Abstract
Eating breakfast may reduce appetite, body weight and CVD risk factors, but the breakfast type that produces the greatest health benefits remains unclear. We compared the effects of consuming a high-fibre breakfast, a non-fibre breakfast, or no-breakfast control on body weight, CVD risk factors and appetite. A total of thirty-six overweight participants (eighteen men and eighteen women) (mean age 33·9 (sd 7·5) years, mean BMI 32·8 (sd 4·7) kg/m2) were randomly assigned to consume oat porridge (n = 12), frosted cornflakes (n = 12) or a water control (n = 12) breakfast daily for 4 weeks. Appetite ratings were collected on the first day and weekly thereafter. Before and after the intervention, body weight, composition, blood pressure and resting energy expenditure (REE) were measured and a fasting blood sample was collected. Across the 4 weeks, fullness was higher and hunger was lower in the oat porridge group compared with the control group (P < 0·05). Mean weight change over the intervention was significantly different in the control group (−1·18 (sd 1·16) kg) compared with both the cornflakes (−0·12 (sd 1·34) kg) and oat porridge (+0·26 (sd 0·91) kg) groups (P < 0·05). However, the control group also showed elevated total cholesterol concentrations relative to the cornflakes and oat porridge groups (P < 0·05). There were no differences between groups in changes in body composition, blood pressure, REE or other CVD risk factors. In conclusion, although skipping breakfast led to weight loss, it also resulted in increased total cholesterol concentrations compared with eating either oat porridge or frosted cornflakes for breakfast.
Key words: Breakfast, Body weight, Oats, Cholesterol
Abbreviation: REE, resting energy expenditure
The proportion of individuals who regularly consume breakfast has declined in recent decades(1), during which time there has been an increase in obesity prevalence(2). Many epidemiological studies report that regular breakfast eaters tend to have a lower BMI than those who do not consume breakfast regularly(3–7). Furthermore, regular breakfast consumption is associated with lower risk of CVD(8), since consuming breakfast has been associated with a lower body weight, a reduction in total and LDL-cholesterol concentrations, lower blood pressure, and greater insulin sensitivity(9,10), which are modifiable risk factors for CVD. However, despite many epidemiological studies reporting associations between the regular consumption of breakfast and various health outcomes, there are a limited number of randomised controlled trials that would establish a plausible cause–effect relationship(11–13). Furthermore, some of the limited randomised controlled trials may be subject to biased research reporting(14).
Some researchers suggest that since breakfast consumption increases fullness and suppresses hunger and desire to eat(3,15), eating breakfast may decrease the likelihood of overeating or snacking later in the day(11,16). What is more, if the reduction in subsequent energy intake is greater than the net energy of the breakfast, overall daily energy intake would be lower when breakfast was eaten than when it was omitted, which could result in weight loss. Alternatively, one could argue that skipping breakfast does not lead to a compensatory increase in subsequent energy intake, which may lead to lower overall daily energy intake and weight loss(13).
The influence of differences in the composition of breakfast on changes in body weight has also not been adequately investigated using randomised controlled trials. Data from the Third National Health and Nutrition Examination Survey (NHANES III) show that individuals who eat a ready-to-eat cereal, cooked cereal, or quick-breads (muffins, pancakes, etc.) for breakfast have a significantly lower BMI than breakfast skippers or those who consume meat and eggs for breakfast(3). Some studies have reported that breakfasts high in fibre reduce subjective appetite more than those low in fibre(17,18). Oats are high in dietary fibre, including the soluble fibre β-glucan(19), which has been shown to reduce hypercholesterolaemia(20).
The aim of the present study was to investigate the effects of consuming a high-fibre oat porridge, an isoenergetic non-fibre frosted cornflakes breakfast, and a no-breakfast water control daily for 4 weeks on body-weight changes, subjective appetite and CVD risk factors in overweight but otherwise healthy individuals.
Participants and methods
Study design
We conducted a randomised, controlled parallel-arm study at the New York Obesity Nutrition Research Center at St Luke's Hospital. Volunteers were screened, and eligible candidates were enrolled and randomly assigned to one of three breakfast groups: (1) oat porridge (n = 12; six men and six women); (2) frosted cornflakes (n = 12; six men and six women); or (3) a no-breakfast control group (n = 12; six men and six women). Participants, stratified by sex, were randomised to the experimental groups using equal-sized blocks, with subsequent replacement as needed for dropouts. The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by St Luke's Roosevelt Hospital Center Institutional Review Board. Written informed consent was obtained from all participants, who received a financial incentive for taking part in the study. Data were collected during 1998 and 1999. The present study was registered at clinicaltrials.gov as NCT02035150.
Participants
Overweight (BMI > 25 kg/m2) candidates were included in the study if they were aged 18–65 years, weight stable (<5 % change in body weight during the past 3 months), and free from chronic disease. They were excluded if they smoked, took medications regularly, currently or previously abused drugs or alcohol, or were currently or intending to undertake a weight-loss diet or exercise programme. Females were excluded if they were pregnant or lactating. Participants were asked not to make changes to their physical activity pattern during the study.
A total of forty-six eligible participants were recruited from the general population of New York City via newspaper advertisements and flyers and enrolled in the study. A total of five participants dropped out during the course of the study (two men and three women), and replacements were recruited. Thus thirty-six participants (eighteen men and eighteen women) completed the study and were included in the final analyses. Participant demographics are displayed in Table 1.
Table 1.
Physical characteristics of study participants
(Mean values and standard deviations)
| Males (n 18) | Females (n 18) | All (n 36) | ||||
|---|---|---|---|---|---|---|
| Mean | sd | Mean | sd | Mean | sd | |
| Age (years) | 35·6 | 6·1 | 32·3 | 8·6 | 33·9 | 7·5 |
| Body weight (kg) | 96·1 | 11·7 | 91·0 | 16·6 | 93·5 | 14·5 |
| BMI (kg/m2) | 32·2 | 3·4 | 34·5 | 5·4 | 32·9 | 4·7 |
| Body fat (kg)* | 32·7 | 10·6 | 40·5 | 11·4 | 36·6 | 11·6 |
| Lean mass (kg)† | 63·4 | 6·7 | 50·6 | 6·5 | 57·0 | 9·2 |
*Measured by air displacement (BOD POD®).
†Calculated as the difference between total body weight and fat mass measured using air displacement.
Protocol
During the study, participants were required to report to the hospital at 08·30 hours following an overnight fast (>10 h) on each weekday for 4 consecutive weeks. On arrival, they were given 15 min to consume their assigned breakfast, which either consisted of oat porridge, frosted cornflakes or no-breakfast (control) (Table 2). The oat porridge breakfast consisted of oat porridge (Quick Oats; Quaker) made with whole milk (3·25 % fat) and heated in a microwave oven (according to the manufacturer's instructions) immediately before serving. The cornflakes breakfast consisted of frosted cornflakes (Frosted Flakes; Kellogg's) served with low-fat (1·7 % fat) milk, and the control breakfast consisted of 350 ml water in a cup. The volumes of the oat porridge and cornflakes breakfast meals were matched to the control breakfast by adding 230 ml water into the oat porridge breakfast, and by serving 190 ml water on the side in a cup for the cornflakes breakfast. All participants also received 200 ml of decaffeinated coffee with 12 ml non-dairy creamer (Coffee Mate; Nestlé) and a 1 g packet of artificial sweetener (Equal; The NutraSweet Company) to consume with their allocated breakfast. On Fridays, participants were provided with two portions of the breakfasts to take home and consume on the weekend days. They were asked to return the empty containers at the beginning of the following week to ensure compliance. On the first day of the intervention and at weekly intervals thereafter, subjective appetite ratings in response to the breakfasts were collected for 3 h. The laboratory assessments were undertaken before the start, and a day after the end of the 4-week intervention.
Table 2.
Nutritional composition of the breakfasts provided during the intervention
| Control | Cornflakes | Oat porridge | |
|---|---|---|---|
| Energy | |||
| kJ | 44 | 1473 | 1472 |
| kcal | 11 | 352 | 351 |
| Total (non-fibre) carbohydrate | |||
| g | 1·0 | 66·3 | 60·6 |
| % Energy | 38 | 75 | 69 |
| Which included | |||
| Sugars (g) | 0·8 | 35·5 | 8·9 |
| Protein | |||
| g | 0 | 7·3 | 14·3 |
| % Energy | 0 | 8 | 16 |
| Fat | |||
| g | 0·5 | 5·7 | 6·6 |
| % Energy | 43 | 15 | 17 |
| Fibre (g) | 0 | 0 | 8·0* |
*4 g soluble fibre and 4 g insoluble fibre.
Procedures, laboratory visits and assessments
Participants were asked to fast overnight (>10 h) and report to the laboratory at 08·30 hours. The laboratory technicians undertaking the pre and post study assessments were blinded to the experimental group of the participants. Pre and post anthropometrics, body composition, blood pressure and resting energy expenditure (REE) were assessed before a fasting venous blood sample was collected. The research assistant was not blinded to the appetite ratings collected during the study.
Anthropometric measurements
Participants were asked to void and to remove all outer clothing and shoes before weight was measured to the nearest 0·1 kg using an electronic scale (Weight-Tronix Inc.). Height was measured to the nearest 1 cm using a stadiometer (Holtain). Participants stood with their feet 25–30 cm apart, and their waists were measured with a flexible nylon tape to the nearest 0·1 cm in a horizontal plane midway between the lower margin of the last rib and the iliac crest(21). Body composition was estimated using air displacement plethysmography (BOD POD®; Life Measurements Inc.). Participants changed into a swimsuit and a swim cap before being seated inside the BOD POD. Total body volume was estimated twice, and the average was used to determine body fat mass based on the manufacturer built-in equations. Fat-free mass was calculated as the difference between total body weight and body fat mass measured using air displacement.
Resting energy expenditure
REE measurements were collected using a metabolic cart (Sensormedics). Standard gas calibrations were performed before each subject was tested. Participants rested comfortably on a bed in a semi-supine position, under thermoneutral conditions for 30 min, before a plastic transparent ventilated hood was placed over their head for 30 min. The first and final 5-min recordings were ignored, and the gas exchange results were converted to REE (kJ/d) using the formula by Weir(22). Gas concentration measurements were reproducible to within 2·6 % for a standard alcohol phantom.
Blood pressure
Blood pressure readings were obtained by sphygmomanometer. Participants rested for 15 min before blood pressure measurements were obtained. Systolic and diastolic measurements were recorded as phase I and V Korotkoff sounds(23). Three separate blood pressure measurements were obtained at 2-min intervals, and the means of the three values for both systolic and diastolic blood pressure were used for analysis.
Blood sample collection and analysis
A fasting blood sample was collected from an antecubital vein in the less dominant forearm using venepuncture. Samples were drawn into serum-separating tubes and allowed to clot for 30 min at room temperature before being centrifuged at 3000 g for 15 min at 4°C. Samples were stored at 4°C until analysis. Serum glucose, protein-bound glucose, insulin and lipids (total cholesterol, TAG and HDL) were assayed at a Center for Disease Control-certified chemistry laboratory (Quest Diagnostics). LDL-cholesterol was calculated using the Friedewald equation, based on the values obtained from total cholesterol, HDL-cholesterol and TAG(24). Homeostasis model assessment for insulin resistance (HOMA-IR) was calculated from fasting glucose and insulin(25). Leptin was determined in-house by RIA (Linco Research), with an intra-assay CV of 5·3 % and an inter-assay CV of 7·3 %.
Subjective appetite ratings
Ratings of hunger and fullness were obtained using a Likert-type rating scale. Participants were asked to select the number which best reflected their current hunger and fullness based on a line with anchor points at: 0, not at all; 20, slightly; 40, moderately; 60, quite; 80, very; and 100, extremely. Appetite ratings were collected when participants arrived at the laboratory immediately before breakfast (baseline), immediately following the consumption of the breakfast (0 min) and at 30, 60 90, 120, 150 and 180 min later. Participants completed appetite ratings at these times on the first day of the intervention and weekly thereafter.
Statistical analyses
SPSS software (version 21; IBM) was used for data entry and analysis. All data are reported as mean values with their standard errors unless otherwise stated. Sex was examined as a factor on the outcome variables, but there were no significant differences between the men and women for any of the outcome variables; hence the data were pooled.
Between-group comparisons of the pre-intervention data were performed using ANOVA with breakfast groups as a between-subjects factor. Post-intervention outcomes and the changes in the outcome variables from pre- to post-intervention were analysed using ANCOVA with the pre-intervention measure as a covariate. If significant effects were observed between the groups, post hoc pairwise comparisons were made by Fisher's least significant difference (LSD) test.
The pre-breakfast appetite ratings for each week were compared between the groups by ANOVA. There were significant differences in the pre-breakfast subjective hunger and fullness ratings between the groups; therefore the change from baseline was used in subsequent analyses. The changes from baseline subjective appetite ratings were examined using repeated-measures ANOVA, with week and time point as the within-subject factors and breakfast group as the between-subject factor. Significance was set at two-tailed P < 0·05.
Results
Physical characteristics
There were no between-group differences for any of the pre-intervention physical characteristics (Table 3). When controlling for initial body weight, there was a significant main effect of breakfast group for final body weight (F(2,32) = 6·4; P = 0·005) and change in body weight (F(2,32) = 6·0; P = 0·006). Pairwise comparisons revealed that final body weight was significantly lower in the control group than in both the cornflakes (P = 0·033) and oat porridge breakfast groups (P = 0·006), and change in body weight was greater in the control group compared with the cornflakes (P = 0·025) and oat porridge breakfast groups (P = 0·002). However, there were no significant differences between the cornflakes and oat porridge breakfast groups for final body weight or change in body weight over the intervention period when controlling for initial body weight. There were no significant between-group differences in final body fat mass, fat-free mass, waist circumference, waist:hip ratio, blood pressure and REE or the change in these variables over the intervention period when the pre-intervention measures were controlled (Table 3).
Table 3.
Physical characteristics of the participants
(Mean values and standard deviations)
| Group… Sex… Ethnicity… |
Control (n = 12) (6 male, 6 female) (4 W, 3 B, 3 H, 1 A, 1 O) |
Cornflakes (n = 12) (6 male, 6 female) (6 W, 3 B, 2 H, 2 A, 1 O) |
Oat porridge (n = 12) (6 male, 6 female) (6 W, 4 B, 1 H, 1 O) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Change | Pre | Post | Change | Pre | Post | Change | ||||||||||
| Mean | sd | Mean | sd | Mean | sd | Mean | sd | Mean | sd | Mean | sd | Mean | sd | Mean | sd | Mean | sd | |
| Body weight (kg)† | 96·9 | 15·0 | 95·7 | 14·5 | −1·2 | 1·2 | 88·8 | 14·0 | 88·7* | 13·9 | −0·1* | 1·3 | 95·1 | 14·4 | 95·4* | 14·1 | 0·3* | 0·9 |
| Waist (cm) | 103·5 | 13·5 | 103·5 | 13·5 | 0·1 | 0·8 | 97·4 | 10·0 | 97·8 | 10·5 | 0·4 | 0·5 | 98·9 | 10·7 | 100·4 | 9·7 | 1·5 | 0·7 |
| Waist:hip ratio | 0·91 | 0·11 | 0·91 | 0·12 | 0·01 | 0·02 | 0·88 | 0·73 | 0·88 | 0·80 | 0·01 | 0·03 | 0·87 | 0·11 | 0·88 | 0·10 | 0·01 | 0·02 |
| Fat mass (kg)‡ | 38·0 | 10·5 | 37·6 | 11·0 | 0·95 | 3·3 | 35·4 | 9·6 | 34·8 | 12·5 | 0·94 | 3·3 | 36·5 | 14·8 | 36·9 | 14·6 | 0·77 | 2·7 |
| Fat-free mass (kg)§ | 58·9 | 8·4 | 58·0 | 6·9 | −0·9 | 3·1 | 53·4 | 10·9 | 53·8 | 12·3 | 0·3 | 3·7 | 58·6 | 7·7 | 58·5 | 8·8 | −0·1 | 2·7 |
| Blood pressure: | ||||||||||||||||||
| Systolic (mmHg) | 118·3 | 3·1 | 116·3 | 2·9 | −2·0 | 7·9 | 117·0 | 3·1 | 117·8 | 2·9 | 0·8 | 4·0 | 119·5 | 3·1 | 119·3 | 2·9 | −0·1 | 3·0 |
| Diastolic (mmHg) | 80·0 | 2·4 | 78·2 | 2·3 | −1·7 | 5·5 | 73·3 | 2·4 | 73·6 | 2·3 | 0·2 | 6·0 | 75·5 | 2·4 | 78·3 | 2·3 | 2·8 | 8·2 |
| REE (kJ/d)‖ | 8374 | 1577 | 7649 | 1507 | −354 | 963 | 7322 | 1033 | 7180 | 1048 | −24 | 552 | 8068 | 1901 | 8234 | 1867 | −69 | 729 |
W, white; B, black; H, Hispanic; A, Asian; O, other; REE, resting energy expenditure.
*Mean value was significantly different from that of the control group (P < 0·05).
†ANCOVA using the pre-intervention measure as a covariate showed a significant effect of breakfast group for body weight (P = 0·006).
‡Measured by air displacement (BOD POD®).
§Calculated from the difference between total body weight and fat mass measured using air displacement.
‖REE assessed by indirect calorimetry using a ventilated hood and metabolic cart.
Metabolic risk factors
There were no significant between-group differences in any of the pre-intervention metabolic risk factors (Table 4). There were no main effects of breakfast group for final values, or for the change from pre- to post-intervention in fasting serum glucose, protein-bound glucose, insulin, plasma leptin or HOMA-IR when pre-intervention values were controlled (Table 4).
Table 4.
Fasting glucose, insulin and lipid profiles pre- and post-intervention and change over the intervention†
(Mean values with their standard errors)
| Control | Cornflakes | Oat porridge | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Change | Pre | Post | Change | Pre | Post | Change | ||||||||||
| Mean | sem | Mean | sem | Mean | sem | Mean | sem | Mean | sem | Mean | sem | Mean | sem | Mean | sem | Mean | sem | |
| Serum glucose (mmol/l) | 5·1 | 0·1 | 5·0 | 0·1 | −0·1 | 0·1 | 5·1 | 0·1 | 5·1 | 0·1 | −0·04 | 0·2 | 4·8 | 0·1 | 5·0 | 0·1 | 0·2 | 0·1 |
| Glycated albumin (mg/g) | 0·97 | 0·02 | 0·9 | 0·02 | −0·01 | 0·02 | 0·93 | 0·02 | 0·91 | 0·02 | −0·02 | 0·01 | 0·96 | 0·02 | 0·93 | 0·02 | −0·03 | 0·03 |
| Serum insulin (pmol/l) | 143·4 | 23·2 | 128·2 | 15·1 | −15·1 | 15·0 | 134·3 | 16·4 | 132·0 | 15·2 | −2·3 | 11·5 | 121·2 | 16·9 | 117·3 | 15·5 | −7·1 | 6·5 |
| Plasma leptin (μg/l) | 21·5 | 4·6 | 19·5 | 4·2 | −2·0 | 1·8 | 20·2 | 4·6 | 22·5 | 4·3 | 2·3 | 1·2 | 24·5 | 4·6 | 23·1 | 4·2 | −1·4 | 2·3 |
| HOMA-IR | 4·7 | 0·8 | 4·1 | 0·5 | −0·6 | 0·5 | 4·3 | 0·5 | 4·3 | 0·5 | −0·1 | 0·3 | 3·8 | 0·6 | 3·8 | 0·6 | 0·1 | 0·2 |
| Plasma cholesterol (mmol/l) | ||||||||||||||||||
| Total | 5·6 | 0·5 | 5·9 | 0·5 | 0·4 | 0·1 | 5·3 | 0·3 | 5·2* | 0·3 | −0·1* | 0·2 | 5·1 | 0·3 | 4·9* | 0·3 | −0·3* | 0·1 |
| HDL | 1·12 | 0·11 | 1·16 | 0·12 | 0·04 | 0·03 | 1·25 | 0·10 | 1·30 | 0·10 | 0·05 | 0·05 | 1·02 | 0·41 | 1·01 | 0·05 | −0·02 | 0·03 |
| LDL | 3·70 | 0·39 | 3·86 | 0·48 | 0·16 | 0·21 | 3·53 | 0·24 | 3·41 | 0·22 | −0·12 | 0·17 | 3·50 | 0·32 | 3·19 | 0·28 | −0·30 | 0·15 |
| Plasma TAG (mmol/l) | 1·66 | 0·41 | 1·77 | 0·41 | 0·11 | 0·15 | 1·07 | 0·20 | 1·05 | 0·14 | −0·02 | 0·15 | 1·34 | 0·25 | 1·48 | 0·30 | 0·14 | 0·19 |
HOMA-IR, homeostasis model assessment for insulin resistance.
*Mean value was significantly different from that of the control group (P < 0·05).
†The effect of breakfast group was analysed using ANOVA for pre-intervention measures, and ANCOVA with the pre-intervention value as a covariate for the post-intervention and for the change (post–pre) in measures.
However, both post-intervention total cholesterol concentrations (F(2,32) = 4·895; P = 0·014) and change in total cholesterol concentrations (F(2,32) = 4·895; P = 0·014) were significantly different between the groups when controlling for pre-intervention total cholesterol concentrations. Pairwise comparisons revealed that post-intervention total cholesterol concentrations were significantly higher in the control group compared with both the cornflakes (P = 0·040) and oat porridge breakfast groups (P = 0·005), although the cornflakes and oat porridge groups did not differ from each other (Table 4). When pre-intervention values were controlled, there was no difference in post-intervention LDL- or HDL-cholesterol concentrations, or the change from pre- to post-intervention between any of the groups.
Subjective ratings
Hunger ratings
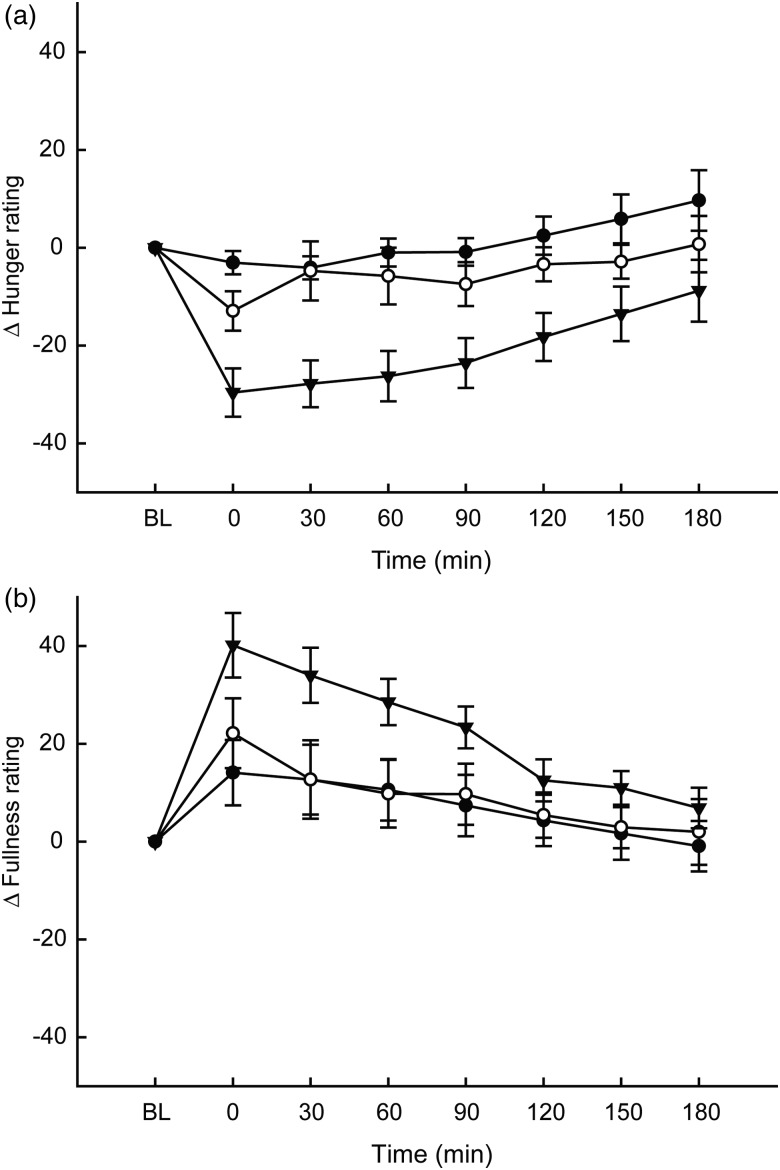
Hunger ratings showed a significant main effect of time (F(7,33) = 11·31; P < 0·001), breakfast group (F(1,33) = 9·105; P < 0·001) and breakfast group × time interaction (F(14,33) = 2·43; P = 0·003), but there was no effect of week (main effect or interactions); thus mean ratings over the 4 weeks are displayed (Fig. 1(a)). Mean change in hunger ratings from the baseline were significantly lower in the oat porridge group compared with the control (P < 0·001) and cornflakes (P = 0·006) groups.
Fig. 1.
Changes compared with baseline (BL) in subjective hunger (a) and fullness (b) ratings over 4 weeks in response to breakfasts consisting of oat porridge (▾; n = 12), frosted cornflakes (○; n = 12) and water (control) (•; n = 12). Values are means, with standard errors represented by vertical bars. Between-within ANOVA showed that there were significant main effects of time (P < 0·001), breakfast group (P < 0·001) and time × breakfast group interaction (P = 0·003) hunger ratings. Fullness ratings displayed a significant main effect of time (P < 0·001) and breakfast × time interaction (P = 0·034) for fullness ratings.
Fullness ratings
Fullness ratings showed a main effect of time (F(7,33) = 19·2; P < 0·001), and breakfast group × time interaction (F(14,33) = 1·84; P = 0·034), but there was no main effect of breakfast group or any effect of week (main effect or interaction); thus mean ratings over the 4 weeks are displayed (Fig. 1(b)). Mean change in fullness ratings from the baseline were significantly higher in the oat porridge group compared with in the control group (P = 0·036).
Discussion
The primary aim of the present study was to compare the effect of consuming oat porridge, a high-fibre cereal, Frosted Flakes, a non-fibre cereal, and a no-breakfast (water) control for 4 weeks on changes in body weight and composition in overweight individuals. Additionally, we investigated the effects on subjective appetite ratings and CVD risk factors. The results showed that changes in body weight differed between the group that skipped breakfast (control), and both groups that consumed a fixed-energy breakfast (oat porridge or cornflakes), but there was no difference between the groups that consumed porridge or frosted cornflakes for breakfast. Body fat change did not differ between the groups, and there were also no changes in lean mass. This may be due to the limitation of air displacement as a measure of body composition, which can be influenced by total body water content(26).
We propose that although skipping breakfast may result in an increase in later intake during the day, individuals may be unable to fully compensate for the energy from the missing meal, which results in a lower daily energy intake(13). In turn, this lower overall daily energy intake could cause the weight loss seen in the control group that did not eat breakfast during the 4-week intervention. These differences in body weight were observed despite participants in the oat porridge group reporting lower hunger compared with the control and cornflakes groups, and higher fullness compared with the control group. It is possible that despite the differences in appetite ratings between the fixed-energy breakfast groups, there was no difference in energy intake later in the day between the oat porridge and cornflakes groups. This would be consistent with reports that although a high-fibre breakfast elicited greater fullness compared with a low-fibre breakfast, subsequent energy intake did not differ between the groups(17,18).
It is important to note that although body-weight loss was greater in the control group relative to either the cornflakes or oat porridge groups, total cholesterol concentrations were also elevated in the control group that skipped breakfast. These findings are consistent with reports that skipping breakfast is associated with increases in cholesterol concentrations(12,27). Furthermore, although there were no significant differences in change in total cholesterol concentrations between the cornflakes and oat porridge groups, the pattern for a greater reduction in cholesterol in the oat porridge group may be due, in part, to the presence of the β-glucan soluble fibre, which can reduce cholesterol concentrations(20,28). There were no other between-group differences in the other CVD risk factors, which may be attributed in part to the relatively short study duration and small sample size.
Other limitations of the study include the absence of measures of total daily energy intake and physical activity patterns. Nevertheless, participants were requested not to change their usual activity routine during the study. Strengths of the present study include the careful supervision of subjects as they consumed the weekday breakfasts, and the careful matching of the two breakfast conditions for energy, weight, volume and energy density. However, despite matching for many attributes, the porridge breakfast contained 7 g more protein than the cornflakes breakfast, and although the total carbohydrate content of the porridge and frosted cornflakes was similar, the frosted cornflakes contained about 27 g more sugar. To match the volume of the two breakfasts, we incorporated water into the porridge and served water on the side of the frosted cornflakes breakfast. Even so, water served on the side may not be as filling as water incorporated in a food(29).
In summary, the present study shows that in overweight individuals, skipping breakfast daily for 4 weeks leads to a reduction in body weight, but this is accompanied by an increase in total cholesterol concentrations compared with consuming either a frosted cornflakes or oat porridge breakfast. There were no differences in changes in body weight or total cholesterol concentrations between the groups consuming the frosted cornflakes no-fibre breakfast or the group that consumed the high-fibre oat porridge breakfast. These findings suggest that although skipping breakfast may be the more effective strategy to achieve weight loss than eating breakfast, there are associated detrimental effects on total cholesterol concentrations.
Acknowledgements
We thank Yi Fang of PepsiCo for his helpful comments on the manuscript.
A. G. was responsible for the study conception and design, and supervised acquisition of the data and edited the manuscript. N. M. A. analysed the data, interpreted the findings and was responsible for drafting of the manuscript. R. A.-F. aided in editing the manuscript. E. Y. was responsible for the data acquisition and aided in editing the manuscript. S. H. provided medical supervision for the data acquisition, and edited the manuscript. All authors approved the final version of the manuscript.
The present study was funded by Quaker Oats Center of Excellence, PepsiCo R&D Nutrition. The funder contributed to the study design and editing of the manuscript.
A. G. received funding from Quaker Oats Center of Excellence, Pepsico R&D Nutrition for the design, conduct and analysis of the study and for the preparation of the manuscript. N. M. A., R. A.-F., E. Y. and S. H. have no conflicts of interest.
Supplementary material
The supplementary material for this article can be found at http://dx.doi.org/10.1017/jns.2014.51
References
- 1.Haines PS, Guilkey DK & Popkin BM (1996) Trends in breakfast consumption of US adults between 1965 and 1991. J Am Diet Assoc 96, 464–470. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, et al. (2012) Prevalence of Obesity in the United States. NCHS Brief Data no. 82. Hyattsville, MD: United States Department of Health and Human Services, Centers for Disease Control and Prevention. [Google Scholar]
- 3.Cho S, Dietrich M, Brown CJ, et al. (2003) The effect of breakfast type on total daily energy intake and BMI: results from the Third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr 22, 296–302. [DOI] [PubMed] [Google Scholar]
- 4.Ma Y, Bertone ER, Stanek EJ III, et al. (2003) Association between eating patterns and obesity in a free-living US adult population. Am J Epidemiol 158, 85–92. [DOI] [PubMed] [Google Scholar]
- 5.Albertson AM, Anderson GH, Crockett SJ, et al. (2003) Ready-to-eat cereal consumption: its relationship with BMI and nutrient intake of children aged 4 to 12 years. J Am Diet Assoc 103, 1613–1619. [DOI] [PubMed] [Google Scholar]
- 6.Berkey CS, Rockett HR, Gillman MW, et al. (2003) Longitudinal study of skipping breakfast and weight change in adolescents. Int J Obes Relat Metab Disord 27, 1258–1266. [DOI] [PubMed] [Google Scholar]
- 7.Wyatt HR, Grunwald GK, Mosca CL, et al. (2002) Long-term weight loss and breakfast in subjects in the National Weight Control Registry. Obes Res 10, 78–82. [DOI] [PubMed] [Google Scholar]
- 8.Hallström L, Labayen I, Ryiz JR, et al. (2013) Breakfast consumption and CVD risk factors in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr 16, 1296–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stanton JL Jr & Keast DR (1989) Serum cholesterol, fat intake, and breakfast consumption in the United States adult population. J Am Coll Nutr 8, 567–572. [DOI] [PubMed] [Google Scholar]
- 10.Sakata K, Matamura Y, Yoshimura N, et al. (2001) Relationship between skipping breakfast and cardiovascular disease risk factors in the National Nutrition Survey data (article in Japanese). Nihon Koshu Eisei Zasshi 48, 837–841. [PubMed] [Google Scholar]
- 11.Schlundt DG, Hill JO, Sbrocco T, et al. (1992) The role of breakfast in the treatment of obesity: a randomized clinical trial. Am J Clin Nutr 55, 645–651. [DOI] [PubMed] [Google Scholar]
- 12.Farshchi HR, Taylor MA & Macdonald IA (2005) Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr 81, 388–396. [DOI] [PubMed] [Google Scholar]
- 13.Levitsky DA & Paconowski CR (2013) Effect of skipping breakfast on subsequent energy intake. Physiol Behav 119, 9–16. [DOI] [PubMed] [Google Scholar]
- 14.Brown AW, Bohan Brown MM & Allison DB (2013) Belief beyond the evidence: using the proposed effect of breakfast on obesity to show 2 practices that distort scientific evidence. Am J Clin Nutr 98, 1298–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Astbury NM, Taylor MA & Macdonald IA (2011) Breakfast consumption affects appetite, energy intake, and the metabolic and endocrine responses to foods consumed later in the day in male habitual breakfast eaters. J Nutr 141, 1381–1389. [DOI] [PubMed] [Google Scholar]
- 16.Keim NL, van Loan MD, Horn MF, et al. (1997) Weight loss is greater with consumption of large morning meals and fat-free mass is preserved with large evening meals in women on a controlled weight reduction regimen. J Nutr 127, 75–82. [DOI] [PubMed] [Google Scholar]
- 17.Burley VJ, Leeds AR & Blundell JE (1987) The effect of high and low-fibre breakfasts on hunger, satiety and food intake in a subsequent meal. Int J Obes 11, Suppl. 1, 87–93. [PubMed] [Google Scholar]
- 18.Turconi G, Bazzano R, Caramella R, et al. (1995) The effects of high intakes of fibre ingested at breakfast on satiety. Eur J Clin Nutr 49, Suppl. 3, S281–S285. [PubMed] [Google Scholar]
- 19.Glore SR, van Treeck D, Knehans AW, et al. (1994) Soluble fiber and serum lipids: a literature review. J Am Diet Assoc 94, 425–436. [DOI] [PubMed] [Google Scholar]
- 20.Tiwari U & Cummins E (2011) Meta-analysis of the effect of β-glucan intake on blood cholesterol and glucose levels. Nutrition 27, 1008–1016. [DOI] [PubMed] [Google Scholar]
- 21.Garrow JS, James WPT & Ralph A (2000) Human Nutrition and Dietetics. Edinburgh: Churchill Livingstone. [Google Scholar]
- 22.Weir JB (1949) New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Korotkoff NC (1905) To the question of methods of determining the blood pressure (from the clinic of Professor CP Federoff). Reports of the Imperial Military Academy 11, 365. [Google Scholar]
- 24.Friedewald WT, Levy RI & Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18, 499–502. [PubMed] [Google Scholar]
- 25.Matthews DR, Hosker JP, Rudenski AS, et al. (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419. [DOI] [PubMed] [Google Scholar]
- 26.Frisard MI, Greenway FL & Delany JP (2005) Comparison of methods to assess body composition changes during a period of weight loss. Obes Res 13, 845–854. [DOI] [PubMed] [Google Scholar]
- 27.Cahill LE, Chiuve SE, Mekary RA, et al. (2013) Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 128, 337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bartram P, Gerlach S, Scheppach W, et al. (1992) Effect of a single oat bran cereal breakfast on serum cholesterol, lipoproteins, and apolipoproteins in patients with hyperlipoproteinemia type IIa. J Parenter Enteral Nutr 16, 533–537. [DOI] [PubMed] [Google Scholar]
- 29.Rolls BJ, Bell EA & Thorwart ML (1999) Water incorporated into a food but not served with a food decreases energy intake in lean women. Am J Clin Nutr 70, 448–455. [DOI] [PubMed] [Google Scholar]