Abstract
Objectives
Nurses are at increased risk of occupational asthma, an observation that may be related to disinfectants exposure. Whether asthma history influences job type or job changes among nurses is unknown. We investigated this issue in a large cohort of nurses.
Methods
The Nurses' Health Study II is a prospective study of U.S. female nurses enrolled in 1989 (ages 24-44 years). Job status and asthma were assessed in biennial (1989-2011) and asthma-specific questionnaires (1998, 2003). Associations between asthma history at baseline (diagnosis before 1989, n=5, 311) and job type at baseline were evaluated by multinomial logistic regression. The relations of asthma history and severity during follow-up to subsequent job changes were evaluated by Cox models.
Results
The analytic cohort included 98,048 nurses. Compared to nurses in education/administration (likely low disinfectant exposure jobs), women with asthma history at baseline were less often employed in jobs with likely high disinfectant exposure, such as operating rooms (odds ratio: 0.73[95%CI, 0.63-0.86]) and ER/inpatient units (0.89[0.82-0.97]). During 22-year follow-up, nurses with a baseline history of asthma were more likely to move to jobs with lower exposure to disinfectants (hazard ratio: 1.13[1.07-1.18]), especially among those with more severe asthma (hazard ratio for mild persistent: 1.13; moderate persistent 1.26; severe persistent: 1.50, compared to intermittent asthma, P trend: 0.004).
Conclusion
Asthma history was associated with baseline job type and subsequent job changes among nurses. This may partly reflect avoidance of tasks involving disinfectant use, and may introduce bias in cross-sectional studies on disinfectant exposure and asthma in nurses.
Keywords: Asthma, Occupational, Nurses, Healthy worker effect, Disinfectants, Occupational exposure
Introduction
Workplace exposures are recognized as an important risk factor for adult-onset asthma.[1,2] Occupational exposures may also cause exacerbation of a pre-existing asthma,[3] and are associated with a more severe and uncontrolled disease.[4–6] Healthcare workers account for a large part of work-related asthma cases in the U.S.[7] and other developed countries,[8–10] especially among women.[11] Among healthcare workers, nurses, nurse aides and cleaning workers have been identified as higher risk occupations for asthma.[7,9,12–17] These findings may be explained partly by occupational exposures to cleaning and disinfecting products.[18] Studies have shown associations between cleaning products and disinfectants exposures and asthma onset,[12,19,20] severity, poor control and exacerbations,[5,21,22] particularly for nurses.[13,23] In addition a Swedish cross-sectional study found that nurses and healthcare workers performing cleaning tasks are more likely to have respiratory-related absence from work than the general population.[17]
Many cleaning and disinfecting products have been identified as respiratory irritants or sensitizers.[18] Associations with asthma have been observed for some specific exposures (e.g., quaternary ammonium compounds, ammonia, bleach, sprays),[14,22–24] but a better knowledge of the putative effects of specific substances is still needed.[18,25] Most existing studies are cross-sectional and subject - among other potential limitations - to a healthy worker effect bias.[26] Indeed, the potential tendency of workers with asthma to avoid or leave hazardous jobs may cause underestimation of the associations between occupational exposures and asthma in cross-sectional studies.[27]
Whether asthma history influences job type or job changes among nurses, and the possibility of a healthy worker effect bias in cross-sectional studies on disinfectant exposure and asthma, have never been investigated. In the Nurses' Health Study II (NHSII), a large, ongoing, prospective study of U.S. female nurses, we aimed to determine whether asthma history and asthma characteristics are associated with subsequent nursing job type and job changes, over a 22-year period.
Methods
Population
The Nurses' Health Study II (NHSII) began in 1989 when 116,430 female registered nurses from 15 US states, aged 25 to 44 years, completed a mailed questionnaire on their medical history and lifestyle characteristics.[28] Every two years, follow-up questionnaires have been sent to update information on potential risk factors and identify newly-diagnosed diseases. This investigation was approved by the Institutional Review Board at the Brigham and Women's Hospital, Boston, Massachusetts, United States.
Asthma
In all biennial questionnaires since 1991, the participants were asked if they had physician-diagnosed asthma, and if yes, when the diagnosis has occurred. Asthma history before baseline was defined by the report of physician-diagnosed asthma in 1991, with date of diagnosis “before September 1989” (Figure 1).
Figure 1.
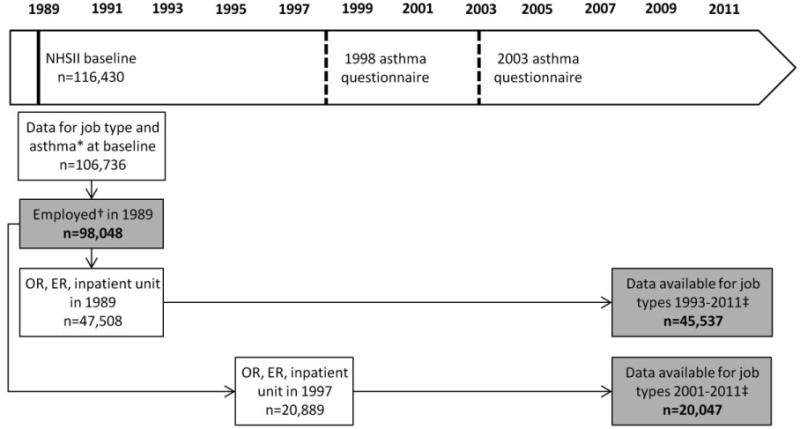
Flow chart of the population showing the different samples included in the analyses (shaded boxes), Nurses' Health Study II.
0R – Operating Room; ER – Emergency Room.
* The question on physician-diagnosed asthma and date of diagnosis was added for the first time in 1991. Asthma history at baseline was defined retrospectively by the report of physician-diagnosed asthma in 1991, with date of diagnosis “before September 1989”.
† Women unemployed in 1989 (excluded) were those who reported being “full-time homemaker”. They reported slightly less often asthma at baseline than employed women (4.9% vs. 5.4%, adjusted p=0.07).
‡ Women who returned at least one questionnaire and provided data on job type over the studied period.
Supplemental questionnaires on asthma were sent in 1998 and 2003, to all living women who had reported a physician diagnosis of asthma in earlier biennial questionnaire(s). More detailed information on dates of symptom onset and diagnosis, asthma symptoms, medications and hospitalizations for asthma were collected. Asthma cases were defined in 1998 and 2003 as participants who reiterated on the supplemental questionnaire that they had physician-diagnosed asthma, and reported using an asthma medication since diagnosis.[28] Age of diagnosis reported in supplemental asthma questionnaire was used to further classify nurses with a history of asthma according to age at asthma onset. In addition, asthma severity in 1998 and in 2003 was defined using a four-level (intermittent, mild persistent, moderate persistent, and severe persistent) classification system[16,29] based on the 1997 U.S. National Institutes of Health asthma guidelines.[30] According to current recommendations this definition would reflect both asthma severity and control.[16] This classification was based on a question on days kept from work or usual activities within the past 12 months because of asthma; four questions on days per week (over the past 4 weeks) with: (a) “wheeze or whistling sound in chest”, (b) “phlegm, sputum, or mucus from chest”, (c) “shortness of breath”, and (d) “cough”; and a question on “breathing between asthma flares”. Women with asthma who reported having ever had hay fever, seasonal allergies or allergic rhinitis in the 1998 supplemental asthma questionnaire were classified as having “allergic asthma”. Finally, latex allergy was evaluated in the biennial questionnaire in 2001.
Job type, job changes, and use of disinfectants
Data on work status and type of nursing job were collected at baseline (1989) and in follow-up questionnaires in 1993, 1997, 2001, 2009, and 2011, with the question “Which best describes your current employment status”. In 1989, options included nursing in inpatient or Emergency Room (ER), Operating Room (OR), outpatient or community; nursing education; nursing administration; other nursing; non nursing employment; or fulltime homemaker. Other options were included in follow-up questionnaires (e.g., Intensive Care Unit [ICU], disabled, retired, other). For the current analyses, job types were regrouped into 5 categories: “non-nursing job”, “education or administration nursing”, “outpatient nursing or other nurses”, “nursing in ER or inpatient units” (including ICU), “operating room nursing”. In 2009 and 2011, a general question regarding the frequency (days/week) of use of disinfectants at work have been added (“Thinking about your current job and the use of disinfectants [such as ethylene oxide, hydrogen peroxide, ortho-phtalaldehyde, formaldehyde, glutaraldehyde and bleach]: (a) On how many days per week, on average, do you clean medical instruments with disinfectants? (b) On how many days per week, on average, do you clean surfaces (like floors, tables) at work with disinfectants?”).
Statistical analyses
Associations between asthma history at baseline (diagnosis before 1989) and job type at baseline were evaluated by multinomial logistic regression. The association between asthma history and subsequent job changes over 1989-2011 was studied among nurses holding jobs with expected high disinfectant exposure at baseline, i.e. nursing in OR, ER, or inpatient units (Figure 1). For this analysis, Cox proportional hazard models were used to study the event “leave jobs with high exposure level” (i.e., transfer to outpatient/community nursing, nursing education/administration or other nursing; non nursing employment, fulltime homemaker or retirement) vs. “stay in a job with high exposure level”. Time-to-event was defined as the time to “definitive” transfer to a job with lower exposure level (i.e., transfer to a job with lower exposure level was considered only if the nurse did not report a “high exposure level job” in a subsequent questionnaire). Women were censored at the date of the last returned questionnaire with information on work status. Among women with asthma, associations between allergy status (assessed in 1998), latex allergy (assessed in 2001), and asthma severity (assessed in 1998 and/or in 2003) and subsequent job changes over 2001-2011 were studied among nurses holding jobs with expected high disinfectant exposure in 1997. Asthma severity was handled as a time-varying covariate in the Cox proportional hazard model.
In all analyses, potential confounders taken into account were age, race (white vs. nonwhite), ethnicity (Hispanic vs. non-Hispanic), smoking habits (non-, ex- or current-smoker) and Body Mass Index (BMI, <25, 25-29.9, >=30 kg/m2). A two-sided P-value <0.05 was considered statistically significant. All analyses were run using SAS 9 (SAS Institute, Cary, NC).
Results
A total of 106,736 women provided information on job type on the NHSII baseline questionnaire (1989), and completed the 1991 questionnaire (including for the first time a question on asthma). After excluding 8,688 women who reported “full-time homemaker” at baseline, the analytic cohort was comprised of 98,048 women (figure 1).
A history of asthma at baseline was reported by 5,311 participants (5%). Women with asthma at baseline were slightly older, more often overweight or obese, more often ex-smokers, and less often current-smokers than nurses without asthma (table 1). Most participants reported working as nurses in ER or inpatient unit (43%) or in outpatient/other nursing (34%) at baseline; other participants worked in nursing education/administration (13%), in OR (5%) or in non-nursing employment (4%). Small but significant differences in job types in 1989 were observed according to the covariates: nurses in ER or inpatient unit (mean age [SD]: 33.3 [4.7] years) or in OR (34.4 [4.5] years) were younger than nurses in education/administration (35.7 [4.3] years, p<0.001). They were also more often nonwhite (7% among nurses in ER or inpatient unit; 8% among OR nurses) than nurses in education/administration (6% nonwhite). Nurses in OR were less often overweight (19%) or obese (10%) than nurses in education/administration (20% overweight, 14% obese).
Table 1. Socio-demographic characteristics according to asthma status at baseline, Nurses' Health Study II.
| Asthma history before 1989 | |||
|---|---|---|---|
|
| |||
| No | Yes | P | |
| n | 92,737 | 5,311 | |
| Age, m (sd) | 34.3 (4.7) | 35.0 (4.6) | <0.001 |
| Age group | |||
| 24-30 | 18.4 | 14.0 | <0.001 |
| 30-35 | 31.9 | 30.6 | |
| 35-40 | 32.5 | 35.7 | |
| 40-44 | 17.2 | 19.8 | |
| Race / ethnicity | |||
| Non white, % | 7.1 | 7.0 | 0.73 |
| Hispanic, % | 1.8 | 2.1 | 0.16 |
| Smoking habits, % | |||
| Never smoker | 65.0 | 64.1 | <0.001 |
| Ex-smoker | 21.1 | 24.5 | |
| Current smoker | 13.8 | 11.3 | |
| missing | 0.1 | 0.1 | |
| BMI, % | |||
| <25 kg/m2 | 69.5 | 60.7 | <0.001 |
| 25-29.9 kg/m2 | 18.6 | 21.0 | |
| ≥ 30 kg/m2 | 11.3 | 17.6 | |
| missing | 0.6 | 0.7 | |
BMI – Body Mass Index
The frequency of disinfectant use was reported by participants for the first time in 2009, and there were clear differences in self-reported disinfectant use according to job type (figure 2). As expected, OR nurses reported the highest level of disinfectant use, with weekly use of disinfectants to clean surfaces (70%) or to clean instruments (36%), compared to nurses in ER or inpatient unit (52% and 30%, respectively), and to nurses in education / administration (13% and 4%).
Figure 2.
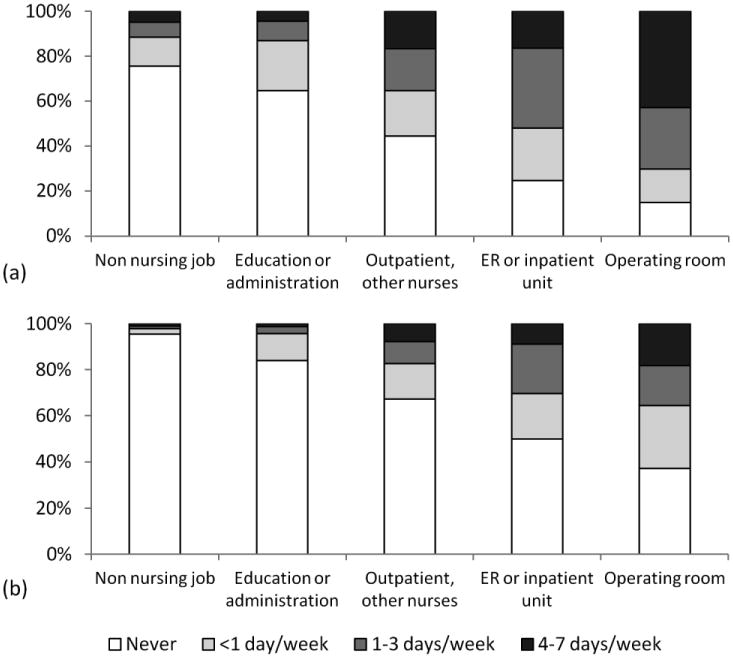
Reported frequency of use of disinfectants to clean (a) surfaces (n=54,738) and (b) medical instruments (n=54,843), according to job type, in 2009, Nurses' Health Study II.
ER – Emergency Room.
The distribution of job types among participants employed in 2009 (n=55,301) was as follows: non nursing job, 7%; education or administration nursing, 18%; outpatient or other nurses, 48%; ER or inpatient unit nursing, 23%; and operating room nursing, 5%.
Asthma history and job type at baseline
Compared to education/administration nurses, women with asthma history were less often employed in OR (odds ratio [95% confidence interval]: 0.73 [0.63-0.86], table 2) and in ER or inpatient units (0.89 [0.82-0.97]) at baseline. Similar results were observed in sensitivity analyses when a more stringent definition for asthma was used (i.e., case who reiterated having physician-diagnosed asthma in supplemental asthma questionnaires, with consistent date of diagnosis), and when studying job type in 1993 instead of job type in 1989 (results not shown). Analyses stratified by age at baseline showed relatively consistent associations across age groups (table E1). Among OR nurses, with regard to age at asthma onset, an association of similar magnitude was observed with childhood-onset asthma (age at diagnosis <18 years, 0.72 [0.56-0.91]) and adult-onset asthma (age at diagnosis ≥18 years, 0.68 [0.53-0.87]). For nursing in ER or inpatient units, an association was observed only with childhood-onset asthma (0.78 [0.68-0.90]) but not with adult-onset asthma (0.97 [0.85-1.10]).
Table 2. Association between asthma status at baseline and job type in 1989, Nurses' Health Study II.
| Asthma before 1989 | Age-adjusted | Multivariable* | ||||
|---|---|---|---|---|---|---|
| Job type in 1989, % | No (n=92,737) | Yes (n=5,311) | Odds ratio | 95% CI | Odds ratio | 95% CI |
| Non nursing job | 4.0 | 4.3 | 0.96 | 0.82-1.12 | 1.00 | 0.86-1.16 |
| Education or administration | 13.2 | 14.8 | 1 | - | 1 | - |
| Outpatient, other nurses | 34.1 | 36.4 | 0.97 | 0.89-1.06 | 0.99 | 0.91-1.08 |
| ER or inpatient unit | 43.2 | 40.3 | 0.89 | 0.82-0.97 | 0.89 | 0.82-0.97 |
| Operating room | 5.5 | 4.2 | 0.72 | 0.62-0.83 | 0.73 | 0.63-0.86 |
Adjusted for age, smoking status, body mass index, race and ethnicity. ER – Emergency Room. Results in bold are statistically significant.
Asthma history and characteristics, and subsequent job changes
The association between asthma history at baseline and job changes over 1989-2011 was studied in 45,537 nurses in OR, ER, or inpatient units in 1989 (table 3). Transition to a job with lower level of disinfectant exposure was observed in 68% of nurses without a history of asthma at baseline, and 71% of nurses with a history of asthma. In the multivariable-adjusted Cox proportional hazard model, nurses with asthma history had a significantly higher rate of transition to a job with lower exposure than nurses without asthma history (hazard ratio [95% confidence interval]: 1.13 [1.07-1.18]). The association between asthma and job changes was more pronounced in older women; the hazard ratio was 1.04 [0.92-1.17] for those 24-29.9 years; 1.05 [0.96-1.15] for 30-34.9 years; 1.24 [1.13-1.35] for 35-39.9 years; and 1.21 [1.07-1.37] for 40-44 years (P interaction: 0.02). In addition, a stronger association was observed among women working in OR at baseline (n=5,043), with a hazard ratio of 1.25 [1.04-1.50] for “leaving OR nursing”.
Table 3. Job changes according to asthma and asthma characteristics, among women employed in OR, ER or inpatient unit, Nurses' Health Study II.
| Person-Years | n event (Move to jobs with lower disinfectant exposure) | Age-adjusted | Multivariable* | |||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | Hazard ratio | 95% CI | |||
| Job changes over 1991-2011, among nurses in OR, ER or inpatient unit in 1989, n=45,537 | ||||||
| Asthma before 1989 | ||||||
| No | 623,166 | 29,330 | 1 | - | 1 | - |
| Yes | 31,270 | 1,632 | 1.13 | 1.07-1.19 | 1.13 | 1.07-1.18 |
|
| ||||||
| Job changes over 2001-2011, among nurses in OR, ER or inpatient unit in 1997, n=20,047 | ||||||
| Asthma before 1997 | ||||||
| No | 207,533 | 10,270 | 1 | - | 1 | - |
| Yes | 23,430 | 1,255 | 1.10 | 1.04-1.17 | 1.10 | 1.04-1.17 |
| Allergy | ||||||
| Asthma without allergy | 2,247 | 117 | 1 | - | 1 | - |
| Asthma with allergy | 17,223 | 922 | 1.04 | 0.86-1.26 | 1.05 | 0.87-1.28 |
| Latex allergy† | ||||||
| Asthma without latex allergy | 18,561 | 990 | 1 | - | 1 | - |
| Asthma with latex allergy | 1,026 | 56 | 1.06 | 0.81-1.39 | 1.08 | 0.83-1.43 |
| Asthma severity‡ | ||||||
| Intermittent | 8,329 | 411 | 1 | - | 1 | - |
| Mild persistent | 7,096 | 375 | 1.13 | 0.95-1.33 | 1.13 | 0.96-1.34 |
| Moderate persistent | 4,612 | 257 | 1.27 | 1.05-1.53 | 1.26 | 1.04-1.52 |
| Severe persistent | 737 | 50 | 1.50 | 1.04-2.17 | 1.50 | 1.03-2.17 |
Adjusted for age, smoking status, body mass index, race and ethnicity.
Evaluated in 2001.
Evaluated in 1998 and/or 2003. OR – Operating Room; ER – Emergency Room. Results in bold are statistically significant.
Similar results were observed for the association between asthma history and job changes over the period 2001-2011 among nurses in OR, ER, or inpatient units in 1997. In addition, increased asthma severity levels were associated with transition to a job with lower exposure (P for trend: 0.004). No difference was observed according to asthma subtypes based on allergy or latex allergy (table 3).
Discussion
Asthma history is associated with both baseline job type and subsequent job changes among U.S. nurses. Women with a history of asthma were less often employed in nursing jobs likely to involve high disinfectant exposure at baseline, and they were more likely to move to jobs involving lower level of exposure during follow-up. This association was more pronounced in nurses with more severe persistent asthma. These results may partly reflect avoidance of tasks involving disinfectant use, and may introduce bias in cross-sectional studies on disinfectant exposure and asthma in nurses.
This analysis, conducted in a large prospective study of nurses followed-up over 22 years, provides an example of the presence of health-related job selection among nurses. Several studies have suggested an association between asthma and avoidance of occupational exposures at risk for respiratory health.[26] Both initial and continuing selection processes have been observed: subjects with asthma before entering the workforce are more likely to choose work environments without hazardous exposures (“healthy worker hire effect”);[31–33] and after entry in the workforce, exposed workers experiencing new-onset or exacerbation of a pre-existing asthma are more likely to move to a non-exposed job (“health worker survivor effect”).[26,27] In the current analysis, women were aged 24-44 years at baseline, and were thus observed at different periods in their working life. Associations between asthma history and job type at baseline were observed among women with childhood-onset as well as adult-onset asthma, and were suggested in younger as well as older nurses. The results are thus likely to reflect both a healthy worker “hire” and “survivor” effect among nurses.
In the U.S. National Health and Nutrition Examination Survey (NHANES), a retrospective analysis of the association between childhood-asthma history and longest-held occupation showed that participants with a childhood-asthma history were more likely to work in health-related occupations (including, for instance, physicians, registered nurses or nursing aides).[34] Although these results may appear discrepant with the present results, they are compatible with our finding that women with asthma history avoid the specific nursing jobs likely to be more hazardous for respiratory health. To our knowledge, the only other study examining job transfer related to respiratory health in healthcare occupation was conducted in 769 Canadian apprentices exposed to high molecular weight agents, including 122 dental hygiene apprentices.[35] Among them (as well as in animal health technology apprentices), history of hay fever, and possibly asthma and respiratory symptoms were predictors of quitting apprenticeship.
Other large studies of the association between asthma and subsequent jobs types or job changes generally investigated a wide range of occupations [32,34,36] and were thus more subject to confounding by socio-economic factors or education level.[37] In the U.S. NHANES, participants with asthma history were found to achieve a higher education level than participants without asthma.[34] A prospective analysis in the French Epidemiological study on the Genetics and Environment of Asthma suggested that education and socioeconomic conditions may modulate asthma-based job selection.[31] The current findings, observed within a population of registered nurses likely to have a more homogeneous education level and socio-economic status, strengthen the hypothesis that the association between asthma and subsequent job choice reflects an actual avoidance of occupations that pose higher risk for respiratory health.
The hypothesis of an asthma-related job selection is further supported by the fact that asthma was well-characterized in this large population of nurses.[28] Although in most analyses asthma was defined by a simple question (ever doctor-diagnosed asthma), results were systematically confirmed when we used data collected in supplementary asthma questionnaires to refine asthma definition. Moreover, stronger associations were observed across increasing levels of asthma severity. Finally, results remained similar after adjusting for two important and common risk factors (body mass index, smoking status) for both asthma and other potential comorbidities (such as diabetes or cardiovascular diseases), supporting the specific role of asthma, rather than a more general poor health condition, in job selection.
Women with asthma were found to be less often employed and to select out of nursing jobs likely to involve high level of disinfectant exposures. As we expected, and consistent with previous reports,[38] the highest level of self-reported disinfectant use in 2009 was observed in OR nursing, and elevated levels were also observed in ER or other inpatient units. Although patterns of disinfectants use (frequency and type of products) may have varied within each job type over the study period (1989-2011), it is likely that higher exposure levels were constantly experienced in the same job types (OR, ER, inpatient units). However, disinfectant use may not be the only reason why asthmatic adults would avoid jobs such as nursing in OR, ER, or inpatient units [16], and no information was available in the current study about the specific reason for job change. Latex exposure, also at high risk for asthma, is likely to correlate with disinfectant exposure in nursing jobs. However, in the current study, latex allergy was not associated with job change among women with asthma. In addition, asthma history was associated with leaving nursing in OR, ER, or inpatient unit similarly over the whole study period (1989-2011) and over the period 2001-2011, while the use of powdered latex gloves have been largely reduced in healthcare settings after 2000.[19] This suggests that our observations are not driven by latex avoidance. Other potential exposures that may influence job choices or changes among nurses with asthma include shift-work or work-related stress. However, in the current analyses, stronger associations were observed when considering OR nursing alone. Nurses in OR are the one who reported the highest level of disinfectant exposures, but most (91%) did not report working night shifts. As for work-related stress, although no information was available in the current study, literature suggests that perception of the numerous workplace stressors vary considerably even between nurses working in the same practice area.[39] Individual work stress in nurses would thus be poorly predicted considering job type only. Overall, we believe these factors are likely to have a minor role in the current results in comparison to exposure to cleaning and disinfecting chemicals.
The absence of data on use of disinfectants by nurses for most of the follow-up period, preventing us to study potential change in disinfectant use according to asthma, was a limitation in this study. However, in healthcare facilities, nurses experience chemical exposures related not only to their own use of disinfectants, but also to cleaning and disinfection tasks performed by other workers in the same unit. It is also unclear to what extent most nurses have control of the disinfection tasks they perform and products they use, which depends on the healthcare facilities' policies. For these reasons, the nurses' overall exposure level - and by extension their exposure avoidance strategies - may be better represented by their job type than by their own self-reported use of disinfectants
Regardless of the exact reason why women with asthma would avoid nursing in OR, ER, or inpatient unit, the observed tendency may bias[26] the results of epidemiological studies on asthma among healthcare workers, including studies trying to examine the effect of exposure to various disinfectants and cleaning products. The association observed between asthma history and job changes during follow-up was modest (HR: 1.13), but nurses with asthma were already less often employed in jobs with high disinfectant exposure at baseline, suggesting that part of asthma-related selection had occurred before start of follow-up. Overall, this healthy worker effect could have a large impact[27] in cross-sectional studies on disinfectant exposure and asthma in nurses. To avoid underestimation of associations between occupational exposures and asthma outcomes, a longitudinal design is strongly preferred, with collection of data on complete occupational history and asthma outcomes over time. To study time-varying asthma characteristics (e.g., asthma severity or control, asthma exacerbations), appropriate statistical methods to adjust for time-varying confounding should also be considered.[27]
Among workers affected by occupational asthma, complete and definitive removal from exposure to the causal agent is associated with better clinical outcomes, and is generally recommended as the preferred management strategy.[2] However, if job transfer is needed to avoid the causal agent, adverse economic, personal and professional consequences are increased.[40] Our results suggest that beyond their impact on the disease itself, exposures associated with asthma in healthcare occupations, including disinfectant exposures, affect career choices and mobility patterns in individuals with asthma. Work trajectories may have an important impact on wage outcomes in nursing jobs,[41] and job transfer is thus likely to cause an additional socio-economic burden in affected workers.
As recently underlined, [18,25] there is an urgent need for further research to better identify the specific chemicals at risk for asthma in healthcare settings, before developing more adequate prevention and management strategies. Our findings emphasize the importance of addressing healthy worker effect bias in future respiratory epidemiological studies among healthcare workers. The choice of a longitudinal study design and an appropriate analytic strategy will be critical to evaluate accurately the effect of hazardous cleaning and disinfecting products on asthma.
What this study adds.
Nurses are at increased risk of occupational asthma, an observation that may be related to exposure to disinfectants. Whether asthma history is associated with subsequent job type or job changes among nurses is unknown.
In a prospective study of 98,048 U.S. female nurses followed-up over 22 years, women with a history of asthma were less often employed in nursing jobs likely to involve high disinfectant exposure at baseline, and they were more likely to move to jobs involving a lower level of exposure during follow-up.
Our findings emphasize the importance of addressing healthy worker effect bias in epidemiological studies that aim to identify asthmagens in healthcare settings.
Acknowledgments
We thank Francine Kauffmann for her participation in the study conception and her helpful advice during the conduct of the study.
Funding: Centers for Disease Control and Prevention R01 OH-10359; National Institutes of Health UM1 CA176726; Fondation pour la Recherche Médicale SPE20130326585; Fond de dotation Recherche en Santé Respiratoire 2013.
Footnotes
Contributorship statement: The authors' contributions were as follows: OD: study conception, statistical programming and data analysis, data interpretation, primary manuscript preparation; RV: study conception, assistance with statistical programming and data analysis, data interpretation and critical revision of the manuscript; JPZ and PKH: data interpretation and critical revision of the manuscript; FES: participation in the acquisition of the data, data interpretation and critical revision of the manuscript; ASW: data management, data interpretation and critical revision of the manuscript; NLM: study conception, data interpretation and critical revision of the manuscript; CAC: study conception, participation in the acquisition of the data, creation of the supplemental asthma questionnaires, data interpretation, critical revision of the manuscript. All authors approved the final version of the manuscript.
References
- 1.Torén K, Blanc PD. Asthma caused by occupational exposures is common - a systematic analysis of estimates of the population-attributable fraction. BMC Pulm Med. 2009;9:7. doi: 10.1186/1471-2466-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med. 2014;370:640–9. doi: 10.1056/NEJMra1301758. [DOI] [PubMed] [Google Scholar]
- 3.Henneberger PK, Redlich CA, Callahan DB, et al. An official american thoracic society statement: work-exacerbated asthma. Am J Respir Crit Care Med. 2011;184:368–78. doi: 10.1164/rccm.812011ST. [DOI] [PubMed] [Google Scholar]
- 4.Le Moual N, Siroux V, Pin I, et al. Asthma severity and exposure to occupational asthmogens. Am J Respir Crit Care Med. 2005;172:440–5. doi: 10.1164/rccm.200501-111OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Moual N, Carsin AE, Siroux V, et al. Occupational exposures and uncontrolled adult-onset asthma in the European Community Respiratory Health Survey II. Eur Respir J. 2014;43:374–86. doi: 10.1183/09031936.00034913. [DOI] [PubMed] [Google Scholar]
- 6.Boulet LP. Asthma control in the workplace. Eur Respir J. 2014;43:319–21. doi: 10.1183/09031936.00137713. [DOI] [PubMed] [Google Scholar]
- 7.Pechter E, Davis LK, Tumpowsky C, et al. Work-related asthma among health care workers: surveillance data from California, Massachusetts, Michigan, and New Jersey, 1993-1997. Am J Ind Med. 2005;47:265–75. doi: 10.1002/ajim.20138. [DOI] [PubMed] [Google Scholar]
- 8.Paris C, Ngatchou-Wandji J, Luc A, et al. Work-related asthma in France: recent trends for the period 2001-2009. Occup Env Med. 2012;69:391–7. doi: 10.1136/oemed-2011-100487. [DOI] [PubMed] [Google Scholar]
- 9.Liss GM, Buyantseva L, Luce CE, et al. Work-related asthma in health care in Ontario. Am J Ind Med. 2011;54:278–84. doi: 10.1002/ajim.20935. [DOI] [PubMed] [Google Scholar]
- 10.McDonald JC, Chen Y, Zekveld C, et al. Incidence by occupation and industry of acute work related respiratory diseases in the UK, 1992-2001. Occup Env Med. 2005;62:836–42. doi: 10.1136/oem.2004.019489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White GE, Seaman C, Filios MS, et al. Gender differences in work-related asthma: surveillance data from California, Massachusetts, Michigan, and New Jersey, 1993-2008. J Asthma. 2014;51:691–702. doi: 10.3109/02770903.2014.903968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kogevinas M, Zock JP, Jarvis D, et al. Exposure to substances in the workplace and new-onset asthma: an international prospective population-based study (ECRHS-II) Lancet. 2007;370:336–41. doi: 10.1016/S0140-6736(07)61164-7. [DOI] [PubMed] [Google Scholar]
- 13.Arif AA, Delclos GL, Serra C. Occupational exposures and asthma among nursing professionals. Occup Env Med. 2009;66:274–8. doi: 10.1136/oem.2008.042382. [DOI] [PubMed] [Google Scholar]
- 14.Dumas O, Donnay C, Heederik D, et al. Occupational exposure to cleaning products and asthma in hospital workers. Occup Env Med. 2012;69:883–9. doi: 10.1136/oemed-2012-100826. [DOI] [PubMed] [Google Scholar]
- 15.Henneberger PK, Mirabelli MC, Kogevinas M, et al. The occupational contribution to severe exacerbation of asthma. Eur Respir J. 2010;36:743–50. doi: 10.1183/09031936.00135109. [DOI] [PubMed] [Google Scholar]
- 16.Le Moual N, Varraso R, Zock JP, et al. Are operating room nurses at higher risk of severe persistent asthma? The Nurses' Health Study. J Occup Env Med. 2013;55:973–7. doi: 10.1097/JOM.0b013e318297325b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim JL, Torén K, Lohman S, et al. Respiratory symptoms and respiratory-related absence from work among health care workers in Sweden. J Asthma. 2013;50:174–9. doi: 10.3109/02770903.2012.760203. [DOI] [PubMed] [Google Scholar]
- 18.Siracusa A, De Blay F, Folletti I, et al. Asthma and exposure to cleaning products - a European Academy of Allergy and Clinical Immunology task force consensus statement. Allergy. 2013;68:1532–45. doi: 10.1111/all.12279. [DOI] [PubMed] [Google Scholar]
- 19.Delclos GL, Gimeno D, Arif AA, et al. Occupational risk factors and asthma among health care professionals. Am J Respir Crit Care Med. 2007;175:667–75. doi: 10.1164/rccm.200609-1331OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghosh RE, Cullinan P, Fishwick D, et al. Asthma and occupation in the 1958 birth cohort. Thorax. 2013;68:365–71. doi: 10.1136/thoraxjnl-2012-202151. [DOI] [PubMed] [Google Scholar]
- 21.Dumas O, Siroux V, Luu F, et al. Cleaning and asthma characteristics in women. Am J Ind Med. 2014;57:303–11. doi: 10.1002/ajim.22244. [DOI] [PubMed] [Google Scholar]
- 22.Arif AA, Delclos GL. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup Env Med. 2012;69:35–40. doi: 10.1136/oem.2011.064865. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez M, Jégu J, Kopferschmitt MC, et al. Asthma among workers in healthcare settings: role of disinfection with quaternary ammonium compounds. Clin Exp Allergy. 2014;44:393–406. doi: 10.1111/cea.12215. [DOI] [PubMed] [Google Scholar]
- 24.Vizcaya D, Mirabelli MC, Antó JM, et al. A workforce-based study of occupational exposures and asthma symptoms in cleaning workers. Occup Env Med. 2011;68:914–9. doi: 10.1136/oem.2010.063271. [DOI] [PubMed] [Google Scholar]
- 25.Heederik D. Cleaning agents and disinfectants: moving from recognition to action and prevention. Clin Exp Allergy. 2014;44:472–4. doi: 10.1111/cea.12286. [DOI] [PubMed] [Google Scholar]
- 26.Le Moual N, Kauffmann F, Eisen EA, et al. The healthy worker effect in asthma: work may cause asthma, but asthma may also influence work. Am J Respir Crit Care Med. 2008;177:4–10. doi: 10.1164/rccm.200703-415PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dumas O, Le Moual N, Siroux V, et al. Work related asthma. A causal analysis controlling the healthy worker effect. Occup Env Med. 2013;70:603–10. doi: 10.1136/oemed-2013-101362. [DOI] [PubMed] [Google Scholar]
- 28.Camargo CA, Jr, Weiss ST, Zhang S, et al. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–8. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 29.Barr RG, Somers SC, Speizer FE, et al. Patient factors and medication guideline adherence among older women with asthma. Arch Intern Med. 2002;162:1761–8. doi: 10.1001/archinte.162.15.1761. [DOI] [PubMed] [Google Scholar]
- 30.National Asthma Education and Prevention Program. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Heart, Lung, and Blood Institute, National Institutes of Health; 1997. [Google Scholar]
- 31.Dumas O, Smit LA, Pin I, et al. Do young adults with childhood asthma avoid occupational exposures at first hire? Eur Respir J. 2011;37:1043–9. doi: 10.1183/09031936.00057610. [DOI] [PubMed] [Google Scholar]
- 32.Olivieri M, Mirabelli MC, Plana E, et al. Healthy hire effect, job selection and inhalation exposure among young adults with asthma. Eur Respir J. 2010;36:517–23. doi: 10.1183/09031936.00125709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iwatsubo Y, Matrat M, Brochard P, et al. Healthy worker effect and changes in respiratory symptoms and lung function in hairdressing apprentices. Occup Env Med. 2003;60:831–40. doi: 10.1136/oem.60.11.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mazurek JM, Schleiff PL, Henneberger PK. Is childhood asthma associated with educational level and longest-held occupation? Am J Epidemiol. 2012;175:279–88. doi: 10.1093/aje/kwr300. [DOI] [PubMed] [Google Scholar]
- 35.Monso E, Malo JL, Infante-Rivard C, et al. Individual characteristics and quitting in apprentices exposed to high-molecular-weight agents. Am J Respir Crit Care Med. 2000;161:1508–12. doi: 10.1164/ajrccm.161.5.9906113. [DOI] [PubMed] [Google Scholar]
- 36.Butland BK, Ghosh R, Strachan DP, et al. Job choice and the influence of prior asthma and hay fever. Occup Env Med. 2011;68:494–501. doi: 10.1136/oem.2010.058065. [DOI] [PubMed] [Google Scholar]
- 37.Patel S, Henderson J, Jeffreys M, et al. Associations between socioeconomic position and asthma: findings from a historical cohort. Eur J Epidemiol. 2012;27:623–31. doi: 10.1007/s10654-012-9703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Donnay C, Denis MA, Magis R, et al. Under-estimation of self-reported occupational exposure by questionnaire in hospital workers. Occup Env Med. 2011;68:611–7. doi: 10.1136/oem.2010.061671. [DOI] [PubMed] [Google Scholar]
- 39.McVicar A. Workplace stress in nursing: a literature review. J Adv Nurs. 2003;44:633–42. doi: 10.1046/j.0309-2402.2003.02853.x. [DOI] [PubMed] [Google Scholar]
- 40.Vandenplas O, D'Alpaos V. Social consequences and quality of life in work-related asthma. In: Sigsgaard T, Heederik D, editors. Occupational asthma. Basel: Birkhäuser/Springer Verlag AG; 2010. pp. 271–80. [Google Scholar]
- 41.Ribas V, Dill JS, Cohen PN. Mobility for care workers: job changes and wages for nurse aides. Soc Sci Med. 2012;75:2183–90. doi: 10.1016/j.socscimed.2012.08.015. [DOI] [PubMed] [Google Scholar]


