 4.75E−02 | 6.17E−02 | 4.27E−02 | 4.50E−02 | 1.52E−02 | 3.38E+01 |
| Lungs | 1.19E−02 | 1.13E−02 | 1.12E−02 | 1.16E−02 | 1.19E−02 | 1.11E−02 | 1.15E−02 | 3.52E−04 | 3.06E+00 |
| Muscle | 1.20E−02 | 1.14E−02 | 1.07E−02 | 1.15E−02 | 1.12E−02 | 1.10E−02 | 1.13E−02 | 4.47E−04 | 3.96E+00 |
| Ovaries | 1.39E−02 | 1.39E−02 | 1.22E−02 | 1.35E−02 | 1.20E−02 | 1.31E−02 | 1.31E−02 | 8.32E−04 | 6.35E+00 |
| Pancreas | 1.62E−02 | 1.49E−02 | 1.78E−02 | 1.57E−02 | 1.86E−02 | 1.69E−02 | 1.67E−02 | 1.37E−03 | 8.20E+00 |
| Pituitary gland | 1.31E−02 | 1.02E−01 | 2.42E−02 | 4.63E−02 | 2.49E−02 | 3.86E−02 | 4.16E−02 | 3.20E−02 | 7.70E+01 |
| Hematopoietic cells | 1.02E−02 | 9.67E−03 | 9.21E−03 | 9.68E−03 | 9.58E−03 | 9.32E−03 | 9.61E−03 | 3.47E−04 | 3.61E+00 |
| Bone-forming cells | 1.67E−02 | 1.57E−02 | 1.46E−02 | 1.58E−02 | 1.55E−02 | 1.49E−02 | 1.55E−02 | 7.39E−04 | 4.76E+00 |
| Salivary glands | 2.15E−03 | 2.27E−02 | 6.85E−03 | 1.30E−02 | 7.02E−03 | 1.85E−02 | 1.17E−02 | 7.82E−03 | 6.68E+01 |
| Skin | 1.03E−02 | 9.77E−03 | 9.09E−03 | 9.83E−03 | 9.63E−03 | 9.31E−03 | 9.66E−03 | 4.24E−04 | 4.39E+00 |
| Spleen | 2.01E−01 | 1.30E−01 | 3.95E−01 | 1.96E−01 | 4.15E−01 | 3.54E−01 | 2.82E−01 | 1.21E−01 | 4.28E+01 |
| Testes | 1.19E−02 | 1.18E−02 | 1.04E−02 | 1.16E−02 | 1.04E−02 | 1.11E−02 | 1.12E−02 | 6.78E−04 | 6.06E+00 |
| Thymus | 1.17E−02 | 1.10E−02 | 1.03E−02 | 1.11E−02 | 1.10E−02 | 1.05E−02 | 1.09E−02 | 4.93E−04 | 4.51E+00 |
| Thyroid | 2.54E−02 | 3.63E−02 | 9.93E−03 | 1.09E−02 | 1.07E−02 | 1.88E−02 | 1.87E−02 | 1.05E−02 | 5.65E+01 |
| Urinary bladder wall | 1.02E−01 | 1.90E−01 | 1.11E−01 | 1.49E−01 | 2.02E−02 | 1.76E−01 | 1.25E−01 | 6.18E−02 | 4.96E+01 |
| Uterus (estimated)* | 1.51E−02 | 1.64E−02 | 1.36E−02 | 1.55E−02 | 1.21E−02 | 1.54E−02 | 1.47E−02 | 1.56E−03 | 1.06E+01 |
| Total body | 1.34E−02 | 1.31E−02 | 1.35E−02 | 1.33E−02 | 1.39E−02 | 1.32E−02 | 1.34E−02 | 2.83E−04 | 2.11E+00 |
| ED | 2.25E−02 | 2.43E−02 | 2.81E−02 | 2.49E−02 | 2.44E−02 | 3.02E−02 | 2.57E−02 | 2.85E−03 | 1.11E+01 |
Uterus dosimetry is estimated because all subjects were men.
FIGURE 2.
Time–activity curves of selected organs. n = 5 subjects for time point 1; n = 6 subjects for time points 2 and 3. admin. = administered.
DISCUSSION
68Ga-labeled somatostatin analog peptides clear rapidly from the blood, with reported peak tumor uptake occurring at ±70 min and no radioactive metabolites detected in the serum at 4 h (Fig. 2) (14). Our data, obtained from 6 patients using 68Ga-DOTATATE, demonstrate overall results similar to those using 68Ga-DOTATOC, though there are no-table differences from those using 68Ga-DOTANOC. The critical organ in our investigation was the spleen (organ dose, 2.82E−01 mSv/MBq), followed by the uroepithelium of the urinary bladder wall, which received 1.25E−01 mSv/MBq. The third highest organ dose was to the kidneys (9.21E−02 mSv/MBq), followed by the liver (4.50E−02 mSv/MBq). To avoid biologic elimination, our subjects did not void after injection of the 68Ga-DOTATATE until after the measured dosimetry study was completed; accordingly, the usual clinical use of this radiopharmaceutical will result in less radiation to the uroepithelium than reported in this investigation. Although the organ doses and EDs for 68Ga-DOTATATE and 68Ga-DOTATOC are similar (though 68Ga-DOTATOC is slightly lower), the reported dosimetry of 68Ga-DOTA-NOC is the lowest of these 3 radiopharmaceuticals. These reports, however, used slightly different techniques, with results obtained in different patients, and thus are not directly comparable (12,13). Importantly, the ED per mega-becquerel for 111In-DTPA-octreotide is approximately 3–5 times higher than for the 68Ga-labeled somatostatin analogs, necessitating a lower typical injected activity of about 74 MBq (2 mCi). This higher radiation exposure to the patient, coupled with the clearly inferior spatial and contrast resolution of the planar and SPECT or SPECT/CT imaging with 111In-DTPA-octreotide, and the need for imaging at 2 time points (typically 4 and 24 h), are important drawbacks of 111In-DTPA-octreotide imaging, compared with the same day (typically 2 h from injection to scan completion) of the 68Ga-based somatostatin receptor PET/CT imaging agents (19). The estimated effective doses for 18F-FDG, 111In-DTPA-octreotide, 68Ga-DOTATATE, 68Ga-DOTATOC, and 68Ga-DOTANOC, using the average adult injected activity for a typical whole-body scan, are given in Table 3. All three 68Ga-labeled radiopharmaceuticals have EDs, per scan, of less than 5 mSv, with an estimated ED per scan for 111In-DTPA-octreotide of 6 mSv and for 18F-FDG of 7 mSv. Accordingly, these 68Ga-labeled somatostatin analogs provide higher quality images, with less total radiation exposure to the patient, than 111In-DTPA-octreotide and 18F-FDG. However, compared with somatostatin receptor scintigraphy, 18F-FDG demonstrates superior prognostic stratification for neuroendocrine tumor patients, with increasing 18F-FDG uptake correlating directly with increasingly aggressive tumors (20,21).
CONCLUSION
We have successfully measured 68Ga-DOTATATE human dosimetry in 6 adult subjects. These results provide the first, to our knowledge, measured human dosimetry for this radiopharmaceutical and will be of use to both investigators and patients. Additionally, we hope these results will help support ultimate approval by the Food and Drug Administration (FDA) of 68Ga-DOTATATE for PET imaging of somatostatin receptor–expressing tumors. Our data demonstrate that both organ-specific and ED exposures are acceptable for this investigational radiopharmaceutical. Similar to other reported 68Ga-labeled synthetic somatostatin analogs, the radiation exposure to the patient from 68Ga-DOTATATE is less than from 111In-DTPA-octreotide (the current FDA-approved somatostatin imaging agent) for a whole-body scan. 68Ga-DOTATATE also provides superior image quality than 111In-octreotide while significantly shortening examination time by a full day. There was no observed toxicity, immediate or delayed, on follow-up of 1 y, for 68Ga-DOTATATE.
Acknowledgments
We acknowledge Dr. Richard Baum for his invaluable advice regarding 68Ga-DOTATATE.
Footnotes
DISCLOSURE
This study was funded by the U.S. Department of Veterans Affairs Merit Review (“The Use of 68Ga-DOTATATE and 18F-FDG PET/CT Imaging in the Evaluation of Newly Diagnosed Lung Nodules and Lung Cancer”; grant I01BX007080). No other potential conflict of interest relevant to this article was reported.
References
- 1.van Essen M, Krenning EP, Kam BL, de Jong M, Valkema R, Kwekkeboom DJ. Peptide-receptor radionuclide therapy for endocrine tumors. Nat Rev Endocrinol. 2009;5:382–393. doi: 10.1038/nrendo.2009.105. [DOI] [PubMed] [Google Scholar]
- 2.van Vliet EI, Teunissen JJ, Kam BL, de Jong M, Krenning EP, Kwekkeboom DJ. Treatment of gastroenteropancreatic neuroendocrine tumors with peptide receptor radionuclide therapy. Neuroendocrinology. 2013;97:74–85. doi: 10.1159/000335018. [DOI] [PubMed] [Google Scholar]
- 3.Pfeifer A, Knigge U, Mortensen J, et al. Clinical PET of neuroendocrine tumors using 64Cu-DOTATATE: first-in-humans study. J Nucl Med. 2012;53:1207–1215. doi: 10.2967/jnumed.111.101469. [DOI] [PubMed] [Google Scholar]
- 4.Kwekkeboom DJ, de Herder WW, Kam BL, et al. Treatment with the radio-labeled somatostatin analog [177 Lu-DOTA 0,Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26:2124–2130. doi: 10.1200/JCO.2007.15.2553. [DOI] [PubMed] [Google Scholar]
- 5.Bodei L, Cremonesi M, Grana C, et al. Receptor radionuclide therapy with 90Y-[DOTA]0-Tyr3-octreotide (90Y-DOTATOC) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2004;31:1038–1046. doi: 10.1007/s00259-004-1571-4. [DOI] [PubMed] [Google Scholar]
- 6.Villard L, Romer A, Marincek N, et al. Cohort study of somatostatin-based radiopeptide therapy with [90Y-DOTA]-TOC versus [90Y-DOTA]-TOC plus [177Lu-DOTA]-TOC in neuroendocrine cancers. J Clin Oncol. 2012;30:1100–1106. doi: 10.1200/JCO.2011.37.2151. [DOI] [PubMed] [Google Scholar]
- 7.Kwekkeboom DJ, Teunissen JJ, Bakker WH, et al. Radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol. 2005;23:2754–2762. doi: 10.1200/JCO.2005.08.066. [DOI] [PubMed] [Google Scholar]
- 8.Hänscheid H, Sweeney RA, Flentje M, et al. PET SUV correlates with radionuclide uptake in peptide receptor therapy in meningioma. Eur J Nucl Med Mol Imaging. 2012;39:1284–1288. doi: 10.1007/s00259-012-2124-x. [DOI] [PubMed] [Google Scholar]
- 9.Pauwels S, Barone R, Walrand S, et al. Practical dosimetry of peptide receptor radionuclide therapy with 90Y-labeled somatostatin analogs. J Nucl Med. 2005;46(suppl 1):92S–98S. [PubMed] [Google Scholar]
- 10.Bodei L, Cremonesi M, Ferrari M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imaging. 2008;35:1847–1856. doi: 10.1007/s00259-008-0778-1. [DOI] [PubMed] [Google Scholar]
- 11.Haug AR, Auernhammer CJ, Wangler B, et al. 68Ga-DOTATATE PET/CT for the early prediction of response to somatostatin receptor-mediated radionuclide therapy in patients with well-differentiated neuroendocrine tumors. J Nucl Med. 2010;51:1349–1356. doi: 10.2967/jnumed.110.075002. [DOI] [PubMed] [Google Scholar]
- 12.Hartmann H, Zophel K, Freudenberg R, et al. Radiation exposure of patients during 68Ga-DOTATOC PET/CT examinations [German] Nuklearmedizin. 2009;48:201–207. doi: 10.3413/nukmed-0214. [DOI] [PubMed] [Google Scholar]
- 13.Pettinato C, Sarnelli A, Di Donna M, et al. 68Ga-DOTANOC: biodistribution and dosimetry in patients affected by neuroendocrine tumors. Eur J Nucl Med Mol Imaging. 2008;35:72–79. doi: 10.1007/s00259-007-0587-y. [DOI] [PubMed] [Google Scholar]
- 14.Virgolini I, Ambrosini V, Bomanji JB, et al. Procedure guidelines for PET/CT tumour imaging with 68Ga-DOTA-conjugated peptides: 68Ga-DOTA-TOC, 68Ga-DOTA-NOC, 68Ga-DOTA-TATE. Eur J Nucl Med Mol Imaging. 2010;37:2004–2010. doi: 10.1007/s00259-010-1512-3. [DOI] [PubMed] [Google Scholar]
- 15.About MIPAV. Center for Information Technology Web site. About MIPAV; Available at: http://mipav.cit.nih.gov/ [Google Scholar]
- 16.Foster DBP. Developing and Testing Integrated Multicompartment Models to Describe a Single-Input Multiple-Output Study Using the SAAM II Software System. Oak Ridge, TN: Oak Ridge Institute for Science and Education; 1999. [DOI] [PubMed] [Google Scholar]
- 17.Stabin MG, Siegel JA. Physical models and dose factors for use in internal dose assessment. Health Phys. 2003;85:294–310. doi: 10.1097/00004032-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 2005;46:1023–1027. [PubMed] [Google Scholar]
- 19.Krenning EP, Bakker WH, Kooij PP, et al. Somatostatin receptor scintigraphy with indium-111-DTPA-D-Phe-1-octreotide in man: metabolism, dosimetry and comparison with iodine-123-Tyr-3-octreotide. J Nucl Med. 1992;33:652–658. [PubMed] [Google Scholar]
- 20.Brix G, Lechel U, Glatting G, et al. Radiation exposure of patients undergoing whole-body dual-modality 18F-FDG PET/CT examinations. J Nucl Med. 2005;46:608–613. [PubMed] [Google Scholar]
- 21.Binderup T, Knigge U, Loft A, Federspiel B, Kjaer A. 18F-fluorodeoxyglucose positron emission tomography predicts survival of patients with neuroendocrine tumors. Clin Cancer Res. 2010;16:978–985. doi: 10.1158/1078-0432.CCR-09-1759. [DOI] [PubMed] [Google Scholar]