Abstract
Japanese encephalitis virus (JEV) is a zoonotic pathogen transmitted by the infectious bite of Culex mosquitoes. The virus causes the development of the disease Japanese encephalitis (JE) in a small proportion of those infected, predominantly affecting children in eastern and southern Asia. Annual JE incidence estimates range from 50,000–175,000, with 25%–30% of cases resulting in mortality. It is estimated that 3 billion people live in countries in which JEV is endemic. The virus exists in an enzootic transmission cycle, with mosquitoes transmitting JEV between birds as reservoir hosts and pigs as amplifying hosts. Zoonotic infection occurs as a result of spillover events from the main transmission cycle. The reservoir avian hosts include cattle egrets, pond herons, and other species of water birds belonging to the family Ardeidae. Irrigated rice fields provide an ideal breeding ground for mosquitoes and attract migratory birds, maintaining the transmission of JEV. Although multiple vaccines have been developed for JEV, they are expensive and require multiple doses to maintain efficacy and immunity. As humans are a “dead-end” host for the virus, vaccination of the human population is unlikely to result in eradication. Therefore, vector control of the principal mosquito vector, Culex tritaeniorhynchus, represents a more promising strategy for reducing transmission. Current vector control strategies include intermittent irrigation of rice fields and space spraying of insecticides during outbreaks. However, Cx. Tritaeniorhynchus is subject to heavy exposure to pesticides in rice fields, and as a result, insecticide resistance has developed. In recent years, significant advancements have been made in the potential use of the bacterial endosymbiont Wolbachia for mosquito biocontrol. The successful transinfection of Wolbachia strains from Drosophila flies to Aedes (Stegomyia) mosquitoes has resulted in the generation of “dengue-refractory” mosquito lines. The successful establishment of Wolbachia in wild Aedes aegypti populations has recently been demonstrated, and open releases in dengue-endemic countries are ongoing. This review outlines the current control methods for JEV in addition to highlighting the potential use of Wolbachia-based biocontrol strategies to impact transmission. JEV and dengue virus are both members of the Flavivirus genus, and the successful establishment of Drosophila Wolbachia strains in Cx. Tritaeniorhynchus, as the principal vector of JEV, is predicted to significantly impact JEV transmission.
Methods
This review was prepared by searching the literature, including publication databases such as PubMed and Web of Science, on current methods used for vector control of Japanese encephalitis virus (JEV) and by providing an up-to-date review of Wolbachia-based biocontrol strategies for dengue and how these strategies could target Japanese encephalitis (JE).
Introduction
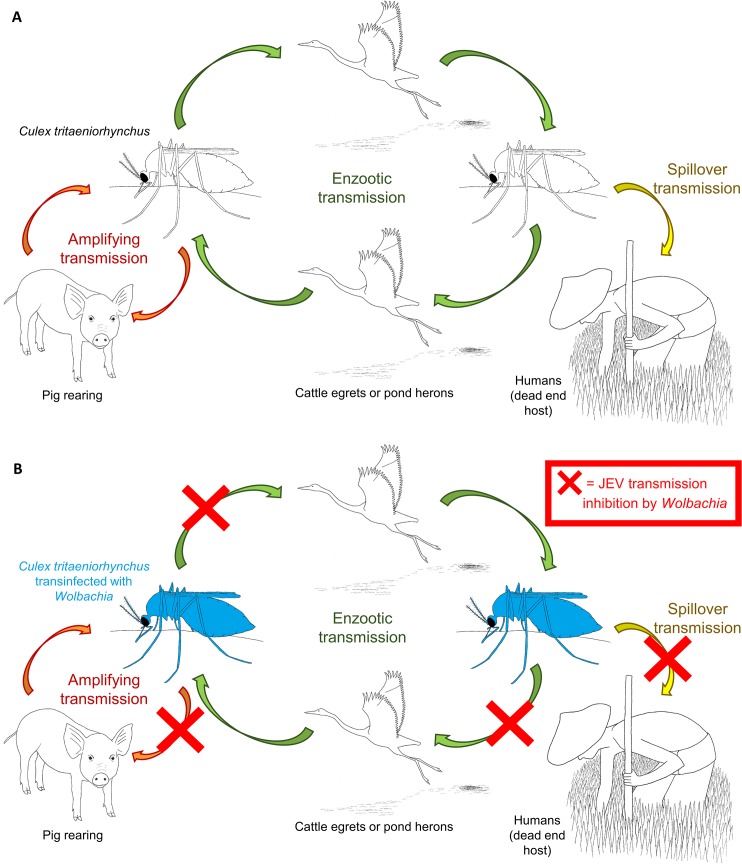
Numerous medically important arthropod-borne viruses (arboviruses) are transmitted to humans through the bites of infected mosquitoes. JEV is a neurotropic flavivirus transmitted primarily by Culex tritaeniorhynchus mosquitoes. The resulting disease, JE, is now endemic in large parts of Asia and the Pacific, with over 3 billion people at risk of infection [1,2]. It is estimated that less than 1% of human JEV infections result in encephalitic disease [3]. However, viral encephalitis caused by JEV can lead to fever, coma, seizures, paralysis, and death. JE is predominantly a disease of children in eastern and southern Asia, with annual incidence estimates ranging from 50,000–175,000 cases and 25%–30% of encephalitis cases resulting in mortality [3]. A further 30%–50% of JE survivors suffer serious neurological, cognitive, or psychiatric sequelae [4]. JEV exists in an enzootic transmission cycle among mosquitoes and domestic pigs, with the reservoir sylvatic bird hosts being primarily water birds from the Ardeidae family, including cattle egrets and pond herons (Fig 1A) [1]. As JEV-infected pigs act as amplifying hosts, domestic pig rearing is an important risk factor for human transmission. Irrigated rice fields provide an ideal breeding ground for Cx. tritaeniorhynchus and attract migratory birds, maintaining sylvatic transmission.
Fig 1. JEV transmission cycle and potential inhibition through the introduction of Wolbachia-infected Cx. tritaeniorhynchus mosquitoes.
(A) The enzootic sylvatic cycle is maintained by reservoir bird hosts (cattle egrets and pond herons) in close association with Cx. tritaeniorhynchus mosquitoes in rice fields. JEV is amplified in pigs, and zoonotic infection occurs as a result of spillover events, but human-to-human transmission is not known to occur at significant levels. (B) The JEV transmission cycle could be interrupted at various points using a Wolbachia-based biocontrol strategy in which JEV-refractory mosquitoes are unable to maintain the enzootic transmission cycles or transmit the virus to humans.
The geographic transmission zone extends from the China–Russia border region in the north to northern Australia in the south and from the Western Pacific islands in the east to the India–Pakistan border region in the west [5]. The epidemiology of JE can be divided into two distinct patterns based on climate. In temperate countries such as China and Japan, seasonal outbreaks are correlated with increased temperatures and rainfall in summer months. In contrast, tropical and subtropical countries in Southeast Asia have sporadic JE cases throughout the year, with reports peaking during the rainy season. The annual incidence of disease in Japan and Korea has declined because of improved living standards and vaccination programs [2]. However, the number of reported cases of human disease has increased in developing countries such as Bangladesh, Pakistan, and Indonesia because of increased population growth, intensified rice cultivation, and pig rearing. JEV also emerged in the Torres Strait Islands and spread to the far north of Australia in the late 1990s [6], highlighting the possibility that the virus could become established in other parts of the world. Transmission of JEV was traditionally considered to be mainly limited to rural areas, where the presence of mosquito vectors in rice fields coincides with pork production. However, several studies in urban areas have detected virus within the local mosquito vector populations, and seroconversion in urban vertebrate hosts (including humans) has been reported [7]. The human population has increased significantly within the past 50 years in both JEV-endemic regions and in areas where epidemics occur, with increasing trends in urbanization and an associated likely increase in urban agriculture. Therefore, the possibility that JEV transmission can occur in urban areas with the presence of vectors and a much greater human population density, combined with the potential for an increase in urban livestock, has the potential to significantly increase the number of cases in the future [7].
JEV and Mosquito Vectors
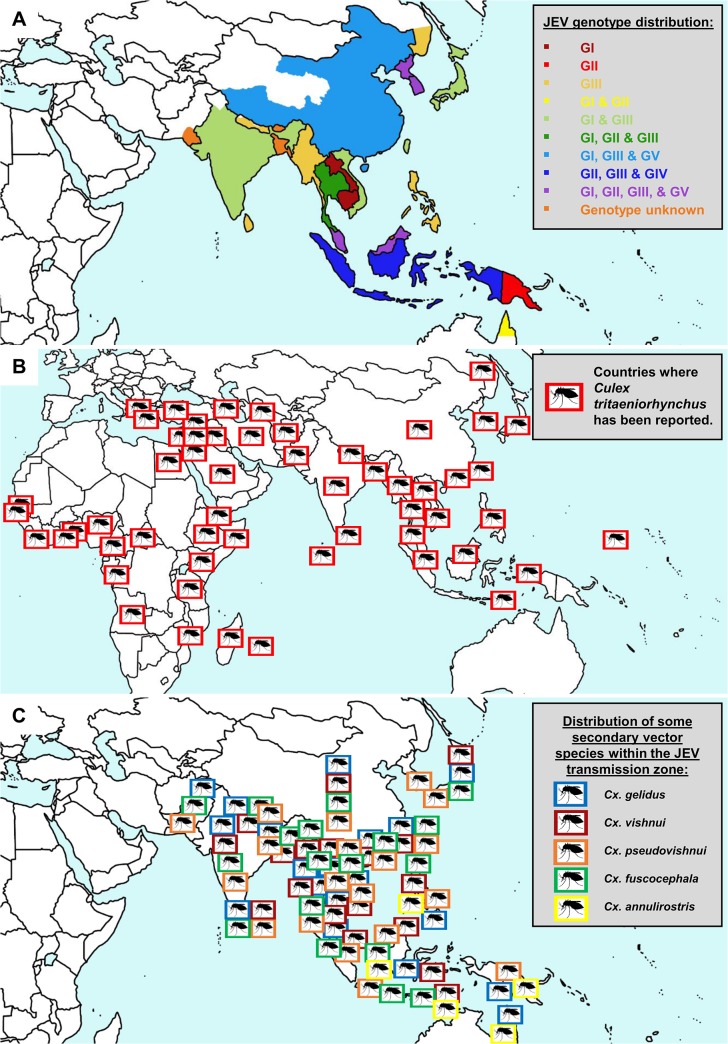
JEV is within the genus Flavivirus, which contains more than 70 enveloped viruses, including other medically important arboviruses such as dengue virus (DENV), West Nile virus (WNV), and yellow fever virus (YFV) [8]. Although first isolated in Japan in 1935, JEV appears to have evolved from its ancestral form to the present genotypic forms in Southeast Asia, over a relatively short period [9]. Phylogenetic studies have classified JEV into five geographically and epidemiologically distinct genotypes: GI to GV [9]. GIII had been the predominant genotype responsible for JE epidemics until the 1990s. However, studies have shown that GI is displacing GIII in many regions and has become the dominant genotype [10,11]. The emergence of GI throughout Asia is likely the result of viral, environmental, and host factors [12]. The principal vector of JEV is Cx. tritaeniorhynchus, which has a wide distribution including parts of Africa, the Middle East, and southern Europe in addition to the JE-endemic areas of Asia. A recent outbreak in China in 2013, resulting in 407 confirmed cases, was attributed to high JEV infection rates in Cx. tritaeniorhynchus (9.1 per 1,000 mosquitoes) using a maximum likelihood estimation [13]. The presence of this species was recently documented in parts of western Greece [14], highlighting the potential risk of JEV transmission in nonendemic areas outside of Asia. The principal vector of JEV in Australia is Cx. annulirostris [15], and other vector species such as Cx. Gelidus, Cx. Vishnui, Cx. Pseudovishnui, and Cx. fuscocephala have been implicated as secondary or regional vectors in certain endemic areas [16]. Fig 2 highlights the presence of JEV genotypes identified in JE-endemic areas, the worldwide geographical range of the principal mosquito vector Cx. Tritaeniorhynchus, and the distribution of some of the secondary vector species within the JEV transmission zone. The control of JEV has focused on vaccines and mosquito vector control (Table 1), as there are still no specific drug treatments available for infected patients.
Fig 2. JEV genotypes, the geographical range of Cx. tritaeniorhynchus and secondary vectors.
(A) The five recognized genotypes of JEV (I–V) are shown in regions where the genotype (G) has been confirmed to be responsible for JE epidemics. (B) The areas in which the principal mosquito vector, Cx. tritaeniorhynchus, has been documented highlight the wide geographical range of this species of mosquito. (C) The distribution of some of the secondary vector species is shown within the JEV transmission zone.
Table 1. Current and potential strategies for controlling Japanese encephalitis and the problems associated with each control method.
| Control Strategy | Difficulties for Implementation |
|---|---|
| Human vaccination | Expensive, multiple doses required, low rates in rural areas |
| Pig vaccination | Expensive, maternal antibodies reduce efficacy |
| Insecticide space spraying | Resistance from exposure to pesticides in rice fields, logistically difficult on a large scale |
| Indoor residual insecticide spraying | Cx. tritaeniorhynchus is exophilic |
| Intermittent irrigation | Logistically difficult in large areas with inadequate infrastructure |
| Genetically modified mosquitoes | Genetic modification of Cx. tritaeniorhynchus required, cost-effectiveness and implementation over large areas |
| Wolbachia-infected mosquitoes | Wolbachia transinfection of Cx. tritaeniorhynchus required: long-term effectiveness unknown |
JE Vaccination
The mouse brain-derived killed-inactivated JE-VAX was the only commercially available vaccine worldwide for several decades despite adverse effects, high production costs, and the need for 2–3 primary doses plus boosters [1,17]. Significant allergic and neurological side effects led to a halt in production of JE-VAX in 2006 [18,19]. A live-attenuated cell culture-derived JE vaccine, SA14-14-2, was developed in China in 1988 and has been administered to Chinese children since production commenced. SA14-14-2 is generated in primary hamster kidney (PHK) cells, and concerns with the quality control of production have prevented its application expanding in order to become an internationally available vaccine [20]. PHK-derived inactivated vaccines have been further adapted to be produced in African green monkey kidney (Vero) cells [21]. One vaccine (designated IC51) has been licensed since 2009 for use in countries including the United States, Europe, Australia, and India under various trade names, including IXIARO [22]. However, as there are concerns with this, the only WHO-recommended vaccine, because of side effects [23], additional vaccines are in various stages of development. A recombinant, live-attenuated vaccine based on a chimeric yellow fever/Japanese encephalitis virus (ChimeriVax-JE) was developed recently [24] and is now commercially available in Australia and Thailand. Although multiple vaccines have been developed for JEV, they are expensive and require multiple doses to maintain efficacy and immunity [25]. In addition, all registered vaccines are derived from GIII [11], which may be problematic given the replacement of GIII with GI as the dominant genotype. In most JEV-endemic rural settings, vaccination rates are often low, and vaccines are unlikely to result in eradication given humans are predominantly “dead-end” hosts, in that viremia is insufficient for onward transmission (Fig 1A). The potential of vaccinating pigs has also been explored, but the majority are slaughtered at 6–8 months. This means annual vaccination of piglets would be required, and the presence of maternal antibodies prevents the live-attenuated vaccine being effective in pigs less than 6 months of age. Therefore, there are too many limitations for this strategy to be effectively implemented [26]. As a result, mosquito vector control strategies represent a method more likely to eradicate JEV transmission than vaccination of humans or pigs, as mosquitoes are also responsible for maintaining transmission in reservoir bird hosts in the sylvatic cycle.
Current Vector Control and the Need for Novel Strategies
Vector control for JEV has predominantly been focused on environmental management of rice fields. Alternative wetting and drying of rice fields (intermittent irrigation) has shown success in reducing mosquito populations [27]. However, there are significant logistical difficulties with intermittent irrigation, including the requirement to apply this method to all rice fields over large areas [28], which is not possible with inadequate infrastructure. The use of insecticides (pyrethroids, organophosphates, and carbamates) has been limited for JEV vector control, although space spraying to target adult mosquitoes has been undertaken during outbreaks of JE in densely populated areas. However, the heavy use of pesticides in rice fields has led to significant levels of insecticide resistance in mosquitoes [29]. Logistical difficulties in employing large-scale insecticide treatment of rice fields, often in isolated rural villages, are also problematic for vector control of JEV. Indoor residual spraying using dichlorodiphenyltrichloroethane (DDT) and other chemicals has been ineffective in reducing JEV transmission, as Cx. tritaeniorhynchus is largely exophilic, resting outdoors [30].
Although climate change could further increase the geographical range of JEV transmission, in a similar way as predicted for DENV [31,32], the potential impact is yet to be determined. It is predicted that climate change will lead to increases in mosquito vector density, incursion of exotic mosquito species into novel areas, changes in agricultural practices, and migration of host reservoir birds. In particular, rice fields in JEV-endemic areas would likely become more arid and the subsequent increase in flooding, either through irrigation or extreme weather events, would provide optimal breeding conditions for Cx. tritaeniorhynchus [2]. Rapid outbreaks of JE are difficult to control, with traditional methods such as space spraying of insecticides having little impact because of the unpredictability and infrequency of outbreaks. Climate change may also influence migration patterns of birds, which may result in long-distance JEV dissemination in new areas. WNV is a closely related zoonotic flavivirus that has a similar enzootic transmission cycle with reservoir migratory birds. The introduction of the closely related WNV to novel areas has been strongly associated with bird migration [33,34], and climate change is likely to influence WNV outbreaks [35,36]. As there is very little known about the particular migration patterns of the avian reservoirs for JEV, the likely impact of climate change remains unknown [37]. In recent years, significant advances have been made in the potential use of the bacterial endosymbiont Wolbachia for mosquito biocontrol. This has included the successful transinfection of Cx. quinquefasciatus to create a wPip strain variant superinfection [38]. Wolbachia transinfection of Cx. tritaeniorhynchus could provide the basis for an environmentally friendly and cost-effective biocontrol strategy that could significantly impact JEV transmission (Box 1), which is likely to remain applicable even if JEV-endemic regions expand in the future as a result of climate change.
Box 1. Key Learning Points
Vaccines for JE have been developed but are expensive, require multiple doses, and are unlikely to result in eradication, as humans are a “dead-end” host.
Current vector control against the principal mosquito, Cx. tritaeniorhynchus, includes intermittent irrigation of rice fields and space spraying of insecticides during outbreaks.
Significant advancements have been made in the potential use of the bacterial endosymbiont Wolbachia for mosquito biocontrol of DENV.
Cx. tritaeniorhynchus do not harbor natural Wolbachia infections, and JEV is closely related to DENV (both in the Flavivirus genus).
Successful establishment of Wolbachia strains in Cx. tritaeniorhynchus can be reasonably expected to significantly impact JEV transmission.
Wolbachia-Based Mosquito Biocontrol Strategies
Wolbachia pipientis are maternally inherited alphaproteobacteria that live intracellularly in over 60% of all insect species [39]. Wolbachia were initially identified in the ovaries of Cx. pipiens mosquitoes, and these endosymbionts manipulate host reproduction to enhance their own transmission. In mosquitoes, Wolbachia induces a phenotype known as cytoplasmic incompatibility (CI), which results in the generation of unviable offspring when an uninfected female mates with a Wolbachia-infected male. In contrast, Wolbachia-infected females can produce viable progeny when they mate with both infected and uninfected males, resulting in a selective reproductive advantage over uninfected females. The CI phenotype allows the maternally transmitted Wolbachia to efficiently invade host populations without being infectious or moving horizontally between individuals [40].
During the 1970s and 1980s, several studies examined the effect of CI and the potential for application of the phenotype for vector control, in addition to elucidating the role of Wolbachia in producing CI in insect populations [41,42]. The discovery in the late 1990s of the virulent wMelPop strain in Drosophila melanogaster flies, which dramatically lowered the lifespan of its host [43], led to the idea that Wolbachia could also be used to manipulate insect longevity to reduce pathogen transmission. Mosquito-borne pathogens such as JEV require a significant extrinsic incubation period (EIP) in the female mosquito after uptake in an infectious blood meal before the pathogen migrates to the salivary glands to be transmitted to a host. For JEV the EIP is believed to be between 7 and 14 days, but it has been found to vary from 6 to 20 days dependent on temperature [16]. The wMelPop strain was proposed as having the potential to shorten the longevity of adult female mosquitoes so that the majority of females die before the EIP has elapsed [44,45]. More recently, several strains of avirulent Wolbachia were found to protect their native Drosophila hosts against infection by pathogenic RNA viruses [46,47]. Interestingly, major mosquito arboviral vectors such as Aedes (Stegomyia) aegypti and Cx. tritaeniorhynchus do not harbor natural Wolbachia infections. However, the successful establishment of Wolbachia strains in Ae. aegypti has now been accomplished, and the phenotypic effects suggest Wolbachia could significantly reduce arboviral transmission in naïve mosquito hosts.
Wolbachia and Dengue Vector Competence in Ae. aegypti Mosquitoes
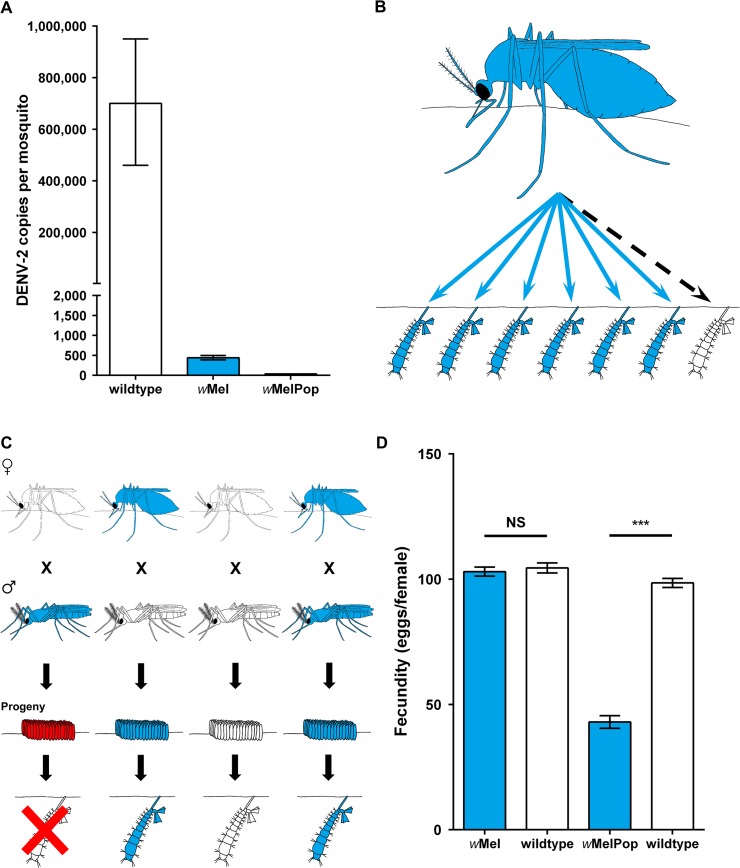
The first successful transinfection of Ae. aegypti used the wAlbB strain of Wolbachia from closely related Ae. albopictus mosquitoes [48]. Transinfection of Drosophila Wolbachia strains wMelPop-CLA and wMel was accomplished by first maintaining the bacteria in mosquito cell lines [49,50]. All three transinfected Wolbachia strains significantly reduce the vector competence of Ae. aegypti for DENV under laboratory conditions [50–52]. Both total (Fig 3A) and disseminated DENV is significantly reduced in Drosophila Wolbachia–infected mosquitoes. Furthermore, the presence of infectious DENV in mosquito saliva was not observed for Wolbachia-infected mosquitoes [50]. The wMel strain was also shown to result in complete blockage of DENV transmission in transinfected Ae. albopictus [53].
Fig 3. Wolbachia phenotypic effects for mosquito biocontrol.
(A) Pathogen inhibition of DENV in Ae. aegypti by transinfected Drosophila Wolbachia strains significantly decreases the DENV infection levels in mosquitoes 14 days after an infectious blood meal. (B) Maternal transmission of Wolbachia from female mosquitoes to progeny is close to 100% for transinfected Drosophila strains in mosquitoes. (C) Wolbachia-induced reproductive phenotype cytoplasmic incompatibility in mosquitoes allowing rapid invasion of uninfected mosquito populations. (D) Fitness costs (e.g., fecundity) of transinfected Drosophila Wolbachia strains to Ae. aegypti, which impact the ability of some strains to invade mosquito populations. (A) and (D) are adapted from [50].
Wolbachia Invasion of Wild Mosquito Populations
The applied use of Wolbachia strains to impact arboviral transmission requires invasion of wild mosquito populations. Wolbachia-infected females must vertically transmit the bacteria to their progeny at a high frequency (Fig 3B), and then CI (Fig 3C) can spread the infection. Wolbachia strains in Ae. aegypti show maternal transmission rates close to 100% and induce CI [48,50,54]. However, Wolbachia-infected mosquitoes can only spread and invade uninfected populations if the fitness costs such as fecundity (Fig 3D) to the mosquito are less than the fitness advantage that CI provides. Ae. aegypti mosquitoes infected with the virulent wMelPop-CLA strain are subject to greater fitness costs than mosquitoes infected with the avirulent wMel strain [50]. These significant fitness costs of the wMelPop-CLA strain were predicted to inhibit invasion of wild mosquito populations [55]. The invasive potential of the two Drosophila Wolbachia strains in Ae. aegypti was tested in large purpose-built semifield cages in northern Australia [56]. The results of these semifield experiments revealed that the wMel strain is likely to be the most successful at invading wild mosquito populations [50]. Ae. aegypti mosquitoes infected with the wMel strain were recently introduced into the wild through open releases in two locations near Cairns, Australia, after obtaining the necessary regulatory approval [57]. The wMel strain successfully invaded these two natural mosquito populations, reaching near-fixation in a few months following releases. After more than 2 years in the field, the infection has continued to demonstrate complete CI with minimal deleterious fitness effects. Although a low frequency of uninfected mosquitoes was detected, it would appear this was due to a low number of immigrants, and the infection appears to be stable under field conditions [58]. The persistence of an inhibitory effect on arboviral replication within wild Wolbachia-infected mosquitoes will be key to the success of any release program. Vector competence assays with field wMel-infected Ae. aegypti mosquitoes, collected 1 year following field release, indicated very low levels of DENV replication and dissemination [59]. The level of viral interference was similar in outcrossed laboratory lines and field-collected mosquitoes. However, the density of Wolbachia increased following blood feeding to a greater extent in field mosquitoes compared to laboratory colonies [59]. As Wolbachia density is correlated to viral interference in both native Drosophila [60] and transinfected Ae. Aegypti [50] hosts, repeated blood feeding on human hosts may increase the viral blocking phenotype in field mosquito populations.
JE as a Potential Target for Wolbachia-Based Biocontrol Strategies
There are several lines of evidence that would suggest that JE could be targeted using Wolbachia-based biocontrol. Firstly, JEV is part of the same genus as DENV (Flavivirus), so there is a reasonable expectation that Wolbachia strains would provide similar inhibitory effects in transinfected mosquitoes. In laboratory experiments, Wolbachia inhibits the replication of multiple DENV serotypes with similar efficacy [59]. Several studies have also shown that Wolbachia has a wide range of inhibitory effects on other mosquito-borne human pathogens when transinfected into naïve mosquito species (Table 2). For example, Drosophila Wolbachia strains also significantly inhibit the replication of Chikungunya virus (CHIKV) in Ae. aegypti [61]. Pathogen inhibition by transinfected Wolbachia strains also occurs for filarial nematodes [62] and malaria parasites [63,64]. The mechanism underlying viral interference is not fully known, but the density of Wolbachia strains in particular insect tissues influences the extent of viral interference [50]. Several mechanisms have been postulated for Wolbachia-mediated antiviral activity, including direct competition for space or cellular resources and effects on various immune signaling pathways; however, further investigation is required [65]. Drosophila Wolbachia strains grow to high densities in their native and transinfected hosts and provide strong inhibition of both insect viruses in Drosophila [46] and DENV in mosquitoes [50]. Therefore, successful establishment of Drosophila Wolbachia strains in Cx. tritaeniorhynchus is reasonably expected to have a significant impact on JEV transmission.
Table 2. List of mosquito vector species infected with native or transinfected Wolbachia strains and their relative inhibitory effect on vector competence of arboviruses.
| Mosquito Species | Wolbachia Strain (Native or Transinfected) | Arbovirus | Inhibitory Effect on Vector Competence | References |
|---|---|---|---|---|
| Ae. aegypti | wAlbB (transinfected) | DENV | ++ | [48,52] |
| wMel (transinfected) | DENV | ++ | [50,59] | |
| CHIKV | + | [61] | ||
| wMelPop (transinfected) | DENV | +++ | [50,51,54] | |
| CHIKV | +++ | [61] | ||
| Ae. albopictus | wAlbA and wAlbB (native) | DENV | + | [66] |
| wMel (transinfected) | DENV | ++ | [53] | |
| CHIKV | ++ | [67] | ||
| Ae. polynesiensis | wPolA (native) | DENV | - | [68] |
| wAlbB (transinfected) | DENV | ++ | [68] | |
| Cx. pipiens | wPip (native) | WNV | + | [69] |
Secondly, Cx. tritaeniorhynchus does not harbor a natural Wolbachia infection [70] and is responsible for the majority of JEV transmission. Although there are additional secondary vectors in Asia and Cx. annulirostris is responsible for the limited JEV transmission in northern Australia [15], the replacement of wild Cx. tritaeniorhynchus with JEV-refractory populations would likely have significant impacts on both virus transmission and human cases of disease. There is also the potential for transinfection of other secondary/regional vector species of importance if Wolbachia biocontrol in Cx. tritaeniorhynchus had brought eradication within reach. Other species of Culex mosquitoes responsible for human disease transmission are infected with native strains of Wolbachia. Indeed, the difference in vector competence of several Culex species may be due to the presence of these resident Wolbachia strains. For example, Cx. quinquefasciatus is infected with the wPip strain of Wolbachia and is generally less susceptible to WNV than Cx. tarsalis [71], which is not infected with Wolbachia. However, resident Wolbachia infections in mosquitoes do not impact arboviral transmission to the same extent as transinfected Drosophila Wolbachia strains.
The epidemiology of JE would also be favorable for Wolbachia-based biocontrol. The generation and release of “JEV-refractory” Cx. tritaeniorhynchus could break the transmission cycle (Fig 1B) at various points. Firstly, the enzootic sylvatic cycle in reservoir bird hosts would be inhibited, preventing circulation of JEV in the local release area. In addition, the prevention of reservoir host bird infections would likely reduce the potential geographical expansion of JEV through bird migration. Secondly, Wolbachia-infected Cx. tritaeniorhynchus mosquitoes would inhibit the enzootic amplification cycle in pigs, significantly reducing overall transmission. Finally, the spillover of JEV transmission to humans would also be inhibited by the presence of Wolbachia-infected Cx. tritaeniorhynchus. As Cx. tritaeniorhynchus are highly zoophilic, outbreaks of JE occur when there is a rapid increase in mosquito populations resulting in a spillover of JEV from the enzootic animal host cycle to humans. Therefore, the potential increase in drought/flooding of rice fields due to changing agricultural practices and climate change in JEV endemic areas could lead to bursts of vector proliferation during flooding, resulting in greater outbreaks in the future [2]. Vector control strategies during outbreaks that target adult mosquitoes are often ineffective, as transmission is already occurring and space spraying does not effectively target Cx. tritaeniorhynchus. Alternative mosquito control strategies that aim to suppress the mosquito population, such as the sterile insect technique (SIT) [72,73] or release of insects with a dominant lethal (RIDL) [74,75], could have a potential role in JE control. However, the likely need for repeated release of large numbers of sterile males for individual outbreaks of JE over a large transmission area would also pose both logistical and financial difficulties. Therefore, a Wolbachia-based biocontrol strategy that aims to simply replace the existing vector population with mosquitoes that are unable to transmit JEV would likely prevent outbreaks occurring even when there is a rapid increase in mosquito vector population densities.
Conclusions
Novel vector control methods for JE are needed, and Wolbachia-based biocontrol may provide sustainable, long-term control. The successful transinfection of Drosophila Wolbachia strains into Cx. tritaeniorhynchus is likely to result in JEV-refractory mosquito lines. The success of the first Ae. aegypti field trials in Australia indicates that a Wolbachia-based method of biocontrol is readily deployable in the field and also shows minimal environmental impact or safety concerns [76]. The stability of the arboviral blocking phenotype, in wild Ae. aegypti mosquitoes [59] and in the long-term evolutionary association between native Wolbachia strains in Drosophila flies [46], suggests an inhibitory effect on JEV with transinfected Cx. tritaeniorhynchus will be present for the medium to long term. If it is demonstrated that Wolbachia-infected JEV vectors cannot transmit the virus, it would suggest this biocontrol strategy could significantly reduce JE morbidity and mortality.
Boxes
Box 2. 5 Key Papers in the Field
Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K (2009) Past, Present, and Future of Japanese Encephalitis. Emerg Infect Dis 15: 1–7.
Solomon T, Ni H, Beasley DW, Ekkelenkamp M, Cardosa MJ, et al. (2003) Origin and Evolution of Japanese Encephalitis Virus in Southeast Asia. J Virol 77: 3091–3098.
Karunaratne SH, Hemingway J (2000) Insecticide Resistance Spectra and Resistance Mechanisms in Populations of Japanese Encephalitis Vector Mosquitoes, Culex tritaeniorhynchus and Cx. gelidus, in Sri Lanka. Med Vet Entomol 14: 430–436.
Walker T, Johnson PH, Moreira LA, Iturbe-Ormaetxe I, Frentiu FD, et al. (2011) The wMel Wolbachia Strain Blocks Dengue and Invades Caged Aedes aegypti Populations. Nature 476: 450–453.
Hoffmann AA, Montgomery BL, Popovici J, Iturbe-Ormaetxe I, Johnson PH, et al. (2011) Successful Establishment of Wolbachia in Aedes Populations to Suppress Dengue Transmission. Nature 476: 454–457.
Funding Statement
TW received a Wellcome Trust/Royal Society grant (101285/Z/13/Z): http://www.wellcome.ac.uk; https://royalsociety.org. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Solomon T. Control of Japanese encephalitis—within our grasp? The New England Journal of Medicine. 2006. August 31;355(9):869–71. [DOI] [PubMed] [Google Scholar]
- 2. Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K. Past, present, and future of Japanese encephalitis. Emerging Infectious Diseases. 2009. January;15(1):1–7. 10.3201/eid1501.080311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM, et al. Estimated global incidence of Japanese encephalitis: a systematic review. Bulletin of the World Health Organization. 2011. October 1;89(10):766–74, 74A-74E. 10.2471/BLT.10.085233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ding D, Hong Z, Zhao SJ, Clemens JD, Zhou B, Wang B, et al. Long-term disability from acute childhood Japanese encephalitis in Shanghai, China. The American Journal of Tropical Medicine and Hygiene. 2007. September;77(3):528–33. [PubMed] [Google Scholar]
- 5. Endy TP, Nisalak A. Japanese encephalitis virus: ecology and epidemiology. Current Topics in Microbiology and Immunology. 2002;267:11–48. [DOI] [PubMed] [Google Scholar]
- 6. Hanna JN, Ritchie SA, Phillips DA, Shield J, Bailey MC, Mackenzie JS, et al. An outbreak of Japanese encephalitis in the Torres Strait, Australia, 1995. The Medical Journal of Australia. 1996. September 2;165(5):256–60. [DOI] [PubMed] [Google Scholar]
- 7. Lindahl JF. Urbanisation and Vector-Borne Disease Emergence—a Possibility for Japanese Encephalitis Virus? British Journal of Virology. 2014;1(1):10–20. [Google Scholar]
- 8. Mukhopadhyay S, Kuhn RJ, Rossmann MG. A structural perspective of the Flavivirus life cycle. Nature Reviews Microbiology. 2005. January;3(1):13–22. [DOI] [PubMed] [Google Scholar]
- 9. Solomon T, Ni H, Beasley DW, Ekkelenkamp M, Cardosa MJ, Barrett AD. Origin and evolution of Japanese encephalitis virus in southeast Asia. Journal of Virology. 2003. March;77(5):3091–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nabeshima T, Loan HT, Inoue S, Sumiyoshi M, Haruta Y, Nga PT, et al. Evidence of frequent introductions of Japanese encephalitis virus from south-east Asia and continental east Asia to Japan. The Journal of General Virology. 2009. April;90(Pt 4):827–32. [DOI] [PubMed] [Google Scholar]
- 11. Fan YC, Chen JM, Chiu HC, Chen YY, Lin JW, Shih CC, et al. Partially neutralizing potency against emerging genotype I virus among children received formalin-inactivated Japanese encephalitis virus vaccine. PLoS Negl Trop Dis. 2012. September;6(9):e1834 10.1371/journal.pntd.0001834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schuh AJ, Ward MJ, Leigh Brown AJ, Barrett AD. Dynamics of the emergence and establishment of a newly dominant genotype of Japanese encephalitis virus throughout Asia. Journal of Virology 2014;88: 4522–4532. 10.1128/JVI.02686-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tao Z, Liu G, Wang M, Wang H, Lin X, Song L, et al. Molecular epidemiology of Japanese encephalitis virus in mosquitoes during an outbreak in China, 2013. Scientific Reports. 2014;4:4908 10.1038/srep04908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lytra I, Emmanouel N. Study of Culex tritaeniorhynchus and species composition of mosquitoes in a rice field in Greece. Acta Tropica. 2014. June;134:66–71. 10.1016/j.actatropica.2014.02.018 [DOI] [PubMed] [Google Scholar]
- 15. Hall-Mendelin S, Jansen CC, Cheah WY, Montgomery BL, Hall RA, Ritchie SA, et al. Culex annulirostris (Diptera: Culicidae) host feeding patterns and Japanese encephalitis virus ecology in northern Australia. Journal of Medical Entomology. 2012. March;49(2):371–7. [DOI] [PubMed] [Google Scholar]
- 16. van den Hurk AF, Ritchie SA, Mackenzie JS. Ecology and geographical expansion of Japanese encephalitis virus. Annual Review of Entomology. 2009;54:17–35. 10.1146/annurev.ento.54.110807.090510 [DOI] [PubMed] [Google Scholar]
- 17. Yun SI, Lee YM. Japanese encephalitis: The virus and vaccines. Human Vaccines & Immunotherapeutics. 2014;10(2):263–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Plesner A, Ronne T, Wachmann H. Case-control study of allergic reactions to Japanese encephalitis vaccine. Vaccine. 2000. March 6;18(17):1830–6. [DOI] [PubMed] [Google Scholar]
- 19. Plesner AM, Arlien-Soborg P, Herning M. Neurological complications to vaccination against Japanese encephalitis. European Journal of Neurology: the Official Journal of the European Federation of Neurological Societies. 1998. September;5(5):479–85. [DOI] [PubMed] [Google Scholar]
- 20. Halstead SB, Thomas SJ. New Japanese encephalitis vaccines: alternatives to production in mouse brain. Expert Review of Vaccines. 2011. March;10(3):355–64. 10.1586/erv.11.7 [DOI] [PubMed] [Google Scholar]
- 21. Monath TP. Japanese encephalitis vaccines: current vaccines and future prospects. Current Topics in Microbiology and Immunology. 2002;267:105–38. [DOI] [PubMed] [Google Scholar]
- 22. Jelinek T. Ixiaro: a new vaccine against Japanese encephalitis. Expert Review of Vaccines. 2009. November;8(11):1501–11. 10.1586/erv.09.112 [DOI] [PubMed] [Google Scholar]
- 23. Nothdurft HD, Jelinek T, Marschang A, Maiwald H, Kapaun A, Loscher T. Adverse reactions to Japanese encephalitis vaccine in travellers. The Journal of Infection. 1996. March;32(2):119–22. [DOI] [PubMed] [Google Scholar]
- 24. Guy B, Guirakhoo F, Barban V, Higgs S, Monath TP, Lang J. Preclinical and clinical development of YFV 17D-based chimeric vaccines against dengue, West Nile and Japanese encephalitis viruses. Vaccine. 2010. January 8;28(3):632–49. 10.1016/j.vaccine.2009.09.098 [DOI] [PubMed] [Google Scholar]
- 25. Solomon T. New vaccines for Japanese encephalitis. Lancet Neurol. 2008. February;7(2):116–8. 10.1016/S1474-4422(08)70004-8 [DOI] [PubMed] [Google Scholar]
- 26. Fan YC, Chen JM, Chen YY, Lin JW, Chiou SS. Reduced neutralizing antibody titer against genotype I virus in swine immunized with a live-attenuated genotype III Japanese encephalitis virus vaccine. Veterinary Microbiology. 2013. May 3;163(3–4):248–56. 10.1016/j.vetmic.2012.12.035 [DOI] [PubMed] [Google Scholar]
- 27. Keiser J, Maltese MF, Erlanger TE, Bos R, Tanner M, Singer BH, et al. Effect of irrigated rice agriculture on Japanese encephalitis, including challenges and opportunities for integrated vector management. Acta Tropica. 2005. July;95(1):40–57. [DOI] [PubMed] [Google Scholar]
- 28. Rajendran R, Reuben R, Purushothaman S, Veerapatran R. Prospects and problems of intermittent irrigation for control of vector breeding in rice fields in southern India. Annals of Tropical Medicine and Parasitology. 1995. October;89(5):541–9. [DOI] [PubMed] [Google Scholar]
- 29. Karunaratne SH, Hemingway J. Insecticide resistance spectra and resistance mechanisms in populations of Japanese encephalitis vector mosquitoes, Culex tritaeniorhynchus and Cx. gelidus, in Sri Lanka. Medical and Veterinary Entomology. 2000. December;14(4):430–6. [DOI] [PubMed] [Google Scholar]
- 30. Reisen WK, Milby MM. Population dynamics of some Pakistan mosquitoes: changes in adult relative abundance over time and space. Annals of Tropical Medicine and Parasitology. 1986. February;80(1):53–68. [DOI] [PubMed] [Google Scholar]
- 31. Naish S, Dale P, Mackenzie JS, McBride J, Mengersen K, Tong SL. Climate change and dengue: a critical and systematic review of quantitative modelling approaches. BMC Infectious Diseases. 2014. March 26;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Colon-Gonzalez FJ, Fezzi C, Lake IR, Hunter PR. The effects of weather and climate change on dengue. PLoS Neglected Tropical Diseases. 2013. November;7(11):e2503 10.1371/journal.pntd.0002503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Roehrig JT. West Nile virus in the United States—a historical perspective. Viruses. 2013. December;5(12):3088–108. 10.3390/v5123088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reisen WK, Wheeler SS, Garcia S, Fang Y. Migratory birds and the dispersal of arboviruses in California. The American Journal of Tropical Medicine and Hygiene. 2010. October;83(4):808–15. 10.4269/ajtmh.2010.10-0200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Harrigan RJ, Thomassen HA, Buermann W, Smith TB. A continental risk assessment of West Nile virus under climate change. Global Change Biology 2014;20: 2417–2425. 10.1111/gcb.12534 [DOI] [PubMed] [Google Scholar]
- 36. Wang G, Minnis RB, Belant JL, Wax CL. Dry weather induces outbreaks of human West Nile virus infections. BMC Infectious Diseases. 2010;10:38 10.1186/1471-2334-10-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mackenzie JS, Gubler DJ, Petersen LR. Emerging flaviviruses: the spread and resurgence of Japanese encephalitis, West Nile and dengue viruses. Nature Medicine. 2004. December;10(12 Suppl):S98–109. [DOI] [PubMed] [Google Scholar]
- 38. Walker T, Song S, Sinkins SP. Wolbachia in the Culex pipiens Group Mosquitoes: Introgression and Superinfection. Journal of Heredity. 2009. Mar-Apr;100(2):192–6. 10.1093/jhered/esn079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hilgenboecker K, Hammerstein P, Schlattmann P, Telschow A, Werren JH. How many species are infected with Wolbachia?—A statistical analysis of current data. FEMS Microbiology Letters. 2008. April;281(2):215–20. 10.1111/j.1574-6968.2008.01110.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hoffmann AA, Turelli M. Cytoplasmic incompatibility in insects In: O'Neill SL, Hoffmann AA, Werren JH, editors. Influential Passengers: Inherited Microorganisms and Arthropod Reproduction. New York: Oxford University Press; 1997. [Google Scholar]
- 41. Curtis CF. Population replacement in Culex fatigans by means of cytoplasmic incompatibility. 2. Field cage experiments with overlapping generations. Bulletin of the World Health Organization. 1976;53(1):107–19. [PMC free article] [PubMed] [Google Scholar]
- 42. Barr AR. Cytoplasmic incompatibility in natural populations of a mosquito, Culex pipiens L. Nature. 1980. January 3;283(5742):71–2. [DOI] [PubMed] [Google Scholar]
- 43. Min KT, Benzer S. Wolbachia, normally a symbiont of Drosophila, can be virulent, causing degeneration and early death. Proceedings of the National Academy of Sciences of the United States of America. 1997. September 30;94(20):10792–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sinkins SP, O'Neill SL. Wolbachia as a vehicle to modify insect populations In: Handler AJA, editor. Insect Transgenesis: Methods and Applications. Boca Raton: CRC Press; 2000. p. 271–88. [Google Scholar]
- 45. Brownstein JS, Hett E, O'Neill SL. The potential of virulent Wolbachia to modulate disease transmission by insects. Journal of Invertebrate Pathology. 2003. September;84(1):24–9. [DOI] [PubMed] [Google Scholar]
- 46. Hedges LM, Brownlie JC, O'Neill SL, Johnson KN. Wolbachia and virus protection in insects. Science. 2008. October 31;322(5902):702 10.1126/science.1162418 [DOI] [PubMed] [Google Scholar]
- 47. Teixeira L, Ferreira A, Ashburner M. The bacterial symbiont Wolbachia induces resistance to RNA viral infections in Drosophila melanogaster . PLoS Biology. 2008. December 23;6(12):e2 10.1371/journal.pbio.1000002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Xi Z, Khoo CC, Dobson SL. Wolbachia establishment and invasion in an Aedes aegypti laboratory population. Science. 2005. October 14;310(5746):326–8. [DOI] [PubMed] [Google Scholar]
- 49. McMeniman CJ, Lane AM, Fong AW, Voronin DA, Iturbe-Ormaetxe I, Yamada R, et al. Host adaptation of a Wolbachia strain after long-term serial passage in mosquito cell lines. Applied and Environmental Microbiology. 2008. November;74(22):6963–9. 10.1128/AEM.01038-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Walker T, Johnson PH, Moreira LA, Iturbe-Ormaetxe I, Frentiu FD, McMeniman CJ, et al. The wMel Wolbachia strain blocks dengue and invades caged Aedes aegypti populations. Nature. 2011. August 25;476(7361):450–3. 10.1038/nature10355 [DOI] [PubMed] [Google Scholar]
- 51. Moreira LA, Iturbe-Ormaetxe I, Jeffery JA, Lu G, Pyke AT, Hedges LM, et al. A Wolbachia symbiont in Aedes aegypti limits infection with dengue, Chikungunya, and Plasmodium . Cell. 2009. December 24;139(7):1268–78. 10.1016/j.cell.2009.11.042 [DOI] [PubMed] [Google Scholar]
- 52. Bian G, Xu Y, Lu P, Xie Y, Xi Z. The endosymbiotic bacterium Wolbachia induces resistance to dengue virus in Aedes aegypti . PLoS Pathogens. 2010. April;6(4):e1000833 10.1371/journal.ppat.1000833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Blagrove MS, Arias-Goeta C, Failloux AB, Sinkins SP. Wolbachia strain wMel induces cytoplasmic incompatibility and blocks dengue transmission in Aedes albopictus . P Natl Acad Sci USA. 2012. January 3;109(1):255–60. 10.1073/pnas.1112021108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. McMeniman CJ, Lane RV, Cass BN, Fong AW, Sidhu M, Wang YF, et al. Stable introduction of a life-shortening Wolbachia infection into the mosquito Aedes aegypti . Science. 2009. January 2;323(5910):141–4. 10.1126/science.1165326 [DOI] [PubMed] [Google Scholar]
- 55. Turelli M. Cytoplasmic incompatibility in populations with overlapping generations. Evolution; International Journal of Organic Evolution. 2010. January;64(1):232–41. 10.1111/j.1558-5646.2009.00822.x [DOI] [PubMed] [Google Scholar]
- 56. Ritchie SA, Johnson PH, Freeman AJ, Odell RG, Graham N, Dejong PA, et al. A secure semi-field system for the study of Aedes aegypti . Plos Neglected Tropical Diseases. 2011;5(3):e988 10.1371/journal.pntd.0000988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hoffmann AA, Montgomery BL, Popovici J, Iturbe-Ormaetxe I, Johnson PH, Muzzi F, et al. Successful establishment of Wolbachia in Aedes populations to suppress dengue transmission. Nature. 2011. August 25;476(7361):454–7. 10.1038/nature10356 [DOI] [PubMed] [Google Scholar]
- 58. Hoffmann AA, Iturbe-Ormaetxe I, Callahan AG, Phillips BL, Billington K, Axford JK, et al. Stability of the wMel Wolbachia Infection following invasion into Aedes aegypti populations. PLoS Neglected Tropical Diseases. 2014. September;8(9):e3115 10.1371/journal.pntd.0003115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Frentiu FD, Zakir T, Walker T, Popovici J, Pyke AT, van den Hurk A, et al. Limited Dengue Virus Replication in Field-Collected Aedes aegypti Mosquitoes Infected with Wolbachia . PLoS Neglected Tropical Diseases. 2014. February;8(2):e2688 10.1371/journal.pntd.0002688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Osborne SE, Iturbe-Ormaetxe I, Brownlie JC, O'Neill SL, Johnson KN. Antiviral protection and the importance of Wolbachia density and tissue tropism in Drosophila simulans . Applied and Environmental Microbiology. 2012. October;78(19):6922–9. 10.1128/AEM.01727-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. van den Hurk AF, Hall-Mendelin S, Pyke AT, Frentiu FD, McElroy K, Day A, et al. Impact of Wolbachia on infection with chikungunya and yellow fever viruses in the mosquito vector Aedes aegypti . PLoS Neglected Tropical Diseases. 2012;6(11):e1892 10.1371/journal.pntd.0001892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kambris Z, Cook PE, Phuc HK, Sinkins SP. Immune activation by life-shortening Wolbachia and reduced filarial competence in mosquitoes. Science. 2009. October 2;326(5949):134–6. 10.1126/science.1177531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bian G, Joshi D, Dong Y, Lu P, Zhou G, Pan X, et al. Wolbachia invades Anopheles stephensi populations and induces refractoriness to Plasmodium infection. Science. 2013. May 10;340(6133):748–51. 10.1126/science.1236192 [DOI] [PubMed] [Google Scholar]
- 64. Hughes GL, Koga R, Xue P, Fukatsu T, Rasgon JL. Wolbachia infections are virulent and inhibit the human malaria parasite Plasmodium falciparum in Anopheles gambiae . PLoS Pathogens. 2011. May;7(5):e1002043 10.1371/journal.ppat.1002043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Rainey SM, Shah P, Kohl A, Dietrich I. Understanding the Wolbachia-mediated inhibition of arboviruses in mosquitoes: progress and challenges. The Journal of General Virology. 2014. March;95(Pt 3):517–30. [DOI] [PubMed] [Google Scholar]
- 66. Mousson L, Zouache K, Arias-Goeta C, Raquin V, Mavingui P, Failloux AB. The native Wolbachia symbionts limit transmission of dengue virus in Aedes albopictus . PLoS Neglected Tropical Diseases. 2012;6(12):e1989 10.1371/journal.pntd.0001989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Blagrove MS, Arias-Goeta C, Di Genua C, Failloux AB, Sinkins SP. A Wolbachia wMel transinfection in Aedes albopictus is not detrimental to host fitness and inhibits Chikungunya virus. PLoS Neglected Tropical Diseases. 2013;7(3):e2152 10.1371/journal.pntd.0002152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Bian G, Zhou G, Lu P, Xi Z. Replacing a native Wolbachia with a novel strain results in an increase in endosymbiont load and resistance to dengue virus in a mosquito vector. PLoS Neglected Tropical Diseases. 2013;7(6):e2250 10.1371/journal.pntd.0002250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Glaser RL, Meola MA. The native Wolbachia endosymbionts of Drosophila melanogaster and Culex quinquefasciatus increase host resistance to West Nile virus infection. PloS One. 2010;5(8):e11977 10.1371/journal.pone.0011977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Tiawsirisup S, Sripatranusorn S, Oraveerakul K, Nuchprayoon S . Distribution of mosquito (Diptera: Culicidae) species and Wolbachia (Rickettsiales: Rickettsiaceae) infections during the bird immigration season in Pathumthani province, central Thailand. Parasitol Res. 2008. March;102(4):731–5. [DOI] [PubMed] [Google Scholar]
- 71. Goddard LB, Roth AE, Reisen WK, Scott TW. Vector competence of California mosquitoes for West Nile virus. Emerg Infect Dis. 2002. December;8(12):1385–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Andreasen MH, Curtis CF. Optimal life stage for radiation sterilization of Anopheles males and their fitness for release. Medical and Veterinary Entomology. 2005. September;19(3):238–44. [DOI] [PubMed] [Google Scholar]
- 73. Gilles J, Schetelig MF, Scolari F, Marec F, Capurro ML, Franz G, et al. Towards mosquito sterile insect technique programmes: Exploring genetic, molecular, mechanical and behavioural methods of sex separation in mosquitoes. Acta Tropica. 2014;132 Suppl:S178–S187. 10.1016/j.actatropica.2013.08.015 [DOI] [PubMed] [Google Scholar]
- 74. Alphey N, Alphey L, Bonsall MB. A model framework to estimate impact and cost of genetics-based sterile insect methods for dengue vector control. PloS One. 2011;6(10):e25384 10.1371/journal.pone.0025384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Phuc HK, Andreasen MH, Burton RS, Vass C, Epton MJ, Pape G, et al. Late-acting dominant lethal genetic systems and mosquito control. BMC Biology. 2007;5:11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Popovici J, Moreira LA, Poinsignon A, Iturbe-Ormaetxe I, McNaughton D, O'Neill SL. Assessing key safety concerns of a Wolbachia-based strategy to control dengue transmission by Aedes mosquitoes. Memorias do Instituto Oswaldo Cruz. 2010. December;105(8):957–64. [DOI] [PubMed] [Google Scholar]